Abstract
Most of the anti-methicillin-resistant Staphylococcus aureus drugs available in Japan are administered intravenously, except for linezolid, which can also be administered orally. Here, we report a lupus patient with methicillin-resistant S. aureus–induced osteomyelitis. Linezolid had to be stopped due to severe anemia. In an effort to treat her on an outpatient basis, we planned to use a combination of minocycline and trimethoprim–sulfamethoxazole that exhibited in vitro sensitivity against the methicillin-resistant S. aureus detected, and rifampicin is used against methicillin-resistant S. aureus in certain cases. The use of rifampicin increased the level of C-reactive protein even though the prednisolone dose used was doubled, so we gave up using it. The combined application of oral minocycline and trimethoprim–sulfamethoxazole, however, controlled the inflammation, and the patient was able to be discharged. Fourteen months later, we discontinued the administration of both drugs and there has been no relapse more than a year. This combination of antibiotics may be useful, especially when patients want to be treated on an outpatient basis.
Keywords: Methicillin-resistant Staphylococcus aureus, osteomyelitis, minocycline, trimethoprim–sulfamethoxazole, linezolid
Introduction
The treatment of osteomyelitis, especially when it is caused by methicillin-resistant Staphylococcus aureus (MRSA) infection, can be highly challenging.1 Linezolid (LZD) is the only oral anti-MRSA agent available in Japan. Thus, if LZD cannot be used due to its side effects, patients with osteomyelitis caused by MRSA may have to be kept in hospital for quite a long period of time. The transition from inpatient- to outpatient-basis treatment may require some trial-and-error process.
Case report
A 43-year-old woman afflicted with systemic lupus erythematosus (SLE) for over 22 years was referred to our department from the department of plastic surgery for further treatment. She was paraplegic due to lupus-related transverse myelitis below the level of thoracic vertebrae 6 (Th6), along with dysfunction of the bladder and bowel. She had been treated mainly at this hospital on an outpatient basis and been in remission with prednisolone (PSL) at a dose of 11 mg/day. In February 2014, an ischial decubitous ulcer was noticed. She was admitted to the department of plastic surgery of this hospital and an operation for the decubitus ulcer (i.e. debridement) was performed in June. MRSA (3+) and Corynebacterium species (1+) were detected in the wound. After the surgery, cefmetazole (1 g, twice daily) was administered for 5 days. During the hospitalization, she developed bilateral polyarthritis of finger and hand joints and was diagnosed with seronegative rheumatoid arthritis (RA) in July (Figure 1(a)). Salazosulfapyridine (SASP, 1 g/day) and tacrolimus (0.5 mg/day, increased to 1 mg/day after 18 days) were started, and SASP was changed to iguratimod (IGT, 25 mg/day) on September 24. IGT was increased to 50 mg/day after 28 days. In November, a subcutaneous abscess at the surgical site was discovered and debridement was performed on December 8. Escherichia coli (30 colonies) and Corynebacterium species (2+) were detected in the site. Tacrolimus was discontinued. On January 26, 2015, she was transferred to this department.
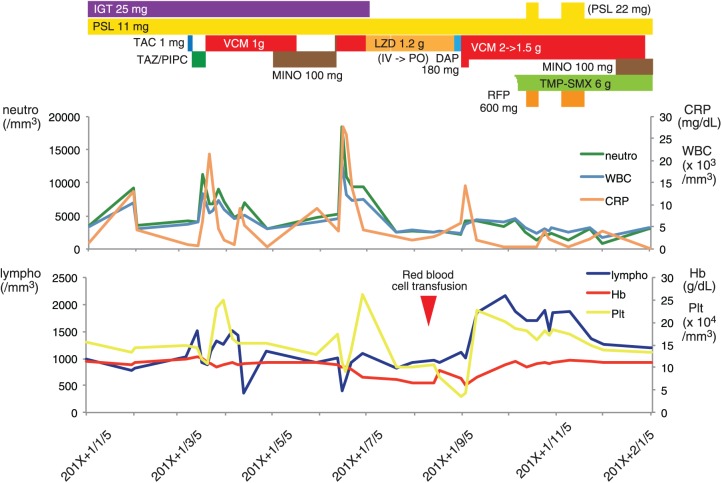
Figure 1.
T1-weighted image (T1WI) and gadolinium-enhanced T1-weighted image (T1WI + Gad) (a) of the right hand at the time of the diagnosis of RA (August 2014) and (b) of the wrist after cellulitis became apparent (April 2015). Note that the bone erosions became much more severe and that the gadolinium-enhancing lesions became more diffuse in (b), suggesting the presence of concomitant osteomyelitis.
When the patient came to this department, her body weight was 32.1 kg and height 158 cm. Her temperature was 36.6°C, blood pressure 105/72 mmHg, pulse 78 beats per minute and respiratory rate 18 breaths per minute, with 99% oxygen saturation while breathing ambient air. There were neither swollen nor tender joints. She had numbness below the costal arch. She could sit up by herself. She had a history of Sjogren’s syndrome with renal tubular acidosis and lupus nephritis (LN III + V, 1995 modified World Health Organization (WHO) classification). She also had recurrent bilateral ureteral stones and had undergone vesicostomy.
Tacrolimus was prescribed again in order to taper the dose of PSL. Two days after that, however, the swelling, tenderness, and warmth of the right-hand joint emerged. With the diagnosis of cellulitis, tazobactam/piperacillin (TAZ/PIPC, 4.5 g, three times a day) was administered the next day (Figure 2). As MRSA was detected from the blood culture (two of the four blood culture bottles drawn were positive for MRSA), vancomycin (VCM, 0.5 g, twice daily) was initiated and TAZ/PIPC was discontinued. The minimal inhibitory concentrations (MICs) for the MRSA strain detected were 1 µg/mL for VCM, 4 µg/mL for minocycline (MINO), ⩽0.5 µg/mL for trimethoprim–sulfamethoxazole (TMP-SMX), 2 µg/mL for LZD, and 0.75 µg/mL for daptomycin (DAP). The diffuse bone inflammation detected by magnetic resonance imaging (MRI) of the right wrist suggested the presence of osteomyelitis (Figure 1(b)). VCM was continued for 59 days. Two weeks before its cessation, oral MINO (50 mg, twice daily) was added. One week after the cessation of VCM, however, the swelling and tenderness of the right hand relapsed. The dose of MINO was increased to 100 mg, twice daily, but the next day, the blood pressure dropped suddenly to 64/42 mmHg and MRSA was detected again in the blood culture specimens (two of the two blood culture bottles were positive for MRSA). MINO was stopped and VCM was administered once again. She complained of back pain. On chest computed tomography (CT), a significant deformity of Th10 was discovered. Chest MRI was also performed and spondylitis in Th10 with an epidural abscess was discovered (Figure 3(a)). VCM was continued for 20 days and then switched to intravenous LZD (0.6 g, twice daily), which was in turn switched to oral LZD 16 days later. Progressive anemia became evident to the point that blood transfusion was necessary (hemoglobin 6.1 g/dL). Approximately 2 months after the initiation of LZD, it was switched to DAP (180 mg, once a day). Only 5 days after that, the serum level of C-reactive protein (CRP) increased and her blood pressure fell to 77/54 mmHg. VCM was readministered. Based on the susceptibility of the MRSA detected, we planned to control the infection by combined treatment of rifampicin (RFP), MINO and TMP-SMX. As the patient reportedly had experienced an allergy to TMP-SMX previously, rapid desensitization to TMP-SMX2 was performed from 0.005 to 6 g/day over a period of 6 days, which was successfully completed. We then tried twice to add RFP (300 mg, twice daily), each time with the PSL dose increased from 11 to 22 mg per day, but we had to give it up both times since the serum CRP level increased. We re-administered MINO (100 mg, once a day, which later increased to 150 mg, once a day) 9 months after the first episode of osteomyelitis of the right-hand joint; 20 days later, VCM was stopped. As no relapse of the local inflammation occurred, she was discharged. No MRSA has been isolated from blood culture thereafter. By the time of discharge, the initial decubitus wound had been fully epithelialized. Occasional paracenteses of subdermal fluid collection were performed by plastic surgeons. The fluid was slightly bloody but aseptic.
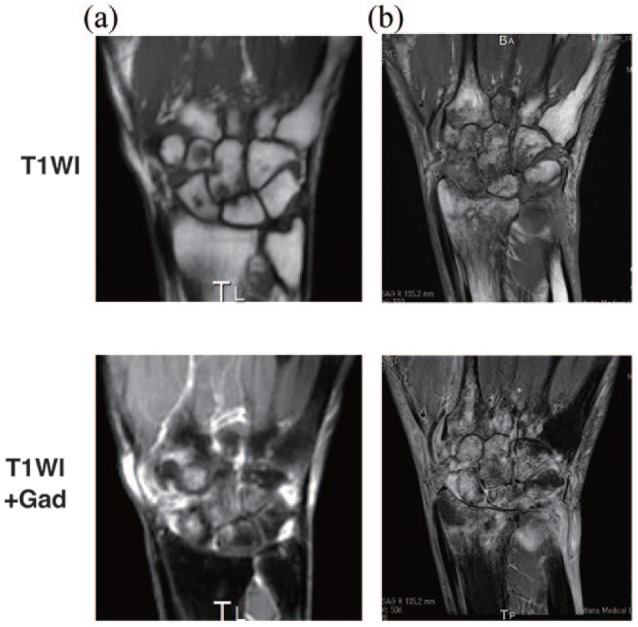
Figure 2.
Clinical course. While vancomycin (VCM) was administered, trough concentrations were monitored. They were maintained within the range of 13–20 µg/mL, except on 2015/9/11 (32.1 µg/mL), after which the dosage of VCM was reduced from 2 to 1.5 g/day.
IGT: iguratimod; PSL: prednisolone; TAC: tacrolimus; LZD: linezolid; TAZ/PIPC: tazobactam/piperacillin; DAP: daptomycin; MINO: minocycline; TMP-SMZ: trimethoprim–sulfamethoxazole; RFP: rifampicin; neutro: neutrophil; lympho: lymohocyte; Plt: platelet.
Figure 3.
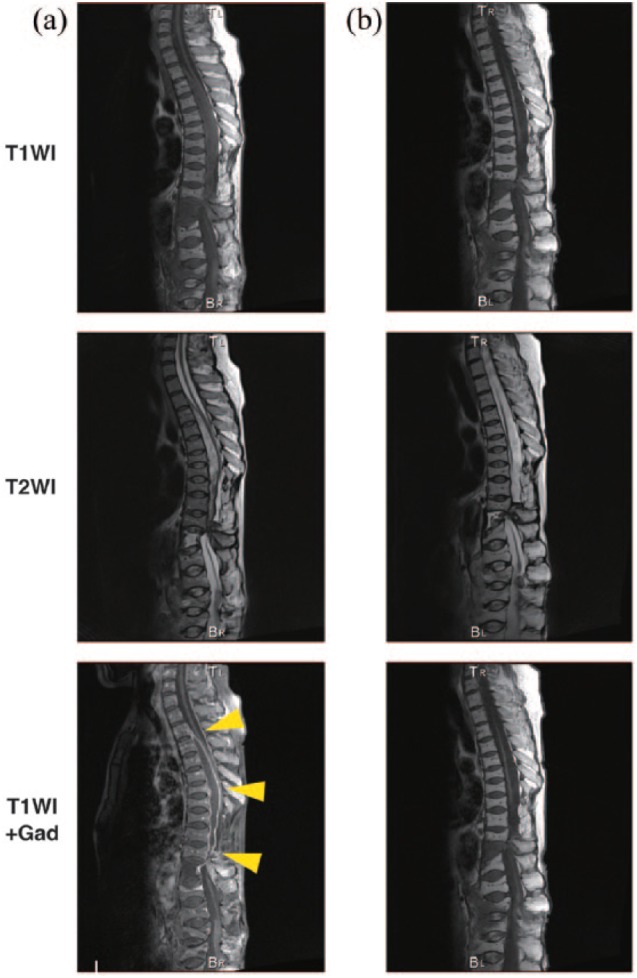
T1WI, T2WI, and T1WI + Gad of the thoracic vertebrae (a) at the time of the diagnosis of spondylitis (July 2015) and (b) at the end of the treatment (June 2016). The epidural abscess observed ranging from Th2 to Th10 (yellow arrowheads in (a)) had almost disappeared in (b).
Discussion
The swelling of the right-hand joint that had been considered to be due to RA at first instead turned out to be osteomyelitis. The possibility is not ruled out that the polyarthritis was of infectious origin from the outset. But we thought it was unlikely because disease-modified anti-rheumatic drugs (DMARDs) had proven to be effective against the polyarthritis and the initial diagnosis of RA was made 10 months before the discovery of osteomyelitis. When she was admitted to the department of plastic surgery for the treatment of the ischial ulcer, MRSA was already detected in the lesion. The sensitivity profiles of the MRSA isolated from the blood samples were almost identical, indicating that those bacteria shared a common origin. Thus, the lesion was likely the entry site of the bacteria. The patient experienced recurring exacerbation of osteomyelitis, and during this period, spondylitis of Th10 with an epidural abscess became evident. Strictly speaking, we could not prove that this spondylitis was caused by MRSA, since we did not perform drainage of the abscess. But the repetitive detection of MRSA in the blood culture specimens strongly indicated clinically that it was MRSA spondylitis. Due to her paraplegia, the patient may not have experienced the pain that would have been expected much earlier. Thus, the diagnosis of spondylitis was most likely delayed. It was thus not clear which of the two diseases was precedent: the osteomyelitis of the right hand or the spondylitis of Th10.
The treatment of osteomyelitis, especially the MRSA-induced type, is not simple. It is recommended to perform a surgical procedure when feasible.1 In this case, such a procedure seemed unrealistic because she had multiple infectious foci. Thus, we had little choice but to proceed with conservative treatment. Although VCM was effective, each time we tried to switch it to oral MINO, the inflammation relapsed. The trough concentrations of VCM were mostly maintained within the range of 15–20 µg/mL. As LZD can be administered both intravenously and orally, we thought it was a favorable substitute for VCM in terms of treating the patient on an outpatient basis. Unfortunately, it caused severe anemia that necessitated blood transfusion. Pure red cell anemia is one of the potential side effects of LZD.3 As the level of blood erythropoietin was high, a response to erythropoietin supplementation was not expected. Soon after the switch of LZD to DAP, the inflammation relapsed; the dose of DAP may have been insufficient. Whichever the case may be, DAP is not a realistic option for outpatient therapy since it is administered only intravenously.
Judging from the course of events, the conventional anti-MRSA agents available in Japan were evidently insufficient to enable discharge to home. Thus, we planned to use MINO and TMP-SMX, to which the MRSA detected were susceptible, along with RFP, a combination therapy which was reported to be effective against staphylococcal infections related to orthopedic surgery.4 Since RFP is only indicated for tuberculosis in this country, we applied to the institutional review board of this hospital for permission to use RFP against the MRSA infection. After receiving approval, RFP was administered twice, but both times the CRP level increased, so it had to be stopped. As RFP is known to accelerate the metabolism of glucocorticoids,5 we doubled the dose of PSL from 11 to 22 mg each time we used RFP. It may be that this increase in PSL was not ample enough. The signs of either adrenal insufficiency or worsening of the SLE were, however, not observed. Relapse of the local inflammation was not observed, either. Finally, we gave up on using RFP and switched the strategy to the combination therapy with MINO and TMP-SMX. Fortunately, this combination proved effective enough to decrease the level of CRP to the normal range, below 0.24 mg/dL, and even after the discontinuation of VCM, the remission continued. There is no reliable information on the appropriate duration of such treatment, but we continued using the combination for 14 months on an outpatient basis and we stopped it after the confirmation of the disappearance of the abscess (Figure 3(b)). No relapse of the local inflammation has since been observed.
Intravenous treatment is a difficult burden for most patients. It was recently reported that oral antibiotics in the management of bone and joint infection were noninferior to intravenous treatment when the drugs were appropriately selected.6 Although the study did not target MRSA infection, oral antibiotic therapy was associated with a shorter length of hospital stay and fewer complications. Thus, it is worth considering replacing intravenous treatment with oral treatment.
Conclusion
MRSA myelitis is a refractory condition that requires the long-term administration of antibiotics. LZD is the only oral anti-MRSA agent in Japan, but patients with MRSA osteomyelitis who are intolerant to LZD may be treated with the oral combination of MINO and TMP-SMX, and this combination is apparently worthy of consideration.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases.
Informed consent: Informed consent was obtained from the patient for anonymized patient information to be published in this article.
ORCID iD: Kojiro Sato  https://orcid.org/0000-0003-4105-3726
https://orcid.org/0000-0003-4105-3726
References
- 1. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis 2011; 52(3): 285–292. [DOI] [PubMed] [Google Scholar]
- 2. Yoshizawa S, Yasuoka A, Kikuchi Y, et al. A 5-day course of oral desensitization to trimethoprim/sulfamethoxazole (T/S) in patients with human immunodeficiency virus type-1 infection who were previously intolerant to T/S. Ann Allergy Asthma Immunol 2000; 85(3): 241–244. [DOI] [PubMed] [Google Scholar]
- 3. Green SL, Maddox JC, Huttenbach ED. Linezolid and reversible myelosuppression. JAMA 2001; 285: 1291. [DOI] [PubMed] [Google Scholar]
- 4. Holmberg A, Thorhallsdottir VG, Robertsson O, et al. 75% success rate after open debridement, exchange of tibial insert, and antibiotics in knee prosthetic joint infections. Acta Orthop 2015; 86(4): 457–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Strayhorn VA, Baciewicz AM, Self TH. Update on rifampin drug interactions, III. Arch Intern Med 1997; 157(21): 2453–2458. [PubMed] [Google Scholar]
- 6. Li HK, Rombach I, Zambellas R, et al. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med 2019; 380(5): 425–436. [DOI] [PMC free article] [PubMed] [Google Scholar]