Abstract
Community-based obesity prevention efforts are dependent on the strength and function of collaborative networks across multiple community members and organizations. There is little empirical work on understanding how community network structure influences obesity prevention capacity. We describe network structures within 19 local government communities prior to a large-scale community-based obesity prevention intervention, Healthy Together Victoria, Australia (2012–2015). Participants were from a large, multi-site, cluster randomized trial (cRCT) of a whole-of-systems chronic disease prevention initiative. Community leaders from 12 intervention and seven comparison (non-intervention) regions identified and described their professional networks in relation to dietary, physical activity, and weight status among young children (<5 years of age). Social network measures of density, modularity, clustering, and centrality were calculated for each community. Comparison of means and tests of association were conducted for each network relationship. One-hundred and seven respondents (78 intervention; 29 comparison) reported on 996 professional network relationships (respondent average per region: 10 intervention; 8 comparison). Networks were typically sparse and highly modular. Networks were heterogeneous in size and relationship composition. Frequency of interaction, close and influential relationships were inversely associated with network density. At baseline in this cRCT there were no significant differences between community network structures of key actors with influence over environments affecting children’s diet and physical activity. Tracking heterogeneity in both networks and measured outcomes over time may help explain the interaction between professional networks and intervention effectiveness of community-based obesity prevention.
Keywords: Social networks, Childhood, Obesity, Prevention, Community, Capacity
Community leadership networks were weakly connected prior to a statewide intervention. Increasing network cohesion is recommended in order to prevent childhood obesity, as it will better influence the environments in which children eat and are physically active.
Implications
Practice: Given the complexity of obesity, identifying capacity for community prevention efforts is critical.
Policy: Effective policy for increasing community obesity prevention capacity needs to consider the utilization of social network analysis methods to help identify existing capacity and inform potential intervention efforts.
Research: Future network research is needed to measure changes in network characteristics with intervention outcomes and process indicators to inform and adapt efforts for achieving program goals.
INTRODUCTION
Childhood obesity continues to be a major public health burden, associated with multiple co-morbidities in childhood [1] and in later life [2]. Despite some evidence of a recent plateau in obesity prevalence among some groups of children [3–5], rates remain at unacceptably high levels [6] and are predicted to increase [7]. Clearly, effective, population-level prevention is urgently required.
At a population level, community approaches to obesity prevention show promise in reducing excess weight gain in children [8]. Reviews of current efforts recognize the importance of taking a whole-of-systems approach to prevention, taking into consideration the complexity of factors contributing to obesity and the multiple strategies needed to achieve change and longer-term results [9, 10]. This includes having contextual understanding of the sociocultural environment in which working relationships for engaging communities are formed and developed [11], and harnessing capacity for intervention implementation and sustainability [8, 12]. It is vital that the beginnings of these working relationships are initiated prior to the intervention period and are nurtured and strengthened throughout and beyond for successful program adoption, implementation, and sustainability [13]. To ensure that the relationships are working effectively, it is imperative that they are regularly evaluated over time.
Social network analysis (SNA) provides an empirical method for describing the existence, complexity, and evolution of social relationships [14], which is critical for understanding the social context for program implementation. Within public health there has been some recent work exploring social networks associated with a range of health conditions and behaviors including: smoking [15]; substance use [16]; mental health, HIV practices, family planning, dieting, exercise [17]; obesity among adults [18, 19] and children [20–23]. Much of the existing obesity literature utilized social network approaches to explore the role of social influence on behavior change at an individual level [18–23]. Through the identification of patterns of behavior or social similarities and influence, SNA methods describe how obesity or related behaviors can spread through networks [18–23]; for example, the influence of peers in childhood and adolescence for engaging in obesity promoting or preventive behavior [21–23]. Although used to successfully explain behavior change at an individual level, the use of SNA can be extended.
SNA has further potential application as a planning, diagnostic, and evaluation tool in community-based public health interventions, providing insight into how relationships impact, or are impacted by, an intervention [13], and to monitor and inform progress towards intervention goals [24–26]. Valente et al. [13] suggest various network measures to identify and describe each stage of an intervention through an analysis of the formation, existence, and development of network structures over time. For example, an obesity prevention intervention for pre-school children designed to expand parental social networks was able to measure intervention success through increased network density and individual connectedness [27]. Network density is a measure of group cohesion, implying a high degree of connectedness facilitates information or behavior flow within a network [14]. Highly cohesive networks are, therefore, desirable in the early stages of an intervention, to support information flow while community capacity is being scoped and developed [25].
In addition to understanding the dynamics of network formation in new projects, SNA has the potential to support identification of potential network leaders for intervention implementation [28], and/or harnessing existing network capacity for information/policy/change diffusion [29, 30]. Schoen et al. [31] used measures of network density, centralization, and average degree (the average number of connections to/from an individual) to analyze partnership and collaboration development among different community networks implementing a range of obesity prevention and/or tobacco reduction programs. An increase in partnership development was demonstrated by higher network density and less network centralization across multiple communities [31].
The application of SNA techniques to understand and enhance public health intervention is very much an emerging field, and as such, many opportunities remain to be explored [13, 32–34]. Despite the increasing awareness that network connections of community leaders have a significant role to play in public health [32, 33, 35], there is little empirical work on understanding community leadership network structures that are explicitly hypothesized to be integral to obesity prevention success [36, 37]. This field is in its infancy, with further evidence within different settings and contexts needed for understanding the role of community-based networks in program development and implementation. The aim of this study was to use SNA methods to describe existing community-based obesity prevention network structures as a measure of potential capacity for childhood obesity prevention efforts across multiple communities in the Australian state of Victoria. In this paper, we aim to address the following research question:
What is the structure of community networks oriented towards prevention of childhood obesity?
Given that childhood obesity is a major public health concern, we expect to see some evidence of an existing infrastructure oriented towards prevention prior to intervention. Based on evidence from similar work [31], this would be apparent in existing levels of network density among professional health networks.
METHODS
Study design
This study was designed to characterize social networks at baseline within intervention and comparison communities (Healthy Together Communities) of the obesity prevention element of a government initiative called Healthy Together Victoria. Each community represents a local government area (LGA), one of 79 geographical and local government administrative divisions within the state of Victoria. Beginning in 2012, the Healthy Together Communities program, with a strong policy and leadership focus, delivered multiple strategies for creating system-wide health promoting environments within schools, workplaces, and early childhood services in 12 prevention areas across the state of Victoria, Australia [38]. Twelve randomized comparison LGAs were also identified, matched on socio-demographic indices (i.e., disadvantage, education, occupation, and resources) [39] and adult overweight/obesity prevalence [40], factors that may influence approaches to childhood obesity prevention. The present study collected social network data pertaining to the initiation of the trial in 2012 from key stakeholders retrospectively (during 2015) to ascertain existing network structures prior to intervention. Ethics clearance was received from the Deakin University Human Ethics Committee (HEAG-H 194_2014).
Sample
All intervention coordinators engaged within Healthy Together intervention communities were asked to identify personnel who were involved at the commencement of the program in relation to supporting healthy environments and behaviors for children under 5 years of age within their community. All identified relevant personnel were then contacted by email and invited into the study through the completion of an online social network survey. Within comparison communities, local government family and child services and maternal and child health services (who provide universal well-child health services from birth to age 5) were contacted by phone and asked to identify and provide a list of community leaders who play a role in decisions around diet and physical activity for children aged under 5 years within their community. Invitations to complete an online survey were sent by email where contact details were available. Where possible, email follow-up of non-responders were made over a 3-month period. Respondents comprised 116 of 191 individuals (61% RR) from 12 intervention communities, and 29 of 449 (6% RR) individuals from seven comparison communities.
Network survey
An online social network survey using the Qualtrics web-based platform (Qualtrics, Provo, UT) was developed to identify and examine key characteristics of professional networks prior to the commencement of the intervention. The survey comprised general demographic questions, for example, the participant’s main organization affiliation prior to intervention. Space was provided to list up to 20 names of people with whom they “discussed important matters (in particular the issue of diet, physical activity and weight gain in children) about [your community].” Respondents were asked to list names for those specifically with a role or influence on settings where children spend their time. Following the completion of relational questions on the first set of names, the online survey format allowed responses for up to a further 20 names and relational questions to be completed if required. Participants indicated completion of the online survey upon entering confirmation of their request to submit.
Relational and attribute questions were asked for each name listed: (i) main community affiliation (selected from list, e.g., local government); (ii) nature of network relationship (selected from list, e.g., co-worker); (iii) whether they discussed (a) health and well-being (yes/no), and/or (b) “obesity, unhealthy weight gain, diet and/or physical activity among children” issues (yes/no); (iv) frequency of interaction (from 1: daily, to 5: yearly); (v) closeness of relationship (from 1: not close, to 5: very close); and (vi) influence of information or advice about “obesity, unhealthy weight gain, diet and/or physical activity among children” issues (from 1: not at all, to 5: quite a lot).
Analysis
Thirty-eight incomplete surveys were removed, resulting in 107 available for analysis. “Completed” surveys for 18 of these participants (10 intervention; 8 comparison) contained no network data and it was inferred that these participants did not have networks with whom they discussed weight-related issues of children within their community. These data were retained for analysis.
Participant network and community characteristics are summarized at the intervention/comparison group level. Community demographics included population density, the proportion of the population under 5 years of age, and socioeconomic ranking. Affiliation response options “maternal and child health,” “long day care,” and “kindergarten” were grouped for reporting as “Early childhood service.” Descriptive analyses of professional network relationships and network metrics were reported by community network size (largest to smallest), determined by the number of participants (egos). Frequent interaction (“daily” + “weekly”), close relationships (“close” + “very close”), and influential (“a fair bit” + “quite a lot”) relationship variables were derived from respective response options.
Network metrics of degree, density, modularity, number of connected components, clustering, and centrality [14] were calculated for each community. Out-degree (the number of outward “ties” or “alters”) refers to the average number of people identified within a participant’s network; for example, the average number of contacts that leadership participants identify whom they discuss healthy weight status with. “Average degree” is the average number of both in-degree (nominations received by an individual) and out-degree ties. Density is a measure of the proportion of ties out of all possible ties within a network; for example, if all nodes (participants) were connected to one another, density would be 100%. Within this analysis, density is used to measure the extent that individuals identify one another within their network. Modularity is a measure of the degree of strength that a network can be divided into groups/modules. A highly modular network has dense connections within groups of individuals, and sparse connections to other modules/groups. This could give an indication of the level of independent subgroups within leadership networks. Connected components refer to the number of pairs/groups that are connected to one another within a network. A network with one connected component indicates all individuals are connected by paths directly or indirectly between one another with no isolated nodes or groups. Networks with multiple connected components, particularly those with low density, indicate gaps within networks; for example, communication not bridging one group to another within a leadership network. The clustering coefficient is a measure of average clustering within a network, i.e., the tendency for individuals to form in groups of three (triangle structures). Centrality is a measure of important, or well-connected, individuals within a network, who may be identified as key leaders within an obesity prevention intervention. Visual depictions of selected community networks are also presented for explanatory purposes.
Comparisons of means between intervention and comparison groups were conducted using t-tests. Tests for correlation between relationship variables, network metrics, and community demographics were conducted for each community network. Due to the number of networks with very few participants, analyses were repeated after excluding networks with less than five egos, to test whether network size differentiated results. Statistical significance was set at p < .05.
Descriptive analyses were performed using Stata 14.0 software (StataCorp LP, College Station, US). Network analysis and visualization were conducted using Gephi software, version 0.9.1.
RESULTS
Demographics
Completed surveys were received from 78 participants from 12 intervention (I) communities (I.1–I.12), and 29 participants from seven comparison (C) communities (C.1–C.7) (Table 1). The proportion of the population under 5 years of age (p = .85), population density (p = .75), and socioeconomic ranking (p = .65) were similar between intervention and comparison communities. Non-respondent comparison communities (data not shown) on average were ranked higher on the socioeconomic scale (decile 7, range 4–9) and had greater population density (mean 1,099 persons/km2). On average, the number of nominated contacts (out-degree) of professional networks identified by community leaders were similar (p = .11) within intervention (10) and comparison (8) communities. Participants were predominately female, and affiliated with state/local government or early childhood services. The nature of network relationships was similar between groups (predominately professional contacts or co-worker).
Table 1.
Community, participant, and network characteristics by intervention and comparison group at baseline
| Intervention | Comparison | Difference | ||
|---|---|---|---|---|
| n = 12 | n = 7 | p | ||
| Proportion of population <5 years of age | LGA mean % (range) | 7 (6–9) | 7 (6–9) | .849 |
| Population density (persons/km2) | LGA mean | 326 | 373 | .749 |
| Employed in education/healthcarea | LGA mean % | 18.8 | 19.7 | .617 |
| Index of advantage and disadvantageb | LGA mean ranking (range) | 6 (2–9) | 5 (3–8) | .645 |
| Participants | Total (mean per LGA) | 78 (7) | 29 (4) | .262 |
| Participant (ego) networks (out-degree) | Total (mean per ego) | 762 (10) | 234 (8) | .110 |
| Participant age, years | Mean (SD) | 41 (5) | 47 (8) | .089 |
| Participant sex | Female (%) | 76 (97) | 29 (100) | .279 |
| Participant community affiliation | ||||
| State/local government | N (%) | 29 (37) | 10 (34) | .188 |
| Early childhood servicec | N (%) | 25 (32) | 16 (55) | .017 |
| Other health/education | N (%) | 17 (22) | 2 (7) | .053 |
| Other | N (%) | 7 (9) | 1 (3) | .998 |
| Network community affiliations | ||||
| State/local government | N (%) | 246 (32) | 80 (35) | .066 |
| Early childhood servicec | N (%) | 167 (22) | 42 (19) | .108 |
| Other health/education | N (%) | 208 (27) | 57 (25) | .726 |
| Other | N (%) | 139 (18) | 48 (21) | .641 |
| Nature of network relationships | ||||
| Professional contact | N (%) | 359 (47) | 104 (44) | .412 |
| Colleague/co-worker | N (%) | 228 (30) | 94 (40) | .466 |
| Manager/employee | N (%) | 108 (14) | 25 (11) | .670 |
| Friend | N (%) | 25 (3) | 4 (2) | .200 |
| Other | N (%) | 40 (5) | 7 (3) | .943 |
Bold-face value denotes statistical significance at the p < .05 level.
LGA: Local government area; SD: standard deviation;
a% of employed population in Education & training, Health care & social assistance.
bSocio-Economic Index for Areas (SEIFA) decile ranking, low (1) to high (10).
cMaternal & Child Health, Long Day Care, Kindergarten.
Professional network relationships
Nine (7 intervention; 2 comparison) networks comprised a minimum of five egos, 10 networks (5 intervention; 5 comparison) had less than five egos (Table 2). Five comparison communities did not participate. On average, the proportion of networks for each professional relationship was higher within the larger networks. For example, 51% of connections in networks with ≥5 egos and 42% of connections in networks with <5 egos were described as influential relationships. Although participants were asked to nominate “people in [their] network with whom [they] discussed … diet, physical activity and weight gain in children …”, the proportion of network ties that discussed weight related issues (77%) was less on average than the proportion discussing general health issues (91%; p < .01).
Table 2.
Network metrics at baseline: Intervention (I) and Comparison (C) communities by number of egos per community
| Professional network relationships | Network metrics | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Communitya | Ego | Altersb | Discuss health?c | Discuss weight?d | Daily/weekly Interactione | Close relationshipsf | Influential relationshipsg | Communitya | Degreeh | Connectedk components | ||||||||||
| N | N | yes | % | yes | % | N | % | N | % | N | % | Out | Average | Densityi | Modularityj | Clusteringl | Centralitym | |||
| I.1 | 15 | 105 | 100 | 95 | 91 | 87 | 60 | 57 | 54 | 51 | 41 | 39 | I.1 | 7.0 | 2.0 | 0.02 | 0.78 | 9 | 0.02 | 0.03 |
| I.2 | 13 | 111 | 101 | 91 | 99 | 89 | 63 | 57 | 64 | 58 | 68 | 61 | I.2 | 8.5 | 2.0 | 0.02 | 0.80 | 6 | 0.01 | 0.04 |
| I.3 | 12 | 106 | 101 | 95 | 91 | 86 | 53 | 50 | 55 | 52 | 68 | 64 | I.3 | 8.8 | 2.1 | 0.02 | 0.72 | 7 | 0.03 | 0.01 |
| C.1 | 12 | 90 | 76 | 84 | 57 | 63 | 48 | 53 | 49 | 54 | 53 | 59 | C.1 | 7.5 | 1.8 | 0.02 | 0.83 | 11 | 0.00 | 0.00 |
| I.4 | 8 | 96 | 86 | 90 | 82 | 85 | 58 | 60 | 40 | 42 | 51 | 53 | I.4 | 12.0 | 2.0 | 0.02 | 0.79 | 4 | 0.01 | 0.02 |
| I.5 | 7 | 113 | 113 | 100 | 92 | 81 | 36 | 32 | 48 | 42 | 42 | 37 | I.5 | 16.1 | 2.1 | 0.02 | 0.73 | 3 | 0.04 | 0.00 |
| I.6 | 5 | 64 | 55 | 86 | 55 | 86 | 16 | 25 | 23 | 36 | 35 | 55 | I.6 | 12.8 | 2.6 | 0.05 | 0.48 | 1 | 0.18 | 0.00 |
| C.2 | 5 | 64 | 58 | 91 | 42 | 66 | 35 | 55 | 23 | 36 | 21 | 33 | C.2 | 12.8 | 1.9 | 0.03 | 0.73 | 3 | 0.00 | 0.00 |
| I.7 | 5 | 31 | 30 | 97 | 24 | 77 | 18 | 58 | 18 | 58 | 17 | 55 | I.7 | 6.2 | 1.7 | 0.05 | 0.74 | 5 | 0.00 | 0.00 |
| Subtotals | 82 | 780 | 720 | 92 | 633 | 81 | 387 | 50 | 374 | 48 | 396 | 51 | Average | 9.5 | 2.0 | 0.03 | 0.73 | 5 | 0.03 | 0.01 |
| I.8 | 4 | 41 | 21 | 51 | 8 | 20 | 28 | 68 | 17 | 41 | 2 | 5 | I.8 | 10.3 | 1.8 | 0.04 | 0.62 | 4 | 0.00 | 0.00 |
| C.3 | 3 | 40 | 40 | 100 | 28 | 70 | 10 | 25 | 19 | 48 | 20 | 50 | C.3 | 13.3 | 1.9 | 0.04 | 0.50 | 3 | 0.00 | 0.00 |
| C.4 | 3 | 16 | 14 | 88 | 0 | 0 | 1 | 6 | 1 | 6 | 0 | 0 | C.4 | 5.3 | 1.7 | 0.09 | 0.31 | 3 | 0.00 | 0.00 |
| I.9 | 3 | 13 | 12 | 92 | 10 | 77 | 4 | 31 | 6 | 46 | 11 | 85 | I.9 | 4.3 | 1.9 | 0.14 | 0.34 | 2 | 0.00 | 0.00 |
| I.10 | 2 | 38 | 38 | 100 | 34 | 89 | 25 | 66 | 23 | 61 | 22 | 58 | I.10 | 19.0 | 1.9 | 0.05 | 0.50 | 2 | 0.00 | 0.00 |
| I.11 | 2 | 27 | 25 | 93 | 24 | 89 | 11 | 41 | 12 | 44 | 18 | 67 | I.11 | 13.5 | 1.9 | 0.07 | 0.38 | 2 | 0.00 | 0.00 |
| I.12 | 2 | 17 | 9 | 53 | 6 | 35 | 5 | 29 | 7 | 41 | 4 | 24 | I.12 | 8.5 | 1.8 | 0.10 | 0.36 | 2 | 0.00 | 0.00 |
| C.5 | 2 | 14 | 12 | 86 | 11 | 79 | 5 | 36 | 5 | 36 | 9 | 64 | C.5 | 7.0 | 1.8 | 0.12 | 0.49 | 2 | 0.00 | 0.00 |
| C.6 | 2 | 8 | 8 | 100 | 5 | 63 | 5 | 63 | 4 | 50 | 3 | 38 | C.6 | 4.0 | 1.6 | 0.18 | 0.38 | 2 | 0.00 | 0.00 |
| C.7 | 2 | 2 | 2 | 100 | 2 | 100 | 2 | 100 | 2 | 100 | 2 | 100 | C.7 | 1.0 | 1.0 | 0.33 | 0.00 | 2 | 0.00 | 0.00 |
| Subtotals | 25 | 216 | 181 | 84 | 128 | 59 | 96 | 44 | 96 | 44 | 91 | 42 | Average | 8.6 | 1.7 | 0.12 | 0.39 | 2 | 0.00 | 0.00 |
| Total | 107 | 996 | 901 | 90 | 761 | 76 | 483 | 48 | 470 | 47 | 487 | 49 | Average | 9.3 | 1.9 | 0.07 | 0.55 | 4 | 0.02 | 0.01 |
aIntervention (I.1–I.12) or Comparison (C.1–C.7) community.
b“People in your network with whom you discussed important matters (in particular the issue of diet, physical activity and weight gain in children) about your community in relation to influence on places where children spend their time.”
c“Did you talk about issues for your community around health and wellbeing?”
d“Did you talk about issues for your community around obesity, unhealthy weight gain, diet and/or physical activity among children?”
e “Daily” and “Weekly” response options from: “How frequently did you typically interact with each person (in person, by mail, telephone or Internet)?”
f“Close” and “Very close” response options from: “How close was your relationship with each person?”
g“A fair bit” and “Quite a lot” response options from: “How influential was information/opinions/advice received, specifically about obesity, unhealthy weight gain, diet and/or physical activity issues.”
hOut-degree: average nominations per ego. Average degree: average of combined “in” and “out degree.”
iProportion of undirected ties out of all possible ties within the network.
jStrength of division of the network into modules/groups.
kNumber of “weakly” connected components within the network.
lDegree of clustering of nodes (participants) within the network.
mCentralization: measure of node importance within the network.
Large variations in the size of networks were found between communities in the following relationships: Discuss health (51–100%); Discuss weight (0–100%); Frequent interaction (6–100%); Close relationships (6–100%); Influential relationships (0–100%). These were not patterned according to network size.
Network metrics
Overall, baseline community networks were sparse (low density), weakly connected, with negligible clustering and centrality (Table 2). As network size (i.e., number of egos per network) increased, we observed slightly more connections per individual participant (higher average degree), lower network density, and increasing modularity. For example, C.1 had one of the highest number of respondents, yet has a very low density (2%) due to having more unrealized, yet potential network connections. With a greater number of unconnected people within the network, C.1 (modularity 83%) has the potential to be divided into subgroups/modules. Only one community (Intervention community I.6) had all members of the network reachable (1 connected component).
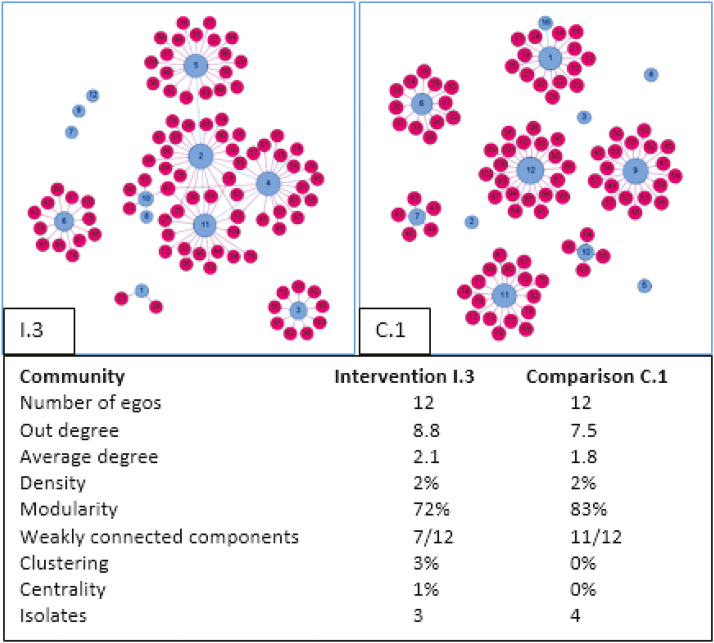
Low density and lack of connectedness can be represented visually in network diagrams. Some evidence of clustering and centrality was observed in larger networks among intervention communities only. For example, Fig. 1 depicts two community networks (I:3; C:1) representing LGAs with similar area-level characteristics. Both networks were of equal size (12 egos), weakly connected and sparse (2% density; 3–4 isolates). Intervention community I.3 has some clustering (3%) and centrality (1%) visualized by connections between some egos, compared with comparison community C.1 with no clustering or centrality; that is, in contrast to I.3, C.1 has only one connection between participants, or have any alters in common within their broader network.
Fig 1.
Sample of one Intervention (I) and one Comparison (C) professional early childhood obesity community network at baseline. Lighter colored nodes (circles) represent community respondents, while darker colored nodes represent alters—the people nominated by respondents as those with whom they discuss weight related issues for children within their community. Node size is proportional to out-degree.
Significance test between groups
Comparisons of means t-test results revealed no statistically significant differences between intervention and comparison groups for each relationship and social network metric. This was also true when excluding smaller networks from the analysis.
Correlations
Correlation coefficients between relational variables and network metrics are given in Table 3. Frequent interaction, close, and influential relationships were each negatively associated with density, and positively associated with modularity, the number of connected components, and centrality within community networks. For example, density (Frequent interaction: r = -.66, p < .01; Closeness: r = -.67; p < .01; Influence: r = -.61, p < .05). Average degree was positively associated with close (r = .49, p < .05) and influential (r = .54, p < .05) relationships. These metrics give an indication of small cohesive subgroups within leadership networks. After adjusting to exclude smaller networks, density continued to be negatively associated, and centrality positively associated, with interaction frequency and closeness of relationships. Frequency of interaction continued to be positively associated with modularity within the “larger communities,” that is, Close groups that frequently interacted were sparsely connected within their “larger” leadership network. No LGA demographic was significantly correlated with network metrics.
Table 3.
Network relationship and metric correlations for all communities and repeated for larger communities only
| Average degree | Density | Modularity | Connected components | Clustering | Centrality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Network relationship | r | p | r | p | r | p | r | p | r | p | r | p |
| All communities | ||||||||||||
| Daily/weekly Interaction | .41 | .08 | −.66 | .00 | .85 | .00 | .73 | .00 | .06 | .81 | .75 | .00 |
| Close relationships | .49 | .04 | −.67 | .00 | .82 | .00 | .73 | .00 | .17 | .48 | .71 | .00 |
| Influential relationships | .54 | .02 | −.61 | .01 | .74 | .00 | .64 | .00 | .27 | .26 | .65 | .00 |
| Larger communities onlya | ||||||||||||
| Daily/weekly Interaction | −.29 | .45 | −.88 | .00 | .69 | .04 | .58 | .10 | −.51 | .16 | .79 | .01 |
| Close relationships | −.10 | .80 | −.84 | .00 | .53 | .15 | .58 | .10 | −.29 | .44 | .68 | .05 |
| Influential relationships | .11 | .78 | −.66 | .05 | .30 | .43 | .42 | .26 | −.09 | .82 | .56 | .12 |
r, correlation coefficient; bold-face values denote statistical significance at the p < .05 level.
aExcluding communities with <5 participants.
DISCUSSION
This was among the first study to describe a large sample of professional childhood obesity prevention networks. In a comparison study between multiple intervention and comparison communities, we described professional community network structures prior to a state-wide community-based childhood obesity prevention intervention. Our results, that baseline community leadership networks in relation to addressing obesity were very sparse, weakly connected, and similar across communities, suggest there was not a well-organized infrastructure tasked with, or thinking about, responding to childhood obesity. This is concerning, given the continuing childhood obesity public health crisis that remains a challenge to address [41].
We observed similarities of low degree, low density, and weak connections throughout the networks. Some individuals appeared to be well connected (8–10 out-degree), despite being within very disconnected networks. Only one community network had everyone connected to at least one other person within their community, and more than half of the networks included isolates (individuals with no connections). Such sparse structures have limited pathways for communication and information flow [34]. Evidence from effective community coalition networks suggest increasing density would be a worthy initial goal to establish connections and cohesive community leadership, promote communication and shared goals necessary for design and dissemination of community intervention [25, 42]. Various network measures have been proposed for monitoring the effectiveness of interventions that improve network connectedness and diffuse behavior change [24]. To this end, it is suggested that network density should be at least 15%, and all individuals connected to at least one other person (no isolates) within a network. Applying these metrics, our baseline results, with an average density of the relatively larger networks (≥5 egos) of 2–3%, show that these communities would require the creation of further connections among community leaders to strengthen existing networks and build capacity for intervention implementation.
As stakeholders, mediators, and drivers, people are at the center of a system [43]. Centralization scores within the current study were negligible, meaning the leadership networks did not particularly focus on key individuals. Decentralized structures appear to be beneficial within preventive networks at early stages of implementation for the promotion of cohesive efforts between multiple players [25, 42, 44], as input from multiple parties is essential when system-wide impact is required. However, more centralized structures in later stages are suited towards efficient program coordination [25, 44] as there needs to be more directive leadership in the implementation stage. Several authors suggest that, once established, intervention diffusion requires identifying and engaging with people who can effectively drive system change [28, 36]. Without the initial identification of central figures, other network characteristics may help identify appropriate individuals or groups with whom to engage. For example, Kim et al. [45] throughout their randomized trial found friendship networks just as influential for delivering public health interventions compared with highly connected individuals (highest network degree). At baseline, within the current study, almost half of all individuals within networks interacted frequently, were close, and were influential in relation to information or advice around childhood obesity issues within the community. That low density was highly correlated with these variables indicates some leadership network capacity exists within modular structures of individuals and their immediate cohorts. The challenge would be to harness existing capacity of these modular units to work in partnership within the broader community network.
While there were similarities between community leadership networks, heterogeneity was also evident. Firstly, leadership networks within five comparison communities were not able to be identified due to non-response. Identifying the existence and structure of networks is important to determine whether networks first need to be formed or strengthened prior to program implementation [13]. Further, some indication of clustering and centrality was evident within intervention community networks only. Within the current study, it may be that networks in intervention communities were in early stages of responding to the prevention program, relative to comparison sites that were static. Follow-up work examining changes in these networks post implementation will identify whether differences between groups became more pronounced. For example, given what we know about the impact of interventions on network formation [27] and building community capacity [31], it will be important to identify whether intervention effects within multiple leadership networks improved connectivity through creation of new networks.
Study strengths and limitations
This study is among the first to quantify leadership networks aimed toward obesity prevention. Limitations include the potential for recall bias due to the retrospective nature of the study, which may have had a differential effect between intervention and comparison communities. This potential bias may be reflected in results from some intervention sites that indicated an emergence of developing networks, supporting evidence that obesity prevention interventions can create connections over time [27]. Identifying appropriate study participants within comparison communities was challenging. Low responses within some communities may have resulted in the inadvertent omission of key respondents and important elements of leadership networks in the community. Network metrics within these communities do not elucidate meaningful information, for example, centralization with only two network members. This lack of data would not allow a complete study of a full bounded network for analysis to be performed. Response rates within comparison communities were a result of sampling methods, whereby invitations were sent to individuals from unvetted, sometimes very long, lists provided by community contacts. These lists predominately included names of workers in early childhood services, rather than leaders necessarily. A sensitivity analysis removing these smaller, low response rate networks did not, however, have a significant impact on the overall findings. It is difficult to ascertain whether heterogeneity of network size and composition are a function of sampling issues, or a true reflection of the state of readiness for addressing childhood obesity within these communities. This potential limitation was partly overcome with the strength of the clustered randomized controlled study design and recruitment of community leaders. Intervention and comparison network members were similar in demographic characteristics, a reflection of the Australian health [46] and education [47] workforce, implying the appropriate individuals were recruited into the study. Further, results from this study are context specific, and may not be generalizable outside of the health promotion workforce structure identified within these communities at the given time.
Implications for policy and practice
Studies of community-based obesity preventions have observed anecdotally the importance of strong partnerships and collaboration between community members, generally without quantification [36, 37, 48]. This study used network analysis to quantify, describe, and compare community leadership networks in communities at a time when they were commencing participation in a large-scale multi-site intervention. Given the complexity of the problem of obesity [49], capacity among community leadership is critical for implementing interventions that involve community engagement and working in partnerships for broad reach within a community [12, 50].
Findings from the current study suggest that there may be limited existing community networks with orientation towards childhood obesity prevention. This points to a critical task and potential policy target in the development and establishment of interventions that actively build community capacity and activate, enhance, or reorient existing networks to respond to childhood obesity. It is clear that obesity prevention program planning in communities cannot assume the pre-existence of strong networks through which the intervention may diffuse to the broader community.
The preliminary evidence from this study, showing relatively weak and sparse networks, also supports a case for collection and analysis of SNA data among the nascent community leadership group, before the commencement of an intervention, to identify the structure of existing networks and the strengths and weaknesses of those networks for supporting the intervention. Leadership networks with properties such as low density and disconnected components require an increase in connections in order to improve information flow and group cohesion. Communities with these network structures may benefit from deliberate fostering of increased connections through facilitated group building or co-participation in structured planning activities with a focus on childhood obesity prevention. Potential strategies may include the establishment of a community steering committee or action coalition to support the intervention, bringing together leaders who may not currently connect in relation to obesity prevention. Baseline network data such as that demonstrated in this study may assist in identifying key actors who will enhance the connection of the intervention with strategic community groups and other potential leaders. Given the importance of partnerships and collaboration for implementation capacity, strategies for the identification, development, activation, and alignment of prevention networks will be a critical first step in making any intervention successful [12, 13].
Future research
Further understanding is needed on the role of social networks for informing future public health intervention and implementing change. The deliberate study and building of networks is an important element that needs to be included in any community-based intervention. Used as a diagnostic tool over the course of an intervention, social network data can play a critical role in the evaluation and alignment of program outcomes [24].
In individual communities, SNA data collected before intervention commencement could in the future be used to identify key people to champion policy change at a community, state, or federal level; people with the influence, contacts, and knowledge to advocate for change. Further, SNA data collected at regular intervals throughout an intervention can provide insights into how networks develop in response to the intervention, the manner in which the intervention is diffusing through the community, and help to identify groups and parts of the system that have not been reached.
Success of Healthy Together Victoria will be assessed in terms of reduced childhood obesity prevalence and changes in community systems of influence to address the problem [40]. Future research is required to understand how the characteristics of leadership networks relate to these intervention outcomes. This may be achieved through tracking of heterogeneous network structures and characteristics alongside measured intervention outcomes over time.
CONCLUSION
SNA provides an alternate means to understand the ways in which key actors and relationships are structured and change over the period of an intervention. This has implications for intervention planning, evaluation, and real-time adjustment. Our findings that baseline community leadership obesity prevention networks were sparse and disconnected, stresses that efforts are needed to strengthen connections for intervention effectiveness. The potential to optimize effectiveness and understand and corral human resource is of particular importance to underserved populations and others where mobilizing resources for population prevention is challenging.
Acknowledgements
We would like to acknowledge the support of the Childhood Obesity Modelling for Prevention And Community Transformation (COMPACT) research group, and the Victorian Department of Health and Human Services. S. Allender is supported by funding from an Australian National Health and Medical Research Council/Australian National Heart Foundation Career Development Fellowship (APP1045836). Aspects of this study were supported by the following grants: the US National Institutes of Health Systems Science to Guide Whole-of-Community Childhood Obesity Interventions (1R01HL115485-01A1), NHMRC Centre for Research Excellence in Obesity Policy and Food Systems (APP1041020).
Compliance With Ethical Standards
Conflict of Interest: The authors declare that they have no conflicts of interest.
Primary Data: Findings reported here have not been previously published, and this manuscript is not being simultaneously submitted elsewhere. The authors have full control of all primary data and agree to allow Translational Behavioral Medicine to review data if requested.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr. 2013;13(1):6–13. [DOI] [PubMed] [Google Scholar]
- 2. Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond). 2011;35(7):891–898. [DOI] [PubMed] [Google Scholar]
- 3. Olds TS, Tomkinson GR, Ferrar KE, Maher CA. Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. Int J Obes (Lond). 2010;34(1):57–66. [DOI] [PubMed] [Google Scholar]
- 4. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. Jama. 2014;311(8):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nichols MS, Silva-Sanigorski AD, Cleary JE, Goldfeld SR, Colahan A, Swinburn BA. Decreasing trends in overweight and obesity among an Australian population of preschool children. Int J Obes (Lond). 2011;35(7):916–924. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization. Facts and figures on childhood obesity [Fact sheet] Available at http://www.who.int/end-childhood-obesity/facts/en/. Accessibility verified October 31, 2016.
- 7. Haby MM, Markwick A, Peeters A, Shaw J, Vos T. Future predictions of body mass index and overweight prevalence in Australia, 2005–2025. Health Promot Int. 2012;27(2):250–260. [DOI] [PubMed] [Google Scholar]
- 8. Wolfenden L, Wyse R, Nichols M, Allender S, Millar L, McElduff P. A systematic review and meta-analysis of whole of community interventions to prevent excessive population weight gain. Prev Med. 2014;62:193–200. [DOI] [PubMed] [Google Scholar]
- 9. NICE. Preventing obesity using a whole system approach at local and community level: National Institute for Health and Clinical Excellence Available at http://guidance.nice.org.uk/PHG/Wave20/53. Accessibility verified December 3, 2010.
- 10. Wang Y, Cai L, Wu Y, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16(7):547–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Allender S, Owen B, Kuhlberg J, et al. A community based systems diagram of obesity causes. PLoS One. 2015;10(7):e0129683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. King L, Gill T, Allender S, Swinburn B. Best practice principles for community-based obesity prevention: development, content and application. Obes Rev. 2011;12(5):329–338. [DOI] [PubMed] [Google Scholar]
- 13. Valente TW, Palinkas LA, Czaja S, Chu KH, Brown CH. Social network analysis for program implementation. PLoS One. 2015;10(6):e0131712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wasserman S, Faust K.. Social network analysis: methods and applications. New York: Cambridge University Press; 1994. [Google Scholar]
- 15. Seo DC, Huang Y. Systematic review of social network analysis in adolescent cigarette smoking behavior. J Sch Health. 2012;82(1):21–27. [DOI] [PubMed] [Google Scholar]
- 16. Jacobs W, Goodson P, Barry AE, McLeroy KR. The role of gender in adolescents’ social networks and alcohol, tobacco, and drug use: a systematic review. J Sch Health. 2016;86(5):322–333. [DOI] [PubMed] [Google Scholar]
- 17. Latkin CA, Knowlton AR. Social network assessments and interventions for health behavior change: a critical review. Behav Med. 2015;41(3):90–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Powell K, Wilcox J, Clonan A, et al. The role of social networks in the development of overweight and obesity among adults: a scoping review. BMC Public Health. 2015;15:996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. [DOI] [PubMed] [Google Scholar]
- 20. Salvy SJ, Bowker JC. Peers and obesity during childhood and adolescence: a review of the empirical research on peers, eating, and physical activity. J Obes Weight Loss Ther. 2014;4(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Macdonald-Wallis K, Jago R, Sterne JA. Social network analysis of childhood and youth physical activity: a systematic review. Am J Prev Med. 2012;43(6):636–642. [DOI] [PubMed] [Google Scholar]
- 22. Sawka KJ, McCormack GR, Nettel-Aguirre A, Hawe P, Doyle-Baker PK. Friendship networks and physical activity and sedentary behavior among youth: a systematized review. Int J Behav Nutr Phys Act. 2013;10:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sawka KJ, McCormack GR, Nettel-Aguirre A, Swanson K. Associations between aspects of friendship networks and dietary behavior in youth: findings from a systematized review. Eat Behav. 2015;18:7–15. [DOI] [PubMed] [Google Scholar]
- 24. Gesell SB, Barkin SL, Valente TW. Social network diagnostics: a tool for monitoring group interventions. Implement Sci. 2013;8:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bess KD. Reframing coalitions as systems interventions: a network study exploring the contribution of a youth violence prevention coalition to broader system capacity. Am J Community Psychol. 2015;55(3–4):381–395. [DOI] [PubMed] [Google Scholar]
- 26. Trickett EJ, Beehler S, Deutsch C, et al. Advancing the science of community-level interventions. Am J Public Health. 2011;101(8):1410–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gesell SB, Bess KD, Barkin SL. Understanding the social networks that form within the context of an obesity prevention intervention. J Obes. 2012;2012:749832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Marks J, Barnett LM, Foulkes C, Hawe P, Allender S. Using social network analysis to identify key child care center staff for obesity prevention interventions: a pilot study. J Obes. 2013;2013:919287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Schell SF, Luke DA, Schooley MW, et al. Public health program capacity for sustainability: a new framework. Implement Sci. 2013;8:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Leeman J, Myers AE, Ribisl KM, Ammerman AS. Disseminating policy and environmental change interventions: insights from obesity prevention and tobacco control. Int J Behav Med. 2015;22(3):301–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schoen MW, Moreland-Russell S, Prewitt K, Carothers BJ. Social network analysis of public health programs to measure partnership. Soc Sci Med. 2014;123:90–95. [DOI] [PubMed] [Google Scholar]
- 32. Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Annu Rev Public Health. 2012;33:357–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sabot K, Wickremasinghe D, Blanchet K, Avan B, Schellenberg J. Use of social network analysis methods to study professional advice and performance among healthcare providers: a systematic review. Syst Rev. 2017;6(1):208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Valente TW. Social networks and health: models, methods, and applications. New York: Oxford University Press; 2010. [Google Scholar]
- 35. Mabry PL, Kaplan RM. Systems science: a good investment for the public’s health. Health Educ Behav. 2013;40(1 suppl):9S–12S. [DOI] [PubMed] [Google Scholar]
- 36. de Groot FP, Robertson NM, Swinburn BA, de Silva-Sanigorski AM. Increasing community capacity to prevent childhood obesity: challenges, lessons learned and results from the Romp & Chomp intervention. BMC Public Health. 2010;10:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Economos CD, Curtatone JA. Shaping up Somerville: a community initiative in Massachusetts. Prev Med. 2010;50(suppl 1):S97–S98. [DOI] [PubMed] [Google Scholar]
- 38. Department of Health and Human Services Victoria. Creating a healthier Victoria through a whole of systems approach. 2015. Available at https://www2.health.vic.gov.au/about/publications/policiesandguidelines/What-is-Healthy-Together-Victoria. Accessibility verified January 5, 2017. [Google Scholar]
- 39. Australian Bureau of Statistics. 2011 Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia (2033.0.55.001 released March 28, 2013). Available at http://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001. Accessibility verified May 6, 2013.
- 40. Strugnell C, Millar L, Churchill A, et al. Healthy together Victoria and childhood obesity—a methodology for measuring changes in childhood obesity in response to a community-based, whole of system cluster randomized control trial. Arch Public Health. 2016;74:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:1–212. [DOI] [PubMed] [Google Scholar]
- 42. Valente TW, Chou CP, Pentz MA. Community coalitions as a system: effects of network change on adoption of evidence-based substance abuse prevention. Am J Public Health. 2007;97(5):880–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. de Savigny D, Adam T.. Systems thinking for health systems strengthening. Geneva: WHO Press; 2009. Available at http://www.who.int/alliance-hpsr/resources/9789241563895/en/index.html. Accessibility verified March 20, 2011. [Google Scholar]
- 44. Feinberg ME, Riggs NR, Greenberg MT. Social networks and community prevention coalitions. J Prim Prev. 2005;26(4):279–298. [DOI] [PubMed] [Google Scholar]
- 45. Kim DA, Hwong AR, Stafford D, et al. Social network targeting to maximise population behaviour change: a cluster randomised controlled trial. Lancet. 2015;386(9989):145–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Australian Institute of Health and Welfare. Who is in the health workforce?2014. . Available at http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129547595. Accessibility verified April 6, 2017.
- 47. Weldon P. The teacher workforce in Australia: supply, demand and data issues. Camberwell: Australian Council for Educational Research; 2015. [Google Scholar]
- 48. Bolton KA, Kremer P, Gibbs L, Swinburn B, Waters E, de Silva A. Expanding a successful community-based obesity prevention approach into new communities: challenges and achievements. Obes Res Clin Pract. 2016;10(2):197–206. [DOI] [PubMed] [Google Scholar]
- 49. World Health Organization. Obesity and overweight [Fact sheet] Available at http://www.who.int/mediacentre/factsheets/fs311/en/. Accessibility verified November 12, 2015.
- 50. Millar L, Robertson N, Allender S, Nichols M, Bennett C, Swinburn B. Increasing community capacity and decreasing prevalence of overweight and obesity in a community based intervention among Australian adolescents. Prev Med. 2013;56(6):379–384. [DOI] [PubMed] [Google Scholar]