Abstract
Objective
To assess the association between stress related disorders and subsequent risk of cardiovascular disease.
Design
Population based, sibling controlled cohort study.
Setting
Population of Sweden.
Participants
136 637 patients in the Swedish National Patient Register with stress related disorders, including post-traumatic stress disorder (PTSD), acute stress reaction, adjustment disorder, and other stress reactions, from 1987 to 2013; 171 314 unaffected full siblings of these patients; and 1 366 370 matched unexposed people from the general population.
Main outcome measures
Primary diagnosis of incident cardiovascular disease—any or specific subtypes (ischaemic heart disease, cerebrovascular disease, emboli/thrombosis, hypertensive diseases, heart failure, arrhythmia/conduction disorder, and fatal cardiovascular disease)—and 16 individual diagnoses of cardiovascular disease. Hazard ratios for cardiovascular disease were derived from Cox models, after controlling for multiple confounders.
Results
During up to 27 years of follow-up, the crude incidence rate of any cardiovascular disease was 10.5, 8.4, and 6.9 per 1000 person years among exposed patients, their unaffected full siblings, and the matched unexposed individuals, respectively. In sibling based comparisons, the hazard ratio for any cardiovascular disease was 1.64 (95% confidence interval 1.45 to 1.84), with the highest subtype specific hazard ratio observed for heart failure (6.95, 1.88 to 25.68), during the first year after the diagnosis of any stress related disorder. Beyond one year, the hazard ratios became lower (overall 1.29, 1.24 to 1.34), ranging from 1.12 (1.04 to 1.21) for arrhythmia to 2.02 (1.45 to 2.82) for artery thrombosis/embolus. Stress related disorders were more strongly associated with early onset cardiovascular diseases (hazard ratio 1.40 (1.32 to 1.49) for attained age <50) than later onset ones (1.24 (1.18 to 1.30) for attained age ≥50; P for difference=0.002). Except for fatal cardiovascular diseases, these associations were not modified by the presence of psychiatric comorbidity. Analyses within the population matched cohort yielded similar results (hazard ratio 1.71 (1.59 to 1.83) for any cardiovascular disease during the first year of follow-up and 1.36 (1.33 to 1.39) thereafter).
Conclusion
Stress related disorders are robustly associated with multiple types of cardiovascular disease, independently of familial background, history of somatic/psychiatric diseases, and psychiatric comorbidity.
Introduction
Most people are, at some point during their life, exposed to psychological trauma or stressful life events such as the death of a loved one, a diagnosis of life threatening illness, natural disasters, or violence.1 2 Accumulating evidence suggests that such adversities might lead to an increased risk of several major diseases (including cardiovascular morbidity, injury, infection, and certain autoimmune diseases but not cancer) and mortality,3 4 5 6 7 8 9 10 with the largest risk elevations usually noted among people who develop psychiatric disorders as a result of their trauma.11 12 13
Stress related disorders are a group of psychiatric disorders for which one of the diagnostic criteria is the presence of a preceding stressful life event. Depending on the type of stressor, the reported symptoms, and their duration, such disorders are mainly categorised as acute stress reaction, post-traumatic stress disorder (PTSD), and adjustment disorder.14 The presence of a life threatening traumatic event is a prerequisite for the former two disorders, whereas adjustment disorder generally refers to physical or psychological distress (“adjustment syndromes”15) triggered by an identifiable and significant life change. PTSD is the most severe and widely studied form of stress related disorder, characterised by re-experiencing, avoidance, negative cognitions and mood, and hyperarousal following the traumatic event.16 We summarised the existing evidence on PTSD and cardiovascular consequences from 11 prospective cohort investigations (see supplementary table A), all of which suggested an elevated incidence of cardiovascular diseases among people with PTSD. However, owing to sample size restrictions of previous studies, the evidence for the role of PTSD in specific types of cardiovascular disease is still limited. Furthermore, the potential role of other stress related disorders—acute stress reaction, adjustment disorder, and other stress reactions—in the development of cardiovascular disease remains largely unexplored. Finally, cardiovascular diseases tend to have a genetic predisposition, as well as risk factors related to lifestyle and comorbidities that may cluster within families and exert an as yet unknown influence on the association between stress related disorders and cardiovascular disease.17 18 19
Taking advantage of the nationwide population and health registers in Sweden, which provide virtually complete information on all medical diagnoses and family links, we did a population based sibling analysis and a matched cohort study to elucidate the role of stress related disorders in the development of cardiovascular disease while controlling for familial confounders, history of psychiatric and somatic conditions, and psychiatric comorbidities.
Methods
Study design
The Swedish personal identification number uniquely assigned to all residents in Sweden at birth or immigration enables data linkage across several nationwide registers in Sweden.20 We first identified an exposed cohort of all people born in Sweden who received their first diagnosis of a stress related disorder between 1 January 1987 and 31 December 2013 (n=156 537; fig 1) from the Swedish National Patient Register. The National Patient Register has nationwide information on inpatient care since 1987 and on hospital based outpatient specialist care since 2001 (with initial coverage of >80%). We excluded patients who received a diagnosis before age 5 (n=139),21 had a history of any cardiovascular disease before the diagnosis of a stress related disorder (n=15 899), or had conflicting information (died or emigrated before the diagnosis of a stress related disorder; n=24). To enable the complete familial links from the Swedish Multi-Generation Register that includes largely complete familial information for people born in Sweden from 1932 onward, we excluded 3838 people born before 1932, leaving 136 637 patients in the analysis. We considered patients with stress related disorders to be exposed from the date of their diagnosis.
Fig 1.
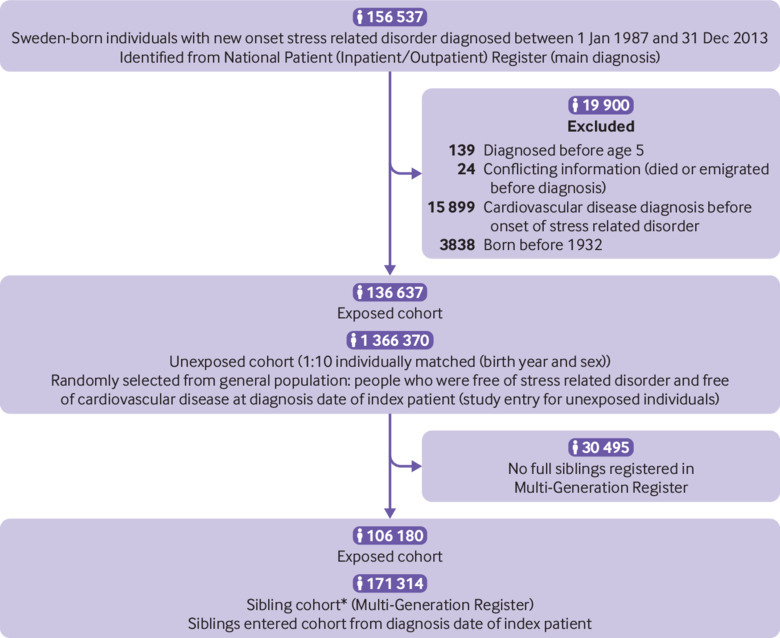
Study design. CVD=cardiovascular disease. *4332 families had more than one identified case of stress related disorder
Sibling cohort
To control for the familial components,22 we identified 106 180 clusters of full siblings discordant for stress related disorders with a total of 171 314 unaffected full siblings who were alive and free of stress related disorders and cardiovascular disease at the diagnosis date of the affected sibling, through the Multi-Generation Register. We used the date of diagnosis of the affected sibling as the index date for both siblings.
Population matched cohort
We compared the patients with stress related disorders with the general population in a matched cohort. For each exposed patient, we randomly selected 10 people from the Total Population Register who were free of stress related disorders and cardiovascular disease at the diagnosis date of the index patient. Exposed patients and unexposed people were individually matched by birth year and sex. We used the date of diagnosis as the index date for both exposed patients and the matched individuals.
Follow-up
Follow-up of all study participants was from the index date until the first primary diagnosis of cardiovascular disease (any or specific subtype), death, emigration, or the end of follow-up (31 December 2013), whichever occurred first. The follow-up time for the unaffected full siblings or matched unexposed people was additionally censored at the time of their first diagnosis of stress related disorder, if any, during the follow-up.
Definition of stress related disorders
We defined stress related disorders as any first outpatient or inpatient visit with the main diagnosis of the 9th or 10th Swedish revisions of the international classification of diseases (ICD) codes 308 or 309 (ICD-9) or F43 (ICD-10), according to the National Patient Register. We further divided stress related disorders into PTSD (ICD-9: 309B; ICD-10: F43.1), acute stress reaction (ICD-9: 308, 309A; ICD-10: F43.0), and adjustment disorder and other stress reactions (ICD-9: 309X; ICD-10: F43.8, F43.9). Because PTSD may initially be preceded by acute stress reaction or other stress related disorders,23 we considered all patients who received a diagnosis of PTSD within one year after their first stress related disorder diagnosis to be PTSD patients.
Definition of cardiovascular diseases
We defined an incident cardiovascular disease event (any; specific subtypes including ischaemic heart disease, cerebrovascular disease, emboli/thrombosis, hypertensive disease, heart failure, and arrhythmia/conduction disorder; or individual events) as an outpatient or inpatient visit (according to the National Patient Register) with a main diagnosis of cardiovascular disease or as a death (according to the Cause of Death Register) with cardiovascular disease as the underlying cause, using corresponding ICD codes (see supplementary table B). We defined a fatal cardiovascular disease as death within 30 days after an incident cardiovascular disease event.24
Covariates
Stress related disorders show substantial comorbidity with other psychiatric disorders, such as mood and anxiety disorders.25 We therefore defined other psychiatric disorders as “history of other psychiatric disorders” if the first diagnosis was made more than three months before the diagnosis of a stress related disorder. We defined other psychiatric disorders that had a first diagnosis made within three months before and one year after the diagnosis of a stress related disorder as “psychiatric comorbidity.” Diagnoses of other psychiatric disorders also came from the National Patient Register (ICD-8: 290-319 except 307, 308.4; ICD-9: 290-319 except 308, 309; and ICD-10: F10-F99 except F43).
We retrieved information about educational level, family income, and marital status from the Longitudinal Integration Database for Health Insurance and Labor Market. History of severe somatic diseases, including chronic pulmonary disease, connective tissue disease, diabetes, renal diseases, liver diseases, ulcer diseases, and HIV infection/AIDS, which are considered to contribute to survival time,26 were collected on the basis of the National Patient Register (ICD codes listed in supplementary table B). We defined family history of cardiovascular disease as any cardiovascular event among any first degree relatives (that is, biological parents and full siblings) of the participants according to the National Patient Register and the Cause of Death Register. In all analyses, we used the most recent information before the index date for each covariate, except for psychiatric comorbidity (as defined above).
Statistical analysis
We first visualised the time dependent associations of stress related disorders with the risk of cardiovascular disease by using flexible parametric survival models.27 Because of the greatly increased risk of cardiovascular disease during the time period immediately after the diagnosis of stress related disorders, compared with thereafter, we assessed the associations separately during the first year after a diagnosis of stress related disorder and beyond this one year period (<1 or ≥1 year of follow-up), using hazard ratios with 95% confidence intervals derived from conditional Cox regression models. We used time since the index date as the underlying time scale.
In the sibling cohort, we stratified all analyses by family identifiers and partially (in simply adjusted models) or fully (in fully adjusted models) adjusted for multiple potential confounders, including age at index date, sex, educational level (<9 years, 9-12 years, >12 years, or unknown), family income (top 20%, middle, lowest 20%, or unknown), marital status (single, married/cohabiting, or divorced/widowed), history of severe somatic diseases (yes or no), and history of psychiatric disorders (yes or no). We considered all stress related disorders as one group and also did separate analyses for PTSD, acute stress reaction, and adjustment disorder and other stress reactions. In subgroup analyses, we calculated the hazard ratios by sex (male or female), age at index date (by thirds: ≤28, 29-42, or ≥43 years), attained age (age during follow-up: <50 or ≥50 years), calendar year at index date (1987-96, 1997-2006, or 2007-13), follow-up period (<1 year, 1-4 years, 5-9 years, or ≥10 years), family history of cardiovascular disease (yes or no), history of severe somatic diseases (yes or no), and history of other psychiatric disorders (yes or no).
In addition to any cardiovascular disease, we examined the hazard ratios for seven major categories (including fatal cardiovascular diseases) and 16 individual diagnoses of cardiovascular disease. We further analysed certain acute cardiovascular events (cardiac arrest, acute myocardial infarction, and acute cerebrovascular disease) as a hypothesised group of immediate cardiac consequences triggered by a stress related disorder, and therefore with more specific time intervals during the first year of follow-up (<1 month, 1-5 months, 6-11 months, 1-4 years, 5-9 years, and ≥10 years).
To study the potential role of psychiatric comorbidity in the studied associations, we did further subgroup analyses by the presence of psychiatric comorbidity. Within one year after the diagnosis of a stress related disorder, we considered psychiatric comorbidity as a time varying variable (that is, the status of psychiatric comorbidity changed from “no” to “yes” at the date of diagnosis of the psychiatric comorbidity).
We did similar analyses in the population matched cohort, in which we used Cox regression models stratified by matching identifiers (birth year and sex) and adjusted for all above mentioned covariates and family history of cardiovascular disease (yes/no). Additionally, to examine the robustness of the observed estimates to the definition of history of psychiatric disorders, we re-ran the analyses by using a six month, instead of three month, threshold before the diagnosis of a stress related disorder, to distinguish “history of psychiatric disorders” from “psychiatric comorbidity.” We used SAS statistical software, version 9.4 and Stata 15 for all analyses.
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. A patient was invited to contribute to the review process of the study, and we are grateful for his input on the readability and accuracy of this document. There are no plans to directly disseminate the results of the research to study participants or the relevant patient community. The dissemination to the Swedish population (which constitutes the study population) will be achieved through media outreach (for example, press release and communication) on publication of this study.
Results
The median follow-up time was 6.2, 6.9, and 6.5 years for exposed patients, unaffected full siblings, and matched unexposed people, respectively, accumulating 2 268 901 person years at risk in the sibling cohort and 12 001 887 person years in the population matched cohort (table 1). Median age at index date was 36 years. Most (63%) people exposed to stress related disorders were women, whereas the unaffected siblings had an equal sex distribution. Having a history of other psychiatric disorders was more common among exposed patients in both cohorts (34-35%) than among the unaffected siblings (12%), as well as among the matched unexposed individuals (8%). In addition, patients with stress related disorders tended to have a higher burden of somatic diseases at the index date and a lower family income level, and to be more likely to be divorced or widowed, compared with their unaffected siblings or matched unexposed people.
Table 1.
Characteristics of study cohorts. Values are numbers (percentages) unless stated otherwise
| Characteristics | Sibling cohort | Population matched cohort | |||
|---|---|---|---|---|---|
| Exposed patients (n=106 180) | Unaffected full siblings (n=171 314) | Exposed patients (n=136 637) | Matched unexposed individuals (n=1 366 370) | ||
| Median (IQR) age at index date, years | 36 (25-46) | 36 (25-47) | 35 (24-46) | 35 (24-46) | |
| Median (IQR) follow-up time, years | 6.2 (2.8-10.3) | 6.9 (3.3-11.6) | 6.2 (2.8-10.4) | 6.5 (3.0-10.8) | |
| Male sex | 39 821 (37.50) | 86 751 (50.64) | 51 251 (37.51) | 512 510 (37.51) | |
| Educational level: | |||||
| <9 years | 3780 (3.56) | 9270 (5.41) | 5207 (3.81) | 45 425 (3.32) | |
| 9-12 years | 75 863 (71.45) | 118 617 (69.24) | 98 295 (71.94) | 891 626 (65.26) | |
| >12 years | 24 771 (23.33) | 38 467 (22.45) | 30 570 (22.37) | 402 935 (29.49) | |
| Unknown | 1766 (1.66) | 4960 (2.90) | 2565 (1.88) | 26 384 (1.93) | |
| Yearly family income level: | |||||
| Lowest 20% | 24 351 (22.93) | 32 905 (19.21) | 31 919 (23.36) | 239 434 (17.52) | |
| Middle | 58 081 (54.70) | 87 383 (51.01) | 73 752 (53.98) | 751 115 (54.97) | |
| Top 20% | 13 014 (12.26) | 25 854 (15.09) | 16 422 (12.02) | 226 400 (16.57) | |
| Unknown | 10 734 (10.11) | 25 172 (14.69) | 14 544 (10.64) | 149 421 (10.94) | |
| Marital status,: | |||||
| Single | 62 369 (58.74) | 98 676 (57.60) | 80 714 (59.07) | 809 763 (59.26) | |
| Married or cohabiting | 30 435 (28.66) | 58 005 (33.86) | 38 545 (28.21) | 461 819 (33.80) | |
| Divorced or widowed | 13 376 (12.60) | 14 633 (8.54) | 17 378 (12.72) | 94 788 (6.94) | |
| History of severe somatic diseases* | 18 929 (17.83) | 24 180 (14.11) | 25 133 (18.39) | 168 825 (12.36) | |
| History of other psychiatric disorder† | 36 559 (34.43) | 21 117 (12.33) | 47 962 (35.10) | 106 160 (7.77) | |
| Family history of cardiovascular disease | 51 969 (48.94)‡ | 84 257 (49.18)‡ | 64 448 (47.17) | 604 782 (44.26) | |
| Type of stress related disorder: | |||||
| Post-traumatic stress disorder | 8660 (8.16) | - | 11 162 (8.17) | - | |
| Acute stress reaction | 48 804 (45.96) | - | 63 058 (46.15) | - | |
| Adjustment disorder and other stress reactions | 48 716 (45.88) | - | 62 417 (45.68) | - | |
| Psychiatric comorbidity§ | 18 893 (17.79) | 2811 (1.64)¶ | 24 169 (17.69) | 12 963 (0.95)¶ | |
IQR=interquartile range.
Includes chronic pulmonary disease, connective tissue disease, diabetes, renal diseases, liver diseases, ulcer diseases, and HIV infection/AIDS.
First diagnosis of a psychiatric disorder, other than stress related disorders, occurred >3 months before index date.
Marginal difference between exposed and unexposed sibling group is due to different number of siblings for exposed patients. Within each family, family history of cardiovascular disease is always the same.
New onset psychiatric disorder, other than stress related disorders, that was diagnosed between 3 months before and 1 year after diagnosis of studied stress related disorder.
For unaffected full siblings and matched unexposed individuals, number and percentage of individuals who had diagnosis of other psychiatric disorder between 3 months and 1 one year after index date.
Using flexible parametric models, we observed a peak of cardiovascular disease risk immediately after diagnosis of a stress related disorder, followed by a rapid decline within the first six months (supplementary figure A). After one year, the magnitude of the hazard ratios tended to be constant (around 1.3 for both sibling based and population based comparisons). During up to 27 years of follow-up, the crude incidence rate of any cardiovascular disease was 10.5, 8.4, and 6.9 per 1000 person years
Within the first year of follow-up, 1617 people in the sibling cohort had a cardiovascular event (table 2, left side). The incidence rate among the exposed patients was almost twice that of their full siblings (crude: 8.1 v 4.9/1000 person years; age standardised: 8.7 v 4.5/1000 person years). With a total number of 18 522 cardiovascular events identified beyond one year of follow-up, the corresponding incidence rates were 10.3 v 8.9/1000 person years (age standardised: 6.0 v 4.5/1000 person years) for exposed patients and their full siblings. When we added history of other psychiatric disorders and history of severe somatic diseases to the Cox models, the obtained hazard ratios decreased from 1.77 (95% confidence interval 1.58 to 1.98) to 1.64 (1.45 to 1.84) for a less than one year period and from 1.39 (1.34 to 1.44) to 1.29 (1.24 to 1.34) for one year or longer. The main attenuation of hazard ratios occurred after additional adjustment for history of other psychiatric disorders. We obtained similar findings when comparing exposed patients with matched unexposed people (table 2, right side), with seemingly larger attenuation of hazard ratios after full adjustment for multiple risk factors, compared with the sibling analysis. Furthermore, although the largest point estimates were observed for PTSD, the subgroup analyses showed comparable hazard ratios for other types of stress related disorders (supplementary tables C-E).
Table 2.
Crude incidence rates and hazard ratios with 95% confidence intervals for cardiovascular diseases among patients with any stress related disorder, compared with their full siblings or matched unexposed individuals, by time of follow-up (<1 or ≥1 year)
| Model information | Sibling cohort | Population matched cohort | |||
|---|---|---|---|---|---|
| No of cases (incidence*) in patients/siblings | Hazard ratio (95% CI)† | No of cases (incidence*) in patients/unexposed individuals | Hazard ratio (95% CI)† | ||
| <1 year of follow-up | |||||
| Controlled for sex, birth year, educational level, family income, and marital status | 811 (8.06)/806 (4.92) | 1.77 (1.58 to 1.98) | 1094 (8.45)/5624 (4.32) | 1.92 (1.80 to 2.05) | |
| As above + history of other psychiatric disorder | 1.65 (1.47 to 1.86) | 1.74 (1.62 to 1.86) | |||
| As above + history of severe somatic diseases | 1.64 (1.45 to 1.84) | 1.72 (1.60 to 1.84) | |||
| As above + family history of cardiovascular disease | - | 1.71 (1.59 to 1.83) | |||
| ≥1 year of follow-up | |||||
| Controlled for sex, birth year, educational level, family income, and marital status | 7246 (10.30)/11 276 (8.87) | 1.39 (1.34 to 1.44) | 9827 (10.81)/69 483 (7.26) | 1.52 (1.49 to 1.56) | |
| As above + history of other psychiatric disorder | 1.30 (1.25 to 1.34) | 1.39 (1.36 to 1.42) | |||
| As above + history of severe somatic diseases | 1.29 (1.24 to 1.34) | 1.37 (1.33 to 1.40) | |||
| As above + family history of cardiovascular disease | - | 1.36 (1.33 to 1.39) | |||
Per 1000 person years.
Derived from Cox regression models, stratified by family identifier (for sibling based comparison) or matching identifier (birth year and sex, for population based comparison) and adjusted for covariates listed in model information column. Time since index date was used as underlying time scale.
We observed similar associations across sex, calendar period, history of severe somatic diseases, history of psychiatric disorders, and family history of cardiovascular disease (table 3 and supplementary table F) but stronger associations among people with younger age at index date (sibling analysis: hazard ratio 1.52 (1.35 to 1.71), 1.26 (1.17 to 1.36), and 1.30 (1.24 to 1.37) for age ≤28, 29-41, and ≥42 years, respectively; P for interaction=0.010). Additionally, we observed a stronger association between stress related disorders and early onset cardiovascular diseases (sibling analysis: hazard ratio 1.40 (1.32 to 1.49) for attained age <50 years) than later onset ones (1.24 (1.18 to 1.30) for attained age ≥50 years) (P for difference=0.002).
Table 3.
Hazard ratios with 95% confidence intervals for cardiovascular diseases among patients with stress related disorders, compared with their full siblings or matched unexposed individuals, by different characteristics
| Characteristics | Sibling cohort* | Population matched cohort† | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All stress related disorders | PTSD | Acute stress reaction | Adjustment disorder and other stress reactions | All stress related disorders | PTSD | Acute stress reaction | Adjustment disorder and other stress reactions | ||
| Overall | 1.32 (1.27 to 1.36) | 1.48 (1.28 to 1.72) | 1.33 (1.26 to 1.40) | 1.27 (1.20 to 1.33) | 1.39 (1.36 to 1.42) | 1.38 (1.27 to 1.50) | 1.41 (1.37 to 1.46) | 1.37 (1.32 to 1.41) | |
| By sex: | |||||||||
| Male | 1.37 (1.28 to 1.46) | 1.83 (1.36 to 2.48) | 1.33 (1.21 to 1.46) | 1.33 (1.20 to 1.48) | 1.38 (1.34 to 1.42) | 1.38 (1.21 to 1.58) | 1.41 (1.35 to 1.48) | 1.34 (1.28 to 1.41) | |
| Female | 1.24 (1.16 to 1.32) | 1.40 (1.09 to 1.80) | 1.26 (1.14 to 1.38) | 1.19 (1.09 to 1.31) | 1.40 (1.36 to 1.44) | 1.38 (1.23 to 1.55) | 1.40 (1.35 to 1.47) | 1.39 (1.33 to 1.45) | |
| By age at index date (thirds), years: | |||||||||
| ≤28 | 1.52 (1.35 to 1.71) | 1.33 (0.88 to 2.02) | 1.53 (1.28 to 1.82) | 1.52 (1.26 to 1.83) | 1.70 (1.59 to 1.81) | 1.92 (1.53 to 2.41) | 1.69 (1.54 to 1.85) | 1.66 (1.51 to 1.84) | |
| 29-42 | 1.26 (1.17 to 1.36) | 1.49 (1.06 to 2.10) | 1.30 (1.16 to 1.45) | 1.17 (1.04 to 1.32) | 1.46 (1.40 to 1.52) | 1.58 (1.34 to 1.87) | 1.50 (1.41 to 1.60) | 1.43 (1.33 to 1.53) | |
| ≥43 | 1.30 (1.24 to 1.37) | 1.44 (1.16 to 1.79) | 1.31 (1.22 to 1.41) | 1.27 (1.18 to 1.36) | 1.31 (1.27 to 1.34) | 1.20 (1.07 to 1.34) | 1.33 (1.28 to 1.38) | 1.30 (1.25 to 1.35) | |
| By attained age (age during follow-up), years: | |||||||||
| <50 | 1.40 (1.32 to 1.49) | 1.72 (1.34 to 2.21) | 1.44 (1.32 to 1.58) | 1.31 (1.19 to 1.44) | 1.57 (1.52 to 1.63) | 1.95 (1.70 to 2.23) | 1.57 (1.49 to 1.66) | 1.53 (1.45 to 1.61) | |
| ≥50 | 1.24 (1.18 to 1.30) | 1.33 (1.08 to 1.64) | 1.24 (1.15 to 1.33) | 1.22 (1.13 to 1.31) | 1.30 (1.26 to 1.33) | 1.11 (0.99 to 1.24) | 1.33 (1.28 to 1.38) | 1.29 (1.24 to 1.34) | |
| By calendar year at index date: | |||||||||
| 1987-96 | 1.32 (1.25 to 1.40) | 1.35 (1.10 to 1.65) | 1.32 (1.22 to 1.43) | 1.32 (1.21 to 1.45) | 1.43 (1.38 to 1.48) | 1.34 (1.18 to 1.51) | 1.45 (1.38 to 1.52) | 1.42 (1.34 to 1.50) | |
| 1997-2006 | 1.30 (1.23 to 1.37) | 1.85 (1.39 to 2.46) | 1.34 (1.23 to 1.45) | 1.21 (1.12 to 1.31) | 1.35 (1.30 to 1.39) | 1.41 (1.21 to 1.65) | 1.37 (1.31 to 1.44) | 1.32 (1.26 to 1.38) | |
| 2007-13 | 1.34 (1.23 to 1.46) | 1.40 (0.98 to 2.00) | 1.33 (1.17 to 1.52) | 1.31 (1.15 to 1.48) | 1.35 (1.30 to 1.39) | 1.49 (1.22 to 1.80) | 1.39 (1.29 to 1.50) | 1.41 (1.31 to 1.52) | |
| By history of severe somatic diseases‡: | |||||||||
| Yes | 1.30 (1.15 to 1.50) | 1.29 (0.66 to 2.50) | 1.40 (1.12 to 1.75) | 1.28(1.02 to 1.61) | 1.30(1.21 to 1.40) | 1.35(1.03 to 1.77) | 1.27(1.15 to 1.41) | 1.32(1.19 to 1.46) | |
| No | 1.33 (1.28 to 1.39) | 1.52 (1.27 to 1.81) | 1.32 (1.27 to 1.41) | 1.26(1.20 to 1.37) | 1.42(1.39 to 1.45) | 1.48(1.34 to 1.63) | 1.45(1.40 to 1.50) | 1.37(1.32 to 1.42) | |
| By previous history of psychiatric disorders§: | |||||||||
| Yes | 1.23 (1.07 to 1.40) | 2.16 (1.23 to 4.55) | 1.36 (1.12 to 1.65) | 0.98 (0.80 to 1.20) | 1.23 (1.14 to 1.32) | 1.35 (1.10 to 1.70) | 1.19 (1.07 to 1.32) | 1.23 (1.10 to 1.36) | |
| No | 1.35 (1.30 to 1.41) | 1.42 (1.17 to 1.71) | 1.35 (1.27 to 1.44) | 1.33 (1.24 to 1.42) | 1.44 (1.41 to 1.48) | 1.52 (1.37 to 1.68) | 1.47 (1.41 to 1.52) | 1.41 (1.36 to 1.46) | |
| By family history of CVD among first to degree relatives: | |||||||||
| Yes | 1.32 (1.26 to 1.38) | 1.64 (1.35 to 1.99) | 1.33 (1.25 to 1.42) | 1.26 (1.18 to 1.35) | 1.37 (1.33 to 1.41) | 1.35 (1.19 to 1.52) | 1.37 (1.31 to 1.43) | 1.37 (1.31 to 1.43) | |
| No | 1.31 (1.24 to 1.39) | 1.28 (1.02 to 1.62) | 1.33 (1.22 to 1.44) | 1.18 (1.08 to 1.29) | 1.42 (1.37 to 1.47) | 1.50 (1.30 to 1.73) | 1.47 (1.39 to 1.55) | 1.35 (1.28 to 1.43) | |
CVD=cardiovascular disease; PTSD-post-traumatic stress disorder.
Cox regression models were stratified by family identifiers and adjusted for age at cohort entry, sex, educational level, family income, marital status, history of severe somatic diseases, and history of other psychiatric disorders. Time since index date was used as underlying time scale.
Cox regression models were stratified by matching identifiers (birth year and sex) and adjusted for educational level, family income, marital status, history of severe somatic diseases, family history of CVD, and history of other psychiatric disorders. Time since index date was used as underlying time scale.
Include chronic pulmonary disease, connective tissue disease, diabetes, renal diseases, liver diseases, ulcer diseases, and HIV infection/AIDS.
First diagnosis of psychiatric disorder, other than stress related disorders, occurred >3 months before index date.
Figure 2 shows increased hazard ratios for all studied categories of cardiovascular diseases (including fatal cardiovascular disease events) and for most individual diagnoses of cardiovascular diseases in patients with stress related disorders compared with their unaffected full siblings. The highest hazard ratios were for heart failure (6.95, 1.88 to 25.68), other cerebrovascular disease (5.64, 1.19 to 26.75), conduction disorder (5.00, 1.58 to 15.80), and cardiac arrest (3.37, 1.05 to 10.75) during the first year after the diagnosis of a stress related disorder. Beyond one year, the relative risk elevations were attenuated (hazard ratios ranged from 1.12 (1.04 to 1.21) for arrhythmia to 2.02 (1.45 to 2.82) for artery thrombosis/embolus). Focusing on acute cardiovascular events only, we found a clear time dependent risk pattern for cardiac arrest, indicating a more than fourfold relative risk within the first six months of diagnosis of a stress related disorder (supplementary table G). The temporal risk patterns for acute myocardial infarction and acute cerebrovascular disease were similar but less prominent.
Fig 2.
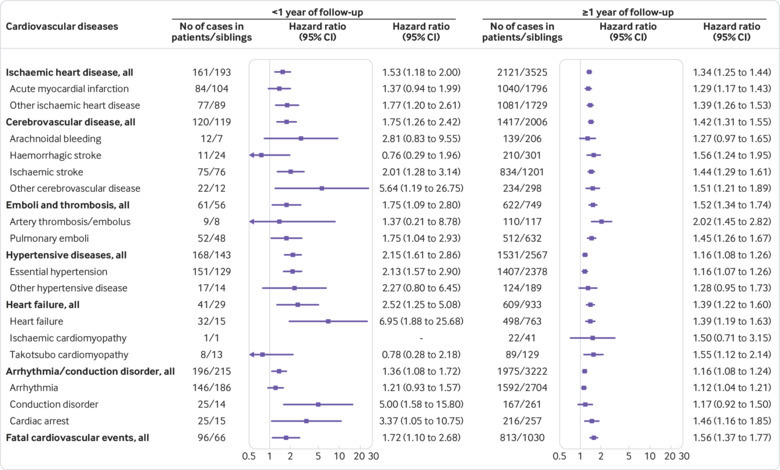
Relative risks of developing different types of cardiovascular disease among patients with any stress related disorder, compared with their full siblings, by time of follow-up (<1 or ≥1 year). All Cox models were stratified by family identifiers and adjusted for age at index date, sex, educational level, family income, marital status, history of severe somatic diseases, and history of other psychiatric disorders. Time since the index date was used as underlying time scale
The presence of psychiatric comorbidity did not substantially modify the risk elevations for cardiovascular disease after a diagnosis of a stress related disorder, except for fatal cardiovascular events, for which the association was distinctly amplified by the presence of psychiatric comorbidity (supplementary figure B). In addition, we obtained almost identical results in the sensitivity analysis using a more conservative definition of “history of other psychiatric disorders” (supplementary table H).
Discussion
In this nationwide population based and sibling controlled study, we found that people with stress related disorders were at elevated risk of multiple types of cardiovascular disease, especially early onset ones (incident age <50). The relative risk elevation was independent of sex, familial background (including family history of cardiovascular disease), history of psychiatric/somatic diseases, and psychiatric comorbidity. Furthermore, the relative risks of severe and acute cardiovascular events (for example, cardiac arrest) were highest during the period adjacent to the diagnosis of a stress related disorder, indicating the first six months after diagnosis as a high risk time window. Likewise, the excess relative risks of other studied cardiovascular diseases were more pronounced during the first year after diagnosis of a stress related disorder than thereafter. Notably, although the highest point estimates were consistently noted for PTSD, other stress related disorders also conferred a considerably increased risk of cardiovascular disease.
Strengths and weaknesses of study
The merits of our study include the population based, sibling controlled design, which provides optimal conditions for relieving important concerns regarding genetic and early life environmental confounders,22 as well as pre-existing or co-occurring psychiatric disorders. The diagnoses of stress related disorders and cardiovascular disease were obtained prospectively and independently, minimising the risk of information bias. The cross linkages to the Cause of Death and Emigration Registers reduced selection bias due to loss of follow-up. Importantly, by involving more than 100 000 patients with stress related disorders with up to 27 years of follow-up, the large sample size provided sufficient power to do most of the planned subgroup analyses. The availability of demographic, clinical, and family information enabled consideration of a wide range of health and disease related factors in the analysis.
Limitations include, firstly, the absence of information from primary care as well as late inclusion of outpatient specialist care records in the National Patient Register, which might have led to an underestimation of the number of patients with milder forms of stress related disorders or less severe cardiovascular diseases. Secondly, changes in the diagnostic criteria for stress related disorders over the 27 year study period may have influenced the observed associations, although our stratified analyses across different calendar periods suggest a minor effect of such diagnostic instability on the reported associations. Thirdly, as traumatic life experiences may be shared within families, a proportion of the reference (sibling) population may also have had milder or undiagnosed stress related disorders, yielding conservative estimates in the sibling analysis. Fourthly, as other psychiatric disorders both are risk factors for and frequently appear together with stress related disorders, distinguishing co-occurring from pre-existing psychiatric disorders in register based studies is challenging. However, such concern was partly alleviated by our sensitivity analyses in which introduction of an alternative definition for “history of other psychiatric disorders” yielded similar results. Fifthly, we had no data on behaviour related factors (such as smoking and alcohol consumption) that may contribute to the observed association as confounders or mediators. As these behavioural factors tend to cluster within families, our sibling analysis should have relieved the concern of residual confounding to some extent. However, further studies with detailed information on lifestyle, especially potential changes in lifestyle after diagnosis of stress related disorders, are warranted to clarify the impact of these factors on the association of interest. Finally, as this study focuses on patients who received a clinical diagnosis of stress related disorders through a hospital visit, its findings might not be directly applicable to people with less severe stress reactions or daily stress.
Comparison with other studies
Our findings corroborate the results from previous prospective studies suggesting a possible role of stress related disorders in the pathogenesis of cardiovascular disease.11 12 28 29 30 31 32 33 34 35 However, the main body of the preceding evidence was primarily derived from studies of male samples (veterans or active duty military personnel),12 29 30 35 focusing almost exclusively on PTSD or self reported symptoms of PTSD.11 30 Data on the role of stress related disorders in cardiovascular disease in women were, until now, limited.31 32 33 34 Although some attempts have been made to control for familial factors and co-occurring psychiatric disorders,12 33 or to study other stress related disorders (for example, adjustment disorder),34 no previous initiative has considered all these concerns in the same study. Also, the modest sample sizes of many previous studies often precluded analyses of different subtypes of cardiovascular disease. As a result, our study is the first to show a robust association between stress related disorders, including but not limited to PTSD, and multiple types of cardiovascular disease among both men and women, independent of familial factors and psychiatric comorbidities. Our findings indicate that the risk elevation generally exists for all studied cardiovascular diseases, with the strongest associations observed for the major categories of heart failure (within one year after the diagnosis of any stress related disorder) and emboli/thrombosis (beyond one year). These findings gain support from previous studies on 49 000 US female nurses, showing a higher hazard ratio for venous thromboembolism by burden of PTSD symptoms compared with other cardiovascular disease outcomes, including myocardial infarction or stroke.32 33 Similarly, one longitudinal study indicated a positive association between PTSD and incident heart failure among veterans, although no risk estimate was provided for the first year after PTSD specifically.36
Clinical observations suggest that experiencing severe emotional or physical stress may trigger immediate cardiovascular consequences, such as heart attack and sudden cardiac arrest, even in apparently healthy people.37 38 Our results consolidate these reported associations by showing that a clinically confirmed stress related disorder (requiring a preceding occurrence of a trauma or significant life stressor) is also associated with these acute cardiovascular events.
Meaning of study
Although the crucial underlying mechanisms remain unclear, many potential mechanisms have been proposed to explain the association between stress related disorders, particularly PTSD, and cardiovascular disease. The physiological effects of an acute stressor can directly affect the cardiovascular system (for example, increased arterial blood pressure), which consequently forms favourable conditions for the onset of acute cardiovascular events,39 40 as well as the further development of hypertension, endothelial dysfunction, and arteriosclerosis.41 In addition, the long lasting effect of severe stress reactions on cardiovascular risk is also plausible through prolonged biological disturbances (for example, inflammation, autonomic dysfunction, dysregulation of hypothalamic-pituitary-adrenal axis, and abnormal neurochemistry)42 43 44 and behaviour related changes (for example, smoking and sleep disturbance).33 A recent study in 4178 US veterans (aged 30-70 years) indicates that the association between PTSD and incident cardiovascular disease may be mediated by behavioural factors, metabolic conditions, and mental disorders.45 As our analyses showed that patients with stress related disorders other than PTSD were also at a considerably excess risk of adverse cardiovascular outcomes, further studies with a broader research scope are warranted to explore the underlying mechanisms between the various subtypes of stress related disorders and the development of cardiovascular disease.
One challenge related to this topic of study is how to assess the immediate effect of stress related disorders on cardiovascular disease. The main concerns include the risk of reverse causality (that is, cardiac symptoms emerge first and contribute to the diagnosis of stress related disorders) and surveillance bias (that is, patients with stress related disorders have more healthcare visits than others, leading to a higher likelihood of receiving a diagnosis of cardiovascular disease). In this study, despite the possibility that we might have missed the greatest risk increase (and some acute fatal outcomes) by following patients from their date of diagnosis of stress related disorders, instead of the date when they were exposed to the actual stressor or trauma, the time dependent hazard ratio for cardiovascular disease indicates that the first year, especially the first six months, after clinical diagnosis of stress related disorders entails the highest excess cardiovascular risk among the affected patients. This may be interpreted as a mixed consequence of the abovementioned factors and a real immediate effect of the stress reactions to trauma on cardiovascular disease. However, the additional analyses on acute and severe cardiovascular events (that is, cardiac arrest, acute myocardial infarction, and acute cerebrovascular disease) that typically result in prompt hospital visit and medical care provide further evidence supporting an immediate effect of stress related disorders on cardiovascular disease, as such analyses are less likely to be affected by surveillance bias or reverse causality. These sudden cardiovascular events carry a high risk of a fatal outcome,46 so increased clinical awareness of these risks among patients with recently diagnosed stress related disorders deserves further attention.
Conclusions
This population based, sibling controlled analysis showed a clear association between clinically confirmed stress related disorders and a higher subsequent risk of cardiovascular disease, particularly during the months after diagnosis of a stress related disorder, in the Swedish population. This association applies equally to men and women and is independent of familial factors, history of somatic/psychiatric diseases, and psychiatric comorbidities. These findings call for enhanced clinical awareness and, if verified, monitoring or early intervention among patients with recently diagnosed stress related disorders.
What is already known on this topic
Accumulating evidence suggests a role of severe stress reactions to significant life events or trauma in cardiovascular disease
Most evidence comes from studies of male samples (veterans or active duty military personnel) focusing on post-traumatic stress disorder (PTSD) or self reported PTSD symptoms
The modest sample sizes of previous studies mean that limited data exist on potential differences in immediate and long term effects of stress reactions on multiple types of cardiovascular disease
What this study adds
Severe stress reactions to significant life events or trauma are associated with considerably elevated risk of multiple types of cardiovascular disease
This is especially the case during the first year after the diagnosis of a stress related disorder
The association between stress related disorders and cardiovascular disease seems particularly strong in cases of early onset diseases (occurring before the age of 50)
Acknowledgments
We thank Peter Green for his input on the readability and accuracy of this document during the review process of the study.
Web extra.
Extra material supplied by authors
Supplementary materials
Contributors: UAV, FF, and HS were responsible for the study concept and design. HS, UV, and FF did the data analysis. UAV, HS, FF, GT, FKA, PL, CA, DMC, LFC, and KF interpreted the data. HS, UAV, FF, FKA, PL, CA, DMC, LFC, KF, and GT drafted the manuscript. HS and UAV had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. HS and UAV are the guarantors.
Funding: The study was supported by Grant of Excellence, Icelandic Research Fund (grant No 163362-051 to UAV), and ERC Consolidator Grant (StressGene, grant No 726413 to UAV); by the Karolinska Institutet (Senior Researcher Award and Strategic Research Area in Epidemiology to FF); and by the Swedish Research Council through the Swedish Initiative for Research on Microdata in the Social And Medical Sciences (SIMSAM) framework (grant No 340-2013-5867 to CA).
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work other than that detailed above; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study was approved by the Regional Ethics Review Board in Stockholm, Sweden (Dnr 2013/862-31/5).
Data sharing: No additional data available.
Transparency: The study guarantors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1. Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. Trauma and PTSD in the WHO World Mental Health Surveys. Eur J Psychotraumatol 2017;8(Suppl 5):1353383. 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. de Vries GJ, Olff M. The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. J Trauma Stress 2009;22:259-67. 10.1002/jts.20429 [DOI] [PubMed] [Google Scholar]
- 3. Fall K, Fang F, Mucci LA, et al. Immediate risk for cardiovascular events and suicide following a prostate cancer diagnosis: prospective cohort study. PLoS Med 2009;6:e1000197. 10.1371/journal.pmed.1000197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shen Q, Lu D, Schelin ME, et al. Injuries before and after diagnosis of cancer: nationwide register based study. BMJ 2016;354:i4218. 10.1136/bmj.i4218 [DOI] [PubMed] [Google Scholar]
- 5. Cohen S, Tyrrell DA, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med 1991;325:606-12. 10.1056/NEJM199108293250903 [DOI] [PubMed] [Google Scholar]
- 6. Song H, Fang F, Tomasson G, et al. Association of Stress-Related Disorders With Subsequent Autoimmune Disease. JAMA 2018;319:2388-400. 10.1001/jama.2018.7028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bergelt C, Prescott E, Grønbaek M, Koch U, Johansen C. Stressful life events and cancer risk. Br J Cancer 2006;95:1579-81. 10.1038/sj.bjc.6603471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gradus JL, Farkas DK, Svensson E, et al. Posttraumatic stress disorder and cancer risk: a nationwide cohort study. Eur J Epidemiol 2015;30:563-8. 10.1007/s10654-015-0032-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gradus JL, Antonsen S, Svensson E, Lash TL, Resick PA, Hansen JG. Trauma, comorbidity, and mortality following diagnoses of severe stress and adjustment disorders: a nationwide cohort study. Am J Epidemiol 2015;182:451-8. 10.1093/aje/kwv066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li J, Precht DH, Mortensen PB, Olsen J. Mortality in parents after death of a child in Denmark: a nationwide follow-up study. Lancet 2003;361:363-7. 10.1016/S0140-6736(03)12387-2 [DOI] [PubMed] [Google Scholar]
- 11. Jordan HT, Stellman SD, Morabia A, et al. Cardiovascular disease hospitalizations in relation to exposure to the September 11, 2001 World Trade Center disaster and posttraumatic stress disorder. J Am Heart Assoc 2013;2:e000431. 10.1161/JAHA.113.000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vaccarino V, Goldberg J, Rooks C, et al. Post-traumatic stress disorder and incidence of coronary heart disease: a twin study. J Am Coll Cardiol 2013;62:970-8. 10.1016/j.jacc.2013.04.085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O’Donovan A, Cohen BE, Seal KH, et al. Elevated risk for autoimmune disorders in iraq and afghanistan veterans with posttraumatic stress disorder. Biol Psychiatry 2015;77:365-74. 10.1016/j.biopsych.2014.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. American Psychiatric Association Diagnosis and startistical manual of medical disorders. 4th ed APA, 1994. [Google Scholar]
- 15. World Health Organization The ICD-10 classification of mental and behavioral disorders: Clinical description and diagnostic guidelines. WHO, 1992. [Google Scholar]
- 16. Ursano RJ, Bell C, Eth S, et al. Work Group on ASD and PTSD. Steering Committee on Practice Guidelines Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry 2004;161(Suppl):3-31. [PubMed] [Google Scholar]
- 17. Auer PL, Stitziel NO. Genetic association studies in cardiovascular diseases: Do we have enough power? Trends Cardiovasc Med 2017;27:397-404. 10.1016/j.tcm.2017.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khera AV, Emdin CA, Drake I, et al. Genetic Risk, Adherence to a Healthy Lifestyle, and Coronary Disease. N Engl J Med 2016;375:2349-58. 10.1056/NEJMoa1605086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Norhammar A, Mellbin L, Cosentino F. Diabetes: Prevalence, prognosis and management of a potent cardiovascular risk factor. Eur J Prev Cardiol 2017;24(Suppl):52-60. 10.1177/2047487317709554 [DOI] [PubMed] [Google Scholar]
- 20. Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 2009;24:659-67. 10.1007/s10654-009-9350-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. National Collaborating Centre for Mental Health (UK) Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. Gaskell, 2005. [PubMed] [Google Scholar]
- 22. D’Onofrio BM, Lahey BB, Turkheimer E, Lichtenstein P. Critical need for family-based, quasi-experimental designs in integrating genetic and social science research. Am J Public Health 2013;103(Suppl 1):S46-55. 10.2105/AJPH.2013.301252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Harvey AG, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder: a 2-year prospective evaluation. J Consult Clin Psychol 1999;67:985-8. 10.1037/0022-006X.67.6.985 [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. Cardiovascular diseases (CVDs). 2017. http://www.who.int/mediacentre/factsheets/fs317/en/.
- 25. Gros DF, Price M, Magruder KM, Frueh BC. Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Res 2012;196:267-70. 10.1016/j.psychres.2011.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 27. Lambert PC, Royston P. Further development of flexible parametric models for survival analysis. Stata J 2009;9:265-90 10.1177/1536867X0900900206 . [DOI] [Google Scholar]
- 28. Jordan HT, Miller-Archie SA, Cone JE, Morabia A, Stellman SD. Heart disease among adults exposed to the September 11, 2001 World Trade Center disaster: results from the World Trade Center Health Registry. Prev Med 2011;53:370-6. 10.1016/j.ypmed.2011.10.014 [DOI] [PubMed] [Google Scholar]
- 29. Boscarino JA. A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention. Psychosom Med 2008;70:668-76. 10.1097/PSY.0b013e31817bccaf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kubzansky LD, Koenen KC, Spiro A, 3rd, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry 2007;64:109-16. 10.1001/archpsyc.64.1.109 [DOI] [PubMed] [Google Scholar]
- 31. Kubzansky LD, Koenen KC, Jones C, Eaton WW. A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychol 2009;28:125-30. 10.1037/0278-6133.28.1.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sumner JA, Kubzansky LD, Elkind MSV, et al. Trauma Exposure and Posttraumatic Stress Disorder Symptoms Predict Onset of Cardiovascular Events in Women. Circulation 2015;132:251-9. 10.1161/CIRCULATIONAHA.114.014492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sumner JA, Kubzansky LD, Kabrhel C, et al. Associations of Trauma Exposure and Posttraumatic Stress Symptoms With Venous Thromboembolism Over 22 Years in Women. J Am Heart Assoc 2016;5:e003197. 10.1161/JAHA.116.003197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gradus JL, Farkas DK, Svensson E, et al. Associations between stress disorders and cardiovascular disease events in the Danish population. BMJ Open 2015;5:e009334. 10.1136/bmjopen-2015-009334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Burg MM, Brandt C, Buta E, et al. Risk for Incident Hypertension Associated With Posttraumatic Stress Disorder in Military Veterans and the Effect of Posttraumatic Stress Disorder Treatment. Psychosom Med 2017;79:181-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Roy SS, Foraker RE, Girton RA, Mansfield AJ. Posttraumatic stress disorder and incident heart failure among a community-based sample of US veterans. Am J Public Health 2015;105:757-63. 10.2105/AJPH.2014.302342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ziegelstein RC. Acute emotional stress and cardiac arrhythmias. JAMA 2007;298:324-9. 10.1001/jama.298.3.324 [DOI] [PubMed] [Google Scholar]
- 38. Connelly KA, MacIsaac AI, Jelinek VM. Stress, myocardial infarction, and the “tako-tsubo” phenomenon. Heart 2004;90:e52. 10.1136/hrt.2004.038851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rosengren A, Hawken S, Ounpuu S, et al. INTERHEART investigators Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:953-62. 10.1016/S0140-6736(04)17019-0 [DOI] [PubMed] [Google Scholar]
- 40. Sharkey SW, Lesser JR, Zenovich AG, et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation 2005;111:472-9. 10.1161/01.CIR.0000153801.51470.EB [DOI] [PubMed] [Google Scholar]
- 41. Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol 2012;9:360-70. 10.1038/nrcardio.2012.45 [DOI] [PubMed] [Google Scholar]
- 42. Koenen KC, Sumner JA, Gilsanz P, et al. Post-traumatic stress disorder and cardiometabolic disease: improving causal inference to inform practice. Psychol Med 2017;47:209-25. 10.1017/S0033291716002294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wentworth BA, Stein MB, Redwine LS, et al. Post-traumatic stress disorder: a fast track to premature cardiovascular disease? Cardiol Rev 2013;21:16-22. 10.1097/CRD.0b013e318265343b [DOI] [PubMed] [Google Scholar]
- 44. Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A 2012;109:5995-9. 10.1073/pnas.1118355109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Scherrer JF, Salas J, Cohen BE, et al. Comorbid Conditions Explain the Association Between Posttraumatic Stress Disorder and Incident Cardiovascular Disease. J Am Heart Assoc 2019;8:e011133. 10.1161/JAHA.118.011133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Engdahl J, Holmberg M, Karlson BW, Luepker R, Herlitz J. The epidemiology of out-of-hospital ‘sudden’ cardiac arrest. Resuscitation 2002;52:235-45. 10.1016/S0300-9572(01)00464-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary materials


