Abstract
Hepatitis B virus (HBV) infection remains a public health problem worldwide. In this review, we aim to assess the current situation of the HBV care pathway in the Kingdom of Saudi Arabia (KSA), identify gaps/barriers therein, and recommend initiatives to be taken to improve the management of such patients. Towards this end, a literature search was conducted in PubMed and free Internet searches. Interviews with individuals and focus group discussions were held with HBV experts in KSA. Although significant improvements have been made in the past 30 years in KSA in terms of the decline in prevalence (currently estimated to be around 1.3%), the morbidity and mortality related to the disease have not shown a parallel decline. This makes HBV an important public health concern. Furthermore, poor disease awareness, low diagnosis rates, and nonadherence to therapy amplify the disease burden. There are several mandated national screening structures present; however, established protocols for those who test positive and subsequent linkage-to-care are inadequate. In the absence of a virologic cure, a concerted effort should be made to provide safe and effective lifelong treatment. This review provides recommendations to reduce the HBV disease burden in the Saudi population.
Keywords: Awareness, diagnosis, epidemiology, hepatitis B, Saudi Arabia, treatment
INTRODUCTION
Hepatitis B virus (HBV) infection remains a public health problem worldwide with an estimated prevalence of 248 million cases in 2010 according to a systematic review.[1] In the World Health Organization (WHO) Eastern Mediterranean Region, an estimated 21 million people (3.3%) of the general population are infected.[2]
The last major review of the epidemiology and management of HBV in the Middle East was published in 2011.[3] The authors observed that the Middle East was in the past regarded as a region of high-to-intermediate epidemicity; however, infant vaccination programs have successfully lowered the prevalence of hepatitis B infection in most countries to that of low-to-intermediate endemicity. Leading hepatologists and gastroenterologists from the Kingdom of Saudi Arabia (KSA) considered it important to assess whether this trend continued, and therefore, the aim of this study was to assess the current situation of the HBV care pathway in KSA, identify gaps therein, and recommend comprehensive initiatives to improve the overall situation.
METHODS
To describe the current situation of the HBV care pathway (epidemiology and awareness; screening, diagnosis, linkage to care; treatment initiation; compliance/adherence) in KSA, a pragmatic literature search was conducted in PubMed, Web of Science, and Cochrane Reviews, using the keywords “Saudi Arabia or KSA,” “hepatitis B or HBV or CHB,” “hepatocellular carcinoma or HCC,” “cirrhosis,” “prevalence,” “awareness,” “epidemiology,” “vaccination,” “diagnosis,” “screening,” “treatment,” “care pathway,” “adherence,” and so on. In addition, the reference lists of the articles found were scanned for any additional publications. Also, free Internet searches were conducted (Google Scholar) using similar keywords to identify relevant reports, guidelines, conference abstracts, posters, presentations, and so on.
To provide context to the results from the literature review and to collect diverse stakeholder perspectives on those areas for which no or limited evidence was found in the literature, discussions were held with various professionals: physicians (general and specialist), regulators, payers (funding and procurement), and staff at nongovernmental organizations. Finally, inputs were taken from a meeting with experts and key opinion leaders (KOLs) in the field of hepatology representing most public sectors and regions in Saudi Arabia.[4] There was one advisory group meeting to align on the first draft of the manuscript followed by individual consultations with these experts to finalize the content of the paper and to review specific points of data.
EPIDEMIOLOGY
A large number of studies have been conducted in KSA,[1,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19] and a systematic review pooling data of 312,787 people from 36 studies published between 1965 and 2013 found a prevalence of 3.2% for the country which is slightly lower than the worldwide prevalence of 3.6%.[1] In this systematic review, a decrease in prevalence has been observed over time, and hence it is expected that the current prevalence rate in KSA would be lower than the average found.[1] The estimate of 3.2% is also based on studies including various populations, primarily conducted in HBV screening settings. The results from those studies including data from population surveys, hemodialysis patients, antenatal care attendees, blood donors, military personnel, premarital screening, and students are probably reasonably representative of the overall prevalence in the country. However, some surveys concentrated more on at-risk populations, such as heroin addicts and HIV-positive patients, where the prevalence of HBV infection is expected to be higher.
Among the more recent studies, a cross-sectional study including a large sample (n = 74,662) of premarital couples recruited from the general population in KSA found a prevalence rate of HBV of 1.3%,[20] which is considerably lower than the average found in the studies conducted from 1964 to 2013. Hepatology experts and KOLs agreed that this is the most reliable estimate currently available, clearly in accordance with the declining prevalence rate in the country.[4] With a Saudi population estimate of about 20 million in 2016, this proportion would give an estimated 260,000 HBV cases in the country.
Prevalence of chronic HBV (CHB) will be lower in the younger population (<30 years), compared with the older population, due to the impact of the vaccination program:
The first large-scale community-based epidemiological study among Saudi children aged 1–12 years was published in 1988 and showed an HBV surface antigen (HBsAg) seroprevalence of approximately 7%.[21] The introduction of the HBV vaccine program in 1989 successfully reduced HBV endemicity in the country as reported in 2008, with a prevalence of 0% among 1,355 vaccinated school students age 16–18 years, from different endemic areas across the country.[10] A review article published in 2003 confirmed that the addition of the HBV vaccine, as well as the Ministry of Health (MoH) strategy for prevention of viral hepatitis infection, led to a decline in the prevalence among children.[11] The same article reported that the prevalence decreased from 4.7% in 1987 to 1.7% in 2000 among blood donors at a large center in Riyadh[11]
For those born in the prevaccination era, the prevalence will be higher. This was seen in a cross-sectional study conducted among 10,234 persons in the Aseer Region, a southern province of KSA.[5] A seroprevalence of 0.8% was found among persons less than 15 years of age, 1.3% among persons 15–24 years of age, and 6.3% among those 25 years of age and older. MoH blood donor results for HBV infection in the year 2000 showed a prevalence rate of 3.2% among persons between 18 and 44 years of age and 5.9% for persons more than 50 years of age (personal communication).[11] Another study rightfully points out that despite the optimism surrounding the low HBV infection rates in the younger Saudi populations, the prevalence in older generations has not been well-characterized and remains a source of concern[22]
The vaccination program for newborns (and the catch-up program for children entering school between 1990 and 1996)[11] has reduced HBV prevalence in children due to effective implementation – 73% coverage of the third dose in the first year of implementation, 93% responders, and a protective efficacy of 99%,[23] with an 88% efficacy rate against HBsAg carriage 8 years after vaccination.[24] However, a catch-up vaccination program that supplemented the childhood program in 1990 to vaccinate healthcare workers (mandatory) and high-risk groups (voluntary)[11] might not have been optimally implemented. Two studies conducted among Saudi dental students and dentists found that 80%[25] and 80.5%[26] were vaccinated, respectively. Another study among medical students in a tertiary care academic hospital found that while 93.9% received the HBV vaccine upon entry to medical school, only 59.5% received all three doses.[27] Finally, a study among healthcare staff in a primary healthcare setting showed only 61% coverage of HBV vaccination (and of those, only 89% received the complete schedule).[28]
With respect to awareness about HBV in the community, in a cross-sectional study of 421 healthy individuals from Arar city, the majority (66.5%) had heard of HBV and were aware of the different modes of transmission (58.2%–78.9%), but only 27.6% knew the early symptoms.[29] Awareness regarding HBV and hepatitis C virus (HCV) was somewhat higher among first-year male and female students of medical sciences, at Jazan University (n = 824) in 2010.[30] The study showed that more than half of the students (64.4%) had basic awareness about HBV and HCV infection as well as about symptoms, and 57.1% had knowledge of the mode of transmission. In 2012, a cross-sectional survey of 180 primary care physicians revealed that the overall mean HBV knowledge level among the physicians was 62.9%.[31]
People with CHB have a lifetime risk of 15%–40% of developing end-stage liver disease including cirrhosis, liver failure, and hepatocellular carcinoma (HCC).[32] Limited data on end-stage liver disease and related deaths due to HBV are available through the Systematic Observatory Liver Disease registry (SOLID)[33] which collects data from several centers in the country. A review study[34] found that about 35% of Saudi HCC patients were HBV-related. In two studies, it was found that for 29%[35] and 24.2%,[36] respectively, HBV was the underlying cause for HCC. In Arab countries, HBV-associated HCC deaths increased at a much faster rate (137% increase) compared with the rest of the world (62% increase) between 1990 and 2010.[37] Another recent study from the SOLID registry that analysed HBV-infected cohorts from the years 2010 and 2015 concluded that compared to 2010, the cohort from 2015 had not only aged significantly but was more likely to have liver disease sequelae such as HCC (1% vs. 12%) and cirrhosis (5% vs. 23%), and other comorbidities such as prevalence of coronary artery disease (4% vs. 10%).[38] This suggests that although the overall prevalence of HBV has decreased dramatically, the associated burden of end-stage liver disease secondary to CHB is likely to increase drastically in KSA in the next 20 years due to aging of the previously infected children.[39]
SCREENING AND DIAGNOSIS
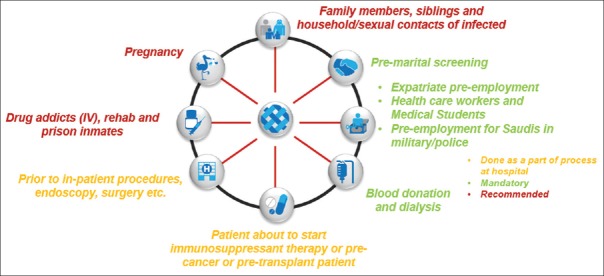
There are a number of mandated screening structures present in the country aimed toward identifying patients through blood tests (HBsAg test, antibodies for blood donors) [Figure 1].[20,40,41,42,43,44]
Figure 1.
Potential HBV screening points in KSA
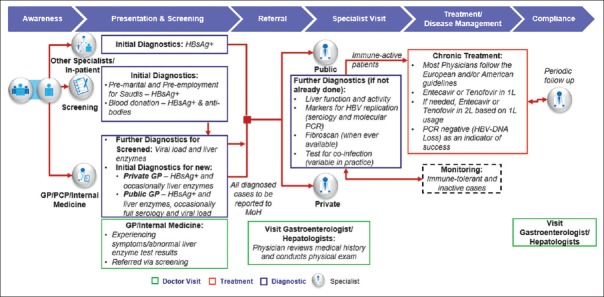
The typical HBV patient journey in KSA is illustrated in Figure 2.[4] It is not known what proportion of the patients who are referred to specialists for further diagnosis come from GPs/primary care facilities or are referred by other specialties such as obstetrics/gynecology, surgery, and endoscopy.[4] Patients are often referred without having received the correct initial diagnostic testing. Diagnostic testing such as serology, molecular testing, liver enzyme tests, and transient elastography is at the specialist's disposal and is routinely conducted in the public sector.[4] Transient elastography may not always be available in all private or public facilities.
Figure 2.
HBV patient journey in KSA
In KSA, any suspected or confirmed case of HBV should be reported to the MoH. In the past 10 years, the number of diagnosed cases has been fairly stable [Figure 345] despite the declining prevalence. However, since prevalence is mainly declining in the younger populations due to the vaccination program, a lag in the trend of the diagnosed cases is to be expected.
Figure 3.
Cases of HBV reported to MoH.[45] Central: Riyadh and Qassem; Western: Makkah, Jeddah, Taif, Medinah, Tabuk, and Qunfudah; Eastern: Eastern Region, Al Ahsa, and Hafr Al Baten; Northern: Hail, Northern Borders, Al Jouf, and Qurayyat; Southern: Asir, Bishah, Jazan, Najran, and Al Baha
LINKAGE TO CARE AND TREATMENT
Most patients with CHB infection are identified at the primary care level, and only those with chronic active HBV needing further evaluation and antiviral therapy would be referred to specialist care, although many centers also follow-up those with inactive carrier stage at specialist level. However, only 15.7% of physicians were of the opinion that primary healthcare facilities are suitable to manage patients with HBV.[24] In KSA, the majority of treatment is delivered in the public sector as it contributes to around 89% of the HBV medication market in the context of nucleos(t)ide analogs (NAs).[46] Private sector facilities are mainly located in metropolitans such as Riyadh and Jeddah.
Figure 4 displays the CHB care pathway cascade in KSA. Of the estimated 260,000 prevalent cases in the country, only 14% have been diagnosed in the past 10 years. It must be noted that this is possibly an underestimation of the actual number with knowledge of their HBV-positive status, but verifiable data on this are not available. Of those diagnosed in the past 10 years, only 14% were on treatment in the past year 5,330 on treatment/37,440 diagnosed – Figure 4].[46] These statistics may be an underestimation, as not all patients need long-term treatment. Therefore, there is no clear estimation of the actual linkage to care for diagnosed/screened patients.
Figure 4.
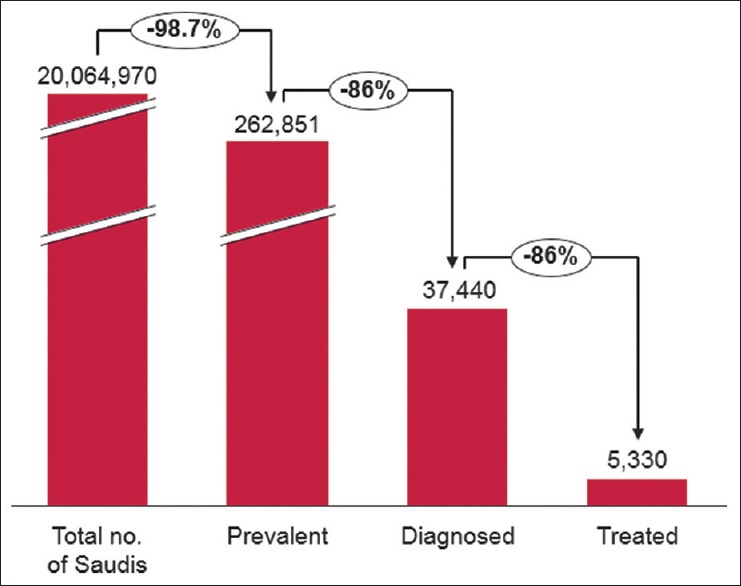
CHB care pathway cascade in KSA. Source: Total no. of Saudis from 2016 MoH Health Statistical Yearbook, Prevalence figure obtained by applying 1.31% on the population estimate, Treated[46]
The Saudi Association for the Study of Liver diseases and Transplantation (SASLT) has developed HBV practice guidelines which were published in 2014.[40] Although specialists also use the WHO,[47] European Association for the Study of the Liver,[48] and American Association for the Study of Liver Diseases[49] guidelines, implementation of these guidelines may differ across practitioners/hospitals. For chronic treatment, the recommended antiviral therapies for CHB treatment in the country are entecavir (ETV) and tenofovir disoproxil fumarate (TDF), although others – pegylated interferon (Peg-IFN-2a), lamivudine (LAM), telbivudine (TEL), adefovir (ADV) – have also been approved. In KSA, all these drugs have market authorization, but only ETV, TDF, and LAM are widely available in the public sector and freely reimbursable to Saudi patients when prescribed by a physician.[4]
There is the perception among some clinical practitioners and patients that current antiviral therapy may invoke long-term toxicity, and that health effects are unknown, while lifelong treatment might be needed. Disease progression is likely to occur when the suppressive effect of NAs is removed in cases of treatment cessation due to drug-related adverse events (AEs) or drug resistance in older publicly available medications.[48,49] The authors acknowledge, however, that newer effective medications may be available that do not carry such risks. There is an unmet need for a globally acknowledged and publicly available treatment that can cure HBV or at least present a higher barrier to resistance and fewer treatment-related AEs, than the currently available treatment options.
COMPLIANCE/ADHERENCE
It is recommended that all patients treated with NAs should be followed with periodical assessments.[40,48] Limited information could be found on chronic care and periodic patient follow-up among HBV patients in KSA.
A cross-sectional study collected data on 328 patients with viral hepatitis in a tertiary care setting;[50] 30% of patients were not compliant with follow-up visits. The loss to follow-up was higher among those who had been diagnosed with HBV compared with those diagnosed with HCV. The most important reasons for this included being unaware that a follow-up appointment was scheduled (69%), never being informed of the need for follow-up by healthcare provider (15%), personal belief that follow-up was not necessary (9%), logistical reasons (3%), and other reasons (5%).
Hepatology experts and KOLs also indicated that some patients defer therapy as it fails to provide a cure and they worry about the long-term effects of treatment as well as the risk of resistance.[4] This points to the need for enhanced patient education.
CONCLUSION AND ACTION POINTS
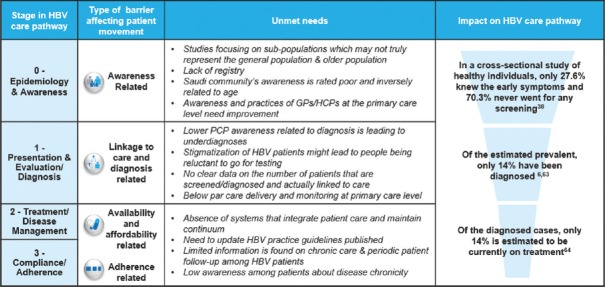
Four broad categories of gaps exist on the patient care pathway [Figure 5], and the related recommendations [Figure 6] are discussed below.
Figure 5.
Barriers on the KSA HBV patient care pathway
Figure 6.
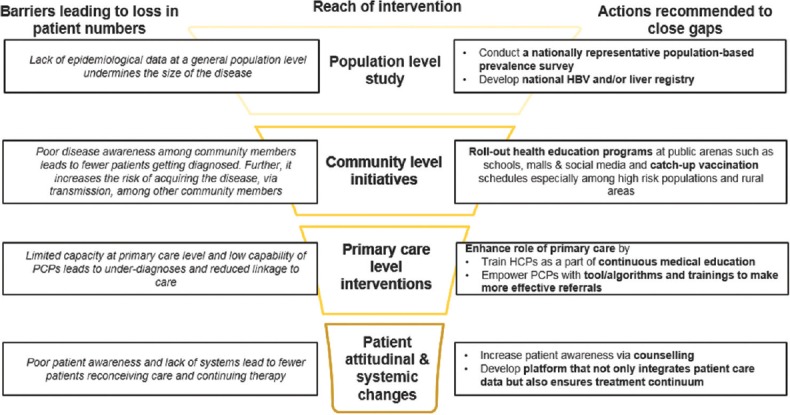
Action recommended to address gaps and optimize care pathway
A task force should be established to assist with developing a national platform/patient registry that integrates data on the HBV care pathway of all patients with HBV. This could keep track of whether patients who are screened are correctly diagnosed; diagnosed patients are followed-up or referred, and referred patients are initiated and retained on treatment with regular follow-up visits. This would assist in establishing the correct overall prevalence of the burden of HBV by age, gender, and resident status. The need for such a platform corroborates the key priority indicator set by the National Transformation Plan to increase the number of Saudi citizens who have a unified digital medical record[51]
Community-based educational interventions encompassing awareness about HBV, particularly the chronic nature of the disease, as well as the option of catch-up vaccination should be conducted. This is to increase knowledge in the general population and in high-risk groups (including medical staff).[43,44,45,46] Special attention should be paid to less developed areas to increase vaccination among high-risk populations and diagnosis of cases
Screening efforts should be increased (especially among those 30+ years and contacts of patients) to diagnose HBV-positive patients and link these to care
Training on HBV should be included as part of continued medical education activities organized by specialist associations such as the Saudi Gastroenterology Association and SASLT. Simple tools/algorithms and training for primary care physicians can empower them to make effective referrals for those patients in need. Also, those in primary care need to be educated on how to adequately follow-up those who do not need to be referred.
In conclusion, significant improvements have been made in KSA over the past 30 years to reduce HBV prevalence. However, challenges still remain concerning CHB management. Efforts must be made by all key stakeholders, including policy makers, in all phases of the HBV care pathway to reduce both morbidity and mortality in the KSA population.
Financial support and sponsorship
This work was supported by funding from Gilead Sciences. The authors had full access to the data and complete autonomy for analysis design, data analysis, data interpretation, manuscript writing, and submissions.
Conflicts of interest
Faisal M. Sanai is editor in chief of the Saudi Journal of Gastroenterology. There are no other conflicts of interest.
REFERENCES
- 1.Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: A systematic review of data published between 1965 and 2013. Lancet. 2015;386:1546–55. doi: 10.1016/S0140-6736(15)61412-X. [DOI] [PubMed] [Google Scholar]
- 2.WHO. WHO. Global Hepatitis Report, 20172017. [Last accessed on 2017 Nov 22]. Available from: http://apps.who.int/iris/bitstream/10665/255016/1/9789241565455.eng.pdf .
- 3.Specialist Panel on Chronic Hepatitis B in the Middle East. A review of chronic hepatitis B epidemiology and management issues in selected countries in the Middle East. J Viral Hepat. 2012;19:9–22. doi: 10.1111/j.1365-2893.2011.01511.x. [DOI] [PubMed] [Google Scholar]
- 4.Hepatology Experts and KOLs Meeting 7 October 2017. Kingdom of Saudi Arabia; 2017. [Google Scholar]
- 5.Al Humayed S, El-Mekki A, Mahfouz A. Hepatitis B virus infection in Aseer Region, south-western Saudi Arabia: A call for an immediate action against a preventable disease. Public Health. 2017;146:24–8. doi: 10.1016/j.puhe.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Alrowaily MA, Abolfotouh MA, Ferwanah MS. Hepatitis B virus sero-prevalence among pregnant females in Saudi Arabia. Saudi J Gastroenterol. 2008;14:70–2. doi: 10.4103/1319-3767.39621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El Beltagy KE, Al Balawi IA, Almuneef M, Memish ZA. Prevalence of hepatitis B virus markers among blood donors in a tertiary hospital in Tabuk, northwestern Saudi Arabia. Int J Infect Dis. 2008;12:495–9. doi: 10.1016/j.ijid.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Gasim GI. Hepatitis B virus in the Arab world: Where do we stand? Arab J Gastroenterol. 2013;14:35–43. doi: 10.1016/j.ajg.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Abdelhay O, Al Rsheed AR, Al Khashan H, Yagoub U. The unfit for military services among potential new recruits in Riyadh KSA. Int J Recent Sci Res. 2015;6:6129–33. [Google Scholar]
- 10.Al-Faleh F, Al-Shehri S, Al-Ansari S, Al-Jeffri M, Al-Mazrou Y, Shaffi A, et al. Long-term protection of hepatitis B vaccine 18 years after vaccination. J Infect. 2008;57:404–9. doi: 10.1016/j.jinf.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Al-Faleh FZ. Changing pattern of hepatitis viral infection in Saudi Arabia in the last two decades. Ann Saudi Med. 2003;23:367–71. doi: 10.5144/0256-4947.2003.367. [DOI] [PubMed] [Google Scholar]
- 12.Alharbi A, Alouffi S, Alcantara J, Kabrah S, Tolba M, Aludhaib M, et al. Prevalence of hepatitis B virus markers among blood donors in Qassim Region, Saudi Arabia. Int J Pharm Res Allied Sci. 2017;6:99–106. [Google Scholar]
- 13.Alhuraiji A, Alaraj A, Alghamdi S, Alrbiaan A, Alrajhi AA. Viral hepatitis B and C in HIV-infected patients in Saudi Arabia. Ann Saudi Med. 2014;34:207. doi: 10.5144/0256-4947.2014.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aljarbou AN. Current prevalence of HBV and HCV seropositivity: The initiative for attentiveness and deterrence of viral hepatitis in the Qassim region of Saudi Arabia. J Antivir Antiretrovir. 2012;4:75–9. [Google Scholar]
- 15.Alshomrani AT. Prevalence of human immunodeficiency virus, hepatitis C virus, and hepatitis B virus infection among heroin injectors in the central region of Saudi Arabia. Saudi Med J. 2015;36:802. doi: 10.15537/smj.2015.7.11475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alswaidi FM, O'Brien S. Is there a need to include HIV, HBV and HCV viruses in the Saudi premarital screening program on the basis of their prevalence and transmission risk factors? J Epidemiol Community Health. 2010;64:989–97. doi: 10.1136/jech.2009.093302. [DOI] [PubMed] [Google Scholar]
- 17.Al-Thaqafy MS, Balkhy HH, Memish Z, Makhdom YM, Ibrahim A, Al-Amri A, et al. Hepatitis B virus among Saudi National Guard personnel: Seroprevalence and risk of exposure. J Infect Public Health. 2013;6:237–45. doi: 10.1016/j.jiph.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Medani KE, Al Fehaid F, Abdalla SM, Bashir AA, Al Mansour M, Yousif E. The prevalence of hepatitis B among medical students, Majmaah University, Kingdom of Saudi Arabia. Int J Pharm Med Res. 2015;3:191–4. [Google Scholar]
- 19.Zampino R, Boemio A, Sagnelli C, Alessio L, Adinolfi LE, Sagnelli E, et al. Hepatitis B virus burden in developing countries. World J Gastroenterol. 2015;21:11941. doi: 10.3748/wjg.v21.i42.11941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alswaidi F, Memish Z, Al-Hakeem R, Atlam S. Saudi Arabian expatriate worker fitness-screening programme: A review of 14 years of data. Eastern Mediterr Health J. 2013;19:664–70. [PubMed] [Google Scholar]
- 21.Al-Faleh F, Ayoola E, Arif M, Ramia S, Al-Rashed R, Al-Jeffry M, et al. Seroepidemiology of hepatitis B virus infection in Saudi Arabian children: A baseline survey for mass vaccination against hepatitis B. J Infect. 1992;24:197–206. doi: 10.1016/0163-4453(92)93006-c. [DOI] [PubMed] [Google Scholar]
- 22.Abdo AA, Sanai FM, Al-Faleh FZ. Epidemiology of viral hepatitis in Saudi Arabia: Are we off the hook? Saudi J Gastroenterol. 2012;18:349–57. doi: 10.4103/1319-3767.103425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Faleh FZ, Ayoola EA, Al-Jeffry M, Arif M, Al-Rashed RS, Ramia S. Integration of hepatitis B vaccine into the expanded program on immunization: The Saudi Arabian experience. Ann Saudi Med. 1993;13:231–6. doi: 10.5144/0256-4947.1993.231. [DOI] [PubMed] [Google Scholar]
- 24.Al-Faleh FZ, Al-Jeffri MH, Al-Rashed RS, Aref M. Efficacy of hepatitis B vaccine in a cohortcommunity-based study in Riyadh and Hail regions of Saudi Arabia. Saudi J Gastroenterol. 2002;8:81–4. [PubMed] [Google Scholar]
- 25.Ahmad IA, Rehan EA, Pani SC. Compliance of S audi dental students with infection control guidelines. Int Dent J. 2013;63:196–201. doi: 10.1111/idj.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al-Dharrab AA, Al-Samadani KH. Assessment of hepatitis B vaccination and compliance with infection control among dentists in Saudi Arabia. Saudi Med J. 2012;33:1205–10. [PubMed] [Google Scholar]
- 27.Ghomraoui FA, Alfaqeeh FA, Algadheeb AS, Al-alsheikh AS, Al-Hamoudi WK, Alswat KA. Medical students' awareness of and compliance with the hepatitis B vaccine in a tertiary care academic hospital: An epidemiological study. J Infect Public Health. 2016;9:60–5. doi: 10.1016/j.jiph.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 28.Alrowaily F, Bedairi A, Aziz A, Wani F, Banday A. A cross-sectional assessment of attitude and practice toward Hepatitis B among primary health care workers in Aljouf region of Saudi Arabia. Int J Med Sci Public Health. 2016;5:313–7. [Google Scholar]
- 29.El-Fetoh N, Alenzi RTR, Ghabban KM, Alanzi HS, Ghabban AM. A cross sectional assessment of knowledge, attitude and practice towards hepatitis B among healthy population of Arar, Saudi Arabia. Merit Res J Med Med Sci. 2017;5:156–64. [Google Scholar]
- 30.Eisa ZM, Eifan SA, Al-Sum BA. Awareness of viral Hepatitis B and C infection among first year medical sciences students in Jazan University. Public Health Res. 2012;2:167–73. [Google Scholar]
- 31.Al-Hazmi AH. Knowledge, attitudes and practice of primary health care physicians towards hepatitis B virus in Al-Jouf province, Saudi Arabia. BMC Res Notes. 2014;7:288. doi: 10.1186/1756-0500-7-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ringelhan M, O'Connor T, Protzer U, Heikenwalder M. The direct and indirect roles of HBV in liver cancer: Prospective markers for HCC screening and potential therapeutic targets. J Pathol. 2015;235:355–67. doi: 10.1002/path.4434. [DOI] [PubMed] [Google Scholar]
- 33.SOLID. Systematic Observatory Liver Diseases Registry 2018. [Last accessed on 2018 July 31]. Available from: www.solid-registry.com/home.html .
- 34.Alavian SM, Haghbin H. Relative importance of hepatitis B and C viruses in hepatocellular carcinoma in EMRO countries and the middle east: A systematic review. Hepat Mon. 2016;16:e35106. doi: 10.5812/hepatmon.35106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qari Y, Mosli M. Epidemiology and clinical features of patients with hepatocellular carcinoma at a tertiary hospital in Jeddah. Niger J Clin Pract. 2017;20:43–7. doi: 10.4103/1119-3077.180062. [DOI] [PubMed] [Google Scholar]
- 36.Aljumah AA, Kuriry H, AlZunaitan M, Al Ghobain M, Al Muaikeel M, Al Olayan A, et al. Clinical presentation, risk factors, and treatment modalities of hepatocellular carcinoma: A single tertiary care center experience. Gastroenterol Res Pract 2016. 2016:1989045. doi: 10.1155/2016/1989045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khan G, Hashim MJ. Burden of virus-associated liver cancer in the Arab World 1990-2010. Asian Pac J Cancer Prev. 2015;16:265–70. doi: 10.7314/apjcp.2015.16.1.265. [DOI] [PubMed] [Google Scholar]
- 38.Sanai FM, Alghamdi H, Alswat KA, Babatin MA, Ismail MH, Alhamoudi WK, et al. Greater prevalence of comorbidities with increasing age: Cross-sectional analysis of chronic hepatitis B patients in Saudi Arabia? Saudi J Gastroenterol. 2018 doi: 10.4103/sjg.SJG_447_18. doi: 10.4103/sjg.SJG_447_18. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aljarbou AN. The emergent concern of Hepatitis B globally with special attention to Kingdom of Saudi Arabia. Int J Health Sci. 2013;7:333. doi: 10.12816/0006062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abaalkhail F, Elsiesy H, AlOmair A, Alghamdi MY, Alalwan A, AlMasri N, et al. SASLT practice guidelines for the management of hepatitis B virus. Saudi J Gastroenterol. 2014;20:5–25. doi: 10.4103/1319-3767.126311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Council of Health Services. Clinical Guidelines for Hemodialysis Centers in the Kingdom of Saudi Arabia. (1st ed) 2013 1435H. [Google Scholar]
- 42.Gulf Health Council. Rules and Regulations for Medical Examination of Expatriates Coming to GCC States for Residency. 4th ed. Dhul-Qaeda: 2016. [Last accessed on 2017 Aug 22]. Available from: https://gcchmc.org/Images/RulesAndRegulationForMedical-Nov2016.pdf . [Google Scholar]
- 43.Ibrahim NK, Bashawri J, Al Bar H, Al Ahmadi J, Al Bar A, Qadi M, et al. Premarital screening and genetic counseling program: Knowledge, attitude, and satisfaction of attendees of governmental outpatient clinics in Jeddah. J Infect Public Health. 2013;6:41–54. doi: 10.1016/j.jiph.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 44.MoH. Kingdom of Saudi Arabia Ministry of Health Guidelines on Blood Donation Saudi Arabia. [Last accessed on 2017 Aug 22]. Available from: http://www.moh.gov.sa/en/HealthAwareness/EducationalContent/Blog/1435/Pages/Artical-2014-06-08.aspx .
- 45.KSA MOH Statistics between 2007 and 2016. Saudi Arabia: Ministry of Health; 2017. [Last accessed on 2018 Jul 15]. Available from: https://www.moh.gov.sa/en/Ministry/Statistics/book/Pages/default.aspx . [Google Scholar]
- 46.IQVIA. Local and MIDAS Sales Data MAT Q4. 2016 [Google Scholar]
- 47.WHO. Guidelines for the Prevention Care and Treatment of Persons with Chronic Hepatitis B Infection. Geneva: World Health Organization; 2015. [Last accessed on 2017 Aug 22]. Available from: https://www.who.int/hiv/pub/hepatitis/hepatitis-b-guidelines/en/ [PubMed] [Google Scholar]
- 48.European Association for the Study of the Liver. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2017;67:370–98. doi: 10.1016/j.jhep.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 49.Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63:261–83. doi: 10.1002/hep.28156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Balkhy HH, El-Saed A, Sanai FM, Alqahtani M, Alonaizi M, Niazy N, et al. Magnitude and causes of loss to follow-up among patients with viral hepatitis at a tertiary care hospital in Saudi Arabia. J Infect Public Health. 2017;10:379–87. doi: 10.1016/j.jiph.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 51.Vision 2030. National Transformation Program 2020. 2017. [Last accessed on 2018 Jul 15]. Available from: https://vision2030.gov.sa/en .