Key Points
CMML patients comprise an elderly and frail patient population with comorbidities that often require surgical intervention.
Postsurgical leukemoid reaction, a life-threatening complication in CMML patients, may be driven by molecular mechanisms.
Introduction
Chronic myelomonocytic leukemia (CMML) is a myelodysplastic/myeloproliferative overlap syndrome characterized by myeloid cell proliferation, dyspoiesis, and ineffective hematopoiesis.1 Patients present with clinical features typical of ineffective hematopoiesis, such as anemia and thrombocytopenia, but simultaneously exhibit signs of myeloid hyperplasia, such as splenomegaly, leukocytosis, and constitutional symptoms. CMML disproportionally affects elderly individuals, with an average age at diagnosis of ∼72 years.2 Patients often have multiple comorbidities that compromise the ability to administer intensive therapies and compete with CMML as contributors to all-cause mortality. Elective or emergent surgical intervention for nonhematologic medical problems is inevitable among the aging CMML population. Here, we describe a series of CMML patients undergoing surgical intervention for unrelated medical causes who developed life-threatening postoperative leukostasis, and highlight the considerable perioperative risks unique to these patients. We discuss how CMML disease biology may contribute to these risks and offer practical advice on perioperative management strategies.
Case description
See Table 1 for preoperative and postoperative laboratory values in each case.
Table 1.
Case preoperative and postoperative laboratory values
| Patient 1: CMML-1 | Patient 2: CMML-0 | Patient 3: CMML-1 | ||||
|---|---|---|---|---|---|---|
| Presurgical | Postsurgical | Presurgical | Postsurgical | Presurgical | Postsurgical | |
| WBC, ×109/L | 5.48 | 346.9 | 20.3 | 119.8 | 9.9 | 104 |
| Hemoglobin, g/dL | 11.1 | 8.4 | 13.8 | 12.3 | 7.7 | 9.2 |
| Hematocrit, % | 36.3 | 25.6 | 41.4 | 37.1 | 24 | 28 |
| Platelet count, ×109/L | 126 | 132 | 70 | 130 | 71 | 83 |
| Absolute band count, ×109/L | 0 | 93.4 | 0 | 32.3 | 0 | 9 |
| Absolute neutrophil count, ×109/L | 3.48 | 134 | 13.9 | 45.5 | 7.72 | 60.32 |
| Absolute lymphocyte count, ×109/L | 1.25 | 6.92 | 3.7 | 3.6 | 1.29 | 3.12 |
| Absolute monocyte count, ×109/L | 0.54 | 44.9 | 2.6 | 31.1 | 0.59 | 8.32 |
| Absolute eosinophil count, ×109/L | <0.03 | 0 | 0.1 | 0 | 0.2 | 1.04 |
| Absolute basophil count, ×109/L | 0.16 | 3.4 | 0.1 | 0 | 0 | 0 |
| Absolute metamyelocyte count, ×109/L | 0 | 20.7 | 0 | 4.8 | N/A | N/A |
| Absolute myelocyte count, ×109/L | 0 | 27.6 | 0 | 1.2 | N/A | N/A |
| Absolute blast count, ×109/L | 0 | 6.92 | 0 | 0 | N/A | N/A |
| LDH, U/L | 134 | 1289 | 245 | 951 | 155 | 341 |
| Creatinine, mg/dL | 0.73 | 0.97 | 1.1 | 2 | 1.44 | 1.81 |
| AST, U/L | 13 | 51 | 30 | 6987 | 17 | 20 |
| ALT, U/L | 13 | 40 | 23 | 3316 | 16 | 19 |
| Total bilirubin, mg/dL | 0.6 | 3.9 | 0.9 | 2.4 | 0.4 | 0.4 |
| Alkaline phosphatase, U/L | 133 | 312 | 49 | 229 | 97 | 86 |
| Lactate, mg/dL | N/A | 18 | N/A | 12.4 | N/A | N/A |
| Somatic mutations | TET2 (2), SRSF2, ASXL1, SETBP1, CBL, FLT3-TKD | TET2, SRSF2, KRAS | ||||
ALT, alanine aminotransferase; AST, aspartate aminotransferase; LDH, lactate dehydrogenase; N/A, not applicable; WBC, white blood cell.
Case 1
A 75-year-old woman with CMML-1 (peripheral blasts 2%-4% and/or bone marrow blasts 5%-9%) and failure of 5-azacitidine had maintained a partial remission on decitabine (20 mg/m2, days 1-5, every 3 weeks) for 3 years. Comorbidities included hypothyroidism and depression. She sustained a fall with left hip fracture prior to cycle 36, was admitted to a community facility, and cleared by hematology for hip arthroplasty. One day after surgery, she experienced hemorrhagic shock from a surgical site hematoma. Following hematoma evacuation, she developed leukocytosis and was transferred to an academic center. Following transfer, she decompensated rapidly, requiring intubation, pressor support, antibiotics, stress-dose steroids, and paralytic agents for respiratory failure and shock. Leukocytosis increased to 346 × 109/L with 2% peripheral blasts, LDH to 1289 U/L, and lactate to 18 mmol/L. Leukapheresis was deferred due to tenuous hemodynamics. Following cardiac arrest, care was withdrawn and she died. Autopsy demonstrated multiorgan leukostasis (Figure 1). Bone marrow at autopsy demonstrated hypercellularity (>95%), with trilineage hematopoiesis and multilineage dysplasia consistent with CMML, without evidence of transformation to acute myeloid leukemia.
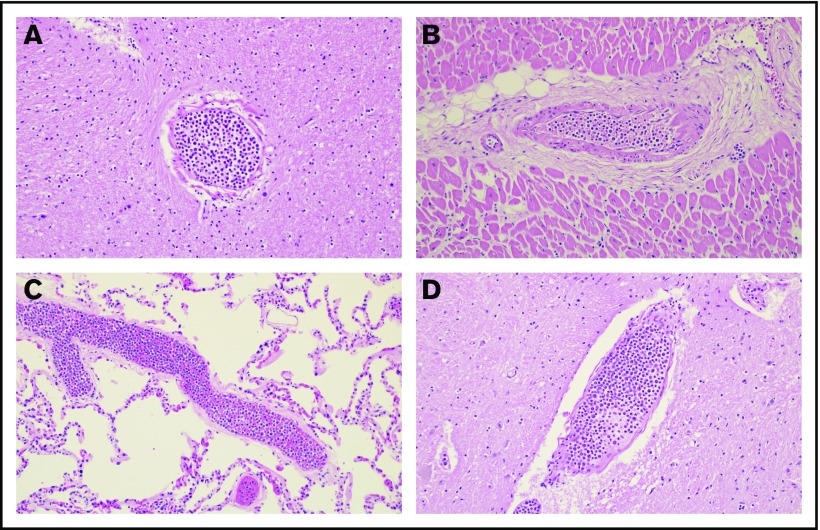
Figure 1.
Multiorgan leukostasis (case 1). Hematoxylin and eosin–stained sections (original magnification ×20) taken from autopsy showed severe diffuse leukostasis in the brain (A), heart (B), lungs (C), and spinal cord (D). Additionally, the spleen, liver, colon, and uterus displayed similar findings with evidence of ischemia and end-organ damage (not shown).
Case 2
A 67-year-old man with aortic valve stenosis and CMML-0 (peripheral blasts <2% and bone marrow blasts <5%) on surveillance was cleared by hematology for aortic valve replacement surgery. The patient had no previous treatment of his CMML. Comorbidities included hypertension and hyperlipidemia. One day after uncomplicated aortic valve surgery, he was noted to have increasing leukocytosis and developed respiratory failure requiring intubation, multiple pressor support, dialysis, and stress-dose steroids. WBC count rose to 119 × 109/L without increase in peripheral blasts. Significant laboratory results included elevated LDH of 951 U/L, lactate of 10.8 mmol/L, alanine aminotransferase of 3316 U/L, and AST of 6987 U/L. The patient had a cardiopulmonary arrest with unsuccessful resuscitation and died 5 days post–valve replacement.
Case 3
An 86-year-old woman with CMML-1, hypertension, and kidney disease underwent cardiology evaluation for heart failure and was recommended for cardiac catheterization. Prior to catheterization, the patient had been on low-dose decitabine therapy (20 mg/m2, days 1-3, every 4 weeks) with persistent bicytopenia but achievement of transfusion independence. She underwent uneventful cardiac catheterization with no critical coronary stenosis identified. Five days later, the patient reported shortness of breath and dizziness. She was found to be in volume overload with pulmonary opacities on chest radiograph and WBC count of 104 × 109/L without increase in peripheral blasts. Echocardiogram showed preserved ejection fraction (65%). She was admitted to intensive care and was treated for pneumonia and volume overload but was unable to be weaned from high oxygen requirement. Leukostasis was suspected and hydroxyurea and decitabine (20 mg/m2 days 1-5) were initiated. Her WBC count decreased to <30 × 109/L; she was weaned off supplemental oxygen and discharged home in stable condition.
Methods
This report is a retrospective chart review of patients from different institutions who developed postsurgical complications. The study was evaluated for local institutional review board approval at each site and found to be exempt.
Results and discussion
We describe 3 patients with CMML who developed acute postoperative complications associated with a rapid rise of WBC count with a clinical picture suggestive of leukostasis and reminiscent of cytokine release syndrome (CRS). All patients required transfer to the intensive care unit.
Advances in CMML biology provide some mechanistic insight into the pathogenesis of the acute postsurgical reaction in these 3 patients. Primary CMML cells exhibit STAT5 activation and colony formation with low doses of granulocyte-macrophage colony-stimulating factor (GM-CSF), consistent with GM-CSF hypersensitivity.3 GM-CSF is essential for monocytic and granulocytic cell proliferation and is recognized as an important mediator of local tissue inflammation at sites of injury, such as the synovial fluid of patients with autoimmune arthritis or in the cerebrospinal fluid of patients with multiple sclerosis.4,5 Moreover, TET2 mutations are one of the most frequently observed molecular abnormalities in CMML and are detected in 50% to 60% of patients.6,7 TET2-deficient mouse macrophages demonstrate increased expression of inflammatory cytokines and chemokines, including CXCL1, CXCL2, CXCL3, platelet factor 4, interleukin-1β (IL-1β), and IL-6, and plasma from patients with clonal hematopoiesis harboring TET2 mutations exhibits increased levels of the CXC chemokine IL-8.8 Similarly, concentrations of proinflammatory cytokines (IL-8, IL-10, IL-1 receptor antagonist, tumor necrosis factor α, IL-6) are increased in CMML patients compared with healthy controls.9 Trauma precipitated by surgery may stimulate local inflammatory cytokine signaling that efficiently recruits clonally derived monocytes and granulocytes from the bone marrow into the circulation. This cycle of stimulation and recruitment is perpetuated to such a degree that a catastrophic hyperinflammatory state characterized by leukostasis ensues. Notably, risk of leukostasis in acute myeloid leukemia with monocytic differentiation and CMML correlates poorly with the proportion or number of blasts in the peripheral blood, suggesting a distinct pathogenesis of leukostasis in monocytic leukemias.10 CMML monocytes frequently overexpress aberrant cell adhesion molecules such as CD56/neural cell adhesion molecule,11 which has been associated with increased risk of severe leukostasis in monocytic acute leukemias, and may explain their “sticky” properties.12
Two patients experienced rapid clinical decline and died from multiorgan failure and shock despite significant attempts at resuscitation, highlighting that postsurgical leukemoid reaction is an unrecognized risk among practitioners. Importantly, all CMML cases underwent informal or formal preoperative clearance by hematology. A literature search revealed another case of a CMML patient with a fatal hyperinflammatory reaction after coronary artery bypass surgery.13 Two of our patients developed leukemoid reaction despite active treatment with decitabine, suggesting that hypomethylating agent therapy does not modulate this risk.
All patients deteriorated within 1 week of surgery. As such, for CMML patients requiring elective or emergent major surgery, we recommend hematology consultation and close daily monitoring of peripheral blood counts postoperatively for 1 week in the inpatient or outpatient setting as clinically appropriate. Early institution of hydroxyurea, allopurinol, and IV fluids should be considered on a case-by-case basis if rising leukocytosis and LDH are observed and there is high clinical suspicion for leukostasis. In view of the rapid deterioration observed in our 3 cases, a low threshold should be applied with respect to inpatient admission for observation of clinical signs associated with leukostasis and/or cytokine release (hypoxia, focal neurologic symptoms, arrhythmia, renal failure). Interestingly, all 3 patients initially presented with the myeloproliferative variant of CMML, and the 2 patients who were sequenced harbored RAS-pathway mutations, a feature associated with the proliferative subtype.14 Patients with the myeloproliferative variant of CMML and those with RAS-pathway mutations may be at higher risk for leukostasis following surgery and even minor procedures (ie, cardiac catherization), and these factors should inform the postoperative monitoring plan.
In our experience, hyperleukocytosis in response to infections is common among CMML patients, but is not typically fatal. Why surgical interventions precipitate a more fulminant reaction reminiscent of CRS is unknown. It is possible that anti-inflammatory agents directed against cytokines known to be elevated in both CMML and CRS, such as siltuximab (monoclonal antibody against IL-6), may be effective in refractory cases. A systematic study of surgical morbidity and mortality in CMML is warranted.
Acknowledgments
The authors acknowledge the contributions of their patients.
A.B.P. was supported by an American Society of Hematology Research Training Award for Fellows.
Authorship
Contribution: A.B.P. wrote the initial draft of the manuscript; A.B.P., E.M.P., S.M.A., and M.W.D. participated in the care of included patients; E.R. provided histologic images; and all authors reviewed the final draft of the manuscript and approved its submission.
Conflict-of-interest disclosure: M.W.D. reports research funding from, and is a paid advisory board member and/or consultant for, the following companies: Blueprint; Pfizer, Inc; Takeda; Ascentage Pharma; Aptitude Health; and Humana. The remaining authors declare no competing financial interests.
Correspondence: Michael W. Deininger, Division of Hematology and Hematologic Malignancies, Huntsman Cancer Institute, The University of Utah, 2000 Circle of Hope Dr, Salt Lake City, UT 84112; e-mail: michael.deininger@hci.utah.edu.
References
- 1.Arber DA, Orazi A, Hasserjian R, et al. . The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391-2405. [DOI] [PubMed] [Google Scholar]
- 2.Solary E, Itzykson R. How I treat chronic myelomonocytic leukemia. Blood. 2017;130(2):126-136. [DOI] [PubMed] [Google Scholar]
- 3.Padron E, Painter JS, Kunigal S, et al. . GM-CSF-dependent pSTAT5 sensitivity is a feature with therapeutic potential in chronic myelomonocytic leukemia. Blood. 2013;121(25):5068-5077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Becher B, Tugues S, Greter M. GM-CSF: from growth factor to central mediator of tissue inflammation. Immunity. 2016;45(5):963-973. [DOI] [PubMed] [Google Scholar]
- 5.Lang RA, Metcalf D, Cuthbertson RA, et al. . Transgenic mice expressing a hemopoietic growth factor gene (GM-CSF) develop accumulations of macrophages, blindness, and a fatal syndrome of tissue damage. Cell. 1987;51(4):675-686. [DOI] [PubMed] [Google Scholar]
- 6.Yamazaki J, Taby R, Vasanthakumar A, et al. . Effects of TET2 mutations on DNA methylation in chronic myelomonocytic leukemia. Epigenetics. 2012;7(2):201-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patnaik MM, Zahid MF, Lasho TL, et al. . Number and type of TET2 mutations in chronic myelomonocytic leukemia and their clinical relevance. Blood Cancer J. 2016;6(9):e472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaiswal S, Natarajan P, Silver AJ, et al. . Clonal hematopoiesis and risk of atherosclerotic cardiovascular disease. N Engl J Med. 2017;377(2):111-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niyongere S, Lucas N, Zhou JM, et al. . Heterogeneous expression of cytokines accounts for clinical diversity and refines prognostication in CMML. Leukemia. 2019;33(1):205-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Novotny JR, Müller-Beissenhirtz H, Herget-Rosenthal S, Kribben A, Dührsen U. Grading of symptoms in hyperleukocytic leukaemia: a clinical model for the role of different blast types and promyelocytes in the development of leukostasis syndrome. Eur J Haematol. 2005;74(6):501-510. [DOI] [PubMed] [Google Scholar]
- 11.Lacronique-Gazaille C, Chaury MP, Le Guyader A, Faucher JL, Bordessoule D, Feuillard J. A simple method for detection of major phenotypic abnormalities in myelodysplastic syndromes: expression of CD56 in CMML. Haematologica. 2007;92(6):859-860. [DOI] [PubMed] [Google Scholar]
- 12.Novotny JR, Nückel H, Dührsen U. Correlation between expression of CD56/NCAM and severe leukostasis in hyperleukocytic acute myelomonocytic leukaemia. Eur J Haematol. 2006;76(4):299-308. [DOI] [PubMed] [Google Scholar]
- 13.Galea SA, Galea J. Urgent coronary artery bypass surgery in a patient with postinfarction angina and active myelomonocytic leukaemia. Case Rep Oncol. 2016;9(3):781-785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ricci C, Fermo E, Corti S, et al. . RAS mutations contribute to evolution of chronic myelomonocytic leukemia to the proliferative variant. Clin Cancer Res. 2010;16(8):2246-2256. [DOI] [PubMed] [Google Scholar]