Abstract
Background
Increased empathy may improve patient perceptions and outcomes. No training tool has been derived to teach empathy to emergency care providers. Accordingly, we engaged patients to assist in creating a concept map to teach empathy to emergency care providers.
Methods
We recruited patients, patient caretakers and patient advocates with emergency department experience to participate in three separate focus groups (n = 18 participants). Facilitators guided discussion about behaviors that physicians should demonstrate to rapidly create trust; enhance patient perception that the physician understood the patient's point of view, needs, concerns, and fears; and optimize patient/caregiver understanding of their experience. Verbatim transcripts from the three focus groups were read by the authors, and by consensus, five major themes with 10 minor themes were identified. After creating a codebook with thematic definitions, one author reviewed all transcripts to a library of verbatim excerpts coded by theme. To test for inter‐rater reliability, two other authors similarly coded a random sample of 40% of the transcripts. Authors independently chose excerpts that represented consensus and strong emotional responses from participants.
Results
Approximately 90% of opinions and preferences fell within 15 themes, with five central themes: provider transparency, acknowledgment of patient's emotions, provider disposition, trust in physician, and listening. Participants also highlighted the need for authenticity, context, and individuality to enhance empathic communication. For empathy map content, patients offered example behaviors that promote perceptions of physician warmth, respect, physical touch, knowledge of medical history, explanation of tests, transparency, and treating patients as partners. The resulting concept map was named the “Empathy Circle.”
Conclusions
Focus group participants emphasized themes and tangible behaviors to improve empathy in emergency care. These were incorporated into the Empathy Circle, a novel concept map that can serve as the framework to teach empathy to emergency care providers.
Empathy can be defined as the ability to understand and share the feelings of another.1 For physicians, empathizing with their patients includes understanding the patient's perspectives, concerns, feelings, and experiences. Empathy also requires physicians to communicate this understanding to their patients, initiating a sense of reciprocity, a key aspect of reassurance.2 Empathy creates a foundation for a successful physician–patient relationship and enhances several aspects of patient care. In settings of recurrent and continuous care (e.g., primary care setting), improved empathy predicts better patient comprehension, more trust in the physicians, higher satisfaction with care, improved adherence, lower anxiety, and better clinical outcomes in chronic disease management.3, 4, 5, 6 Strategies to enhance physician empathy might reduce patient thoughts of suing a physician in the event of an adverse outcome.7 To improve provider empathy, several tools and courses have been created and tested in the primary care setting.3, 8 However, current literature reveals no specific method or tool that has been derived to enhance empathy in the emergency care setting. The emergency care setting and associated patient experiences imposes a different set of challenges than other health care setting. These include the nature of the single encounter between strangers, reduced information and time availability of providers, patient exposure to long wait times, isolation, overcrowding and lack of privacy,9 and multiple patient factors, including unpredictable disease acuity, high psychosocial stress, and anxiety.9, 10
To ensure that the content of our concept map and ultimately empathy training contains the patient perspective, we convened three focus groups as a forum for advocates, patients, and caretakers to discuss different aspects of their experiences in the emergency department (ED). The patient perspective is important as we only have insight to the provider perspective of the relationship. We planned in advance for the facilitators to direct the dialogue toward a better understanding of specific verbal and nonverbal clinician behaviors that would improve perceptions of empathy in the patient–provider relationship.10, 11 Our objective was to use patient input from our focus groups to allow the construction of an empathy concept map to enhance empathic communication in the ED.
Methods
Theoretical Construct of the Work
From a learning perspective, the authors assume that the method to create empathy contains unknown domains to learners (a “black box”) that must be broken into understandable actions, words, and behaviors (i.e., a knowledge structure).12 Thus, we undertook a cognitivist approach, meaning that a framework in the form of a visual concept map would facilitate acquisition and recall of the behaviors that enhance empathy.13 This approach draws from the findings of a prior multicenter investigation of the thoughts and opinions of patients undergoing low‐value computerized tomographic imaging in the ED.11 In that sample, we directed patients in the ED to provide a Likert scale ranking of 11 specific phrases and to provide their own examples of words to enhance empathy, trust, and positive feelings toward their physician. The present work takes the next step to interview patients, caretakers, and advocates and allow a more personalized and detailed discussion to generate a concept map to teach empathy to emergency care providers. We hypothesized that patient‐provided information would enable effective categorization and description of semantics and behaviors in a domain map as the center point to effectively teach empathy.
Participants
We conducted three focus groups between February 2017 and April 2018 with a goal of 18 participants, a sample size that has been found to produce 90% thematic saturation in comparable studies.14 Each group comprised six participants with experience as a patient or family member in the ED. The first focus group took place in Indianapolis, IN, with participants from California (n = 4, all African American), Pennsylvania (n = 1, white), and Texas (n = 1, White). In addition to all being patients themselves, these six were also recognized patient advocates, each associated with one or more patient advocacy organizations. The second focus group was conducted in Dallas, TX, with participants from that area, including four of Hispanic ethnicity. The third group was again conducted in Indianapolis, IN, with participants from that area, including four African American and two white participants. These locations were chosen for convenience with the primary intent to include a diverse group of patients. Participants from focus group 1 were all patient partners in the Society for Academic Emergency Medicine's 2016 Consensus Conference on shared decision making. Participants in focus groups 2 and 3 were recruited by research coordinators through direct solicitation in the ED. The coordinators identified participants who had more than five lifetime visits to the ED. The patients were asked if they were willing to participate in a focus group. Those that were willing received a follow‐up phone call to schedule the focus group. Tables 1 and 2 show the relevant demographic and medical characteristics of the focus group members. Specific ages of our participants were not collected, but authors estimate an age range of 30 to 65 years among participants.
Table 1.
Demographic Characteristics of Focus Group Participants
| Focus Group Participants (n = 18) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Race | Ethnicity | Place of residence | |||||||
| Male | female | White | Non‐white | Latino | Non‐Latino | South | Midwest | East | West | |
| Total number | 4 | 14 | 10 | 8 | 3 | 15 | 7 | 6 | 1 | 4 |
| Percentage | 22 | 78 | 56 | 44 | 17 | 83 | 39 | 33 | 6 | 22 |
Table 2.
Medical Conditions Represented by Focus Group Participants by Report
|
Focus group 1 BF—History of connective tissue disease and possibly multiple sclerosis BF—History of hypertension, diabetes, chronic anxiety; experienced patient advocate for care of urban patients with health care disparities BF—Prior history of chronic migraine headaches, law student and participant in patient advocacy groups BF—Chronic anemia, multiple ED visits and hospitalizations for postsurgical (hysterectomy) complications WM—Stable heart disease of chronic medical condition, patient advocate representing a cardiovascular group WF—Caretaker of a severely brain injured child Focus group 2 WM—Heart failure, chronic musculoskeletal pain LF—Prior history of cholelithiasis requiring cholecystectomy, hypertension, diabetes LF—Caretaker of child with chromosomal abnormality causing multiple organ dysfunction LF—Multiple chronic medical conditions requiring frequent ED visits WF—Schoolteacher with stable and minor medical problems BF—Chronic recurring chest pain ultimately diagnosed as hypertrophic asymmetric cardiomyopathy Focus group 3 BM—End‐stage renal disease requiring dialysis WF–Chronic somatic pain diagnosed as fibromyalgia BF—Caregiver for family member with pancreatic cancer BM—Elderly, wheelchair bound, heart failure WF—Chronic recurring skin infections requiring frequent ED visits WF—Chronic lung disease and heart failure requiring defibrillator |
BF = black female; BM = black male; LF = Latino female; WF = white female; WM = white male.
Procedures
The study was deemed exempted by the Indiana University Institutional Review Board. Each focus group was led by a different nonphysician facilitator with experience in focus group facilitation and guided by established techniques.15, 16 The facilitators were made aware of our study hypothesis but were allowed the flexibility to navigate the focus group without physician interference. Focus groups lasted between 4 and 6 hours and were video and audio recorded. At the onset, participants were informed of the purpose of the study. The focus groups used a semistructured protocol that started by asking participants to share their previous experiences in the ED. The facilitator subsequently asked more directed questions to encourage the participants to reflect on important aspects of a desirable physician–patient relationship. One recurrent role of the facilitator was frequent redirection of participants toward explanation of and elaboration on positive verbal and nonverbal behaviors displayed by providers. These questions varied slightly for each focus group based on the flow of the conversation. Each focus group was also attended by at least three authors, who each created independent real‐time field notes about the content of discussions with specific annotation about which discussions elicited the highest emotional reactions, and noncodable indications of nonverbal agreement from other participants (e.g., uniform head nodding, “uh huh” or “that's right” from other members). The authors introduced themselves to the patients at the beginning of the focus group but served in an observer role unless a patient asked a direct question to them, which happened rarely. This was done so that the authors had limited influence on the conversation. Upon completion, participants were compensated with a $100 gift certificate for their time, possible lost wages, and any travel and/or parking costs.
Data Analysis
We used a focused coding approach to determine the themes expressed by participants and develop a concept map, which became the framework for both our teaching tool and empathy training course.17 The focus group sessions were transcribed verbatim and independently reviewed by three investigators to identify major themes and subthemes for creation of a codebook (see Data Supplement S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10328/full). The authors then used the codebook to code passages from the transcripts for the focus groups. Authors also used this opportunity to connect the on‐site emotional strength of each passage as documented in their real‐time field notes. Randomly selected portions of the transcripts were coded by two authors to verify agreement. Verbatim phrases were tabulated under each theme and subtheme. Patient race strongly affects trust in medical systems, which may in turn affect perception of provider empathy; therefore, we included race of the speaker with excerpted phrases from focus group participants.
Initial thematic analysis of the qualitative data was conducted utilizing the constant comparative method.18, 19 Researchers applied codes representing the sentiment of each paragraph or data cluster and/or developed codes identifying patterns within the data themes.20, 21 The authors also reviewed field notes individually and then together to generate consensus interpretations of strong and consistent observations.
Consolidation of Themes Into a Concept Map
After the initial focus group, authors used field notes, the preliminary codebook, and coding of the transcript to develop an initial concept map. Near the end of the following two focus groups, participants were shown a preliminary, unpublished draft of the concept map and asked to provide opinions, either verbally or by writing on paper copies. Participants were encouraged to provide opinions on words, actions, and content of the figure including its overall appearance and visual organization.
Results
Transcript coding and thematic analysis revealed five major themes (provider transparency, patient's emotional state, provider disposition, trust in physician, and listening to patient) and 10 minor themes (Table 3). Each of these themes are described below and ordered by frequency.
Table 3.
Results of Transcript Coding: Focus Group Themes, Definitions, and Frequency
| Rank | Coded Theme | Description | Frequency |
|---|---|---|---|
| 1 |
TRAa
Transparency |
The extent to which the physician describes each step of the interaction/visit or helps a patient understand their disease process or situation | 15.3% |
| 2 |
DISa
Disposition |
How the physician presents him or herself | 12% |
| 3 |
TRUa
Trust |
Refers to patients having or developing trust in their physician | 10.7% |
| 4 |
EMOa
Emotion: fear/anxiety |
Emotional state of the patient, specifically those emotions of fear or anxiety | 10.7% |
| 5 |
NVC Nonverbal communication |
Describes all aspects of nonverbal communication | 8% |
| 6 |
SPI Spirituality |
Patient reference to their spirituality or whether spirituality should be addressed | 8% |
| 7 |
EXP Understanding patient expectations |
Issues that refer to physician or ED as a whole not meeting expectations that a patient had going in to the ED visit | 7.7% |
| 8 |
ENV Environmental issues |
Patient perception of the physical space and their surroundings in the hospital/ED | 7% |
| 9 |
COM Communication with healthcare team |
Alignment of physicians, nurses, techs, etc., in terms of words and instructions Also refers to the way a physician talks to the rest of the team |
5% |
| 10 |
LISa
Listen |
Refers to the physician listening and paying attention to the patient and his/her needs | 4.6% |
| 11 |
HD Disparities |
Any issue, story, example, concern that involves disparity in health care | 3.3% |
| 12 |
HIS History |
Physician knowledge of the patient's medical history | 2.7% |
| 13 |
INV Involve |
Soliciting involvement of others in the patient's health care—family in the room, health care providers in follow‐up. This also refers to treating the patient as a teammate in their own health care |
2% |
| 14 |
SPE Speech |
Physician speech volume, pattern, or tone | 1.7% |
| 15 |
WHO Whole person |
Treating the patient as a whole person and not a disease process | 1.7% |
Selected as a major theme.
Although we considered the frequency and duration of topic discussion as highly important, we used other factors observed in real time to make inclusions for Table 3. For example, our last major theme was not one of the most frequently discussed themes; however, the authors agreed that when it was discussed among the group it was very impactful and felt that it needed to be a major theme.
Provider Transparency
Transparency, defined as an open explanation of each step by the emergency physician, was the most common theme, present in 15% of coded phrases. Participants expressed the desire to hear physicians explain their thought processes behind testing, or not testing, and the plan of care for the visit. In addition, patients stated the desire for education to better understand their disease process or situation.
Participants stated strongly the desire for physicians to communicate with them as if they were a family member by using easily understandable language rather than medical jargon. As one black male participant explained, “Just talk to us cause we just like family. That's what they let me know, you know. And I appreciate that cause it made me kind of like communicate better with them.”
Participants felt that having a physician who walked them through his/her thought process was helpful. Individuals shared that it was important to have the ability to align understanding as exemplified by the following passage from a white female participant:
I think if he shares what he's thinking, that puts us more in tune so he can treat me better. Because if he's over here and I'm over here and we're never connecting, then how is he ever going to find out exactly what's going on with … he knows … with the symptom, where he can understand the symptoms and he can understand my level of pain or whatever I'm going through at that moment. We have to be on the same page, basically.
Patients consistently expressed a clear desire to be involved in deciding testing or treatment options. This desire for shared governance is illustrated by the following excerpt from a white female:
I think they should sit down and give you all the options, cause … I mean, you don't have to … there's several things that would run through their mind that they could do to test for this, and to sit down instead of just throwing you through the ringer of everything—to be like this is what your options are.
Participants expressed dissatisfaction when the provider was not transparent and when they felt like they were alienated until they were able to see the information in writing on the discharge paperwork.
When you get the discharge paperwork is when you finally see everything in print what they've done and what the results were. So I guess while you're in the ER, while all this is going on, something where I can see and go back to it and understand what's happening, why is this happening, and what is gonna come from it. Cause you really don't see that until you get discharged. (Black male)
Patient's Emotional State
Participants believed that empathy could not be achieved unless physicians had concern for their patients’ emotional state. The most common emotions experienced and discussed repeatedly were fear and anxiety, present in approximately 10% of coded phrases. According to field notes taken by providers present during the focus groups, this was one of the more powerful messages. One black female participant stated, “We wait until we are almost dead to go to the emergency room.”
Participants recognized that the provider's perception is often that the patient is healthy, but that perception discounts the fear that patients have at the time of their visit. As an example, one black female participant explains her fear during one of her visits when she took her blood pressure at home and it was elevated:
You guys got to figure out what's wrong with me because I'm scared. I'm really scared.
Participants indicated that anxiety escalates with the perception of abandonment, as stated by a white female:
It makes people anxious to think they are forgotten.
Participants indicated the need for cognitive reassurance (providing facts and thought processes with transparency) to alleviate fear:22
The lack of knowledge is the scariest thing when you have pain in your body. The way that they were there with me. The way that they talked to me and everything. It just put me at ease. I was not as scared. (White female)
Having answers puts you at ease. It puts your mind to ease, you know. (Hispanic female)
Provider Disposition
One participant offered the simple but strong recommendation that emergency physicians should “Come in warm.” Provider disposition was a theme in 10% of coded transcripts and underscored the importance of nonverbal and verbal greetings to set the tone for the entire encounter. Example behaviors to “Come in warm” include smiling, shaking hands and making eye contact. The location of the physician in the room (sitting or standing, at the bedside or behind a computer) while interacting with patients is also important. One white female stated, “Um, eye contact for me. You know, making eye contact for me and just kind of like, instead of just standing over me, maybe sit down maybe instead of just standing there. Being more, you know, at my level instead of just lording over me is how I feel like.” Another white female participant reiterated the importance of this by sharing, “I mean, if a doctor was to come to sit next to me and actually talk to me with eye contact, it would make a world of difference than just standing behind a computer and talking to me from across the room.”
Several participants shared how they appreciated when the physician was light‐hearted and approachable. A black female participant shared the example of telling a joke, “I like when they come in, they crack a joke even though it ain't funny, and they try to make you laugh a little bit, try to ease you a little bit more. They … I like … that's a plus for me.”
Trust in Physician
Participants shared the sentiment that they tended to trust physicians more when they felt that their opinions and information were valued. One white female shared, “If, uh, the doctor is talking over you instead of talking to you or not listening to what I'm actually saying, which is like just talking telling me what he's gonna do and not listening to what I'm saying, it's one of the things that would make me feel like there's distrust.”
Participants explained that trust was eroded if physicians appeared to be using scripts, memorized words, or other behavior that belied authenticity. A black male participant described this the following way, “And you can tell the difference when someone's trying to make the effort and trying to understand versus them just doing it for the show.” Participants shared that they would be more willing to trust a doctor who admitted to uncertainty and expressed desire for a second opinion from a specialist.
I actually think, um, if a doctor was to come to me and say, ‘I'm actually not 100% sure what's wrong with you. I think you should see this person and this person.’ or whatever—refer you to other doctors—it gives me more trust in them than them trying to fake that they know what I know. (white female)
Listening to Patient
Listening encompassed multiple themes but can be summarized as the capacity of physicians to make patients feel that their voice is heard. The simple concept of listening appeared to be another absolute prerequisite to the perception of empathy.
If they haven't walked in your shoes, they don't know what you're going through, so therefore don't act like a know‐it‐all. Instead, trying to sympathize and actually listen to you, and try to understand even though … instead of being like, ‘Oh, I've seen this before. Here's what we're gonna do. Bye.’ Instead actually have that communication and understanding or trying to understand. (white female)
The theme of listening was most strongly stated by participants who had or were caretakers of family members with chronic conditions. These participants pointed out that they believed they often have valuable information that is often ignored by physicians.
Honestly, every time I go to the ER, I say, ‘Look, I'm a special case. Ya'll gonna want to think this way.’ And I tell them. I swear, ya'll. I tell them this. Ya'll gonna think this way. Please, just listen. Just listen. And they do their own thing. Then two days later, I'm back up in there. Every single time. So I'm waiting to meet that one doctor who's actually gonna listen. (black male)
Another black female participant stated, “When we come in and we tell them what's wrong and we've already been through this so many times, and then they ignore the fact that we already told them that, it … it does happen quite a few times with me.”
Construction of the Concept Map
To create the first draft of the concept map, the authors consolidated what they had learned from the multicenter survey and the focus groups to create 8 to 10 nodes represented by visual icons and words. The icons were sequenced to temporally match the typical ED visit. The authors employed a physician with artistic ability (LKS) to draw a rough draft and then paid a professional medical illustrator to create Figure 1. The first derivation of the concept map and initial empathy teaching tool is shown. This concept map thus incorporates initial content from Lin et al.,11 together with semantics and behaviors exemplifying themes with high frequency and emotional response from the present work. One patient participant specifically suggested the concepts be organized as a circle rather than a line and noted “Y'all can call it the empathy circle.” The sequence is meant to reflect the usual temporal set of events during an ED visit, as opposed to an order of importance. The intent of the figure is to serve as a cognitive learning aid that illuminates components of the black box of empathy and to facilitate a didactic session to teach empathy to emergency care providers.
Figure 1.
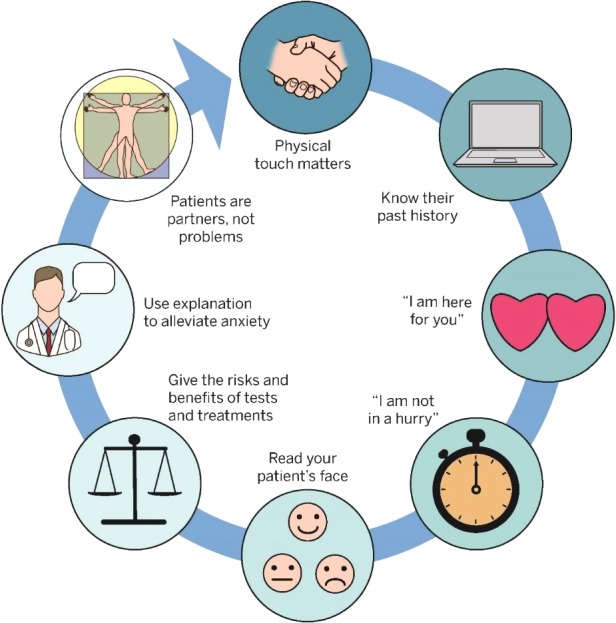
Empathy Circle: tool for teaching important aspects of empathy in emergency care.
Discussion
This work provides the first empirical basis for the creation of a patient‐informed concept map to teach empathy to emergency care providers. The rationale is clear because empathy benefits both patients and providers and has been tied to improved patient outcomes.3, 4, 23, 24 Unfortunately, allopathic and osteopathic medical school and residency training appears to reduce the capacity for empathy.25, 26 However, physician empathy can be enhanced through purposeful interventions.3, 24
This work addresses an unmet need in emergency care education and training. The unique challenges (patient volume and acuity, limited resources, and boarding, for example) of creating an empathic relationship in the ED setting and the lack of a published method to teach empathy to emergency care providers motivated this work. The themes in Table 3 together with the excerpts, the concept map, and precedent literature on teaching empathy in other settings allows the construction of an emergency care–specific training course for empathy. Since the physician–patient relationship is by definition dyadic, it was critical to obtain patient perspectives for the components of the concept map in Figure 1. Patient input on other measures of health care have been obtained successfully through methods of focus groups or structured interviewing.27
The Empathy Circle contains the important aspects of empathic care as described by the patients in our three focus groups. We included all of the main themes as well as some of the minor themes within the circle. The Empathy Circle allows the adoption of a personalized approach to each unique patient–provider encounter. Participants were clear that an insincere attempt to connect with patients or “scripting” would not be successful.
The Empathy Circle thus represents the framework for a didactic session to improve empathic care in the ED setting. Further research can determine the best way to teach these concepts to emergency care providers achieve better patient care by enhancing the patient–provider relationship, decreasing unnecessary testing and cost, and improving patient compliance and outcomes. The authors created a 3‐hour empathy training workshop using the Empathy Circle as a center point and are in the process of testing its effect on provider and patient perceptions of empathy in the ED setting.
Limitations
Limitations of this work include the fact that the Empathy Circle, representing the concept map for a cognitivist approach to teaching empathy, is not a one‐size‐fits‐all tool for patients or for providers. For example, the second step of the tool recommends that providers indicate that they have knowledge of the patient's prior medical conditions. In many encounters, emergency physicians do not have access to medical records. Additionally, our focus group was 78% female, which could limit applicability. The Empathy Circle and associated training can only give providers a cognitive framework to understand how to be empathic and cannot create caring providers. The Empathy Circle may not apply to patients with cognitive impairment, mental illness, or critical illness. We fully acknowledge that many factors affect empathy that may overwhelm training including personal stress, lack of sleep, burnout, overcrowding, and patient factors. The most important limitation is that the Empathy Circle has not yet been tested on learners and therefore both the Empathy Circle itself and the empathy training workshop may require refinement.
Conclusions
Thematic coding of transcripts from three focus groups representing geographic, ethnic and disease diversity revealed five major and 10 minor themes. These themes, together with field notes and information from a prior multicenter survey, allowed the construction of the Empathy Circle, a concept map and basis of a didactic to teach empathy to emergency care providers.
The authors would like to thank Dr. Lauren Stewart (LKS) for her illustration assistance in creating the empathy circle and Dr. Ashley Satorius for her assistance coding the focus group transcripts.
Supporting information
Data Supplement S1. Facilitator guide.
AEM Education and Training 2019;3:136–144
Supported by a Lilly Foundation Physician Scientist Initiative.
JAK reports grant money to Indiana University School of Medicine to conduct research conceived and written by JAK from Bristol Meyer Squibb and Janssen Pharmaceuticals. The other authors have no potential conflicts to disclose.
Author contributions: KEP—study concept and design, acquisition of data, analysis and interpretation of data, and drafting of the manuscript; NAR—acquisition of data, analysis and interpretation of data, and critical revision of the manuscript for important intellectual content; HW—acquisition of data and critical revision of the manuscript for important intellectual content; SS—acquisition of data, analysis and interpretation of data, and drafting of the manuscript; DMC—acquisition of data, analysis and interpretation of data, and critical revision of the manuscript for important intellectual content; AMM—critical revision of the manuscript for important intellectual content; and JAK—study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, and acquisition of funding.
References
- 1. Riess H. The science of empathy. J Patient Exp 2017;4:74–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Finset A, Ørnes K. Empathy in the clinician‐patient relationship: the role of reciprocal adjustments and processes of synchrony. J Patient Exp 2017;4:64–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Derksen F, Bensing J, Lagro‐Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract 2013;63:e76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Del Canale S, Louis DZ, Maio V, et al. The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med 2012;87:1243–9. [DOI] [PubMed] [Google Scholar]
- 5. Melnick ER, O'Brien EG, Kovalerchik O, Fleischman W, Venkatesh AK, Taylor RA. The association between physician empathy and variation in imaging use. Acad Emerg Med 2016;23:895–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang H, Kline JA, Jackson BE, et al. Association between emergency physician self‐reported empathy and patient satisfaction. PLoS One 2018;13:e0204113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith DD, Kellar J, Walters EL, Reibling ET, Phan T, Green SM. Does emergency physician empathy reduce thoughts of litigation? A randomised trial. Emerg Med J 2016;33:548–52. [DOI] [PubMed] [Google Scholar]
- 8. Riess H, Kraft‐Todd G. E.M.P.A.T.H.Y.: a tool to enhance nonverbal communication between clinicians and their patients. Acad Med 2014;89:1108–12. [DOI] [PubMed] [Google Scholar]
- 9. Wang H, Kline JA, Jackson BE, et al. The role of patient perception of crowding in the determination of real‐time patient satisfaction at emergency department. Int J Qual Health Care 2017;29:722–7. [DOI] [PubMed] [Google Scholar]
- 10. Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Mechanisms and outcomes. J Gen Intern Med 2006;21 Suppl 1:S28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lin MP, Probst MA, Puskarich MA, et al. Improving perceptions of empathy in patients undergoing low‐yield computerized tomographic imaging in the emergency department. Patient Educ Couns 2018;101:717–22. [DOI] [PubMed] [Google Scholar]
- 12. Torre DM, Daley BJ, Sebastian JL, Elnicki DM. Overview of current learning theories for medical educators. Am J Med 2006;119:903–7. [DOI] [PubMed] [Google Scholar]
- 13. Novak J, Gowin DB. Learning How to Learn. New York, NY: Cambridge University Press, 1984. [Google Scholar]
- 14. Guest G, Namey E, McKenna K. How many focus groups are enough? Building an evidence base for nonprobability sample size. Field Methods 2016;29:3–22. [Google Scholar]
- 15. Morgan DL, Morgan D. Focus Groups as Qualitative Research. Thousand Oaks, CA: Sage Publications, 1997. [Google Scholar]
- 16. Krueger RA. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications, 2014. [Google Scholar]
- 17. Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. London/Thousand Oaks, CA: SAGE Publications, 2006. [Google Scholar]
- 18. Glaser BG. The constant comparative method of qualitative analysis. Social Problems 1965;12:436–45. [Google Scholar]
- 19. Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park, CA: Sage Publications, 1985. [Google Scholar]
- 20. Creswell JW. Educational Research: Planning, Conducting, and Evaluating Quantitative and Qualitative Research. Upper Saddle River, NJ: Pearson/Merrill Prentice Hall, 2008. [Google Scholar]
- 21. Hill CE, Knox S, Thompson BJ, Williams EN, Hess SA, Ladany N. Consensual qualitative research: an update. J Couns Psychol 2005;52:196–205. [Google Scholar]
- 22. Pincus T, Holt N, Vogel S, et al. Cognitive and affective reassurance and patient outcomes in primary care: a systematic review. Pain 2013;154:2407–16. [DOI] [PubMed] [Google Scholar]
- 23. Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med 2011;86:359–64. [DOI] [PubMed] [Google Scholar]
- 24. Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ 2014;14:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McTighe AJ, DiTomasso RA, Felgoise S, Hojat M. Effect of medical education on empathy in osteopathic medical students. J Am Osteopath Assoc 2016;116:668–74. [DOI] [PubMed] [Google Scholar]
- 26. Neumann M, Edelhauser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med 2011;86:996–1009. [DOI] [PubMed] [Google Scholar]
- 27. Samuels‐Kalow ME, Rhodes KV, Henien M, et al. Development of a patient‐centered outcome measure for emergency department asthma patients. Acad Emerg Med 2017;24:511–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Facilitator guide.


