A 63-year-old woman with aggravating dyspnea was referred to our center. Her symptoms began three months ago and worsened throughout this period. She reported a history of breast cancer treated with mastectomy and chemoradiation therapy five years ago, with no recurrence noted in her subsequent follow-ups. She had also suffered from an episode of pulmonary emboli at the start of her chemotherapy. Echocardiography revealed moderate right ventricular dysfunction and an elevated systolic pulmonary artery of 85 mm Hg as well as multiple perfusion defects in the ventilation-perfusion (V/Q) scan (Fig. 1a). Hence, the patient was referred to our center for further evaluation of chronic thromboembolic pulmonary hypertension (CTEPH). Pulmonary CT angiography (CTA) revealed extensive mediastinal and bihilar fibrotic changes, which diffusely encroached pulmonary vasculature (Fig. 1b-e). Of note, co-existing small, pulmonary emboli were detected in few segmental arterial branches Figure 1b; these account for the perfusion defect noted in the initial V/Q scan.
Figure 1.
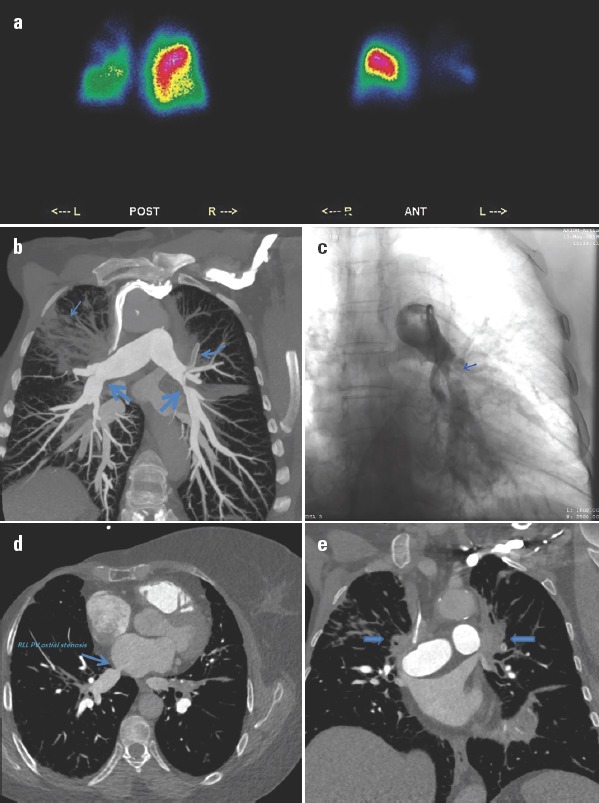
(a) Diffusely decreased radiotracer uptake in the left lung along with multiple wedge-shaped pleural-based segmental pulmonary perfusion defects in both lungs. Planar images from different angles (POST, posterior; ANT, anterior) (b) Oblique coronal reconstructed view of CT pulmonary angiography (CTPA). Remarkable post-radiation right upper lobe pulmonary fibrosis (thin arrow) accompanied by extensive mediastinal and bihilar fibrotic changes. Significant ostial stenosis of bilateral lower lobar arteries (thick arrows) as well as thromboemboli in left upper lobe segmental arterial branch (curved arrow). Complete occlusion of the right upper lobar arterial branch was noted. (c) Anterior–posterior view of pulmonary angiography. Significant ostial stenosis of the left lower lobe artery depicted in b (d) Oblique coronal reconstructed view of CTPA. Right side mastectomy and significant ostial stenosis of the right lower lobe pulmonary vein (RLL PV) (e) Coronal view of CTPA. Extensive bihilar post-radiation fibrosis with bilateral upper pulmonary vein occlusion (arrows)
Although fibrosing mediastinitis is primarily caused by granulomatous infections, it might be rarely observed in patients with a history of radiotherapy (1). Diffusely decreased radiotracer uptake accompanied with perfusion defects in the V/Q scan might be inspected in both fibrosing mediastinitis and CTEPH. However, despite broad mediastinal and bilateral hilar fibrosis, almost normal peripheral branch arborization in CTA is more favorable for fibrosing mediastinitis than CTEPH. This discrimination plays a crucial role in patient management and future prognosis.
References
- 1.Morrone N, Gama e Silva Volpe VL, Dourado AM, Mitre F, Coletta EN. Bilateral pleural effusion due to mediastinal fibrosis induced by radiotherapy. Chest. 1993;104:1276–8. doi: 10.1378/chest.104.4.1276. [DOI] [PubMed] [Google Scholar]


