Abstract
Objectives
Approximately 45% of youth presenting to the emergency department (ED) for mental health (MH) concerns will have a repeat ED visit. Since youth greatly depend on their caregivers to access MH services, the objective of this study was to determine if family characteristics were associated with repeat ED visits.
Methods
A retrospective cohort study of youth aged 6–18 years (62% female) treated at a tertiary pediatric ED for a discharge diagnosis related to MH was conducted. Data were gathered from medical records, telephone interviews, and questionnaires. Family factor contribution was analyzed using a multivariable logistic regression model controlling for demographic, clinical and service utilization factors. Variables associated with earlier and more frequent visits were determined using cox regression and negative binomial regression.
Results
Of 266 participants, 70 (26%) had a repeat visit. While caregiver history of MH treatment decreased the odds of having a repeat ED visit, family functioning and perceived family burden were not associated with repeat visits. Post-visit MH services, prior psychiatric hospitalization, higher severity of symptoms, and living closer to the hospital increased the odds of repeat visits.
Conclusions
This study examined the contribution of multiple family factors in predicting repeat MH visits to the ED. Results suggest caregiver characteristics may impact the decision to return. Healthcare providers should therefore consider caregiver and youth service utilization factors to inform patient management and discharge planning.
Keywords: mental health, emergency department, repeat visits
Résumé
Objectifs
Environ 45 % des adolescents qui se présentent au service d’urgence (SU) pour des raisons de santé mentale (SM) auront une visite répétée au SU. Puisque les adolescents dépendent beaucoup de leurs aidants pour avoir accès aux services de SM, l’objectif de cette étude était de déterminer si les caractéristiques familiales étaient associées aux visites répétées au SU.
Méthodes
Une étude de cohorte rétrospective a été menée sur des adolescents de 6 à 18 ans (62 % de sexe féminin) traités dans un SU pédiatrique tertiaire pour un diagnostic lié à la SM posé au moment du congé. Les données ont été recueillies d’après les dossiers médicaux, les entrevues téléphoniques et les questionnaires. La contribution des facteurs familiaux a été analysée à l’aide d’un modèle de régression logistique multivariable après contrôle des facteurs démographiques, cliniques et d’utilisation des services. Les variables associées à des visites précédentes et plus fréquentes ont été déterminées à l’aide de la régression de Cox et la régression binomiale négative.
Résultats
Sur les 266 participants, 70 (26 %) avaient une visite répétée. Les antécédents de traitement de SM des aidants diminuaient les probabilités d’avoir une visite répétée au SU, et le fonctionnement familial et le fardeau familial perçu n’étaient pas associés à des visites répétées. Les services de SM ultérieurs à la visite, une hospitalisation psychiatrique précédente, une gravité plus élevée des symptômes et le fait d’habiter à proximité de l’hôpital augmentaient les probabilités de visites répétées.
Conclusions
Cette étude a examiné la contribution de multiples facteurs familiaux à la prédiction de visites répétées au SU pour raisons de SM. Les résultats suggèrent que les caractéristiques des aidants puissent influer sur la décision de retourner au SU. Les prestataires de soins de santé devraient donc prendre en compte les facteurs d’utilisation des services des aidants et des adolescents afin d’éclairer la prise en charge des patients et la planification du congé.
Mots clés: santé mentale, service d’urgence, visites répétées
Pediatric emergency departments (EDs) play a critical role in the care of youth with mental health (MH) concerns. The top three reasons given by caregivers and youth for visiting the ED are: suicidal thoughts, depression/mood, and suicide attempt (Cloutier, Kennedy, Maysenhoelder, Glennie, Cappelli, & Gray, 2010). Although only 4–7% of hospital emergency visits pertain to MH issues, up to 45% of youth MH presentations are repeat visits (Cloutier et al., 2017; Mapelli, Black, & Doan, 2015; Newton et al., 2009). Of the children and adolescents who are repeat visitors, 50% come back to the ED within one month (Christodulu, Lichenstein, Weist, Shafer, & Simone, 2002; Goldstein, Frosch, Davarya, & Leaf, 2007; Peterson, Zhang, Santa Lucia, King, & Lewis, 1996; Tossone, Jefferis, Bhatta, Bilge-Johnson, & Seifert, 2014) and 65–85% come back within six months (Newton et al., 2010; Peterson et al., 1996). Return visits for MH concerns contribute to ED overcrowding (Dolan & Fein, 2011), require additional resources (Chun, Katz, Duffy, & Gerson, 2015), and might not be for emergent concerns (Mapelli et al., 2015).
Unlike adults, youth depend on their caregivers to access MH services as they are usually central to the process of seeking and securing MH care (Logan & King, 2001). Family factors associated with health and MH service access and utilization include: family functioning, caregiver burden/strain, parental coping styles, maternal depression and family conflict (Angold et al., 1998; Blader, 2004; Brannan, Heflinger, & Foster, 2003; Fite, Stoppelbein, & Greening, 2009; Fontanella, 2008). However, our systematic review demonstrates that literature on pediatric repeat MH ED visits primarily focuses on demographic, clinical and service utilization characteristics (Leon et al., 2017). Our understanding of the impact of family factors on ED use for MH concerns is limited. Only one study has investigated a family factor, prior caregiver experience seeking MH care for their child, and found it was significantly associated with repeated ED visits (Sobolewski, Richey, Kowatch, & Grupp-Phelan, 2013). Considering that 56–62% of youth are accompanied by a caregiver when presenting to the ED (Cloutier et al., 2010; Grupp-Phelan et al., 2009), focusing on youth characteristics alone does not take into account the influence of caregivers (Logan & King, 2001). Such findings could be used to help reduce repeat MH visits to the ED.
The primary objective of this study is to determine whether family factors are independently associated with repeat MH ED visits after controlling for demographic, clinical and service utilization factors. We hypothesize that poorer family functioning, greater perceived MH burden on the family, and caregiver history of MH treatment are associated with an increased risk of having a repeat MH ED visit. Secondary objectives are to determine which factors are associated with earlier and more frequent ED visits. We hypothesize that demographic (age, biological sex, child welfare involvement), clinical (clinical severity, psychotic, mood, and anxiety disorders), service utilization (post-index visit MH service utilization, living closer to the hospital) and the above family factors contribute to earlier and more frequent MH ED visits.
Methods
Design
This study used a retrospective cohort design to investigate risk factors for repeat MH ED visits. Through medical record review, we identified all youth who presented to the Children’s Hospital of Eastern Ontario’s (CHEO) ED with MH complaints from April 2014 to April 2015. The first ED visit made by a youth within this period was labeled “index visit” and any additional visit occurring within six months of the index visit was considered a “repeat visit”. A six-month repeat window was chosen, because 85% of MH repeat visits occur within six months of the index ED visit (Newton et al., 2010; Peterson et al., 1996).
Participants
Study eligibility was assessed based on age and primary discharge diagnosis. Participants aged 6–18 years who had a visit with the following ICD-10-CM diagnosis codes related to mental and behavioural disorders were eligible: psychoactive substance use (F10–19), schizophrenia and delusional (F20–29); mood and affective (F30–39); neurotic, stress-related and somatoform (F40–45, 48); syndromes associated with physiological and physical factors (F50–55, 59); other disorders with onset usually occurring in childhood and adolescence (F91–94, 98, 99); intentional self-harm (X71–82) and codes related to non-specific mental health symptoms (R45–46). Those with a neurodevelopmental diagnosis code (F84, F90) and who had a MH chief complaint were also eligible. Youth were excluded if: (a) they had a MH diagnosis but sought ED services for medical reasons (e.g., fever); (b) they presented with an unclear ED visit (e.g., secondary non-MH medical diagnosis, diagnosis containing “possible” or “query”) that occurred after February 2015; (c) they needed inpatient hospitalization for their MH condition since the needs and experiences of patients discharged from inpatient units might differ and have been investigated elsewhere (Blader, 2004; Fontanella, 2008); (d) they visited the ED six months prior to their index visit; (e) they lived outside of the province of Ontario; and (f) the primary respondent was not English- or French-speaking. Adolescents aged 14 and above were given the opportunity to participate alone if they wished; therefore primary respondents were either caregivers (biological or adoptive parent, step-parent or grandparent) or the adolescent themselves.
Data Collection
Six months following their index visit, eligible youth and their caregivers were asked to provide consent to be contacted for research by ED volunteers. Those who consented were contacted by researchers and were given the opportunity to provide informed consent for participation in this study. Youth who revisited the ED within six months following the index visit were labeled “repeaters”; those who did not were labeled “non-repeaters” (Leon et al., 2017). Data were collected from medical record review, telephone interview, and questionnaires six to twelve months post-index ED visit. The questionnaire package was offered through a secure web-based tool (Research Electronic Data Capture; REDCap; Harris et al., 2009) or sent by mail with a pre-paid return envelope, depending on participant preference. All interviews and measures were in the participants’ preferred language (English or French).
Variables and measures
Dependent variables
The three study outcomes were extracted from youth’s medical records. Repeat visit is a dichotomous variable, frequent repeat visits is measured as the number of repeat visits within six months, and earlier repeat visits is measured as the number of days between the index and the first repeat visit.
Independent variables
Family factors
Family functioning was measured by the Family Assessment Measures (FAM-III) general scale, a 50-item self-report questionnaire which was part of the questionnaire package (Skinner, Steinhauer, & Sitarenios, 2000). The FAM-III’s general scale has high internal consistency (α = 0.93) and acceptable test-retest reliability (r = 0.57–0.66; Skinner et al., 2000). The burden of MH concerns on family, as perceived by the respondent, was measured by a single 4 point Likert item on the Impact Supplement of the SDQ. This item has adequate test-retest reliability (ICC = 0.44) and correlation with a standardized interview rating of burden (r = 0.74; Goodman, 1999). To determine history of caregiver MH treatment, the respondent was asked during the telephone interview whether any caregiver had ever received counselling/therapy or been prescribed medication for emotional or behavioural difficulties (excluding couples therapy and family therapy aimed at addressing their child’s MH issues).
Demographic factors
Youth age, biological sex, neurodevelopmental co-morbidity (presence of ADHD, Autism disorder, Tourette syndrome, pervasive developmental disorder, etc.), and child welfare agency involvement were extracted from medical records, while caregiver education was captured during the telephone interview. Statistics Canada (2015) collects median family incomes for Canadian postal codes. Family income (in Canadian dollars) of each participating family was estimated by looking up the corresponding median family income participant postal code.
Service utilization factors
Length of stay (LOS) in the ED was extracted from the medical record and dichotomized using CHEO’s 5.5 hour benchmark for urgent ED presentations. Estimated distance from hospital (in kilometers; kms) was determined based on postal codes. Due to its highly skewed distribution, distance from the hospital was dichotomized using one standard deviation (40.87 kms) from the mean (36.01 kms) as the cut-off (i.e., approximately 77 kms). Satisfaction with care during the index visit was elicited over the telephone and measured by the 8-item self-report Client Satisfaction Questionnaire (CSQ-8; Attkinson & Greenfield, 2004). The CSQ-8 has good internal consistency (α = 0.83–0.93) and is correlated with other symptom checklists measures (Attkisson & Zwick, 1982; LeVois, Nguyen, & Attkisson, 1981). Prior psychiatric hospitalization and post-index visit MH service utilization was queried over the telephone and measured using questions from The Services for Children and Adolescents - Parent Interview (SCA-PI), an interview designed to assess caregiver’s reports of youth’s MH services received across multiple settings (Jensen et al., 2004). The SCA-PI has good test-retest reliability (k = 0.97; Hoagwood et al., 2004) and concordance with medical records (Ford, Hamilton, Dosani, Burke, & Goodman, 2007).
Clinical factors
Diagnosis (ICD-10-CM code) and presence of suicidality at the index visit were extracted from medical records. Symptom severity was captured by the total score on the HEADS-ED; a 7-item MH screening tool completed by ED providers at the time of the visit (Cappelli et al., 2012; 2017). HEADS-ED forms were available for 55% of participants. Missing forms were completed by a trained rater blinded to study hypotheses using physician/crisis worker notes present in the youth’s medical record. A second rater also completed 53% of the HEADS-EDs in this sample. Interrater reliability was assessed by intraclass correlation coefficient (ICC) to determine the degree of coder consistency (Hallgren, 2012; Koo & Li, 2016). The resulting ICCs (M = 0.71) indicated an acceptable degree of agreement and similar interrater reliability as previously reported for this measure (Cappelli et al., 2012). Perceived severity was measured by the Strengths and Difficulties Questionnaire (SDQ)’s total scale, a 25-item screening questionnaire of youth behaviour, which was part of the questionnaire package (Goodman, 1997). The SDQ has good internal consistency (α = 0.73), cross-informant correlation (r = 0.34) and test-retest reliability (r = 0.62; Goodman, 2001).
Setting
CHEO is a pediatric tertiary care teaching hospital affiliated with the University of Ottawa. It serves the city of Ottawa as well as other regions of Eastern Ontario. The hospital’s ED has an annual volume of approximately 70,000 patient visits for those under 18 years-old, 4.5% of which are MH visits. The crisis intervention program, located within the ED, responds to MH emergencies daily between 7:30 A.M. and 11:00 P.M. Outside these hours and during peak times, emergency physicians assess and treat patients with MH complaints. Residents and emergency physicians are typically first to assess patients with a MH complaint combined with an accompanying medical concern (e.g., drug ingestion), psychosis, or with an application for psychiatric assessment. Emergency physicians can request a consultation from an on-call pediatric psychiatrist.
Data Analysis
The data were analyzed using IBM SPSS v.25.0.0.0 (IBM SPSS, 2017). A minimum sample size of 210 was calculated a priori in order to attain adequate statistical power for the planned analyses with 21 variables. Attrition at the questionnaire package portion of the study (38%) resulted in having to use Markov Chain Monte Carlo Multiple Imputation (MI) to retain all 266 participants in the adjusted regression analyses (Rezvan, Lee, & Simpson, 2015). All variables were included in the imputation model. Pooled estimates from 50 imputed datasets are presented.
Univariate logistic regressions (unadjusted Odds Ratios, ORs; 95% confidence interval, CI) were conducted to determine which variables were independently associated with repeat visits. A hierarchical four-block multivariate logistic regression model (adjusted OR; aOR; 95%CI) was built based on theory and included the univariate logistic regression variables (Sperandei, 2014) to determine the unique contribution of family factors above all other variables. Demographic variables were entered in block 1, service utilization factors in block 2, clinical factors in block 3, and family factors in block 4. Using the same model building strategy, a multivariate cox regression (adjusted Hazard Ratios, aHRs; 95% CI) was used to determine variables associated with earlier repeat visits, while multivariate negative binomial regression (adjusted Relative Risk, aRRs; 95% CI) was used to determine variables associated with more frequent repeat ED visits. Pooled RR estimates were obtained using mice package v. 3.1.0 (Van Buuren and Groothuis- Oudshoorn, 2011) in R v. 3.5.1 (R Core Team, 2018). Pooled OR and HR estimates were provided by SPSS 25. Chi-square and independent samples t-tests were used to: compare repeaters to non-repeaters, determine study generalizability, and determine MI sensitivity.
Ethics
This study was approved by the CHEO’s Research Ethics Board (14/44X) and the University of Ottawa’s Research Ethics Board (A10-14-03) and all procedures contributing to this work comply with the ethical standards. In keeping with Canadian research ethics board principles and as recommended by CHEO’s research ethics board, ethnicity was not collected for this study.
Results
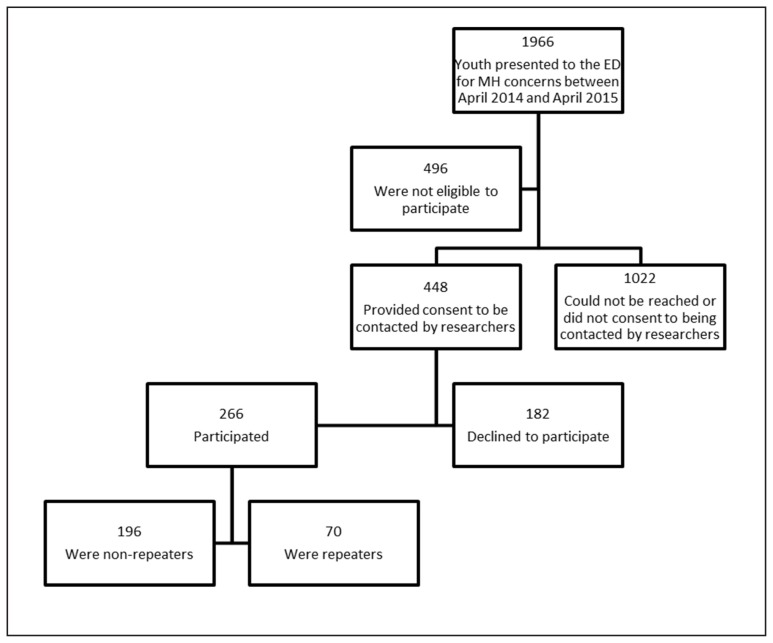
During the study period, 448 eligible patients consented to being contacted by study researchers. Of these, 266 (59.4%) participated, including 70 (26.3%) repeat visitors (see flowchart in Figure 1). Participating youth (M age=13.41; SD=2.72) were mostly female (62%) and had an estimated family income (M = $82,195; SD = $14,794) higher than the overall Canadian median ($67,044) (Statistics Canada, 2015). Primary respondents were mostly caregivers (81.5%) and participated in English (86.8%). At the index visit, 95.1% of youth were accompanied by a caregiver, 48.1% were taking psychotropic medication, 24.8% obtained a psychiatry consultation, and 50.4% were referred to the crisis intervention program. Demographic data and results from repeaters and non-repeaters group comparisons are reported in Table 1.
Figure 1.
Study Flow Chart
Table 1.
Descriptive and inferential statistics of repeaters vs. non-repeaters
| Total sample N = 266 |
Repeaters n = 70 |
Non-Repeaters n = 196 |
t-score/χ2 | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||
| Demographic Factors | |||||||
| Month of the index presentation, M (SD) | 6.66 | (4.10) | 6.84 | (3.97) | 6.59 | (4.15) | 0.44 |
| Age 1, M (SD) | 13.41 | (2.72) | 13.83 | (2.32) | 13.27 | (2.84) | 1.64 |
| Biological sex | |||||||
| Female, n (%) | 165 | (62.00) | 47 | (67.10) | 118 | (60.20) | 1.05 |
| Neurodevelopmental co-morbidity | |||||||
| Yes, n (%) | 76 | (28.60) | 22 | (31.40) | 54 | (27.60) | 0.38 |
| Average caregiver education | |||||||
| Below university level education, n (%) | 126 | (51.00) | 33 | (50.80) | 93 | (51.10) | 0.002 |
| Missing | 19 | (7.10) | 5 | (7.10) | 14 | (7.10) | |
| Estimated median family income, M (SD) | 82,195 | (14,794) | 84,072 | (12,691) | 81,525 | (15,451) | 1.24 |
| Involvement with a child welfare agency 2 | |||||||
| Involved, n (%) | 15 | (5.70) | 7 | (10.00) | 8 | (4.10) | 3.27 |
| Missing | 3 | (1.10) | 0 | (0) | 3 | (1.50) | |
| Service Utilization Factors | |||||||
| Estimated distance from the hospital 2 | |||||||
| Below 1 SD away from the mean (76.89 km), n (%) | 233 | (87.60) | 66 | (94.30) | 167 | (85.20) | 3.91* |
| Length of Stay in the ED | |||||||
| < 5.5h benchmark, n (%) | 220 | (90.90) | 55 | (84.60) | 165 | (93.20) | 4.26* |
| Missing | 24 | (9.00) | 5 | (7.10) | 19 | (9.70) | |
| Satisfaction with services (CSQ), M (SD) | 22.44 | (6.78) | 22.90 | (6.26) | 22.25 | (6.96) | 0.69 |
| Missing | 1 | (0.40) | 0 | (0) | 1 | (0.50) | |
| Prior psychiatric hospitalization | |||||||
| Yes, n (%) | 25 | (9.40) | 11 | (15.70) | 14 | (7.10) | 4.45* |
| Post-index visit MH service utilization | |||||||
| Yes, n (%) | 195 | (73.30) | 58 | (82.90) | 137 | (69.90) | 4.43* |
| Clinical Factors | |||||||
| Severity (HEADS-ED), M (SD) | 3.91 | (2.01) | 4.51 | (2.06) | 3.69 | (1.96) | 2.99* |
| Missing | 4 | (1.50) | 0 | (0) | 4 | (2.00) | |
| Perceived Severity (SDQ), M (SD) | 19.51 | (6.49) | 19.72 | (6.07) | 19.43 | (6.65) | 0.27 |
| Missing | 75 | (28.20) | 20 | (28.60) | 55 | (28.10) | |
| Diagnostic category, n (%) | |||||||
| Anxiety disorders | 141 | (53.00) | 38 | (54.30) | 103 | (52.60) | 0.06 |
| Mood disorders 2 | 52 | (19.50) | 14 | (20.00) | 38 | (19.40) | 0.01 |
| Behavioural disorders 2 | 29 | (10.90) | 9 | (12.90) | 20 | (10.20) | 0.37 |
| Substance disorders 2 | 9 | (3.40) | 2 | (2.90) | 7 | (3.60) | 0.81 |
| Eating disorders 2 | 3 | (1.10) | 0 | (0) | 3 | (1.50) | 1.08 |
| Psychotic disorders 2 | 4 | (1.50) | 1 | (1.40) | 3 | (1.50) | 0.004 |
| Other disorders 2 | 28 | (10.50) | 6 | (8.60) | 22 | (11.20) | 0.39 |
| Suicidality | |||||||
| Present, n (%) | 135 | (50.80) | 42 | (60.00) | 93 | (47.40) | 3.25 |
| Family Factors | |||||||
| Caregiver history of treatment for MH concerns | |||||||
| Present, n (%) | 175 | (68.40) | 36 | (52.20) | 139 | (74.30) | 11.44** |
| Missing | 10 | (3.80) | 1 | (1.40) | 9 | (4.60) | |
| Perceived burden 2 | |||||||
| Quite a lot – A great deal, n (%) | 132 | (73.10) | 37 | (75.50) | 95 | (71.40) | 0.30 |
| Missing | 84 | (31.60) | 21 | (30.00) | 63 | (32.10) | |
| Family functioning, M(SD) | 53.80 | (8.62) | 55.83 | (9.15) | 53.14 | (8.33) | 1.79 |
| Missing | 103 | (38.70) | 25 | (35.70) | 78 | (39.80) | |
Chi square tests were used to examine differences between frequencies (N)
Independent samples t-tests are reported for differences between means (M).
Missing N’s for each group are reported separately.
Significant at the 0.05 level;
significant at the 0.01 level
Equal variances not assumed below 5
Fisher’s Exact Test used to correct for small sample size
Questionnaire completers were compared to non-completers to determine if the low questionnaire completion/return rate (38%) impacted results. Those who completed questionnaires had significantly higher caregiver education (p=.035), higher estimated income (p=.001) and lived closer to the hospital (p=.018). Study participants were compared to those who were eligible but did not participate (unreachable or declined to participate) on available clinical and demographic characteristics (age, diagnosis, estimated income, and month of index presentation) to determine the representativeness of our sample. A significant greater proportion of families of children 6–12 years old (Mdn = 10, IQR = 9.0–11.5) participated than families of adolescents 13–18 years old (Mdn = 15, IQR = 14.0–16.0). Participants also presented with significantly more anxiety disorders [X2 (1, N=1876) = 5.53, p =.019] and behavioural disorders [X2 (1, N=1876) = 4.58, p =.032], but with significantly less substance disorders [X2 (1, N=1876) = 12.55, p =.000] than non-participants.
Both unadjusted and adjusted logistic regressions are reported in Table 2. Based on the unadjusted logistic regressions, only estimated income was not entered into the multivariate analyses as it was not at all associated with repeat visits (OR=1.00; 95%CI 1.00–1.00). Adjusted analyses indicated that having a parent with a history of treatment for MH concerns significantly predicted decreased odds of repeat visits, whereas family functioning and perceived burden were not significantly associated. Goodness-of-fit tests detected that family factors significantly added to the overall prediction of the model [X2 (df=20) = 50.78, p = 0.000]. Other variables were also found to be significant predictors: post-index visit MH service utilization, prior psychiatric hospitalization, higher severity of symptoms, and living closer to the hospital.
Table 2.
Predictors of repeat ED visits
| Unadjusted OR | 95% CI | Adjusted OR | 95% CI | |
|---|---|---|---|---|
| Demographic Factors | ||||
| Age | 1.083 | 0.974–1.204 | 1.054 | 0.912–1.217 |
| Female | 1.351 | 0.760–2.400 | 1.178 | 0.565–2.456 |
| Having a neurodevelopmental co-morbidity | 1.205 | 0.665–2.183 | 1.632 | 0.701–3.803 |
| Estimated median family income | 1.000 | 1.000–1.000 | ||
| Average caregiver education | 1.013a | 0.575–1.785 | 1.032 | 0.521–2.044 |
| Involvement with CAS | 2.569b | 0.896–7.371 | 3.216 | 0.891–11.602 |
| Service Utilization Factors | ||||
| Living closer to the hospital (below 1 SD) | 2.865 | 0.970–8.467 | 5.934* | 1.622–21.703 |
| LOS above recommended 5.5h benchmark | 2.500*c | 1.024–6.106 | 1.077 | 0.349–3.325 |
| Satisfaction (CSQ) | 1.015d | 0.974–1.057 | 1.021 | 0.969–1.076 |
| Post-index visit MH service utilization | 2.082* | 1.041–4.160 | 2.430* | 1.050–5.628 |
| Prior psychiatric hospitalization | 2.424* | 1.044–5.628 | 2.874* | 1.001–8.251 |
| Clinical Factors | ||||
| Having a mood-related ICD code at the index visit | 1.039 | 0.524–2.061 | 0.836 | 0.370–1.891 |
| Having a behaviour-related ICD code at the index visit | 1.298 | 0.561–3.004 | 1.511 | 0.481–4.745 |
| Having a psychosis-related ICD code at the index visit | 0.932 | 0.095–9.114 | 2.891 | 0.227–36.863 |
| Suicidality | 1.661 | 0.954–2.892 | 1.461 | 0.720–2.964 |
| Severity (HEADS-ED) | 1.223*e | 1.067–1.402 | 1.287* | 1.082–1.531 |
| Perceived Severity (SDQ) | 1.007f | 0.958–1.058 | 0.979 | 0.912–1.050 |
| Family Factors | ||||
| Caregiver history of treatment for MH concerns | 0.377*g | 0.212–0.670 | 0.272* | 0.138–0.539 |
| Perceived Family Functioning (FAM) | 1.038h | 0.996–1.083 | 1.024 | 0.975–1.076 |
| High level of perceived burden | 1.233i | 0.581–2.616 | 1.164 | 0.485–2.797 |
N Adjusted = 266 non repeaters (79.2%) and 70 repeaters (20.8%)
N unadjusted = 266 non repeaters (70 repeaters) unless otherwise specified.
247(65);
263(70);
242(65);
265(70);
262(70);
191(50);
256(69);
163(45);
182(49)
Nearly half of repeaters (47%) revisited the ED within 30 days of the index visit and 75% revisited within three months. Number of repeat visits ranged from 1 to 11. Variables associated with earlier and more frequent repeat visits are reported in Table 3. Results showed that having a parent with a history of treatment for MH was significantly associated with a reduced risk of earlier and more frequent repeat visits, while family functioning and perceived burden was not. Post-index visit MH service utilization and more severe MH symptoms predicted both more frequent and earlier repeat ED visits, while living closer to the hospital, having a past psychiatric hospitalization, and presence of suicidality only predicted more frequent repeat visits and longer ED stay only predicted earlier repeat visits.
Table 3.
Predictors of Recency and Frequency of Repeat ED Visits
| Recency of repeat visits N=266 | Frequency of repeat visits N=266 | |||
|---|---|---|---|---|
|
|
|
|||
| Adjusted HR | 95% CI | Adjusted RR | 95% CI | |
| Demographic Factors | ||||
| Age | 1.070 | 0.948 – 1.209 | 1.050 | 0.937 – 1.176 |
| Female | 1.142 | 0.626 – 2.081 | 0.956 | 0.537 – 1.703 |
| Having a neurodevelopmental co-morbidity | 1.352 | 0.692 – 2.643 | 1.091 | 0.550 – 2.167 |
| Average caregiver education | 1.046 | 0.611 – 1.792 | 1.010 | 0.583 – 1.748 |
| Involvement with CAS | 2.125 | 0.780 – 5.789 | 2.545 | 0.969 – 6.681 |
| Service Utilization Factors | ||||
| Living closer to the hospital (below 1 SD) | 4.585 * | 1.493 – 14.081 | 5.996 * | 1.913 – 18.789 |
| LOS above recommended 5.5h benchmark | 0.981 | 0.426 – 2.255 | 0.905 | 0.394 – 2.076 |
| Satisfaction (CSQ) | 1.025 | 0.982 – 1.069 | 1.000 | 0.960 – 1.040 |
| Post-index visit MH service utilization | 2.265 * | 1.124 – 4.563 | 2.072 * | 1.058 – 4.060 |
| Prior psychiatric hospitalization | 1.818 | 0.818 – 4.563 | 2.341 * | 1.029 – 5.329 |
| Clinical Factors | ||||
| Having a mood-related ICD code at the index visit | 0.951 | 0.501 – 1.805 | 0.620 | 0.314 – 1.222 |
| Having a behaviour-related ICD code at the index visit | 2.395 | 0.277 – 20.670 | 1.270 | 0.519 – 3.104 |
| Having a psychosis-related ICD code at the index visit | 1.927 | 0.766 – 4.847 | 1.408 | 0.134 – 14.731 |
| Suicidality | 1.377 | 0.787 – 2.409 | 1.971 * | 1.129 – 3.442 |
| Severity (HEADS-ED) | 1.213 * | 1.066 – 1.381 | 1.155 * | 1.013 – 1.317 |
| Perceived Severity (SDQ) | 0.976 | 0.923 – 1.030 | 0.972 | 0.914 – 1.032 |
| Family Factors | ||||
| Caregiver history of treatment for MH concerns | 0.362 * | 0.216 – 0.605 | 0.337 * | 0.204 – 0.560 |
| Perceived Family Functioning (FAM) | 1.034 | 0.994 – 1.076 | 1.027 | 0.984 – 1.032 |
| High level of perceived burden | 1.333 | 0.640 – 2.777 | 1.686 | 0.771 – 3.686 |
Discussion
The high volume of pediatric MH repeat visits to the ED contributes to ED overcrowding and may reveal unmet clinical needs in some patients. The role of caregiver’s has been largely neglected within this context. In this study, one of the three family factors investigated the caregiver’s history of MH treatment― was found to be significantly associated with a reduced risk of their child having a repeat visit, earlier and more frequent repeat visits. The other two family factors, family functioning and perceived family burden, were not.
While our study examines prior caregiver experience of seeking MH care for themselves, one other study has investigated prior caregiver experience of seeking MH care for their child and found this family factor to increase the odds of repeated ED visits (Sobolewski et al., 2013). These findings may therefore suggest that experiences with pediatric vs. adult MH services have a differential impact on pediatric MH return visits. Although the relationship between these two variables was not measured, it is possible that the family variable described in the Sobolewski et al. (2013) study might be capturing families who are familiar with seeking MH services within the pediatric system (and therefore possibly heavy users). In this study, while in this study caregivers who are familiar with the adult MH system from their own past experiences may be less likely to bring their child back to the ED repeatedly as they may face more obstacles in recognizing symptoms and accessing community MH resources for their child (Logan & King, 2001). Alternatively, these caregivers may be better advocates and navigators of community-based services in general, making them less likely to seek urgent services for their child. Current caregiver MH was also shown to impact seeking services for their child’s physical concerns as severity of maternal depression symptoms is significantly associated with perceived difficulty in taking care of their child, missed pediatric outpatient visits, adherence to medication management, and six-month ED use (Flynn, Davis, Marcus, Cunningham, & Blow, 2004; Grupp-Phelan, Whitaker, & Naish, 2003). Future research should explore whether caregiver type, gender, age, MH diagnosis, MH severity, and service utilization mediate the association between caregiver history of MH treatment and repeat ED visits.
Results from demographic factors are consistent with findings from a recent systematic review (Leon et al., 2017). For identified service utilization factors, we found that distance from hospital and receiving MH services were predictors of repeat ED visits as well as earlier and more frequent visits, while past psychiatric hospitalization was associated with repeat ED visits and more frequent visits, but not earlier visits. These results are also consistent with the systematic review which showed that living closer to the hospital, receipt of MH services, and past psychiatric hospitalization were common predictors across several studies (Leon et al., 2017). In terms of clinical factors, we also found severity of symptoms at the index visit to be an important predictor of repeated visits, repeating earlier and more frequently. However there are mixed findings in the past literature (Leon et al., 2017). For example, in repeat visits to the ED related to mood disorders, neurotic/stress related disorders, or psychotic- related illnesses, clinical acuity as measured by triage level did not appear to worsen between ED visits in one study (Yu, Rosychuk, & Newton, 2011). In this study, the HEADS-ED total score was used rather than triage level, since nearly all MH patients were triaged as urgent in our sample. While triage level is a single item indicator of clinical severity (i.e., how long a patient can safely wait before being seen), the HEADS-ED takes into consideration multiple indicators of MH functioning (e.g., home; education; activities and peers) which might better capture overall severity of MH symptoms. Suicidality at the index visit only predicted more frequent visits which may suggest that the ED is considered the first point of access when safety planning for youth with suicidal ideation. Professionals may tend to more readily direct youth to the ED for immediate monitoring and further assessment when suicidality is involved, but not necessarily for other MH concerns.
Strengths and Limitations
This study examines the contribution of multiple family factors in predicting repeated, earlier, and more frequent pediatric visits to the ED for MH reasons and used an integrated approach of medical records, clinician assessment, and self-reported data. This allowed for data corroboration, less reliance on potentially missing records, and a greater breadth of information on motivations behind return ED visits. However, there are also limitations to this method of data collection. First, we considered selection bias and determined that findings may not be generalizable to older adolescents or those with substance use disorders. Moreover, previous research has found that, at CHEO, approximately 15% of MH visits result in hospitalizations and that symptom severity (measured by the HEADS-ED) was not the only factor driving the decision to admit (Cappelli et al., 2017). Since those who were admitted at the index visit were excluded from this study, results are not applicable to a subgroup of youth who may have had higher severity and other relevant factors leading to hospitalization. Second, attrition was also an issue. We addressed this by using MI; which uses existing data to replace missing data with plausible values (Rezvan et al., 2015). Results from the FAM-III and the SDQ may therefore not be generalizable to lower income, lower educational achievement and more rural households. Third, family income was estimated based on postal code which might not have reflected the true variation in family incomes in this sample. Fourth, the finding that caregiver history of MH treatment is a significant predictor could be confounded by mediating variables, such as: parental MH diagnosis, MH severity, efficacy in navigating MH care system. Finally, as health care in Canada is publicly funded by province, findings might be less generalizable to other provinces and countries. Nevertheless, overall findings were in line with previous Canadian and American research on repeat visits and repeat psychiatric admissions (Leon et al., 2017).
Clinical and Research Implications
The finding that pediatric patients who are connected to MH services post-index visit, having had prior psychiatric hospitalization and higher severity of symptoms increase the risk of repeat ED visits indicates that these youths generally have higher needs and are experienced users of the MH system. Caregiver history of MH treatment was also predictive of reduced MH ED visits and may further suggest that families as a whole may have greater needs. Our data did not permit us to determine adherence/compliance, satisfaction, responsiveness, availability, and appropriateness of current or past MH services, which might help to better understand how families and youth move through the continuum of MH services.
During their assessment, ED providers might find it useful to determine if post-index visit MH services meet all patient MH needs as some might be facing more complex issues, difficulty meeting service eligibility criteria, or escalating environmental stressors. Using assessment tools within the ED, such as the HEADS-ED (Cappelli et al., 2012; 2017), that evaluate current MH discharge resources (e.g., well connected, somewhat connected, waitlisted, non-compliant, or services not meeting current needs), assess family stressors, and link to local MH resources may be useful. The HEADS-ED’s online tool (www.ottawa.heads-ed.com) is unique in that it helps identify the most appropriate community MH service by linking individual item responses to these resources, therefore increasing the likelihood of meeting patient needs and decreasing the burden on physicians to remain up-to-date on available resources. The online HEADS-ED tool for the Ottawa area and region is currently being used and evaluated as part of an ED MH Clinical Pathway implemented across four EDs in Ontario (ClinicalTrials.gov, 2015; Jabbour et al., 2016).
Clinical pathways specific to pediatric MH are important for standardizing MH care in the ED and in providing timely follow-up to appropriate MH resources (Jabbour et al., 2018). As repeat patients are heavy users of the ED, implications include that volumes and wait times will continue to increase until these patients can get connected within days of their visit. The fact that EDs, unlike primary care, offer crisis management and access without a referral may also play a role in repeat ED visits (Gill et al., 2017; Padgett & Brodsky, 1992). Therefore, clinical pathways that are family- centered and that emphasize collaboration and integration with other sectors, including primary care, schools and community-based MH agencies, may help reduce repeated visits (Stiffman et al., 2000).
Acknowledgments/Conflicts of Interest
We acknowledge the contribution of CHEO’s Clinical Research Unit (CRU) for their guidance and support around study design, methodology and statistical analysis.
References
- Angold A, Messer SC, Stangl D, Farmer EM, Costello EJ, Burns BJ. Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health. 1998;88(1):75–80. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attkisson C, Greenfield TK. The UCSF client satisfaction scales: The client satisfaction questionnaire-8. In: Maruish ME, editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. NJ: Lawrence Erlbaum Associates; 2004. pp. 799–811. [Google Scholar]
- Attkisson CC, Zwick R. The client satisfaction questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation & Program Planning. 1982;5:233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Blader JC. Symptom, family, and service predictors of children’s psychiatric rehospitalization within one year of discharge. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(4):440–451. doi: 10.1097/00004583-200404000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brannan AM, Heflinger CA, Foster EM. The role of caregiver strain and other family variables in determining children’s use of mental health services. Journal of Emotional & Behavioral Disorders. 2003;11(2):77–91. doi: 10.1177/106342660301100202. [DOI] [Google Scholar]
- Cappelli M, Glennie JE, Cloutier P, Kennedy A, Vloet M, Newton A, Gray C. Physician management of pediatric mental health patients in the emergency department: Assessment, charting, and disposition. Pediatric Emergency Care. 2012;28(9):835–841. doi: 10.1097/PEC.0b013e31826764fd. [DOI] [PubMed] [Google Scholar]
- Cappelli M, Zemek R, Polihronis C, Thibedeau NR, Kennedy A, Gray C, …Cloutier P. The HEADS-ED: Evaluating the clinical use of a brief, action-oriented, pediatric mental health screening tool. Pediatric Emergency Care. 2017;0(0):1–7. doi: 10.1097/PEC.0000000000001180. [DOI] [PubMed] [Google Scholar]
- Christodulu KV, Lichenstein R, Weist MD, Shafer ME, Simone M. Psychiatric emergencies in children. Pediatric Emergency Care. 2002;18(4):268–270. doi: 10.1097/00006565-200208000-00009. [DOI] [PubMed] [Google Scholar]
- ClinicalTrials.gov. Improving Transitions in Care for Children and Youth With Mental Health Concerns. 2015. Available at https://clinicaltrials.gov/ct2/show/NCT02590302.
- Cloutier P, Kennedy A, Maysenhoelder H, Glennie EJ, Cappelli M, Gray C. Pediatric mental health concerns in the emergency department. Pediatric Emergency Care. 2010;26(2):99–106. doi: 10.1097/PEC.0b013e3181cdcae1. [DOI] [PubMed] [Google Scholar]
- Cloutier P, Thibedeau N, Barrowman N, Gray C, Kennedy A, Leon S, Cappelli M. Predictors of repeated visits to a pediatric emergency department crisis intervention program. Canadian Journal of Emergency Medicine. 2017;19(2):122–130. doi: 10.1017/cem.2016.357. [DOI] [PubMed] [Google Scholar]
- Chun TH, Katz ER, Duffy SJ, Gerson RS. Challenges of managing pediatric mental health crises in the emergency department. Child & Adolescent Psychiatric Clinics of North America. 2015;24:21–40. doi: 10.1016/j.chc.2014.09.003. [DOI] [PubMed] [Google Scholar]
- Dolan MA, Fein JA The Committee on Pediatric Emergency Medicine. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics. 2011;127(5):e1356–1366. doi: 10.1542/peds.2011-0522. [DOI] [PubMed] [Google Scholar]
- Fite PJ, Stoppelbein L, Greening L. Predicting readmission to a child psychiatric inpatient unit: The impact of parenting styles. Journal of Child & Family Studies. 2009;18:621–629. doi: 10.1007/s10826-009-9284-8. [DOI] [Google Scholar]
- Flynn HA, Davis M, Marcus SM, Cunningham R, Blow FC. Rates of maternal depression in pediatric emergency department and relationship to child service utilization. General Hospital Psychiatry. 2004;26:316–322. doi: 10.1016/j.genhosppsych.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Fontanella CA. The influence of clinical, treatment and healthcare system characteristics on psychiatric readmission of adolescents. American Journal of Orthopsychiatry. 2008;78(2):187–198. doi: 10.1037/a0012557. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford T, Hamilton H, Dosani S, Burke L, Goodman R. The children’s services interview: Validity and reliability. Social Psychiatry & Psychiatric Epidemiology. 2007;42:36–49. doi: 10.1007/s00127-006-0092-9. [DOI] [PubMed] [Google Scholar]
- Gill PJ, Saunders N, Gandhi S, Gonzalez A, Kurdyak P, Vigod S, Guttmann A. Emergency department as a first contact for mental health problems in children and youth. Journal of the American Academy of Child & Adolescent Psychiatry. 2017;56(6):475–482.e4. doi: 10.1016/j.jaac.2017.03.012. [DOI] [PubMed] [Google Scholar]
- Goldstein AB, Frosch E, Davarya S, Leaf PJ. Factors associated with a six-month return to emergency services among child and adolescent psychiatric patients. Psychiatric Services. 2007;58(11):1489–1492. doi: 10.1176/appi.ps.58.11.1489. [DOI] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology & Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. The extended version of the strengths and difficulties questionnaire as a guide to child psychiatric caseness and consequent burden. Journal of Child Psychology & Psychiatry. 1999;40(5):791–799. [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Grupp-Phelan J, Mahajan P, Foltin GL, Jacobs E, Tunik M, Sonnett M Pediatric Emergency Care Applied Research Network. Referral and resource use patterns for psychiatric-related visits to pediatric emergency departments. Pediatric Emergency Care. 2009;25(4):217–220. doi: 10.1097/pec.0b013e31819e3523. [DOI] [PubMed] [Google Scholar]
- Grupp-Phelan J, Whitaker RC, Naish AB. Depression in mothers of children presenting for emergency and primary care: Impact on mothers’ perceptions of caring for their children. Ambulatory Pediatrics. 2003;3(3):142–146. doi: 10.1367/1539-4409(2003)003<0142:dimocp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Hallgren KA. Computing inter-rater reliability for observational data: An overview and tutorial. Tutorials in Quantitative Methods for Psychology. 2012;8(1):23–34. doi: 10.20982/tqmp.08.1.p023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoagwood KE, Jensen PS, Arnold LE, Roper M, Severe J, Odbert C The MTA Cooperative Group. Reliability of the services for children and adolescents – parent interview. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(11):1345–1354. doi: 10.1097/01.chi.0000139558.54948.1f. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp; (Released 2017) [Google Scholar]
- Jabbour M, Hawkins J, Day D, Cloutier P, Polihronis C, Cappelli M, Kennedy A, Gray C. An emergency department clinical pathway for children and youth with mental health conditions. Child & Adolescent Psychiatric Clinics of North America. 2018;27(3):413–425. doi: 10.1016/j.chc.2018.02.005. [DOI] [PubMed] [Google Scholar]
- Jabbour M, Reid S, Polihronis C, Cloutier P, Gardner W, Kennedy A, Cappelli M. Improving mental health care transitions for children and youth: A protocol to implement and evaluate an emergency department clinical pathway. Implementation Science. 2016;11(1):90. doi: 10.1186/s13012-016-0456-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Hoagwood KE, Roper M, Arnold LE, Odbert C, Crowe M, Wells K. The services for children and adolescents – parent interview: Development and performance characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(11):1334–1344. doi: 10.1097/01.chi.0000139557.16830.4e. [DOI] [PubMed] [Google Scholar]
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon SL, Cloutier P, Polihronis C, Zemek R, Newton AS, Gray C, Cappelli M. Child and adolescent mental health repeat visits to the emergency department: A systematic review. Hospital Pediatrics. 2017;7(3):177–186. doi: 10.1542/hpeds.2016-0120. [DOI] [PubMed] [Google Scholar]
- LeVois M, Nguyen TD, Attkisson CC. Artifact in client satisfaction assessment: Experience in community mental health settings. Evaluation & Program Planning. 1981;4:139–150. doi: 10.1016/0149-7189(81)90004-5. [DOI] [PubMed] [Google Scholar]
- Logan DE, King CA. Parental facilitation of adolescent mental health service utilization: A conceptual and empirical review. Clinical Psychology: Science & Practice. 2001;8(3):319–333. [Google Scholar]
- Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. Journal of Pediatrics. 2015;167(4):905–910. doi: 10.1016/j.jpeds.2015.07.004. [DOI] [PubMed] [Google Scholar]
- Newton AS, Ali S, Johnson DW, Haines C, Rosychuk RJ, Keaschuk RA, Klassen TP. A 4-year review of pediatric mental health emergencies in Alberta. Canadian Journal of Emergency Medicine. 2009;11(5):447–455. doi: 10.1017/s1481803500011647. [DOI] [PubMed] [Google Scholar]
- Newton AS, Ali S, Johnson DW, Haines C, Rosychuk RJ, Keaschuk RA, Klassen TP. Who comes back? Characteristics and predictors of return to emergency department services for pediatric mental health care. Academic Emergency Medicine. 2010;17:177–186. doi: 10.1111/j.1553-2712.2009.00633.x. [DOI] [PubMed] [Google Scholar]
- Padgett DK, Brodsky B. Psychosocial factors influencing non-urgent use of the emergency room: A review of the recommendations for research and improved service delivery. Social Science & Medicine. 1992;35(9):1189–1197. doi: 10.1016/0277-9536(92)90231-e. [DOI] [PubMed] [Google Scholar]
- Peterson BS, Zhang H, Santa Lucia R, King RA, Lewis M. Risk factors for presenting problems in child psychiatric emergencies. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(9):1162–1173. doi: 10.1097/00004583-199609000-00014. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2018. [Google Scholar]
- Rezvan PH, Lee KJ, Simpson JA. The rise of multiple imputation: A review of the reporting and implementation of the method in medical research. BMC Medical Research Methodology. 2015;15(30):1–14. doi: 10.1186/s12874-015-0022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner H, Steinhauer P, Sitarenios G. Family assessment measure (FAM) and process model of family functioning. Journal of Family Therapy. 2000;22:190–210. [Google Scholar]
- Sobolewski B, Richey L, Kowatch RA, Grupp-Phelan J. Mental health follow-up among adolescents with suicidal behaviors after emergency department discharge. Archives of Suicide Research. 2013;17(4):323–334. doi: 10.1080/13811118.2013.801807. [DOI] [PubMed] [Google Scholar]
- Sperandei S. Understanding logistic regression analysis. Biochemia Medica. 2014;24(1):12–18. doi: 10.11613/BM.2014.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. Postal CodeOM Conversion File Plus (PCCF+) Version 6C, Reference Guide. Ottawa: Minister of Industry; 2015. 2016. (Statistics Canada Catalogue no. 82-E0086-XDB). [Google Scholar]
- Stiffman AR, Hadley-Ives E, Doré P, Polgar M, Horvath VE, Striley C, Elze D. Youths’ access to mental health services: The role of providers’ training, resource connectivity, and assessment of need. Mental Health Services Research. 2000;2(3):141–154. doi: 10.1023/a:1010189710028. [DOI] [PubMed] [Google Scholar]
- Tossone K, Jefferis E, Bhatta MP, Bilge-Johnson S, Seifert P. Risk factors for rehospitalization and inpatient care among pediatric psychiatric intake response center patients. Child & Adolescent Psychiatry & Mental Health. 2014;8(27):1–10. doi: 10.1186/1753-2000-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K. Mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software. 2011;45(3):1–67. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- Yu AY, Rosychuk RJ, Newton AS. Clinical acuity of repeat pediatric mental health presentations to the emergency department. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2011;20(3):208–213. [PMC free article] [PubMed] [Google Scholar]