Abstract
Study Objectives:
To estimate the prevalence of insomnia disorder among older veterans and to study relationships among age and self-rated health, with insomnia disorder, self-reported sleep duration and sleep efficiency.
Methods:
A cross-sectional postal survey of community-dwelling older veterans (older than 60 years) seen at one VA Healthcare System in the prior 18 months was performed, which was constructed to align with the general diagnostic criteria for insomnia disorder (International Classification of Sleep Disorders, Second Edition [ICSD-2]). The survey also queried self-reported sleep duration, bedtime, and wake time, which were used to calculate sleep efficiency. The survey also asked about race/ethnicity and self-rated health (using the general health item from the Short Form-36).
Results:
A completed survey was returned by 4,717 individuals (51.9% response rate; mean age 74.1 years). Of those, 2,249 (47.7%) met ICSD-2 diagnostic criteria for insomnia disorder. In logistic regression analyses, insomnia disorder was more likely among younger age categories (odds ratios [OR] 1.4–2.5) and in those with worse self-rated health (OR 2.1–14.4). Both total nocturnal sleep time and time in bed increased with older age (all P < .001), whereas sleep efficiency did not differ. Worse self-rated health was associated with shorter total nocturnal sleep time, more time in bed, and lower (worse) sleep efficiency.
Conclusions:
Results of the postal survey suggest that almost half of community-dwelling older veterans have insomnia disorder, which was more common in young-old and among those with worse self-rated health. Additional work is needed to address the high burden of insomnia among older adults, including those with poor health.
Citation:
Ryden AM, Martin JL, Matsuwaka S, Fung CH, Dzierzewski JM, Song Y, Mitchell MN, Fiorentino L, Josephson KR, Jouldjian S, Alessi CA. Insomnia disorder among older veterans: results of a postal survey. J Clin Sleep Med. 2019;15(4):543–551.
Keywords: aging, insomnia, self-rated health, survey study
BRIEF SUMMARY
Current Knowledge/Study Rationale: There has been a wide range of estimates of insomnia in older patients. The purpose of this study was to estimate the prevalence of insomnia disorder in an older veteran population using a survey instrument designed to align with diagnostic criteria for insomnia disorder.
Study Impact: Nearly half of the community-dwelling veterans surveyed responded in a manner consistent with diagnostic criteria for insomnia disorder. Older age and better self-rated health were associated with a decreased likelihood of having insomnia disorder.
INTRODUCTION
Insomnia is common among older adults, and some evidence suggests it is particularly common among veterans.1 However, reported prevalence varies widely and most studies report insomnia symptoms rather than established diagnostic criteria for insomnia disorder.2–6 Insomnia is associated with adverse consequences on health and quality of life,4–6 but the relationship between sleep and health may be bidirectional.7,8 Insomnia symptoms are common in older people with comorbidities,9–11 and the severity of chronic insomnia seems to correlate with worse health-related quality of life12–15 and greater health care utilization.16,17 Furthermore, there may be significant economic consequences of insomnia.18 The relationship between insomnia and advanced age is unclear, with some studies suggesting insomnia symptoms increase with age,19,20 whereas other studies have found nonlinear relationships with sleep complaints actually decreasing after age 60 years.21,22
Insomnia symptoms are common among military veterans.23–25 In addition, a recent study of older veterans with impairment in activities of daily living showed that 71% had at least mild daytime sleepiness.26 One reason why identifying those with insomnia disorder is so critical is that treatments (such as cognitive behavioral therapy for insomnia [CBT-I]) depend on the patient meeting diagnostic criteria (for example, CBT-I is not used for other sleep disorders or for insufficient sleep). As the Department of Veterans Affairs (VA) (and other health care systems) seeks to expand the availability of CBTI through a nationwide dissemination program,27 identifying how many veterans are likely appropriate for this treatment has become essential.
To identify veterans with insomnia who may be appropriate for CBT-I, we conducted a postal survey of all community-dwelling patients aged 60 years and older who had received care at one large VA ambulatory care center in the prior 18 months. The objectives of the current study were to determine the prevalence of insomnia disorder according to established diagnostic criteria, and to examine the relationships between insomnia disorder, age, and self-rated health. Associations between age and self-rated health with self-reported nocturnal sleep time, time in bed, and sleep efficiency were also examined.
METHODS
Participants
Using electronic data, we identified all patients aged 60 years and older who had received care at one large VA ambulatory care center within the previous 18-months. We developed a survey instrument, which was mailed to all patients (n = 9,080) who were aged 60 years and older, and lived within 30 miles of the ambulatory care center (based on ZIP codes), in random blocks between May 2010 and January 2012. Returned surveys were reviewed and participants with vague or missing responses were contacted by telephone by research staff for clarification unless they checked an “opt out” box indicating they did not wish to be contacted. If the survey was not returned, a second copy was mailed 3 weeks later. There were 21 surveys completed by someone other than the patient (for example, a family member), which were dropped. All other returned surveys that provided adequate information to determine insomnia diagnosis (as described in the next paragraphs) were included in the analyses. This survey was implemented in the recruitment phase of a randomized controlled trial assessing the efficacy of CBT-I using nonclinician health coaches in older veterans, and was used to both assess the prevalence of insomnia and to identify those who might be eligible for the trial.28 The study procedures were approved by the Institutional Review Board at the VA Greater Los Angeles Healthcare System and a waiver of documentation of informed consent was obtained.
Procedures
The survey instrument was developed by the research team to determine whether respondents had insomnia based on the International Classification of Sleep Disorders, Second Edition (ICSD-2) general diagnostic criteria for insomnia,29 which were the diagnostic criteria in place at the time of the study. In ICSD-2, these general criteria apply to several insomnia diagnoses (eg, psychophysiological insomnia, idiopathic insomnia). Our interest focused on individuals with “chronic insomnia” rather than “adjustment (acute) insomnia. For simplicity (and in keeping with International Classification of Sleep Disorders, Third Edition [ICSD-3]), throughout this manuscript we use the term “insomnia disorder,” rather than the more technically correct term (per ICSD-2) “insomnia disorders other than adjustment (acute) insomnia.” In addition, as described in the next section, in keeping with ICSD-3, our focus was on participants with chronic insomnia disorder (≥ 3 months duration). Differences between the ICSD-2 diagnostic criteria used in the current study, and the more recent update (ICSD-3)30 are indicated in the next section. Survey items were developed using four steps:
Previously published and validated scales for sleep and insomnia were reviewed for potential survey items.
Items were adapted and simplified, and reading level (with a goal of a fifth-grade level) adjusted for use as a postal survey.
Cognitive interviews with older patients were performed to ensure respondents understood questions consistently and as intended.
After revising items based on cognitive interviews, three investigators (JLM, CAA, KJ) independently reviewed the items and finalized the survey in a consensus process.
The finalized survey (see supplemental materials) contained 25 items that queried sleep-related items over the previous month. Self-reported race/ethnicity information was collected from a single item (stating “Which of these categories best describes you,” with instructions to check all that apply). The survey also included the general health item from the Short Form-36 (SF-36), which asks the participant to rate their general health on a five-point Likert scale from poor to excellent health.
Measures
Survey responses identified patients who met ICSD-2 criteria for insomnia disorder that was of chronic duration using four steps, which determined the presence of: (1) nighttime sleep disturbance, (2) the sleep disturbance occurs despite adequate opportunity and circumstances for sleep, (3) daytime symptoms, and (4) duration of symptoms of 3 months or more. Respondents who met criteria in all four steps were considered to have insomnia disorder. The survey items related to diagnostic criteria for insomnia disorder are shown in the supplemental material.
Step 1 determined ICSD-2 criterion A, which includes at least one of the following sleep complaints: difficulty falling asleep, difficulty staying asleep, waking too early, or sleep that is nonrestorative. Survey items queried whether on a typical night respondents have trouble falling asleep, trouble staying asleep all night, or wake up earlier than they wanted; an additional item asked them to describe their sleep in general as very good, fairly good, fairly bad, or very bad (sleep quality). Based on cognitive interviewing, the candidate items for “nonrestorative” sleep did not meet acceptable standards, and were not included in the final survey. Of note, this also agrees with the most recent update of diagnostic criteria for insomnia, where nonrestorative sleep has been removed.30 The survey also asked about typical bedtime, minutes to fall asleep, usual time to get out of bed in the morning, and hours of actual sleep. These items were used to calculate sleep efficiency (ie, hours of sleep divided by time in bed calculated as the difference between bedtime and rise time) and sleep latency (ie, minutes to fall asleep). Criterion A was met if the respondent reported difficulty falling asleep, difficulty staying asleep, waking too early, sleep quality reported as “fairly bad” or “very bad,” sleep efficiency less than 80%, or sleep latency greater than 30 minutes.31
Step 2 determined ICSD-2 criterion B, which requires that the sleep complaint cannot be explained by an inadequate place or opportunity to sleep. The survey included a question asking whether the respondent had a “comfortable place to sleep.” Criterion B was met if respondents answered yes to this question and reported a time in bed of at least 5 hours (calculated as the elapsed time from bedtime to rise time reported on the survey).
Step 3 addressed ICSD-2 criterion C, which requires the presence of at least one daytime consequence related to the nighttime sleep complaint. Specific daytime consequences listed in ICSD-2 were operationalized in a lay language, yes/ no format. These items asked whether during the past month the respondent had any of the following daytime symptoms because he or she did not sleep well at night: feel tired or fatigued; trouble paying attention, concentrating, or remembering things; difficulty with work or social life; feel irritable, depressed, or anxious; feel sleepy during the day; have less motivation, energy or drive; make mistakes or have accidents; feel achy, have headaches or stomach problems; take a nap or doze off during the daytime; and have concerns about sleep (derived from sleep quality reported as “fairly bad” or “very bad”).
Step 4 assessed the duration of insomnia. We were primarily interested in chronic insomnia, which is also consistent with the most recent diagnostic criteria for insomnia.30 An item queried how long the respondents had problems with their sleep. Respondents who selected “less than 3 months” or “I don't have sleep problems” did not meet Step 4. Respondents who selected a duration of “3 months to 12 months” or “more than 12 months” met Step 4.
Our survey did not query whether the nighttime sleep disturbance and daytime symptoms occurred at least three times per week, which was added in the most recent diagnostic criteria for insomnia.30
Reassessment of Insomnia
Survey respondents who met criteria for insomnia and met other study eligibility requirements were invited to participate in the behavioral treatment trial, which included a baseline in-person assessment.28 During the baseline assessment, the survey items addressing the ICSD-2 diagnostic criteria were repeated and the Insomnia Severity Index (ISI)32 and Pittsburgh Sleep Quality Index (PSQI)33 were administered, providing confirmatory evidence for insomnia. We compared survey results with repeat in-person ICSD-2 diagnosis of insomnia and ISI and PSQI scores among survey participants (n = 429) who completed this in-person assessment.
Statistical Analysis
All statistical analyses were completed using Stata version 13.1 (StataCorp LP, College Station, Texas, United States).
The prevalence of insomnia was determined by calculating the proportion of responders who met the aforementioned diagnostic criteria. Descriptive statistics were computed for selected demographic and other variables, computing mean and standard deviation (SD) for continuous variables and frequency for categorical variables.
We tested for differences between responders and nonresponders using variables obtained from the administrative database including age, sex, and months since last visit at the VA Healthcare System. Patients were classified as responders versus nonresponders with the intent to adjust prevalence rates for response bias. For returned surveys, a responder was defined as providing a sufficiently complete survey to ascertain diagnostic criteria for insomnia. All others (and those who did not return a survey) were categorized as nonresponders. Responders were older than nonresponders (mean age 74.1 years versus 73.2 years, P < .001) and had less time since their last clinic visit (mean of 8.8 versus 9.2 months, P < .001). There was no difference in sex between responders and nonresponders (χ2(1) = 1.87, P = .17). Age and time since last visit were used to create nonresponse weights. These variables were computed by entering age and time since last visit as predictors in a logistic regression model predicting nonresponse. The inverse of the predicted probability of being a responder was used as a nonresponse weight for analyses of prevalence estimates. As described in the next paragraphs, 47.7% of responders met insomnia diagnostic criteria. The estimated prevalence of insomnia adjusted for response bias was 48.1%. Because the difference between the observed and adjusted prevalence of insomnia was small, our subsequent analyses were not adjusted for potential response bias.
We also investigated the degree to which insomnia rates were sensitive to more stringent application of criterion C (daytime consequences), by calculating the prevalence of insomnia when satisfaction of criterion C required two or more, and three or more daytime consequences.
A logistic regression model was used to predict the presence of insomnia disorder based on age, sex, race/ethnicity, and self-reported health. The logistic regression model was used to compute predicted probabilities as a function of age and self-reported health status by computing the average marginal value. Seemingly unrelated regression (SUR) models (ie, where the error terms in the regression equations are correlated) were used to predict other sleep-related variables (ie, total nocturnal sleep time, time in bed and sleep efficiency) with age category, self-rated health status, race/ethnicity and sex as predictor variables.34 Tests of categorical predictors (within the SUR models) were tested using Wald χ2 tests. The differences in hours of sleep, time in bed, and sleep efficiency between those with and without insomnia disorder were compared using t tests.
RESULTS
Survey Participant Characteristics
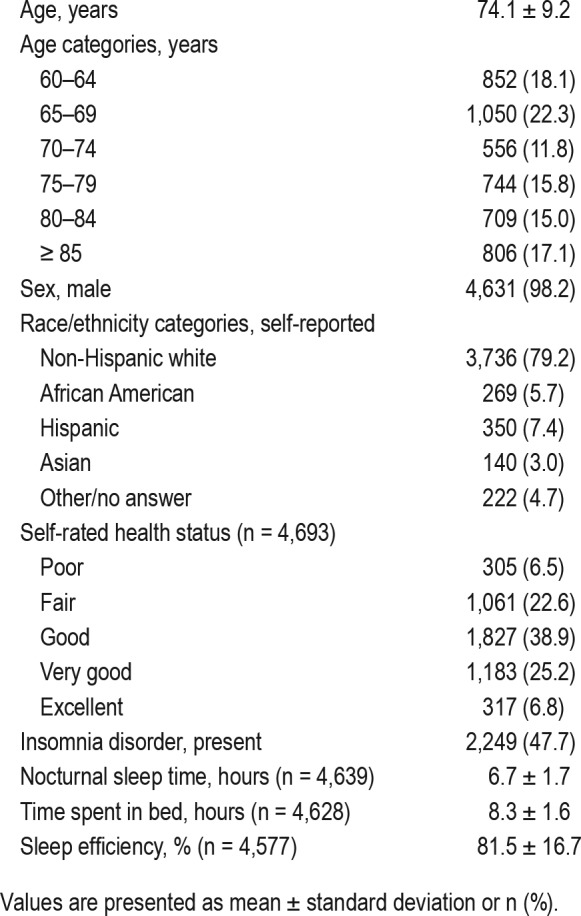
Of the 9,080 patients mailed a survey, 4,717 patients (51.9%) returned a sufficiently completed survey. Descriptive statistics are presented in Table 1. Mean age was 74.1 years (range 60–100 years). Most respondents were male, reflecting the older veteran population. A total of 2,249 respondents (47.7%) met diagnostic criteria for insomnia disorder (as described previously). Chi-square omnibus testing showed that overall there was a significant relationship between age and insomnia disorder (χ2(5) = 53.9, P < .001), as well as between self-rated health and insomnia disorder (χ2(4) = 365.1, P < .001).
Table 1.
Demographic information, self-reported health, insomnia disorder, self-reported total nocturnal sleep time, time spent in bed, and sleep efficiency (n = 4,717).
Sensitivity Analysis of Insomnia Prevalence
When criteria were adjusted to require at least two daytime consequences for meeting criterion C, the number of patients meeting criteria for insomnia decreased to 2,140 (45.4%). If at least 3 daytime consequences were required for criterion C, the number of patients meeting criteria of insomnia decreased to 1,994 (42.3%).
Factors Related to Insomnia Disorder
Table 2 shows the results of the logistic regression model predicting insomnia disorder. Insomnia was more likely in those who were younger and in those with poorer self-rated health. Insomnia was less likely among African Americans and Asians compared to Whites. Figure 1A illustrates the relationship between insomnia and age, showing that the probability of insomnia disorder decreases as a function of age. The relationship between insomnia and self-rated health is illustrated in Figure 1B, which shows that the probability of insomnia decreases with increasing (ie, better) self-rated health.
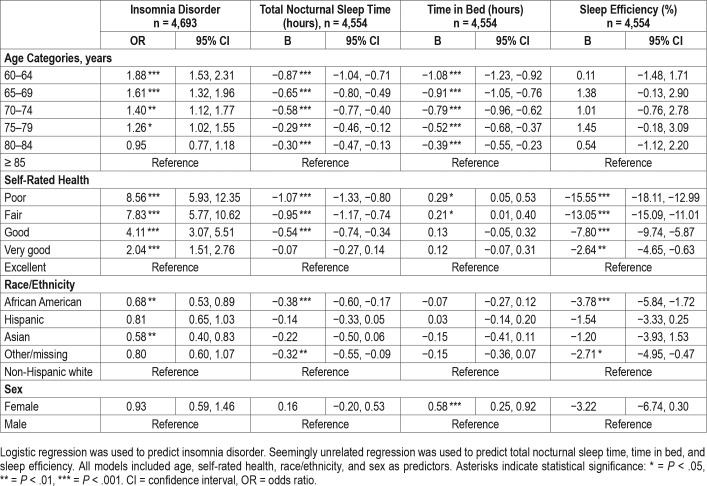
Table 2.
Models predicting insomnia disorder, total nocturnal sleep time, time in bed, and sleep efficiency.
Figure 1. Predicted probability of insomnia disorder (adjusting for age, self-rated health, race/ethnicity, and sex).
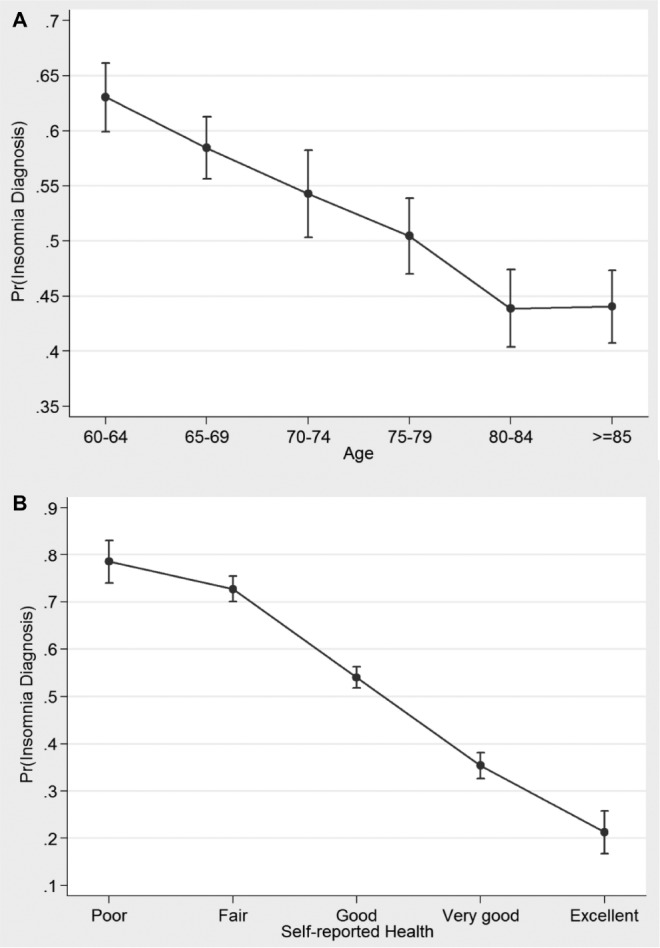
(A) Predicted probability of insomnia disorder as a function of age. (B) Predicted probability of insomnia disorder as a function of self-rated health.
Factors Related to Total Nocturnal Sleep Time, Time in Bed, and Sleep Efficiency
The results of the seemingly unrelated regression models with the outcomes of total nocturnal sleep time, time in bed, and sleep efficiency are also shown in Table 2.
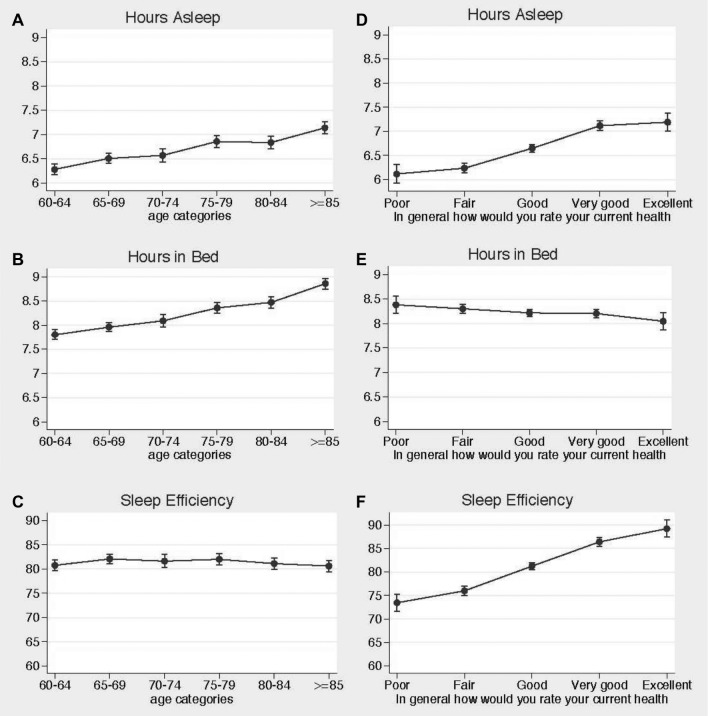
There was a significant relationship between age and total nocturnal sleep time (Wald χ2(5) = 135.8, P < .001) and time in bed (Wald χ2(5) = 251.7, P < .001), but not sleep efficiency (Wald χ2(5) = 6.2, P = .29). Specifically, total nocturnal sleep time and time in bed both increased with increasing age (Figure 2, panels A, B, and C).
Figure 2. Predicted mean of nocturnal sleep time, time in bed, and sleep efficiency (adjusting for age, self-rated health, race/ ethnicity, and sex).
(A) Predicted mean of total nocturnal sleep time as a function of age. (B) Predicted mean of time in bed as a function of age. (C) Predicted mean of sleep efficiency as a function of age. (D) Predicted mean of total nocturnal sleep time as a function of self-rated health. (E) Predicted mean of time in bed as a function of self-rated health. (F) Predicted mean sleep efficiency as a function of self-rated health.
Self-rated health was significantly associated with nocturnal sleep time (Wald χ2(4) = 217.2, P < .001) and sleep efficiency (Wald χ2(4) = 368.9, P < .001) but not time in bed (Wald χ2(4) = 7.5, P = .113). Total nocturnal sleep time and sleep efficiency were higher with increasing (ie, better) self-rated health, whereas time spent in bed decreased slightly with improved self-rated health (Figure 2, panels D, E, and F).
Differences in Other Self-Reported Sleep Measures By Insomnia Disorder
Not surprisingly, there were significant differences in total nocturnal sleep time, time in bed, and sleep efficiency between respondents who did and did not meet diagnostic criteria for insomnia. In those with insomnia disorder, the mean nocturnal sleep time was 6.0 hours versus 7.3 hours in those without insomnia (P < .001). There was no significant difference in time in bed: 8.3 hours in those with insomnia disorder versus 8.2 hours in those without insomnia (P = .507). Mean sleep efficiency was 74.0% in those with insomnia disorder versus 88.4% in those without (P < .001).
Reassessment of Insomnia
Of the 429 participants who met criteria for insomnia disorder based on the postal survey, and completed an in-person assessment, 381 (88.8%) still met the basic criteria for insomnia disorder at the time of the baseline assessment (on average, 73 days later). The mean ISI score was 10.7 (SD 5.4), and 69.9% had at least mild insomnia. The mean PSQI score was 8.6 (SD 3.8), 74.6% (n = 250) had a score higher than 5, consistent with clinically significant poor-quality sleep. Similarly, when the more stringent criteria were used to identify those with daytime consequences on the survey (ie, requiring at least 3 daytime symptoms), 310 (71.6%) still met criteria for those more stringent criteria for insomnia disorder at the time of the baseline assessment, 70.9% (n = 224) had at least mild insomnia on the ISI, and 74.7% (n = 230) had a PSQI score higher than 5, consistent with clinically significant poor-quality sleep.
DISCUSSION
Using a postal survey to identify older patients who met basic criteria for insomnia disorder, we found that 47.7% of community-dwelling veterans aged 60 years and older had evidence of insomnia and therefore may be in need of treatment for their sleep-related difficulties. When more strict criteria for daytime consequences are applied, the rate of insomnia decreased by only 5.4%, to 42.3%. Previous population-based studies of insomnia have varied widely in estimated prevalence of insomnia, from 7.9% to more than 50%.22,35 This variation may be the result of differences in population studied and in methods used to identify insomnia. We used established diagnostic criteria; requiring nighttime symptoms, daytime impairment, and longstanding symptoms. This definition of insomnia disorder facilitates identification of those in need of treatment in clinical settings. In a recent study using VA administrative data, only 3.4% of veterans had an insomnia diagnosis based on presence of an ICD-9 code for insomnia in their medical record.36
We found the prevalence of insomnia disorder decreased with increasing age in our sample (ie, there was more insomnia in the “young-old” compared to the “older-old”), even after adjusting for self-rated health. This was not likely due to sampling error at the extremes of age because each age category had a relatively large number of respondents. Prior research addressing the relationship between insomnia and advanced age has had mixed results, with some evidence suggesting a decrease,21,37 and other evidence suggesting an increase in insomnia with advancing age.2,35,38,39 For example, Jaussent et al. found the odds of insomnia increased in each 5-year cohort after age 65 years, particularly in men.20
The increased prevalence of insomnia disorder we found in the young-old may be related to “cohort” differences in young-old versus older-old individuals who seek care in the VA. It is also possible that increasing rates of cognitive impairment may have affected the ability of the older-old individuals to accurately recall details about their sleep habits and quality over the past month. In addition, sleep complaints have been linked to comorbidities in older populations,40 and a healthy survivor effect may be one factor explaining less insomnia in the older-old veterans. However, the persistent relationship between insomnia and age after controlling for self-rated health status suggests this does not explain the entire story. Another possibility is that young-old patients are more likely to report symptoms of insomnia. A study from Norway found increased nocturnal sleep disturbance with age, but reports of daytime symptoms were decreased with age.41 Thus, it is conceivable that older patients have fewer daytime complaints, which prevents them from meeting insomnia diagnostic criteria. Furthermore, the factors that go into satisfaction with sleep seem to change with age.42 Previous studies in older patients without insomnia complaints found they had more self-reported and objectively disturbed sleep compared to younger counterparts, suggesting a possible adaptation to what they consider acceptable sleep.43 A prior study suggests that total nocturnal sleep time and sleep efficiency decrease with increasing age.44 In our sample, however, self-reported nocturnal sleep time actually increased with age, which may reflect that insomnia disorder also decreased with increasing age. However, sleep efficiency did not change with increasing age, perhaps related to the increased time in bed with age.
The relationship between worse self-rated health and insomnia was strong, and is largely consistent with prior research.12,37,39,45,46 Worse self-rated health may indicate a higher level of medical illness burden, which may affect sleep quality. Insomnia itself may be a risk factor for worse health, or the self-perception of worse health. Given the cross-sectional nature of our study, we cannot make inferences about the direction of causality between self-rated health and insomnia in this population. Unfortunately, we did not have access to more complete comorbidity data; however, this is an important area for future investigation as frailty, disease burden, and markers of “physiological aging” may be important.
We found that non-Hispanic whites had a small but signifi-cant increase in the odds of insomnia, which differs from some prior research.47 Further study of the relationship between race/ ethnicity and insomnia among veterans is required to confirm this finding.
Several study limitations need to be acknowledged. As a cross-sectional sample using self-report, we are unable to infer causality, and there may be inaccuracies associated with self-reported data. However, insomnia disorder is clinically diagnosed based on the self-report of symptoms.31,32 Another limitation is that the survey instrument has not been formally tested for psychometric validity; however, there are no validated instruments for assessing ICSD-2 criteria that can be used in a postal survey format (eg, with no skip patterns or multipart questions), and relying on medical record evidence of insomnia disorder is likely to underestimate the number of older veterans in need of treatment. We did draw many of the survey items from validated instruments, and sensitivity analyses (eg, for number of daytime symptoms) suggested high rates of insomnia even with more conservative criteria using our survey items. Furthermore, of the participants who completed an in-person assessment (as part of the parent clinical trial), 89% still screened positive for insomnia based on ICSD-2 criteria. This supports the test-retest reliability of the postal survey in identifying those with insomnia. However, our inability to retest those with a survey response that was negative for insomnia meant we could not calculate a kappa coefficient to more rigorously assess test-retest reliability. Another limitation is that this survey did not assess the frequency of symptoms, which has been added to the insomnia diagnostic criteria in recent years. Likewise, the space and structure limitations of the postal survey design prevented us from being able to assess the severity of the daytime symptoms.
Another limitation of the study is that we did not have access to administrative or electronic health record data among participants who completed the survey (access to these data was not allowed for the survey sample by our institutional review board). Therefore, we do not have access to medical record information regarding comorbidities, functional status, and other factors that may have affected participant responses. Another limitation was that, in this predominantly male, older veteran population, there were too few women to reliably test for sex differences; however, a study of women veterans found similarly high rates of insomnia disorder across age groups.48
The survey response rate (51.9%) might also be considered a limitation of the study, however, this rate is similar to average response rates reported in a meta-analysis of surveys (52.3% average response rate),49 and an older report of mailed surveys published in medical journals (60% average response rate).50 Analysis of the limited demographic data available from the administrative database used to obtain address information suggests that, compared to nonresponders, responders were older and more recently visited the ambulatory care center. It is possible that the prevalence of insomnia disorder is different between responders and nonresponders; we are unable to test this possibility with the available data. Finally, this study did not account for important covariates such as obstructive sleep apnea, psychiatric conditions, and pain, although insomnia should likely be treated even in the context of these comorbid conditions.
In conclusion, we found that nearly half of veterans 60 years of age and older suffer from insomnia disorder that likely meets established diagnostic criteria for insomnia and therefore may benefit from treatments such as CBT-I. Insomnia disorder was less common among older-old versus young-old respondents, and less common in those with better self-rated health. Prior reports of a low prevalence of insomnia in clinical databases suggest that much of the insomnia in older veterans is undiagnosed. Further work is needed to improve access to care in older adults for this important and highly prevalent condition.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Work for this study was performed at VA Greater Los Angeles Geriatric Research, Education and Clinical Center. This work was funded by Merit Review IIR 08-295-1 from the United States Department of Veterans Affairs Health Services Research and Development Program. Additional support was provided by the National Institutes of Health, National Institute on Aging (NIA), the American Federation for Aging Research (AFAR), UCLA Claude D. Pepper Center, the UCLA Clinical and Translational Science Institute and the VA Greater Los Angeles Healthcare System Geriatric Research Education and Clinical Center (GRECC). Parts of this work were presented at the annual meeting of the American Geriatrics Society in 2013 as well as the annual meeting of Associated Professional Sleep Societies in 2015. The authors report no conflicts of interest.
ABBREVIATIONS
- CBT-I
cognitive behavioral therapy for insomnia
- ICD
International Classification of Diseases
- ICSD
International Classification of Sleep Disorders
- ISI
Insomnia Severity Index
- PSQI
Pittsburgh Sleep Quality Index
- SF-36
Short Form-36
- SUR
seemingly unrelated regression
- VA
Veterans Affairs
REFERENCES
- 1.Alexander M, Ray MA, Hebert JR, et al. The National Veteran Sleep Disorder Study: Descriptive Epidemiology and Secular Trends, 2000-2010. Sleep. 2016;39(7):1399–1410. doi: 10.5665/sleep.5972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lichstein KL, Durrence HH, Riedel BW, Taylor DJ, Bush AJ. Epidemiology of Sleep: Age, Gender and Ethnicity. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 2004. [Google Scholar]
- 3.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foundation survey. Sleep. 1999;22(Suppl 2):S347–S353. [PubMed] [Google Scholar]
- 4.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 5.Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;37(1):9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 6.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 7.Ohayon MM, Zulley J, Guilleminault C, Smirne S, Priest RG. How age and daytime activities are related to insomnia in the general population: Consequences for older people. J Am Geriatr Soc. 2001;49(4):360–366. doi: 10.1046/j.1532-5415.2001.49077.x. [DOI] [PubMed] [Google Scholar]
- 8.Sivertsen B, Lallukka T, Salo P, et al. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res. 2014;23(2):124–132. doi: 10.1111/jsr.12102. [DOI] [PubMed] [Google Scholar]
- 9.Walsh JK, Coulouvrat C, Hajak G, et al. Nighttime insomnia symptoms and perceived health in the America Insomnia Survey (AIS) Sleep. 2011;34(8):997–1011. doi: 10.5665/SLEEP.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sivertsen B, Krokstad S, Overland S, Mykletun A. The epidemiology of insomnia: associations with physical and mental health. The HUNT-2 study. J Psychosom Res. 2009;67(2):109–116. doi: 10.1016/j.jpsychores.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30(2):213–218. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 12.Leger D, Morin CM, Uchiyama M, Hakimi Z, Cure S, Walsh JK. Chronic insomnia, quality-of-life, and utility scores: Comparison with good sleepers in a cross-sectional international survey. Sleep Med. 2012;13(1):43–51. doi: 10.1016/j.sleep.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 13.LeBlanc M, Beaulieu-Bonneau S, Merette C, Savard J, Ivers H, Morin CM. Psychological and health-related quality of life factors associated with insomnia in a population-based sample. J Psychosom Res. 2007;63(2):157–166. doi: 10.1016/j.jpsychores.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Lee M, Choh AC, Demerath EW, et al. Sleep disturbance in relation to health-related quality of life in adults: The fels longitudinal study. J Nutr Health Aging. 2009;13(6):576–583. doi: 10.1007/s12603-009-0110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leger D, Scheuermaier K, Philip P, Paillard M, Guilleminault C. SF-36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63(1):49–55. doi: 10.1097/00006842-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Kaufmann CN, Canham SL, Mojtabai R, et al. Insomnia and health services utilization in middle-aged and older adults: results from the health and retirement study. J Gerontol A Biol Sci Med Sci. 2013;68(12):1512–1517. doi: 10.1093/gerona/glt050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bin YS, Marshall NS, Glozier N. The burden of insomnia on individual function and healthcare consumption in Australia. Aust N Z J Public Health. 2012;36(5):462–468. doi: 10.1111/j.1753-6405.2012.00845.x. [DOI] [PubMed] [Google Scholar]
- 18.Ozminkowski RJ, Wang SH, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30(3):263–273. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 19.McCrae CS, Wilson NM, Lichstein KL, et al. Self-reported sleep, demographics, health, and daytime functioning in young old and old old community-dwelling seniors. Behav Sleep Med. 2008;6(2):106–126. doi: 10.1080/15402000801952906. [DOI] [PubMed] [Google Scholar]
- 20.Jaussent I, Dauvilliers Y, Ancelin ML, et al. Insomnia symptoms in older adults: associated factors and gender differences. Am J Geriatr Psychiatry. 2011;19(1):88–97. doi: 10.1097/JGP.0b013e3181e049b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grandner MA, Martin JL, Patel NP, et al. Age and sleep disturbances among American men and women: data from the US Behavioral Risk Factor Surveillance System. Sleep. 2012;35(3):395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uhlig BL, Sand T, Odegard SS, Hagen K. Prevalence and associated factors of DSM-V insomnia in Norway: the Nord-Trondelag Health Study (HUNT 3) Sleep Med. 2014;15(6):708–713. doi: 10.1016/j.sleep.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 23.Faestel PM, Littell CT, Vitiello MV, Forsberg CW, Littman AJ. Perceived insufficient rest or sleep among veterans: Behavioral Risk Factor Surveillance System 2009. J Clin Sleep Med. 2013;9(6):577–584. doi: 10.5664/jcsm.2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mustafa M, Erokwu N, Ebose I, Strohl K. Sleep problems and the risk for sleep disorders in an outpatient veteran population. Sleep Breath. 2005;9(2):57–63. doi: 10.1007/s11325-005-0016-z. [DOI] [PubMed] [Google Scholar]
- 25.Meissner HH, Reimer A, Santiago SM, Stein M, Goldman MD, Williams AJ. Failure of physician documentation of sleep complaints in hospitalized patients. West J Med. 1998;169(3):146–149. [PMC free article] [PubMed] [Google Scholar]
- 26.Papp KK, Abbott KH, Rose JH, Strohl KP. Sleepiness in elderly veterans. Sleep Breath. 2014;18(2):283–287. doi: 10.1007/s11325-013-0879-3. [DOI] [PubMed] [Google Scholar]
- 27.Manber R, Carney C, Edinger J, et al. Dissemination of CBTI to the non-sleep specialist: protocol development and training issues. J Clin Sleep Med. 2012;8(2):209–218. doi: 10.5664/jcsm.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alessi C, Martin JL, Fiorentino L, et al. Cognitive behavioral therapy for insomnia in older veterans using nonclinician sleep coaches: randomized controlled trial. J Am Geriatr Soc. 2016;64(9):1830–1838. doi: 10.1111/jgs.14304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Academy of Sleep Medicine. International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 30.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 31.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41(4):427–445. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 32.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 33.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 34.Zellner A. An efficient method of estimating seemingly unrelated regressions and tests for aggregation bias. J Am Stat Assoc. 1962;57:348–368. [Google Scholar]
- 35.Kim WH, Kim BS, Kim SK, et al. Prevalence of insomnia and associated factors in a community sample of elderly individuals in South Korea. Int Psychogeriatr. 2013;25(10):1729–1737. doi: 10.1017/S1041610213000677. [DOI] [PubMed] [Google Scholar]
- 36.Hermes E, Rosenheck R. Prevalence, pharmacotherapy and clinical correlates of diagnosed insomnia among Veterans Health Administration service users nationally. Sleep Med. 2014;15(5):508–514. doi: 10.1016/j.sleep.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 37.Roth T, Coulouvrat C, Hajak G, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. 2011;69(6):592–600. doi: 10.1016/j.biopsych.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 38.Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999-2010. Sleep. 2014;37(2):343–349. doi: 10.5665/sleep.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schubert CR, Cruickshanks KJ, Dalton DS, Klein BEK, Klein R, Nondahl DM. Prevalence of sleep problems and quality of life in an older population. Sleep. 2002;25(8):889–893. [PubMed] [Google Scholar]
- 40.Fagerstrom C, Hellström A. Sleep complaints and their association with comorbidity and health-related quality of life in an older population in Sweden. Aging Mental Health. 2011;15(2):204–213. doi: 10.1080/13607863.2010.513039. [DOI] [PubMed] [Google Scholar]
- 41.Pallesen S, Sivertsen B, Nordhus IH, Bjorvatn B. A 10-year trend of insomnia prevalence in the adult Norwegian population. Sleep Med. 2014;15(2):173–179. doi: 10.1016/j.sleep.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 42.Zilli I, Ficca G, Salzarulo P. Factors involved in sleep satisfaction in the elderly. Sleep Med. 2009;10(2):233–239. doi: 10.1016/j.sleep.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 43.Vitiello MV, Larsen LH, Moe KE. Age-related sleep change - gender and estrogen effects on the subjective-objective sleep quality relationships of healthy, noncomplaining older men and women. J Psychosom Res. 2004;56(5):503–510. doi: 10.1016/S0022-3999(04)00023-6. [DOI] [PubMed] [Google Scholar]
- 44.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 45.Seib C, Anderson D, Lee K. Prevalence and correlates of sleep disturbance in postmenopausal women: the Australian Healthy Aging of Women (HOW) Study. J Womens Health (Larchmt) 2014;23(2):151–158. doi: 10.1089/jwh.2013.4472. [DOI] [PubMed] [Google Scholar]
- 46.Furihata R, Uchiyama M, Takahashi S, et al. The association between sleep problems and perceived health status: a Japanese nationwide general population survey. Sleep Med. 2012;13(7):831–837. doi: 10.1016/j.sleep.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 47.Singareddy R, Vgontzas AN, Fernandez-Mendoza J, et al. Risk factors for incident chronic insomnia: A general population prospective study. Sleep Med. 2012;13(4):346–353. doi: 10.1016/j.sleep.2011.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martin JL, Schweizer CA, Hughes JM, et al. Estimated prevalence of insomnia among women veterans: results of a postal survey. Womens Health Issues. 2017;27(3):366–373. doi: 10.1016/j.whi.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anseel F, Lievens F, Schollaert E, Choragwicka B. Response rates in organizational science, 1995–2008: a meta-analytic review and guidelines for survey researchers. J Bus Psychol. 2010;25:335–349. [Google Scholar]
- 50.Asch D, Jedrziewski K, Christakis N. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.