Abstract
Study Objectives:
The prevalence of sleep disorders in the Lebanese population is unknown. We assessed the prevalence of insomnia and sleep apnea risk and examined their relationship with sociodemographic, lifestyle, and health characteristics in a sample from Greater Beirut.
Methods:
This cross-sectional pilot survey included 501 adults from the community (age 45.2 ± 15.2 years, 64% females). Insomnia symptoms, insomnia disorder, and sleep apnea risk were assessed using the Sleep Heart Health Study and Berlin Questionnaire. Characteristics were compared between individuals with and without insomnia symptoms, insomnia disorder, and sleep apnea. Correlates were assessed using multivariate regression.
Results:
A total of 44.5% of participants reported insomnia symptoms > 15 nights/mo and 34.5% reported insomnia. Predictors of insomnia symptoms and disorder included female sex (odds ratio [OR] 1.51, 95% confidence interval [CI] 1.01–2.27 and OR 1.76, 95% CI 1.13–2.75, respectively), education level below high school (OR 1.96, 95% CI 1.31–2.95 and OR 2.40, 95% CI 1.52–3.77, respectively) and medical comorbidities (OR 2.27, 95% CI 1.30–3.95 and OR 3.02, 95% CI 1.3–5.27, respectively). Although 31% of participants were at high risk for sleep apnea, only 5% received the diagnosis from a physician. Increased sleep apnea risk was associated with unemployment (OR 1.96, 95% CI 1.11–3.49), high body mass index (OR 1.17, 95% CI 1.11–1.24), snoring (OR 16.7, 95% CI 9.0–31.0), hypertension (OR 4.33, 95% CI 2.28–8.22), arthritis (OR 2.00, 95% CI 1.01–4.01), and other medical comorbidities (OR 2.65, 95% CI 1.24–5.68).
Conclusions:
Insomnia and sleep apnea are highly prevalent and likely underdiagnosed in this cohort from Lebanon and are associated with disadvantaged socioeconomic status and medical comorbidities. This alarming prevalence of sleep difficulties and disorders calls for future research exploring the causes including the potential effect of social, economic, and political instability, mental and psychological stress, local customs, and environmental factors.
Citation:
Chami HA, Bechnak A, Isma'eel H, Talih F, Nasreddine L, Nasrallah M, Tamim H. Sleepless in Beirut: sleep difficulties in an urban environment with chronic psychosocial stress. J Clin Sleep Med. 2019;15(4):603–614.
Keywords: insomnia, sleep apnea, sleep difficulties
BRIEF SUMMARY
Current Knowledge/Study Rationale: Data regarding sleep difficulties and disorders in the Lebanese population are lacking. This study aimed to assess insomnia and sleep apnea and examine their relationship with demographic, lifestyle, and health characteristics in a sample of the Lebanese population residing in Greater Beirut.
Study Impact: Insomnia symptoms and disorder are highly prevalent in this cohort from a low to medium income country, especially among women and individuals with disadvantaged socioeconomic status. Sleep apnea is significantly underdiagnosed. This study leads the way for further comparative research that assesses local-regional and sociocultural determinants of insomnia, and sleep apnea.
INTRODUCTION
The importance of sleep quality and its effect on well-being has been increasingly appreciated in recent decades. Indeed, poor sleep quality and sleep disorders such as insomnia and sleep apnea have been associated with multiple adverse health outcomes including increased overall mortality.1 The careful study of these sleep disorders is therefore crucial in the assessment of a population's health and quality of life.
Insomnia symptoms, which include trouble falling asleep, trouble staying asleep, and early morning awakening with inability to resume sleep, is estimated to affect on average 30% of the general adult population.2 The prevalence of insomnia symptoms varies largely between reports from the adult general population, partly because of methodological differences in defining symptoms frequency and the sociodemographic characteristics of the population. For instance, the prevalence of insomnia symptoms was 19% on ≥ 3 nights/wk in Korea (age: 18–64 years, 60% females),3 21.4% often or always in Japan (age older than 20 years, 51% female),4 27.6% on ≥ 3 nights/wk in Italy (age older than 15 years, 52% female),5 27% on most nights in the United Kingdom (age 16–93 years, 50% female)6 and 32% on any night in the United States (older than 18 years, 56% female).7
Insomnia disorder, which additionally includes the presence of daytime impairment related to the nocturnal insomnia symptoms, is estimated to affect 6% to 10% of the general adult population depending on the adopted duration and comorbidi-ties criteria.2 The prevalence of insomnia disorder varies between reports from adult communities, ranging from 5.6% in France (age older than 15 years, 52% females)8 to 13.4% in Canada (average age 49 years, 51% females).9 Individuals reporting even occasional insomnia also reported poor concentration and memory impairment.10 Furthermore, insomnia is associated with increased risk of medical conditions such as cardiovascular diseases, diabetes, and arthritis.11 Insomnia has also been linked to anxiety and to the development of depression and to substance abuse and suicidal ideation. Evaluating the prevalence of insomnia in different populations is therefore important in view of the societal, psychological, and medical effects of this disorder.
Likewise, untreated sleep apnea is associated with daytime sleepiness, poor concentration,12 hypertension, stroke, and ischemic heart disease.13 The prevalence of sleep apnea risk assessed using the Berlin Questionnaire varies in different countries ranging from as low as 4.4% in Turkey14 to 33% in the Kingdom of Saudi Arabia.15
In Lebanon, data on the prevalence and effect of sleep difficulties and disorders in the general Lebanese adult population is lacking. Prior studies estimated the prevalence of poor sleep quality to range between 41% and 49%16 in Lebanese university students aged between 18 and 25 years old using the Pittsburgh Sleep Quality Index.16,17 Furthermore, the high prevalence of anxiety and depression reported in Lebanon in association with conflict and war trauma18 suggests that insomnia would also be highly prevalent in the Lebanese population. Indeed, sleep disorders are highly prevalent in Lebanese psychiatric patients with psychotic, mood, eating, and substance use disorders.19,20 However, the prevalence of insomnia and sleep apnea has not been specifically assessed in the general Lebanese adult population. A socioecological model on the determinants of sleep suggested that sleep is influenced by the interactions of individuals and their surrounding environments (physical, social, and institutional).21 Therefore, it is expected that local demographic and adverse socioeconomic factors,8 local customs22 such as late evening meals, alcohol6 and caffeine23 consumption, environmental factor such as high noise pollution24 and the prevalence of medical conditions,25 anxiety and depression,26 and anxiolytic self-prescription would influence sleep quality and disorders.
This pilot study aimed to assess the prevalence of insomnia symptoms, insomnia disorder, and sleep apnea in the Lebanese adult population, and to examine their relationship with socioeconomic, demographic, lifestyle, and health characteristics in a sample of Lebanese adults residing in Greater Beirut.
METHODS
Study Design and Sample Size
This cross-sectional study was conducted between March and May 2014 as part of the Greater Beirut Cardiovascular Cohort, a prospective observational study among a representative sample of the Lebanese adults from Greater Beirut and its suburbs. A random area multistage probability sampling was performed, stratified by the districts of Greater Beirut. The sampling methods have been previously reported.27 Individuals who reported having a mental health problem were excluded. Participants were surveyed using an investigator-administered questionnaire. The study was approved by the American University of Beirut institutional review board (IM. HT.03). Informed consent was obtained from all participants.
Data Collection and Variable Specification
Presence of sleep difficulties and insomnia were assessed using an Arabic translation of the Sleep Heart Health Study questionnaire.28 The questionnaire was translated to Arabic by a team of local experts, then backtranslated to English and piloted prior to initiating the study. Responses were integer values. Sleep apnea was assessed using the Berlin Questionnaire, a simple, and standardized questionnaire that has been validated in several languages, including Arabic.29 The Berlin Questionnaire is divided into three categories that include questions on snoring and witnessed apnea in category 1, on daytime sleepiness in category 2, and on self-reported hypertension and body mass index (BMI) in category 3. The Berlin Questionnaire was found to predict a respiratory disturbance index > 5 events/h with a sensitivity of .69 and a specificity of .84 in the general population.29
Insomnia symptoms, insomnia disorder, and sleep apnea risk were treated as dichotomous variables. Presence of insomnia symptoms was defined as having trouble falling asleep or waking up during the night with difficulty resuming sleep, or waking up too early in the morning with inability to resume sleep on most nights (16–30 nights/mo). Insomnia disorder was defined as presence of any of the insomnia symptoms (16–30 nights/mo); in addition to feeling tired or fatigued after sleep and during waking time at least 3 times/wk or having nodded off or fallen asleep while driving at least once. This definition is based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)30 and the International Classification of Sleep Disorders, Third Edition (ICSD-3).31 High risk for sleep apnea was defined as scoring positive in two or more of the three Berlin Questionnaire categories. However, low risk for sleep apnea was defined as scoring positive in fewer than two Berlin Questionnaire categories. Snoring and witness apnea more than 3 times/wk or presence of snoring that is louder than talking or that bothers other people defines a positive response in category 1. Symptoms more than 3 times/wk in two or more questions on fatigue, sleepiness, or drowsy driving defines a positive response in category 2. Self-reported hypertension or a BMI > 30 kg/m2 defines a positive response in category 3.
Other Characteristics
Other characteristics were assessed using an investigator-administered questionnaire including demographic and socioeconomic characteristics (age at the time of the interview (in years), sex, education level (below high school/high school/ university), employment status (employed/unemployed) and monthly income (< $1,000/ ≥ $1,000). Health behaviors were also assessed, including current smoking status and alcohol and caffeine consumption. Dietary intake was assessed using an 80-item semiquantitative food frequency questionnaire that estimated the frequency of consumption of each food item and the amount usually consumed over the previous year.32,33 The daily energy and macronutrient intake levels were computed using the Nutritionist Pro Software (Nutritionist Pro version 6.3.0, Axxya Systems LLC, Woodinville, Washington, United States). Physical activity was assessed using the Arabic short version of the International Physical Activity Questionnaire.34 Accordingly, total physical activity level was determined by weighting each type of activity by its energy requirements defined in MET-minutes (multiples of the resting metabolic rate for an activity multiplied by the minutes performed). Three categories of physical activity were identified, including low, moderate, and high intensity based on the calculated MET-min/wk following International Physical Activity Questionnaire criteria.35
Medical history assessment included conditions previously associated with or thought to affect sleep disorders including presence of hypertension, arthritis, diabetes, dyslipidemia, thyroid disease, coronary artery disease (CAD), chronic bronchitis or emphysema, liver disease, cancer, and stroke. CAD and later conditions were grouped in the analysis because their individual frequencies were low in our sample. Height, weight, blood pressure, and heart rate were measured at the time of the visit and BMI was calculated.
Statistical Analyses
Descriptive statistics included frequency of insomnia symptoms, insomnia disorder, snoring, and sleep apnea diagnosis and risk among study participants, and are presented for the whole sample and stratified by sex or by age categories. Participant characteristics were summarized as mean and standard deviation for continuous variables and frequency and percentage for categorical variables, and were stratified by presence of insomnia symptoms, insomnia diagnosis, or high sleep apnea risk.
Characteristics were compared between strata using chi-square test and two-sample t test to determine bivariate differences for categorical and continuous variables, respectively. Multivariate logistic regression was used to assess the determinants of sleep difficulties and sleep disorders. The dependent variables were insomnia symptoms, insomnia diagnosis, and sleep apnea. These variables were treated as dichotomous variables. Regression models included known significant bivariate predictors of sleep difficulties/insomnia in our sample. Adjusted odds ratio (OR) and a 95% confidence interval (CI) are reported. A value of P < .05 was considered to be statistically significant. All analyses were performed using IBM SPSS Version 24 (IBM Corp., Armonk, New York, United States).
RESULTS
Insomnia Symptoms
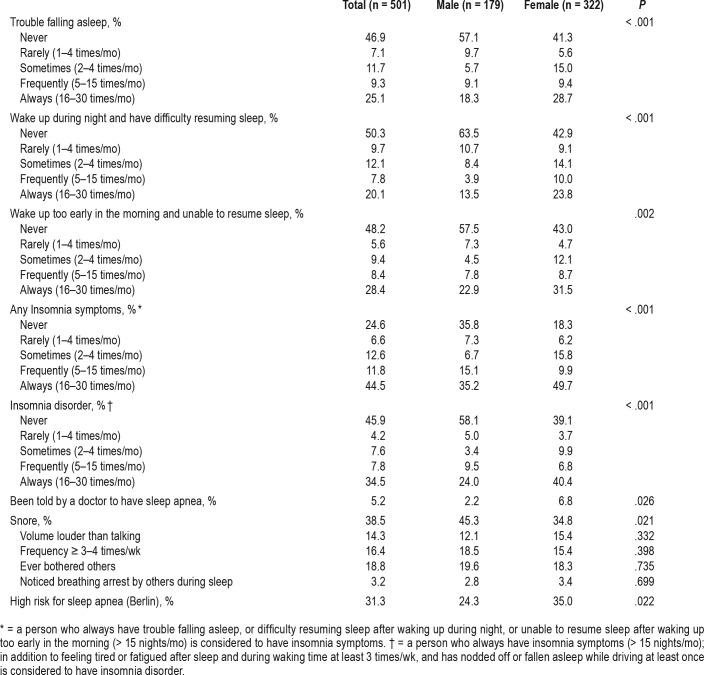
A total of 44.5% participants reported having one or more insomnia symptom regularly (> 15 nights/mo), whereas 56.3% have insomnia symptoms frequently (> 4 times/mo) and 75.4% ≥ 1 time/mo. The prevalence of regular difficulty initiating sleep, maintaining sleep, and early awakening with inability to resume sleep (> 15 nights/mo) was comparable at 25.1%, 20.1%, and 28.4%, respectively (Table 1). Overall, females were more likely than males to report regular insomnia symptoms (49.7% versus 35.2%, P < .001) including trouble initiating asleep (28.7% versus 18.3%, P < .001), trouble maintaining sleep (23.8% versus 13.5%, P < .001), and early morning awakening with inability to resume sleep (31.5% versus 22.9% P = .002) (Table 1).
Table 1.
Association of sleep problems and sex among a Lebanese sample (n = 501).
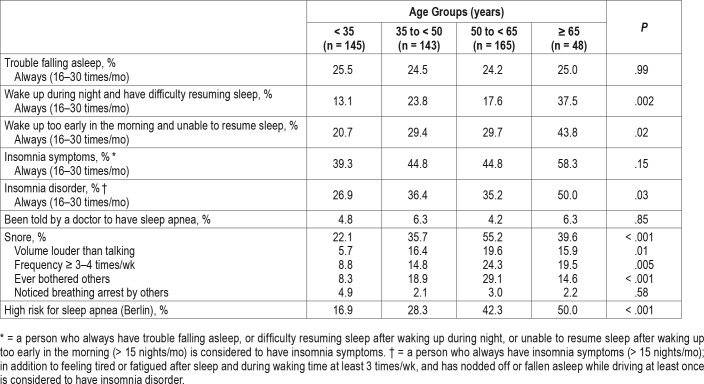
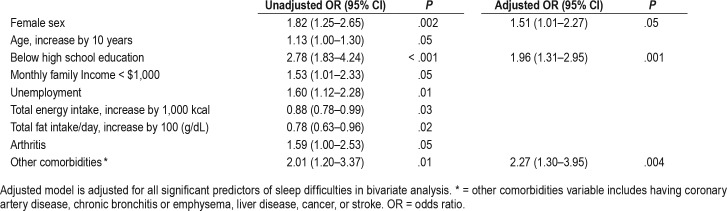
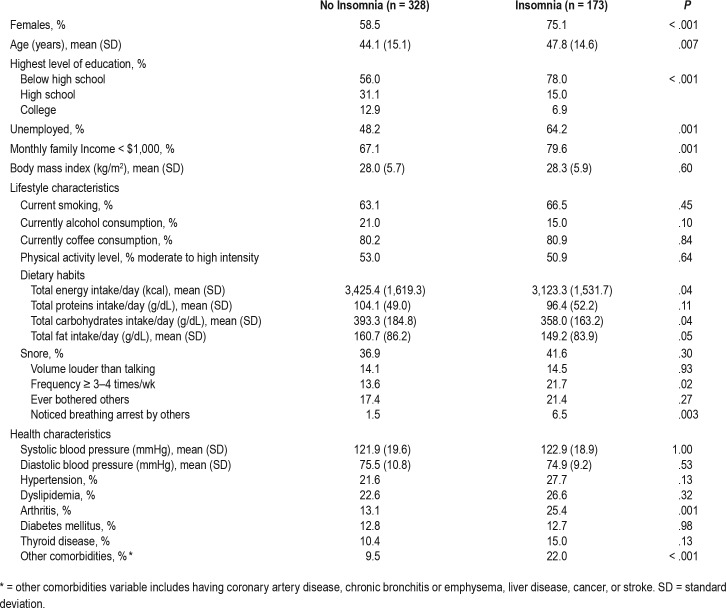
The distribution of sleep problems across different age groups is presented in Table 2, whereas demographic, lifestyle, and health characteristics of respondents with and without regular insomnia symptoms (> 15 nights/mo) are presented in Table 3. Although the difference in insomnia symptom prevalence between age groups did not reach statistical significance (58% versus 39.3% among participants older than 65 years and younger than 35 years respectively P = .15), a linear trend for increased overall insomnia symptoms prevalence across age groups was statistically significant (OR 1.13, 95% CI 1.00–1.30). Furthermore, older individuals were more likely to report difficulty maintaining sleep (37.5% versus 13.1% of individuals older than 65 years and younger than 35 years respectively, P = .002) and early morning awakening (43.8% versus 20.7% of participants older than 65 years and younger than 35 years respectively, P = .02). Female sex, age, education level below high school, unemployment, lower calorie and fat intake, arthritis, and medical comorbidities (CAD, chronic bronchitis, emphysema, liver disease, cancer, and stroke) were predictors of insomnia symptoms in bivariate analysis. However, only female sex (OR 1.51, 95% CI 1.01–2.27), education level below high school (OR 1.96, 95% CI 1.31–2.95), and presence of medical comorbidities (OR 2.27, 95% CI 1.30–3.95) remained significant predictors of insomnia symptoms in the multivariable adjusted analysis (Table 4).
Table 2.
Association between sleep problems and age group among a Lebanese sample (n = 501).
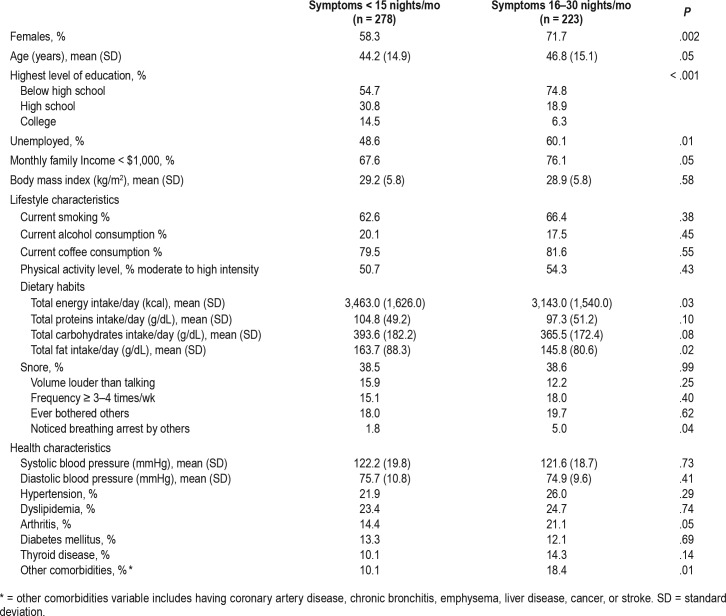
Table 3.
Associations between insomnia symptoms and demographic, lifestyle, and health characteristics among a Lebanese sample (n = 501).
Table 4.
Significant predictors of insomnia symptoms on majority of nights.
Insomnia
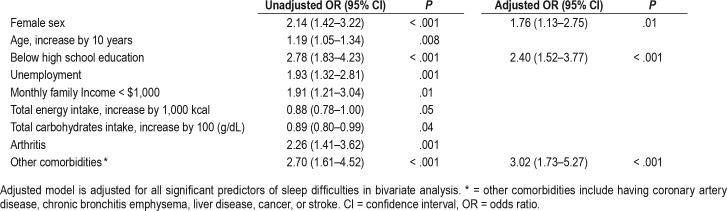
A total of 34.5% of participants reported symptoms compatible with insomnia disorder more than 15 nights/mo. Insomnia disorder was more common in females (40.4% versus 24% in males, P = .002). Insomnia disorder was also more common in older individuals (50.0% versus 26.9%, among participants older than 65 years and younger than 35 years respectively P = .03) (Table 2). Female sex, older age, education level below high school, low family income, and unemployment were significant predictors of insomnia in bivariate analysis. Insomnia was also associated with lower total energy and carbohydrate intake, arthritis, and other medical comorbidities (Table 5 and Table 6). However, similar to insomnia symptoms only female sex (OR 1.76, 95% CI 1.13–2.75) education level below high school (OR 2.40, 95% CI 1.52–3.77), and other medical comorbidities (OR 3.02, 95% CI 1.73–5.27) were significant predictors of insomnia in multivariable-adjusted analyses (Table 6).
Table 5.
Associations between insomnia disorder and demographic, lifestyle, and health characteristics among a Lebanese sample (n = 501).
Table 6.
Significant predictors of insomnia disorder.
Sleep Apnea
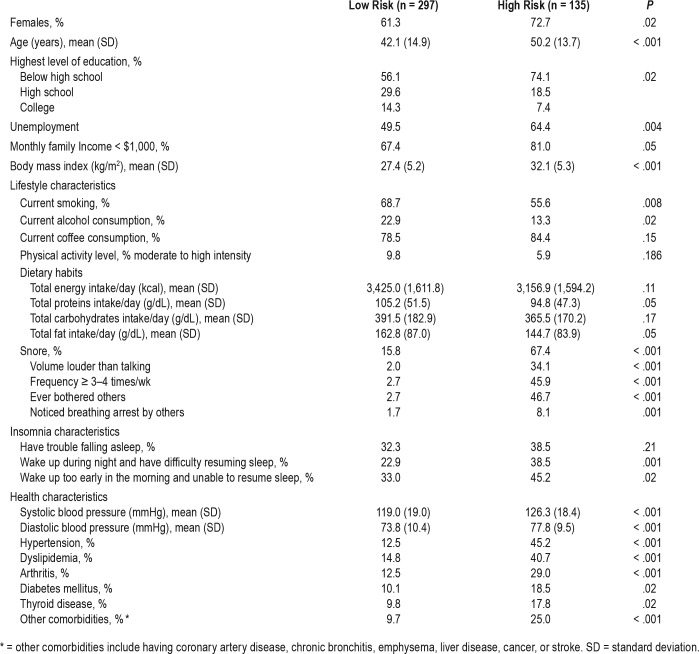
Thirty-eight percent of respondents reported habitual snoring and 31.3% were at high risk for having sleep apnea as assessed using the Berlin definition. Nevertheless, only 5.2% of participants reported a diagnosis of sleep apnea by their physician. Among individuals at high risk for sleep apnea, 34.1% reported snoring at a volume louder than talking, 46.7% have bothered others by their snoring, and 8.1% have had someone notice that they stop breathing while asleep, compared to 2% (P < .001), 2.7% (P < .001), and 1.7% (P = .001), respectively, in the low sleep apnea risk group. Forty-five percent of respondents reported feeling tired after a full night's sleep (71% in the high risk for sleep apnea group and 33% in the low risk group), and 48.1% reported feeling tired throughout the day (73% in the high risk for sleep apnea group and 37% in the low risk group). Approximately 42% of the surveyed individuals had a BMI of ≥ 30 kg/m2. The average BMI of people at high risk for sleep apnea was 32.1 ± 5.3 kg/m2, compared to 27.4 ± 5.2 kg/m2 for individuals at low risk (P < .001). In addition, symptoms of waking up during the night or early morning with inability to get back to sleep were correlated with sleep apnea (P = .001 and .02, respectively) (Table 7).
Table 7.
Associations between sleep apnea risk and demographic, lifestyle, and health characteristics among a Lebanese sample (n = 432).
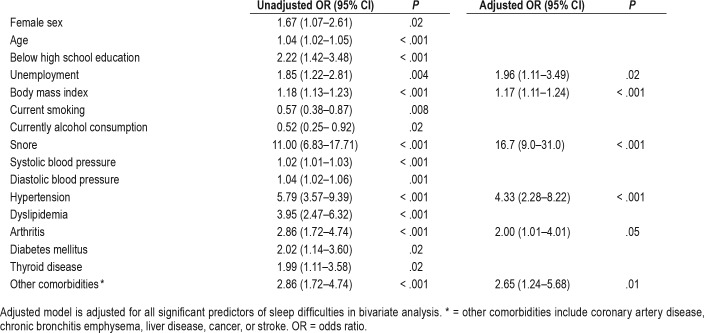
Female sex, older age, education level below high school, unemployment, BMI, blood pressure, smoking status, alcohol consumption, snoring, hypertension, dyslipidemia, arthritis, diabetes, thyroid disease, and other medical comorbidities were all significantly associated with increased sleep apnea risk in bivariate analyses. However, only unemployment (OR 1.96, 95% CI 1.11–3.47), BMI (OR 1.17, 95% CI 1.11–1.24), snoring, (OR 16.7, 95% CI 9.0–31.0) hypertension (OR 4.33, 95% CI 2.28–8.22), arthritis (OR 2.00 95% CI 1.02–4.01), and other comorbidities (OR 2.65, 95% CI 1.24–5.68), which include CAD, chronic bronchitis and emphysema, liver disease, stroke, and cancer, remained significantly associated with increased sleep apnea risk in multivariable-adjusted analyses (Table 8).
Table 8.
Significant predictors of sleep apnea risk.
DISCUSSION
This is the first epidemiological pilot study to evaluate the prevalence and correlates of sleep apnea and insomnia symptoms and disorder among the adult population in Greater Beirut, Lebanon. This study suggests that insomnia symptoms and disorder are highly prevalent in the general adult population of Lebanon, a low- to medium-income Middle Eastern country on the east coast of the Mediterranean. Since gaining independence in 1943, Lebanon has endured decades of instability due to regional conflict including a protracted civil war that lasted for 15 years, ending in the early 1990s.36 Although Lebanon is not currently at war, it remains subject to regional turmoil and political instability causing serious economic and social stress on the population.36 This is manifested through the high unemployment rate, low education level, low family income, and high levels of smoking and caffeine consumption observed in our sample, and the previously reported high levels of anxiety and depression18 and sedative-anxiolytic use and self-prescription in the Lebanese population.37 These factors could be bidirectional, contributing to the striking results observed in this study, where 44.5% of participants reported insomnia symptoms more than 15 nights/mo and 34.5% had insomnia disorder by ICSD-3 and DSM-5 criteria.
Insomnia Symptoms
The prevalence of insomnia symptoms on most nights in our sample at 44.5%, is significantly higher than previous reports from primarily developed countries where the prevalence in studies that used similar definition ranged from 19% in Korea to 27% in Italy5 and Greater Britain.6 The prevalence of insomnia symptoms on any night of 75.4% in our sample is also higher than prevalence of 50% in the adult population of neighboring Turkey.38 This high prevalence of insomnia symptoms in Lebanon may be related to the high prevalence of anxiety and depression among the Lebanese adult population.18 Another likely factor is the prevalent low education level in our sample. Other sociodemographic factors such as lower socioeconomic status and unemployment previously associated with insomnia symptoms8 were associated with insomnia symptoms in bivariate but not multivariate-adjusted analyses in our sample possibly due to colinearity with low education level and female sex. Local customs such as napping and late evening meals22 could also be contributing factors. Finally, the high level of noise pollution previously reported in Beirut is known to disturb sleep by increasing awakenings and arousals.39
The association of insomnia symptoms with chronic medical conditions after adjustment for other predictors in our sample is also consistent with prior studies. However, other previously reported predictors of insomnia symptoms such as alcohol and coffee consumption,23 and physical inactivity6 were not predictors of sleep difficulties in our sample; however, arthritis40 was associated with sleep difficulties in our sample in bivariate but not in multivariable-adjusted analyses.
We found a linear trend but no significant difference in the prevalence of insomnia symptoms or difficulty initiating sleep across age groups; however, difficulty maintaining sleep and early morning awakening were significantly more common among older individuals, findings consistent with the literature.41 The higher prevalence of insomnia symptoms, including difficulty initiating and maintaining sleep and early morning awakening among women, is also a finding consistent with the literature.8 This could be explained by a higher prevalence of socioeconomic predictors of insomnia symptoms among Lebanese females in our sample including low education status, unemployment, and low family income. The higher prevalence of undiagnosed anxiety and depression among females in the Lebanese population could also be contributing to the higher prevalence of insomnia in Lebanese women.18
Insomnia Disorder
The prevalence of insomnia disorder in our study (34.5%) is also much higher than previously reported in studies from other countries that used the DSM-IV definition of insomnia, which ranges from 5.6% in France, (older than 15 years, 52% females),8 up to 13.4% in Canada (average age 49 years, 51% females). A nationwide survey from neighboring Turkey also reported a lower prevalence of 12.2% in the general adult population (older than 18 years, 52% females).38 Studies from neighboring Arab countries evaluated the prevalence of insomnia in specific populations including adolescents,42 the elderly,43 medical students,44 and patients with renal failure45 and liver cirrhosis.46 One study that reported a very high prevalence of insomnia symptoms of 91.6% and insomnia diagnosis of 77.7% in the Saudi population included hospital employees and blood bank donors from a single medical center and did not specify the frequency or duration of symptoms.47
Insomnia was previously linked to female sex, marital status,8 low educational and low income level,7 unemployment,6 and presence of chronic physical illness and psychiatric disorders.48 Similarly, female sex, education level below high school, and the presence of chronic medical conditions (including CAD, chronic bronchitis, emphysema, cancer, stroke, and liver disease) were associated with insomnia in our study. However, similar to insomnia symptoms older age, low family income and unemployment were significant predictors of insomnia disorder in bivariate but not in multivariable-adjusted analyses; this finding was likely due to colinearity of these variables with low education status and presence of medical comorbidi-ties. This is consistent with prior literature suggesting that the higher prevalence of sleep disturbance in the elderly is partly explained by the higher prevalence of health conditions and social factors rather than due to aging.49 The high prevalence of insomnia disorder in females could also be partly explained by the higher prevalence of socioeconomic predictors of insomnia disorder such as low education status among females in our sample and the higher prevalence of undiagnosed anxiety and depression among females in the Lebanese population.18
The high prevalence of anxiety and mood disorders in Lebanon, estimated at 16.7% and 12.6% respectively18 compared to other countries, has been associated with war and exposure to war trauma,18 and might explain the high prevalence of insomnia in our study. The high prevalence of unemployment and low educational levels in our sample have also been associated with the tumultuous geopolitical conditions of the country50 and are also potentially important factors contributing to the high prevalence of insomnia.4,7 Furthermore, the high noise pollution previously reported in Greater Beirut, which is 65–79 dBA, higher than levels recommended by the World Health Organization (45–55 dBA),24 could also be contributing.39 Finally, the high levels of sedative-anxiolytic use and self-medication reported in 43% and 22% of the Lebanese population, respectively, could be bidirectionally associated with insomnia.37
Sleep Apnea
The prevalence of sleep apnea determined using the Berlin Questionnaire (33.3% of our sample) was higher than previously reported in other studies around the world using similar methods.14,51–55 A similarly high prevalence of sleep apnea was reported in Saudi males15 and females56 in primary care clinics; however, the prevalence was significantly lower at 4.4% in neighboring Turkey (average age 43, 0% females).14 Other studies from the region also reported lower but variable prevalence of sleep apnea of 5% in a sample of 3,600 Iranians (average age 39 years, 53% female),51 27.3% in an older sample of 527 Iranians with fewer females (average age 49 years, 12% females)52 and 10% to 12.5% in Pakistan (average age 32 years, 21% females).53 In comparison, the prevalence was 26% in the United States (average age 49 years, 51% female).54 Similar to our findings, sleep apnea risk in these studies was associated with high BMI, disadvantaged socioeconomic status such as low educational status and low income, and chronic medical conditions. The difference in the prevalence of sleep apnea in these studies could be attributed to variability in demographic factors, although ethnic/racial variances could also be contributing, as craniofacial morphology is an important predictor of sleep apnea risk differs across races.57
In our study, BMI was the most significant predictor for sleep apnea risk; with every unit increase in BMI, an individual's odds of being in the high versus low risk sleep apnea category increase by 17% (OR 1.17, 95% CI 1.11–1.24, P < .001) (Table 8). Participants who snore constituted 67.4% of the individuals at high risk for sleep apnea, and only 15.8% of those at low risk for sleep apnea (P < .001). In addition, hypertension was five times more prevalent among individuals at risk for sleep apnea (P < .001). Insomnia symptoms such as waking up during the night or early in the morning and being unable to go back to sleep were more common in individuals at high risk for sleep apnea, suggesting possible comorbidity of the two sleep disorders.58 The bivariate association of female sex with elevated sleep apnea risk became nonsignificant in multivariable analyses, suggesting that the higher prevalence of sleep apnea risk among females at 35% versus 24% in males is likely attributed to other independent risk factors of sleep apnea. Indeed, the average BMI in our sample was higher in females compared with males (29.7 ± 6.0 versus 28.0 ± 5.2 kg/m2 respectively, P = .002). Similarly, a high prevalence of sleep apnea risk was reported among females in Saudi Arabia, and was attributed to the high prevalence of obesity among Saudi females.56
The prevalence of physician-diagnosed sleep apnea in our sample was much lower than the prevalence estimated using the Berlin Questionnaire across all age groups and in both males and females, suggesting that sleep apnea is significantly underrecognized. Likewise, sleep apnea was underdiagnosed in population studies from the United States.59 Because Lebanon is a developing country with limited resources, screening for sleep apnea may not be a priority for the treating physician and awareness about sleeping disorders among patients may be poor,60 leading to the underdiagnosis of sleep apnea in our population.
This study is limited by the cross-sectional design that does not allow determination of the direction of association and causality. The reliance on self-reported data could be biased, driven by the desire to appear normal or to express dissatisfaction or recall biases. Furthermore, although individuals with self-reported mental health problems were excluded, assessment of undiagnosed depression and anxiety, two determinants of sleep disorders, are lacking, thus limiting the interpretation of our findings. Finally, the use of the Berlin Questionnaire also warrants caution when attempting to accurately assess the clinical diagnosis of sleep apnea. The Berlin Questionnaire is an inexpensive and quick screening tool for the diagnosis of sleep apnea in the general population, with a sensitivity of .69 and a specificity of .84, in the population.61 Although, polysomnography remains the gold standard for accurately diagnosing sleep apnea, it is not an optimal screening tool because of the associated cost and procedure duration. Strengths of this study that balance out these limitations include the evaluation of a well-characterized community-based sample, the adoption of systematic sampling methods with face-to-face interview, and the novelty of evaluating insomnia in a developing country in an area of ongoing conflict and suggesting a link between sleep disorders and geopolitical conditions.
In conclusion, this study suggests that sleep difficulties and disorders including insomnia and sleep apnea are highly prevalent in Lebanon compared to other countries, especially among women and individuals with disadvantaged socioeconomic status. Furthermore, sleep apnea seems to be significantly underdiagnosed. The high prevalence of anxiety in the Lebanese population,18 and the high rates of unemployment and low education status, especially among women,50 are likely important contributors to the high prevalence of insomnia symptoms and disorder. These factors are accentuated by the political and economic instability, recent wars, and inability of Lebanese societal and economic system to cope with the spillover from regional wars.36 These findings are alarming and their implications important because of the well-known negative effect of sleep disorders on the health and well-being of the population,1 thus suggesting the need for strengthened screening in primary care settings and increasing awareness of sleep health and disorders among health professionals and the public. Further multinational comparative research that objectively assess the causes and implications of sleep disorders in developing countries, especially those subject to conflicts, wars, and political and economic turmoil are needed to evaluate the implications of these factors on sleep health and disorders and the overall well-being of affected individuals. A larger scale follow-up study further examining the effect of mental health issues, local customs (napping/late evening meals), and expectations about sleep, as well as environmental factors such as noise pollution, is also recommended.
DISCLOSURE STATEMENT
Work for this study was performed at the American University of Beirut. All authors have seen and approved the manuscript. This work was supported by the medical practice plan grants at the American University of Beirut and the Lebanese National Council for Scientific Research. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors acknowledge the contribution of the following volunteer students under the Medical Research Volunteer Program (MRVP) at the American University of Beirut: Michael Dagher, Abdulhamid Sabih, Lama Assi, Muhieddine Laban, Hisham Wehbe, Alaa Osta, Carine Baassiri, and Ali Jaber. Moreover, we thank Juliana Breidy, Patricia Moghames, Joanna Bou Rizk, Christelle Cordahi, Zeinab Awada, Aya Noubani, Lara Itani, and Mohamad Medawar for their contribution in data collection and Maha Makki for her contribution to data analysis.
ABBREVIATIONS
- BMI
body mass index
- CAD
coronary artery disease
- CI
confidence interval
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ICSD
International Classification of Sleeping Disorders
- OR
odds ratio
REFERENCES
- 1.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12(4):289–298. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 3.Kim B-S, Jeon HJ, Hong JP, et al. DSM-IV psychiatric comorbidity according to symptoms of insomnia: a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. 2012;47(12):2019–2033. doi: 10.1007/s00127-012-0502-0. [DOI] [PubMed] [Google Scholar]
- 4.Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep. 2000;23(1):41–47. [PubMed] [Google Scholar]
- 5.Ohayon M, Smirne S. Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med. 2002;3(2):115–120. doi: 10.1016/s1389-9457(01)00158-7. [DOI] [PubMed] [Google Scholar]
- 6.Groeger JA, Zijlstra F, Dijk DJ. Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some 2000 British adults. J Sleep Res. 2004;13(4):359–371. doi: 10.1111/j.1365-2869.2004.00418.x. [DOI] [PubMed] [Google Scholar]
- 7.Bixler EO, Kales A, Soldatos CR, Kales JD, Healey S. Prevalence of sleep disorders in the Los Angeles metropolitan area. Am J Psychiatry. 1979;136(10):1257–1262. doi: 10.1176/ajp.136.10.1257. [DOI] [PubMed] [Google Scholar]
- 8.Ohayon M. Epidemiological study on insomnia in the general population. Sleep. 1996;19(suppl_3):S7–S15. doi: 10.1093/sleep/19.suppl_3.s7. [DOI] [PubMed] [Google Scholar]
- 9.Morin CM, LeBlanc M, Bélanger L, Ivers H, Mérette C, Savard J. Prevalence of insomnia and its treatment in Canada. Can J Psychiatry. 2011;56(9):540–548. doi: 10.1177/070674371105600905. [DOI] [PubMed] [Google Scholar]
- 10.Ancoli-Israel S. Sleep and its disorders in aging populations. Sleep Med. 2009;10(Suppl 1):S7–S11. doi: 10.1016/j.sleep.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 11.Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behav Sleep Med. 2003;1(4):227–247. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- 12.Abramson Z, Susarla SM, Lawler M, Bouchard C, Troulis M, Kaban LB. Three-dimensional computed tomographic airway analysis of patients with obstructive sleep apnea treated by maxillomandibular advancement. J Oral Maxillofac Surg. 2011;69(3):677–686. doi: 10.1016/j.joms.2010.11.037. [DOI] [PubMed] [Google Scholar]
- 13.Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2014;(1):CD007736. doi: 10.1002/14651858.CD007736.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Kart L, Dutkun Y, Altın R, Ornek T, Kıran S. Prevalence of major obstructive sleep apnea syndrome symptoms in coal miners and healthy adults. Tuberk Toraks. 2010;58(3):261–267. [PubMed] [Google Scholar]
- 15.BaHammam AS, Alrajeh MS, Al-Jahdali HH, BinSaeed AA. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi males in primary care. Saudi Med J. 2008;29(3):423. [PubMed] [Google Scholar]
- 16.Assaad S, Costanian C, Haddad G, Tannous F. Sleep patterns and disorders among university students in Lebanon. J Res Health Sci. 2014;14(3):198–204. [PubMed] [Google Scholar]
- 17.Kabrita CS, Hajjar-Muça TA, Duffy JF. Predictors of poor sleep quality among Lebanese university students: association between evening typology, lifestyle behaviors, and sleep habits. Nat Sci Sleep. 2014;6:11–18. doi: 10.2147/NSS.S55538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karam EG, Mneimneh ZN, Dimassi H, et al. Lifetime prevalence of mental disorders in Lebanon: first onset, treatment, and exposure to war. PLoS Med. 2008;5(4):e61. doi: 10.1371/journal.pmed.0050061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Talih F, Ajaltouni J, Kobeissy F. Restless leg syndrome in hospitalized psychiatric patients in Lebanon: a pilot study. Neuropsychiatr Dis Treat. 2016;12:2581–2586. doi: 10.2147/NDT.S116271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Talih F, Ajaltouni J, Tamim H, Kobeissy F. Risk of obstructive sleep apnea and excessive daytime sleepiness in hospitalized psychiatric patients. Neuropsychiatr Dis Treat. 2017;13:1193–1200. doi: 10.2147/NDT.S131311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson CL, Redline S, Emmons KM. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health. 2015;36:417–440. doi: 10.1146/annurev-publhealth-031914-122838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schenck CH, Mahowald MW, Sack RL. Assessment and management of insomnia. JAMA. 2003;289(19):2475–2479. doi: 10.1001/jama.289.19.2475. [DOI] [PubMed] [Google Scholar]
- 23.Satti GM, Alsaaid HF, Nabil NM, Saeed AA, AlHamdan N, El-bakri NK. The prevalence of sleep problems and its impact on sleep quality and academic performance. Merit Research Journal of Education and Review. 2015;3(2):126–131. [Google Scholar]
- 24.Korfali SI, Massoud M. Assessment of community noise problem in greater Beirut area, Lebanon. Environ Monit Assess. 2003;84(3):203–218. doi: 10.1023/a:1023322507415. [DOI] [PubMed] [Google Scholar]
- 25.Katz DA, McHorney CA. The relationship between insomnia and health-related quality of life in patients with chronic illness. J Fam Pract Title. 2002;51(3):229–234. [PubMed] [Google Scholar]
- 26.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30(2):213–218. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 27.Nasrallah MP, Nakhoul NF, Nasreddine L, et al. Prevalence of diabetes in greater Beirut area: worsening over time. Endocr Pract. 2017;23(9):1091–1100. doi: 10.4158/EP171876.OR. [DOI] [PubMed] [Google Scholar]
- 28.Quan SF, Howard BV, Iber C, et al. The sleep heart health study: design, rationale, and methods. Sleep. 1997;20(12):1077–1085. [PubMed] [Google Scholar]
- 29.Saleh ABM, Ahmad MA, Awadalla N. Development of Arabic version of Berlin questionnaire to identify obstructive sleep apnea at risk patients. Ann Thorac Med. 2011;6(4):212. doi: 10.4103/1817-1737.84775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association Publishing; 2013. [Google Scholar]
- 31.Sateia MJ. International Classification of Sleep Disorders-Third Edition. Chest. 2014;146(5):1387–1394. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 32.Nasreddine L, Hwalla N, Sibai A, Hamze M, Parent-Massin D. Food consumption patterns in an adult urban population in Beirut, Lebanon. Public Health Nutr. 2006;9(2):194–203. doi: 10.1079/phn2005855. [DOI] [PubMed] [Google Scholar]
- 33.Naja F, Nasreddine L, Itani L, et al. Dietary patterns and their association with obesity and sociodemographic factors in a national sample of Lebanese adults. Public Health Nutr. 2011;14(9):1570–1578. doi: 10.1017/S136898001100070X. [DOI] [PubMed] [Google Scholar]
- 34.International Physical Activity Questionnaire website. Downloadable questionnaires. [Accessed March 20, 2019]. https://sites.google.com/site/theipaq/questionnaire_links.
- 35.International Physical Activity Questionnaire website. IPAQ scoring protocol. [Accessed March 20, 2019]. https://sites.google.com/site/theipaq/scoring-protocol.
- 36.BBC website. Lebanon profile - Timeline. [Accessed March 20, 2019]. www.bbc.com/news/world-middle-east-14649284. Published April 25, 2018.
- 37.Naja W, Pelissolo A, Haddad R, Baddoura R, Baddoura C. A general population survey on patterns of benzodiazepine use and dependence in Lebanon. Acta Psychiatr Scand. 2000;102(6):429–431. doi: 10.1034/j.1600-0447.2000.102006429.x. [DOI] [PubMed] [Google Scholar]
- 38.Benbir G, Demir AU, Aksu M, et al. Prevalence of insomnia and its clinical correlates in a general population. Neuropsychiatry Clin Neurosci. 2015;69(9):543–552. doi: 10.1111/pcn.12252. [DOI] [PubMed] [Google Scholar]
- 39.Janssen S, Basner M, Griefahn B, Miedema H, Kim R World Health Organization Regional Office for Europe. Burden of disease from environmental noise: Quantification of healthy life years lost in Europe. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2011. Environmental noise and sleep disturbance; pp. 55–70. [Google Scholar]
- 40.Katz DA, McHorney CA. Clinical correlates of insomnia in patients with chronic illness. Arch Intern Med. 1998;158(10):1099–1107. doi: 10.1001/archinte.158.10.1099. [DOI] [PubMed] [Google Scholar]
- 41.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 42.Abdel-Khalek AM. Prevalence of reported insomnia and its consequences in a survey of 5,044 adolescents in Kuwait. Sleep. 2004;27(4):726–731. doi: 10.1093/sleep/27.4.726. [DOI] [PubMed] [Google Scholar]
- 43.Ayoub AI, Attia M, El Kady HM, Ashour A. Insomnia among community dwelling elderly in Alexandria, Egypt. J Egypt Public Health Assoc. 2014;89(3):136–142. doi: 10.1097/01.EPX.0000456621.42258.79. [DOI] [PubMed] [Google Scholar]
- 44.Siddiqui AF, Al-Musa H, Al-Amri H, Al-Qahtani A, Al-Shahrani M, Al-Qahtani M. Sleep patterns and predictors of poor sleep quality among medical students in King Khalid University, Saudi Arabia. Malays J Med Sci. 2016;23(6):94–102. doi: 10.21315/mjms2016.23.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ibrahim JM, Wegdan OM. Epidemiology of sleep disorders in patients with chronic renal disease in Cairo, Egypt. J Egypt Public Health Assoc. 2011;86(3–4):68–72. doi: 10.1097/01.EPX.0000399136.00486.4e. [DOI] [PubMed] [Google Scholar]
- 46.AL-Jahdali H, Al Enezi A, Anwar AE, et al. Prevalence of insomnia and sleep patterns among liver cirrhosis patients. J Circadian Rhythms. 2014;12:2. [Google Scholar]
- 47.Ahmed AE, Al-Jahdali H, Fatani A, et al. The effects of age and gender on the prevalence of insomnia in a sample of the Saudi population. Ethn Health. 2017;22(3):285–294. doi: 10.1080/13557858.2016.1244624. [DOI] [PubMed] [Google Scholar]
- 48.Sivertsen B, Lallukka T, Salo P, et al. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res. 2014;23(2):124–132. doi: 10.1111/jsr.12102. [DOI] [PubMed] [Google Scholar]
- 49.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: Results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56(5):497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 50.World Bank Group. Lebanon: Promoting Poverty Reduction and Shared Prosperity: A Systematic Country Diagnostic. Washington, DC: World Bank Group; 2015. [Google Scholar]
- 51.Amra B, Farajzadegan Z, Golshan M, Fietze I, Penzel T. Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath. 2011;15(3):425–429. doi: 10.1007/s11325-010-0353-4. [DOI] [PubMed] [Google Scholar]
- 52.Khazaie H, Naja F, Rezaie L, Tahmasian M, Sepehry AA, Herth FJ. Prevalence of symptoms and risk of obstructive sleep apnea syndrome in the general population. Arch Iran Med. 2011;14(5):335–338. [PubMed] [Google Scholar]
- 53.Taj F, Aly Z, Arif O, Khealani B, Ahmed M. Risk for sleep apnea syndrome in Pakistan: a cross-sectional survey utilizing the Berlin questionnaire. Sleep Breath. 2009;13(1):103–106. doi: 10.1007/s11325-008-0220-8. [DOI] [PubMed] [Google Scholar]
- 54.Hiestand DM, Britz P, Goldman M, Phillips B. Prevalence of symptoms and risk of sleep apnea in the US population. Chest. 2006;130(3):780–786. doi: 10.1378/chest.130.3.780. [DOI] [PubMed] [Google Scholar]
- 55.Faria AC, da Costa CH, Rufino R. Sleep apnea clinical score, Berlin Questionnaire, or Epworth Sleepiness Scale: which is the best obstructive sleep apnea predictor in patients with COPD? Int J Gen Med. 2015;8:275–281. doi: 10.2147/IJGM.S86479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bahammam AS, Al-Rajeh MS, Al-Ibrahim FS, Arafah MA, Sharif MM. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi women in primary care. Saudi Med J. 2009;30(12):1572–1576. [PubMed] [Google Scholar]
- 57.Cakirer B, Hans MG, Graham G, Aylor J, Tishler PV, Redline S. The relationship between craniofacial morphology and obstructive sleep apnea in whites and in African-Americans. Am J Respir Crit Care Med. 2001;163(4):947–950. doi: 10.1164/ajrccm.163.4.2005136. [DOI] [PubMed] [Google Scholar]
- 58.Luyster FS, Buysse DJ, Strollo PJ., Jr Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196–204. [PMC free article] [PubMed] [Google Scholar]
- 59.Kapur V, Strohl KP, Redline S, Iber C, O'Connor G, Nieto J. Underdiagnosis of sleep apnea syndrome in US communities. Sleep Breath. 2002;6(2):49–54. doi: 10.1007/s11325-002-0049-5. [DOI] [PubMed] [Google Scholar]
- 60.Altevogt BM, Colten HR. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 61.Senaratna CV, Perret JL, Matheson MC, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2017;36:116–124. doi: 10.1016/j.smrv.2017.04.001. [DOI] [PubMed] [Google Scholar]