Abstract
Study Objectives:
This study aimed to explore the effects of a single bout of light-intensity walking on sleep in older women with mild sleep impairment.
Methods:
A total of 40 women aged 55 years or older with mild sleep impairment were randomized to either a treadmill walking session for 50 minutes or a quiet-rest control. All participants completed the study (mean age: 60.4 ± 4.7 years). Sleep quality was assessed by ActiGraph for 2 nights before (pretest) and 2 nights after exercise (posttest). A mixed-design analysis of variance was used with group as the between-subjects factor and time point as the within-subjects factor.
Results:
No significant group difference in demographic variables, body mass index, physical and mental status, and eight sleep parameters were observed at baseline. Significant group-time interactions existed for sleep latency (P < .001) and sleep efficiency (P = .025). After the intervention, the walking group reduced sleep latency by 3.3 minutes (P = .001) and also had greater sleep efficiency (increase 3.8%, P = .008), but no significant change was found in the control group. No significant group-time interactions were present for the other six sleep parameters (activity counts, total sleep time, wake after sleep onset, number and length of awakenings, or time in bed).
Conclusions:
A single session of light-intensity walking led to a modest reduction in sleep latency and improvement of sleep efficiency in older women with mild sleep impairment.
Citation:
Chen LJ, Stevinson C, Fang SH, Taun CY, Ku PW. Effects of an acute bout of light-intensity walking on sleep in older women with sleep impairment: a randomized controlled trial. J Clin Sleep Med. 2019;15(4):581–586.
Keywords: elderly, insomnia, physical activity, sleep disorder, walking
BRIEF SUMMARY
Current Knowledge/Study Rationale: Previous research tended to focus on the effects of moderate- or high-intensity exercise on sleep and has been generally limited to good sleepers. This study aimed to explore the effects of a single bout of light-intensity walking on sleep in older women with mild sleep impairment.
Study Impact: Light-intensity walking can lead to modest benefits in sleep latency and efficiency in older women with sleep impairment. A single session of exercise is more effective for sleep initiation than for sleep maintenance among older adults.
INTRODUCTION
Sleep impairment is a common problem among older adults.1,2 It has been estimated that more than one-third of older adults have insomnia symptoms, with women more likely to report sleep difficulties than men.3 Associations between sleep impairment and deleterious health outcomes have been established, including increased risk of mortality,4 diabetes,5 metabolic syndrome,6 dementia,7,8 depression, and anxiety,9 as well as impaired quality of life.10
By contrast, exercise has a range of health benefits, such as reducing risk factors for cardiovascular disease and diabetes11,12 and improving mental well-being.13 Additionally, several reviews suggest that exercise is effective for improving sleep quality and reducing sleep complaints.14–20 However, much of this research is based on samples of good sleepers, limiting the scope for improvement because of ceiling and floor effects.15,17,18,21
Exercise intensity may be one of the important contributing factors to the sleep response.17 Previous research tended to focus on the effects of moderate- or high-intensity exercise on sleep outcomes.22–25 A review examining exercise training effects on sleep quality in middle-aged and older adults showed that all aerobic exercise programs were of moderate intensity.16 Another review reported similar results with few studies adopting light-intensity exercise program.14 Furthermore, inconsistent results have been reported from those trials that have examined light-intensity exercise in older adults.26–28
Mode of exercise may also affect the sleep outcome, but no single exercise type has been identified as optimal.14,17 Walking is an accessible and common physical activity for older adults,29 offering a convenient low- cost form of exercise that can be incorporated into everyday life with minimal injury risk or other adverse effects.11,30,31 Research has shown benefits of walking on sleep in a longitudinal study32 and after a 4-week walking program among older adults, though intensity was not recorded.30
In addition to the benefits demonstrated for regular exercise, there is evidence of acute improvements in sleep after single exercise bouts.14 However, these studies largely involved younger healthy adults performing moderate to vigorous intensity exercise. There is a paucity of research on the effects of a single bout of light-intensity exercise on the sleep of older adults with sleep impairment. Because poor sleep quality is a significant public health issue33 and walking is an accessible exercise option, this study explored the effects of a single session of light-intensity walking on sleep outcomes in older women with sleep impairment.
METHODS
Participants
Potential participants were recruited from two communities in central Taiwan by telephone with the help of community organizers. Only women were recruited in this study because previous research indicates more sleep difficulties in females than in males. Those who were interested in the study were invited to attend an orientation meeting if they met the following eligibility criteria: age 55 years or older; without cognitive impairment; able to communicate; reporting poor sleep quality; not taking sleep/psychotropic medications; no clinical diagnosis of sleep apnea or other sleep disorder; and not exercising regularly (ie, more than twice per week). Forty-five older women participated in the preliminary meeting, at which the researchers described the study purpose, procedure, and the exercise program and rest condition. These potential participants completed the Physical Activity Readiness Questionnaire (PAR-Q) and initial sleep assessments. The PAR-Q is a simple self-administered health questionnaire to examine the safety or possible risk of exercising for individuals based on their health conditions.34 Participants who answered yes to one or more PAR-Q questions were excluded. The initial sleep assessment was made through the Chinese version of the self-reported 5-item Athens Insomnia Scale (AIS-5).35 This study aimed to examine the effects of a single session of exercise among individuals with less than optimal sleep quality; thus, individuals who scored above 5 on the AIS-5 were included in the study.32 Among the 45 potential participants, 3 did not meet the criteria and 2 decided not to attend the study because they could not accommodate the schedule, resulting in a sample size of 40. These participants signed consent forms and were assigned a number from 1 to 40. A simple randomization method was used to randomize participants into two groups using Microsoft Excel 2016 (Microsoft, Redmond, Washington, United States). They were randomly assigned to either a treadmill walking session (n = 20) or a quiet-rest control (n = 20). All participants were aware of their group assignment. Participants who attended the study were rewarded with TWD 400 (approximately USD 14). All participants completed the study. Previous research has indicated a minimum of 12 participants per group is able to detect a small effect size of physical activity on sleep outcome with setting beta at 20% and alpha at 5%.36 The study was approved by the institutional review board of Antai Medical Care Corporation Antai Tian-Sheng Memorial Hospital, Taiwan.
Intervention
Participants were asked to walk on a treadmill at light intensity for 50 minutes (10 minutes of warm-up, 30 minutes of walking at 45% to 55% of age-predicted maximal heart rate (MaxHR), and 10 minutes of cool-down) in the afternoon. Walking speed was adjusted to maintain heart rate at target levels. The speed of the treadmill was between 3.0–4.2 km/h and the Rate of Perceived Exertion Scale (10-point scale) indicated a self-reported exercise-intensity level ranging from 3 to 4. The mean heart rates before, during, and 10 minutes after exercise were 74.15, 90.25, and 75.75, respectively, measured by a wrist-worn heart rate monitor (Fenix 3 HR, Garmin, Olathe, Kansas, United States). Each treadmill session was performed individually and was supervised by a certified instructor. Sessions were scheduled on Wednesdays between the hours of 2:00 pm and 4:00 pm. Members of the control group attended at the same times of day. They were instructed to sit quietly on their own during this period in a separate room where water, books, newspapers, and magazines were available and were accompanied by a research assistant.
Measures of Sleep
Participants wore a wrist ActiGraph (wActiSleep, Pensacola, Florida, United States) on the nondominant hand for 4 nights from Monday to Thursday. The means of measurements taken for 2 nights before and 2 nights after the exercise session were used as pretest and posttest data, respectively. The sleep data were obtained from ActiGraph monitors and analyzed by ActiLife software version 6 using the Cole-Kripke algorithm, including eight sleep indices (sleep latency, total counts, sleep efficiency, total sleep time [TST], wake after sleep onset [WASO], number of awakenings, length of awakenings, time in bed).22,37 Participants also recorded the time they went to bed and woke up in the morning to enable coordinate checks with the actigraphic data.
Participants self-reported age, marital status, years of schooling, average napping time, smoking, alcohol consumption, and chronic diseases. Mental health was assessed with the Satisfaction with Life Scale.22 Height and weight were measured from which body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters (kg/m2). Resting systolic/diastolic blood pressure was measured by an automated machine (Hartmann Tensoval Comfort, Germany). Hand grip tests were performed with the dominant hand using a digital straingauge hand dynamometer (Takei TKK 5401, Takei Scientific Instruments, Tokyo, Japan)6 with the mean scores (lb) of two tests recorded as the measures of muscle strength.
Data Analyses
Descriptive statistics were calculated for exercise and control groups. Tests were performed (t tests or χ2 tests) to test for differences at baseline between the two groups. A 2 × 2 mixed-design analysis of variance with repeated measures was used to examine the effects of the intervention. The between-subjects factor was group (exercise group and control group) and the within-subjects factor was time point (pretest and posttest assessments for each sleep index). If significant interactions were found, simple effects of time within each group were examined. The level of significance was set at .05 for all statistical analyses which were performed with SPSS statistics version 22 (IBM, Armonk, New York, United States).
RESULTS
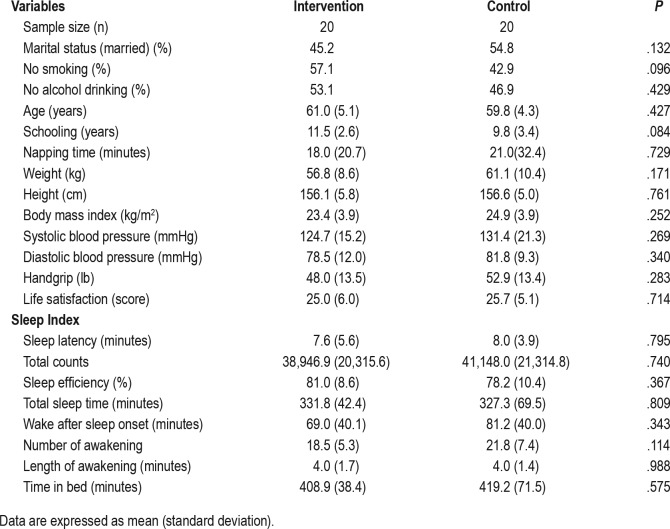
Table 1 shows the baseline characteristics of participants. Briefly, participants had a mean age of 60.4 (± 4.7), a mean BMI of 24.1 (± 3.9) kg/m2, and mean systolic blood pressure of 128.1 (± 18.5) mmHg. There were no significant differences between the two groups at baseline on demographic variables (age, years of schooling, marital status, smoking, alcohol consumption, and average napping time), physical status (BMI, blood pressure, and muscle strength), or mental well-being (life satisfaction).
Table 1.
Baseline characteristics of participants in intervention and control groups.
Based on the 2-day actigraphy monitoring before exercise, there were also no significant differences on any of the sleep indices between the intervention and control groups at baseline. Overall TST was short at 329.5 (± 56.9) minutes, although greater variation was noted among the control group. Mean sleep efficiency was 79.6 (± 9.5) % placing this sample in the poor sleep range since a sleep efficiency of 85% or more is regarded as normal.22,37 As often seen in this population, sleep maintenance was more problematic than sleep initiation, with a mean time for WASO of 75.1 (± 39.9) minutes.
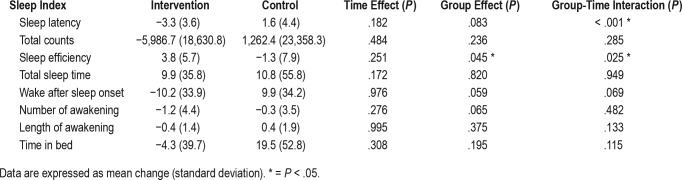
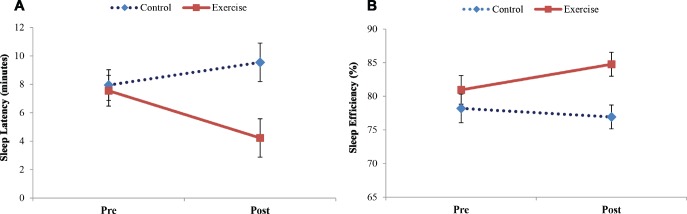
Results of the analysis of variance and the mean changes in sleep parameters pretest to posttest in each group are presented in Table 2. A significant group × time interaction was noted in sleep latency (F1,38 = 15.062, P < .001, partial eta squared = .284). To break down the interaction, the simple effect of time within each group was tested. After the intervention, the walking group had significantly reduced sleep latency from pretest to posttest by 3.3 minutes (P = .001) whereas the control group increased sleep latency by 1.6 minutes (P = .120). The interaction graph reveals a mean difference of 5.3 minutes in sleep latency between the two groups at posttest (Figure 1).
Table 2.
Results of the analysis of variance and mean changes in sleep outcomes pretest to posttest between groups.
Figure 1. Sleep latency and sleep efficiency between groups by time.
Sleep latency (A) and sleep efficiency (B) between groups by time.
A significant group difference was seen in sleep efficiency (F1,38 = 4.287, P = .045, partial eta squared = .101) and it was qualified by a significant group × time interaction (F1,38 = 5.453, P = .025, partial eta squared = .125). Probing the interaction revealed that the walking group reported a significant increase in sleep efficiency from pretest to posttest (increase 3.8%, P = .008), but the control group had a 1.3% decrease in sleep efficiency (P = .480). The interaction graph shows a mean difference of 7.8% in sleep efficiency at posttest between the two groups (Figure 1).
No significant main effects or interactions for the other six sleep parameters (activity counts, TST, WASO, number and length of awakenings, time in bed) were observed (all P > .05).
DISCUSSION
This study was designed to examine the effects of a single session of light-intensity walking on sleep outcomes in older women with sleep impairment. The results demonstrated that an acute bout of light-intensity walking has modest effects for two of the eight sleep outcomes for this population, in reducing sleep latency and increasing sleep efficiency.
These findings are in agreement with earlier studies using chronic intervention designs among older adults that suggested light-intensity exercise had benefits for some sleep parameters.26,28 One study examined the effects of an 8-week light- and moderate-intensity exercise (10 minutes warm-up, 35 minutes walking/running, 10 minutes cool-down) on self-reported sleep measures among older men. The results showed that the light-intensity exercise group (40% to 50% MaxHR) reported significantly better sleep quality and all other sleep parameters than the control group, although exercise at moderate intensity (60% to 70% MaxHR) led to the best sleep outcomes.26 Another study investigated effects of a 9-month light- and moderate-intensity exercise (15 minutes warm-up, 30 minutes cycling, 10–15 minutes cool-down) on self-reported sleep measures among older adults. It found that light- and moderate-intensity exercise (30% to 40%, and 60% to 70% of heart rate reserve respectively) improved to a similar degree on self-reported sleep quantity, indicating no superiority of moderate-intensity over light-intensity exercise.28
The area of acute exercise research is still unexplored and the results are not conclusive due to the limited trials available.21 One study similar to this work showed no significant improvement on sleep outcomes with device-based measures after a single session of treadmill walking (72 ± 15 minutes) at light intensity (45% VO2peak) among healthy older women.27 One of the reasons for the inconsistent findings may relate to the existing sleep patterns of participants. Women in the previous study were good sleepers with a baseline TST of 431 minutes. However, participants in this study were individuals with sleep impairment, reporting less than 6 hours (329.5 minutes) total sleep at baseline. Ceiling or floor effects may therefore have underestimated the value of light-intensity exercise on sleep in previous research. Moreover, the earlier study did not provide results relating to sleep latency and sleep efficiency, which were shown to significantly improve after an acute bout of light-intensity exercise in this study.
Interestingly, the reductions in sleep latency and improvement in sleep efficiency, considered two of the most important indicators of sleep quality,38 were not matched by any signifi-cant changes in TST or WASO in this study. This might suggest that an acute bout of exercise is more effective for sleep initiation than for sleep maintenance among older adults. Some support for this comes from another acute exercise trial involving adults with insomnia.39 Following a moderate intensity exercise session, the largest benefits were for reducing sleep latency. Mechanisms of exercise effects on sleep include anxiety reduction, body temperature elevation, and energy depletion.17,21 These might help explain the reduced sleep latency, which contributes to the improvement of sleep efficiency among participants in this study.
Strengths and Limitations
This study is the first to assess the effects of an acute walking intervention on sleep quality in older adults with sleep impairment. It used a rigorous randomized design, a carefully monitored exercise session, and objective measurement of sleep. Nonetheless, some limitations should be acknowledged. This study only included older women. Caution is needed therefore when interpreting these findings, which may not generalize to other populations. Wrist actigraphy is useful in the estimation of several sleep parameters (eg, TST, WASO), but is less reliable in terms of estimating sleep latency.40 However, we asked participants to record the time they went to bed, which might mitigate the effects. In addition, the time of day for napping among participants was not reported. Naps taken at different times of the day may differently affect sleep.41 It is also conceivable that the enhancement of sleep in some of the participants might be explained by the exercise program coinciding with usual napping times, hence preventing the nap. Furthermore, expectancy effects cannot be ruled out, because an exercise session was compared with a rest condition. We did not administer any subjective measures of sleep quality. From a behavioral perspective, it would be interesting to know if some participants might perceive improved sleep after exercise and continue the practice. Finally, because the current study assessed the acute effect of a single bout of light-intensity exercise, it did not provide data on any sustained effect on sleep over subsequent nights.
In conclusion, this study suggests that low-intensity walking can lead to modest benefits in sleep latency and efficiency in older women with sleep impairment. These findings may provide clinicians with reassurance that even small increases in exercise for patients may have some benefit to sleep, and this may be a starting point toward meaningful behavioral change. More research is needed on this topic to investigate how to optimize the potential improvements in sleep in this population to increase the public health reach.
DISCLOSURE STATEMENT
All authors have read and agree to the publication of the manuscript. This study is in part supported by Ministry of Science and Technology, Taiwan (MOST105-2410-H-028-004-MY2). The sponsor had no role in the study design, data collection, data analysis, data interpretation, or the writing of the report. The authors report no conflicts of interest.
ABBREVIATIONS
- AIS-5
Athens Insomnia Scale-five item
- BMI
body mass index
- MaxHR
maximal heart rate
- PAR-Q
Physical Activity Readiness Questionnaire
- TST
total sleep time
- WASO
wake after sleep onset
REFERENCES
- 1.Lopes CS, Robaina JR, Rotenberg L. Epidemiology of insomnia: prevalence and risk factors. In: Sahoo S, editor. Can't sleep? Issues of being an insomniac. Rijeka: InTech; 2012. pp. 3–22. [Google Scholar]
- 2.Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult: a mini-review. Gerontology. 2010;56(2):181–189. doi: 10.1159/000236900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grewal R, Doghramji K. Epidemiology of insomnia. In: Attarian HP, Schuman C, editors. Clinical Handbook of Insomnia, Current Clinical Neurology. New York, NY: Humana Press; 2010. pp. 13–22. [Google Scholar]
- 4.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: systematic review and meta-analysis. Sleep Med Rev. 2016;30:11–24. doi: 10.1016/j.smrv.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Chen LJ, Lai YJ, Sun WJ, Fox KR, Chu D, Ku PW. Associations of exercise, sedentary time and insomnia with metabolic syndrome in Taiwanese older adults: a 1-year follow-up study. Endocr Res. 2015;40(4):220–226. doi: 10.3109/07435800.2015.1020547. [DOI] [PubMed] [Google Scholar]
- 7.Spira AP, Chen-Edinboro LP, Wu MN, Yaffe K. Impact of sleep on the risk of cognitive decline and dementia. Curr Opin Psychiatry. 2014;27(6):478–483. doi: 10.1097/YCO.0000000000000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Almondes KM, Costa MV, Malloy-Diniz LF, Diniz BS. Insomnia and risk of dementia in older adults: systematic review and meta-analysis. J Psychiatr Res. 2016;77:109–115. doi: 10.1016/j.jpsychires.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 9.Potvin O, Lorrain D, Belleville G, Grenier S, Preville M. Subjective sleep characteristics associated with anxiety and depression in older adults: a population-based study. Int J Geriatr Psychiatry. 2014;29(12):1262–1270. doi: 10.1002/gps.4106. [DOI] [PubMed] [Google Scholar]
- 10.Tel H. Sleep quality and quality of life among the elderly people. Neurol Psychiatry Brain Res. 2013;19(1):48–52. [Google Scholar]
- 11.Murtagh EM, Nichols L, Mohammed MA, Holder R, Nevill AM, Murphy MH. The effect of walking on risk factors for cardiovascular disease: an updated systematic review and meta-analysis of randomised control trials. Prev Med. 2015;72:34–43. doi: 10.1016/j.ypmed.2014.12.041. [DOI] [PubMed] [Google Scholar]
- 12.Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065–2079. doi: 10.2337/dc16-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Windle G, Hughes D, Linck P, Russell I, Woods B. Is exercise effective in promoting mental well-being in older age? A systematic review. Aging Ment Health. 2010;14(6):652–669. doi: 10.1080/13607861003713232. [DOI] [PubMed] [Google Scholar]
- 14.Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427–449. doi: 10.1007/s10865-015-9617-6. [DOI] [PubMed] [Google Scholar]
- 15.Passos GS, Poyares DLR, Santana MG, Tufik S, de Mello MT. Is exercise an alternative treatment for chronic insomnia? Clinics. 2012;67(6):653–659. doi: 10.6061/clinics/2012(06)17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang PY, Ho KH, Chen HC, Chien MY. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. J Physiother. 2012;58(3):157–163. doi: 10.1016/S1836-9553(12)70106-6. [DOI] [PubMed] [Google Scholar]
- 17.Driver HS, Taylor SR. Exercise and sleep. Sleep Med Rev. 2000;4(4):387–402. doi: 10.1053/smrv.2000.0110. [DOI] [PubMed] [Google Scholar]
- 18.Youngstedt SD, O'Connor PJ, Dishman RK. The effects of acute exercise on sleep: a quantitative synthesis. Sleep. 1997;20(3):203–214. doi: 10.1093/sleep/20.3.203. [DOI] [PubMed] [Google Scholar]
- 19.Kubitz KA, Landers DM, Petruzello SJ, Han M. The effects of acute and chronic exercise on sleep: a meta-analytic review. Sports Med. 1996;21(4):277–291. doi: 10.2165/00007256-199621040-00004. [DOI] [PubMed] [Google Scholar]
- 20.Dolezal BA, Neufeld EV, Boland DM, Martin JL, Cooper CB. Interrelationship between sleep and exercise: a systematic review. Adv Prev Med. 2017;2017:1364387. doi: 10.1155/2017/1364387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ZubiaVeqar ME. Sleep quality improvement and exercise: a review. International Journal of Scientific and Research Publications. 2012;2(8):1–8. [Google Scholar]
- 22.Chen LJ, Fox KR, Ku PW, Chang Y. Effects of aquatic exercise on sleep in older adults with mild sleep impairment: a randomized controlled trial. Int J Behav Med. 2016;23(4):501–506. doi: 10.1007/s12529-015-9492-0. [DOI] [PubMed] [Google Scholar]
- 23.Roveda E, Sciolla C, Montaruli A, Calogiuri G, Angeli A, Carandente F. Effects of endurance and strength acute exercise on night sleep quality. Int Sportmed J. 2011;12(3):113–124. [Google Scholar]
- 24.Reid KJ, Baron KG, Lu B, Naylor E, Wolfe L, Zee PC. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 2010;11(9):934–940. doi: 10.1016/j.sleep.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baron KG, Reid KJ, Zee PC. Exercise to improve sleep in insomnia: exploration of the bidirectional effects. J Clin Sleep Med. 2013;9(8):819–824. doi: 10.5664/jcsm.2930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamrani AAA, Shams A, Dehkordi PS, Mohajeri R. The effect of low and moderate intensity aerobic exercises on sleep quality in men older adults. Pak J Med Sci. 2014;30(2):417–421. doi: 10.12669/pjms.302.4386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X, Youngstedt SD. Sleep quality improved following a single session of moderate-intensity aerobic exercise in older women: results from a pilot study. J Sport Health Sci. 2014;3(4):338–342. doi: 10.1016/j.jshs.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stevenson JS, Topp R. Effects of moderate and low intensity long-term exercise by older adults. Res Nurs Health. 1990;13(4):209–218. doi: 10.1002/nur.4770130403. [DOI] [PubMed] [Google Scholar]
- 29.Balboa-Castillo T, León-Muñoz LM, Graciani A, Rodríguez-Artalejo F, Guallar-Castillón P. Longitudinal association of physical activity and sedentary behavior during leisure time with health-related quality of life in community-dwelling older adults. Health Qual Life Outcomes. 2011;9:47. doi: 10.1186/1477-7525-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chalise HN, Lamsal U. Walking and sleep quality of Nepalese older adults residing in an old age home. J Gerontol Geriatr Med. 2017;3(1) 015. [Google Scholar]
- 31.Morris JN, Hardman AE. Walking to health. Sports Med. 1997;23(5):306–332. doi: 10.2165/00007256-199723050-00004. [DOI] [PubMed] [Google Scholar]
- 32.Chen LJ, Fox KR, Sun WJ, Tsai PS, Ku PW, Chu D. Associations between walking parameters and subsequent sleep difficulty in older adults: a 2-year follow-up study. J Sport Health Sci. 2018;7(1):95–101. doi: 10.1016/j.jshs.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. WHO technical meeting on sleep and health. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 34.Shephard RJ. PAR-Q, Canadian Home Fitness Test and exercise screening alternatives. Sports Med. 1988;5(3):185–195. doi: 10.2165/00007256-198805030-00005. [DOI] [PubMed] [Google Scholar]
- 35.Chiang H-L, Chen H-C, Bai C-H, et al. A validation study of Chinese version of the Athens Insomnia Scale. Taiwanese Journal of Psychiatry. 2009;23(1):43–52. [Google Scholar]
- 36.Hartescu I, Morgan K, Stevinson CD. Increased physical activity improves sleep and mood outcomes in inactive people with insomnia: a randomized controlled trial. J Sleep Res. 2015;24(5):526–534. doi: 10.1111/jsr.12297. [DOI] [PubMed] [Google Scholar]
- 37.ActiGraph Software Department. ActiLife 6 user's manual. Pensacola, FL: ActiGraph Software Department; 2012. [Google Scholar]
- 38.Shrivastava D, Jung S, Saadat M, Sirohi R, Crewson K. How to interpret the results of a sleep study. J Community Hosp Intern Med Perspect. 2014;4(5):24983. doi: 10.3402/jchimp.v4.24983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Passos GS, Poyares D, Santana MG, Garbuio SrA, Tufik S, Mello MTl. Effect of acute physical exercise on patients with chronic primary insomnia. J Clin Sleep Med. 2010;6(3):270–275. [PMC free article] [PubMed] [Google Scholar]
- 40.Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139(6):1514–1527. doi: 10.1378/chest.10-1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Milner CE, Cote KA. Benefits of napping in healthy adults: impact of nap length, time of day, age, and experience with napping. J Sleep Res. 2009;18(2):272–281. doi: 10.1111/j.1365-2869.2008.00718.x. [DOI] [PubMed] [Google Scholar]