Abstract
Background
Heatwaves are hot weather events, which breach regional or national thresholds, that last for several days. They are likely to occur with increasing frequency in some parts of the world. The potential consequences were illustrated in Europe in August 2003 when there were an estimated 30,000 excess deaths due to a heatwave. Electric fans might be used with the intention of reducing the adverse health effects of a heatwave. Fans do not cool the ambient air but can be used to draw in cooler air from outside when placed at an open window. The aim of the fans would be to increase heat loss by increasing the efficiency of all normal methods of heat loss, but particularly by evaporation and convection methods. However, it should be noted that increased sweating can lead to dehydration and electrolyte imbalances if these fluids and electrolytes are not replaced quickly enough. Research has also identified important gaps in knowledge about the use of fans, which might lead to their inappropriate use.
Objectives
To determine whether the use of electric fans contributes to, or impedes, heat loss at high ambient temperatures during a heatwave, and to contribute to the evidence base for the public health impacts of heatwaves.
Search methods
We sought unpublished and published studies that had been published in any language. The review team were able to assess studies reported in English, Chinese, Dutch, French and German; and reports in other languages would have been translated into English as necessary. We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, CINAHL, the Indian biomedical literature (IndMED and MedIND) and databases of Chinese literature (Chinese Journal Net and Digital Periodical of WanFang Data). The most recent electronic searches were done in April 2012. We also checked the reference lists of relevant articles and the websites of relevant national and international organisations, and consulted with researchers and policy makers with experience in strategies to manage heatwaves to identify additional studies. The titles and abstracts from each search were checked independently by two review authors. The full text articles that we retrieved were checked independently by at least two authors for their relevance and for references to potentially eligible studies.
Selection criteria
Randomised trials and other experimental designs, such as interrupted time series and controlled before‐and‐after studies, comparing the use of electric fans with no fans during a heatwave were eligible for this review. The electric fans could be hand‐held (battery operated), portable or mounted on the wall or ceiling, or in a window. We sought interventions delivered to anyone for whom a heatwave was likely to have serious adverse health impacts. This would include people of all ages but with a particular focus on some groups (for example older people). Populations from high‐, middle‐ and low‐income countries were eligible for the review.
Data collection and analysis
If we had identified eligible studies, they would have been assessed independently by at least two review authors and data would have been extracted on the characteristics of the study, its participants and interventions, as well as the effects on health outcomes. The primary outcomes were mortality, hospital admission and other contacts with healthcare services.
Main results
We did not identify any eligible studies despite the extensive searching and correspondence with several experts in this topic area. We identified retrospective, observational studies, usually with a case‐control design, that investigated the association between the use of electric fans and health outcomes, including death. The results of these studies were mixed. Some studies found that the use of fans was associated with better health outcomes, others found the reverse.
Authors' conclusions
The evidence we identified does not resolve uncertainties about the health effects of electric fans during heatwaves. Therefore, this review does not support or refute the use of electric fans during a heatwave. People making decisions about electric fans should consider the current state of the evidence base, and they might also wish to make themselves aware of local policy or guidelines when making a choice about whether or not to use or supply electric fans. The main implication of this review is that high quality research is needed to resolve the long standing and ongoing uncertainty about the benefits and harms of using electric fans during a heatwave, for example randomised trials comparing the health effects in people with electric fans to those in people without them.
Keywords: Humans, Body Temperature Regulation, Body Temperature Regulation/physiology, Electrical Equipment and Supplies, Extreme Heat, Extreme Heat/adverse effects, Household Articles, Household Articles/instrumentation, Ventilation, Ventilation/instrumentation, Ventilation/methods
Plain language summary
Electric fans for reducing the health effects of heatwaves
Heatwaves are set to become more common and their effects can be devastating. For example, up to 30,000 people may have died because of the heatwave that occurred in Europe during August 2003. One way to try to get relief from the heat is to use an electric fan, but whether this will do more good or harm is uncertain. A fan might help to increase heat loss if the temperature is below 35 °C and the fan is not directly aimed at the person, but, when temperatures are above 35 °C, the fan might actually contribute to heat gain. Excess sweating can also lead to dehydration and other health problems. It is important, therefore, to know about the potential benefits and harms of electric fans when choosing whether to use one. This applies if the decision is about your own use of a fan, but it is also relevant to broader public health decisions, such as whether to give electric fans to groups of people during a heatwave. This is particularly important for people who are considered more vulnerable to the effects of heat, such as older adults who are less able to cool down through sweating or increasing the flow of blood to their skin.
This Cochrane Review tried to provide some of the answers that would help decision makers. We looked for high quality research that had compared groups of people using fans with groups who didn't use them during a heatwave However, we didn't find any research that met our requirements. We did find some studies which used designs that are less reliable for answering this sort of question, and these had mixed results. Some suggested that fans might reduce health problems, while others suggested that the fans might make things worse.
Therefore, the research that has been done to date does not resolve uncertainties about the health effects of electric fans during heatwaves. People who have to make decisions should consider the current evidence, alongside local policies and guidelines when making their choices. They may wish to help resolve the continuing uncertainty by conducting the type of high quality research that would provide the reliable evidence needed to determine the benefits and harms of using electric fans during a heatwave.
Background
While there is no universal definition of heatwaves, they are understood to be hot weather events that breach regional or national thresholds and last for several days. According to the Intergovernmental Panel on Climate Change (IPCC), heatwaves are likely to occur with increasing frequency in some parts of the world (IPCC 2012) as a result of climate change. Climate modelling undertaken by the IPCC suggests "a 1‐in‐20 year hottest day is likely to become a 1‐in‐2 year event by the end of the 21st century in most regions, except in the high latitudes of the Northern Hemisphere, where it is likely to become a 1‐in‐5 year event" (IPCC 2012). The potential consequences were illustrated in parts of Europe, particularly Northern France, in August 2003 when unprecedented high day‐ and night‐time temperatures for a period of three weeks resulted in more than 15,000 excess deaths in France and an estimated 30,000 across Europe (Fouillet 2008; Robine 2008).
The vast majority of those deaths during the heatwave were among the elderly ,which could be because of a diminished capacity to thermoregulate by older people due to a decreased ability to sweat, decreased blood flow to the skin and extremities (needed for heat dissipation) and a decreased plasma volume and cardiac output (Kenny 2010)as well as other physiological mechanisms such as chronic illness, co‐morbid medical conditions, and particular medications (DCLG 2008; Hajat 2010). Also, not all heatwaves are alike as the meteorological conditions during a heatwave make some events more potentially dangerous, particularly those with both high heat and humidity, and where temperatures remain high during the night. High night temperatures do not allow the human body to recover in the night and may place the human body in more physiological stress, leading to excessive heat‐related deaths (McGeehin 2001).
Description of the condition
Heatwaves have a clear impact on society, including a rise in mortality and morbidity. Heatwaves place an increased strain on infrastructure (power, water and transport). Clothes and food retailing, tourism and ecosystem services can also be affected. In some instances, heatwaves may even trigger social disturbance. The impact of heatwaves is immense and can be catastrophic, as in the large number of heat‐related deaths recorded across Europe in 2003. While the effects of heat may be exacerbated in cities because of the heat island effect, the livelihoods and social well‐being of non‐urban communities can also be severely disrupted during and following periods of unusually hot weather.
Description of the intervention
The electric fans investigated in this Cochrane Review can either be mounted on the wall or ceiling, in a window, or be portable (for example a floor, table or battery operated hand‐held fan), and the review investigates their use during a heatwave.
How the intervention might work
Normal thermoregulation
The normal, healthy human body has a core temperature range of 36.1 ˚C to 37.8 ˚C and can cope with a temporary increase up to 38 ˚C or 39 ˚C without causing damage to health (Koppe 2004; Kovats 2008; Matthies 2008). Regulation and maintenance of core body temperature within these parameters is managed by the hypothalamus through a careful and precise balance of heat generation and loss (Koppe 2004; Matthies 2008). Maintaining this balance is known as thermoregulation. Thermoneutrality describes the parameters to maintain a healthy core body temperature, and can be defined as the point at which metabolic activity is minimal. It varies around the circadian rhythm, sleep‐wake cycles and the menstrual cycle (Skinner 2002). The heat remaining within the body is the difference between the heat generated and the heat lost. Consequently, core body temperature will rise if heat generation exceeds loss and will drop if heat loss exceeds gain (Koppe 2004) providing that excess heat cannot be dissipated or generated, respectively. Heat is produced during and following activity since the body produces and releases heat through its use of energy (Koppe 2004). Body temperature can also rise as a result of high external environmental temperatures (Koppe 2004). Thermoreceptors, which are present throughout the skin, deep tissues and organs, can immediately detect an increase of as little as 1˚C (Matthies 2008). They communicate with the hypothalamus (in the hypothalamic thermoregulatory centre) which, in turn, initiates the response to increase the physiological response of heat loss (Matthies 2008). The human body loses heat via a number of routes, which include convection, conduction, radiation and evaporative cooling (Koppe 2004). These responses are summarised and explained in Table 1.
1. Mechanisms for the loss of body heat.
| Route | Mechanism |
| Convection | When air or water passes over the skin |
| Conduction | Contact with cooler objects on the skin |
| Radiation | Electromagnetic waves in the form of infrared rays |
| Sweating | Heat is released through the evaporation of sweat |
Adapted from Koppe 2004, Matthies 2008 and Analitis 2009.
Increasing heat and thermoregulation
When the surrounding air temperature is higher than body temperature, heat loss via the convection route can be impaired and heat will be gained from the environment to the skin (Koppe 2004). This will result in a raised core body temperature and the body will then initiate physiological responses, such as sweating, to aid in cooling (Koppe 2004). Sweating is the most effective mechanism through which the body can lose heat and maintain thermoneutrality (Allen 2009; HPA 2011; Koppe 2004). The human body can produce up to two litres of sweat per hour (containing sodium, potassium and water) and sweating can lead to dehydration and electrolyte imbalances if these fluids and electrolytes are not replaced quickly enough (Koppe 2004).
Heat‐related illness
Health impacts resulting from raised body temperature range from mild heat‐related illnesses to potentially severe consequences and death. Mild conditions include dehydration, heat cramps, heat oedema (swelling), heat syncope (fainting) and heat rash (DH 2011). Severe consequences include dehydration, heat exhaustion, heat stroke, cardiovascular and respiratory disease exacerbation, and death (DH 2011). Certain groups of people are more at risk of heat‐related illness than others (Applegate 1981). These include people with mental health illnesses, those on certain medications, the elderly (particularly the socially isolated or living alone and those residing in nursing or care homes), young children, and disabled and chronically ill people (particularly with cardiovascular and respiratory conditions) (DH 2011).
Role of fans
The aim of fans in a heatwave is to increase heat loss by increasing the efficiency of all normal methods of heat loss, but particularly by evaporation and convection methods. As indicated above, increased sweating can lead to dehydration and electrolyte imbalances if those substances are not replaced quickly enough.
Why it is important to do this review
There has been little comparative intervention research on the physiological effects of electric fans, and some studies have found important gaps in knowledge about the use of fans, which might lead to their inappropriate use (Ibrahim 2012). Therefore, it is difficult to assess the associated benefits and harms of their use by older people and other vulnerable populations during periods of high heat and humidity. There are good theoretical grounds for thinking that fans could help, but there are also theoretical risks that fans could lead to adverse effects. Evidence on the use of fans is limited. There are observational epidemiological studies (Kaiser 2001; Naughton 2002) that have described varied effects of fan use on severe morbidity and mortality. Some studies have found no association between the use of electric fans and the onset of heat stroke; in other studies fan use has been found to be slightly protective. For example, a meta‐analysis conducted by Bouchama et al found a protective association (for all‐cause deaths during heatwaves) with the use of fans (odds ratio (OR) 0.60, 95% CI 0.4 to 1.1) but this result was not statistically significant and the authors cautioned that the use of fans could not be justified by an evidence base until further research is completed (Bouchama 2007).
Objectives
To determine whether the use of electric fans contributes to or impedes heat loss at high ambient temperatures and to continue to develop the evidence base for the public health impacts of heatwaves.
Methods
Criteria for considering studies for this review
Types of studies
The most relevant study designs for this topic are randomised trials (including cluster trials) and other experimental designs such as interrupted time series and controlled before‐and‐after studies. In cluster studies, the likely clusters would include hospitals or communities, rather than individuals, as the unit of analysis.
Types of participants
Heat stroke may be divided into exertional and non‐exertional (classic) heat stroke (Shahid 1999). Exertional heat stroke, as its name suggests, occurs most often in otherwise healthy people who are exercising, usually in hot and humid climates, probably without being acclimatised. Classic heat stroke occurs during extreme heatwaves, with older people being particularly vulnerable (Grogan 2002). The focus of this study was restricted to classic heat stroke. Any physiological experiments on previously healthy young people were outside the scope of this study as they are likely to represent exertional heat stroke. In addition, experimental studies undertaken in a laboratory‐based, controlled clinical environment differ from the domestic, residential setting of our study population. The heat would be induced in a different way and the underlying vulnerabilities (physiological, psychological and physical) would differ between healthy volunteers in such experiments and the wider, general population. Therefore, the results of such experiments could not confidently be extrapolated to the general population that this review aimed to study.
We sought interventions that were delivered to anyone for whom a heatwave was likely to have serious adverse health impacts. This included people of all ages but with a particular focus on some groups (for example older people) (Applegate 1981). Populations from high‐, middle‐ and low‐income countries were eligible for the review.
Types of interventions
Electric‐ or battery‐operated fans that are eligible for this review included a:
table fan,
floor fan,
ceiling fan,
wall‐mounted fan,
window fan,
hand‐held fan.
Exhaust fans (or similar) were not eligible for this review.
The comparison group was participants:
who did not use an electric fan,
who used interventions other than a fan for cooling.
Types of outcome measures
Outcomes included measures of the effect on adverse health events.
Primary outcomes
The primary outcomes for this review were mortality, hospital admission and other contacts with healthcare services, either in person (for example an appointment with a general or family practitioner, or visit to a walk‐in health centre) or by telephone (for example to a service such as NHS Direct in the UK). Outcome measures have been identified on the basis that they should be meaningful to public health professionals, emergency management officials and people experiencing the effects of a heatwave.
Search methods for identification of studies
We sought unpublished and published studies that had been published in any language. The review team were able to assess studies reported in English, Chinese, Dutch, French and German. Reports in other languages would have been translated into English as necessary.
Electronic searches
We adapted search terms according to the requirements of individual databases, to take account of their specific subject heading terminology and syntax. We searched the following databases:
Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 4, 2012)
MEDLINE (from 1966 to 2012)
EMBASE (from 1980 to 2012)
CINAHL (from 1982 to 2012)
Indian biomedical literature (IndMED and MedIND)
Chinese full text journal databases (CJN and WangFang).
We searched prospective registries of trials through the World Health Organization (WHO) International Clinical Trial Registry Platform (Ghersi 2009), for both ongoing and closed trials. We searched MEDLINE, EMBASE and CINAHL in February 2012 using our preliminary but extensive search strategy (Appendix 1) and repeated this search in April 2012 to identify articles added to these databases in the interim. The search strategy was peer reviewed by an independent information specialist who suggested changes which retrieved a smaller number of records than our initial search. We ran this search in April 2012; it was modified to avoid the retrieval of records that we had already checked (Appendix 2). CENTRAL was also searched in April 2012.
Two databases of Chinese articles were searched for relevant articles: Chinese Journal Net (CJN) and Digital Periodical of WanFang Data (WanFang). Both databases offer the full text of all listed articles. The CJN database catalogues over 8700 journals published in China; subjects include natural science, engineering, agriculture, philosophy, medicine, humanities and social sciences. Publication dates can be as early as 1915 but the majority of articles listed were published from 1994 onwards. The WanFang database covers more than 6000 journals published in China from 1998 onwards. The searches of the Chinese databases were done in March 2012. The Mandarin Chinese characters used in the search are shown in Figure 1 for the CJN database and in Figure 2 for the WanFang database, which has a search limit of 200 words and therefore required each of the eight searches to be performed and then combined.
1.
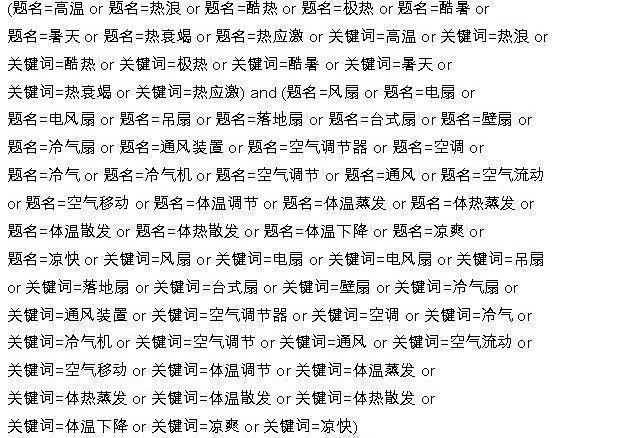
CJN database search strategy (1994 ‐ March 2012)
2.
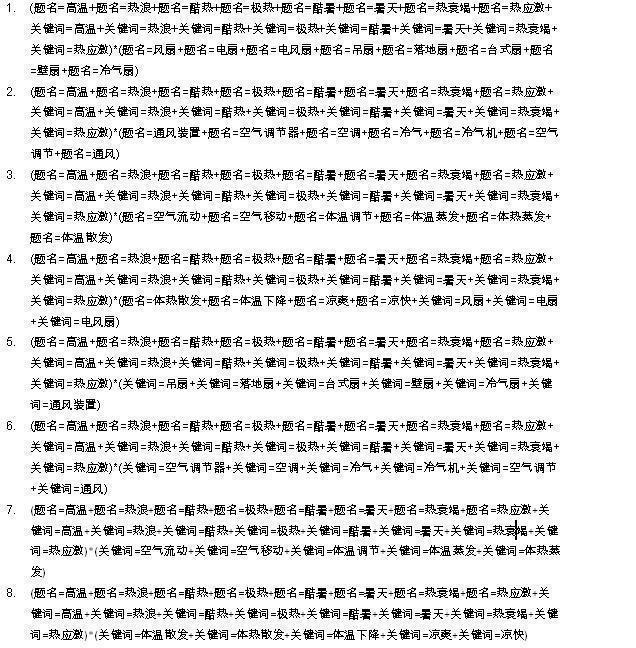
WanFang database search strategy (1998 ‐ March 2012)
Searching other resources
Reference lists of key articles
We handsearched reference lists of all relevant articles for any additional relevant reports (Horsley 2011).
Targeted internet searching of websites of key organisations
We searched key sites, including those of Centers for Disease Control and Prevention (www.cdc.gov) Health Canada (www.hc‐sc.gc.ca), Health Protection Agency (www.hpa.org.uk).Intergovernmental Panel on Climate Change (www.ipcc.ch), WHO (www.who.int/en ) and the World Meteorological Organization (www.wmo.int).
Handsearching
We handsearched the proceedings of relevant workshops (for example International Web Workshop of Experts on Extreme Heat and Health).
Researchers and policy makers
We consulted with researchers and policy makers with experience in strategies to manage heatwaves to identify additional studies.
Data collection and analysis
Selection of studies
The titles and, where available, the abstracts retrieved by the searches were independently checked by at least two review authors. We retrieved all articles identified as potentially eligible by at least one review author. The full‐text articles were assessed independently by two review authors to determine eligibility for this review. A third review author resolved any disagreement related to inclusion of articles. We documented excluded studies and reasons for exclusion.
If information that was not available in the full report was needed to determine eligibility for inclusion, we contacted the original authors to obtain the additional information (Young 2011).
Data extraction and management
We would have extracted data from the reports of all studies that were eligible for this review using two review authors working independently but without blinding to the original study authors or institutions. A third review author would have resolved discrepancies and lead authors would have been contacted for missing data (Young 2011). Data would have been extracted to allow each study to be reported in a narrative format, including information on study design, interventions and outcomes. The following data were to be sought for each included study.
1. Study: a. type of study, b. method of participant selection, c. unit of allocation (to distinguish individual and cluster trials), d. study duration, e. sample size, f. control group selection (if not randomised).
2. Participants: a. country, b. study setting and population characteristics, c. recruitment rates, d. age, e. sex.
3. Interventions: a. focus of interventions, b. interventions, c. location of interventions, d. intervention timing (i.e. seasonal) and duration, e. length of follow‐up, f. evaluation points.
4. Outcomes evaluated: a. general health measures, b. long‐term health outcomes, c. policies produced, d. withdrawals and dropouts.
Assessment of risk of bias in included studies
We would have assessed relevant studies for methodological quality using the Cochrane Collaboration's tool for assessing 'Risk of bias'. Two review authors would have independently rated articles, with a third author available to resolve any disagreements. We would have used the recommendations in Chapter 15 of the Cochrane Handbook for Systematic Reviews of Interventions to guide the analysis of non‐randomised controlled trials (Shemilt 2011).
We planned to assess studies for the five general domains of bias: sequence generation, allocation concealment, blinding, attrition and outcome reporting. Each study would have been assessed for 'low', 'unclear' or 'high' risk of bias, according to the 'Risk of bias' tool. Each study would have received an overall rating of methodological quality (strong, moderate or weak), agreed within the review author team through consensus.
Measures of treatment effect
If data had been available from eligible studies, we would have expressed effect sizes for dichotomous outcomes as relative risks with 95% confidence intervals. For continuous outcomes, we intended to use weighted mean differences with 95% confidence intervals. If a study tested more than one type of electric fan against a control group, we would have examined the overall effects of the intervention versus control using the pooled results from the intervention groups.
Unit of analysis issues
If trials had randomised or allocated participants at the cluster level, we would have used meta‐analyses to estimate effect sizes and their standard errors. The analyses would have been adjusted for the clustering effect, with the intent of re‐analyzing those studies that did not account for clustering during their original analysis. Alternatively, if appropriate, we would have employed statistical methods that allowed analysis at the level of the individual while accounting for the clustering.
Dealing with missing data
In the case of missing data from eligible studies, we would have contacted authors to request additional data (Young 2011). If it was not possible to obtain the missing data, this would have been captured in the data extraction form and reported in the 'Risk of bias' table or elsewhere in the description of the study, as appropriate.
Assessment of heterogeneity
The decision about whether to complete a meta‐analysis would have been made after the data were extracted. We intended to assess consistency of effects across studies using the I2 statistic (Higgins 2003), together with qualitative consideration of whether studies should be combined. We would have conducted subgroup analyses as a means of investigating heterogeneous results.
Assessment of reporting biases
As recommended in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), we intended to plot trial effects against standard error and present funnel plots. We would also have constructed an ORBIT outcome matrix to illustrate the potential for selective reporting within studies (http://ctrc.liv.ac.uk/orbit/) (Kirkham 2010).
Data synthesis
We would have reported all outcomes regardless of the statistical significance of their effect estimates, reporting data according to the type of study design (randomised trials, interrupted time series, controlled before‐and‐after studies). As noted above, the decision about whether to complete a meta‐analysis would have been determined after data extraction and only when data were sufficiently homogeneous. We would have used Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions to guide decision‐making regarding use of meta‐analytic procedures (Deeks 2011).
Subgroup analysis and investigation of heterogeneity
If data were available, we would have done subgroup analysis by:
extremes of age (age over 65 years, children including infants),
country,
siting of fan (e.g. wall mounted, ceiling, etc.).
Sensitivity analysis
If we had been able to conduct meta‐analyses, we would have done sensitivity analyses based on the study designs of the studies included in the meta‐analyses, excluding non‐randomised studies.
Protocol
The protocol for this review was accepted by the Gynaecological Cancer Group in April 2012 and published in the Cochrane Database of Systematic Reviews in May 2012 (Gupta 2012).
Results
Description of studies
Results of the search
Our searches identified a total of more than 4500 records for checking and led to the retrieval of more than 120 full‐text articles, but none of these met the eligibility criteria for the review. The findings from the various elements of the search are described below.
The largest proportion of records to check came from the searches of the major English language databases: MEDLINE (original search: 1739 records; update of this search: seven additional records; revised search: 54 additional records), EMBASE (2184; 17; 107) and CINAHL (118; 0; 0). The search of CENTRAL identified 10 records. After checking all these titles and, where available, their abstracts, we identified 62 that warranted consideration of the full‐text article. Our checking of the references in the retrieved articles and suggestions from elsewhere led to an additional 46 full‐text articles and reports to be checked. At the time of finalising this version of the review, 101 of this total of 108 articles have been read in full. The remaining seven articles are still pending assessment but, based on their abstract or the context in which they were cited by other articles, none of these are likely to be the report of an eligible study.
A total of 12 articles were identified in the search of the Indian biomedical literature (IndMED and MedIND) (http://indmed.nic.in/indmed.html) and we did not seek the full text for any of these. This was because our assessment of the titles and abstracts did not reveal any studies that were likely to be eligible for the review or any articles that might be potential sources of eligible studies.
A total of 297 articles were identified in the search of the Chinese Journal Net (CJN) database. The titles and abstracts of these were reviewed for potential eligibility and the majority (279) were not research studies. Of the 18 articles that were research studies and were checked in detail, none met the eligibility criteria for this review. A total of nine articles were identified in the search of the WanFang database. Checking of the titles and abstracts identified four research studies but none of these were eligible.
Our searches of the 10 websites of organisations that were selected as most likely to be particularly relevant to this review (Table 2) and our correspondence with experts in the topic area did not identify any reports or articles that were eligible. However, they did provide useful background information, which is included in the Background or Discussion sections of this review, and they helped to inform the Implications for practice and Implications for research sections of this review.
2. Websites searched.
| Organisation | Website |
| Health Canada | www.hc‐sc.gc.ca/index‐eng.php |
| Intergovernmental Panel on Climate Change | www.ipcc.ch |
| World Health Organization | www.who.int/en |
| World Meteorological Organization | www.wmo.int |
| Centers for Disease Control and Prevention | www.cdc.gov |
| Health Protection Agency | www.hpa.org.uk |
| British Columbia Centre for Disease Control | http://www.bccdc.ca/default.htm |
| Pacific Institute for Climate Research | http://www.pics.uvic.ca/ |
| Environmental Protection Agency | http://www.epa.gov/ |
| National Collaborating Centre for Environmental Health | http://ncceh.ca/ |
Figure 3 shows the flow of articles through our search.
3.
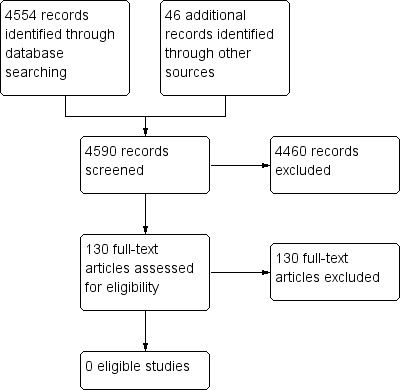
Study flow diagram.
Included studies
We did not identify any eligible studies despite the extensive searching and correspondence with several experts in this topic area.
Excluded studies
The articles which reported on the effects of electric fans and mortality and morbidity included experimental studies that, for example, examined the effects of fans in specialized groups such as during the recovery of fire fighters (Carter 1999; Hostler 2010) or athletes (Barwood 2009; Duffield 2008) who had been exposed to high temperatures. There were also studies in laboratory conditions (Riggs 1981) and randomised trials of fans as a way to produce cooling in the treatment of head trauma (Harris 2007). We identified some observational studies that examined the association between fans (and other cooling strategies) and morbidity or mortality in heat waves, typically within case‐control studies, and these studies are discussed in more detail below (see Effects of interventions). There were also several studies citing beneficial effects of air conditioning (for example, Applegate 1981) or investigating the effects of fans on agricultural animals (for example, Zhang 2009), as well as case reports or small case series of the effects of a variety of fans or fan‐like devices. These included one report of the effects of using the downdraft from a light utility helicopter to treat three patients with serious heatstroke (Poulton 1987). We also identified recent examples of research which examined the information seeking behaviours of people during heat waves (Chan 2011) and the awareness of healthcare practitioners about interventions (Ibrahim 2010; Ibrahim 2012). The latter survey, conducted in Australia in 2008 with 327 respondents, found what the original authors described as gaps in knowledge about the use of electric fans in heatwaves, noting that “less than half of respondents understood that ‘fans do not cool the air’ and that ‘fans are less effective on a very humid day’” (Ibrahim 2012).
Risk of bias in included studies
We did not identify any eligible studies for inclusion in this review, and we did not formally assess the risk of bias in the excluded studies which are discussed below. These case‐control studies are at high risk of bias, primarily because of the possibility of confounding.
Effects of interventions
We did not identify any eligible studies for inclusion in this review and are unable to provide estimates of the potential benefits and harms of the use of electric fans during heatwaves. As noted in the 'Description of studies' section, we did identify some observational studies that examined the relationship between the use of fans and morbidity and mortality during heatwaves. The findings of these case‐control studies are mixed and do not provide a reliable assessment of the effects of electric fans. However, they are described briefly here to help set the scene for the Discussion section, which follows; as well as Authors' conclusions section.
Some of the case‐control studies were brought together in a meta‐analysis of prognostic factors for heatwave‐related deaths by Bouchama et al (Bouchama 2007). This included a meta‐analysis of three studies (Kaiser 2001; Lorente 2005; Naughton 2002) and, in Bouchama et al’s words, found that estimates of the effects of using electric fan ventilation during a heat wave “were associated with a trend toward lower risk of death but were not statistically significant”. The meta‐analysis produced an odds ratio (OR) for death of 0.60 (95% CI 0.4 to 1.1, P = 0.31) in favour of electric fans. Bouchama et al concluded that recommendations to use an electric fan needed further evaluation, not least of all because of the possibility of harm. The three studies included by Bouchama et al were identified in our searches and are summarised below.
Kaiser et al analysed data from 17 people who died during a 1999 heat wave (from July 1st to August 22nd) in Cincinnati, USA and 34 controls from the same neighbourhood (Kaiser 2001); with a particular focus on mental illness given that eight of the people who died had a mental illness. The authors concluded that “The use of electrical fans was not protective”, finding that 16 (94%) of the 17 cases and 32 (97%) of 33 (data were not available for one) controls had a working electric fan. They reported a crude OR for death of 0.5 (95% CI 0.01 to 39) in favour of electric fans. They also noted that the death investigation reports showed that 12 of the dead people had fans and that these were in use when 10 of them were found.
Naughton et al collected data for people who died in a Chicago, USA heatwave between 29 July and 6 August 1999, and for controls who were matched on the basis of neighbourhood and age (Naughton 2002). They found that 56 (90%) of the 63 cases and 67 (88%) of the 77 controls had a working electric fan, and reported an adjusted OR of 0.71 (95% CI 0.2 to 2.3), meaning that fans were non‐significantly less likely to be in the homes of cases compared to control. In comparing their findings with those of an earlier study of a 1995 heatwave in Chicago (Semenza 1996) (see below), they concluded “Fans were not significantly protective, either when evaluated separately in the two studies or when examined in a pooled analysis using 1995 and 1999 data” but they did not present the numerical results from this pooled analysis.
Lorente et al presented the results from two case‐control studies conducted in residential facilities for the elderly from among the many research studies that followed the French heatwave of August 2003 (Lorente 2005). The first study investigated 350 facilities that had a higher than average mortality and that were located in an area with higher than normal temperatures during the heatwave; it sought to identify mortality risk factors related to the facility (architectural features, equipment and operations). The second study investigated 628 people who lived in facilities located in an area that had higher than average mortality during the heatwave. It included 314 people who died during 5 to 15 August 2003 (cases) and 314 controls known to be alive on 1 September 2003, and sought to identify individual risk factors for mortality during the heatwave. The studies found some evidence to suggest that there was an increased risk of death when an electric fan was present, but there were mixed findings regarding the risk associated with the use of electric fans. For example, in the first study, families had installed additional fans in buildings in 75% of cases and the OR for death was 2.5 (95% CI 1.5 to 4.2) if additional fans had been installed. In the second study, 17% of cases compared to 12% of controls had a fan (fixed or mobile) in their house and fans were significantly more common in the rooms of cases (OR 1.9, 95% CI 1.1 to 3.4) (Lorente 2005). The presence of fans was also found to be associated with an increased risk of mortality when they were installed in individual rooms (OR 1.8, 95% CI 1.0 to 3.3) and common rooms (OR 1.3, 95% CI 0.9 to 3.1). However, the data from the Lorente et al research that were used in the Bouchama meta‐analysis came from their analysis of whether the building of the participants did not have a fan (fixed or mobile), and they used the matched analysis adjusted for sex and autonomy which suggested an increased risk of death (OR 1.7, 95% CI 0.9 to 3.1, not significant) when a fan was not present (Bouchama 2007; Lorente 2005, page 94).
In addition to the three studies which were included in the Bouchama meta‐analysis, we identified two further, similar studies that did not find an association between the use of electric fans and mortality in a heatwave (Kilbourne 1982; Semenza 1996) and one that found an association for "cooling techniques and devices" that included mechanical fans but with insufficient information on the effects of the electric fans themselves (Vandentorren 2006).
Semenza et al compared 339 people who died during 14 to 17 July 1995 in Chicago, USA with 339 controls who were matched to the cases according to neighbourhood and age (Semenza 1996). They reported “We did not detect any reduction in mortality in association with the use of electric fans (data not shown)” and concluded “we did not find any evidence that the use of fans was protective, nor did we determine that any level of use of electric fans was associated with increased mortality”.
Kilbourne et al conducted their study in the context of a heatwave in St Louis and Kansas City, USA, during July and August 1980 (Kilbourne 1982). They gathered questionnaire data for 156 people with heatstroke (severe heat illness with documented hyperthermia) and for 462 controls who were matched by age, sex and neighbourhood of residence. The data included the number of hours of home electric fan use per day and they concluded “We could not demonstrate a significant inverse association between the use of electric fans and heatstroke”. This lack of an association meant that electric fan use was not included in their regression analysis and so the relevant data were not reported in the paper. They also noted that “The distribution of fans was a prominent part of the emergency response to the 1980 heat wave” and that their finding “suggests that scarce relief resources should not be allocated in this manner in future heat waves”.
Vandentorren et al undertook a matched case control study in Paris to analyse risk factors of heatwave‐related mortality for elderly people living at home between August 8th and 13th 2003.(Vandentorren 2006); 315 cases and 282 controls were randomly selected and identified and matched for age, sex and location. Cooling devices were shown to be protective against heat‐related mortality. Behavioural adjustment to the heatwave in univariate paired analysis of all causes of death showed that using cooling devices or techniques had a protective effect, with an OR of 0.53 (95% CI 0.33 to 0.84). However, the original authors defined “cooling techniques and devices” as a variable which included any of the following: a mister, damp cloth, cool or cold bath or shower, sponge bath, mechanical fan or air conditioner. It was, therefore, difficult to extrapolate the results of mechanical fans as a solitary intervention.
We also identified older articles which made inferences about the beneficial effects of electric fans based on comparisons between heatwaves decades apart. For example, in 1956, Austin and Berry commented that “the use of air conditioning units, fans and other devices will effect a reduction in the number of casualties” after contrasting their findings from a study of hospital admissions for heatstroke in three hot summers in St Louis in 1952, 1953 and 1954; with the “larger number of admissions” in an earlier study that looked at 1934 to 1936 (Austin 1956).
Discussion
This review sought to determine if using electric fans reduces adverse health outcomes in the general population during a heatwave. We found no randomised trials or other eligible studies despite an extensive search of the published and grey literature, and contact with relevant experts. The research that we identified was observational in nature and contained a variety of findings, suggesting both benefits and harms from the use of fans. The use of fans is still promoted in some healthcare guidance, with previous heatwave responses having included the initiation of fan distribution programmes (Bernard 2004). However, some authors recommended against their use in heatwaves. For example, in their study of a heatwave in St Louis and Kansas City, USA, during July and August 1980, Kilbourne et al wrote “The distribution of fans was a prominent part of the emergency response to the 1980 heat wave. Our failure to find a demonstrable protective effect of fan use suggests that scarce relief resources should not be allocated in this manner in future heat waves” (Kilbourne 1982). Likewise, in reference to fan interventions during heatwaves, Bernard and McGeehin summarised that in their study “Five of the cities reported fan distribution programs, despite evidence that fans do not reduce mortality risk during heat waves and can increase heat stress if used improperly” (Bernard 2004). US Senate 1983.
Following the European heatwave of August 2003, which led to an estimated 30,000 excess deaths (Robine 2008), some countries developed ‘heat health warning systems’ (Kovats 2006). Alongside a meteorological alert system, a main component of these systems is provision of public health recommendations and actions to prevent heat‐related morbidity and mortality (Kovats 2006). There is a need for these recommendations to be based on the most up to date and available evidence but, in the case of advice on electric fans, the recommendations are not well supported by the evidence (Hajat 2010). One hypothesis suggests that the use of fans may contribute to an increased risk of potentially life threatening heat illness when the ambient air temperature is above body temperature, because of an increase in the rate of dehydration (DCLG 2008; Hajat 2010; Kovats 2006; WHO 2009). In addition, when ambient temperature is higher than skin temperature (35 °C), it has been theorized that an electric fan can increase convective heat gain by blowing hot air over the body (Lee 1980). This can cause heat exhaustion to occur more rapidly (Ibrahim 2012). However, the temperature threshold at which fans are contraindicated varies within the literature. Some suggest 35 ºC and others 37 ºC (Kovats 2006; WHO 2009). It has also been argued that temperature alone is not a sufficient indicator of effect and attention towards concurrent high humidity levels or a person’s inability to sweat, as well as other physiological mechanisms (such as chronic illness, age and medications), need to be taken into account (DCLG 2008; Hajat 2010). High humidity and lack of sweating (anhydrosis) reduces the ability for heat to be released through evaporative cooling (DCLG 2008; Hajat 2010). However, it has been suggested that if a person is unable to sweat because of physical, pharmaceutical or physiological reasons, then air movement will be of benefit to them if water is sprinkled onto their skin first (misting) (DCLG 2008). High humidity has been proposed as one of the reasons why advice on fan use often differs between countries with varying levels of humidity (Hajat 2010).
Climate modelling by the Intergovernmental Panel on Climate Change (IPCC) has shown that it is very likely that heatwaves will increase in duration, frequency and intensity as a result of climate change (IPCC 2012). This indicates that heatwave‐related health protection recommendations will need to be put into action with increasing frequency as the climate warms and extremes of temperature become more common. In considering this, cooling interventions such as air conditioning units might be unsustainable in a warming climate for a number of reasons. This is because of the positive feedback loop they create through their high energy consumption, which will further add to climate change by increasing emissions, the increased risk of blackouts due to pressures on the energy grid, and their high operational cost. It is also important to highlight that 'ownership of electric fan' is at best a proxy indicator to actual behavior (for example the use of such a device during a heatwave or temperature stress) among population subgroups. It needs to be considered that although people may own an electric fan, they may not use it due to fear of robbery through leaving windows open, the cost of higher utility bills, inability to open windows, or failure to use the fan properly because of a lack of knowledge. In order to provide the high quality evidence to support public health protection programs and policy making, future studies should also be built on the understanding of socio‐demographic differences in health risk awareness and temperature sensitivity towards device utilization, factors impacting on or affecting device ownership (such as cost), and capacity to respond (including lack of knowledge of when and how to use the device).
In summary, in light of the increased risk of future heatwaves, the unsustainability of air conditioning and the current uncertainty over the health effects of electric fans, there is a need for future research into their health impacts during heatwaves. This research should take the form of randomised trials (see Implications for research) so that the evidence base on their potential benefits and harms can be strengthened. This will in turn inform public health recommendations within heatwave policies around the world.
Authors' conclusions
Implications for practice.
In light of the lack of any eligible studies for this review and the uncertainties around the effects of electric fans in the observational studies that we identified, and the potential for harm as well as for benefit in their use, this review does not support or refute the use of electric fans during heatwaves. People making decisions on their own behalf, on behalf of others or for inclusion within local or national guidance and policies should consider the current state of the evidence base when making a choice about whether or not to use or supply electric fans.
The main implication of this review is that research is needed to resolve the long standing and ongoing uncertainty about the benefits and harms of using electric fans during a heatwave. Therefore, decision makers and policy makers may wish to help resolve this uncertainty by encouraging and conducting the type of research that is needed to measure reliably the benefits and harms of using electric fans during a heatwave. Any findings of future research in this area would have potential implications not only for individuals, but also have significant influence on the evidence base on which policy (local, national and international) is based. Such research findings would serve to potentially strengthen national heat wave plans and health care guidance. Public health professionals may wish to give details regarding the potential benefits and disadvantages of using an electric fan during a heatwave, to help individuals make informed decisions regarding their use.
Implications for research.
The need for research to resolve the ongoing uncertainties about the potential beneficial and harmful effects of the use of electric fans during heatwaves was highlighted by several of the studies that we found, but which were not eligible for this review because of their study design. For example, Semenza et al wrote “The effectiveness of fans in preventing death during periods of high heat and humidity remains a matter of controversy and deserves further attention” (Semenza 1996); and Bouchama et al drew the general conclusion that “other common recommendations, such as using a fan, drinking extra water, taking extra showers, and reducing outdoor activities, would need further evaluation, particularly as they are not without potential adverse effects” (Bouchama 2007). We obtained similar views from our correspondence with various international organisations as well as policy makers across the world.
No reliable evidence to estimate the effects of electric fans during heatwaves has been found for this Cochrane Review. Such evidence could be generated by an appropriate randomised trial in a naturally occurring heatwave of electric fans versus no fans within the general adult population of an area, but with a focus on older people, measuring outcomes such as heat‐related morbidity and mortality. We have, therefore, suggested the design for one such trial using the framework proposed by Brown et al (Brown 2006) (Table 3). This design has been provided as an outline only and the details would need to be adapted to the area in which any such a study is undertaken. Furthermore, studies of this topic might adopt similar methods to those used in studies to determine the effects of smoke alarms in residential settings (DiGuiseppi 2001).
3. Design of a randomised trial.
| Element | Example |
| Existing evidence | Estimates of the effects of electric fans currently rely on retrospective observational research (case‐control studies). This Cochrane review did not find any randomised trials or other prospective comparisons of electric fans versus no fans. |
| Population | Adults of any age with or without co‐morbidity who are likely to be representative of general population, with a particular focus on participants aged 65 years or older, people in residential or care homes; who are exposed to a naturally occurring heatwave. |
| Intervention | Electric fan most suitable or practical for the setting (e.g. window, ceiling etc). |
| Comparison | Routine care. |
| Outcomes | Use of healthcare services (including phone calls to advice lines, visits to health website, attendance at primary care, emergency department visits) Hospitalisation (due to heat related illness) Hospitalisation (due to any cause) Death (due to heat related illness Death (from any cause) Self‐reported comfort |
| Timing | During the heatwave |
| Study design | Randomised trial, possibly a cluster trial with randomisation of specific settings (e.g. care homes) or areas (e.g. small geographic regions). |
We recognise that there are some characteristics of such a study which would make it particularly challenging. For example, the unpredictable nature of extreme events such as heatwaves, where the researchers would need to adopt a watch and wait approach with the trial and the necessary resources being ready to activate, potentially for several years. Examples already exist of such plans, for example in a series of studies funded by the National Institute for Health Research in the UK which will be activated in an influenza pandemic and the work of the International Severe Acute Respiratory Infection Consortium (ISARIC) (Yong 2012).
It would also be important to ensure that any recommendations on interventions to be used, either alongside the electric fans or as a comparator, are evidence‐based. This systematic review has not assessed the evidence behind any of the other interventions used in heatwaves and even where evidence is available the comparisons would have to be done carefully. For example, a comparison of the effects of electric fans versus air conditioning on health and environmental impact would be dependent on the context of their use, particularly in terms of the comfort temperature requirements of the occupants, the level of heat gain in the space and zoning. Air conditioning energy use may be affected by choice of local or multiple room systems, or their unintentional combination via doors and stairways, the outside air heat rejection temperatures coincident with operation, and the selection and appropriate setting of controls for comfortable temperatures and operating periods. The comparison with air conditioning is therefore not straightforward due to the variations in system choice and method of operation. Comparisons may also need to consider the ability of fans to manage high internal heat gain and noise generation issues.
Another challenge might be to ensure that all important aspects of the atmosphere ( meteorological conditions such as wind speed, humidity, temperature inside various rooms, insulation of building, placement of doors and windows, etc) can be measured and reported accurately, reliably and consistently to show that any effect attributed to the electric fans is not affected by confounding by any other factor.
What's new
| Date | Event | Description |
|---|---|---|
| 10 July 2017 | Review declared as stable | Currently not a priority topic area. |
History
Protocol first published: Issue 5, 2012 Review first published: Issue 7, 2012
| Date | Event | Description |
|---|---|---|
| 1 April 2015 | Amended | Contact details updated. |
| 24 February 2015 | Amended | Contact details updated. |
| 11 February 2015 | Amended | Contact details updated. |
| 27 March 2014 | Amended | Contact details updated. |
Notes
Currently not a priority topic area.
Acknowledgements
We are grateful to Sheila O'Malley of Health Protection Agency for running the search strategy and extracting the relevant articles, Kate Misso of Kleijnen Systematic Reviews Ltd for reviewing the search strategy, and Dr Rosamund Southgate and Professor Kevin Hung for assisting with the search of the Chinese literature.
Appendices
Appendix 1. Initial search strategy for MEDLINE, EMBASE and CINAHL
1. MEDLINE; heatwave*.ti,ab; 116 results. 2. MEDLINE; (heat AND wave*).ti,ab; 2351 results. 3. MEDLINE; heat‐wave*.ti,ab; 507 results. 4. MEDLINE; (hot AND temperature*).ti,ab; 6182 results. 5. MEDLINE; (high AND temperature*).ti,ab; 83359 results. 6. MEDLINE; (hot AND weather).ti,ab; 535 results. 7. MEDLINE; *EXTREME HEAT/; 32 results. 8. MEDLINE; *HEAT EXHAUSTION/; 1064 results. 9. MEDLINE; *HEAT STRESS DISORDERS/; 1226 results. 10. MEDLINE; 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9; 91759 results. 11. MEDLINE; fan*.ti,ab; 15989 results. 12. MEDLINE; *AIR CONDITIONING/; 1149 results. 13. MEDLINE; *AIR MOVEMENTS/; 597 results. 14. MEDLINE; *BODY TEMPERATURE REGULATION/; 12224 results. 15. MEDLINE; (evaporative AND cool*).ti,ab; 464 results. 16. MEDLINE; 11 OR 12 OR 13 OR 14 OR 15; 30132 results. 17. MEDLINE; 10 AND 16; 1739 results. 18. EMBASE; heatwave*.ti,ab; 136 results. 19. EMBASE; (heat AND wave*).ti,ab; 2330 results. 20. EMBASE; heat‐wave*.ti,ab; 572 results. 21. EMBASE; (hot AND temperature*).ti,ab; 6648 results. 22. EMBASE; (high AND temperature*).ti,ab; 87128 results. 23. EMBASE; (hot AND weather).ti,ab; 627 results. 24. EMBASE; *EXTREME HEAT/; 12767 results. 25. EMBASE; *HEAT EXHAUSTION/; 604 results. 26. EMBASE; *HEAT STRESS DISORDERS/; 828 results. 27. EMBASE; 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26; 105797 results. 28. EMBASE; fan*.ti,ab; 18378 results. 29. EMBASE; *AIR CONDITIONING/; 3728 results. 30. EMBASE; *AIR MOVEMENTS/; 4028 results. 31. EMBASE; *BODY TEMPERATURE REGULATION/; 11120 results. 32. EMBASE; (evaporative AND cool*).ti,ab; 470 results. 33. EMBASE; 28 OR 29 OR 30 OR 31 OR 32; 37347 results. 34. EMBASE; 27 AND 33; 2184 results. 35. CINAHL; heatwave*.ti,ab; 50 results. 36. CINAHL; (heat AND wave*).ti,ab; 146 results. 37. CINAHL; heat‐wave*.ti,ab; 106 results. 38. CINAHL; (hot AND temperature*).ti,ab; 373 results. 39. CINAHL; (high AND temperature*).ti,ab; 1244 results. 40. CINAHL; (hot AND weather).ti,ab; 106 results. 41. CINAHL; *HEAT STRESS DISORDERS/; 348 results. 42. CINAHL; *HEAT EXHAUSTION/; 159 results. 43. CINAHL; 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42; 2180 results. 44. CINAHL; fan*.ti,ab; 1373 results. 45. CINAHL; *AIR CONDITIONING/; 58 results. 46. CINAHL; *BODY TEMPERATURE REGULATION/; 539 results. 47. CINAHL; (evaporative AND cool*).ti,ab; 14 results. 48. CINAHL; 44 OR 45 OR 46 OR 47; 1980 results. 49. CINAHL; 43 AND 48; 118 results.
Appendix 2. Peer reviewed search strategy for MEDLINE, EMBASE and CINAHL
1. MEDLINE; heatwave*.ti,ab; 122 results. 2. MEDLINE; (heat AND wave*).ti,ab; 2408 results. 3. MEDLINE; heat‐wave*.ti,ab; 530 results. 4. MEDLINE; (hot AND temperature*).ti,ab; 6302 results. 5. MEDLINE; (high AND temperature*).ti,ab; 85060 results. 6. MEDLINE; (hot AND weather).ti,ab; 547 results. 7. MEDLINE; *EXTREME HEAT/; 36 results. 8. MEDLINE; *HEAT EXHAUSTION/; 1065 results. 9. MEDLINE; *HEAT STRESS DISORDERS/; 1243 results. 10. MEDLINE; 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9; 93610 results. 11. MEDLINE; fan*.ti,ab; 16246 results. 12. MEDLINE; *AIR CONDITIONING/; 1155 results. 13. MEDLINE; *AIR MOVEMENTS/; 606 results. 14. MEDLINE; *BODY TEMPERATURE REGULATION/; 12284 results. 15. MEDLINE; (evaporative AND cool*).ti,ab; 472 results. 16. MEDLINE; 11 OR 12 OR 13 OR 14 OR 15; 30467 results. 17. MEDLINE; 10 AND 16; 1757 results. 18. EMBASE; heatwave*.ti,ab; 143 results. 19. EMBASE; (heat AND wave*).ti,ab; 2427 results. 20. EMBASE; heat‐wave*.ti,ab; 610 results. 21. EMBASE; (hot AND temperature*).ti,ab; 6851 results. 22. EMBASE; (high AND temperature*).ti,ab; 89879 results. 23. EMBASE; (hot AND weather).ti,ab; 647 results. 24. EMBASE; *EXTREME HEAT/; 13563 results. 25. EMBASE; *HEAT EXHAUSTION/; 619 results. 26. EMBASE; *HEAT STRESS DISORDERS/; 873 results. 27. EMBASE; 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26; 109534 results. 28. EMBASE; fan*.ti,ab; 18985 results. 29. EMBASE; *AIR CONDITIONING/; 3825 results. 30. EMBASE; *AIR MOVEMENTS/; 4247 results. 31. EMBASE; *BODY TEMPERATURE REGULATION/; 11379 results. 32. EMBASE; (evaporative AND cool*).ti,ab; 482 results. 33. EMBASE; 28 OR 29 OR 30 OR 31 OR 32; 38538 results. 34. EMBASE; 27 AND 33; 2259 results. 35. CINAHL; heatwave*.ti,ab; 50 results. 36. CINAHL; (heat AND wave*).ti,ab; 149 results. 37. CINAHL; heat‐wave*.ti,ab; 109 results. 38. CINAHL; (hot AND temperature*).ti,ab; 379 results. 39. CINAHL; (high AND temperature*).ti,ab; 1272 results. 40. CINAHL; (hot AND weather).ti,ab; 106 results. 41. CINAHL; *HEAT STRESS DISORDERS/; 353 results. 42. CINAHL; *HEAT EXHAUSTION/; 159 results. 43. CINAHL; 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42; 2217 results. 44. CINAHL; fan*.ti,ab; 1385 results. 45. CINAHL; *AIR CONDITIONING/; 59 results. 46. CINAHL; *BODY TEMPERATURE REGULATION/; 549 results. 47. CINAHL; (evaporative AND cool*).ti,ab; 14 results. 48. CINAHL; 44 OR 45 OR 46 OR 47; 2003 results. 49. CINAHL; 43 AND 48; 120 results. 50. EMBASE; heatwave*.ti,ab; 143 results. 51. EMBASE; ((heat adj4 wave*)).ti,ab; 733 results. 52. EMBASE; (((hot OR high) adj3 temperature*)).ti,ab; 25219 results. 53. EMBASE; (hot AND weather).ti,ab; 647 results. 54. EMBASE; *HEAT/ OR *HEAT STRESS/; 15758 results. 55. EMBASE; exp HEAT INJURY/; 5040 results. 56. EMBASE; exp THERMAL EXPOSURE/; 2856 results. 57. EMBASE; exp HEAT SHOCK RESPONSE/; 1949 results. 58. EMBASE; (sunstroke* OR sun‐strokes*).ti,ab; 38 results. 59. EMBASE; ((thermal* OR heat) adj4 (discomfort* OR comfort* OR toleran* OR intoleran* OR distress* OR injur* OR illness* OR trauma*)).ti,ab; 10087 results. 60. EMBASE; 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59; 57016 results. 61. EMBASE; (fan OR fans OR fanned OR fanning).ti,ab; 4205 results. 62. EMBASE; (air adj2 (cooler* OR condition*)).ti,ab; 3621 results. 63. EMBASE; (AC OR climat* AND control*).ti,ab; 10770 results. 64. EMBASE; *AIR CONDITIONING/; 3825 results. 65. EMBASE; *COLD AIR/; 169 results. 66. EMBASE; (evaporat* adj4 cool*).ti,ab; 459 results. 67. EMBASE; 50 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66; 22236 results. 68. EMBASE; 60 AND 67; 991 results. 69. EMBASE; 68 [Limit to: Human]; 499 results. 70. MEDLINE; heatwave*.ti,ab; 122 results. 71. MEDLINE; (heat adj4 wave*).ti,ab; 656 results. 72. MEDLINE; ((hot OR high) adj3 temperature*).ti,ab; 25381 results. 73. MEDLINE; (hot AND weather).ti,ab; 547 results. 74. MEDLINE; *EXTREME HEAT/; 36 results. 75. MEDLINE; *HEAT EXHAUSTION/; 1065 results. 76. MEDLINE; ((thermal* OR heat) adj4 (discomfort* OR comfort* OR toleran* OR intoleran* OR distress* OR injur* OR illness* OR trauma*)).ti,ab; 9195 results. 77. MEDLINE; (sunstroke* OR sun‐stroke*).ti,ab; 54 results. 78. MEDLINE; *HEAT STRESS DISORDERS/; 1243 results. 79. MEDLINE; 70 OR 71 OR 72 OR 73 OR 74 OR 75 OR 76 OR 77 OR 78; 36773 results. 80. MEDLINE; (fan OR fans OR fanned OR fanning).ti,ab; 3626 results. 81. MEDLINE; (air adj2 (cooler* OR condition*)).ti,ab; 2793 results. 82. MEDLINE; (AC OR climat* AND control*).ti,ab; 8897 results. 83. MEDLINE; *AIR CONDITIONING/; 1155 results. 84. MEDLINE; *AIR MOVEMENTS/; 606 results. 85. MEDLINE; (evaporat* adj4 cool*).ti,ab; 437 results. 86. MEDLINE; 80 OR 81 OR 82 OR 83 OR 84 OR 85; 16792 results. 87. MEDLINE; 79 AND 86; 578 results. 88. MEDLINE; 87 [Limit to: Humans]; 308 results. 89. CINAHL; heatwave*.ti,ab; 50 results. 90. CINAHL; (heat adj4 wave*).ti,ab; 113 results. 91. CINAHL; (hot adj3 temperature*).ti,ab; 99 results. 92. CINAHL; (high adj3 temperature*).ti,ab; 289 results. 93. CINAHL; (hot AND weather).ti,ab; 106 results. 94. CINAHL; *HEAT/; 1360 results. 95. CINAHL; *HEAT EXHAUSTION/; 159 results. 96. CINAHL; (heat ADJ discomfort*).ti,ab; 2 results. 97. CINAHL; (heat ADJ comfort*).ti,ab; 5 results. 98. CINAHL; (heat ADJ toleran*).ti,ab; 38 results. 99. CINAHL; (heat ADJ intoleran*).ti,ab; 17 results. 100. CINAHL; (heat ADJ distress*).ti,ab; 2 results. 101. CINAHL; (heat ADJ injur*).ti,ab; 99 results. 102. CINAHL; (heat ADJ illness*).ti,ab; 194 results. 103. CINAHL; (heat ADJ trauma*).ti,ab; 15 results. 104. CINAHL; (thermal* AND discomfort*).ti,ab; 35 results. 105. CINAHL; (thermal* AND comfort*).ti,ab; 76 results. 106. CINAHL; (thermal* AND toleran*).ti,ab; 82 results. 107. CINAHL; (thermal* AND intoleran*).ti,ab; 9 results. 108. CINAHL; (thermal* AND distress*).ti,ab; 23 results. 109. CINAHL; (thermal* AND injur*).ti,ab; 810 results. 110. CINAHL; (thermal* AND illness*).ti,ab; 39 results. 111. CINAHL; (thermal* AND trauma*).ti,ab; 133 results. 112. CINAHL; (sunstroke* OR sun‐stroke*).ti,ab; 5 results. 113. CINAHL; *HEAT STRESS DISORDERS/; 353 results. 114. CINAHL; 89 OR 90 OR 91 OR 92 OR 93 OR 94 OR 95 OR 96 OR 97 OR 98 OR 99 OR 100 OR 101 OR 102 OR 103 OR 104 OR 105 OR 106 OR 107 OR 108 OR 109 OR 110 OR 111 OR 112 OR 113; 3287 results. 115. CINAHL; (fan OR fans OR fanned OR fanning).ti,ab; 382 results. 116. CINAHL; (air adj2 cooler*).ti,ab; 1 results. 117. CINAHL; (air adj2 condition*).ti,ab; 205 results. 118. CINAHL; (AC OR climat* AND control*).ti,ab; 1367 results. 119. CINAHL; *AIR CONDITIONING/; 59 results. 120. CINAHL; *AIR/; 214 results. 121. CINAHL; (evaporat* adj4 cool*).ti,ab; 17 results. 122. CINAHL; 115 OR 116 OR 117 OR 118 OR 119 OR 120 OR 121; 2197 results. 123. CINAHL; 114 AND 122; 77 results. 124. CINAHL; 123 [Limit to: (Gender Female or Male)]; 25 results. 125. MEDLINE; 79 NOT 10; 7921 results. 126. MEDLINE; 86 NOT 16; 11013 results. 127. MEDLINE; 125 AND 126; 54 results. 128. EMBASE; 60 NOT 27; 16240 results. 129. EMBASE; 67 NOT 33; 13779 results. 130. EMBASE; 128 AND 129; 107 results. 131. MEDLINE,EMBASE; Duplicate filtered: [125 AND 126], [128 AND 129]; 161 results.
Differences between protocol and review
We were unable to search some of the databases that we had planned to search.
Contributions of authors
The protocol was drafted by SG, VM and MC; and approved by all authors. The full review was drafted by MC, SG and CC; and approved by all authors. All authors were involved in assessing the eligibility of identified studies.
Sources of support
Internal sources
Centre for Radiation, Chemicals and Environmental Hazards, Health Protection Agency, UK.
Climate Change and Health Office, Health Canada, Ottawa, Canada.
Centre for Public Health, Queens University Belfast, Belfast, Ireland.
Evidence Aid/The Cochrane Collaboration, Oxford, UK.
External sources
No sources of support supplied
Declarations of interest
None known
Stable (no update expected for reasons given in 'What's new')
References
Additional references
Allen 2009
- Allen A, Segal‐Gidan F. Heat related illness in the elderly. Clinical Geriatrics 2009:37‐45. [Google Scholar]
Analitis 2009
- Analitis A, Becker P, Biggeri A, Bouchama A, De'Donato F, D'Ippoliti D, et al. Improving public health responses to extreme weather/heat‐waves: EuroHEAT. WHO (Regional Office for Europe), 2009. [Google Scholar]
Applegate 1981
- Applegate WB, Runyan JW Jr, Brasfield L, Williams ML, Konigsberg C, Foucbe C. Analysis of the 1980 heat wave in Memphis. Journal of the American Geriatrics Society 1981;29(8):337‐42. [DOI] [PubMed] [Google Scholar]
Austin 1956
- Austin MG, Berry JW. Observations on one hundred cases of heatstroke. JAMA 1956;161:1525‐9. [DOI] [PubMed] [Google Scholar]
Barwood 2009
- Barwood MJ, Davey S, House JR, Tipton MJ. Post‐exercise cooling techniques in hot, humid conditions. European Journal of Applied Physiology and Occupational Physiology 2009;107(4):385‐96. [DOI] [PubMed] [Google Scholar]
Bernard 2004
- Bernard SM, McGeehin MA. Municipal heat wave response plans. American Journal of Public Health 2004;94(9):1520‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bouchama 2007
- Bouchama A, Dehbi M, Mohamed G, Matthies F, Shoukri M, Menne B. Prognostic factors in heat wave related deaths: a meta‐analysis. Archives of Internal Medicine 2007;167:2170‐6. [PUBMED: 17698676] [DOI] [PubMed] [Google Scholar]
Brown 2006
- Brown P, Brunnhuber K, Chalkidou K, Chalmers I, Clarke M, Fenton M, et al. How to formulate research recommendations. BMJ 2006;333(7572):804‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter 1999
- Carter JB, Banister EW, Morrison JB. Effectiveness of rest pauses and cooling in alleviation of heat stress during simulated fire‐fighting activity. Ergonomics 1999;42(2):299‐313. [DOI] [PubMed] [Google Scholar]
Chan 2011
- Chan EY, Goggins WB, Kim JJ, Griffiths S, Ma TK. Help‐seeking behavior during elevated temperature in Chinese population. Journal of Urban Health 2011;88(4):637‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
DCLG 2008
- Department of Communities and Local Government. Review of Health and Safety Risk Drivers. Department of Communities and Local Government, 2008. [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
DH 2011
- Department of Health. Heatwave Plan for England. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_127235.pdf 2011.
DiGuiseppi 2001
- DiGuiseppi C, Goss CW, Higgins JPT. Interventions for promoting smoke alarm ownership and function. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD002246] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duffield 2008
- Duffield R. Cooling interventions for the protection and recovery of exercise performance from exercise‐induced heat stress. Medicine and Sport Science 2008;53:89‐103. [DOI] [PubMed] [Google Scholar]
Fouillet 2008
- Fouillet A, Rey G, Wagner V, Laaidi K, Empereur‐Bissonnet P, Tertre A, et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. International Journal of Epidemiology 2008;37(2):309‐17. [PUBMED: 18194962] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ghersi 2009
- Ghersi D, Pang T. From Mexico to Mali: four years in the history of clinical trial registration. Journal of Evidence‐Based Medicine 2009;2:1‐7. [DOI] [PubMed] [Google Scholar]
Grogan 2002
- Grogan H, Hopkins PM. Heat stroke: implications for critical care and anaesthesia. British Journal of Anaesthesia 2002;88(5):700‐7. [PUBMED: 12067009] [DOI] [PubMed] [Google Scholar]
Hajat 2010
- Hajat S, O’Conner M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet 2010;375:856‐63. [DOI] [PubMed] [Google Scholar]
Harris 2007
- Harris BA, Andrews PJ, Murray GD. Enhanced upper respiratory tract airflow and head fanning reduce brain temperature in brain‐injured, mechanically ventilated patients: a randomized, crossover, factorial trial. British Journal of Anaesthesia 2007;98(1):93‐9. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Horsley 2011
- Horsley T, Dingwall O, Sampson M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.MR000026.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hostler 2010
- Hostler D, Reis SE, Bednez JC, Kerin S, Suyama J. Comparison of active cooling devices with passive cooling for rehabilitation of firefighters performing exercise in thermal protective clothing: a report from the Fireground Rehab Evaluation (FIRE) trial. Prehospital Emergency Care 2010;14(3):300‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
HPA 2011
- Health Protection Agency. Heatwave Questions and Answers. www.hpa.org.uk/Topics/EmergencyResponse/ExtremeWeatherEventsAndNaturalDisasters/Heatwaves/HeatwaveQuestionsAndAnswers/ (accessed 17 April 2012).
Ibrahim 2010
- Ibrahim JE, McInnes JA, Andrianopoulos N, Evans S. Minimising harm to older persons from heatwaves: a survey of the awareness, knowledge and practices of community‐based health professionals and care providers in Victoria, Australia. Injury Prevention 2010;16:A84. [DOI] [PubMed] [Google Scholar]
Ibrahim 2012
- Ibrahim JE, McInnes JA, Andrianopoulos N, Evans S. Minimising harm from heatwaves: a survey of awareness, knowledge, and practices of health professionals and care providers in Victoria, Australia. International Journal of Public Health 2012;57:297‐304. [DOI] [PubMed] [Google Scholar]
IPCC 2012
- Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, et al. Summary for Policymakers. In: Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change. Cambridge University Press, Cambridge, UK 2012:1‐19.
Kaiser 2001
- Kaiser R, Rubin CH, Henderson AK, Wolfe MI, Kieszak S, Parrott CL, et al. Heat‐related death and mental illness during the 1999 Cincinnati heat wave. The American Journal of Forensic Medicine and Pathology 2001;22(3):303‐7. [PUBMED: 11563746] [DOI] [PubMed] [Google Scholar]
Kenny 2010
- Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O. Heat stress in older individuals and patients with common chronic diseases. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne 2010;182(10):1053‐60. [PUBMED: 19703915] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kilbourne 1982
- Kilbourne EM, Choi K, Jones TS, Thacker SB, and The Field Investigation Team. Risk factors for heatstroke: a case‐control study. JAMA 1982;247:3332‐6. [PubMed] [Google Scholar]
Kirkham 2010
- Kirkham JJ, Dwan KM, Altman DG, Gamble C, Dodd S, Smyth R, Williamson PR. The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ 2010;340:c356. [DOI] [PubMed] [Google Scholar]
Koppe 2004
- Koppe C, Kovats S, Jendritzky G, Menne B. Heat‐waves: risks and responses. Health and Global Environmental Change. Series, No. 2. WHO (Regional Office for Europe), 2004. [Google Scholar]
Kovats 2006
- Kovats RS, Ebi K. Heatwaves and public health in Europe. European Journal of Public Health 2006;16(6):592‐9. [DOI] [PubMed] [Google Scholar]
Kovats 2008
- Kovats S, Hajat S. Heat stress and public health: a critical review. Annual Review of Public Health 2008;29:41‐55. [DOI] [PubMed] [Google Scholar]
Lee 1980
- Lee DH. Seventy‐five years of searching for a heat index. Environmental Research 1980;22:331‐56. [DOI] [PubMed] [Google Scholar]
Lorente 2005
- Lorente C, Sérazin C, Salines G, Adonias G, Gourvellec G, Lauzeille D, et al. [Etude des facteurs de décès des personnes âgées résidant en établissement durant la vague de chaleur d’août 2003]. Etude des facteurs de décès des personnes âgées résidant en établissement durant la vague de chaleur d’août 2003. 2005. [Google Scholar]
Matthies 2008
- Matthies F, Bickler G, Marín NC, Hales S. Heat‐health action plans. WHO (Regional Office for Europe), 2008. [Google Scholar]
McGeehin 2001
- McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature‐related morbidity and mortality in the United States. Environmental health perspectives 2001;109 Suppl 2:185‐9. [PUBMED: 11359685] [DOI] [PMC free article] [PubMed] [Google Scholar]
Naughton 2002
- Naughton MP, Henderson A, Mirabelli MC, Kaiser R, Wilhelm JL, Kieszak SM, et al. Heat‐related mortality during a 1999 heat wave in Chicago. American Journal of Preventive Medicine 2002;22(4):221‐7. [PUBMED: 11988377] [DOI] [PubMed] [Google Scholar]
Poulton 1987
- Poulton TJ, Walker RA. Helicopter cooling of heatstroke victims. Aviation Space and Environmental Medicine 1987;58(4):358‐61. [PubMed] [Google Scholar]
Riggs 1981
- Riggs CE, Johnson DJ, Konopka BJ, Kilgour RD. Exercise heart rate response to facial cooling. European Journal of Applied Physiology and Occupational Physiology 1981;47:323‐30. [DOI] [PubMed] [Google Scholar]
Robine 2008
- Robine JM, Cheung SL, Roy S, Oyen H, Griffiths C, Michel JP, Herrmann FR. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes Rendus Biologie 2008;331(2):171‐8. [PUBMED: 18241810] [DOI] [PubMed] [Google Scholar]
Semenza 1996
- Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders A, Howe HL, Wilhelm JL. Heat‐related deaths during the July 1995 heat wave in Chicago. New England Journal of Medicine 1996;335:84‐90. [DOI] [PubMed] [Google Scholar]
Shahid 1999
- Shahid MS, Hatle L, Mansour H, Mimish L. Echocardiographic and Doppler study of patients with heatstroke and heat exhaustion. International Journal of Cardiac Imaging 1999;15(4):279‐85. [PUBMED: 10517377] [DOI] [PubMed] [Google Scholar]
Shemilt 2011
- Shemilt I, Mugford M, Byford S, Drummond M, Eisenstein E, Knapp M, et al. Chapter 15: Incorporating economics evidence. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Skinner 2002
- Skinner RD. Temperature regulation and sleep. In: Lee‐Choing TL, Sateia M, Carskadon MA editor(s). Sleep Medicine. Hanley and Belflus, 2002:Chapter 9. [Google Scholar]
US Senate 1983
- US Senate Special Commission on Aging. Heat Stress and Older Americans: Problems and Solutions. Washington, DC: US Government Printing Office, 1983. [Google Scholar]
Vandentorren 2006
- Vandentorren S, Bretin P, Zeghnoun A, Mandereau‐Bruno L, Croisier A, Cochet C, et al. August 2003 heat wave in France: Risk factors for death of elderly people living at home. European Journal of Public Health 2006;16:583‐91. [DOI] [PubMed] [Google Scholar]
WHO 2009
- World Health Organization. Improving public health responses to extreme weather/heat‐waves: EuroHEAT ‐ Technical Summary. Copenhagen: WHO Regional Office for Europe, 2009. [Google Scholar]
Yong 2012
- Yong E. Trials at the ready: preparing for the next pandemic. BMJ (Clinical research ed.) 2012;344:e2982. [PUBMED: 22556048] [DOI] [PubMed] [Google Scholar]
Young 2011
- Young T, Hopewell S. Methods for obtaining unpublished data. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.MR000027.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2009
- Zhang M, Diao QY, Zhao GQ, Jiang CG, Tu Y. The impact of drinking water temperature and fan use on welfare of sheep in summer. Animal Husbandry and Veterinary Medicine 2009;41(6):44‐6. [Google Scholar]
References to other published versions of this review
Gupta 2012
- Gupta S, Murray V, Clarke MJ, Carmichael C, Allen C, Simpson C. Electric fans for reducing adverse health impacts in heatwaves. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD009888] [DOI] [PMC free article] [PubMed] [Google Scholar]


