Abstract
Background
Immunosuppressed cancer patients are at increased risk of serious influenza‐related complications. Guidelines, therefore, recommend influenza vaccination for these patients. However, data on vaccine effectiveness in this population is lacking, and the value of vaccination in this population remains unclear.
Objectives
To assess the effectiveness of influenza vaccine in immunosuppressed adults with malignancies. The primary review outcome is all‐cause mortality, preferably at the end of the influenza season. Influenza‐like illness (ILI, a clinical definition), confirmed influenza, pneumonia, any hospitalization and influenza‐related mortality were defined as secondary outcomes.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and LILACS databases up to August 2013. We searched the following conference proceedings: ICAAC, ECCMID, IDSA (infectious disease conferences), ASH, ASBMT, EBMT (hematological), and ASCO (oncological) between the years 2006 to 2010. In addition, we scanned the references of all identified studies and pertinent reviews. We searched the websites of the manufacturers of influenza vaccine. Finally, we searched for ongoing or unpublished trials in clinical trial registry databases using the website.
Selection criteria
Randomized controlled trials (RCTs), prospective and retrospective cohort studies and case‐control studies were considered, comparing inactivated influenza vaccines versus placebo, no vaccination or a different vaccine, in adults (16 years and over) with cancer. We considered solid malignancies treated with chemotherapy, haematological cancer patients treated or not treated with chemotherapy, cancer patients post‐autologous (up to six months after transplantation) or allogeneic (at any time) hematopoietic stem cell transplantation.
Data collection and analysis
Two review authors independently assessed the risk of bias and extracted data from included studies adhering to Cochrane methodology. Meta‐analysis could not be performed because of different outcome and denominator definitions in the included studies.
Main results
We identified four studies: one RCT and three observational studies, including 2124 participants. One study reported results in person‐years while the other three reported per person. The studies were performed between 1993 and 2012 and included adults with haematological diseases (two studies), patients following bone marrow transplantation (one study) and solid malignancies (three studies). Only two observational studies reported all‐cause mortality; one showing an adjusted hazard ratio (HR) of 0.88 (95% CI 0.77 to 0.99) for death with vaccination and the other reporting an odds ratio (OR) of 0.43 (95% CI 0.26 to 0.71). The RCT reported a statistically significant reduction in ILI with vaccination, while no difference was observed in one observational study. Confirmed influenza rates were lower with vaccination in the three observational studies, the difference reaching statistical significance in one. Pneumonia was observed significantly less frequently with vaccination in one observational study, but no difference was detected in another or in the RCT. The RCT showed a reduction in hospitalizations following vaccination, while an observational study found no difference. No life‐threatening or persistent adverse effects from vaccination were reported. The strength of evidence is limited by the low number of included studies and by their low methodological quality (high risk of bias).
Authors' conclusions
Observational data suggests a lower mortality with influenza vaccination. Infection‐related outcomes were lower or similar with influenza vaccination. The strength of evidence is limited by the small number of studies and by the fact that only one was a RCT. Influenza vaccination is safe and the evidence, although weak, is in favour of vaccinating adults with cancer receiving chemotherapy.
Keywords: Adult; Humans; Bone Marrow Transplantation; Case‐Control Studies; Cause of Death; Cohort Studies; Hematologic Neoplasms; Hematologic Neoplasms/immunology; Hematologic Neoplasms/mortality; Immunocompromised Host; Immunocompromised Host/immunology; Influenza Vaccines; Influenza Vaccines/administration & dosage; Influenza Vaccines/immunology; Influenza, Human; Influenza, Human/epidemiology; Influenza, Human/immunology; Influenza, Human/prevention & control; Neoplasms; Neoplasms/immunology; Neoplasms/mortality; Observational Studies as Topic; Randomized Controlled Trials as Topic
Influenza (flu) vaccination for preventing influenza in adults with cancer
Adults with cancer are prone to serious complications from influenza, more than healthy adults. The influenza vaccine protects against influenza and its complications. However, its effectiveness among cancer patients is unclear, as the immune dysfunction that accompanies cancer and as a result of chemotherapy might lower immune response to the vaccine. Cancer patients, therefore, do not have clear information on the importance, need and safety of the vaccine.
This review focused on the effectiveness of influenza vaccination in adults with cancer who have a suppressed immune system because of the cancer or chemotherapy. We identified four clinical studies addressing this question, only one of which was a randomized controlled trial, where patients were randomly selected to get or not to get the vaccine. Two studies showed that adults with cancer who were vaccinated were found to have lower rates of death, but these studies were not randomized. Pooling (combining) results from the different studies was not possible because of different methods or different way of reporting results. There was a significantly lower rate of influenza‐like illness (any febrile respiratory illness), pneumonia, confirmed influenza and hospitalization, for any reason, among vaccine recipients in at least one study for each outcome. No side‐effects to the vaccine were reported in these studies. The strength of evidence is limited by the low number of studies and by their low methodological quality (high risk of bias). It is unlikely that there will be any future controlled trials to investigate this issue but the current evidence, although weak, suggests a benefit for influenza vaccination amongst adults with cancer and the vaccine was not found to be harmful. Influenza vaccines given to adults with cancer contain an inactivated virus that cannot cause influenza or other viral infection. The possibility for benefit shown in this review supports yearly influenza vaccination in adults with cancer receiving chemotherapy.
Summary of findings
Summary of findings for the main comparison.
influenza vaccination for prevention of influenza among adults with cancer
| influenza vaccination for prevention of influenza among adultswith cancer | ||||||
| Patient or population: patients with prevention of influenza among adults with cancer Settings: Intervention: influenza vaccination | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Influenza vaccination | |||||
| All‐cause mortality Follow‐up: 4‐12 months | Study population | OR 0.88 (0.78 to 1) | 1577 (1 study) | ⊕⊝⊝⊝ very low1,2 | Earle 2003 | |
| 397 per 1000 | 367 per 1000 (340 to 397) | |||||
| Moderate | ||||||
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| All‐cause mortality Follow‐up: 5‐7 months | Study population | OR 0.42 (0.24 to 0.75) | 806 (1 study) | ⊕⊝⊝⊝ very low1,3,4 | Vinograd 2013 | |
| 191 per 1000 | 90 per 1000 (54 to 150) | |||||
| Moderate | ||||||
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Observational study, adjusted results reported but confounding cannot be ruled out 2 95% confidence interval up to 1 3 Broad 95% confidence intervals 4 58% reduction in the odds for death in the adjusted analysis
Background
Influenza is an acute respiratory illness caused by infection with influenza viruses. The illness affects the upper, lower or entire respiratory tract and is often accompanied by systemic signs. There are three types of seasonal influenza viruses: A, B and C. Human influenza A and B viruses cause seasonal epidemics of the disease almost every winter. Influenza C causes mild respiratory illness and occurs much less frequently than A and B. Type A influenza viruses are further categorised into subtypes according to different kinds and combinations of virus surface glycoproteins: hemagglutinin (HA) and neuraminidase (NA) (UpToDate 2010).
Symptoms of influenza include fever, myalgia, headache, cough, chills, nasal congestion and sore throat (Kamps 2006). The major complication of influenza is pneumonia, with secondary bacterial pneumonia being the most common form. Primary influenza pneumonia is a rare but severe condition. Other complications include otitis media, bronchiolitis in infants and young children and exacerbations of chronic respiratory disease. There are also non‐respiratory complications, including febrile convulsions, Reye’s syndrome (a rare, acute encephalopathy characterised by fever, vomiting, fatty infiltration of the liver, disorientation, and coma, occurring mainly in children and usually following a viral infection), neurological sequelae and myocarditis (Angelo 2004; Wiselka 1994). The major morbidity associated with influenza is probably worsening of chronic health problems. Complications occur most frequently in certain groups of people with underlying chronic illnesses who are classified as at 'high‐risk' for this infection (Glezen 2008; WHO Influenza 2009). These high‐risk groups include those with illnesses that involve the cardiovascular or pulmonary systems; people with diabetes mellitus, renal disease or immunosuppression; residents of nursing homes or chronic care facilities; healthy individuals over the age of 65, children aged 6 to 23 months; and pregnant women. Pneumonia and influenza‐related death rates range from fewer than ten per 100,000 healthy adults up to more than 600 per 100,000 chronically ill adults (WHO Surveillance 2009). However, these estimated rates have wide variability depending on case definitions, the statistical models used for estimation and the categories considered as cause for death (CDC MMWR 2010). Typically, there are between three and five million cases of severe illness and up to 500,000 deaths yearly world wide related to influenza (WHO Surveillance 2009).
Description of the condition
Influenza among adults with cancer
People with haematological or solid cancers undergoing chemotherapy and bone marrow transplant recipients are at increased risk of influenza‐related complications (CDC Cancer prevention 2010; Kunisaki 2009). People at highest risk include those with impaired cell‐mediated and antibody‐mediated immunity, as reflected by a decrease in the number or function of T and B lymphocytes (Pirofski 1998). Highest‐risk people include those following allogeneic bone marrow transplant (or haematopoietic stem‐cell transplant, hereafter referred to collectively as hematopoietic stem cell transplantation (HSCT) recipients), especially during episodes of graft‐versus‐host disease (GVHD). Low‐risk people with impaired lymphocyte function include adults with chronic lymphocytic leukaemia (CLL), multiple myeloma, and probably those treated with specific anti‐lymphocyte antibodies such as rituximab, alemtuzumab and others (Issa 2009). The main immune deficit affecting other people with cancer is neutropenia, which is associated mainly with higher risk for bacterial infections rather than viral infections. However, influenza‐related complications are more common among these patients compared to the general population. Different studies report a wide range of influenza rates and influenza‐related pneumonia and deaths rates among people with malignancies admitted to hospital with respiratory symptoms (Table 3). Overall, influenza‐related hospitalisation rates are four times higher and mortality ten times higher among people with cancer compared with the general population (Cooksley 2005; Yousuf 1997). Influenza and its complications may also trigger delays or cancellation of chemotherapy treatment, with possible consequences for cancer disease control.
Table 1.
Influenza frequency and related outcomes in HSCT recipients and adults with cancer
| Ref. | Type of malignancy (influenza years) | No of cases | Influenza cases | Outcome |
| Ljungman 2001 | allogeneic BMT/HSCT recipients (1997 to 1998) | 819 | 1.7% | Deaths 29% |
| autologous BMT/HSCT recipients (1997 to 1998) | 1154 | 0.2% | Deaths 0% | |
| allogeneic BMT/HSCT recipients (1997 to 2000) | >819 | Deaths 23% | ||
| autologous BMT/HSCT recipients (1997 to 2000) | >1154 | Deaths 22% | ||
| Hassan 2003 | allogeneic BMT/HSCT recipients (1996 to 2001) | 230 | 2.2% | Deaths 20% |
| autologous BMT/HSCT recipients (1996 to 2001) | 396 | 0% | ||
| Nichols 2004 | HSCT recipients (within 120 days after transplantation) (1989 to 2002) | 4797 | 1.3% | Deaths 10% Pneumonia 29% |
| Machado 2003 | HSCT recipients (URTI symptoms present) (2001 to 2002) | 179 | 23% | Deaths 0% |
| Chemaly 2006 | HSCT recipients AND hematologic malignancies (retrospective study of patients with laboratory confirmed viral respiratory infection) (2000 to 2002) | 343 | 33% | Deaths 4% Pneumonia 30% |
| HSCT recipients | 230 | 29% | ||
| Leukaemia | 61 | 33% | ||
| Lymphoma | 37 | 51% | ||
| Multiple myeloma | 15 | 40% | ||
| Yousuf 1997 | CLL /acute leukaemia (hospitalized patients) (1993 to 1994) | 45 | 33% | Deaths 27% Pneumonia 80% |
| Elting 1995 | CLL /acute leukaemia (1991 to 1992) | 37 | 11% | Deaths 25% Pneumonia 75% |
| Redelman‐Sidi 2010 | solid cancers (H1N1 2009 pandemic) | 226 | 7% | 0% Deaths |
| hematologic malignancies (H1N1 2009 pandemic) | 167 (96 HSCT) | 17% (22%) | 0% Deaths |
Due to paucity of data, it is difficult to estimate the differences in influenza and influenza‐related complications rates for specific risk‐groups among all people with cancer. Although data are limited, allogeneic HSCT recipients seem to be more susceptible to influenza than autologous HSCT recipients. Solid tumours were only included in one study (Earle 2003), so results cannot be generalised to all people with cancer. In one study, absolute lymphocyte count of less than 200 cells/mL (indicating severe immune dysfunction) was an independent predictor of progression to influenza‐related pneumonia (Chemaly 2006).
Description of the intervention
Influenza vaccines contain antigens of the circulating influenza viruses and are intended to trigger antibody‐mediated protection. Influenza A viruses undergo continual changes in the hemagglutinin (HA) and neuraminidase (NA) proteins, which necessitate annual updating of the influenza vaccine components (Glezen 2008). Current influenza vaccines are available as trivalent inactivated vaccine (TIV, three strains; usually A/H1N1, A/H3N2, and B) or as a nasal spray of live attenuated influenza vaccine (LAIV) (CDC Flu activity 2010). There are three types of TIV: (1) whole virion vaccines which consist of complete viruses which have been inactivated, so that they are not infectious but retain their strain‐specific antigenic properties; (2) subunit virion vaccines which are made of surface antigens (HA and NA) only; (3) split virion vaccines in which the viral structure is broken up by a disrupting agent. These vaccines contain both surface and internal antigens. The subunit or split vaccines are those used routinely for seasonal vaccination in adults. Currently, both TIV and the nasal spray are manufactured using chicken eggs. TIV is indicated for all individuals aged six months and older. LAIV has been approved by the United States Food and Drug Administration (FDA) for healthy persons aged 2 to 49 years and is contra‐indicated in immunosuppressed individuals (Fiore 2009). The protective efficacy of the vaccine is largely determined by the relationship (closeness of 'fit' or 'match') between the strains in the vaccine and the viruses that circulate in the season. Vaccine effectiveness may also be lower among persons with chronic medical conditions (see immune suppression below) and among the elderly, compared with healthy young adults and children (CDC Seasonal Influenza 2009).
How the intervention might work
Inactivated influenza vaccines probably have a protective effect among people with cancer, despite immunosuppression. On one hand, immunosuppression might attenuate the response to influenza vaccine (Kunisaki 2009). People with cancer with cell‐mediated immune dysfunction are likely to have lower responses to influenza vaccination. Some degree of lymphopenia and cellular dysfunction also accompany the neutropenia that follows chemotherapy, and thus most people with cancer will have a poor response to the vaccine. On the other hand, people with cancer have more to gain from any degree of protection because influenza is more severe among immunosuppressed patients. Inactivated vaccine cannot cause influenza, because the inactivated virus is non‐pathogenic, thus there is no danger in administering it even to the most immune compromised patients.
Why it is important to do this review
Given an increased risk for complications combined with the expected lower immunogenicity of the vaccine among people with cancer, data on vaccine effectiveness is needed for this population. Furthermore, as people with cancer are heterogeneous with respect to chemotherapy regimens and underlying malignant disease, data are needed for specific subgroups. No systematic review has so far conducted a meta‐analysis of the evidence for influenza vaccine in adults with cancer, although previous narrative reviews have summarised the evidence (Alistair 2002; Arrowood 2002; Kunisaki 2009; Melcher 2005). Two reviews recommend vaccination every year, timed to occur either more than two weeks before receiving chemotherapy or between chemotherapy cycles (Arrowood 2002; Melcher 2005). The other two state that it is reasonable to offer vaccination to immunosuppressed patients (under chemotherapy treatment in one review, and with HIV, solid organ transplants, on haemodialysis and haemopoietic stem cell transplants in the other), but further studies are warranted to inform vaccination recommendations (Alistair 2002; Kunisaki 2009). An accurate assessment of the existing evidence on influenza vaccine effects (death, serological response, clinical outcome and adverse effects) in adults with cancer is essential to support comprehensive, rational decisions concerning influenza vaccination.
Objectives
To assess the effectiveness of influenza vaccine in immunosuppressed adults with malignancies. The primary review outcome was all‐cause mortality, preferably at the end of the influenza season.
Methods
Criteria for considering studies for this review
Types of studies
We include randomized controlled trials (RCTs), cohort studies and case‐control studies. We also consider observational studies to fully examine the empirical data on vaccine trials and their use in adults with cancer.
Types of participants
Adults (16 years and over) with cancer, including:
Solid malignancies treated with chemotherapy;
Haematological cancers treated or not treated with chemotherapy (since people might be immunosuppressed even without chemotherapy);
adults with cancer, post‐autologous (up to six months after transplantation) or allogeneic (at any time) haematopoietic stem cell transplantation.
Types of interventions
We considered for inclusion studies comparing inactivated influenza vaccines versus placebo, versus no vaccination or versus a different vaccine. We included inactivated influenza vaccine of any type, any dose and any schedule:
Trivalent or other
Whole, subunit or split virion vaccine
Vaccines could be matched or unmatched to circulating strains, and vaccine fit was recorded if reported. Comparisons of the same or different vaccines given during different influenza seasons or to different cancer populations were excluded. We did not include studies comparing vaccine effects in adults with cancer versus healthy adults.
Types of outcome measures
Clinical outcomes were collected for a maximum follow‐up period until the end of the influenza season following vaccination. We documented the duration of follow‐up in each study. We assessed immunological response up to three months after vaccination, as defined in each study. We assessed adverse events up to two weeks after vaccination. We included studies reporting on at least one of the review‐defined outcomes (primary or secondary).
Primary outcomes
All‐cause mortality, preferably at the end of the influenza season. We selected all‐cause mortality as the primary outcome, since this is the ultimate goal of influenza vaccination, and the composite outcome of infections, hospitalisations, chemotherapy delays and other effects of influenza.
Secondary outcomes
Influenza‐like illness (ILI): A clinical definition of febrile respiratory illness. We accepted the definitions of ILI used in the study.
Confirmed influenza using the methods defined in the study.
Pneumonia from any cause.
Any hospitalisation and number of hospital days.
Chemotherapy interruptions.
Influenza‐related mortality.
Immunological: seroconversion or rise in titre as defined in the study.
Adverse events (AEs): local events on injection site (tenderness/soreness, erythema, arm stiffness), systemic events (myalgia, fever, headache, fatigue, rash).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL, Aug 2013; Appendix 1), MEDLINE (1948 to Aug week 3 2013; Appendix 2), EMBASE (1980 to 2013; Appendix 3), LILACS (to Aug 2013) databases. We also searched PubMed (1948 to Aug week 3 2013), combining search terms in PubMed with a highly sensitive search filter for identifying RCTs as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Cochrane Handbook) and with the SIGN search strategy for identifying observational studies (SIGN 2010; Appendix 4).
We contacted the first or corresponding author of each included study for additional information, and researchers active in the field for information on unpublished studies. There were no language or publication type restrictions.
The latest search was executed by the author team.
Searching other resources
We searched the following conference proceedings: Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC), European Society of Clinical Microbiology and Infectious Diseases (ECCMID), Infectious Disease Conferences (IDSA), American Society of Hematology (ASH), American Society for Blood and Marrow Transplantation (ASBMT), European Group for Blood and Marrow Transplantation (EBMT), and American Society of Clinical Oncology (ASCO) between the years 2006 and 2010. We also scanned the references of all identified studies and pertinent reviews. We searched the websites of the manufacturers of influenza vaccines (Aug 2013). Finally, we searched for ongoing or unpublished studies in clinical trials registry databases using the http://www.controlled‐trials.com/mrct/ website (Aug 2013).
Data collection and analysis
Selection of studies
We included all studies fulfilling the eligibility criteria for design, participants and interventions. We did not restrict inclusion by outcomes reported in the abstract, but obtained the full text and attempted to identify at least one of the review‐defined outcomes from the text or from author correspondence. Two review authors independently applied the inclusion criteria to all identified and retrieved articles. We documented reasons for excluding studies from the review (Characteristics of excluded studies).
Data extraction and management
Two review authors independently performed data extraction using a data extraction form. We extracted data on the following study characteristics:
study design;
length of the follow‐up;
dates of study;
location of study;
risk of bias;,
description of vaccines (content, timing of vaccination and antigenic match);
description of viral circulation degree;
description of outcomes;
characteristics of participants: age, sex, type of malignancy, bone marrow transplantation, anti‐cancer treatment, expected baseline immune suppression: primarily cellular immune dysfunction, severe; primarily cellular immune dysfunction, moderate; primarily neutropenia, severe.
Assessment of risk of bias in included studies
Two review authors (NER, ILV) independently assessed the risks of bias in studies fulfilling the review inclusion criteria. We contacted authors for additional information where necessary.
RCTs
Assessment of the methodological quality of the RCTs was according to the guidelines of The Cochrane Collaboration’s tool for assessing risk of bias (Cochrane Handbook; see Appendix 5). We assessed studies according to the following criteria: allocation sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other possible sources of bias.
Cohort studies
For quality assessment of cohort studies we used the Newcastle‐Ottawa Scale adapted for our review (NOS 2010; see Appendix 6). We assessed the following items:
Selection: including representativeness of the exposed cohort, selection of the non‐exposed cohort, and ascertainment of exposure.
Comparability of cohorts.
Outcome: including assessment of outcome (independent blind assessment /record linkage/self report/no description), length of follow‐up for outcomes to occur, adequacy of follow‐up of cohorts.
We recorded whether an adjusted analysis was reported in the studies.
Measures of treatment effect
We calculated unadjusted odds ratios (ORs) with 95% confidence interval (CI) from RCTs and non‐RCTs (cohort and case‐control studies) for dichotomous data and rates (events per person‐years). For non‐RCTs, we extracted adjusted ORs with 95% CI, as available.
Unit of analysis issues
We expected that the studies might report influenza‐like illness (ILI) as episodes that occur more than once per person. In this case, we tried to extract the number of adults experiencing at least one event, however these data were not available and studies reporting on events per person‐time were analysed as rates.
Dealing with missing data
Whenever data were missing, we attempted to contact the authors of the study and request the information.
Assessment of heterogeneity
The I² statistic was calculated for each pooled estimate, in order to assess the impact of statistical heterogeneity. I² may be interpreted as the proportion of total variation among effect estimates that is due to heterogeneity rather than to sampling error, and it is intrinsically independent of the number of studies. An I² less than 30% would suggest there is little concern about statistical heterogeneity (Higgins 2002; Higgins 2003).
Assessment of reporting biases
Given the paucity of studies in each analysis we were not able to formally assess reporting biases.
Data synthesis
Due to the paucity of trials and heterogenous reporting of events per person or per person‐time a meta‐analysis could not be performed. We had planned to stratify the analysis by the following factors, however, due to the paucity of data we could not conduct the stratified analyses:
participant's type of malignancy and expected degree of immune dysfunction;
degree of viral circulation;
vaccine matching with the seasonal circulating strains.
Subgroup analysis and investigation of heterogeneity
We planned to perform subgroup analyses by the expected severity of immune suppression:
primarily cellular immune dysfunction, severe: participants postallogeneic haematopoietic stem cell transplantation (HSCT);
primarily cellular immune dysfunction, moderate: chronic lymphocytic leukemia (CLL) treated with alkylating agents, multiple myeloma (MM) treated with monoclonal antibodies;
primarily neutropenia, severe: participants with severe neutrophil dysfunction: administration of vaccine during neutropenia (e.g. acute leukemias, autologous HSCT, sarcoma).
Due to the paucity of data we could not perform subgroup analyses. As data accumulate in future updates we will reconsider these analyses.
Sensitivity analysis
We had planned sensitivity analyses based on studies' risk of bias for the primary outcome, but restricting the analysis to RCTs with adequate allocation generation and concealment methods, and to cohort studies at low risk of bias according to the Newcastle‐Ottawa Scale adapted for our review (NOS 2010). As previously, data did not permit such analyses.
Results
Description of studies
Results of the search
We retrieved 4439 records from the electronic database searches. The CENTRAL search identified 155 records, MEDLINE identified 2798 records and EMBASE identified 1486 records. We identified 307 records in conference proceedings. We inspected all records. We did not evaluate studies in which the abstract suggested a patient population or vaccine incompatible with our inclusion criteria. We also excluded studies in which all participants were vaccinated, studies comparing vaccinated adults with cancer with the healthy population or studies comparing different doses of influenza vaccine. We retrieved 45 publications for full‐text inspection, of which 41 were excluded, mainly because all participants were vaccinated, or the comparison was with the healthy population, or different doses of influenza vaccine were compared). See Figure 1 for a flow diagram of studies identified.
Figure 1.

Study flow diagram.
Included studies
Four studies comparing adults with cancer receiving influenza vaccination versus a group that did not receive the vaccine fulfilled the inclusion criteria: one case control (Machado 2005), two cohort studies (Earle 2003, Vinograd 2013) and one randomized controlled trial (RCT) (Musto 1997). The studies were conducted between 1993 and 2012, and encompassed 2124 participants, with haematological diseases, including multiple myeloma patients and patients following bone marrow transplantation, and solid malignancies. The influenza TIV vaccine was used in all studies, in a single dose. There was a good fit with seasonal strains in the three studies providing this information. In the study that did not provide information, the fit of the vaccine with seasonal strains was good up to 1996, but in the 1997 to 1998 season there was a mismatch between the H3N2 influenza vaccine component (Wuhan vaccine) and the major epidemic H3N2 strain (Sydney field) (De Jong 2000). There was no information regarding when the vaccine was given in relation to participants' chemotherapy treatment cycle. Study details can be found in the Characteristics of included studies.
Excluded studies
Reasons for exclusion are detailed in the Characteristics of excluded studies table. The main reasons were that all participants were vaccinated (23 studies), comparison was made with a healthy population (15 studies) or the comparison was between different doses of influenza vaccine (4 studies). One RCT investigated the influenza vaccination on immune responses in adults with cancer undergoing surgery (Spies 2008). However, no outcomes were reported for the control group except for mortality, reported only at two‐year follow‐up.
Risk of bias in included studies
In the RCT (Musto 1997), the method of randomization was not stated, allocation concealment was unclear, and there was no blinding. Attempts to obtain additional information from the author concerning methodological quality were unsuccessful.
The three cohort/case control studies scored between 5 to 10 (out of a maximum of 13 points) on the Newcastle‐Ottawa Scale adapted for our review. (Appendix 6; Table 4). Two of the studies focusing on a specific cancer population were regarded as not representative of the average cancer population. Only Vinograd 2013 controlled for cancer stage and functional status, although only in the mortality outcome assessment.
Table 2.
Newcastle‐Ottawa Grading
| Selection | Comparability | Outcome | total stars score | ||||||
| Representativeness of the exposed cohort | Selection of the non exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability * | Assessment of outcome | Was follow‐up long enough for outcomes to occur | Adequacy of follow up of cohorts ** | ||
| Earle 2003 | c | a | a | a | No | d *** | a | a | 5 |
| Machado 2005 | c | a | a | a | No | b | a | a | 6 |
| Vinograd 2013 | b | a | a+b | a | a+b | b+c | a | a | 10 |
* The most important factor to control for was the cancer stage. The second most important factor was functional capacity
** A follow‐up rate of >=80% was considered adequate
*** Procedure was described but considered inadequate (through billing accounts and other administrative databases)
Earle 2003 reported results in person‐years and results per person were not available. Two cohort studies reported an adjusted analysis for mortality, using multivariable analysis (Earle 2003; Vinograd 2013); all other outcomes were non‐adjusted.
Allocation
See above text.
Blinding
None of the studies was blinded. In the only RCT (Musto 1997) the study was open label, patients allocated to vaccine versus none and no placebo used.
Incomplete outcome data
In Musto 1997 there was no mention of an intention‐to‐treat analysis, and the number of dropouts per study arm was not reported. Therefore, analysis by evaluated patients only in the sensitivity analysis was possible, making it susceptible to attrition bias.
In one cohort study (Earle 2003), follow‐up until death was completed in 86% of participants, making it susceptible to attrition bias. Mortality data were given only for 697 of 1054 patients.
Selective reporting
We had no specific concerns over selective reporting.
Other potential sources of bias
The sponsor of the RCT (Musto 1997) and one of the cohorts (Machado 2005) was not mentioned. The National Cancer Institute sponsored Earle 2003 and Vinograd 2013 was supported an internal hospital grant.
There was no mention of sample size calculations, except for one study (Vinograd 2013).
Effects of interventions
See: Table 1
Two studies reported on all‐cause mortality. Two reported on influenza‐like illnesses (ILIs), three reported confirmed influenza, three reported on pneumonia, two reported any hospitalization and none reported on serological results.
Primary outcome
All cause mortality
Two cohort studies addressed our primary outcome of all‐cause mortality, both reporting on adjusted results (Analysis 1.1). The results could not be combined since one study reported results per person‐years (Earle 2003) and the other per person (Vinograd 2013). Influenza vaccination in Earle 2003 was associated with an adjusted hazard ratio (HR) for death of 0.88 (95% CI 0.77 to 0.99). In Vinograd 2013, influenza vaccination was associated with an adjusted OR for death of 0.43 (95% CI 0.26 to 0.71). A propensity‐matched analysis was also reported in this study and the association with mortality remained significant (adjusted OR 0.41, 95% CI 0.23 to 0.75).
Analysis 1.1.
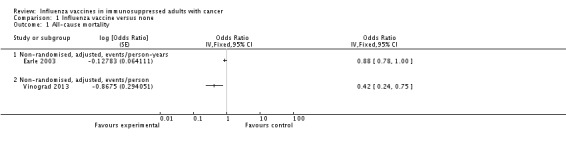
Comparison 1 Influenza vaccine versus none, Outcome 1 All‐cause mortality.
Secondary outcomes
Influenza‐like illness
Two studies (856 participants) reported on clinically‐defined ILI; one RCT (Musto 1997) and one cohort study (Vinograd 2013). The RCT showed a significant reduction in ILI with vaccination and the cohort study showed no association between influenza vaccination and ILI (Analysis 1.2).
Analysis 1.2.
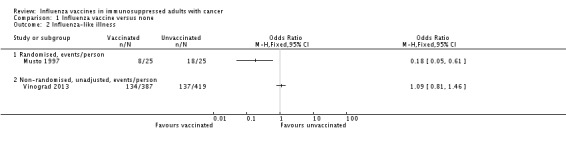
Comparison 1 Influenza vaccine versus none, Outcome 2 Influenza‐like illness.
Confirmed influenza
The three non‐randomized studies (NRS) (2074 participants) reported on confirmed influenza (Analysis 1.3) but none could be combined: Vinograd 2013 reported results per person; Machado 2005 reported results per person with ILI; and Earle 2003 reported events/ person‐year. The event rate was very low and lower with vaccination in all three studies, reaching statistical significance in one study.
Analysis 1.3.
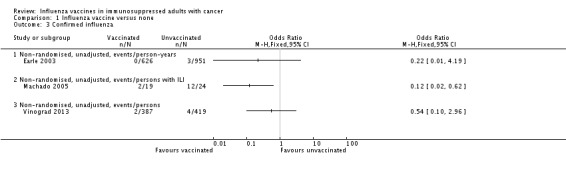
Comparison 1 Influenza vaccine versus none, Outcome 3 Confirmed influenza.
Pneumonia
Three studies (2081 participants) reported on pneumonia, which could not be combined: one RCT (Musto 1997) and two cohort studies (Earle 2003, Vinograd 2013). Two of the studies separately showed a reduction in pneumonia rates in vaccinated patients, one significant and one non‐significant (Analysis 1.4).
Analysis 1.4.
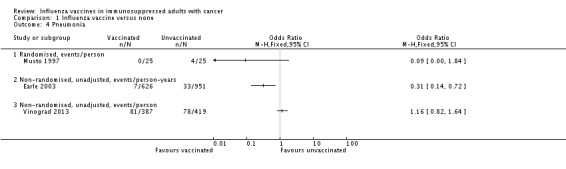
Comparison 1 Influenza vaccine versus none, Outcome 4 Pneumonia.
Any hospitalization
Two studies reported on hospitalizations, the RCT (Musto 1997) and one cohort study (Vinograd 2013). The RCT showed a significantly lower rate of hospitalisations in vaccinated participants, while in the cohort study there was no difference (Analysis 1.5). Two cohort studies reported on hospitalization duration (Earle 2003, Vinograd 2013), both showing no significant associations, but a mean duration shorter by 0.9 to 1.8 days with vaccination.
Analysis 1.5.
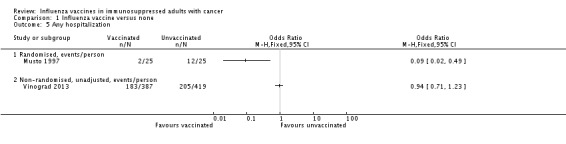
Comparison 1 Influenza vaccine versus none, Outcome 5 Any hospitalization.
Influenza‐related mortality
Two studies (1275 participants) reported on influenza‐related deaths, of which one (Musto 1997) reported only deaths due to influenza pneumonia. Both studies showed a statistically non‐significant decrease in influenza‐related deaths with vaccination, but could not be pooled.
Given the paucity of the studies, the results of each study are described separately. The main outcomes are summarized also in Table 5.
Table 3.
Summary of Main Outcomes
| Outcome | Design | all‐cause mortality | influenza‐like‐ illness | influenza‐ related mortality | confirmed influenza | pneumonia | any hospitalization | chemotherapy interruptions | ||||||
| Vaccination status | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | ||
| Earle 2003 | Retrospective observational | Cox adjusted HR 0.88 (95% CI 0.77 to 0.99), 626 versus 951 py * | 0/626 py | 2/951 py | 0/626 py | 3/951 py | 7/626 py * | 33/951 py * | mean days 15.6, 95% CI 13.3 to 17.8 (N = 626 py) | mean days 16.4, 95% CI 14.3 to 18.4 (N = 951 py) | mean 5.06 days (N = 626 py) ** | mean 6.04 days (N = 951 py) ** | ||
| Machado 2005 | Retrospective case control | 2/19 * | 12/24 * | |||||||||||
| Musto 1997 | Randomized, open label | 8/25 * | 18/25 * | 0/25 | 2/25 | 0/25 | 4/25 | 2/25 * | 12/25 * | |||||
| Vinograd 2013 | Prospective observational | MV adjusted OR 0.43 (95% CI 0.26 to 0.71) (387 versus 419p); MV adjusted OR in propensity‐matched cohort 0.42 (95% CI 0.76 to 0.24) (218p versus 218p) | 134/387 | 137/419 | 2/387 | 4/419 | 81/387 | 78/419 | 183/387 | 205/419 | 97/387 | 116/419 | ||
py= persons years
* denoted statistically significant difference, P < 0.05
** mean interval between chemotherapy bills
A presumably open label (no placebo used) RCT, recruiting 50 adults with multiple myeloma, of which 25 were randomized to receive the vaccine. The follow‐up period was four months. ILI occurred in 8 out of 25 (32%) vaccine recipients and in 18 out of 25 (72%) controls (P < 0.001). The mean duration of febrile illness was significantly higher in controls (12 versus 5 days, P < 0.001). Pneumonia was observed in 4 (16%) control and in none of the vaccinated participants (OR 0.09, 95% CI 0.005 to 1.84), and was lethal in two cases. This was the only data on mortality. Twelve unvaccinated participants (48%) required hospitalisation versus two vaccinated (8%, P < 0.001). Sixty per cent of vaccinated participants complained of mild local symptoms at the site of the injection.
A retrospective case‐control study (cases with confirmed influenza versus controls without influenza). A total of 177 bone marrow transplantation (BMT) recipients were followed, mostly (71%) following allogeneic BMT. One hundred and thirty‐four were within the first six months after transplantation and were, therefore, not eligible for influenza vaccination. Of this group, 25 (18.6%) acquired influenza, and are not included in our meta‐analysis. Of the remaining 43 participants eligible to receive influenza vaccination, 19 were vaccinated and 24 were not. Two (10%) of the vaccinated participants had confirmed influenza compared with 12 (50%) unvaccinated (P = 0.015). No other outcomes were reported in the study.
A retrospective observational cohort study including adults with advanced colorectal cancer undergoing treatment. A total of 1225 participants (1577 person‐years) were observed. Of these person‐years, 626 (39.7%) were vaccinated and 951 (60.3%) were not. Follow‐up until death was completed in 86% of participants. The one‐year survival rate was 60.2% (376 person‐years) in the vaccinated group and 55.3% (525 person‐years) in those not vaccinated. On multivariate analysis, influenza vaccination treated as a time‐dependent variable was associated with a hazard ratio (HR) for death of 0.88 (95% CI 0.77 to 0.99). The number of participants with confirmed influenza was 0/626 person years vaccinated versus 3/951 person years unvaccinated (difference not statistically significant). Vaccinated adults had less pneumonia (7/626 versus 33/951 person years) The mean days of hospitalisation was 15.6, 95% CI 13.3 to 17.8 in the vaccinated group versus 16.4, 95% CI 14.3 to 18.4 among unvaccinated adults, difference non‐significant. No deaths due to influenza were observed in the vaccinated group versus two (0.2%) in the unvaccinated. The interval between chemotherapy bills was significantly longer for patients who were not vaccinated (unvaccinated versus vaccinated, 6.04 versus 5.06 days).
A prospective observational cohort study, including adults with cancer with solid malignancies undergoing chemotherapy and haematological patients with active disease. A total of 806 patients were observed during a single season (2010 to 11). Of these, 387 (48%) were vaccinated and 419 (52%) were unvaccinated. The only outcome significantly associated with vaccination was all cause mortality, occuring in 46/387 (11.9%) of vaccinated versus 80/419 (19.1%) of unvaccinated patients (P = 0.005). On multivariate analysis, influenza vaccination was associated with an OR for death of 0.43 (95% CI 0.26 to 0.71). The association with mortality remained significant in a vaccination propensity‐matched analysis (OR 0.41, 95% CI 0.23 to 0.75). ILI was diagnosed in 134/387 (34.6%) of vaccinated versus 137/419 (32.7%) in unvaccinated. Confirmed influenza was reported only in 2/387 versuss 4/419 patients, respectively. Pneumonia was reported in 81/387 (20.9%) of vaccinated patients versus 78/419 (18.6%) of unvaccinated. Of the vaccinated patients 183/387 (47.3%) were hospitalized during follow up compared to 205/419 (48.9%) of the unvaccinated. The Number of hospitalization days (mean ± SD) in vaccinated patients was 5.55 ± 11.50 versus 7.39 ± 14.00 in unvaccinated. Chemotherapy interruptions were reported in 97/387 (25.1%) of vaccinated versus116/419 (27.7%) of unvaccinated. All differences were not statistically significant. Of the 561 patients that were interviewed for adverse events, 267 were vaccinated. Fifty nine patients (24.6%) reported local and other mild AE. Nine patients (3.3%) reported fever related to vaccination.
Discussion
In this review of influenza vaccines for adults with cancer, we identified only one open‐label randomized trial and three observational studies comparing vaccination versus no vaccination, encompassing 2,124 patients. The studied population, the outcomes examined and reporting methods were highly heterogenous, precluding a meta‐analysis for all outcomes.
Summary of main results
Two cohort studies assessed all‐cause mortality, the primary review outcome, showing that influenza vaccination was associated with significantly lower mortality in an analysis adjusted for other risk factors for death. For all other outcomes, either no differences were observed or fewer infections occurred among vaccination patients (Summary of findings table 1). Confirmed influenza occurred less frequently among vaccinated patients in the three observational studies, reaching statistical significance in one.
Overall completeness and applicability of evidence
Despite a thorough search of the literature we found only a few studies that compared vaccinated and unvaccinated adults with cancer and no placebo‐controlled RCTs. Only one study included patients with haematological malignancies and no study reported separately on patients following allogeneic HSCT. The immune response and vaccine effect after allogeneic BMT is different from other cancer populations, because of impaired cell‐mediated and antibody‐mediated immunity. Due to the paucity of data we could not compare between populations and it is questionable whether the results of these studies can be generalised to adults with all malignancies. Data on adverse effects of vaccination and mortality were incomplete. There is no study comparing different dosing regimens (e.g. one versus two vaccine doses).
Quality of the evidence
Observational studies assessing the effects of influenza vaccination have the inherent limitations of selection bias. An adjusted analysis was presented in two studies only and only for the outcome of mortality.
The only RCT included in the current review had unclear methods of randomization and was open‐label. Hence the quality of the evidence is low.
Potential biases in the review process
Inclusion of studies with different methodology and missing data might have introduced bias.
Assessment of the effects of influenza vaccine on mortality is difficult in our review. One can argue that all‐cause mortality is not an appropriate outcome in non‐RCTs because most deaths are related to the primary cancer rather than to influenza. But since ultimately prevention of mortality is the ultimate goal and reason for vaccination and is the composite outcome of infections, hospitalisations, chemotherapy delays and other effects of influenza, we decided to select mortality as the primary outcome. In the first version of our protocol, we defined a composite primary outcome of ILI, pneumonia of any cause or influenza‐related death. We realized that obtaining a composite outcome in an aggregate meta‐analysis without having access to individual patient data is impossible. Furthermore, influenza‐related deaths are difficult to assess because the cause of death is difficult to establish in adults with cancer.
In order to avoid publication bias we searched the website of the manufacturers of influenza vaccine and tried to obtain information on ongoing studies by correspondence with the authors and in clinical trial registry databases. However, no further studies were identified.
Agreements and disagreements with other studies or reviews
This is the first systematic review trying to compile the clinical evidence on influenza vaccine effects among adults with cancer. Previous narrative reviews summarised the evidence, reaching similar conclusions (Alistair 2002; Arrowood 2002; Kunisaki 2009; Melcher 2005). A Cochrane review assessed the effectiveness of influenza vaccine among children with cancer (Goossen 2013). In addition to the interventions and comparisons included in our review, this review included also studies comparing the serological response of children with cancer with that of control groups, including children without cancer. One RCT and eight observational studies were included. In five observational studies, the immune response to TIV and BIV in children receiving chemotherapy was weaker than in children off chemotherapy, but not for all influenza virus strains tested. A four‐fold rise in antibody titre was observed in 38% to 65% of children receiving chemotherapy compared with 71% to 89% of healthy children (three observational studies). One observational study reported a lower vaccine response in children with acute lymphoid leukaemia on chemotherapy than in children with asthma. None of the studies evaluated clinical influenza or laboratory‐confirmed influenza as outcomes. The authors concluded that children with cancer receiving chemotherapy are able to generate an immune response to influenza vaccine, however, immune response is weaker in children receiving chemotherapy (a four‐fold rise of 25% to 52%) than in those children who were off chemotherapy for at least one month (50% to 86%) and in healthy children (71% to 89%). A meta‐analysis of four studies (two controlled cohorts, one case‐control and one RCT) assessed the effectiveness of influenza vaccine in HIV‐positive adults (Anema 2008). Meta‐analysis of the three prospective studies resulted in a 66% reduction in the risk for symptomatic influenza, while the one RCT yielded a 41% reduction.
Multiple guidelines recommend influenza vaccination for adults infected with HIV, who have received solid‐organ transplants, who have received haemopoietic stem‐cell transplants, and adults on haemodialysis. The Centers for Disease Control (CDC) guidelines recommend annual vaccination to persons who are immunosuppressed (including immunosuppression caused by medications or by human immunodeficiency virus), to adults with cancer or a history of cancer, and to adults who live with or care for those with cancer and survivors (CDC Cancer prevention 2011‐2012). The evidence we showed, though weak, supports influenza vaccination for adults with cancer.
Authors' conclusions
The existing evidence on the effectiveness of influenza vaccine in immune‐suppressed adults with malignancies is mostly observational, incomplete and of low quality. It was previously shown that Influenza‐related complications are more common among these adults compared to the general population, including hospitalisation and death. Although the data available are sparse and of low quality, there is no harm in the vaccine and possible benefit with regard to survival, confirmed influenza, influenza‐like illness, pneumonia and hospitalizations. Data on all‐cause mortality were presented only in two cohort studies, but were significantly lower in vaccinated participants. The strength of evidence is limited by the low number of studies (four) and by the fact that only one was a randomized controlled trial (RCT). Influenza vaccination is safe in this population. The evidence (though weak) is in favour of vaccinating this population. The summary of the available evidence should be used to encourage carers and adults with cancer to accept yearly influenza vaccination.
Performing a placebo or no‐treatment controlled randomized controlled trial of influenza vaccination among adults with cancer is ethically questionable. We believe that the vaccine carries some degree of benefit and have no reason to believe that the vaccine is harmful or that adverse events will be different than those observed in the general population. In place of RCTs, we suggest well‐conducted observational studies. Such studies should encompass people of a defined age group, and a variety of malignancies treated with different modalities (chemotherapy, immunotherapy, targeted therapy, and especially hematological malignancies, autologous or allogeneic stem cell transplant). These kind of studies should also include many influenza seasons (many years of follow up) and would allow a better propensity score to be done.Studies should have a minimal risk of bias, the outcomes employed should be clinically important and include all‐cause mortality, confirmed influenza, influenza‐like illness, pneumonia and influenza‐related death. Exact data on immunological response to vaccination, how influenza is confirmed, hospitalisations and hospital days, chemotherapy interruptions, adverse effects of vaccination, should be collected. A retrospective comparison of influenza vaccine effectiveness in years with a good match versus years with a poor match of vaccine and circulating influenza strains could also be useful.
Acknowledgements
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Gynaecological Cancer Group. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor Influenza, Human, this term only #2 MeSH descriptor Influenza A virus explode all trees #3 MeSH descriptor Influenza B virus explode all trees #4 MeSH descriptor Influenzavirus C, this term only #5 inluenza* or grippe or flu or orthomyxovir* or myxovirus* #6 (#1 OR #2 OR #3 OR #4 OR #5) #7 MeSH descriptor Influenza Vaccines, this term only #8 vaccin* #9 flumist or CAIV‐T or trivalent or LAIV or fluzone or fluarix or fluinsure or fluviral or invivac or influvac or flublok or fluvirin or vaxigrip or mutagrip or flushield or fluogen #10 (#7 OR #8 OR #9) #11 MeSH descriptor Neoplasms explode all trees #12 MeSH descriptor Bone Marrow Transplantation, this term only #13 MeSH descriptor Stem Cell Transplantation explode all trees #14 cancer* or neoplas* or tumor* or tumour* or malignan* or carcinoma* or metasta* or oncolog* or leukemi* or leukaemi* or lymphoma* or myeloma* or sarcoma* #15 MeSH descriptor Antineoplastic Agents explode all trees #16 chemotherap* or transplant* or HSCT or BMT #17 MeSH descriptor Neutropenia, this term only #18 neutropenia #19 lymphocyte* near/5 (function* or count* or number*) #20 MeSH descriptor Immune Tolerance explode all trees #21 (immuno‐suppress* or immunosuppress*) #22 (immunity or immune) near/5 (suppress* or impair* or dysfunction*) #23 immuno‐compromise* or immunocompromise* #24 (#11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23) #25 (#6 AND #10 AND #24)
Appendix 2. MEDLINE search strategy
1 Influenza, Human/ 2 exp influenzavirus a/ 3 exp Influenzavirus B/ 4 Influenzavirus C/ 5 (influenza* or grippe or flu or orthomyxovir* or myxovirus*).mp. 6 1 or 2 or 3 or 4 or 5 7 Influenza Vaccines/ 8 vaccin*.mp. 9 (flumist or CAIV‐T or trivalent or LAIV or fluzone or fluarix or fluinsure or fluviral or invivac or influvac or flublok or fluvirin or vaxigrip or mutagrip or flushield or fluogen).mp. 10 7 or 8 or 9 11 exp Neoplasms/ 12 Bone Marrow Transplantation/ 13 exp Stem Cell Transplantation/ 14 (cancer* or neoplas* or tumor* or tumour* or malignan* or carcinoma* or metasta* or oncolog* or leukemi* or leukaemi* or lymphoma* or myeloma* or sarcoma*).mp. 15 exp Antineoplastic Agents/ 16 (chemotherap* or transplant* or HSCT or BMT).mp. 17 Neutropenia/ or neutropenia.mp. 18 (lymphocyte* adj5 (function* or count* or number*)).mp. 19 exp Immune Tolerance/ 20 (immuno‐suppress* or immunosuppress*).mp. 21 ((immunity or immune) adj5 (suppress* or impair* or dysfunction*)).mp. 22 (immuno‐compromise* or immunocompromise*).mp. 23 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 24 6 and 10 and 23 25 randomized controlled trial.pt. 26 controlled clinical trial.pt. 27 randomized.ab. 28 placebo.ab. 29 drug therapy.fs. 30 randomly.ab. 31 trial.ab. 32 Epidemiologic studies/ 33 exp case control studies/ 34 exp cohort studies/ 35 case control.tw. 36 (cohort adj (study or studies)).tw. 37 cohort analy*.tw. 38 (follow up adj (study or studies)).tw. 39 (observational adj (study or studies)).tw. 40 longitudinal.tw. 41 retrospective.tw. 42 cross sectional.tw. 43 cross‐sectional studies/ 44 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 45 24 and 44
key: mp=protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier pt=publication type tw=textword ab=abstract fs=floating subheading
Appendix 3. EMBASE search strategy
1 exp influenza/ 2 (influenza* or grippe or flu or orthomyxovir* or myxovirus*).mp. 3 1 or 2 4 exp influenza vaccine/ 5 vaccin*.mp. 6 (flumist or CAIV‐T or trivalent or LAIV or fluzone or fluarix or fluinsure or fluviral or invivac or influvac or flublok or fluvirin or vaxigrip or mutagrip or flushield or fluogen).mp. 7 4 or 5 or 6 8 exp neoplasm/ 9 exp bone marrow transplantation/ 10 stem cell transplantation/ 11 (cancer* or neoplas* or tumor* or tumour* or malignan* or carcinoma* or metasta* or oncolog* or leukemi* or leukaemi* or lymphoma* or myeloma* or sarcoma*).mp. 12 exp chemotherapy/ 13 exp antineoplastic agent/ 14 (chemotherap* or transplant* or HSCT or BMT).mp. 15 exp neutropenia/ or neutropenia.mp. 16 (lymphocyte* adj5 (function* or count* or number*)).mp. 17 exp Immune Tolerance/ 18 (immuno‐suppress* or immunosuppress*).mp. 19 ((immunity or immune) adj5 (suppress* or impair* or dysfunction*)).mp. 20 (immuno‐compromise* or immunocompromise*).mp. 21 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 22 3 and 7 and 21 23 crossover procedure/ 24 randomized controlled trial/ 25 single blind procedure/ 26 random*.mp. 27 factorial*.mp. 28 (crossover* or cross over* or cross‐over).mp. 29 placebo*.mp. 30 (doubl* adj blind*).mp. 31 (singl* adj blind*).mp. 32 assign*.mp. 33 allocat*.mp. 34 volunteer*.mp. 35 controlled clinical trial/ 36 Clinical study/ 37 case control study/ 38 Family study/ 39 Longitudinal study/ 40 Retrospective study/ 41 Prospective study/ 42 Cohort analysis/ 43 (cohort adj (study or studies)).mp. 44 (case control adj (study or studies)).tw. 45 (follow up adj (study or studies)).tw. 46 (observational adj (study or studies)).tw. 47 (epidemiologic* adj (study or studies)).tw. 48 (cross sectional adj (study or studies)).tw. 49 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 50 22 and 49
key: mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword tw=textword
Appendix 4. SIGN search strategy for observational studies
Adapted for MEDLINE
| 1 | Epidemiologic studies/ |
| 2 | Exp case control studies/ |
| 3 | Exp cohort studies/ |
| 4 | Case control.tw. |
| 5 | (cohort adj (study or studies)).tw. |
| 6 | Cohort analy$.tw. |
| 7 | (Follow up adj (study or studies)).tw. |
| 8 | (observational adj (study or studies)).tw. |
| 9 | Longitudinal.tw. |
| 10 | Retrospective.tw. |
| 11 | Cross sectional.tw. |
| 12 | Cross‐sectional studies/ |
| 13 | Or/1‐12 |
Appendix 5. Assessment of risk of bias in RCTs
Studies will be classified according to the following criteria: Allocation sequence generation: A=adequate (e.g. a random number table; a computer random number generator) B= inadequate (e.g. sequence generated by date) C= unclear or not described
Allocation concealment A= adequate (e.g. numbered drug containers of identical appearance) B= inadequate (e.g. using an open random allocation schedule) C= unclear or not described
Blinding
A= adequate (e.g. outcome measurement are not likely to be influenced by blinding approach) B= inadequate (e.g. outcome measurement are likely to be influenced by blinding approach) C= unclear or not described
Incomplete outcome data addressing (separately for each outcome defined in the study) A= adequate (e.g. no missing outcome data) B= inadequate (e.g. reason for missing outcome data likely to be related to true outcome) C= unclear or not described
Lack of selective outcome reporting (separately for each outcome defined in the study) A= adequate (e.g. published reports include all expected outcomes) B= inadequate (e.g. not all of the study’s pre‐specified primary outcomes have been reported) C= unclear or not described
Absence of other source of bias
A= adequate (e.g. the study appears to be free of other sources of bias) B= inadequate (e.g. the study had a potential source of bias related to the specific study design)
Follow up
Duration of follow up and percent of participants lost to follow up.
Appendix 6. Assessment of risk of bias in cohort studies
Adapted Newcastle‐Ottawa Scale:
We will classify studies as low risk of bias (up to one inadequate item in the NOS), medium risk of bias (up to three inadequate items) and high risk of bias (more than three inadequate or no description of methods. The following items will be assessed:
Selection
1) Representativeness of the exposed cohort (active cancer patients, undergoing chemotherapy, whose immune status is well characterized) a) truly representative of the exposed cohort ✶ b) somewhat representative of the exposed cohort ✶ c) selected group of exposed cancer patients. eg nurses, volunteers d) no description of the derivation of the cohort
2) Selection of the non exposed cohort a) drawn from the same community as the exposed cohort ✶ b) drawn from a different source c) no description of the derivation of the non exposed cohort
3) Ascertainment of exposure a) secure record ✶ b) structured interview ✶ c) written self report d) no description
4) Demonstration that outcome of interest was not present at start of study a) yes ✶ b) no
Comparability
1) Comparability of cohorts on the basis of the the following items a) study controls for cancer stage ✶ b) study controls for functional status ✶
Outcome
1) Assessment of outcome a) independent blind assessment ✶ b) record linkage ✶ c) self report d) no description
2) Was follow‐up long enough for outcomes to occur (the end of influenza season) a) yes (select an adequate follow up period for outcome of interest) ✶ b) no
3) Adequacy of follow up of cohorts a) complete follow up ‐ all subjects accounted for ✶ b) subjects lost to follow up unlikely to introduce bias ‐ small number lost ‐ > 80% (select an adequate %) follow up, or description provided of those lost) ✶ c) follow up rate < 80% (select an adequate %) and no description of those lost d) no statement
Data and analyses
Comparison 1.
Influenza vaccine versus none
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 All‐cause mortality | 2 | Odds Ratio (Fixed, 95% CI) | Totals not selected | |
| 1.1 Non‐randomised, adjusted, events/person‐years | 1 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Non‐randomised, adjusted, events/person | 1 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Influenza‐like illness | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Randomised, events/person | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Non‐randomised, unadjusted, events/person | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Confirmed influenza | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Non‐randomised, unadjusted, events/person‐years | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Non‐randomised, unadjusted, events/persons with ILI | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Non‐randomised, unadjusted, events/persons | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pneumonia | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Randomised, events/person | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Non‐randomised, unadjusted, events/person‐years | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Non‐randomised, unadjusted, events/person | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Any hospitalization | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Randomised, events/person | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Non‐randomised, unadjusted, events/person | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
What's new
Last assessed as up‐to‐date: 20 August 2013.
| Date | Event | Description |
|---|---|---|
| 21 September 2016 | Amended | Contact details updated. |
History
Protocol first published: Issue 2, 2011 Review first published: Issue 10, 2013
| Date | Event | Description |
|---|---|---|
| 1 April 2015 | Amended | Contact details updated. |
| 24 February 2015 | Amended | Contact details updated. |
| 11 February 2015 | Amended | Contact details updated. |
| 27 March 2014 | Amended | Contact details updated. |
| 26 February 2014 | Amended | Contact details updated. |
Differences between protocol and review
The primary protocol‐defined outcome was: 'Influenza‐like illness defined as: ILI definition in study or Pneumonia of any cause or influenza‐related death'. We have changed the primary outcome to 'all‐cause mortality' since ultimately this is the goal of influenza vaccination and the composite outcome of infections, hospitalisations, chemotherapy delays and other effects of influenza. All components of the former primary outcome are included as secondary outcomes.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Earle 2003
| Methods | Retrospective, observational Location and setting:USA, Boston | |
| Participants | Stage 4 colorectal adenocarcinoma, with active chemotherapy treatment 1225 adults, 1577 person‐years: 626 person‐years vaccinated, 951 person‐years unvaccinated mean age 74 year in both groups |
|
| Interventions | Yearly influenza vaccination, examined through medical bills | |
| Outcomes |
|
|
| Notes | Results given per person‐years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐random |
| Allocation concealment (selection bias) | High risk | Non‐random |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients follow‐up |
| Selective reporting (reporting bias) | Unclear risk | none identified |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded |
Machado 2005
| Methods | Retrospective case‐control (confirmed influenza versusno influenza) Location and setting: Brazil | |
| Participants | BMT recipients (CML, acute leukemia, severe aplastic anemia, NHL, MM, other) 43 participants eligible to receive influenza vaccination: 19 vaccinated 24 unvaccinated mean age not reported |
|
| Interventions | Influenza vaccination, obtained from review of participants' charts | |
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐random |
| Allocation concealment (selection bias) | High risk | Non‐random |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Mortality ‐ no record |
| Selective reporting (reporting bias) | High risk | The only outcome reported was documented influenza |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded |
Musto 1997
| Methods | Randomized trial, open‐label Location and setting:Italy |
|
| Participants | Multiple myeloma, with active chemotherapy treatment 50 adults: 25 vaccinated 25 unvaccinated mean age not reported |
|
| Interventions | Influenza vaccination versus no vaccination, assigned by randomization | |
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | |
| Selective reporting (reporting bias) | Unclear risk | Mortality reported only due to influenza pneumonia |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo used |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | None |
Vinograd 2013
| Methods | Prospective observational Location and setting: Israel | |
| Participants | Solid malignancies, with active chemotherapy and haematological patients with active disease 806 adults: 387 vaccinated versus 419 unvaccinated mean age 66 years in vaccinated group versus 60 years in unvaccinated |
|
| Interventions | Patients were followed up through medical personal hard copy files and through electronic patients’ health records, including inpatient and outpatient records. Telephone or personal interviews were also conducted to collect data on clinical outcomes and assure vaccination status. | |
| Outcomes | 1. A composite of hospitalizations for fever or acute respiratory infection; and/or pneumonia necessitating antibiotic treatment; and/or chemotherapy interruptionsr elated to an infectious condition. 2. All cause mortality 3. Influenza‐like illness 4. Laboratory confirmed influenza 5. Individual components of the primary outcome 6. Any hospitalization and hospitalizations days 7. Antibiotic treatment necessity in hospitalization 8. All delays in planned chemotherapy courses |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐random |
| Allocation concealment (selection bias) | High risk | Non‐random |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | |
BMT: bone marrow tranplant;CML: chronic myelogenous leukemia; MM: multiple myeloma; NHL:non‐hodgkin's lymphoma
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adell 2002 | All participants vaccinated |
| Anderson 1999 | All participants vaccinated |
| Avetisyan 2008 | All participants vaccinated |
| Bedognetti 2009 | Lymphoma participants compared to healthy participants |
| Bedognetti 2010 | Lymphoma participants compared to healthy participants |
| Brydak 1999 | All participants vaccinated |
| Brydak 2001 | Healthy participants not vaccinated compared to breast cancer participants vaccinated |
| Brydak 2006 | Lymphoma participants compared to healthy participants |
| Buccalosi 1995 | All participants vaccinated Lymphoma participants compared to healthy participants |
| Centkowski 2007 | All participants vaccinated Lymphoma participants compared to healthy participants |
| Chadha 2009 | All participants vaccinated |
| De Lavallade 2011 | Comparison to healthy participants |
| Engelhard 1993 | All participants vaccinated Comparing different doses of influenza vaccine |
| Feery 1977 | Comparison to healthy participants |
| Ganz 1978 | Comparison to healthy participants |
| Gribabis 1994 | All participants vaccinated |
| Hodges 1979 | Comparison to healthy participants |
| Issa 2011 | All participants vaccinated |
| Jo 2009 | Comparing different doses of influenza vaccine |
| Lachenal 2010 | Vaccination rate in haematological participants |
| Lankes 2009 | Association between influenza vaccination and risk of developing Non‐Hodgkin lymphoma |
| Ljungman 2005 | Comparing different doses of influenza vaccine |
| Lo 1993 | Comparing different doses of influenza vaccine |
| Mazza 2005 | All participants vaccinated Lymphoma participants compared to healthy participants |
| Mulder 2009 | All participants vaccinated Comparison to healthy participants |
| Nordoy 2002 | All participants vaccinated |
| Ortbals 1977 | All participants vaccinated |
| Puthillath 2011 | All participants vaccinated Serological outcomes only |
| Rapezzi 2003 | All participants vaccinated Lymphoma participants compared to healthy participants |
| Robertson 2000 | Myeloma participants vaccinated compared to healthy participants' serum |
| Safdar 2006 | Comparing different influenza vaccines in Non‐Hodgkin lymphoma patients |
| Schafer 1979 | All participants vaccinated Haematological participants compared to healthy participants |
| Shildt 1979 | All participants vaccinated |
| Spies 2008 | No information about control group vaccination prior to study. Mortality is reported in a two‐year follow‐up, while we stated maximal follow‐up period until end of the influenza season following vaccination |
| Spitaleri 2010 | All participants vaccinated |
| Stiver 1978 | All participants vaccinated |
| Takata 2009 | All participants vaccinated |
| Van der Velden 2001 | All participants vaccinated |
| Xu 2009 | All participants vaccinated Comparison to healthy participants |
| Yalc 2010 | All participants vaccinated |
Contributions of authors
Inbal Levi‐Vinograd (ILV) wrote the original protocol. Noa Eliakim Raz (NER) co‐ordinated the review, guided by Mical Paul (MP). NER and ILV were responsible for undertaking searches and organised retrieval of papers. NER and Inbal Levi‐Vinograd (ILV) were responsible for data collection, writing to study authors for additional information. NER, ILV, AZT, LL and MP were responsible for screening search results, screening retrieved papers against inclusion criteria and appraising quality of papers and abstracting data from papers (the latter review author was arbiter in case of disagreement). NER was responsible for entering data into Review Manager 5. All review authors participated in analysis and interpretation of data. NER was responsible for writing the review.
Sources of support
Internal sources
None, Not specified.
External sources
Beilinson Young Researcher Foundation, Israel.
Clalit Foundation, Israel.
Declarations of interest
None
Edited (no change to conclusions)
References
References to studies included in this review
- Earle C C. Influenza vaccination in elderly patients with advanced colorectal cancer. Journal of Clinical Oncology 2003;21(6):1161‐6. [DOI] [PubMed] [Google Scholar]
- Machado CM, Cardoso MRA, Rocha IF, Boas LSV, Dulley FL, Pannuti CS. The benefit of influenza vaccination after bone marrow transplantation. Bone Marrow Transplantation 2005;36:897‐900. [DOI] [PubMed] [Google Scholar]
- Musto P, Carotenuto M. Vaccination against influenza in multiple myeloma. British Journal of Haematology 1997;97(2):504‐10. [PubMed] [Google Scholar]
- Vinograd I, Eliakim‐Raz N, Farbman L, Baslo R, Taha A, Sakhnini A, et al. Clinical effectiveness of seasonal influenza vaccine among adult cancer patients. Cancer 2013;16 SEP:Epub ahead of print. [10.1002/cncr.28351] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Adell C, Bayas JM, Vilella A, Perales M, Vidal J, Bertran MJ, et al. Post‐transplantation vaccination of bone‐marrow transplant recipients [Vacunacion de pacientes receptores de trasplante de progenitores hematopoyeticos]. Medicina Clinica Journal 2002;119(11):405‐9. [DOI] [PubMed] [Google Scholar]
- Anderson H, Petrie K, Berrisford C, Charlett A, Thatcher N, Zambon M. Seroconversion after influenza vaccination in patients with lung cancer. British Journal of Cancer 1999;80:219‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avetisyan G, Aschan J, Hassan M, Ljungman P. Evaluation of immune responses to seasonal influenza vaccination in healthy volunteers and in patients after stem cell transplantation. Transplantation 2008;86(2):257‐63. [DOI] [PubMed] [Google Scholar]
- Bedognetti D, Zoppoli G, Massucco C, Zupo S, Sertoli MR. Impaired humoral response to influenza vaccine and prolonged B memory cell depletion as a consequence of rituximab‐based immunochemotherapy in non‐hodgkin lymphoma patients. Journal of Immunotherapy 2009;32(9):992–3. [Google Scholar]
- Bedognetti D, Zoppoli G, Zanardi E, Massucco C, Sertoli MR. Prolonged lack of humoral response to influenza vaccine associated with a persistent depletion of B memory cells in non‐hodgkin’s lymphoma patients treated with rituximab‐containing immunochemotherapy. Clinical Immunology 2010;135:84. 20096637 [Google Scholar]
- Brydak LB, Calbecka M. Immunogenicity of influenza vaccine in patients with hemato‐oncological disorders. Leukemia and Lymphoma 1999;32(3‐4):369‐74. [DOI] [PubMed] [Google Scholar]
- Brydak LB, Guzy J, Starzyk J, Machala M, Gozdz SS. Humoral immune response after vaccination against influenza in patients with breast cancer. Support Care Cancer 2001;9(1):65‐8. [DOI] [PubMed] [Google Scholar]
- Brydak LB, Machala M, Centkowski P, Warzocha K, Bilinski P. Humoral response to hemagglutinin components of influenza vaccine inpatients with non‐Hodgkin malignant lymphoma. Vaccine 2006;24:6620‐23. [DOI] [PubMed] [Google Scholar]
- Bucalossi A, Marotta G, Galieni P, Bigazzi C, Valenzin PE, Dispensa E. Immunological response to influenza virus vaccine in B‐cell chronic lymphocytic leukaemia patients. Acta Haematologica 1995;93(1):56. [DOI] [PubMed] [Google Scholar]
- Centkowski P, Brydak L, Machala M, Kalinka‐Warzocha E, Blasinska‐Morawiec M, Federowicz I, et al. Immunogenicity of influenza vaccination in patients with non‐Hodgkin lymphoma. Journal of Clinical Immunology 2007;27(3):339‐46. [DOI] [PubMed] [Google Scholar]
- Chadha MK, Fakih MG, Tian L, Mashtare T, Nesline M. Effect of 25 hydroxy vitamin D status on serological response to influenza vaccine in cancer patients. Journal of Clinical Oncology 2009;27:e20575. [Google Scholar]
- Lavallade H, Garland P, Sekine T, Hoschler K, Marin D, Stringaris K, et al. Repeated vaccination is required to optimize seroprotection against H1N1 in the immunocompromised host. Haematologica 2011;96(2):307‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhard D, Nagler A, Hardan I, Morag A, Aker M, Baciu H, et al. Antibody response to a two‐dose regimen of influenza vaccine in allogeneic T cell depleted and autologous BMT recipients. Bone Marrow Transplant 1993;11(1):1‐5. [PubMed] [Google Scholar]
- Feery BJ, Sullivan JR, Hurley TH, Evered MG. Immunization with influenza vaccine in patients with haematological malignant disease. Medical Journal of Australia 1977;1:292‐4. [DOI] [PubMed] [Google Scholar]
- Ganz PA, Shanley JD, Cherry JD. Responses of patients with neoplastic diseases to influenza virus vaccine. Cancer 1978;42:2244–7. [DOI] [PubMed] [Google Scholar]
- Gribabis DA, Panayiotidis P, Boussiotis VA, Hannoun C, Pangalis GA. Influenza virus vaccine in B‐cell chronic lymphocytic leukaemia patients. Acta Haematologica 1994;91(3):115‐8. [DOI] [PubMed] [Google Scholar]
- Hodges GR, Davis JW, Lewis HD Jr, Whittier FC Jr, Siegel CD, Chinn TD, et al. Response to influenza A vaccine among high‐risk patients. Southern Medical Journal 1979;72(1):29–32. [DOI] [PubMed] [Google Scholar]
- Issa NC, Marty FM, Gagne LS, Koo S, Verrill KA, Alvea EP, et al. Seroprotectivetiters against 2009 H1N1 influenza A virus after vaccination in allogeneic hematopoietic stem cell transplantation recipients. Biological Blood MarrowTransplant 2011;17(3):434–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo YM, Song JY, Hwang IS, Lee J, Oh SC, Kim JS, et al. Dose sparing strategy with intradermal influenza vaccination in patients with solid cancer. Journal of Medical Virology 2009;81(4):722‐7. [DOI] [PubMed] [Google Scholar]
- Lachenal F, Sebban C, Duruisseaux M, Biron P, Blay JY, Ghesquières H. Influenza vaccination in patients with haematologic malignancies: analysis of practices in 200 patients in a single center. Bulletin du Cancer 2010;97(4):E33‐6. [DOI] [PubMed] [Google Scholar]
- Lankes HA, Fought AJ, Evens AM, Weisenburger DD, Chiu BC. Vaccination history and risk of non‐Hodgkin lymphoma: a population‐based, case‐control study. Cancer Causes and Control 2009;20(5):517‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljungman P, Nahi H, Linde A. Vaccination of patients with haematological malignancies with one or two doses of influenza vaccine: a randomised study. British Journal of Haematology 2005;130(1):96‐8. [DOI] [PubMed] [Google Scholar]
- Lo W, Whimbey E, Elting L, Couch R, Cabanillas F, Bodey G. Antibody response to a two‐dose influenza vaccine regimen in adult lymphoma patients on chemotherapy. European Journal of Clinical Microbiology & Infectious Diseases 1993;12(10):778‐82. [DOI] [PubMed] [Google Scholar]
- Mazza JJ, Yale SH, Arrowood JR, Reynolds CE, Glurich I, Chyou PH, et al. Efficacy of the influenza vaccine in patients with malignant lymphoma. Clinical Medicine and Research 2005;3(4):214‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulder SF, Jacobs JFM, Olde Nordkamp MAM, Kremer IK, Mulders PFA. Immunological response to influenza vaccine in cancer patients undergoing treatment with sunitinib or sorafenib. European Journal of Cancer 2009;7:116. [Google Scholar]
- Nordoy T, Aaberge IS, Husebekk A, Samdal HH, Steinert S, Melby H, et al. Cancer patients undergoing chemotherapy show adequate serological response to vaccinations against influenza virus and Streptococcus pneumoniae. Medical Oncology 2002;19(2):71‐8. [DOI] [PubMed] [Google Scholar]
- Ortbals DW, Liebhaber H, Presant CA, Amburg AL 3rd, Lee JY. Influenza immunization of adult patients with malignant diseases. Annals of Internal Medicine 1977;87(5):552‐7. [DOI] [PubMed] [Google Scholar]
- Puthillath A, Trump DL, Andrews C, Bir A, Romano K, Wisniewski M, et al. Serological immune responses to influenza vaccine in patients with colorectal cancer. Cancer Chemotherapy and Pharmacology 2011;67(1):111‐5. [DOI] [PubMed] [Google Scholar]
- Rapezzi D, Sticchi L, Racchi O, Mangerini R, Ferraris AM, Gaetani GF. Influenza vaccine in chronic lymphoproliferative disorders and multiple myeloma. European Journal of Haematology 2003;70(4):225‐30. [DOI] [PubMed] [Google Scholar]
- Robertson JD, Nagesh K, Jowitt SN, Dougal M, Anderson H, Mutton K, et al. Immunogenicity of vaccination against influenza, Streptococcus pneumoniae and Haemophilus influenzae type B in patients with multiple myeloma. British Journal of Cancer 2000;82(7):1261‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safdar A, Rodriguez MA, Fayad LE, Rodriguez GH, Pro B, Wang M, et al. Dose‐related safety and immunogenicity of baculovirus‐expressed trivalent influenza vaccine: a double‐blind, controlled trial in adult patients with non‐Hodgkin B cell lymphoma. Journal of Infectious Diseases 2006;194(10):1394‐7. [DOI] [PubMed] [Google Scholar]
- Schafer AI, Churchill WH, Ames P, Weinstein L. The influence of chemotherapy on response of patients with hematologic malignancies to influenza vaccine. Cancer 1979;43(1):25‐30. [DOI] [PubMed] [Google Scholar]
- Shildt RA, Luedke DW, Kasai G, El‐Beheri S, Laham MN. Antibody response to influenza immunization in adult patients with malignant disease. Cancer 1979;44(5):1629‐35. [DOI] [PubMed] [Google Scholar]
- Spies CD, Kip M, Lau A, Sander M, Breuer JP, Meyerhoefer J, et al. Influence of vaccination and surgery on HLA‐DR expression in patients with upper aerodigestive tract cancer. Journal of International Medical Research 2008;36:296‐307. [DOI] [PubMed] [Google Scholar]
- Spitaleri G, Delmonte A, Toffalorio F, Pas TM, Gregorc V. Safety of concomitant administration of seasonal and/or H1N1 flu vaccination in patients receiving erlotinib for advanced non‐small cell lung cancer. Journal of Thoracic Oncology 2010;5(5):752‐4. [DOI] [PubMed] [Google Scholar]
- Stiver HG, Weinerman BH. Impaired serum antibody response to inactivated influenza A and B vaccine in cancer patients. Canadian Medical Association Journal 1978;119(7):733‐8. [PMC free article] [PubMed] [Google Scholar]
- Takata T, Suzumiya J, Ishikawa T, Takamatsu Y, Ikematsu H, Tamura K. Attenuated antibody reaction for the primary antigen but not for the recall antigen of influenza vaccination in patients with non‐Hodgkin B‐cell lymphoma after the administration of rituximab‐CHOP. Journal of Clinical Experimental Hematopathology 2009;49(1):9‐13. [DOI] [PubMed] [Google Scholar]
- Velden AM, Mulder AH, Hartkamp A, Diepersloot RJ, Velzen‐Blad H, Biesma DH. Influenza virus vaccination and booster in B‐cell chronic lymphocytic leukaemia patients. European Journal of Internal Medicine 2001;12(5):420‐4. [DOI] [PubMed] [Google Scholar]
- Xu Y, Methuku N, Coimbatore P, Fitzgerald T, Huang Y, Xiao YY, et al. A prospective study of the immunogenicity of inactivated influenza A (H1N1) 2009 monovalent vaccine in patients who have solid or hematologic malignancies. 48th Annual Meeting of the Infectious Diseases Society of America, 21–24 October 2010; Vancouver, Canada. 2010; Vol. Abstract 5075, posterLB‐5013. [Google Scholar]
- Yalçin SS, Kondolot M, Albayrak N, Altaş AB, Karacan Y, Kuşkonmaz B, et al. Serological response to influenza vaccine after hematopoetic stem cell transplantation. Annals of Hematology 2010;89(9):913‐8. [DOI] [PubMed] [Google Scholar]
Additional references
- Alistair R, Gavin M, Christopher S, Peter H. Influenza vaccination and chemotherapy: a shot in the dark?. Supportive Care in Cancer 2002;10:462‐65. [DOI] [PubMed] [Google Scholar]
- Anema A, Mills E, Montaner J, Brownstein JS, Cooper C. Efficacy of influenza vaccination in HIV‐positive patients: a systematic review and meta‐analysis. HIV Medicine 2008;9(1):57‐61. [DOI] [PubMed] [Google Scholar]
- Angelo SJ, Marshall PS, Chrissoheris MP, Chaves AM. Clinical characteristics associated with poor outcome in patients acutely infected with Influenza A. Connecticut Medicine 2004;68:199‐205. [PubMed] [Google Scholar]
- Arrowood JR, Hayney MS. Immunization recommendations for adults with cancer. Annals of Pharmacotherapy 2002;36:1219‐29. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cancer prevention and control. Available from: http://www.cdc.gov/cancer/flu/ (accessed 12th December 2010).
- Centers for Disease Control and Prevention. Preventing infections in cancer patients. Available from:http://www.cdc.gov/cancer/flu/#4 (Accessed 30th November 2012).
- Centers for Disease Control and Prevention. Flu Activity & Surveillance. Available from: http://www.cdc.gov/flu/weekly/fluactivity.htm (accessed 12th December 2010).
- Centers for Disease Control and Prevention. Estimates of deaths associated with seasonal influenza ‐ United States, 1976‐2007. Morbidity and Mortality Weekly Report (MMWR) 2010 Aug 27;59(33):1057‐62. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Seasonal Influenza. Available from: http://www.cdc.gov/flu/professionals/vaccination/effectivenessqa.htm (accessed 3oth November 2009).
- Chemaly RF, Ghosh S, Bodey GP, Rohatgi N, Safdar A, Keating MJ, et al. Respiratory viral infections in adults with hematologic malignancies and human stem cell transplantation recipients: a retrospective study at a major cancer center. Medicine (Baltimore) 2006;85(5):278‐87. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
- Cooksley CD, Avritscher EB, Bekele BN, Rolston KV, Geraci JM, Elting LS. Epidemiology and outcomes of serious influenza‐related infections in the cancer population. Cancer 2005;104:618‐28. [DOI] [PubMed] [Google Scholar]
- Jong JC, Beyer WE, Palache AM, Rimmelzwaan GF, Osterhaus AD. Mismatch between the 1997/1998 influenza vaccine and the major epidemic A(H3N2) virus strain as the cause of an inadequate vaccine‐induced antibody response to this strain in the elderly. Journal of Medical Virology 2000;61(1):94‐9. [PubMed] [Google Scholar]
- Elting LS, Whimbey E, Lo W, Couch R, Andreeff M, Bodey GP. Epidemiology of influenza A virus infection in patients with acute or chronic leukemia. Supportive Care in Cancer 1995;3(3):198‐202. [DOI] [PubMed] [Google Scholar]
- Fiore AE, Shay DK, Broder K, Iskander JK, Uyeki TM, Mootrey G, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recommendations and Reports 2009;58:1‐52. [PubMed] [Google Scholar]
- Glezen WP. Clinical practice. Prevention and treatment of seasonal influenza. New England Journal of Medicine 2008;359:2579‐85. [DOI] [PubMed] [Google Scholar]
- Goossen GM, Kremer LCM, Wetering MD. Influenza vaccination in children being treated with chemotherapy for cancer. Cochrane Database of Systematic Reviews 2013, Issue 8. [DOI: 10.1002/14651858.CD006484] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan IA, Chopra R, Swindell R, Mutton KJ. Respiratory viral infections after bone marrow/peripheral stem‐cell transplantation: the Christie hospital experience. Bone Marrow Transplant 2003;32(1):73‐77. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐ analysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issa NC, Fishman JA. Infectious complications of antilymphocyte therapies in solid organ transplantation. Clinical Infectious Diseases 2009;48(6):772‐86. [DOI] [PubMed] [Google Scholar]
- Kamps BS, Hoffmann C, Preiser W. Influenza report. http://www.influenzareport.com/influenzareport.pdf (accessed 31st December 2006).
- Kunisaki KM, Janoff EN. Influenza in immunosuppressed populations: a review of infection frequency, morbidity, mortality, and vaccine responses. Lancet Infectious Diseases 2009;9:493‐504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljungman P. Respiratory virus infections in stem cell transplant patients: the European experience. Biology of Blood and Marrow Transplantation 2001;7:5S‐7S. [DOI] [PubMed] [Google Scholar]
- Machado CM, Boas LS, Mendes AV, Santos MF, Rocha IF, Sturaro D, et al. Low mortality rates related to respiratory virus infections after bone marrow transplantation. Bone Marrow Transplantation 2003;31(8):695‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melcher L. Recommendations for influenza and pneumococcal vaccinations in people receiving chemotherapy. Clinical Oncology (Royal College of Radiologists) 2005;17(1):12‐15. [DOI] [PubMed] [Google Scholar]
- Nichols WG, Guthrie KA, Corey L, Boeckh M. Influenza infections after hematopoietic stem cell transplantation: risk factors, mortality, and the effect of antiviral therapy. Clinical Infectious Diseases 2004;39(9):1300‐06. [DOI] [PubMed] [Google Scholar]
- Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. Newcastle Ottawa Scale (NOS) for assessing the quality of non‐randomized studies in meta‐analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm (accessed June 2010).
- Pirofski LA, Casadevall A. Use of licensed vaccines for active immunization of the immunocompromised host. Clinical Microbiology Reviews 1998;11(1):1‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redelman‐Sidi G, Sepkowitz KA, Huang CK, Park S, Stiles J, Eagan J, et al. 2009 H1N1 influenza infection in cancer patients and hematopoietic stem cell transplant recipients. Journal of Infection 2010;60(4):257‐63. [DOI] [PubMed] [Google Scholar]
- Scottish Intercollegiate Guideline Network. Search Filters, Methodology. Available from: http://www.sign.ac.uk/methodology/filters.html (last modified 16 June 2010; accessed 21st June 2010).
- Dolin, R. Clinical manifestations and diagnosis of seasonal influenza in adults. www.uptodate.com (accessed 31st December 2010).
- World Health Organization. Influenza (Seasonal). Fact sheet N°211; 2009. Available from: http://www.who.int/mediacentre/factsheets/fs211/en/ (accessed 31st December 2010).
- World Health Organization. Global influenza surveillance 2009. Available from: http://www.who.int/csr/disease/influenza/influenzanetwork/en/index.html (accessed 31st December 2010).
- Wiselka M. Influenza: diagnosis, management, and prophylaxis. BMJ 1994;308(6940):1341‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousuf HM, Englund J, Couch R, Rolston K, Luna M, Goodrich J, et al. Influenza among hospitalized adults with leukemia. Clinical Infectious Diseases 1997;24:1095‐99. [DOI] [PubMed] [Google Scholar]


