Abstract
Background
Baby‐led breastfeeding is recommended as best practice in determining the frequency and duration of a breastfeed. An alternative approach is described as scheduled, where breastfeeding is timed and restricted in frequency and duration. It is necessary to review the evidence that supports current recommendations, so that women are provided with high‐quality evidence to inform their feeding decisions.
Objectives
To evaluate the effects of baby‐led compared with scheduled (or mixed) breastfeeding for successful breastfeeding, for healthy newborns.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (23 February 2016), CINAHL (1981 to 23 February 2016), EThOS, Index to Theses and ProQuest database and World Health Organization's 1998 evidence to support the 'Ten Steps' to successful breastfeeding (10 May 2016).
Selection criteria
We planned to include randomised and quasi‐randomised trials with randomisation at both the individual and cluster level. Studies presented in abstract form would have been eligible for inclusion if sufficient data were available. Studies using a cross‐over design would not have been eligible for inclusion.
Data collection and analysis
Two review authors independently assessed for inclusion all potential studies we identified as a result of the search strategy. We would have resolved any disagreement through discussion or, if required, consulted a third review author, but this was not necessary.
Main results
No studies were identified that were eligible for inclusion in this review.
Authors' conclusions
This review demonstrates that there is no evidence from randomised controlled trials evaluating the effect of baby‐led compared with scheduled (or mixed) breastfeeding for successful breastfeeding, for healthy newborns. It is recommended that no changes are made to current practice guidelines without undertaking robust research, to include many patterns of breastfeeding and not limited to baby‐led and scheduled breastfeeding. Future exploratory research is needed on baby‐led breastfeeding that takes the mother's perspective into consideration.
Plain language summary
Patterns of breastfeeding, according to the baby or according to the clock
What is the issue?
Patterns of breastfeeding can vary greatly. Two very different approaches are often used to determine when the baby will breastfeed and for how long. One approach is led by the baby, and is known as baby‐led, unrestricted or breastfeeding on demand. The other approach is led by the clock, and is known as scheduled, timed or restricted breastfeeding.
From the early 20th century women in many health settings were advised to breastfeed according to the clock; timing and restricting both the frequency and length of breastfeeds. This advice was based on bottle‐feeding patterns. This practice changed when baby‐led or demand breastfeeding was advocated. With baby‐led breastfeeding, the amount of milk produced is determined by the baby's demand. The baby then controls the supply of milk, ensuring that enough milk is produced to meet his or her needs. With this approach, close contact between the mother and her baby is encouraged with no restrictions placed on their time together. However, the mother may not always be in a position to breastfeed her baby on demand due to, for example, being separated from her baby for any reason, and there can be uncertainty for the mother if and when her baby does not demand a breastfeed.
Why is this important?
Mothers require information on the frequency and duration of breastfeeds but they receive conflicting advice. Current guidelines encourage baby‐led breastfeeding. It is important to systematically review the evidence, to inform women's decisions on the relative effectiveness of each method.
This review is also important as baby‐led breastfeeding is not always followed, as many women and caregivers seem more comfortable with scheduled rather than baby‐led feeding patterns.
What evidence did we find?
We searched for evidence on 23 February 2016 and identified no new studies for inclusion in the update of this review.
What does this mean?
We looked for studies that compared baby‐led with scheduled (or mixed) breastfeeding for successful breastfeeding for healthy newborn babies. However, no studies were found that met the inclusion criteria. It is recommended that no changes are made to current practice guidelines without undertaking robust research, to include many patterns of breastfeeding and not limited to baby‐led and scheduled breastfeeding. Future exploratory research on baby‐led breastfeeding is also needed that takes the mother's perspective into consideration.
Background
Description of the condition
Breastfeeding is the optimal method of infant feeding with numerous benefits for mother and baby (Victoria 2016). Early initiation of breastfeeding is important in reducing neonatal and early infant mortality (Neovita Study Group 2016). It is recommended that infants are breastfed, exclusively, for the first six months of life (WHO 2001), followed by continued breastfeeding for up to two years or beyond, with appropriate complementary foods (WHO 2002). The World Health Organization (WHO) has set a target of increasing exclusive breastfeeding rates at six months to 50% (WHO 2014). Successful breastfeeding can be considered to have occurred when these targets have been met, but the individual woman’s experience also contributes to her sense of breastfeeding success.
Exclusive breastfeeding requires that the breastfed infant takes no other food or drink for the first six months of life (WHO 2008). Specific benefits of exclusive breastfeeding for six months have been identified (Kramer 2012), but achieving this target has proved difficult. Some increases in exclusive breastfeeding for six months have been reported (CDC 2013), although there are variations between countries and continents in rates of exclusive breastfeeding at six months (Callen 2004). In England, 81% of women initiated breastfeeding while 1% exclusively breastfed at six months (McAndrew 2012). In Norway, where 98% of women initiated breastfeeding, 80% continued at six months with 2.1% breastfeeding exclusively (Häggkvist 2010). In Canada, 89% of women initiated breastfeeding, with 26% exclusively breastfeeding at six months (Gionet 2013). In the USA, 80% of women initiated breastfeeding with 21.9% breastfeeding exclusively at six months (CDC 2016). In Asian and Pacific countries, exclusive breastfeeding at six months was achieved to a greater extent and varied from 7% in Hong Kong to 89% in Korea (OECD/WHO 2014).
While many studies report on exclusive breastfeeding rates at six months, few report data at 24 months, but those that do, report rates higher than exclusive breastfeeding rates at six months in most cases. For example, in Northeast Italy, 98% of women initiated breastfeeding, with 6% exclusively breastfeeding at six months and 12% continuing to breastfeed at 24 months (Carletti 2011). A study from Lao People's Democratic Republic reports that 98.8% of women initiated breastfeeding, with 19.4% exclusively breastfeeding at six months and 18.6% continuing to breastfeed at 24 months (Putthakeo 2009), and in Central and Western China, 98.3% of infants were breastfed, 28.7% were exclusively breastfed under six months and 9.4% continued breastfeeding for two years (Guo 2013). While in Mauritius, 93.4% of women initiated breastfeeding, with 17.9% exclusively breastfeeding at six months and 26.1% continuing to breastfeed for up to two years (Motee 2013).
Description of the intervention
The frequency and duration of a breastfeed
Many factors contribute to successful breastfeeding. One such factor is a combination of the frequency and duration of a breastfeed (WHO 1998). Historically, the frequency and duration of a breastfeed has been guided by two approaches: baby‐led and scheduled breastfeeding. Baby‐led breastfeeding, also known as breastfeeding on demand, unrestricted or breastfeeding in response to infant cues, is recommended as best practice (WHO 1998). The alternative approach is described as scheduled or restricted, where the frequency and duration of a breastfeed follows a predetermined, scheduled pattern.
Baby‐led breastfeeding is recommended as the most suitable approach to determine the frequency and duration of a breastfeed. It is advocated by the Baby Friendly Hospital Initiative (BFHI) in 'The ten steps to successful breastfeeding' (WHO 1998). The 'ten steps' were introduced in 1991 in a global attempt to protect, support and promote breastfeeding (WHO 2009). Collectively, the 'ten steps' are associated with an increase in the initiation of breastfeeding (Hawkins 2014), exclusive breastfeeding (Yotebieng 2015), and duration of breastfeeding (Nickel 2013). However, many studies that assessed the impact of the BFHI have methodological limitations (Howe‐Hayman 2016). Scheduled breastfeeding became popular for a short time in the mid‐18th century among wealthier women (Fildes 1986), and again in the 20th century as a result of increased medicalisation of infant feeding (Klaus 1987; Manz 1999). Demand or baby‐led feeding began to emerge after mid‐20th century as the preferred approach (Crowther 2009).
The frequency and duration of a breastfeed vary greatly (Kent 2012), and infants who breastfeed usually feed more frequently compared to infants who bottle feed or who combine bottle and breastfeeding (Casiday 2004). The baby's demand influences the quantity of milk produced (Jonas 2016). In this way, baby‐led breastfeeding supports the physiology of lactation as a supply‐demand feedback mechanism and ensures sufficient breast milk is produced to meet the demands and needs of the baby (Kent 2012). A baby‐led approach lends itself to unrestricted access between the mother and her baby. This supports the mother as she makes the transition to motherhood; the baby as he or she adapts to extrauterine life; and both together, as they begin to form a very special bond (Crenshaw 2007).
One major limitation of baby‐led breastfeeding is its failure to acknowledge the significance of the mother. The woman's needs and the demands of mothering can influence her breastfeeding experience (Shloim 2015). At the very least, maternal issues such as pain (Brown 2016), extra demands with multiple births (Leonard 2000) or socio‐economic concerns (Ghosh 2006) could challenge the mother's ability to sustain what is considered to be a baby‐led approach. There could be concerns for the mother when the baby does not demand a breastfeed within what is regarded as a reasonable amount of time (Renfrew 2005), and when no limits exist, there could be uncertainty with demand breastfeeding (Dykes 2005; Leurer 2015). Greater consideration of the mother is evident in other approaches to breastfeeding, for example 'responsive' breastfeeding (Entwistle 2013, p. 74) and 'breastfeeding mutuality' (Schafer 2015, p. 548).
Baby‐led breastfeeding
Baby‐led or demand breastfeeding is defined by the WHO as occurring when mothers of healthy babies are encouraged to "have no restrictions placed on the frequency or length of their babies' breastfeeds. They should be advised to breastfeed their babies whenever they are hungry or as often as the baby wants and they should wake their babies for breastfeeding if the babies sleep too long or the mother’s breasts are overfull" (WHO 1998 p. 68).
Scheduled breastfeeding
Scheduled breastfeeding occurs when mothers of healthy babies breastfeed their babies on a schedule, that is not determined by the baby. The frequency of feeds is predetermined and usually time‐restricted. Common frequencies include three‐ or four‐hourly breastfeeds throughout a 24‐hour period. The duration of feeds may also be predetermined and time‐restricted. The duration can be restricted to a predetermined number of minutes, for one or both breasts per feeding episode.
Mixed patterns of breastfeeding
Mixed patterns of breastfeeding occur when mothers of healthy babies who are breastfeeding:
alternate between approaches (e.g. the mother may breastfeed on demand on some occasions and may breastfeed according to a schedule on other occasions);
combine aspects from both approaches (e.g. the frequency of the breastfeed may be baby‐led and the duration scheduled or the frequency may be scheduled and the duration baby‐led).
How the intervention might work
There are many ways in which the frequency and duration of a breastfeed might work and contribute to successful breastfeeding. Emotional, informational and practical aspects of the intervention might have an effect. The frequency with which a baby breastfeeds may be a source of reassurance or cause difficulty for women in the early days, especially if the baby is perceived to be feeding frequently. This can be misinterpreted as insufficient milk; and has been cited by women as one of the main reasons for supplementing with formula (Pierro 2016) and discontinuing breastfeeding (Marshall 2007; Hinsliff‐Smith 2014; Teich 2014). Frequent feeding can also lead the health professional or family to recommend a bottle feed (Marshall 2007), and complementary bottle feeds have been identified as posing a risk to successful breastfeeding (Howel 2013; Parry 2013).
The informational aspect of the frequency and duration of a breastfeed is crucial to successful breastfeeding. Frequent feeding can undermine a woman's confidence with breastfeeding but women are reassured when they know the reason for frequent feeding (Marshall 2007). Baby‐led breastfeeding encourages the supply feedback mechanism that underpins the physiology of lactation. Baby‐led breastfeeding allows the milk supply to meet the demand set by the baby (Kent 2006; Kent 2012; Jonas 2016), thereby sustaining lactation, encouraging exclusive breastfeeding. However, antenatal expectations of breastfeeding do not always match the woman's reality postnatally (Hoddinott 2012; Hinsliff‐Smith 2014).
Practical (technical) aspects of the frequency and duration of a breastfeed might contribute to successful breastfeeding. It is important especially in the early days that someone sits with the mother for the duration of a breastfeed (Hoddinott 2012) and provides guidance on practical aspects such as; recognising infant feeding cues, milk production and transfer, responsive breastfeeding (Entwistle 2013), attachment and positioning. Some women can find breastfeeding demanding (Hinsliff‐Smith 2014), while others will not find it so (Hoddinott 2012). Scheduled breastfeeding provides a structured and predictable pattern to the frequency and duration of a breastfeed, which would allow the mother to deal with competing demands on her time (Diaz 1995; Leonard 2000; Ghosh 2006) and establish a pattern that would allow her exclusively to breastfeed. However, flexible working hours can also help the working mother continue breastfeeding (Skafida 2012). Mixed patterns of breastfeeding could facilitate baby‐led breastfeeding, and at other times accommodate a schedule.
Why it is important to do this review
Current guidelines issued by the WHO and the United Nations Children’s Fund (WHO 2009), through the Baby Friendly Hospital initiative, encourage baby‐led breastfeeding. It is important to systematically review the evidence of the effectiveness of baby‐led and scheduled breastfeeding, to provide high‐quality evidence to inform women's decisions on the relative effectiveness of each method. It may seem counter‐intuitive to undertake this review and question an aspect of breastfeeding practice that has become so accepted, but it is important to not only base practice on evidence, but also to question and assess such evidence. A review of practice bulletins from the American College of Obstetricians revealed that just one third were based on "good and consistent scientific evidence"'' (Wright 2011, p. 505) and a review of the 'Green Top Guidelines' from the Royal College of Obstetricians and Gynaecologists revealed that overall, less than one fifth were based on high‐quality evidence (Prusova 2014). When questioning an engrained practice such as baby‐led breastfeeding, there is an obligation to undertake research that is robust (Woolridge 2008). Therefore a review of existing trials is an appropriate starting point.
This review is also important as baby‐led breastfeeding despite being considered "an entrenched piece of evidenced based practice" (Woolridge 2008 p. 353), is not always followed, as many women and caregivers seem uncomfortable with baby‐led feeding patterns that deviate from scheduled feeding patterns (Renfrew 2005). This review is necessary to initiate dialogue, as history tells us that the frequency and duration of a breastfeed are very susceptible to changing fashion and trends (Fildes 1986), and the impact of scheduling breastfeeds in the 20th century continues to exert an influence (Manz 1999). Current popular media bears testament to this, where it is evident that guidance is frequently provided to mothers that is not consistent with practice guidelines, as various schedules and restrictions are recommended. Mothers require information on the frequency and duration of breastfeeds (Leurer 2015), but receive conflicting advice (Graffy 2005). Health professionals also require up‐to‐date information (Ogburn 2011), based on the best available evidence.
Objectives
To evaluate the effects of baby‐led compared with scheduled (or mixed) breastfeeding on successful breastfeeding, for healthy newborns.
Methods
Criteria for considering studies for this review
Types of studies
Randomised and quasi‐randomised trials with randomisation at both the individual and cluster level. Studies presented in abstract form were eligible for inclusion but only if sufficient data were available. Given the nature of the intervention and the changing pattern of infant behaviours, cross‐over studies were not eligible for inclusion.
Types of participants
Breastfeeding mothers.
Breastfeeding healthy newborns (born at 37 to 42 completed weeks' gestation, including singleton or multiple births).
Types of interventions
Interventions
Scheduled breastfeeding: where the frequency and the duration of breastfeeds are scheduled, timed or restricted.
Baby‐led breastfeeding: where the frequency and the duration of breastfeeds are baby‐led or on demand.
Mixed patterns of breastfeeding: where the frequency and duration of breastfeeds is a combination of, or alternates between, baby‐led and scheduled breastfeeding.
Comparisons
Baby‐led compared with scheduled breastfeeding.
Baby‐led compared with mixed patterns of breastfeeding.
Scheduled breastfeeding compared with mixed patterns of breastfeeding.
Types of outcome measures
Primary outcomes
1. Proportion of women breastfeeding exclusively up to six months
Exclusive breastfeeding means that "the infant receives breast milk (including expressed breast milk or breast milk from a wet nurse) and allows the infant to receive ORS (oral rehydration solutions), drops and syrups (vitamins, minerals, medicines) but nothing else" (WHO 2008).
2. Proportion of women breastfeeding up to 24 months
Breastfeeding means that the infant receives breast milk (including expressed breast milk or breast milk from a wet nurse) and allows the infant to receive any food or liquid including non‐human milk and formula (WHO 2008).
Secondary outcomes
Neonatal secondary outcomes
Exclusive breastfeeding may influence neonatal outcomes as blood glucose levels become stabilised following birth with unrestricted breastfeeding (Watt 2013); dehydration, hypernatraemia and weight loss are associated with inadequate breastfeeding (Watt 2013); and both physiological jaundice and prolonged jaundice are more likely to develop in the breastfed baby in comparison to the bottle‐fed baby (NICE 2010).
Neonatal hypoglycaemia (low blood sugar measurement (Tin 2014)).
Neonatal hypernatraemia (high blood sodium measurement (Oddie 2013).
Infant's growth, as measured by head circumference, length and weight.
Neonatal jaundice.
Maternal secondary outcomes
Maternal outcomes such as sore nipples (Kent 2015) have been linked to cessation of breastfeeding (McClellan 2012; Brown 2016); breast engorgement may prevent successful breastfeeding (Mangesi 2016); and exclusive breastfeeding might influence maternal satisfaction as many mothers intend to breastfeed exclusively but some do not achieve their aim (Perrine 2012).
Sore nipples.
Breast engorgement.
Mother's satisfaction as measured by trial authors.
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting their Information Specialist (23 February 2016).
The Register is a database containing over 22,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate the Pregnancy and Childbirth Group’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth Group in the Cochrane Library and select the ‘Specialized Register ’ section from the options on the left side of the screen.
Briefly, the Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by their Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth Group review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set which has been fully accounted for in the relevant review section (Excluded studies).
We also searched CINAHL (1981 to 23 February 2016) using the search strategy detailed in Appendix 1.
Supplementary to the search by the Information Specialist, we searched EThOS, Index to Theses and ProQuest databases (10 May 2016) (see:Appendix 2).
Searching other resources
We also assessed trials included in the WHO's evidence to support the 'Ten Steps' to successful breastfeeding (WHO 1998) (see: Appendix 2)
We did not apply any language or date restrictions.
Data collection and analysis
Two review authors (Anne Fallon (AF) and Deirdre van der Putten (DvdP)) independently assessed for inclusion all the potential studies we identified as a result of the search strategy. No studies were eligible for inclusion. We would have resolved any disagreement through discussion with a third person (Declan Devane (DD)), but this was not necessary, although DD reviewed excluded studies and agreed with reasons for exclusion.
Full methods of data collection and analysis to be used in future updates of this review, if eligible studies are identified, are given in Appendix 3.
Results
Description of studies
No studies were eligible for inclusion in this review as outlined in Characteristics of excluded studies table.
Results of the search
Our search of the literature identified 16 citations referring to 10 studies.
The search of the Cochrane Pregnancy and Childbirth Group's Trials Register identified 13 citations that referred to eight studies (Illingworth 1952; Johnson 1976; Carlsson 1978; Salariya 1978; Ojofeitimi 1982; Gale 1989; Pinilla 1993; Maisels 1994).
A CINAHL search undertaken by the Information Specialist identified 387 citations, but no relevant studies.
The supplementary search (Appendix 2) of EThOS, Index to Theses and ProQuest databases identified 340, 247, 602 citations, respectively, but none were considered relevant for this review.
The search of the WHO's evidence to support the 'Ten Steps' to successful breastfeeding (WHO 1998) identified four citations that referred to three studies. One study had been identified in the search of the Cochrane Pregnancy and Childbirth Group's register (Illingworth 1952). The remaining three citations referred to two studies (Slaven 1981; De Carvalho 1983).
See Figure 1.
1.
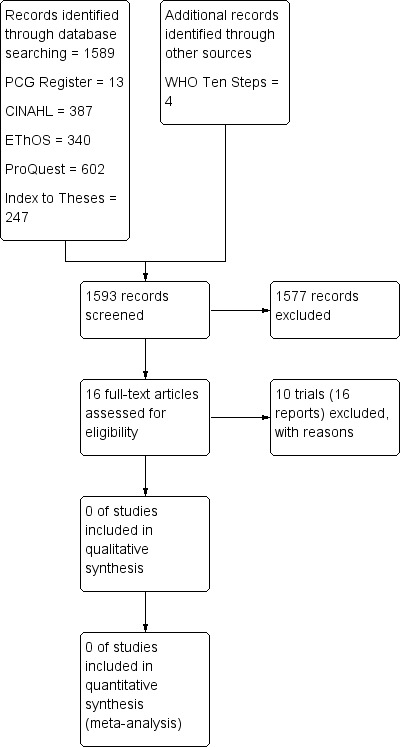
Study flow diagram.
Included studies
No studies were eligible for inclusion.
Excluded studies
Ten studies were excluded as follows.
Four trials did not examine patterns of breastfeeding (Johnson 1976; Carlsson 1978; Ojofeitimi 1982; Pinilla 1993).
Two trials compared different schedules of breastfeeding but did not include baby‐led breastfeeding (Salariya 1978; Gale 1989).
One trial was excluded because it was not possible to determine the confounding effect of the study site from any observed differences due to the intervention (Illingworth 1952).
One trial was excluded as it was not possible to determine the confounding effect of the time period used in the trial from any observed differences resulting from the intervention (De Carvalho 1983).
One trial was excluded as the gestational age of infants did not meet the inclusion criteria for this review (Maisels 1994).
One trial provided insufficient detail to inform judgements as to whether it should be included or excluded (Slaven 1981).
Risk of bias in included studies
Risk of bias was not assessed as no studies were included in the review.
Effects of interventions
Effects of interventions were not assessed as no studies were included in the review.
Discussion
Although this review has not been able to demonstrate which pattern is optimum, it is important to note that baby‐led breastfeeding was interpreted differently across studies that were considered for inclusion. For example, when compared with scheduled breastfeeding, baby‐led breastfeeding was described as breastfeeding the baby frequently in one excluded study (De Carvalho 1983), but not considered frequent in another (Maisels 1994). Furthermore, schedules identified in excluded studies were imposed by the ward routine or the study protocol not by the mother (Characteristics of excluded studies), and the mother's perspective was largely omitted from baby‐led breastfeeding. Clarity on the tenets of baby‐led breastfeeding is therefore required, so that greater guidance is provided to mothers on the frequency and duration of a breastfeed.
In addition to the reasons for excluding studies (Characteristics of excluded studies), it is important to note the context in which the identified studies took place as many practices would not be considered supportive today (Ahluwalia 2012; Howel 2013; Parry 2013). These practices include giving dextrose or water supplements, giving formula supplements, delaying the first breastfeed up to six hours after birth, and breastfeeding on a schedule for the first 48 hours prior to baby‐led breastfeeding. There is a need for greater research on this topic and it should be considered that the ideal feeding pattern for mother and baby might lie outside or indeed in addition to, baby‐led or scheduled breastfeeding.
Authors' conclusions
Implications for practice.
There is no evidence from randomised trials to inform decisions about optimum feeding patterns. It is beyond the scope of this review to identify or recommend other sources of evidence, as they have not been considered in this review.
It is recommended that no changes are made to current practice guidelines (WHO 1998) without undertaking robust research, as recommended in (Implications for research) section below.
Implications for research.
This review demonstrates that there is no evidence from randomised controlled trials to evaluate the effects of baby‐led compared with scheduled (or mixed) breastfeeding on successful breastfeeding, for healthy newborns.
It is important to consider the historical context of research undertaken on this topic as it has implications for future research. Breastfeeding schedules re‐surfaced in the 20th century, at a time when healthcare professionals provided guidance to mothers on the frequency and duration of breastfeeds, based on bottle‐feeding patterns (Crowther 2009). With the realisation that breastfeeding did not follow a bottle‐feeding pattern, baby‐led or demand breastfeeding emerged as the alternative. Research undertaken from the mid‐20th century was therefore based on the premise that scheduled breastfeeding was the problem and demand breastfeeding was the solution or vice versa, thus restricting the breadth and depth of research undertaken. In addition the mother's perspective was largely omitted from baby‐led breastfeeding with the result that the mother's perspective has not been adequately considered in research on this topic.
Future research is needed, that explores all aspects of the frequency and duration of breastfeeding, as the foundation on which this topic is based is weak at best.
What's new
| Date | Event | Description |
|---|---|---|
| 23 February 2016 | New search has been performed | Search updated and no new studies were identified. |
| 23 February 2016 | New citation required but conclusions have not changed | The conclusions have not changed essentially, however the need to include the mother in the concept of baby‐led feeding is now highlighted. |
Acknowledgements
We wish to acknowledge the contribution of Lynn Hampson (Information Specialist), Frances Kellie (Managing Editor) and Leanne Jones (Associate Editor) of Cochrane Pregnancy and Childbirth.
This research was supported by a grant from the Evidence and Programme Guidance Unit, Department of Nutrition for Health and Development, World Health Organization (WHO). The findings, interpretations and conclusions expressed in this paper are entirely those of the authors and should not be attributed in any manner whatsoever to WHO.
Appendices
Appendix 1. CINAHL search strategy
1. exp CLINICAL TRIALS/
2. (clinic* ADJ trial*).ti,ab
3. (trebl* ADJ blind*).ti,ab
4. (trebl* ADJ mask*).ti,ab
5. (tripl* ADJ blind*).ti,ab
6. (tripl* ADJ mask*).ti,ab
7. (doubl* ADJ blind*).ti,ab
8. (doubl* ADJ mask*).ti,ab
9. (singl* ADJ blind*).ti,ab
10. (singl* ADJ mask*).ti,ab
11. (randomi* ADJ control* ADJ trial*).ti,ab
12. RANDOM ASSIGNMENT/
13. (random* ADJ allocat*).ti,ab
14. placebo*.ti,ab
15. PLACEBOS/
16. QUANTITATIVE STUDIES/
17. (allocat* ADJ random*).ti,ab
18. schedule*.ti,ab
19. pattern*.ti,ab
20. restrict*.ti,ab
21. unrestrict*.ti,ab
22. cue*.ti,ab
23. baby‐led.ti,ab
24. infant‐led.ti,ab
25. demand*.ti,ab
26. time.ti,ab
27. timing.ti,ab
28. routine*.ti,ab
29. natural.ti,ab
30. breastfeeding.ti,ab
31. breastfed.ti,ab
32. exp BREAST FEEDING/
33. (breast ADJ fe*).ti,ab
34. breast‐fe*.ti,ab
35. 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17
36. 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29
37. 30 OR 31 OR 32 OR 33 OR 34
38. 35 AND 36 AND 37
Appendix 2. Supplementary search strategy
| Supplementary search to the search undertaken by the Information Specialist | |||||
| Date of search December 2011, updated 6 November 2013, updated 10 May 2016. | |||||
| Source | Search terms | Hits /titles screened | Abstracts screened | Full text reviewed | Results |
| EThOS | Breastfeeding | 128 | 3 | 0 | 0 |
| Breast‐feeding | 68 | 5 | 0 | 0 | |
| Breastfeed | 26 | 1 | 0 | 0 | |
| Breast‐feed | 68 | 0 | 0 | 0 | |
| Breastfed | 28 | 0 | 0 | 0 | |
| Breast‐fed | 22 | 0 | 0 | 0 | |
| Proquest | Breastfeeding | 223 | 0 | 0 | 0 |
| Breast‐feeding | 210 | 0 | 0 | 0 | |
| Breastfeed | 55 | 0 | 0 | 0 | |
| Breast‐ feed | 55 | 0 | 0 | 0 | |
| Breastfed | 59 | 0 | 0 | 0 | |
| Index to theses | Breastfeeding | 132 | 0 | 0 | 0 |
| Breast‐feeding | 48 | 0 | 0 | 0 | |
| Breastfeed | 23 | 0 | 0 | 0 | |
| Breast‐feed | 6 | 0 | 0 | 0 | |
| Breastfed | 9 | 0 | 0 | 0 | |
| Breast‐fed | 29 | 0 | 0 | 0 | |
| WHO (1998) Evidence for the ten steps to successful breastfeeding |
Step 8. | 4 | 4 | 4 | 0 |
Appendix 3. Methods of data collection and analysis to be used in future updates of this review
Data collection and analysis
The following methods of data collection and analysis are based on Cochrane Pregnancy and Childbirth standard methods text template.
Selection of studies
Two review authors (Anne Fallon (AF) and Deirdre van der Putten (DvdP)) will independently assess for inclusion all the potential studies we identify as a result of the search strategy. We will resolve any disagreement through discussion or, if required, consult a third person (Declan Devane (DD)).
The following sections describe the methods that will be used, in future updates of this review, if eligible studies are identified.
Data extraction and management
We will design a form to extract data. For eligible studies, at least two review authors (AF, DvdP) will extract the data using the agreed form. We will resolve discrepancies through discussion or, if required, we will consult a third person (DD). We will enter data into Review Manager software (RevMan 2014) and check for accuracy.
When information regarding any of the above is unclear, we will attempt to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors (AF, DvdP) will independently assess risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We will resolve any disagreement by discussion or by involving a third assessor (DD).
(1) Random sequence generation (checking for possible selection bias)
We will describe for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We will assess the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We will describe for each included study the method used to conceal allocation to interventions prior to assignment and will assess whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We will assess the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We will describe for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We will consider that studies are at low risk of bias if they were blinded, or if we judge that the lack of blinding would be unlikely to affect results. We will assess blinding separately for different outcomes or classes of outcomes.
We will assess the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We will describe for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We will assess blinding separately for different outcomes or classes of outcomes.
We will assess methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We will describe for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We will state whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information is reported, or can be supplied by the trial authors, we will re‐include missing data in the analyses which we undertake.
We will assess methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
We will discuss whether missing data greater than 20% might (a) be reasonably expected (acknowledging that with long‐term follow‐up, complete data are difficult to attain), and (b) impact on outcomes.
(5) Selective reporting (checking for reporting bias)
We will describe for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We will assess the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We will describe for each included study any important concerns we have about other possible sources of bias.
We will assess whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We will make explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to (1) to (6) above, we will assess the likely magnitude and direction of the bias and whether we consider it is likely to impact on the findings. We will explore the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Assessment of the quality of the evidence using the GRADE approach
For this update the quality of the evidence will be assessed using the GRADE approach as outlined in the GRADE handbook in order to assess the quality of the body of evidence relating to the following outcomes for the main comparisons.
Proportion of women breastfeeding exclusively up to six months.
Proportion of women breastfeeding up to 24 months.
Neonatal hypoglycaemia (low blood sugar measurement (Tin 2014)).
Infant's growth, as measured by head circumference, length and weight.
Neonatal jaundice.
Sore nipples.
Mother's satisfaction as measured by trial authors.
We will use the GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create ’Summary of findings’ tables. A summary of the intervention effect and a measure of quality for each of the above outcomes will be produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we will present results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we will use the mean difference if outcomes are measured in the same way between trials. We will use the standardised mean difference to combine trials that measure the same outcome, but use different methods.
Unit of analysis issues
Cluster‐ randomised trials
We will include cluster‐randomised trials in the analyses along with individually‐randomised trials. We will adjust their sample sizes using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Dealing with missing data
For included studies, we will note levels of attrition. We will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we will carry out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we will attempt to include all participants randomised to each group in the analyses, and all participants will be analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial will be the number randomised minus any participants whose outcomes are known to be missing.
Assessment of heterogeneity
We will assess statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We will regard heterogeneity as substantial if an I² is greater than 30% and either the Tau² is greater than zero, or there is a low P value (< 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
If there are 10 or more studies in the meta‐analysis, we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We will carry out statistical analysis using the Review Manager software (RevMan 2014). We will use fixed‐effect meta‐analysis for combining data where it is reasonable to assume that studies are estimating the same underlying treatment effect: i.e. where trials are examining the same intervention, and the trials’ populations and methods are judged sufficiently similar. If there is clinical heterogeneity sufficient to expect that the underlying treatment effects differ between trials, or if substantial statistical heterogeneity is detected, we will use random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials is considered clinically meaningful. The random‐effects summary will be treated as the average of the range of possible treatment effects and we will discuss the clinical implications of treatment effects differing between trials. If the average treatment effect is not clinically meaningful, we will not combine trials.
If we use random‐effects analyses, the results will be presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
If we identify substantial heterogeneity, we will investigate it using subgroup analyses and sensitivity analyses. We will consider whether an overall summary is meaningful, and if it is, use random‐effects analysis to produce it. We have not specified any a priori subgroup analyses.
Sensitivity analysis
We will perform sensitivity analysis based on trial quality, separating high‐quality trials from trials of lower quality. We will define 'high quality', for the purposes of this sensitivity analysis, as a trial having adequate allocation concealment and a 'reasonably expected loss to follow‐up' classified as less than 20%, given the stated importance of attrition as a quality measure (Tierney 2005). We will restrict sensitivity analyses to primary outcomes.
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Carlsson 1978 | This study examined the effects of different amounts of body contact between mothers and newborns immediately following birth on nursing behaviour. Mother and infant pairs (n = 62) were selected and assigned to 1 of 3 groups. Group A received extended contact at birth where the mother kept her baby for 1 hour after birth and followed a new ward routine where more contact between mother and baby was encouraged. Group B also received extended contact at birth and followed the old ward routine. Group C received limited contact at birth where mother held her baby for a maximum of 5 minutes and then followed the old ward routine. This study was excluded as it did not compare baby‐led to scheduled breastfeeding and therefore did not meet the inclusion criteria for this review. |
| De Carvalho 1983 | This is a quasi‐randomised trial of 44 mother‐infant pairs. Mothers (n = 24) were allocated to the control group if they delivered during the months of July and August. Mothers in the control group were advised to breastfeed their infants according to the ward routine (3 to 4 hourly). Mothers (n = 20) were allocated to the intervention group if they delivered during the months of September and October and were encouraged to nurse their infants frequently. As there was only 1 control and 1 intervention period, it is not possible to determine the confounding effect of the time period from any observed differences, resulting from the intervention. |
| Gale 1989 | This study compared 2 schedules of breastfeeding; 3‐hourly versus 4‐hourly which were described by the authors as "two common breast‐feeding regimes on a maternity ward" (p. 458). Baby‐led breastfeeding was not included, therefore the study did not meet the inclusion criteria for this review. |
| Illingworth 1952 | It is unclear how participants were allocated in this study. This appears to be a controlled clinical trial without randomisation or quasi‐randomisation. Further, this study compared a self‐demand with a rigid schedule of breastfeeding. Mothers and babies were housed on 2 hospital floors. All babies were breastfed on a schedule for the first 2 days on both floors. On the third postnatal day, one floor was allocated to a 'self‐demand' and one to a 'rigid' schedule. Infants allocated to the rigid schedule were fed 4‐hourly by day and once at night as per the study protocol. Half way through the study, an attempt was made to switch the floor allocation, but it was not successful. There was resistance on one floor to switching from the 'self‐demand' to the 'rigid schedule', as it was found easier. As a result no babies on one of the two floors were fed on a rigid schedule. Therefore, it is not possible to determine the confounding effect of site from any observed differences due to the intervention rather than to other site‐specific variable. |
| Johnson 1976 | This study compared initiation of breastfeeding at 1 hour following birth with initiation at 16 hours following birth. The study did not meet the inclusion criteria for this review. |
| Maisels 1994 | Infants were randomly assigned to a frequent or demand breastfeeding schedule. Infants allocated to the frequent group were advised to feed their infants at least every two hours during the day and no less than every three hours at night, according to the study protocol. This study was excluded as infants with a gestational age of ≥ 36 weeks were included in the study, which was not within the definition used for term babies in this review. The trial reported on the 10th to the 90th percentile (inner 80%); as a result it is likely that infants at both the lower and upper limits were excluded. |
| Ojofeitimi 1982 | This study compared early initiation of colostrum with glucose water on intestinal bacteria in neonates. Baby‐led and scheduled breastfeeding were not studied. The study did not meet the inclusion criteria for this review. |
| Pinilla 1993 | This study investigated if exclusively breast‐fed infants could be taught to sleep through the night. The study did not meet the inclusion criteria for this review. |
| Salariya 1978 | This study compared 2 schedules of breastfeeding; 2‐hourly versus 4‐hourly according to the study protocol. The study did not meet the inclusion criteria for this review. |
| Slaven 1981 | This trial was reported only in the form of a response letter, that compared timed versus unlimited breastfeeding. Two wards were allocated to the timed regimen and 2 wards 'allowed mothers to breastfeed for any length of time that seemed suitable to them'. It is not clear how mothers were assigned to the intervention or the control group. A policy of breastfeeding on demand existed at the time in the hospital where the study took place. Limited detail was provided in the report. |
Differences between protocol and review
Supplementary to the search by the Information Specialist, we changed our search methods to search EThOS, Index to Theses and ProQuest databases. We also assessed trials included in the World Health Organization's (WHO 1998) evidence to support demand breastfeeding. A search of Embase is included in the Pregnancy and Childbirth Group's Trials Register and the CINAHL search was undertaken by the Information Specialist.
Changes were made to the background section of the protocol and our methods have been updated in line with the Cochrane Handbook for Systematic Reviews of Intervention and the standard methods text template of Cochrane Pregnancy and Childbirth.
We also added definitions to two of our neonatal secondary outcomes:
neonatal hypoglycaemia (low blood sugar measurement (Tin 2014);
neonatal hypernatraemia (high blood sodium measurement (Oddie 2013).
The title of the review changed from 'Baby‐led versus scheduled breastfeeding for healthy newborns' (at the protocol stage) to 'Baby‐led compared with scheduled (or mixed) breastfeeding for successful breastfeeding' at the review stage.
Deirdre van der Putten joined and Christina Engel left the review team.
An update to the review was undertaken in June 2016, no new studies were included.
Contributions of authors
Anne Fallon drafted the protocol and review. She provided a midwife's clinical perspective and assessed studies for inclusion.
Deirdre van der Putten joined the review team after the protocol stage. She provided a midwife's clinical perspective for the review, assessed studies for inclusion and also commented on all sections through to the final review.
Edina Moylett provided a paediatrician's clinical perspective and commented on all sections of the protocol through to the final review.
Cindy Dring provided a consumer's perspective and commented on all sections of the protocol through to the final review.
Gerard Fealy commented on all sections of the protocol through to the final review.
Declan Devane provided a midwife's clinical perspective, a methodological perspective and advice on writing the protocol and review. He was consulted on decisions to include or exclude studies.
Sources of support
Internal sources
National University of Ireland Galway, Galway, Ireland.
University College Dublin, Dublin, Ireland.
External sources
-
Health Research Board, Ireland.
Cochrane Fellowship
Evidence and Programme Guidance Unit, Department of Nutrition for Health and Development, World Health Organization, Switzerland.
Declarations of interest
Anne Fallon is an International Board Certified Lactation Consultant (IBCLC) and Health Research Board (Ireland) Cochrane Research Fellow.
Deirdre Van der Putten: none known.
Cindy Dring is a Leader with La Leche League International.
Edina H Moylett: none known.
Gerard Fealy: none known.
Declan Devane: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies excluded from this review
Carlsson 1978 {published data only}
- Carlsson SG, Fagerberg H, Horneman G, Hwang CP, Larsson K, Rodholm M, et al. Effects of amount of contact between mother and child on the mother's nursing behavior. Developmental Psychobiology 1978;11:143‐50. [DOI] [PubMed] [Google Scholar]
- Carlsson SG, Fagerberg H, Horneman G, Hwang CP, Larsson K, Rodholm M, et al. Effects of various amounts of contact between mother and child on the mother's nursing behavior: a follow‐up study. Infant Behaviour and Development 1979;2:209‐14. [DOI] [PubMed] [Google Scholar]
- Carlsson SG, Larsson K, Schaller J. Early mother‐child contact and nursing. Reproduction, Nutrition, Development 1980;20:881‐9. [DOI] [PubMed] [Google Scholar]
De Carvalho 1983 {published data only}
- Carvalho M, Robertson S, Friedman A, Klaus M. Effect of frequent breast‐feeding on early milk production and infant weight gain. Pediatrics 1983;72(3):307‐11. [PubMed] [Google Scholar]
- Carvalho M, Robertson S, Klaus M. Does the duration and frequency of early breastfeeding affect nipple pain?. Birth 1984;11(2):81‐4. [DOI] [PubMed] [Google Scholar]
Gale 1989 {published data only}
- Gale R, Dollberg S, Branski D, Stevenson DK, Seidman DS. Breast‐feeding of term infants. Three‐hour vs four‐hour non‐demand. A randomized controlled reappraisal of hospital‐based feeding schedules. Clinical Pediatrics 1989;28(10):458‐60. [DOI] [PubMed] [Google Scholar]
Illingworth 1952 {published data only}
- Illingworth RS, Stone DGH, Jowett GH, Scott JF. Self‐demand feeding in a maternity unit. Lancet 1952;1:683‐7. [DOI] [PubMed] [Google Scholar]
Johnson 1976 {published data only}
- Johnson NW. Breast‐feeding at one hour of age. American Journal of Maternal Child Nursing 1976;1:12‐6. [PubMed] [Google Scholar]
Maisels 1994 {published data only}
- Acquavita A, Vain N, Maisles MJ, Cohen A, Blanco N, Digregorio J. Effect of breast feeding frequency on serum bilirubin (SB) levels [abstract]. Pediatric Reserach 1991;30:390. [Google Scholar]
- Maisels J, Vain N, Acquavita AM, Blanco NV, Cohen A, DiGregorio J. The effect of breast‐feeding frequency on serum bilirubin levels. American Journal of Obstetrics and Gynecology 1994;170(3):880‐3. [DOI] [PubMed] [Google Scholar]
- Vain N, Acquavita AM, Maisels MJ, Blanco NV, Cohen A, Gregorio J. Effect of breast feeding frequency on serum bilirubin (SB) levels. Pediatric Research 1990;27(4):259A. [Google Scholar]
Ojofeitimi 1982 {published data only}
- Ojofeitimi EO, Elegbe IA. The effect of early initiation of colostrum feeding on proliferation of intestinal bacteria in neonates. Clinical Pediatrics 1982;21:39‐42. [DOI] [PubMed] [Google Scholar]
Pinilla 1993 {published data only}
- Pinilla T, Birch LL. Help me make it through the night: behavioral entrainment of breast‐fed infants' sleep patterns. Pediatrics 1993;91(2):436‐44. [PubMed] [Google Scholar]
Salariya 1978 {published data only}
- Salariya EM, Easton PM, Cater JI. Duration of breast‐feeding after early initiation and frequent feeding. Lancet 1978;2(8100):1141‐3. [DOI] [PubMed] [Google Scholar]
- Salariya EM, Easton PM, Cater JI. Early and often for best results. RCT on breast feeding. Nursing Mirror 1979;148:15‐7. [PubMed] [Google Scholar]
Slaven 1981 {published data only}
- Slaven S, Harvey D. Unlimited sucking time improves breast feeding. Lancet 1981;317(8216):392‐3. [DOI] [PubMed] [Google Scholar]
Additional references
Ahluwalia 2012
- Ahluwalia IB, Morrow B, D’Angelo D, Li R. Maternity care practices and breastfeeding experiences of women in different racial and ethnic groups: pregnancy risk assessment and monitoring system (PRAMS). Maternal and Child Health Journal 2012;16:1672–8. [DOI] [PubMed] [Google Scholar]
Brown 2016
- Brown A, Rance J, Bennett P. Understanding the relationship between breastfeeding and postnatal depression: the role of pain and physical difficulties. Journal of Advanced Nursing 2016;72(2):273‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Callen 2004
- Callen J, Pinelli J. Incidence and duration of breastfeeding for term infants in Canada, United States, Europe, and Australia: a literature review. Birth 2004;31(4):285‐92. [DOI] [PubMed] [Google Scholar]
Carletti 2011
- Carletti C, Pani P, Knowles A, Monasta L, Montico M, Cattaneo A. Breastfeeding to 24 months of age in the northeast of Italy: a cohort study. Breastfeeding Medicine 2011;6(4):177‐82. [DOI] [PubMed] [Google Scholar]
Casiday 2004
- Casiday RE, Wright CM, Panter‐Brick C, Parkinson KN. Do early infant feeding patterns relate to breast‐feeding continuation and weight gain?. European Journal of Clinical Nutrition 2004;58:1290‐6. [DOI] [PubMed] [Google Scholar]
CDC 2013
- Centre for Disease Control and Prevention. Progress in increasing breastfeeding and reducing racial/ethnic dfferences‐United States, 2000‐2008 births. Morbidity and Mortality Weekly Report 2013;62(5):77‐90. [PMC free article] [PubMed] [Google Scholar]
CDC 2016
- Centre for Disease Control and Prevention. Breastfeeding among U.S. Children Born 2002‐2012, CDC National Immunization Surveys. www.cdc.gov/breastfeeding/data/nis_data/index.htm (accessed May 2016).
Crenshaw 2007
- Crenshaw J. Care practice #6: No separation of mother and baby, wIth unlimited opportunities for breastfeeding. Journal of Perinatal Education 2007;16(3):39‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crowther 2009
- Crowther SM, Reynolds LA, Tansey EM (eds). The Resurgence of Breastfeeding, 1975‐2000. Wellcome Witnesses to Twentieth Century Medicine. Vol. 35, London: Wellcome Trust Centre for the History of Medicine at UCL, 2009. [Google Scholar]
Dykes 2005
- Dykes F. 'Supply' and 'demand': breastfeeding as labour. Social Science and Medicine 2005;60:2283‐93. [DOI] [PubMed] [Google Scholar]
Entwistle 2013
- Entwistle FM. The Evidence and Rationale for the UNICEF UK Baby Friendly Initiative standards. UNICEF UK, 2013. [Google Scholar]
Fildes 1986
- Fildes V. Breasts, Bottles and Babies a History of Infant Feeding. Edinburgh: Edinburgh University Press, 1986. [Google Scholar]
Ghosh 2006
- Ghosh R, Mascie‐Taylor N, Rosetta L. Longitudinal study of the frequency and duration of breastfeeding in rural Bangladeshi women. American Journal of Human Biology 2006;18:630‐8. [DOI] [PubMed] [Google Scholar]
Gionet 2013
- Gionet L. Statistics Canada, Heath at a Glance. Breastfeeding Trends in Canada. www.statcan.gc.ca/pub/82‐624‐x/2013001/article/11879‐eng.htm (accessed July 2016) 2013.
Graffy 2005
- Graffy J, Taylor J. What information, advice, and support do women want with breastfeeding?. Birth 2005;32(3):179‐86. [DOI] [PubMed] [Google Scholar]
Guo 2013
- Guo S, Fu X, Scherpbier RW, Wang Y, Zhou H, Wang X, et al. Breastfeeding rates in central and western China in 2010: implications for child and population health. Bulletin of the World Health Organization 2013;91:322‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawkins 2014
- Hawkins SS, Stern AD, Baum CF, Gillman MW. Compliance with the baby‐friendly hospital initiative and impact on breastfeeding rates. Archives of Disease in Childhood. Fetal and Neonatal Edition 2014;99:F138‐F145. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hinsliff‐Smith 2014
- Hinsliff‐Smith K, Spencer R, Wash D. Realities, difficulties and outcomes for mothers choosing to breastfeed: Primigravid mothers experiences in the early postpartum period (6‐8 weeks). Midwifery 2014;30:e14‐e19. [DOI] [PubMed] [Google Scholar]
Hoddinott 2012
- Hoddinott P, Craig, LCA, Britten J, McInnes RJ. A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open 2012;2:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Howe‐Hayman 2016
- Howe‐Hayman A, Lutenbacher M. The Baby‐Friendly Hospital Initiative as an Intervention to Improve breastfeeding rates: a review of the literature. Journal of Midwifery & Women's Health 2016;61(1):77‐102. [DOI] [PubMed] [Google Scholar]
Howel 2013
- Howel D, Ball H. Association between length of exclusive breastfeeding and subsequent breastfeeding continuation. Journal of Human Lactation 2013;29:579‐85. [DOI] [PubMed] [Google Scholar]
Häggkvist 2010
- Häggkvist AP, Brantsaester AL, Grjibovski AM, Helsing E, Meltzer HM, Haugen M. Prevalence of breastfeeding in Norwegian Mother and Child Cohort Study and health‐service correlates of cessation of full breastfeeding. Public Health Nutrition 2010;13(12):2076‐86. [DOI] [PubMed] [Google Scholar]
Jonas 2016
- Jonas W, Woodside B. Physiological mechanisms, behavioural and psychological factors influencing the transfer of milk from mothers to their young. Hormones and Behaviour 2016;77:167‐81. [DOI] [PubMed] [Google Scholar]
Kent 2006
- Kent JC, Mitoulas LR, Cregan MD, Ramsay DT, Doherty DA, Hartmann PE. Volume and frequency of breastfeeding and fat content of breast milk throughout the day. Pediatrics 2006;117(3):e387‐e395. [DOI] [PubMed] [Google Scholar]
Kent 2012
- Kent JC, Prime DK, Garbin CP. Principles for maintaining or increasing breast milk production. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN 2012;41(1):114‐21. [DOI] [PubMed] [Google Scholar]
Kent 2015
- Kent JC, Ashton E, Hardwick CM, Rowan MK, Chia ES, Fairclough KA, et al. Nipple pain in breastfeeding mothers: incidence, causes and treatments. International Journal of Environmental Research and Public Health 2015;12:12247‐63. [DOI: 10.3390/ijerph121012247] [DOI] [PMC free article] [PubMed] [Google Scholar]
Klaus 1987
- Klaus MH. The frequency of suckling. A neglected but essential ingredient of breast‐feeding. Obstetrics and Gynecology Clinics of North America 1987;14(3):623‐33. [PubMed] [Google Scholar]
Kramer 2012
- Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD003517.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leonard 2000
- Leonard L. Breastfeeding triplets. The at‐home experience. Public Health Nursing 2000;17(3):211‐21. [DOI] [PubMed] [Google Scholar]
Leurer 2015
- Leurer MD, Misskey E. "Be positive as well as realistic": a qualitative description analysis of information gaps experienced by breastfeeding mothers. International Breastfeeding Journal 2015;10(10):2‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mangesi 2016
- Mangesi L, Zakarija‐Grkovic I. Treatments for breast engorgement during lactation. Cochrane Database of Systematic Reviews 2016, Issue 6. [DOI: 10.1002/14651858.CD006946.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Manz 1999
- Manz F, Van't Hof MA, Haschke F. The mother‐infant relationship: who controls breastfeeding frequency? Euro Growth Study Group. Lancet 1999;353:1152. [DOI] [PubMed] [Google Scholar]
Marshall 2007
- Marshall JL, Godfrey M, Renfrew MJ. Being a ‘good mother’: managing breastfeeding and merging identities. Social Science & Medicine 2007;65(10):2147‐59. [DOI] [PubMed] [Google Scholar]
McAndrew 2012
- McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey 2010. Health and Social Care Information Centre.
McClellan 2012
- McClellan HL, Hepworth AR, Kent JC, Garbin CP, Williams TM, Hartmann PE, et al. Breastfeeding frequency, milk volume, and duration in mother–infant dyads with persistent nipple pain. Breastfeeding Medicine 2012;7(4):275‐81. [DOI] [PubMed] [Google Scholar]
Motee 2013
- Motee A, Ramasawmy D, Pugo‐Gunsam P, Jeewon R. An assessment of the breastfeeding practices and infant feeding pattern among mothers in Mauritius. Journal of Nutrition and Metabolism, Article ID 243852, doi.org/10.1155/2013/243852 2013; Vol. 2013. [DOI] [PMC free article] [PubMed]
Neovita Study Group 2016
- Neovita Study Group. Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. Lancet 2016;4:e266‐e275. [DOI] [PubMed] [Google Scholar]
NICE 2010
- National Institute for Clinical Evidence. Jaundice in newborn babies under 28 days. National Institute for Clinical Evidence London 2010 (Updated 2016).
Nickel 2013
- Nickel NC, Labbok MH, Hudgens MG, Daniels JL. The extent that noncompliance with the ten steps of successful breastfeeding influences breastfeeding. Journal of Human Lactation 2013;29(1):59‐70. [DOI] [PubMed] [Google Scholar]
Oddie 2013
- Oddie SJ, Craven V, Deakin K, Westman J, Scally A. Severe neonatal hypernatraemia: a population based study. Archives of Disease in Childhood. Fetal and Neonatal Edition 2013;98:F384‐F387. [DOI] [PubMed] [Google Scholar]
OECD/WHO 2014
- OECD/WHO. Infant and Young Child Feeding. www.oecd‐ilibrary.org/social‐issues‐migration‐health/health‐at‐a‐glance‐asia‐pacific‐2014/infant‐and‐young‐child‐feeding_health_glance_ap‐2014‐20‐en (accessed July 2016) 2014.
Ogburn 2011
- Ogburn T, Philipp BL, Epsey E, Merewood A, Espindola D. Assessment of breastfeeding information in general obstetrics and gynaecology textbooks. Journal of Human Lactation 2011;27(1):58‐62. [DOI] [PubMed] [Google Scholar]
Parry 2013
- Parry JE, Ip DKM, Chau PYK, Wu KM, Tarrant M. Predictors and consequences of in‐hospital formula supplementation for healthy breastfeeding newborns. Journal of Human Lactation 2013;29(4):527–36. [DOI] [PubMed] [Google Scholar]
Perrine 2012
- Perrine CG, Scanlon KS, Li R, Odom E, Grummer‐Strawn LM. Baby‐Friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics 2012;130(1):54‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pierro 2016
- Pierro J, Abulaimoun B, Roth P, Blau J. Factors associated with supplemental formula feeding of breastfeeding infants during postpartum hospital stay. Breastfeeding Medicine 2016;11:196‐202. [DOI] [PubMed] [Google Scholar]
Prusova 2014
- Prusova K, Tyler A, Churcher L, Lokugamage U. Royal College of Obstetricians and Gynaecologists guidelines: How evidenced‐based are they?. Journal of Obstetrics and Gynaecology 2014;34(8):705‐11. [DOI: 10.3109/01443615.2014.920794] [DOI] [PMC free article] [PubMed] [Google Scholar]
Putthakeo 2009
- Putthakeo P, Ali M, Ito C, Vilayhong P, Kuroiwa C. Factors influencing breastfeeding in children less than 2 years of age in Lao PDR. Journal of Paediatrics and Child Health 2009;45:487‐92. [DOI] [PubMed] [Google Scholar]
Renfrew 2005
- Renfrew M, Dyson L, Wallace L, D'Sousa L, McCormack F, Spiby H. The Effectiveness of Public Health Interventions to Promote the Duration of Breastfeeding: Systematic Review. 1st Edition. London: NICE, 2005. [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schafer 2015
- Schafer R, Genna CW. Physiologic breastfeeding: a contemporary approach to breastfeeding initiation. Journal of Midwifery & Women's Health 2015;60(5):546‐53. [DOI] [PubMed] [Google Scholar]
Shloim 2015
- Shloim N, Hugh‐Jones S, Rudolf MCJ, Feltbower RG, Lans O, Hetherington MM. "It's like giving him a piece of me.": Exploring UK and Israeli women's accounts of motherhood and feeding. Appetite 2015;95:58‐66. [DOI] [PubMed] [Google Scholar]
Skafida 2012
- Skafida V. Juggling work and motherhood: the impact of employment and maternity leave on breastfeeding duration: a survival analysis on Growing Up in Scotland data. Maternal and Child Health Journal 2012;16(2):519‐27. [DOI] [PubMed] [Google Scholar]
Teich 2014
- Teich AS, Barnett J, Bonuck K. Women’s perceptions of breastfeeding barriers in early postpartum period: a qualitative analysis nested in two randomized controlled trials. Breastfeeding Medicine 2014;9(1):9‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tierney 2005
- Tierney JF, Stewart LA. Investigating patient exclusion bias in meta‐analysis. International Journal of Epidemiology 2005;34:79‐87. [DOI] [PubMed] [Google Scholar]
Tin 2014
- Tin W. Defining neonatal hypoglycaemia: a continuing debate. Seminars in Fetal & Neonatal Medicine 2014;19:27‐32. [DOI] [PubMed] [Google Scholar]
Victoria 2016
- Victoria CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms and lifelong effect. Lancet 2016;387:475‐90. [DOI] [PubMed] [Google Scholar]
Watt 2013
- Watt J, Mead J. What paediatricians need to know about breastfeeding. Paediatrics and Child Health 2013;23(8):362‐6. [Google Scholar]
WHO 1998
- World Health Organization. Evidence for the Ten Steps to Successful Breastfeeding. Geneva: World Health Organization, 1998. [Google Scholar]
WHO 2001
- WHO. The Optimal Duration of Exclusive Breastfeeding. Report of an Expert Consultation. World Health Organization 2001.
WHO 2002
- WHO. Global Strategy on Infant and Young Child Feeding. WHO 2002. [PubMed]
WHO 2008
- World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices. Part 1, Definitions. Geneva: World Health Organization, 2008. [Google Scholar]
WHO 2009
- World Health Organization and United Nations Children’s Fund. Baby Friendly Hospital Initiative Revised, Updated and Expanded for Integrated Care. Geneva: World Health Organization, 2009. [PubMed] [Google Scholar]
WHO 2014
- WHO UNICEF. Global Nutrition Targets 2025. Breastfeeding Policy Brief. www.who.int/nutrition/publications/globaltargets2025_policybrief_breastfeeding/en/ (accessed July 2016) 2014.
Woolridge 2008
- Woolridge MW, Ingram JC. ‘‘Rigid’’ versus ‘‘baby‐led’’—no contest. Archives of Disease in Childhood 2008;93(4):353. [PubMed] [Google Scholar]
Wright 2011
- Wright JD, Pawar N, Gonzalez JSR, Lewin SN, Burke WM, Simpson LL, et al. Scientific evidence underlying the American College of Obstetricians and Gynecologists’ Practice Bulletins. Obstetrics & Gynecology 2011;118(3):505‐12. [DOI] [PubMed] [Google Scholar]
Yotebieng 2015
- Yotebieng M, Labbok M, Soeters HM, Chalachala JL, Lapika B, Vitta BS, et al. Ten Steps to Successful Breastfeeding programme to promote early initiation and exclusive breastfeeding in DR Congo: a cluster‐randomised controlled trial. Lancet 2015;3(9):e546‐e555. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Fallon 2014
- Fallon A, Putten D, Dring C, Moylett EH, Fealy G, Devane D. Baby‐led compared with scheduled (or mixed) breastfeeding for successful breastfeeding. Cochrane Database of Systematic Reviews 2014, Issue 7. [DOI: 10.1002/14651858.CD009067.pub2] [DOI] [PubMed] [Google Scholar]


