Abstract
Background
Ovarian cancer is the sixth most common cancer and seventh commonest cause of death in women worldwide. Traditionally, many people who have been treated for cancer undergo long‐term follow‐up in secondary care. However, it has been suggested that the use of routine review may not be effective in improving survival, quality of life (QoL), or relieving anxiety, or both. In addition, traditional follow‐up may not be cost‐effective.
Objectives
To compare the potential benefits of different strategies of follow‐up in patients with epithelial ovarian cancer following completion of primary treatment.
Search methods
For this update we searched the Cochrane Gynaecological Cancer Group Trials Register, the Cochrane Central Register of Controlled Trials (CENTRAL) Issue 7, 2013, MEDLINE and EMBASE from November 2010 to July 2013. We also searched reference lists of review articles and contacted experts in the field.
Selection criteria
All relevant randomised controlled trials (RCTs) that evaluated follow‐up strategies for women with epithelial ovarian cancer following completion of primary treatment.
Data collection and analysis
Two review authors independently abstracted data and assessed risk of bias.
Main results
The authors did not identify any new studies that were eligible for inclusion in this update of the review. The search for the original review identified only one RCT that met the inclusion criteria, which included 529 women. This study reported data on immediate treatment of ovarian cancer relapse following rise of serum CA125 levels versus delaying treatment until symptoms developed. All the women participating had previous confirmation of remission, with normal CA125 concentration and no radiological evidence of disease, after surgery and first‐line chemotherapy for ovarian cancer.
Overall survival between the immediate and delayed arms showed no difference after a median follow‐up of 56.9 months (unadjusted hazard ratio (HR) 0.98, 95% confidence interval (CI) 0.80 to 1.20; P value 0.85). Time from randomisation to first deterioration in global health score or death was shorter in the immediate treatment group than in the delayed treatment group (HR 0.71, 95% CI 0.58 to 0.88; P value < 0.01). The trial was at low risk of bias.
Authors' conclusions
Limited evidence from a single trial suggests that routine surveillance with CA125 in asymptomatic patients and treatment at CA125 relapse does not seem to offer survival advantage when compared to treatment at symptomatic relapse. RCTs are needed to compare different types of follow‐up, looking at survival, QoL, cost and psychological effects as outcomes.
Plain language summary
Evaluation of follow‐up strategies for patients with epithelial ovarian cancer following completion of primary treatment
Ovarian cancer is the sixth most common cancer and seventh commonest cause of cancer death in women worldwide. Traditionally, many people who have been treated for cancer undergo long‐term follow‐up in a hospital outpatient setting. However, it has been suggested that the use of routine review (check‐ups) may not result in women with ovarian cancer living longer. We set out to review the evidence for different types of follow‐up for women who have completed treatment for the commonest type of ovarian cancer. Only one randomised study was found, and it did not find that immediate treatment with chemotherapy for relapse (identified by a tumour marker ‐ CA125 ‐ blood test) produced a benefit compared to delaying treatment until the women developed symptoms. The limited evidence suggests that there may be no benefit from early detection of recurrence of ovarian cancer and starting chemotherapy before symptoms develop. In addition, early treatment of recurrence with chemotherapy may reduce overall quality of life.
Randomised controlled trials are needed to compare different types of follow‐up, looking at survival and quality of life outcomes. If new treatments become available for relapsed ovarian cancer, the methods of follow‐up may need to be re‐assessed to see if earlier intervention improves survival.
Background
Description of the condition
Ovarian cancer is the sixth most common cancer among women (GLOBOCAN 2008). Worldwide there are more than 200,000 new cases of ovarian cancer each year, accounting for around 4% of all cancers diagnosed in women. A woman's risk of developing cancer of the ovaries by the age of 75 varies between countries, and ranges from 0.5% to 1.6% (IARC 2002). This corresponds to an age‐standardised rate of ovarian cancer of between 5 to 14 cases per 100,000 women under 75 years of age per year. In Europe, 37% to 41% of women with ovarian cancer are alive five years after diagnosis (EUROCARE 2003). The poor survival associated with ovarian cancer is largely because most women are diagnosed when the cancer is at an advanced stage (Jemal 2008).
Description of the intervention
Traditionally, many people who have been treated for cancer undergo long‐term, even life‐long, follow‐up in secondary care (Barnhill 1992; Kerr‐Wilson 1995; Kew 2006). The rationale for this is that, if a recurrence of cancer is picked up early, i.e. before the onset of symptoms, it is more likely to be amenable to treatment and therefore survival rates will be improved (Kunkler 1991). Furthermore, it is proposed that this routine review provides other opportunities, including management of symptoms ‐ either from the disease itself or from side‐effects of treatment ‐ and access to supportive and palliative care. Patients may also be provided with reassurance that the cancer has not returned, which maintains their psychological well‐being, and these appointments also allow for the collection of outcome data and provide positive feedback for the clinicians involved in patients' care (Kerr‐Wilson 1995).
It has been suggested that the use of routine review may not be effective in achieving the aims listed above. Detection of recurrence may even be delayed as some women will not present with symptoms until their next routine appointment (Olaitan 2001). Evidence from endometrial, cervical and vulval cancers has called into question the benefit of detecting recurrence at an asymptomatic stage (Kew 2005), as, in most cases, detection of recurrent disease at an asymptomatic stage did not appear to confer any survival benefit. However, it would appear that studies investigating gynaecological cancers are hampered by retrospective design and poor methodological quality (Kew 2005). A meta‐analysis of randomised controlled trials (RCTs) of follow‐up after bowel cancer has suggested that intensive follow‐up provides a benefit that is not conferred by little or no follow‐up. The effect was most pronounced in trials that used computed tomography (CT) and frequent measurements of serum carcinoembryonic antigen (CEA) (Renehan 2002). There was an absolute reduction in all‐cause five‐year mortality of 10%. However, salvage surgery offered a second chance of cure in a small number of cases (2% to 5%), and the additional gain in survival might have been attributable to other factors. These factors included increased psychological well‐being, or altered lifestyle, or improved treatment of coincidental disease through regular medical contact, or a combination of all three, which may have contributed to the improved survival (Renehan 2005).
How the intervention might work
Qualitative work in gynaecological cancer on women who have been treated for early stage disease, including those who have been treated for ovarian cancer, has shown that the over‐riding reason that women want continued follow‐up is fear of recurrence. In one survey 82% of women attributed their lack of cancer recurrence to close medical follow‐up (Stewart 2001). Women find routine visits to the hospital reassuring, especially if they are experiencing unexpected symptoms (Bradley 2000). However, for some, feelings of anxiety and apprehension are severe (Stewart 2001), and may actually deter them from attending (Bradley 2000). A study suggested that living with the risk of cancer recurrence is a life‐long social and psychological challenge, affecting women and their families, with the women’s approaches to managing that risk affecting their perception of the future (Roberts 2009).
The use of other follow‐up strategies, such as the use of nurse‐led follow‐up (in lung cancer) (Moore 2002), or primary care follow‐up (in breast cancer) (Grunfeld 1996), have been shown to be as effective as the traditional secondary care model. However, their impact on quality of life (QoL) issues has not been assessed.
Why it is important to do this review
The objectives of follow‐up for epithelial ovarian cancer include psychological support, treatment of symptoms due to side effects of treatment, and audit, as well as treatment of recurrence of the cancer. Treatment of recurrent ovarian cancer represents a challenge, with poor long‐term prognosis. Whilst there is no curative salvage treatment for recurrent ovarian disease in those who previously responded to platinum‐based chemotherapy, surgery with or without chemotherapy may offer an opportunity to produce significant periods of disease remission after recurrence in some women (Bristow 2009). The follow‐up of asymptomatic women generally includes consideration of the complete clinical history, taking a serum CA125 sample, making a physical examination, and may also include imaging, such as a CT scan, although this is usually performed when symptoms or signs appear.
It is difficult to extrapolate management of other malignancies to ovarian cancer, since it has a different natural history to both non‐gynaecological cancer and other gynaecological cancers. The use of CA125 for early detection of recurrence is widespread (Barnhill 1992; Kew 2006), but the impact of this on the timing of chemotherapy has yet to be determined (Goonewardene 2007: Vaidya 2003). This is an update, which previously identified one RCT (Rustin 2010). This review set out to evaluate systematically the evidence available for the role of follow‐up after the primary treatment of ovarian cancer, and the optimal use of investigations.
Objectives
To compare the potential benefits of different strategies of follow‐up in patients with epithelial ovarian cancer following completion of primary treatment.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs)
Types of participants
Women of any age diagnosed with primary ovarian cancer of epithelial histological sub‐type who have completed primary treatment.
Types of interventions
We considered any of the following comparisons:
medical follow‐up using various interventions including symptomatology, physical examination, serum tumour markers and radiological investigations;
nurse‐led follow‐up;
primary care follow‐up;
patient‐directed follow‐up.
Types of outcome measures
Primary outcomes
Overall survival: survival until death from all causes (survival from the time when women were randomised).
Secondary outcomes
Health‐related quality of life (QoL), measured using a scale that has been validated through reporting of norms in a peer‐reviewed publication.
Psychological effects, measured using a scale that has been validated through reporting of norms in a peer‐reviewed publication.
Cost‐effectiveness.
Search methods for identification of studies
We sought papers in all languages and performed translations when necessary.
Electronic searches
See: Cochrane Gynaecological Cancer Group methods used in reviews. For this update we searched the following electronic databases:
the Cochrane Gynaecological Cancer Review Group's Trial Register;
the Cochrane Central Register of Controlled Trials (CENTRAL Issue 7, 2013);
MEDLINE (November 2010 to July week 4 2013);
EMBASE (November 2010 to 2013).
The search strategy from our original Cochrane review, that aimed to identify RCTs that compared follow‐up strategies in women with epithelial ovarian cancer, was adopted for MEDLINE, EMBASE and CENTRAL and used to search from November 2010 onwards. These strategies are presented in Appendix 1, Appendix 2 and Appendix 3, respectively.
Databases were searched up to July 2013.
Searching other resources
The authors checked the reference lists of articles and other reviews on the subject in order to retrieve further information about published or unpublished trials, and contacted researchers involved in this area.
Data collection and analysis
Selection of studies
All titles and abstracts retrieved by electronic searching were downloaded to a reference management database (Endnote), duplicates were removed and the remaining references were examined by two review authors independently. The authors excluded those studies that clearly did not meet the inclusion criteria. Full text copies of potentially relevant studies were obtained for independent assessment of eligibility by both review authors.
Data extraction and management
A review author extracted data from the only eligible trial identified onto a pre‐designed data extraction form. Data extracted included:
author, year of publication and journal citation (including language);
country;
setting;
inclusion and exclusion criteria;
study design, methodology;
participant characteristics (age, stage and postoperative residuum of malignancy);
numbers of participants in each arm of the trial;
type of intervention and control (follow‐up by different professional groups, use of investigations, timing of follow‐up visits and decision to give further treatment);
data relating to risk of bias in trial ‐ see below;
duration of follow‐up;
-
outcomes – overall survival, health‐related QoL:
for each outcome: outcome definition (with diagnostic criteria if relevant);
unit of measurement (if relevant);
for scales: upper and lower limits, and whether high or low score is good;
results: number of participants allocated to each intervention group;
for each outcome of interest: sample size; missing participants.
For time‐to‐event data (e.g. overall survival), we extracted the log of the hazard ratio (log(HR)) and its standard error from trial reports; if these were not reported, we attempted to estimate them from other reported statistics using the methods of Parmar 1998.
We extracted both unadjusted and adjusted statistics, where reported.
Where possible, we extracted all data concerning intention‐to‐treat analysis, in which participants were analysed in groups to which they were assigned.
We noted the time points at which outcomes were collected and reported.
Assessment of risk of bias in included studies
The risk of bias in the included RCT was assessed using the Cochrane Collaboration's tool for assessment of risk of bias and the criteria specified in Chapter 8 of the Cochrane Handbook 2011. This included assessment of:
sequence generation;
allocation concealment;
blinding (of participants, healthcare providers and outcome assessors);
-
incomplete outcome data:
we recorded the proportion of participants whose outcomes were not reported at the end of the study; we noted if loss to follow‐up was not reported.
-
we coded whether the level of loss to follow‐up for each outcome was satisfactory as follows:
'yes', if fewer than 20% of patients were lost to follow‐up and reasons for loss to follow‐up were similar in both treatment arms;
'no', if more than 20% of patients were lost to follow‐up or reasons for loss to follow‐up differed between treatment arms;
'unclear' if loss to follow‐up was not reported.
selective reporting of outcomes;
other possible sources of bias.
The 'Risk of bias' tool was applied independently by two review authors (AB, KG), who resolved differences through discussion. Results are presented in a 'Risk of bias' graph.
Measures of treatment effect
For time‐to‐event outcomes, we used the HR.
Dealing with missing data
We did not impute missing outcome data.
Data synthesis
We only identified one included study so it was not possible to perform a meta‐analysis. Therefore it was not appropriate to assess heterogeneity between results of trials and we were unable to assess reporting biases using funnel plots or conduct any subgroup analyses or sensitivity analyses.
Results
Description of studies
Results of the search
The updated search strategy identified 532 unique references. The authors read the titles and abstracts of these and excluded articles that obviously did not meet the inclusion criteria at this stage. The authors retrieved 13 articles in full, translated articles into English where appropriate, and identified updated versions of relevant studies. The full text screening of these 13 references led to an empty search since no studies met the inclusion criteria, for the reasons described in Characteristics of excluded studies. Only one completed RCT, that had been previously identified in the original Cochrane review (Kew 2011), met our inclusion criteria and is described in Characteristics of included studies.
Included studies
This update of the review did not identify any new RCTs. Only one prospective study met the inclusion criteria (Rustin 2010). This was a randomised controlled, multi‐centre trial in ovarian cancer of immediate treatment of disease relapse based on CA125 level alone versus delayed treatment based on conventional clinical indicators (MRC OV05/EORTC 55955 trials). The trial registered 1442 participants: 529 of these women showed an increase in CA125 level and were then randomly assigned to treatment groups and included in the analysis, with all 529 assessed at the end of the trial (265 in the immediate treatment group and 264 in the delayed treatment group). At the start of the trial all the women had confirmation of remission, with normal CA125 concentration and no radiological evidence of disease after surgery and first‐line chemotherapy. The primary outcome measure was overall survival, calculated from the date of randomisation to the date of the last follow‐up or death from any cause.
Women assigned to immediate treatment started chemotherapy 4.8 months earlier (95% confidence interval (CI) 3.6 to 5.3 months) than those allocated to delayed treatment. The median length of follow‐up was 56.9 months (interquartile range (IQR) 37.4 to 81.8 months from randomisation), and there were a total of 370 deaths in the trial (186 in the immediate treatment group and 184 in the delayed treatment group). Median age at registration was 61 years (range: 53 to 68); 81% were FIGO stage III/IV. Second‐line chemotherapy started a median of five months earlier in the immediate treatment arm. Chemotherapy treatment was given according to local institutional protocols. Predominant histologies were serous and endometrioid, involving 53% and 17%, respectively, among the randomised participants. Median follow‐up from randomisation was 49 months.
Median survival from randomisation was 25.7 months (95% CI 23.0 to 27.9) for women on immediate treatment and 27.1 months (95% CI 22.8 to 30.9) for those on delayed treatment, with a median follow‐up of 56.9 months (IQR 37.4 to 81.8) from randomisation and 370 deaths (186 immediate treatment, 184 delayed treatment).
Median time spent with good global health score was 7.2 months (95% CI 5.3 to 9.3) for women assigned to immediate treatment and 9.2 months (95% CI 6.4 to 10.5) for those assigned to delayed treatment.
The trial reported overall survival as the primary outcome measure and provided unadjusted and several adjusted estimates of the HR. The trialists used the following stratification factors to adjust the HR for overall survival; age; International Federation of Gynecology and Obstetrics stage; first‐line chemotherapy; time from completion of first‐line chemotherapy to doubling of CA125 concentration; and country. A second adjusted HR used the following prognostic factors: histology; World Health Organization (WHO) performance status; and time from doubling of CA125 concentration to randomisation. The trialists also reported a HR adjusted for both stratification and prognostic factors. A sensitivity analysis of non‐curtailed data (all follow‐up data received, not curtailed at five years for MRC OV05 and three years for EORTC 55955) was also performed for overall survival.
The trial also reported time to second‐line chemotherapy (calculated from the date of randomisation to the date of initiation of second‐line chemotherapy, with women who did not receive second‐line chemotherapy censored at the date of last contact), and time to third‐line treatment or death, but these outcomes were not of interest to this review.
Health‐related QoL was reported by calculating time to first deterioration in QoL score or death using the EORTC QLQ‐C30 questionnaire.
The trialists had also performed subgroup analyses of individual components of the QLQ‐C30 sub‐scales, and reported the following functional QoL components: physical; role; emotional; cognitive; and social. Some of these were then sub‐divided into symptom QoL components. There were inconsistencies in HRs and their 95% CIs for most components in Table 4 (in the paper) and the reported significance probabilities, and it was not clear what adjustment(s) had been made on the estimates.
Excluded studies
Thirteen references were excluded after obtaining the full text for the following reasons:
not an RCT (Bapsy 2012; Geurts 2011; Hall 2011; Kitajima 2012; Lajtman 2011; Madry 2011; Pastalozzi 2011; Pignata 2011; Rustin 2011; van de Poll‐Franse 2011);
retrospective study (Fuso 2011);
primary or secondary outcomes not assessed (Alexandre 2012);
incorrect participants (Buys 2012).
For further details of all the excluded studies see Characteristics of excluded studies.
Risk of bias in included studies
The one included trial was at low risk of bias as it satisfied four criteria used to assess risk of bias (Rustin 2010; see Figure 1).
1.
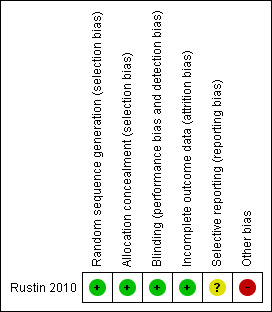
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
The trial reported the method of generation of the sequence of random numbers used to allocate women to treatment arms and concealed this allocation sequence from participants and healthcare professionals involved in the trial. All women had CA125 levels monitored and those whose CA125 levels rose to more than two times the upper limit of normal were randomised to one of two treatment arms. Participants and clinicians were blinded to monitored CA125 levels. Clinicians of women randomised to the immediate treatment arm were informed that CA125 levels had risen, a confirmatory test was performed and women were treated according to local protocols. Clinicians and women in the delayed treatment group remained unaware of the monitoring CA125 levels; if symptoms developed, CA125 was performed locally to monitor response to treatment and women were treated according to standard local practice. All women who were randomised were analysed, but it was unclear whether outcomes had been selectively reported. Point estimates and 95% confidence intervals did not tally with corresponding P values for time to first deterioration in quality of life score or death for many of the individual sub‐scales of the EORTC QLQ‐C30 questionnaire (Table 4, Rustin 2010), so we scored the 'free of other bias' item in the 'Risk of bias' assessment as being at high risk of bias.
Effects of interventions
Immediate versus delayed treatment in patients with increased CA125 levels
We found one study, which included 529 women, that met our inclusion criteria (Rustin 2010). This study reported data on immediate versus delayed treatment in women who had confirmation of remission (defined as normal CA125 concentration and no radiological evidence of disease) after surgery and first‐line chemotherapy.
Overall survival
(Analysis 1.1 ‐ unadjusted estimate)
1.1. Analysis.
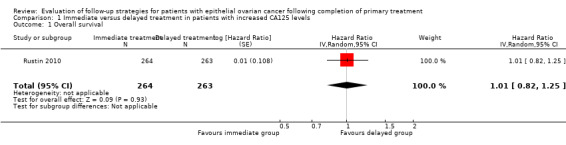
Comparison 1 Immediate versus delayed treatment in patients with increased CA125 levels, Outcome 1 Overall survival.
There was no statistically significant difference in the risk of death between women who received immediate treatment and those who received delayed treatment (unadjusted HR 0.98; 95% CI 0.80 to 1.20; P value 0.85). The unadjusted estimate was robust to estimates that were adjusted for stratification factors (age, International Federation of Gynecology and Obstetrics stage, first‐line chemotherapy, time from completion of first‐line chemotherapy to doubling of CA125 concentration, and country: HR 0.99; 95% CI 0.80 to 1.22), prognostic factors (histology, WHO performance status, and time from doubling of CA125 concentration to randomisation: HR 0.98; 95% CI 0.79 to 1.21) and the adjustment of both stratification and prognostic factors (HR 1.01; 95% CI 0.82 to 1.25). The trial authors also carried out a sensitivity analysis of non‐curtailed data (all follow‐up data received, not curtailed at five years for MRC OV05 and three years for EORTC 55955: HR 1.01; 95% CI 0.82 to 1.23).
Quality of life
Time to first deterioration in quality of life score or death using EORTC QLQ‐C30 questionnaire
Time from randomisation to first deterioration in global health score or death was shorter in the immediate group (median 3.2 months; 95% CI 2.4 to 4.3) than in the delayed group (5.8 months; 95% CI 4.4 to 8.5; HR 0.71; 95% CI 0.58 to 0.88; P value 0.002). The trial authors claimed that subgroup analyses of individual components of the QLQ‐C30 sub‐scales showed deterioration in score sooner in the immediate group than in the delayed group for almost all sub‐scales, and there was evidence of significant disadvantages for role, emotional, social, and fatigue sub‐scales with immediate treatment. However this was not consistent with the 95% confidence intervals stated in Table 4 in the trial report, and it was not clear what adjustment(s) had been made on the estimates.
The trial report also mentioned that since the QLQ‐C30 questionnaire asks only about symptoms in the previous week, and the forms were completed just before each course of chemotherapy, this method could underestimate any reduction in quality of life due to chemotherapy.
Discussion
Summary of main results
The authors did not identify any new randomised controlled trials (RCTs) that could be included in this update of the review. Only one previously identified randomised controlled trial (RCT), which included 529 women, met our inclusion criteria (Rustin 2010). This trial reported data on immediate treatment of recurrence versus delayed treatment in women who at the time of recruitment to the trial had confirmation of remission with normal CA125 concentration and no radiological evidence of disease after surgery and first‐line chemotherapy. It showed that overall, there may be no survival advantage from immediate treatment following a raised serum marker level alone. There was a total of 370 deaths in the trial, and there was no evidence of a difference in overall survival between the immediate and delayed arms. Therefore, there may be no value in the routine measurement of CA125 in the follow‐up of women with ovarian cancer who have a clinical complete remission following primary surgery and first‐line platinum‐based chemotherapy.
Women treated in the immediate treatment arm (treated on the basis of a CA125 rise alone) received 12 more total cycles of chemotherapy on average than women in the delayed treatment arm (30 months versus 18 months). Immediate treatment appeared to have a negative impact on quality of life (QoL). The decrease in QoL observed in the trial may have been attributable to additional cycles of chemotherapy resulting in additional toxicity (e.g. neuropathy (nerve damage), fatigue or hospital admissions secondary to neutropenia (a blood disorder)), and more time spent in hospital as an outpatient or inpatient. These data suggest that treatment may be safely delayed until there is evidence of clinical relapse.
There is a paucity of good quality data in this important area. We did not expect to identify a large number of RCTs, but the review was restricted to high quality evidence as retrospective case series are of inadequate quality and are at high risk of bias. The main limitation of this review is the fact that conclusions are based on single trial analyses.
Overall completeness and applicability of evidence
To date one RCT has compared immediate treatment of relapse, based on CA125 level alone, versus delayed treatment, based on conventional clinical indicators.
Overall, the quality of the evidence was moderate (GRADE Working Group); although the review comprised evidence from only one included trial, this trial was of a sufficient size. Outcomes were incompletely reported as separate comprehensive reporting of QoL and psychological effects was not carried out and cost‐effectiveness was not assessed. Even though the trial was judged to have been at low risk of bias (Rustin 2010), the fact that there were no accompanying trials to support the evidence resulted in a downgrading of the evidence to reflect the uncertainty in the single trial analyses.
Quality of the evidence
The single included trial included a reasonably large number of women (529 participants) and was at low risk of bias, largely because it was a well conducted and reported trial. Outcomes were analysed using appropriate statistical techniques and a hazard ratio was used for time‐to‐event data, which is the best statistic for summarising the difference in risk in two treatment groups over the duration of a trial, when there is 'censoring', that is, when the time to death is unknown for some women as they were still alive at the end of the trial. The trial also performed sensitivity analyses to adjust for important stratification and prognostic factors to test the robustness of unadjusted estimates. However, the confidence intervals and significance probabilities in subgroup analyses of individual components of the QLQ‐C30 sub‐scales were not consistent, and it was unclear whether these factors were statistically significant or not. This does not change the overall judgement regarding the quality of the evidence greatly, since the quality of the trial appears to be good, but the amount of evidence available does not allow robust conclusions to be reached in comparison of different follow‐up strategies.
Potential biases in the review process
A comprehensive search was performed, and all studies were sifted and data extracted by at least two reviewers independently. The review was restricted to RCTs, as these provide the strongest level of evidence available. Hence we made every attempt to minimise bias in the review process.
The greatest threat to the validity of the review is likely to be the possibility of publication bias, that is studies that did not find the intervention to have been effective may not have been published. We were unable to assess this possibility as no new studies were identified.
Agreements and disagreements with other studies or reviews
One previous review, which pre‐dates our only included study, suggested that there is uncertainty about whether the early detection of recurrence is beneficial in terms of survival, and that review did not demonstrate a clinical advantage of an intensive follow‐up programme (Gaducci 2007). The authors concluded that the definition of specific guidelines for the surveillance of patients with this malignancy was still controversial. Moreover, retrospective analyses assessing the value of postoperative surveillance programmes have some potential bias (lead time, length time bias).
Apart from Rustin 2010, all other studies on follow‐up strategies use the detection of recurrence as the primary endpoint. This is problematic, since the data from Rustin 2010 demonstrate that time to detection of recurrence is not an adequate surrogate marker for overall survival and may have an adverse effect on the patient. The two may diverge depending on treatments available at relapse. Furthermore detection of recurrence without subsequent information about survival risks the introduction of lead‐time bias. In other words, tests that detect recurrence earlier may simply increase the length of time that the recurrence is known about, rather than making any difference to the overall time period from diagnosis to death. There is also the concern of length time bias, whereby more indolent (slow growing) tumours have a longer pre‐clinical course and are therefore more likely to be detected by periodic tests. Women with more indolent tumours are likely to have better survival rates.
Whilst recognising that detection of recurrence is not an endpoint of this review, there are vast numbers of sources that have investigated follow‐up strategies after treatment for epithelial ovarian cancer, which does permit consideration of these strategies for future studies
Authoritative guidelines
We identified three sets of national/international guidelines.
National Institute for Health (USA, 1994) Trimble 1994
This guideline, formed at a consensus meeting, acknowledged that the ideal follow‐up after ovarian cancer was unclear at that time. However the contributors recommended three‐ or four‐monthly follow‐up for the first two years after completion of primary therapy, with frequency reducing after this time. The guideline recommended that each visit should include the complete history, physical examination ‐ including rectal and vaginal examination ‐ and CA125 measurement; it also recommended that radiological investigations should be individualised.
European Society of Medical Oncology (Europe, 2008 Annals of Oncology)
This guideline recommends follow‐up every three months for two years, every four months during the third year, and every six months during years four and five or until progression is documented (Aebi 2008). Each visit should include history and physical examination including pelvic examination. The guideline recommends that CA125 should be performed at each follow‐up visit, and that a CT scan should be performed if there is clinical or CA125 evidence for progressive disease.
No evidence is provided to support any of these recommendations, other than that CA125 can accurately predict tumour recurrence.
ACR Appropriateness Criteria 2007
This guideline provided no recommendations for follow‐up (Javitt 2007).
Early detection of recurrence
See table in Appendix 4.
Physical examination
Physical examination alone is a poor tool for detecting recurrence and has a sensitivity of only 39.4% (Menczer 2006). Chan reported on a sample of 80 women with recurrent ovarian cancer; all women who had abnormal findings on examination (51%) had either suspicious symptoms or a raised CA125, or both (Chan 2008).
CA125
CA125 can accurately predict recurrence of disease (Kaesemann 1986; Tuxen 2002; Vinokurov 1992). A doubling of the CA125 level is significant. A rise of CA125 occurs one to nine months before clinical and radiological relapse (Bruzzone 1990; Crombach 1985; Hising 1991; Kaesemann 1986; Palmer 2006; Parker 2006; Rustin 1996a; Tuxen 2002). However a recently reported randomised study of 529 women who had completed first line platinum‐based chemotherapy showed no survival advantage from immediate treatment at the time of CA125 relapse, when compared with treatment at symptomatic relapse (Rustin 2010). Second‐line chemotherapy was given, on average, five months earlier in the immediate treatment arm. Furthermore, knowledge of the CA125 result has been shown to be associated with depression and anxiety (Parker 2006). Some anxiety can be reduced by having the CA125 result available at the clinic visit, rather than waiting until the clinic to take the blood and then receiving the result at a later stage (Palmer 2006).
Other tumour markers
A number of other tumour markers have been investigated, either alone or in combination with CA125, in order to improve detection of recurrence, but none has provided evidence of benefit in terms of survival if recurrence is detected earlier.
Investigations ofcarcinogenic embryonic antigen (CEA) have been reported in several papers. This marker is raised in 65% of women with ovarian cancer (Khoo 1979), and it is more likely to be raised in mucinous tumours, so may be of use in women with these tumours when the CA125 level is normal at diagnosis (Lenehan 1986).
Imaging
A number of papers have looked at different methods of imaging to try to detect recurrence.
Ultrasound has been shown to be more sensitive than clinical examination alone in detecting recurrence and has an overall accuracy of 98% when compared to findings with laparotomy (Khan 1986). In women with no clinical or biochemical signs of relapse, ultrasound has been shown to have a positive predictive value of 100% with only one false negative (i.e. cancer present, but not identified as being present) out of 275 cases (Testa 2005). However use of a combination of CA125 level and clinical examination can identify 98% of recurrences (Fehm 2005). CT or, where that is inconclusive, magnetic resonance imaging (MRI) are more useful than ultrasound for proving macroscopic disease recurrence (Prayer 1993; Testa 2005). Ultrasound may have a role in the detection of extraperitoneal lesions (Okai 1992).
Women in whom recurrence is suspected on the basis of CA125 level and clinical review require imaging to plan treatment (Fehm 2005). CT or MRI remain the imaging of choice. Both have good sensitivity and specificity for the detection of recurrence (Gritzmann 1986; Kubik 2000; Low 1999).There is no role for additional CT of the chest (Sella 2001), over and above CT of the abdomen and pelvis, unless there are respiratory symptoms (Dachman 2001). The role of RIS/PET and PET CT has yet to be fully established. In one report PET seemed to have no benefit when compared to MRI or CT (Kubik 2000). However initial data in small series would seem to suggest that its role is likely to be in the diagnosis of recurrence where initial CT or MRI has been inconclusive (Barzen 1990; García 2003; Grabiec 2006; Hauth 2005; Kim 2007; Mangili 2007; Nakamoto 2001; Thrall 2007; Torizuka 2002; Zhu 2002; Zimny 2001). It may also have an additional role in determining the mode of treatment for the recurrence, in particular the place of surgery and prediction of resectability (whether the tumour can be removed) (Kitajima 2008; Lenhard 2008). However, it is probably inferior to CA125 level for evaluating prognosis in women during follow‐up. In the case of central pelvic masses there may be a role for transvaginal colour Doppler ultrasound in discriminating between malignant and non‐malignant causes (Testa 2002).
Peritoneal cytology
One large series of 577 aspirations of the Pouch of Douglas in 110 women during follow‐up after ovarian cancer showed a sensitivity of 60% (Engblom 1995). It was the first or only indication of recurrence in nine patients (33%). Accuracy of the technique is not improved by performing the technique under ultrasound guidance (VillaSanta 1980; Vuento 2007).
In another series of 31 women, a reservoir was implanted in the peritoneal cavity at the time of debulking surgery and used for monitoring (Sugiyama 1996). Six patients had positive cytology as the only sign of recurrence. Sensitivity and specificity were not reported.
Other methods
One small case series looked at gynaegnost (lactate dehydrogenase (LDH) on vaginal tampons), but did not draw any significant conclusions (Cerejeira 1989).
Laparoscopy
Von Georgi found no benefit from early detection of recurrence. Laparoscopy reduces the false negative rate in comparison to CA125 (Shinozuka 1994), but requires an invasive procedure without evidence of additional benefit.
Authors' conclusions
Implications for practice.
The evidence in this review comes from a single, large trial. This trial provided no evidence that routine surveillance of CA125 levels in asymptomatic patients, thus permitting immediate treatment at relapse, offers any survival advantage when compared to delaying treatment until symptomatic relapse.
In the absence of symptoms and with a normal CA125 result, clinical examination is not mandatory.
The additional surveillance of other tumour markers does not offer significant advantage in terms of detecting recurrence when compared with CA125 alone. Routine radiological examination has not shown to be of benefit in asymptomatic women.
Immediate treatment with chemotherapy appears to have a negative impact on quality of life; this maybe attributable to additional cycles of chemotherapy resulting in additional toxicity.
Implications for research.
Current routine cancer follow‐up strategies are costly and need to be justified in order to derive maximal benefit from the available healthcare resources. Further research into follow‐up strategies is needed; this should be directed towards quality of life (QoL) issues and psychological impact, in addition to investigating survival outcomes and cost‐effectiveness.
The one study identified in this review concentrated on women, most of whom had already been treated with chemotherapy at time of relapse. Prospective trials on follow‐up methods should also evaluate whether second‐line debulking surgery is beneficial in women treated with surgery for recurrent ovarian cancer, since the effect of timing of surgical treatment on survival and QoL issues may be different to chemotherapy‐only regimens.
Prospective trials are needed to evaluate interventions during follow‐up that may help to reduce anxiety and promote return to normal functioning for asymptomatic women.
Interventions may include a move away from traditional models of hospital‐based routine follow‐up towards other strategies, such as nurse‐led, telephone and patient‐initiated follow‐up and the relative merits of these strategies should also be evaluated in prospective studies. Individual patient needs and patient choice require further investigation, as part of a long‐term survivorship assessment. However, alterations in practice would need prospective evaluation.
What's new
| Date | Event | Description |
|---|---|---|
| 12 September 2018 | Amended | Eleven references added to 'Classification pending' after a horizon scanning literature search in August 2018. |
History
Protocol first published: Issue 3, 2006 Review first published: Issue 6, 2011
| Date | Event | Description |
|---|---|---|
| 1 September 2014 | New citation required but conclusions have not changed | Text amended, author list updated |
| 31 July 2013 | New search has been performed | No new studies were identified during this update |
Acknowledgements
Fiona Kew was the lead author of the original review published in 2011.
We thank Jo Morrison for clinical and editorial advice, Jane Hayes for designing the search strategy and Gail Quinn and Clare Jess for their contribution to the editorial process. Special thanks to Karen Roberts for her contribution to the Implications for research section.
Najindra Das and Katherine Deane for assisting with the development of the protocol.
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Gynaecological Cancer Group.
The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health
Appendices
Appendix 1. MEDLINE search strategy
exp Ovarian Neoplasms/
(ovar* adj5 (cancer* or tumor* or tumour* or neoplas* or malignan* or carcinoma*)).mp.
1 or 2
Follow‐Up Studies/
(follow up or follow‐up).mp.
surveillance.mp.
Aftercare/
(aftercare or after care or after‐care).mp.
4 or 5 or 6 or 7 or 8
3 and 9
randomized controlled trial.pt.
controlled clinical trial.pt.
13 randomized.ab.
14 placebo.ab.
15 clinical trials as topic.sh.
16 randomly.ab.
17 trial.ab.
18 11 or 12 or 13 or 14 or 15 or 16 or 17
19 10 and 18
key: mp = title, original title, abstract, name of substance word, subject heading word, unique identifier, pt = publication type, ab = abstract
Appendix 2. Embase search strategy
exp ovary tumor/
(ovar* adj5 (cancer* or tumor* or tumour* or neoplas* or malignan* or carcinoma*)).mp.
1 or 2
follow up/
(follow up or follow‐up).mp.
surveillance.mp.
aftercare/
(aftercare or after care of after‐care).mp.
4 or 5 or 6 or 7 or 8
3 and 9
random*.mp.
factorial*.mp.
(crossover* or cross over* or cross‐over*).mp.
placebo*.mp.
(doubl* adj blind*).mp.
(singl* adj blind*).mp.
assign*.mp.
allocat*.mp.
volunteer*.mp.
crossover procedure/
double blind procedure/
randomized controlled trial/
single blind procedure/
11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23
10 and 24
key: mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer
Appendix 3. Central search strategy
MeSH descriptor Ovarian Neoplasms explode all trees
ovar* near/5 (cancer* or tumor* or tumour* or neoplas* or malignan* or carcinoma*)
(#1 OR #2)
MeSH descriptor Follow‐Up Studies explode all trees
(follow up) or follow‐up
MeSH descriptor Aftercare explode all trees
aftercare or (after care) or after‐care
surveillance
(#4 OR #5 OR #6 OR #7 OR #8)
(#3 AND #9)
Appendix 4. Tumour markers
| Tumour marker | Paper | Summary |
| IGF‐1 | Bese Add paper | No correlation with disease |
| CA125 + b2m | Hernádi 1992 | b2m has low specificity for detection of ovarian cancer. CA125 performs better |
| CA72.4 | Fayed 1998 | Added to CA125 it improves sensitivity and specificity for detecting recurrence, especially in mucinous tumours |
| CEA |
Khoo 1974 Khoo 1979 Lenehan 1986 |
Persistently low levels are consistent with a good prognosis Serial samples were useful in predicting relapse in a small number of women; clinical role is limited to a small subset of patients |
| CA72.4, CA19.9 | Fioretti 1992 | Useful for detecting recurrence in patients with normal CA125 at diagnosis |
| PLAP‐A, PLAP‐C | Fisken 1989 | No correlation with disease |
| Anti‐p53 | Gadducci 1995 | Not clinically useful |
| CYFRA 21‐1 | Gadducci 1998 | |
| D‐dimer | Gadducci 2001 | |
| Urinary neopterine | Hetzel 1983 | |
| TPA | Inoue 1985 | Lacks tumour specificity |
| SLX | Iwanari 1989 | May be of benefit in combination with CA125 |
| CA125 + CA15.3 + CA72.4 + SCC + 90K | Garzetti 1991 | Includes all gynaecological malignancies. CA125 plus 90K identified 86% of recurrences |
| CA125 + CEA + ferritin + TPA | Lahousen 1987 | If normal can avoid second look laparotomy |
| CA125 + CASA | Oehler 1999 | CASA less sensitive than CA125, CASA may be useful when CA125 inconclusive |
| Sialyl Le(x)‐i | Kobayashi 1989 | Upto 96% showed rise in levels with tumour progression |
| OPN | Schorge 2004 | Inferior to CA125 in determining response to treatment, but showed an earlier rise in recurrent disease |
| CA125 + TPS | Sliutz 1995 | Improved detection of recurrence when compared to CA125 alone |
| IAP | Shimizu 1986 | May have a role in early detection of recurrence |
| TPS |
Tempfer 1998 Zakrzewska 2000 |
TPS is useful, but cannot replace CA125 TPS may rise before CA125 rises in women with recurrence |
Data and analyses
Comparison 1. Immediate versus delayed treatment in patients with increased CA125 levels.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Overall survival | 1 | 527 | Hazard Ratio (Random, 95% CI) | 1.01 [0.82, 1.25] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Rustin 2010.
| Methods | A randomised controlled, multi‐centre trial in ovarian cancer of immediate treatment of relapse based on CA125 level alone versus delayed treatment based on conventional clinical indicators (MRC OV05/EORTC 55955 trials) OV05/55955 was designed to determine whether there were benefits from immediate treatment based on a confirmed elevation of CA125 levels versus delaying treatment until clinically indicated Women whose CA125 levels rose to more than two times the upper limit of normal were randomised to one of two treatment arms that received immediate or delayed treatment Randomisation to the immediate or delayed treatment groups used a 1:1 ratio and was done independently by each co‐ordinating centre From 1996‐2005, 1442 participants registered from 59 sites in 10 countries (centres across the UK, Spain, Norway, the Netherlands, France, Russia, Belgium, Ireland, Austria, and South Africa). Randomisation closed on 31 March 2008 when the targeted number of events (deaths) was reached, with 529 participants randomised (265 to the immediate treatment group and 264 to the delayed treatment group) |
|
| Participants | Eligible participants were women with ovarian cancer who were in complete clinical remission following first‐line platinum‐based chemotherapy and establishment of a normal CA125 level Women with the following histologies were included: epithelial ovarian cancers, fallopian tube cancers or primary serous peritoneal carcinoma After randomisation baseline characteristics were well balanced between the groups. Median age at registration was 61 years (range: 53‐68); 81% were FIGO stage III/IV Second‐line chemotherapy began a median of 5 months earlier in the immediate arm. Predominant histologies were serous and endometrioid, involving 53% and 17%, respectively, among randomised participants |
|
| Interventions | Women whose serum CA125 levels exceeded twice the upper limit of normal were randomised to either:
Relapses, regardless of modality of detection, were treated according to local standard practice by the gynaecological oncologist |
|
| Outcomes |
Primary outcome Overall survival calculated from date of randomisation to date of last follow‐up or death from any cause. At the time of analysis, survivors were censored at the date they were last known to be alive Secondary outcomes
|
|
| Notes | Intention‐to‐treat analysis Median follow‐up from randomisation was 56.9 (IQR 37.4 to 81.8) months The primary outcome measurement was overall survival and the trial was designed to detect a 10% improvement in 2‐year overall survival in the immediate treatment arm with at least 85% power and 5% significance level Median survival from randomisation was 25.7 months (95% CI 23.0 to 27.9) for women on immediate treatment and 27.1 months (95% CI 22.8 to 30.9) for those on delayed treatment, with a median follow‐up of 56.9 months (IQR 37.4 to 81.8) from randomisation and 370 deaths (186 immediate, 184 delayed) Median time spent with good global health score was 7.2 months (95% CI 5.3 to 9.3) for women assigned to immediate and 9.2 months (95% CI 6.4 to10.5) for those assigned to delayed treatment QoL assessed at baseline, at each follow‐up visit, and, if treatment was instituted, before each chemotherapy course Participants were followed‐up every 3 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The method of minimisation was used with the stratification factors: International Federation of Gynecology and Obstetrics (FIGO) stage (I versus II versus III versus IV); first‐line chemotherapy (single agent platinum versus platinum combination without taxane versus platinum taxane combination versus other); time from completion of first‐line chemotherapy to raised CA125 concentration (<6 versus 6 to 11 versus 12 to 24 versus >24 months); age (MRC OV05 at randomisation, EORTC 55955 at registration; <30 versus 30 to 55 versus 56 to 65 versus >65 years); and site". |
| Allocation concealment (selection bias) | Low risk | "CA125 results were masked to sites and patients until randomisation to early treatment or until clinical recurrence for those in the delayed treatment group". |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Serum CA‐125 was measured every three months but patients and investigators were blinded to the results, which were only available to the trials units". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100% analysed: 529/529 for primary outcome, and overall survival analysed using appropriate statistical techniques that accounted for censoring 21 (4%) women were lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available to permit judgement |
| Other bias | High risk | Point estimates and 95% CIs did not tally with corresponding P values for time to first deterioration in QoL score or death for many of the individual sub‐scales of EORTC QLQ‐C30 questionnaire (Table 4 in trial report). For example, for the emotional sub‐scale in the functional QoL category the upper 95% CI was 1.02 and the P value was 0.02. Similarly, significant sub‐scale factors appeared to have a vastly decreased P value from that which might be expected given the point and CI estimates It was also unclear for what the HRs in Table 4 were adjusted |
Abbreviations
CI = confidence interval FIGO = International Federation of Gynecology and Obstetrics HR = hazard ratio IQR = interquartile range QoL = quality of life
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alexandre 2012 | Primary or secondary outcomes not assessed |
| Bapsy 2012 | Not a randomised control trial |
| Buys 2012 | Incorrect participants. Not a randomised control trial |
| Fuso 2011 | Not a randomised control trial. A retrospective study |
| Geurts 2011 | Not a randomised control trial |
| Hall 2011 | Not a randomised control trial |
| Kitajima 2012 | Not a randomised control trial |
| Lajtman 2011 | Not a randomised control trial |
| Madry 2011 | Not a randomised control trial |
| Pastalozzi 2011 | Not a randomised control trial |
| Pignata 2011 | Not a randomised control trial |
| Rustin 2011 | Not a randomised control trial |
| van de Poll‐Franse 2011 | Primary outcome not assessed |
Characteristics of ongoing studies [ordered by study ID]
Lanceley.
| Trial name or title | Randomised study comparing satisfaction with follow‐up led by a trained cancer nurse versus conventional medical follow‐up after primary treatment for ovarian cancer |
| Methods | Prospective RCT |
| Participants | Women undergoing treatment for ovarian cancer The trial recruited 113 women, and closed to recruitment on 31 December 2008. The study completed in December 2010 and is yet to be reported |
| Interventions | Conventional medical follow‐up Follow‐up care led by a trained cancer nurse |
| Outcomes | Primary outcome measures are patient satisfaction and QoL |
| Starting date | 1 November 2005 |
| Contact information | Ms A Lanceley Gynaecological Oncology Gynaecological Cancer Research Centre Institute for Women's Health University College London, Maple House, 149 Tottenham Court Road London |
| Notes |
Differences between protocol and review
The search strategy was amended and run on MEDLINE, rather than dialog datastar. Two authors from the protocol (Nagindra Das and Katherine Deane) did not contribute to the main review. One new author joined the group for the main review. Disease free survival has been removed as an outcome. This is because time to detection of recurrence is not an adequate surrogate marker for overall survival. The two may diverge depending on treatments available at relapse. Furthermore detection of recurrence without subsequent information about survival risks the introduction of lead‐time bias. There is also the concern of length time bias whereby more indolent tumours have a longer pre‐clinical course and are therefore more likely to be detected by periodic tests.
Contributions of authors
Fiona Kew was the lead author of the original review published in 2011. Tilean Clarke updated the content for this update (2014). Raj Naik developed the original title, protocol and search strategy. He performed the original search and reviewed the papers and assisted in writing the review. Khadra Galaal reviewed the data and assisted in writing the original review and update. Andy Bryant provided statisical and methodological expertise.
Sources of support
Internal sources
R&D Department, Queen Elizabeth Hospital, Gateshead, UK.
External sources
-
Department of Health, UK.
NHS Cochrane Collaboration Programme. Grant Scheme CPG‐506
Declarations of interest
Tilean Clarke: none known Raj Naik: none known Khadra Galaal: none known Andrew Bryant: none known
Edited (no change to conclusions)
References
References to studies included in this review
Rustin 2010 {published data only}
- Rustin GJ, Burg ME, Griffin CL, Guthrie D, Lamont A, Jayson GC et al on behalf of MRC and EORTC collaborators. Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955): a randomised trial. Lancet 2010;376 (9747):1155‐63. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alexandre 2012 {published and unpublished data}
- Alexandre J, Brown C, Coeffic D, Raban N, Pfistere J, Mäenpää J, et al. CA‐125 can be part of the tumour evaluation criteria in ovarian cancer trials: experience of the GCIG CALYPSO trial. British Journal of Cancer 2012;106:633‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bapsy 2012 {published and unpublished data}
- Bapsy P. Ovarian cancer. Journal of the Indian Medical Association 2012;110(12):894‐7. [PubMed] [Google Scholar]
Buys 2012 {published and unpublished data}
- Buys S, Partridge E, Black A. Screening CA‐125 and transvaginal ultrasound does not reduce ovarian cancer mortality. Journal of the National Medical Association 2012;104:116. [Google Scholar]
Fuso 2011 {published and unpublished data}
- Fuso L, Evangelista A, Pagano E, Piovano E, Perotto S, Mazzola S. Variation in gynecological oncology follow‐up practice: attributable to cancer centers or to patient characteristics? A Piedmont Regional Oncology Network Study.. Tumori 2011;97:551‐8. [DOI] [PubMed] [Google Scholar]
Geurts 2011 {published and unpublished data}
- Geurts SME, Altena AM, Vegt F, Tjan‐Heijnen VCG, Massuger LFAG, Dijck JAAM, et al. No supportive evidence for clinical benefit of routine follow‐up in ovarian cancer. A Dutch multicentre study. International Journal of Gynecological Cancer 2011;21(4):647‐53. [DOI] [PubMed] [Google Scholar]
Hall 2011 {published and unpublished data}
- Hall M, Rustin G. Recurrent ovarian cancer: when and how to treat. Current Oncology Reports 2011;13:459‐71. [DOI] [PubMed] [Google Scholar]
Kitajima 2012 {published and unpublished data}
- Kitajima K, Ueno Y, Suzuki K, Kita M, Ebina Y, Yamada H, et al. Low‐dose non‐enhanced CT versus full‐dose contrast‐enhanced CT in integrated PET/CT scans for diagnosing ovarian cancer recurrence. European Journal of Radiology 2012;81:3557‐62. [DOI] [PubMed] [Google Scholar]
Lajtman 2011 {published and unpublished data}
- Lajtman E, Mlyncek M, Uharcek P, Matejka M. Follow‐up after primary therapy of malignant epithelial ovarian tumours (review). Bratislavske Lekarske Listy 2011;112(10):579‐85. [PubMed] [Google Scholar]
Madry 2011 {published and unpublished data}
- Madry R, Adamczak‐Ratajczak A. The Gordon Rustin revolution ‐ the measurement of CA125 in the surveillance of patients with ovarian cancer. Family Medicine and Primary Care Review 2011;13(2):189‐91. [Google Scholar]
Pastalozzi 2011 {published and unpublished data}
- Pastalozzi BC. Follow‐up: what is evidence‐based? Breast and gynecologic tumors. Onkologie 2011;34(6):14. [Google Scholar]
Pignata 2011 {published and unpublished data}
- Pignata S, Cannella L, Leopardo D, Bruni GS, Facchini G, Pisano C. Follow‐up with CA125 after primary therapy of advanced ovarian cancer: in favor of continuing to prescribe CA125 during follow‐up. Annals of Oncology 2011;22(8):40‐4. [DOI] [PubMed] [Google Scholar]
Rustin 2011 {published and unpublished data}
- Rustin GJS. Follow‐up with CA125 after primary therapy of advanced ovarian cancer has major implications for treatment outcome and trial performances and should not be routinely performed. Annals of Oncology 2011;22(8):45‐8. [DOI] [PubMed] [Google Scholar]
van de Poll‐Franse 2011 {published and unpublished data}
- Poll‐Franse LV, Nicolaije KAH, Vos MC, Pijnenborg JMA, Boll D, Husson O, et al. The impact of a cancer Survivorship Care Plan on gynecological cancer patient and health care provider reported outcomes (ROGY Care): study protocol for a pragmatic cluster randomized controlled trial. Trials Journal 2011;12(256). [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Lanceley {published data only}
- Lanceley A. A randomised study comparing satisfaction with follow‐up led by a trained cancer nurse versus conventional medical follow‐up after primary treatment for ovarian cancer. [ISRCTN59149551 ]
Additional references
Aebi 2008
- Aebi S, Castiglione M. Epithelial ovarian carcinoma: ESMO Clinical Recommendations for diagnosis, treatment and follow‐up. Annals of Oncology 2008;19(Suppl 2):ii14‐6. [DOI] [PubMed] [Google Scholar]
Barnhill 1992
- Barnhill D, O'Connor D, Farley J, Teneriello M, Armstrong D, Park R. Clinical surveillance of gynecologic cancer patients. Gynecological Oncology 1992;46(3):275‐80. [DOI] [PubMed] [Google Scholar]
Barzen 1990
- Barzen G, Cordes M, Langer M, Friedman W, Mayr AC, Felix R. Value of radioimmunoscintigraphy compared to computed tomography in the diagnosis and follow‐up of primary ovarian carcinoma. RöFo:Fortschritte auf dem Gebiete der Röntgenstrahlen und derNuklearmedizin 1990;153(1):85‐91. [DOI] [PubMed] [Google Scholar]
Bradley 2000
- Bradley E, Pitts M, Redman C, Calvert E, Howells R, Wafai C. What are the factors associated with the follow‐up preferences of women in long‐term remission from gynaecological cancer?. Journal of Obstetrics and Gynaecology 2000;20(4):408‐11. [DOI] [PubMed] [Google Scholar]
Bristow 2009
- Bristow RE, Puri I, Chi DS. Cytoreductive surgery for recurrent ovarian cancer: a meta‐analysis. Gynecologic Oncology 2009;112(1):265‐74. [DOI] [PubMed] [Google Scholar]
Bruzzone 1990
- Bruzzone M, Onetto M, Campora E, Chiara S, Oliva C, Guido T, et al. CA‐125 monitoring in the management of ovarian cancer. Anticancer research 1990;10(5A):1353‐9. [PubMed] [Google Scholar]
Cerejeira 1989
- Cerejeira L, Pinto FMM, Otilia BMO, Moutinho J. Validity of gynaegnost in the follow‐up of patients treated for ovarian cancer. Revue Française de Gynécologie et d'Obstétrique 1989;84(4):347‐9. [PubMed] [Google Scholar]
Cochrane Handbook 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Crombach 1985
- Crombach G, Zippel HH, Würz H. Clinical significance of cancer antigen 125 CA 125 in ovarian cancer. Cancer detection and prevention 1985;8(1‐2):135‐9. [PubMed] [Google Scholar]
Dachman 2001
- Dachman AH, Visweswaran A, Battula R, Jameel S, Waggoner SE. Role of chest CT in the follow‐up of ovarian adenocarcinoma. American Journal of Roentgenology 2001;176(3):701‐5. [DOI] [PubMed] [Google Scholar]
Engblom 1995
- Engblom PR, Grènman SE, Klemi PJ, Hirvonen TE, Rantanen VT, Salmi TA. The role of cul‐de‐sac aspiration cytology in the follow‐up of ovarian cancer. Acta Oncologica (Stockholm Sweden) 1995;34(6):783‐5. [DOI] [PubMed] [Google Scholar]
EUROCARE 2003
- Sant M, Aareleid T, Berrino F, Bielska Lasota M, Carli PM, Faivre J et al and the EUROCARE Working Group. EUROCARE‐3: survival of cancer patients diagnosed 1990‐94 ‐ results and commentary. Annals of Oncology 2003;14 (Supplement 5):v61‐v118. [DOI] [PubMed] [Google Scholar]
Fayed 1998
- Fayed ST, Ahmad SM, Kassim SK, Khalifa A. The value of CA 125 and CA72‐4 in management of patients with epithelial ovarian cancer. Disease Markers 1998;14(3):155‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fehm 2005
- Fehm T, Heller F, Krämer S, Jäger W, Gebauer G. Evaluation of CA125, physical and radiological findings in follow‐up of ovarian cancer patients. Anticancer Research 2005;25(3A):1551‐4. [PubMed] [Google Scholar]
Fioretti 1992
- Fioretti P, Gadducci A, Ferdeghini M, Prontera C, Malagnino G, Facchini V, et al. The concomitant determination of different serum tumor markers in epithelial ovarian cancer: relevance for monitoring the response to chemotherapy and follow‐up of patients. Gynecologic Oncology 1992;44(2):155‐60. [DOI] [PubMed] [Google Scholar]
Fisken 1989
- Fisken J, Leonard RC, Shaw G, Bowman A, Roulston JE. Serum placental‐like alkaline phosphatase PLAP: a novel combined enzyme linked immunoassay for monitoring ovarian cancer. Journal of Clinical Pathology 1989;42(1):40‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gadducci 1995
- Gadducci A, Marrai R, Baicchi U, Ferdeghini M, Fanucchi A, Facchini V, et al. The measurement of plasma D‐dimer DD levels in the follow‐up of patients with ovarian cancer. Anticancer Research 1995;15(6B):2683‐6. [PubMed] [Google Scholar]
Gaducci 2007
- Gadducci A, Cosio S, Zola P, Landoni F, Maggino T, Sartori E. Surveillance procedures for patients treated for epithelial ovarian cancer: a review of the literature. International Journal of Cancer 2007;17(1):21‐31. [DOI] [PubMed] [Google Scholar]
García 2003
- García VMJ, Boán GJF, Villar LLM, Aramendía BJM, López GG, Richter EJA. F‐18‐FDG positron emission tomography in the diagnosis of ovarian recurrence. Comparison with CT scan and CA 125. Revista Espanola de Medicina Nuclear 2003;22(4):217‐23. [DOI] [PubMed] [Google Scholar]
Garzetti 1991
- Garzetti GC, Di LRM, Ciavattini A, Pallotta MR, Marchegiani F, Valensise H, et al. Tumor markers in the early diagnosis of recurrence in gynecologic neoplasms: combined determination of CA‐125, CA 15‐3, CA 724, SCC, 90 K. Annali di Ostetricia, Ginecologia, Medicina Perinatale 1991;112(5):320‐3. [PubMed] [Google Scholar]
GLOBOCAN 2008
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C. GLOBOCAN 2012. Cancer incidence, mortality worldwide. IARC CancerBase No. 11, version 1.0. IARCPress, Lyon 2012.
Goonewardene 2007
- Goonewardene TI, Hall MR, Rustin GJS. Management of asymptomatic patients on follow‐up for ovarian cancer with rising CA‐125 concentrations. Lancet Oncology 2007;8(9):813‐21. [DOI] [PubMed] [Google Scholar]
Grabiec 2006
- Grabiec M, Walentowicz M, Nowicki P. The value of FDG PET/CT, ultrasound and CT in diagnosing recurrent ovarian carcinoma. Ginekologia Polska 2006;77(10):746‐52. [PubMed] [Google Scholar]
GRADE Working Group
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gritzmann 1986
- Gritzmann N, Karnel F, Imhof H, Wagner G, Müller T E, Dittrich C. Abdominal computerized tomography in the after‐care of ovarian cancers. Digitale Bilddiagnostik 1986;6(4):171‐5. [PubMed] [Google Scholar]
Grunfeld 1996
- Grunfeld E, Mant D, Yudkin P, Adewuyi‐Dalton R, Cole D, Stewart J, et al. Routine follow up of breast cancer in primary care: randomised trial. BMJ 1996;313:665‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hauth 2005
- Hauth EAM, Antoch G, Stattaus J, Kuehl H, Veit P, Bockisch A, et al. Evaluation of integrated whole‐body PET/CT in the detection of recurrent ovarian cancer. European Journal of Radiology 2005;56(2):263‐8. [DOI] [PubMed] [Google Scholar]
Hernádi 1992
- Hernádi Z, Molnár V, Juhász B, Pólka R, Margitai B. Predictive value of the tumor marker combination CA‐125 and beta‐2‐ microglobulin in ovarian cancer. Zentralblatt für Gynäkologie 1992;114(1):6‐9. [PubMed] [Google Scholar]
Hetzel 1983
- Hetzel H, Bichler A, Fuchs D, Hausen A, Reibnegger G, Wachter H. Significance of urinary neopterine in gynecological oncology: follow‐up of patients with ovarian cancer. Cancer Detection and Prevention 1983;6(1‐2):263‐6. [PubMed] [Google Scholar]
Hising 1991
- Hising C, Anjegård IM, Einhorn N. Clinical relevance of the CA 125 assay in monitoring of ovarian cancer patients. American Journal of Clinical Oncology 1991;14(2):111‐4. [DOI] [PubMed] [Google Scholar]
IARC 2002
- Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB. Cancer Incidence in Five Continents, Volume VIII. In: Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB editor(s). IARC Scientific Publication No 155. Lyon: IARC Scientific Publication, 2002. [Google Scholar]
Inoue 1985
- Inoue M, Fujita Y, Abe Y, Inoue Y, Ueda G, Tanizawa O, et al. Tissue polypeptide antigen as a tumor marker for gynecologic malignancies. Nippon Sanka Fujinka Gakkai Zasshi 1985;37(9):1799‐805. [PubMed] [Google Scholar]
Iwanari 1989
- Iwanari O, Miyako J, Date Y, Moriyama M, Yoshino N, Kijima S, et al. Diagnosis and follow‐up of ovarian cancer by a combination assay of serum sialyl SSEA‐1 antigen and CA125 levels. Nippon Gan Chiryo Gakkai Shi 1989;24(6):1256‐60. [PubMed] [Google Scholar]
Javitt 2007
- Javitt MC. ACR Appropriateness Criteria on staging and follow‐up of ovarian cancer. Journal of the American College of Radiology 2007;4(9):586‐9. [DOI] [PubMed] [Google Scholar]
Jemal 2008
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T. Cancer statistics. CA: A Cancer Journal for Clinicians 2008;58:71‐96. [DOI] [PubMed] [Google Scholar]
Kaesemann 1986
- Kaesemann H, Caffier H, Hoffmann FJ, Crombach G, Würz H, Kreienberg R, et al. Monoclonal antibodies in the diagnosis and follow‐up of ovarian cancer CA 125 as a tumor marker A cooperative study of the Gynecologic Tumor Marker Group GTMG. Klinische Wochenschrift 1986;64(17):781‐5. [DOI] [PubMed] [Google Scholar]
Kerr‐Wilson 1995
- Kerr‐Wilson RH, McCrum A. Follow‐up of patients with gynaecological cancer. Australian and New Zealand Journal of Obstetrics and Gynaecology 1995;35(3):298‐9. [DOI] [PubMed] [Google Scholar]
Kew 2005
- Kew FM, Roberts AP, Cruickshank DJ. The role of routine follow‐up after gynecological malignancy. International Journal of Gynecological Cancer 2005;15(3):413‐9. [DOI] [PubMed] [Google Scholar]
Kew 2006
Khan 1986
- Khan O, Cosgrove DO, Fried AM, Savage PE. Ovarian carcinoma follow‐up: US versus laparotomy. Radiology 1986;159(1):111‐3. [DOI] [PubMed] [Google Scholar]
Khoo 1974
- Khoo SK, Mackay EV. Carcinoembryonic antigen by radioimmunoassay in the detection of recurrence during long‐term followup of female genital cancer. Cancer 1974;34(3):542‐8. [DOI] [PubMed] [Google Scholar]
Khoo 1979
- Khoo SK, Whitaker S, Jones I, Mackay E. Predictive value of serial carcinoembryonic antigen levels in long‐term follow‐up of ovarian cancer. Cancer 1979;43(6):2471‐8. [DOI] [PubMed] [Google Scholar]
Kim 2007
- Kim CK, Park BK, Choi JY, Kim B‐G, Han H. Detection of recurrent ovarian cancer at MRI: comparison with integrated PET/CT. Journal of Computer Assisted Tomography 2007;31(6):868‐75. [DOI] [PubMed] [Google Scholar]
Kitajima 2008
- Kitajima K, Murakami K, Yamasaki E, Domeki Y, Kaji Y, Fukasawa I, et al. Performance of integrated FDG‐PET/contrast‐enhanced CT in the diagnosis of recurrent ovarian cancer: comparison with integrated FDG‐PET/non‐contrast‐enhanced CT and enhanced CT. European Journal of Nuclear Medicine & Molecular Imaging 2008;35(8):1439‐48. [DOI] [PubMed] [Google Scholar]
Kobayashi 1989
- Kobayashi H. Clinical usefulness of serum sialyl Lex‐i measurement in patients with ovarian cancer. Nippon Sanka Fujinka Gakkai Zasshi 1989;41(1):15‐9. [PubMed] [Google Scholar]
Kubik 2000
- Kubik HRA, Dörffler W, von SGK, Marincek B, Köchli OR, Seifert B, et al. Value of 18F‐FDG positron emission tomography, computed tomography, and magnetic resonance imaging in diagnosing primary and recurrent ovarian carcinoma. European Radiology 2000;10(5):761‐7. [DOI] [PubMed] [Google Scholar]
Kunkler 1991
- Kunkler IH, Kerr GR, Ludgate SM. The value of follow‐up in stage II carcinoma of the cervix. Clinical Oncology 1991;3(1):28‐31. [DOI] [PubMed] [Google Scholar]
Lahousen 1987
- Lahousen M, Stettner H, Pickel H, Urdl W, Pürstner P. The predictive value of a combination of tumor markers in monitoring patients with ovarian cancer. Cancer 1987;60(9):2228‐32. [DOI] [PubMed] [Google Scholar]
Lenehan 1986
- Lenehan PM, Dembo AJ, Miceli PN, Malkin DG, Malkin A. Clinical correlations of carcinoembryonic antigen in post‐operative patients with epithelial ovarian cancer. Tumour Biology : the journal of the International Society for Oncodevelopmental Biology and Medicine 1986;7(5‐6):389‐405. [PubMed] [Google Scholar]
Lenhard 2008
- Lenhard MS, Burges A, Johnson TR, Stieber P, Kumper C, Ditsch N, et al. PET‐CT in recurrent ovarian cancer: impact on treatment planning. Anticancer Research 2008;28(4C):2303‐8. [PUBMED: 18751410] [PubMed] [Google Scholar]
Low 1999
- Low RN, Saleh F, Song SY, Shiftan TA, Barone RM, Lacey CG, et al. Treated ovarian cancer: comparison of MR imaging with serum CA‐125 level and physical examination‐‐a longitudinal study. Radiology 1999;211(2):519‐28. [DOI] [PubMed] [Google Scholar]
Mangili 2007
- Mangili G, Picchio M, Sironi S, Vigano R, Rabaiotti E, Bornaghi D, et al. Integrated PET/CT as a first‐line re‐staging modality in patients with suspected recurrence of ovarian cancer. European Journal of Nuclear Medicine & Molecular Imaging 2007;34(5):658‐66. [DOI] [PubMed] [Google Scholar]
Menczer 2006
- Menczer J, Chetrit A, Sadetzki S, Golan A, Levy T. Follow‐up of ovarian and primary peritoneal carcinoma: the value of physical examination in patients with pretreatment elevated CA125 levels. Gynecologic Oncology 2006;103(1):137‐40. [DOI] [PubMed] [Google Scholar]
Moore 2002
- Moore S, Corner J, Haviland J, Wells M, Salmon E, Normand C, et al. Nurse led follow up and conventional medical follow up in management of patients with lung cancer: randomised trial. BMJ 2002;325:1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nakamoto 2001
- Nakamoto Y, Saga T, Ishimori T, Mamede M, Togashi K, Higuchi T, et al. Clinical value of positron emission tomography with FDG for recurrent ovarian cancer. American Journal of Roentgenology 2001;176(6):1449‐54. [DOI] [PubMed] [Google Scholar]
Oehler 1999
- Oehler MK, Sütterlin M, Caffier H. CASA and Ca 125 in diagnosis and follow‐up of advanced ovarian cancer. Anticancer Research 1999;19(4A):2513‐8. [PubMed] [Google Scholar]
Okai 1992
- Okai T, Kagawa H, Masuda H, Kozuma S, Mizuno M. Assessment of ovarian tumors by transvaginal scanning and clinical significance of ultrasonic examination in postoperative follow up. Rinsho Byori. The Japanese Journal of Clinical Pathology 1992;40(4):363‐8. [PubMed] [Google Scholar]
Olaitan 2001
- Olaitan A, Murdoch J, Anderson R, James J, Graham J, Barley V. A critical evaluation of current protocols for the follow‐up of women treated for gynecological malignancies: a pilot study. International Journal of Gynecologic Cancer 2001;11(5):349‐53. [DOI] [PubMed] [Google Scholar]
Palmer 2006
- Palmer C, Pratt J, Basu B, Earl H. A study to evaluate the use of CA125 in ovarian cancer follow‐up: a change in practice led by patient preference. Gynecologic Oncology 2006;101(1):4‐11. [DOI] [PubMed] [Google Scholar]
Parker 2006
- Parker PA, Kudelka A, Basen‐Engquist K, Kavanagh J, Moor J, Cohen L. The associations between knowledge, CA125 preoccupation, and distress in women with epithelial ovarian cancer. Gynecologic Oncology 2006;100(3):495‐500. [PUBMED: 16242759] [DOI] [PubMed] [Google Scholar]
Parmar 1998
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta‐analyses of the published literature for survival endpoints. Erratum in Statistics in Medicine 2004 Jun 15;23(11):1817. Statistics in Medicine 1998 Dec 30;17(24):2815‐34. [DOI] [PubMed] [Google Scholar]
Prayer 1993
- Prayer L, Kainz C, Kramer J, Stiglbauer R, Schurawitzki H, Baldt M, et al. CT and MR accuracy in the detection of tumor recurrence in patients treated for ovarian cancer. Journal of Computer Assisted Tomography 1993;17(4):626‐32. [DOI] [PubMed] [Google Scholar]
Renehan 2002
- Renehan AG, Egger M, Saunders MP, O'Dwyer ST. Impact on survival of intensive follow up after curative resection for colorectal cancer: systematic review and meta‐analysis of randomised trials. BMJ 2002;324:813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Renehan 2005
- Renehan AG, Egger M, Saunders MP, O'Dwyer ST. Mechanisms of improved survival from intensive follow up in colorectal cancer: a hypothesis. British Journal of Cancer 2005;92(3):430‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberts 2009
- Roberts K, Clarke C. Future disorientation following gynaecological cancer: Women’s conceptualisation of risk after a life threatening illness. Health, Risk & Society 2009;11(4):353–366. [Google Scholar]
Rustin 1996a
- Rustin G, Tuxen M. Use of CA 125 in follow‐up of ovarian cancer. Lancet 1996;348(9021):191‐2. [DOI] [PubMed] [Google Scholar]
Schorge 2004
- Schorge JO, Drake RD, Lee H, Skates SJ, Rajanbabu R, Miller DS, et al. Osteopontin as an adjunct to CA125 in detecting recurrent ovarian cancer. Clinical Cancer Research: an official journal of the American Association for Cancer Research 2004;10(10):3474‐8. [DOI] [PubMed] [Google Scholar]
Sella 2001
- Sella T, Rosenbaum E, Edelmann DZ, Agid R, Bloom AI, Libson E. Value of chest CT scans in routine ovarian carcinoma follow‐up. American Journal of Roentgenology 2001;177(4):857‐9. [DOI] [PubMed] [Google Scholar]
Shimizu 1986
- Shimizu Y, Akagaki E, Hirota K, Kono M, Miura S, Okudaira Y, et al. Significance of immunosuppressive acidic protein in the diagnosis and follow‐up of patients with ovarian cancer, in particular as a marker for chemotherapeutic effects. Nippon Sanka Fujinka Gakkai Zasshi 1986;38(4):554‐60. [PubMed] [Google Scholar]
Shinozuka 1994
- Shinozuka T, Miyamoto T, Hirazono K, Ebisawa K, Murakami M, Kuroshima Y, et al. Follow‐up laparoscopy in patients with ovarian cancer. The Tokai Journal of Experimental and Clinical Medicine 1994;19(1‐2):53‐9. [PubMed] [Google Scholar]
Sliutz 1995
- Sliutz G, Tempfer C, Kainz C, Mustafa G, Gitsch G, Koelbl H, et al. Tissue polypeptide specific antigen and cancer associated serum antigen in the follow‐up of ovarian cancer. Anticancer Research 1995;15(3):1127‐9. [PubMed] [Google Scholar]
Stewart 2001
- Stewart DE, Duff S, Wong F, Melancon C, Cheung AM. The views of ovarian cancer survivors on its cause, prevention, and recurrence. Medscape Women's Health 2001;6(5):5. [PubMed] [Google Scholar]
Sugiyama 1996
- Sugiyama Y, Shimizu Y, Umezawa S, Yamauchi K, Hasumi K. Feasibility of peritoneal washing cytology through the totally implanted reservoir for early detection of peritoneal recurrence of ovarian cancer. Nippon Sanka Fujinka Gakkai Zasshi 1996;48(3):213‐9. [PubMed] [Google Scholar]
Tempfer 1998
- Tempfer C, Hefler L, Haeusler G, Reinthaller A, Koelbl H, Zeisler H, et al. Tissue polypeptide specific antigen in the follow‐up of ovarian and cervical cancer patients. International Journal of Cancer. Journal International du Cancer 1998;79(3):241‐4. [DOI] [PubMed] [Google Scholar]
Testa 2002
- Testa AC, Ciampelli M, Mastromarino C, Lopez R, Zannoni GF, Mancuso S, et al. Detection of central pelvic recurrent disease with transvaginal color Doppler ultrasound in women treated for gynecological malignancy. Ultrasound in Obstetrics & Gynecology 2002;19(5):490‐5. [DOI] [PubMed] [Google Scholar]
Testa 2005
- Testa AC, Fruscella E, Ludovisi M, V Rosa, Malaggese M, Corrado G, et al. The role of sonographic examination in the follow‐up of gynecological neoplasms. Gynecologic Oncology 2005;99(3):696‐703. [DOI] [PubMed] [Google Scholar]
Thrall 2007
- Thrall MM, DeLoia JA, Gallion H, Avril N. Clinical use of combined positron emission tomography and computed tomography FDG‐PET/CT in recurrent ovarian cancer. Gynecologic Oncology 2007;105(1):17‐22. [DOI] [PubMed] [Google Scholar]
Torizuka 2002
- Torizuka T, Nobezawa S, Kanno T, Futatsubashi M, Yoshikawa E, Okada H, et al. Ovarian cancer recurrence: role of whole‐body positron emission tomography using 2‐fluorine‐18‐fluoro‐2‐deoxy‐ D‐glucose. European Journal of Nuclear Medicine and Molecular Imaging 2002;29(6):797‐803. [DOI] [PubMed] [Google Scholar]
Tuxen 2002
- Tuxen MK, Sölétormos G, Dombernowsky P. Serum tumor marker CA 125 for monitoring ovarian cancer during follow‐up. Scandinavian Journal of Clinical and Laboratory Investigation 2002;62(3):177‐88. [DOI] [PubMed] [Google Scholar]
Vaidya 2003
- Vaidya AP, Curtin JP. The follow‐up of ovarian cancer. Seminars in Oncology 2003;30(3):401‐12. [DOI] [PubMed] [Google Scholar]
VillaSanta 1980
- VillaSanta U, Jovanovski D. Follow‐up study of ovarian carcinoma by cytology of cul‐de‐sac aspirates. Gynecologic Oncology 1980;10(1):58‐62. [DOI] [PubMed] [Google Scholar]
Vinokurov 1992
- Vinokurov VL, Dudarev AL, Jurkova LE, Lapchenkov VI, Barbanel EJ. Tumor marker CA 125 in diagnosis, monitoring management and follow‐up of patients with ovarian tumors. European Journal of Gynaecological Oncology 1992;13(2):205‐8. [PubMed] [Google Scholar]
Vuento 2007
- Vuento M, Salmi T, Klemi P, Grénman S. Ultrasonographic‐guided pervaginal cul‐de‐sac cytology in the follow‐up of ovarian carcinoma. Anticancer Research 2007;27(2):1015‐8. [PubMed] [Google Scholar]
Zhu 2002
- Zhu X, Shen K, Lang J, Wu M, Huang H, Pan L. Role of positron emission tomography in detecting recurrent epithelial ovarian carcinoma. Zhonghua Fu Chan Ke za Zhi 2002;37(6):356‐8. [PubMed] [Google Scholar]
Zimny 2001
- Zimny M, Siggelkow W, Schröder W, Nowak B, Biemann S, Rath W, et al. 2‐Fluorine‐18‐fluoro‐2‐deoxy‐d‐glucose positron emission tomography in the diagnosis of recurrent ovarian cancer. Gynecologic Oncology 2001;83(2):310‐5. [DOI] [PubMed] [Google Scholar]


