Abstract
Background
Excess dietary sodium consumption is a risk factor for high blood pressure, stroke and cardiovascular disease. Currently, dietary sodium consumption in almost every country is too high. Excess sodium intake is associated with high blood pressure, which is common and costly and accounts for significant burden of disease. A large number of jurisdictions worldwide have implemented population‐level dietary sodium reduction initiatives. No systematic review has examined the impact of these initiatives.
Objectives
• To assess the impact of population‐level interventions for dietary sodium reduction in government jurisdictions worldwide.
• To assess the differential impact of those initiatives by social and economic indicators.
Search methods
We searched the following electronic databases from their start date to 5 January 2015: the Cochrane Central Register of Controlled Trials (CENTRAL); Cochrane Public Health Group Specialised Register; MEDLINE; MEDLINE In Process & Other Non‐Indexed Citations; EMBASE; Effective Public Health Practice Project Database; Web of Science; Trials Register of Promoting Health Interventions (TRoPHI) databases; and Latin American Caribbean Health Sciences Literature (LILACS). We also searched grey literature, other national sources and references of included studies.
This review was conducted in parallel with a comprehensive review of national sodium reduction efforts under way worldwide (Trieu 2015), through which we gained additional information directly from country contacts.
We imposed no restrictions on language or publication status.
Selection criteria
We included population‐level initiatives (i.e. interventions that target whole populations, in this case, government jurisdictions, worldwide) for dietary sodium reduction, with at least one pre‐intervention data point and at least one post‐intervention data point of comparable jurisdiction. We included populations of all ages and the following types of study designs: cluster‐randomised, controlled pre‐post, interrupted time series and uncontrolled pre‐post. We contacted study authors at different points in the review to ask for missing information.
Data collection and analysis
Two review authors extracted data, and two review authors assessed risk of bias for each included initiative.
We analysed the impact of initiatives by using estimates of sodium consumption from dietary surveys or urine samples. All estimates were converted to a common metric: salt intake in grams per day. We analysed impact by computing the mean change in salt intake (grams per day) from pre‐intervention to post‐intervention.
Main results
We reviewed a total of 881 full‐text documents. From these, we identified 15 national initiatives, including more than 260,000 people, that met the inclusion criteria. None of the initiatives were provided in lower‐middle‐income or low‐income countries. All initiatives except one used an uncontrolled pre‐post study design.
Because of high levels of study heterogeneity (I2 > 90%), we focused on individual initiatives rather than on pooled results.
Ten initiatives provided sufficient data for quantitative analysis of impact (64,798 participants). As required by the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) method, we graded the evidence as very low due to the risk of bias of the included studies, as well as variation in the direction and size of effect across the studies. Five of these showed mean decreases in average daily salt intake per person from pre‐intervention to post‐intervention, ranging from 1.15 grams/day less (Finland) to 0.35 grams/day less (Ireland). Two initiatives showed mean increase in salt intake from pre‐intervention to post‐intervention: Canada (1.66) and Switzerland (0.80 grams/day more per person); however in both countries the pre‐intervention data point was from several years prior to the initiation of the intervention. The remaining initiatives did not show a statistically significant mean change.
Seven of the 10 initiatives were multi‐component and incorporated intervention activities of a structural nature (e.g. food product reformulation, food procurement policy in specific settings). Of those seven initiatives, four showed a statistically significant mean decrease in salt intake from pre‐intervention to post‐intervention, ranging from Finland to Ireland (see above), and one showed a statistically significant mean increase in salt intake from pre‐intervention to post‐intervention (Switzerland; see above).
Nine initiatives permitted quantitative analysis of differential impact by sex (men and women separately). For women, three initiatives (China, Finland, France) showed a statistically significant mean decrease, four (Austria, Netherlands, Switzerland, United Kingdom) showed no significant change and two (Canada, United States) showed a statistically significant mean increase in salt intake from pre‐intervention to post‐intervention. For men, five initiatives (Austria, China, Finland, France, United Kingdom) showed a statistically significant mean decrease, three (Netherlands, Switzerland, United States) showed no significant change and one (Canada) showed a statistically significant mean increase in salt intake from pre‐intervention to post‐intervention.
Information was insufficient to indicate whether a differential change in mean salt intake occurred from pre‐intervention to post‐intervention by other axes of equity included in the PROGRESS framework (e.g. education, place of residence).
We identified no adverse effects of these initiatives.
The number of initiatives was insufficient to permit other subgroup analyses, including stratification by intervention type, economic status of country and duration (or start year) of the initiative.
Many studies had methodological strengths, including large, nationally representative samples of the population and rigorous measurement of dietary sodium intake. However, all studies were scored as having high risk of bias, reflecting the observational nature of the research and the use of an uncontrolled study design. The quality of evidence for the main outcome was low. We could perform a sensitivity analysis only for impact.
Authors' conclusions
Population‐level interventions in government jurisdictions for dietary sodium reduction have the potential to result in population‐wide reductions in salt intake from pre‐intervention to post‐intervention, particularly if they are multi‐component (more than one intervention activity) and incorporate intervention activities of a structural nature (e.g. food product reformulation), and particularly amongst men. Heterogeneity across studies was significant, reflecting different contexts (population and setting) and initiative characteristics. Implementation of future initiatives should embed more effective means of evaluation to help us better understand the variation in the effects.
Plain language summary
National government initiatives to reduce salt intake in populations
The problem In almost all countries worldwide, most people eat too much salt. This is a problem because eating too much salt can cause high blood pressure, which can lead to health problems such as heart disease and stroke. To reduce the amount of salt eaten, governments in many countries have developed national salt reduction initiatives.
The review question Our aim was to examine whether national salt reduction initiatives have been effective in reducing the amount of salt consumed in those populations.
Study characteristics We searched research papers and government reports and had direct communication with individuals working in salt reduction in their respective countries. The evidence is current as of 5 January 2015, when we last searched electronic databases. Initiatives in 15 countries met the inclusion criteria. Ten of these countries provided sufficient data for quantitative analysis, gathered from studies that included 64,798 participants. Initiatives ranged from one activity (e.g. in Japan, which at the time of writing had a public information campaign) to many activities (e.g. in the United Kingdom, which provided five activities including on‐package nutrition information, restrictions on marketing to children and food product reformulation). Of the 15 countries that met inclusion criteria, seven provided information about funding source, of which six reported non‐industry funding. The other eight countries did not report a funding source for one or more data point(s).
Key results and quality of the evidence Five of the 10 countries included in the quantitative analysis (China, Finland, France, Ireland and England) showed a decrease in salt intake after the intervention. Two of the 10 countries (Canada, Switzerland) showed an increase in salt intake after the intervention, however, in both countries the only data available were from several years prior to the intervention starting. Because the initiatives were very different, we cannot present an overall finding of whether these types of initiatives work.
When we focused on the subset of seven countries whose salt reduction initiatives included multiple components and were not focused solely on educating the public, we found that more than half (four of seven) showed a decrease in salt intake from pre‐intervention to post‐intervention.
When we examined the nine initiatives that analysed men and women separately, we found that amongst men, more than half (five of nine) showed a decrease in salt intake after the intervention. Amongst women, the pattern of findings was less clear, with three of nine interventions showing a decrease, two showing an increase and four showing no change in salt intake.
Low‐bias study designs, such as randomised controlled trials, typically are not suitable for evaluating complex initiatives such as these; therefore, we rated all of the studies included in this review as having low methodological quality. Large nationally representative samples of the population and careful measurement of dietary sodium intake were strengths of several studies. However, because of study design limitations, the trustworthiness of study results is not clear.
Overall, our results show that national government initiatives have the potential to achieve population‐wide reductions in salt intake, especially amongst men, and particularly if they employ more than one strategy and include structural activities such as food product reformulation (i.e. food companies putting less salt in food products). The wide variation of results across the studies we found presents a challenge in interpreting the current evidence and this warrants more research to help us understand this.
Summary of findings
for the main comparison.
| Population‐level interventions in national government jurisdictions to reduce sodium consumption | ||||||
|
Patient or population: people of all ages Settings: government jurisdictions Intervention: population‐level intervention to reduce dietary sodium consumption Comparison: mean change in salt intake (grams/d) from pre‐intervention to post‐intervention | ||||||
| Outcomes | Illustrative comparative risks | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Pre‐intervention estimate | Post‐intervention estimate | |||||
| Salt intake in grams per day ‐ all eligible studies that provided sufficient data for quantitative analysis of overall impact (n = 10 countries) | Mean salt intake at pre‐intervention ranged from 6.1 to 12.7 grams/d | Mean salt intake at post‐intervention ranged from 5.5 to 11.9 grams/d | Not shown owing to high study heterogeneity | 64,798 participants (12 studies)* | ⊕⊝⊝⊝ very low | As the result of high study heterogeneity (I2 > 90% in all analyses), we focus on individual studies rather than pooled effects. We downgraded the quality of evidence from low to very low due to all studies having high risk of bias (confounding domain) and the substantial inconsistency of effect sizes and the direction of the effect, which varied across the studies. |
| Salt intake in grams per day ‐ subset of initiatives that are multi‐component and incorporate activities of a structural nature (n = 7 countries) | Mean salt intake at pre‐intervention ranged from 6.3 to 11.8 grams/d | Mean salt intake at post‐intervention ranged from 5.5 to 10.6 grams/d | Not shown owing to high study heterogeneity | 34,227 participants (9 studies)* |
⊕⊝⊝⊝ very low | |
| Salt intake in grams per day ‐ women only (n = 9 countries) | Mean salt intake at pre‐intervention ranged from 4.7 to 12.2 grams/d | Mean salt intake at post‐intervention ranged from 4.1 to 11.4 grams/d | Not shown owing to high study heterogeneity | 27,184 participants (11 studies)* |
⊕⊝⊝⊝ very low | |
| Salt intake in grams per day ‐ men only (n = 9 countries) | Mean salt intake at pre‐intervention ranged from 6.1 to 13.2 grams/d | Mean salt intake at post‐intervention ranged from 5.2 to 12.5 grams/d | Not shown owing to high study heterogeneity | 22,977 participants (11 studies)* |
⊕⊝⊝⊝ very low | |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
*Includes evaluations of the United Kingdom for England only, Scotland only and Great Britain. Including only Great Britain does not change overall findings
We rated the overall quality of evidence using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) framework (GRADE n.d.), which is based on 5 considerations: risk of bias, imprecision, inconsistency, indirectness and publication bias. All of our studies started at 'low' quality because of their observational, uncontrolled nature.
Background
We have made minor changes to this section. See Differences between protocol and review.
Please note that, throughout the review, we use both terms ‐ "sodium" and "salt" ‐ to respect the term used in the cited document. For our analysis (see below), we converted all estimates to a common metric: salt intake in grams per day.
Description of the issue
Excess dietary sodium consumption is a risk factor for high blood pressure, stroke, cardiovascular disease and other adverse health outcomes (He 2009; Mohan 2009; Strazzullo 2009). Particularly strong evidence suggests a direct relationship between sodium intake and high blood pressure (He 2009). Hypertension is common (Vasan 2002) and costly (Gaziano 2009) and accounts for a significant burden of disease and death. The World Health Organization (WHO) considers high blood pressure to be the leading preventable risk factor for death in the world (Ezzati 2002; Lopez 2006). It has been estimated that mean salt consumption in 181 of 187 countries exceeded the daily intake of salt recommended by WHO in 2010, and 51 of these countries reported mean intakes greater than double the recommended amount (WHO 2007; Powles 2013).
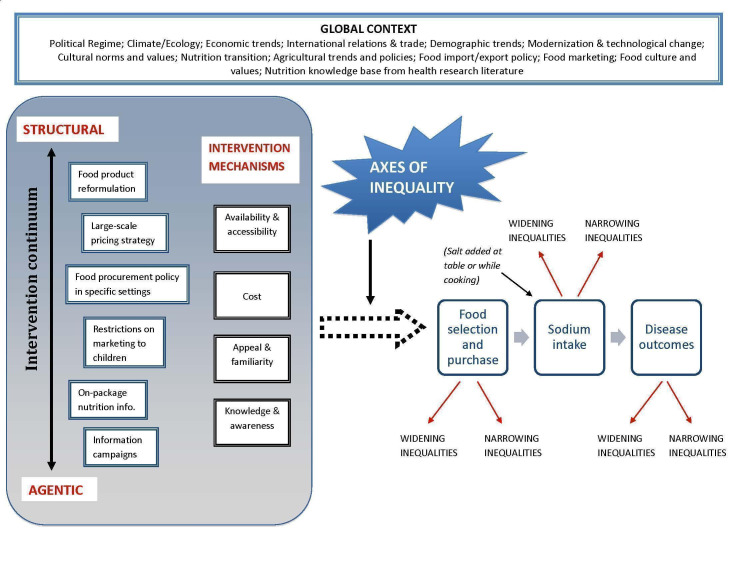
Dietary sodium reduction may be addressed through a population‐level intervention approach. Population‐level interventions target whole populations (e.g. jurisdictions), including individuals with higher risk profiles and those with more moderate risk profiles (Rose 1992; McLaren 2010). This contrasts with a high‐risk strategy whereby efforts are focused on individuals at highest level of risk. The population‐level approach may provide significant leverage for impact because the societal impact of moving the entire distribution of risk to the left (i.e. in the direction of lower risk) may be very large (Figure 1) (Rose 1992). Dietary sodium reduction lends itself to a population‐level intervention approach for several reasons. First, the association between sodium intake and blood pressure is linear with no obvious threshold (SWG 2010) and thus no clear cutoff from which a discrete high‐risk group of individuals can be identified for targeted intervention. Second, modelling studies have shown that the population impact of a widespread reduction in sodium intake is potentially very large (e.g. Joffres 2007; Smith‐Spangler 2010) and could yield significant cost savings (Joffres 2007; Dall 2009) such that cost‐effectiveness exceeds that of clinical interventions (e.g. Bibbins‐Domingo 2010). A study of 23 low‐income and middle‐income countries, which account for 80% of global deaths from chronic disease, estimated that 8.5 million deaths could be averted over 10 years through a 15% reduction in salt intake across the population (Asaria 2007). Third, knowledge of the main sources of sodium in the diet of a given population provides guidance about leverage points for population intervention in different countries. Specifically, in affluent countries, most (75% to 80%) sodium consumed comes from processed foods (Mattes 1991; Andersen 2009); therefore the food industry represents an important leverage point for intervention. In lower‐income and middle‐income countries, most sodium is consumed through addition of salt during the cooking or eating process to sauces and seasonings that are very high in salt (WHO 2007); thus a sodium reduction intervention in these countries might take the form of reduced salt content in condiments, increased use of salt substitutes and development of information campaigns aimed at individual behaviour change.
1.
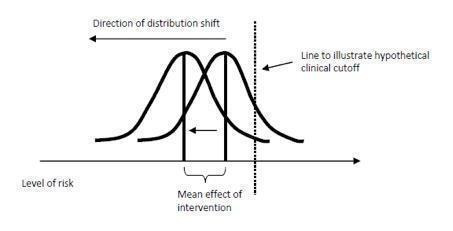
Depiction of the hypothetical impact of a population‐level intervention, achieved by shifting the frequency distribution of the risk factor in a direction of lower risk (adapted from Rose 1992).
When population‐level sodium reduction interventions are undertaken, it is important that they do not worsen socio‐economic inequities in health (Whitehead 2007; Frohlich 2008), including those involving sodium intake (Ji 2014; McLaren 2014). Concern about the presence of and increase in socio‐economic inequities in health has been voiced by various national and international health organisations, including the World Health Organization (WHO) (CSDH 2008), the US Department of Health and Human Services (USDHHS) and the Public Health Agency of Canada (PHAC 2006). Despite enduring existence of and concern about socio‐economic inequities in health worldwide (CSDH 2008), we currently know very little about whether, or the extent to which, population‐level interventions are equitable in their impact (Whitehead 2007; Bambra 2010). By using dietary sodium reduction as an example, this review provides insight into the broader question of whether and how population‐level interventions can achieve impact that is both overall and equitable.
Description of the intervention
Review authors focused on population‐level initiatives (i.e. interventions that target whole populations, in this case, government jurisdictions, worldwide) for dietary sodium reduction.
From the dietary sodium reduction literature, we identified six types of population‐level interventions for dietary sodium reduction that may occur within government jurisdictions. These intervention types may be conceptualised as existing on a continuum anchored by more agentic interventions (i.e. act on behaviours) at one end, and more structural interventions (i.e. act on circumstances in which behaviours occur) at the other end (McLaren 2010).
Food product reformulation: large‐scale efforts to lower the sodium content of food products at the time of production. By 'large‐scale', we mean efforts that characterise whole jurisdictions (e.g. provinces, countries), transcending specific settings within jurisdictions (see 'food procurement policy', below).
Pricing interventions: large‐scale strategies (e.g. taxation, subsidisation) designed to manipulate the price of food products in a way that encourages the purchase of healthier foods and discourages the purchase of less healthy foods. By 'large‐scale', we mean efforts that span whole jurisdictions (e.g. provinces, countries), transcending specific settings within jurisdictions. This may include strategies to manipulate the price of table salt or of high salt‐containing products (e.g. condiments) in lower‐income and middle‐income countries.
Food procurement policy in specific settings: nutrition policy (e.g. limits on sodium content in foods) implemented within a system of contained food service settings or environments, particularly publicly funded environments such as schools, colleges/universities, childcare settings, workplaces, recreational facilities, prisons, hospitals and long‐term care facilities.
Restrictions on marketing to children: efforts by government to restrict the extent or nature of promotional/marketing activities conducted by companies. As an example, the province of Quebec, Canada, has banned television advertising to children since 1980 under sections 248 and 249 of the Consumer Protection Act (CPA 1978). By 'marketing', we mean use of various media, including but not limited to television.
On‐package nutrition information: nutrition information provided directly on food packaging. We have identified three subtypes of on‐package nutrition information: (1) information on calories, nutrients and percentage daily value of nutrients (e.g. Canada's Nutrition Facts Table); (2) on‐package symbols provided to assist consumers with healthy food selection (e.g. the 'traffic light' system of the UK, which tells consumers at a glance whether a food is high (red), medium (amber) or low (green) in salt, sugar, fat and saturated fat, respectively); and (3) on‐package high‐salt warning labels (e.g. mandatory warning labels on foods in Finland whose sodium content exceeds defined limits).
Information campaigns: public information/education campaigns that focus specifically on salt/sodium or more broadly on diet (including sodium). Campaigns may be delivered via diverse media, including television, radio, posters/billboards, newspapers, other print materials, social media (e.g. Facebook, Twitter), RSS (really simple syndication) feeds, email subscriptions, online advertising and cell phones (health 'apps', text message updates) but must pertain to a whole government jurisdiction to be eligible for our review.
How the intervention might work
This review is anchored in scholarly literature on social determinants of health, population health and health promotion (e.g. Ottawa Charter 1986; Whitehead 2007; CSDH 2008; Raphael 2009). From this perspective, a general starting point is a major, although sometimes unclear, distinction between interventions that are individually oriented and those that are structurally oriented. Individually oriented interventions include efforts that aim to strengthen individuals by providing information, education or skills. The underlying theory (implicit or explicit) is that the health issue (in this case, excess sodium consumption and associated health problems) reflects personal deficits such as lack of information, knowledge or skills, and the interventions are designed to offset, or make up for, these deficiencies (Whitehead 2007). Structurally oriented interventions aim to improve the environment, settings or conditions in which individuals live, work, go to school and recreate. The underlying theory (implicit or explicit) is that the health issue reflects structural deficits such as limited availability of appropriate foods or limited access or opportunity to procure appropriate foods as the result of restricted social and economic resources such as income, social status, place of residence and cultural/ethnic group (Whitehead 2007; Raphael 2009). Structurally oriented interventions are designed to offset, or make up for, these deficiencies.
Building on the foundational work of Rose (Rose 1992), we (McLaren 2010; Sumar 2011) distinguished between population‐level interventions that are more agentic (target behaviour change amongst individuals) and those that are more structural (target conditions in which behaviours occur). The intervention types listed above convey the breadth of approaches available for dietary sodium reduction, ranging from individually oriented or agentic, to structurally oriented, as illustrated in our logic model (Figure 2) and accompanying glossary (Appendix 1).
2.
Logic model.
We have identified four broad, overlapping categories of mechanisms by which interventions may affect food selection and purchase, sodium intake and ultimately health.
Availability and accessibility: number or proportion of lower‐sodium food products available on the market or within settings of interest.
Cost: purchase price of lower‐sodium products, relative to higher‐sodium products, especially relative to higher‐sodium versions of the same product.
Appeal and familiarity: symbolic desirability of or attachment to a food product as experienced by consumers, established through effective marketing or some other means (e.g. personal tastes and preferences).
Knowledge and awareness: consumer cognizance of dietary sodium specifically or of diet generally, including associations with health.
A single, one‐to‐one relationship between intervention type and mechanism may not be evident. For example, large‐scale pricing strategies may facilitate selection of lower‐sodium food via 'cost' while impeding selection via 'appeal and familiarity' if the lower‐sodium products do not appeal to the individual.
Why it is important to do this review
We focus on population‐level dietary sodium reduction interventions that are implemented by governments. This focus is important because an increasing number of jurisdictions worldwide are developing and/or implementing population‐level dietary sodium reduction interventions (Webster 2011; Trieu 2015). Although some countries have a long history of population‐level sodium reduction efforts (e.g. Finland, where efforts have been ongoing since the 1970s), most initiatives have been implemented more recently. The number of countries with active programmes has increased enormously since the early 2000s, when the World Health Organization first publicised its global target of < 5 grams salt/d (corresponding to < approximately 1967 mg/d of sodium, which sometimes is rounded to < 2000 mg/d of sodium) (WHO 2003; Penney 2011; Trieu 2015).1 It is important and timely to systematically assess (1) the overall impact and (2) the differential impact of these initiatives.
Other Cochrane reviews on dietary sodium reduction have focused on patient populations and intensive clinical interventions (Hooper 2004), or have combined diverse target populations and interventions in the interest of focusing specifically on the main effects of sodium reduction per se (Taylor 2011). Further, none have examined the equity of intervention impact. Our focus on population‐level dietary sodium reduction interventions in government jurisdictions, including how equitable they are in terms of their impact, is unique and has important implications for policy‐makers worldwide in terms of identifying potentially impactful and cost‐effective mechanisms for sodium reduction that lie outside the health sector.
Objectives
To assess the impact of population‐level interventions for dietary sodium reduction in government jurisdictions worldwide.
To assess the differential impact of those initiatives by social and economic indicators.
Methods
Criteria for considering studies for this review
Types of studies
This section is substantively the same as the protocol (McLaren 2013).
Because of the unit of intervention (populations, not individuals) and the scale and scope of the interventions of interest (government jurisdictions), inclusion criteria go beyond randomised controlled trials to include other study designs.
The jurisdictional nature of intervention delivery is such that the interventions of interest often resemble a natural experiment whereby assessment of impact is based on jurisdictional (e.g. national, provincial) data gathered before and after the intervention, as we found in a similar review (Sumar 2011), in which almost all (18 of 19) included studies used an interrupted time series design or an uncontrolled pre‐post design.
The following study characteristics were included.
Cluster‐randomised studies (i.e. studies in which populations (jurisdictions) are randomised to one intervention condition or another).
Controlled pre‐post studies (i.e. studies with pre‐intervention and post‐intervention data from the intervention population and a comparison population).
Interrupted time series studies (i.e. studies reporting more than one data point before, and more than one data point after, the intervention, in a single population).
Uncontrolled pre‐post studies (i.e. studies reporting at least one pre‐intervention data point and at least one post‐intervention data point from the same or a comparable jurisdiction (e.g. both pre‐intervention and post‐intervention data points were national estimates).
Please note that we use the term "study" to refer to the interventions or initiatives considered in this review.
Types of participants
This section is the same as the protocol (McLaren 2013).
We included populations of males and females, of any age, living in any geographic region worldwide.
To be included, the study had to focus on a population, which for this review was defined as a government jurisdiction (e.g. country, state/region/province, municipality).
We excluded studies that focused on (1) a population subgroup defined by health or socio‐demographic indicators or (2) an area or setting that was not a government jurisdiction (e.g. school, community).
Types of interventions
We have made minor changes to this section. See Differences between protocol and review.
We included population‐level interventions in government jurisdictions (e.g. national, state/regional/provincial, municipal) for dietary sodium reduction in which activities were under way (vs in the planning stages) and for which a start date could be identified (for the purpose of confirming pre‐intervention and post‐intervention data points). Interventions included at least one of the following activities.
Public information/education campaign.
On‐package nutrition information.
Restriction on marketing to children.
Food procurement policy in specific settings.
Pricing intervention.
Food product reformulation.
We excluded the following.
Interventions targeting those at high risk (e.g. individuals with pre‐existing hypertension).
Interventions, regardless of target population, delivered in a one‐on‐one or small group format.
Pharmaceutical interventions.
Types of outcome measures
We have made important changes to this section. See Differences between protocol and review.
Primary outcomes
Any measure of dietary sodium consumption, including the following.
Dietary survey (e.g. 24‐hour recall, food frequency questionnaire, consumption as estimated from reported food purchasing).
Urine sample (e.g. 24‐hour urine, spot urine).
All estimates were converted to a common metric ‐ salt intake in grams per day ‐ through the following conversions.
1 gram of salt = 393.4 milligrams of sodium.
Salt intake (grams/d) = urinary sodium concentration (mmol/d) * molecular weight of sodium chloride (0.058 grams/mmol).
One gram of salt, or 393.4 milligrams of sodium, corresponds to approximately 1/6 of a teaspoon of table salt, which represents approximately 1/5 of the World Health Organization global target of 5 grams of salt per day (WHO 2003).
Secondary outcomes
None (see Differences between protocol and review).
Search methods for identification of studies
Electronic searches
This section is the same as in the protocol (McLaren 2013).
We searched the following research databases from their start date to 5 January 2015.
Cochrane Central Register of Controlled Trials (CENTRAL).
Cochrane Public Health Group Specialised Register (via communication with the Cochrane Public Health Group Trials Search Co‐ordinator).
MEDLINE (Ovid platform).
MEDLINE In Process & Other Non‐Indexed Citations (Ovid platform).
EMBASE (Ovid platform).
Effective Public Health Practice Project Database.
Web of Science.
Trials Register of Promoting Health Interventions (TRoPHI) databases.
Latin American Caribbean Health Sciences Literature (LILACS) database published by BIREME (http://new.paho.org/bireme/, a Pan American Center of the Pan American Health Organization, Regional Office of WHO).
We developed a detailed search strategy by combining established search terms and free text terms for each database. Searches combined dietary sodium search terms with terms designed to capture studies on the breadth of population‐level intervention types as described above (food product reformulation, pricing interventions, food procurement policy, marketing restrictions, on‐package nutrition information, information campaigns). We validated the search against key articles known to be important for our review. We developed the search strategy for MEDLINE and adapted it for the other databases to take account of differences in search terms and syntax rules. The search strategies used for the research databases are shown in Appendix 2.
We applied no date or language limits.
Searching other resources
We have made changes to this section. See Differences between protocol and review.
Grey literature
We searched the following grey literature websites and resources, using the search strategy indicated.
| Grey literature website or resource | Search term/strategy applied |
| OpenGrey | Sodium or salt (discipline ‘Medicine’) |
| World Health Organization | Dietary sodium or salt and reduc* or decrease and strategies or intervention |
| Public Health Agency of Canada | Dietary sodium or salt and reduc* or decrease |
| Centers for Disease Control and Prevention | Salt (http://www.cdc.gov/salt/publications.htm) → Publications |
| Pan American Health Organization (Caribbean Food and Nutrition Institute) |
Health topics → Salt reduction (http://www.paho.org/hq/index.php?option=com_content&view=article&id=2015&Itemid=4024) |
| World Action on Salt and Health (WASH) | World Action and search for information about relevant literature from each country |
| Institute of Medicine | Keyword search: sodium or salt or sodium chloride |
Country questionnaires
On the basis of the searches described above, and led by review authors Webster and Trieu (Trieu 2015), we established a list of national sodium reduction initiatives and sent it to international experts and representatives of the World Health Organization to identify whether we had missed any countries with initiatives.
Led by Webster and Trieu (Trieu 2015), we prepared a questionnaire (Appendix 3) and sent it to 87 country programme leaders identified through the expert review. We followed up queries with country programme leaders or the relevant WHO regional expert or through a targeted search. Those findings are published in our companion review (Trieu 2015), and we considered all 75 initiatives reported in that paper for inclusion in this review.
Other modes of obtaining information
We handsearched the reference lists of included studies and performed related reference searches on PubMed and citation searches on Web of Science to ensure that we had identified all available published material for each intervention. As we refined the list of initiatives (countries) to be included in this review, we undertook purposive Internet searching for materials pertaining to those initiatives (e.g. government statistical agency reports or websites describing survey methods).
In the event of missing information or uncertainty, we attempted to contact study authors or country contacts via email.
Data collection and analysis
Selection of studies
This section is substantively the same as in the protocol (McLaren 2013).
Two review authors (NS and LM, or AB and LM) independently screened the titles and abstracts (when available) of all reports identified through the online searches. We retrieved in full all reports that appeared to meet inclusion criteria, or for which titles and abstracts provided insufficient detail. Two review authors (NS and LM, or AB and LM) independently assessed the full reports to determine whether they met inclusion criteria, resolving disagreements by discussion.
Data extraction and management
This section is substantively the same as in the protocol (McLaren 2013).
Two review authors (AB and LM) collaboratively extracted data using data extraction forms designed for this review, which had been pilot tested and revised before finalisation. We resolved disagreements on data extraction via discussion and contacted authors of primary studies and/or country contacts to request clarification of unclear data or to obtain missing information. When we received responses, we included this information in the review.
For each initiative, we extracted the following information.
Study design.
Participants (age, sex, region of residence).
Sampling strategy.
Sample size.
Response rate.
Details of the intervention, including time frame and main activities.
Outcomes (measures and units of dietary sodium intake).
Axes of inequality (PROGRESS indicators included, if any. PROGRESS, a framework for incorporating focus on equity in systematic reviews, includes the following axes: place of residence; race/ethnicity/culture/language; occupation; gender/sex; religion; education; socioeconomic status; social capital).
Funding source(s).
Conflicts of interest.
Sources of data points and references.
Assessment of risk of bias in included studies
We have made changes to this section. See Differences between protocol and review.
We assessed risk of bias using an adapted version of the Cochrane risk of bias tool (Higgins 2011). Our adapted risk of bias tool is similar to, and was informed by, the one used in a recently published Cochrane systematic review (Iheozor‐Ejiofor 2015). We assessed the following seven bias domains: sampling, confounding, reliability/validity of outcome measures, blinding of outcome assessment, representativeness of sample of underlying population, risk of selective outcome reporting and other sources of bias.
Two review authors (AB and LM, with the assistance of a research assistant (non‐author)) independently assessed risk of bias (high, low, unclear) for each bias domain for each initiative. Risk of bias assessment was based on information obtained from multiple, diverse materials (e.g. scientific journal article, government report or website, country questionnaire) for each data point. Assessment for each bias domain was based on the worst (highest risk of bias) rating, across data points. For example, for the sampling domain, if an initiative was assessed as having high risk of bias for one data point and low risk of bias for the other data point, the overall assessment for the sampling domain for that initiative assigned high risk of bias.
To assign a summary risk of bias assessment for an initiative (i.e. across all domains), the procedure is to assign low risk of bias overall when risk of bias is low for all domains, unclear risk of bias overall when risk of bias is unclear for one or more domains, and high risk of bias overall when risk of bias for one or more domains is high. However, because all of our interventions had at least one domain rated as having high risk of bias (and thus was scored as having high risk of bias overall), we sought a way to capture variation in methodological quality across our included studies. Accordingly, we computed the proportion of bias domains (number out of 7) scored as high or uncertain risk for each intervention.
We rated the overall quality of evidence using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) framework (GRADE n.d.), which is based on five considerations: risk of bias, imprecision, inconsistency, indirectness and publication bias. We assigned four possible GRADE ratings: high, moderate, low and very low. Observational studies start at a GRADE rating of low, which may be increased or decreased. The grade may be decreased by one or (if very serious) two levels in the following circumstances: serious or very serious limitations to study quality; important inconsistency; some or major uncertainty about directness; imprecise or sparse data; or high probability of reporting bias. The grade may be increased in the following circumstances: strong evidence of association based on consistent evidence from two or more observational studies, with no plausible confounders (+1); very strong evidence of association based on direct evidence with no major threats to validity (+2); evidence of a dose‐response gradient (+1); or all plausible confounders with reduced effect (+1) (GRADE n.d.).
Measures of treatment effect
We have made minor changes to this section. See Differences between protocol and review.
Two review authors (AB and LM) collaboratively conducted data entry.
For analysis, we included estimates of daily average sodium intake obtained by any method (e.g. dietary survey, urine sample). We converted reported estimates into daily salt intake in grams per day with standard deviation (if not already provided in that format), when possible. We based analyses on estimates from comparable measurement tools (i.e. dietary survey at both time points, or urine sample at both time points).
We calculated overall impact based on mean change in salt intake (grams/d) from pre‐intervention to post‐intervention. We examined differential impact by sex on the basis of mean change in salt intake (grams/d) from pre‐intervention to post‐intervention, for men and women separately.
We intended to examine differential impact by other axes of social inequality based on PROGRESS indicators (place of residence, race/ethnicity, occupation, gender, religion, education, social capital, socio‐economic position); however, the data did not permit this.
When multiple data points were available for an initiative, we based analysis of impact on the pre‐intervention data point closest in time to the start year of the intervention, and the post‐intervention data point farthest away in time from the start year of the initiative. As a sensitivity check, we re‐ran analysis of impact using alternative post‐intervention data points, along with alternative pre‐intervention data points, when available.
Unit of analysis issues
Unit of analysis issues were not relevant to this review because of the nature of eligible studies. However, review authors may need to consider unit of analysis issues in future iterations of the review; for example, if eligible cluster‐randomised controlled trials are identified.
Dealing with missing data
This section is the same as in the protocol (McLaren 2013).
When overall estimates (for the full population) were not provided, we calculated them (when possible) using other information (e.g. using data reported for men and women separately to compute an overall estimate). When this was not possible, we contacted study authors or country contacts in an attempt to obtain the missing information. When we could not obtain missing data, despite these efforts, we documented this on our data extraction and risk of bias form.
Assessment of heterogeneity
This section is substantively the same as in the protocol (McLaren 2013).
We conducted statistical tests for heterogeneity (I2) to determine whether a meta‐analysis was feasible. We considered clinical heterogeneity (i.e. related to the populations, interventions, comparators and outcomes framework (PICO)) and heterogeneity related to study design.
Assessment of reporting biases
This section is substantively the same as in the protocol (McLaren 2013)
We undertook extensive efforts to ensure a comprehensive search, specifically, a grey literature search that cast a wide net, consultation with experts in the field and direct contact with individuals engaged in national sodium reduction efforts worldwide (see Searching other resources). We anticipated that the comprehensiveness of our search process and the significant proportion of grey literature resources obtained (reports, websites, personal contacts) would reduce the likelihood of publication bias.
Nonetheless, we also created a funnel plot to examine possible reporting biases in keeping with the recommendation to do so if more than 10 interventions are included (Higgins 2011).
Data synthesis
We have made changes to these three sections: Data synthesis, Subgroup analysis and investigation of heterogeneity, Sensitivity analysis (see Differences between protocol and review).
We based the primary analysis on all included studies (for which required information was not missing), regardless of risk of bias.
We used Review Manager 5.3 to calculate mean change in salt intake (grams/d) from pre‐intervention to post‐intervention. See Data and analyses.
Subgroup analysis and investigation of heterogeneity
We intended to examine differences in overall impact by type(s) of intervention activities (see Description of the intervention). However, we could not do this because most initiatives involved more than one intervention activity. However, the pool of initiatives did vary in the extent to which they included activities of a more structural nature, as we have conceptualised it (e.g. food product reformulation, food procurement policy in specific settings), with some countries providing some structural activities and others providing none. Therefore, we examined separately the subset of interventions that included some activities of a structural nature.
We intended to examine differences by economic status of country (e.g. high vs low‐middle) and by duration of the initiative (see Differences between protocol and review). However, the small number of studies identified overall and limited variation amongst them on these dimensions (see Included studies below) precluded these subgroup analyses.
Sensitivity analysis
For initiatives with multiple available data points, we based the analysis of impact on the pre‐intervention data point closest in time to the start year of the intervention, and the post‐intervention data point farthest away in time from the start year of the initiative. As a sensitivity check, we re‐ran analyses of impact using alternative post‐intervention data points, along with alternative pre‐intervention data points, when available.
The data did not permit sensitivity analysis based on other dimensions (e.g. risk of bias).
Presentation of main results
We presented results and overall quality of the evidence (GRADE n.d.) in Table 1.
Research ethics board review
We secured research ethics board approval for this study from the Conjoint Health Research Ethics Board at the University of Calgary (Ethics ID E‐24264). Regarding country questionnaires, we informed programme leaders of the purpose of the study through an introductory email sent with the questionnaire; consent for use of the information as part of the study was conveyed through return of the questionnaire. The University of Sydney Human Research Ethics Committee granted approval for the questionnaire portion of this work (#14923).
Results
Description of studies
Results of the search
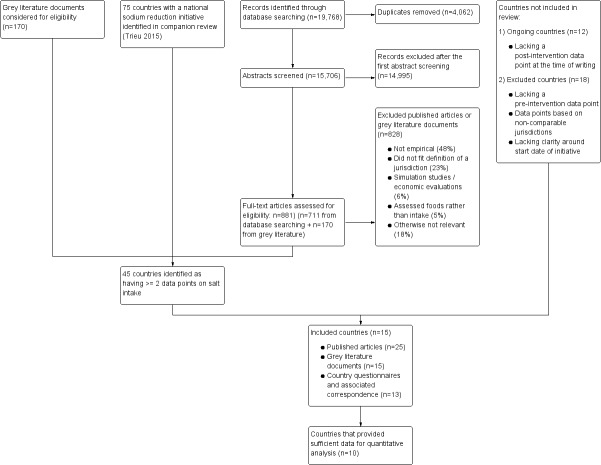
We identified 15,706 unique records (19,768 total records) through the database search (conducted in December 2013 and updated in January 2015), of which 14,995 were eliminated as irrelevant upon screening of titles/abstracts (leaving 711 retained). The grey literature search yielded 170 documents.
We assessed 881 full‐text documents/sources (711 from the published literature + 170 from the grey literature) for eligibility. We eliminated 828 of these. Although we eliminated many documents for multiple reasons, the approximate breakdown by main reason was as follows: not empirical (e.g. commentaries, letters), 48%; did not fit our definition of a jurisdiction (e.g. non‐governmental regions such as communities), 23%; simulation studies (e.g. predicted impact of interventions), 6%; assessed salt content of foods rather than individual salt intake, 5%; otherwise not relevant, 18%.
At that point, we considered the 75 countries that had been identified in our companion review (Trieu 2015) for possible inclusion in this review. We identified that 45 of the 75 countries had two or more data points, and thus were potentially eligible for inclusion in our review. We excluded 18 of these 45 for one or more of three reasons: (1) The country lacked a pre‐intervention data point (i.e. lacked a data point that preceded the start year of the initiative); (2) existing data points were based on non‐comparable jurisdictions (e.g. one national data point and one provincial or regional data point); (3) the start date of the initiative remained unclear, despite efforts to clarify the date. We classified another 12 countries as "ongoing" because, at the time of writing, they lacked a post‐intervention data point (see Characteristics of ongoing studies). For countries designated as excluded or ongoing owing to missing or non‐comparable data points, we made efforts to locate useable data points (e.g. contacted country contacts, searched national health ministry or statistics agency websites, in addition to performing our comprehensive literature search) before finalizing the designation as excluded or ongoing.
We ultimately included 15 initiatives (countries). All initiatives were national in scope. Key documentation for those 15 countries consisted of 25 published articles, 15 grey literature documents and 13 country questionnaires and associated correspondence.
It is important to note that in many instances, we did not evaluate the impact of an initiative by relying on a single research article, but rather we pieced information together from several discrete materials, including published articles, grey literature documents and country questionnaires and associated correspondence. Accordingly, we deemed it necessary to treat the country or initiative as the unit of analysis. For each initiative, we identified one main publication to be used in in‐text citations throughout the Results and Discussion sections of the review. The main publication is the one that, in our view, provides the most information about that initiative. However, the main publication usually is not comprehensive, and for a more thorough understanding of each initiative, we recommend that all corresponding documents should be consulted.
We have presented results of the search in Figure 3.
3.
Flow diagram.
Included studies
Description of included initiatives
We have described the 15 included countries (15 national initiatives) in the Characteristics of included studies tables. The initiative in the United Kingdom counts as one initiative, but because it has been evaluated through data for England only (Millett 2012), for Scotland only (Scottish Centre for Social Research 2011) and for Great Britain as a whole (Wyness 2012), we have prepared three tables to describe it. The total sample size for the 15 initiatives exceeds 260,000 participants. Because many of the initiatives include multiple samples and subsamples (e.g. full dietary survey vs urine sample; full sample vs working‐age subsample), computing the precise total sample size for the 15 initiatives is not a straightforward process. Our analyses (see later) are based on a subset of initiatives, and on a subset of data points within those initiatives. We have included in the Characteristics of included studies table all data points that we identified, including those that were not eligible for analysis.
For Finland (Laatikainen 2006), our comparisons are based on estimates for the Kuopio region. The Finland national sodium reduction initiative began in the early 1970s in North Karelia, and after a five‐year pilot phase was extended to other regions (Puska 2008‐ see Finland). Because our earliest data point for that country was 1979, Kuopio was the only region that satisfied our requirement of at least one comparable data point pre‐initiative and post‐initiative.
The included studies are diverse in terms of settings and interventions, as we have described in the following sections.
Twelve of the 15 countries are classified by the World Bank as 'high‐income', and three (China Du 2014, Thailand Supornsilaphachai 2013, and Turkey Erdem 2010) as 'upper‐middle‐income'. As reported in our companion review (Trieu 2015), national sodium reduction efforts have been identified in countries representing all of the income categories of the World Bank. However, we have included in this review none of the initiatives provided in 'lower‐middle‐income' or 'low‐income' categories because we determined that they were in planning stages (i.e. no substantive activity at the time of writing), or because we found limitations such as no pre‐intervention data.
Of the six World Health Organization regions, four are represented in our review: Europe (Austria ‐ Austria country questionnaire 2014‐2015, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, Turkey ‐ Erdem 2010, United Kingdom ‐ Millett 2012Wyness 2012Scottish Centre for Social Research 2011); Western Pacific (China ‐ Du 2014, Japan ‐ Udagawa 2008, New Zealand ‐ New Zealand Ministry for Primary Industries); the Americas (Canada ‐ McLaren 2014, United States of America ‐ Pfeiffer 2014); and South‐East Asia (Thailand ‐ Supornsilaphachai 2013). Although our companion review (Trieu 2015) identified national sodium reduction efforts in all six regions, we have included no initiatives from the African or Eastern Mediterranean regions in this review because we determined that they were in planning stages (i.e. no substantive activity at the time of writing), or because we found limitations such as no pre‐intervention data.
We identified the intervention activities for each initiative and classified them as aligning with the intervention types listed under Description of the intervention. It is important to note that we made these classifications on the basis of substantive activities that were under way during the time frame (data points) considered in this review. In some cases (e.g. Canada ‐ McLaren 2014, Japan ‐ Udagawa 2008), other substantive activities have been initiated more recently (e.g. working with industry towards food reformulation) and were not captured within available data points. Updates of this review will need to consider the evolution of some initiatives over time, as additional post‐intervention data points become available.
With this in mind, we have classified initiatives as follows. Most initiatives (12/15) included multiple (more than one) intervention activities. The United Kingdom (Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012) initiative included five intervention activities, and initiatives in four countries (Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, Netherlands ‐ Hendriksen 2013, Thailand ‐ Supornsilaphachai 2013) included four activities. Three countries (Canada ‐ McLaren 2014, China ‐ Du 2014, Japan ‐ Udagawa 2008) were characterised as having (during the time frame of available data) single‐component initiatives, which in all cases consisted of public information/education campaigns.
Initiatives in all 15 countries included public information/education campaigns. Other intervention types, by frequency of occurrence, consisted of food product reformulation (this included structured voluntary efforts; see Appendix 1) (Austria ‐ Austria country questionnaire 2014‐2015, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, Netherlands ‐ Hendriksen 2013, New Zealand ‐ New Zealand Ministry for Primary Industries, Switzerland ‐ Chappuis 2011, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012); food procurement policy in specific settings (Austria ‐ Austria country questionnaire 2014‐2015, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012); on‐package nutrition labelling (Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, Ireland ‐ Perry 2010, Netherlands ‐ Hendriksen 2013, New Zealand ‐ New Zealand Ministry for Primary Industries, Thailand ‐ Supornsilaphachai 2013, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014); and restrictions on marketing to children (United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012). No initiatives included pricing strategies (e.g. taxation, subsidisation).
Overall, 11 of the 15 initiatives could be considered as multi‐component and incorporating activities of a structural nature; the remaining four initiatives (Canada ‐ McLaren 2014, China ‐ Du 2014 , Japan ‐ Udagawa 2008, United States of America ‐ Pfeiffer 2014) were less structural and included fewer (one or two) activities.
In terms of the start year of initiatives, we must note that identifying a clear start date was not always a straightforward task because the activities involved in developing and implementing a national sodium reduction initiative are complex and evolve over time. From the best information we could gather, we determined that the start year of the initiatives in our review ranged from 1979 (Finland ‐ Laatikainen 2006) to 2011 (Austria ‐ Austria country questionnaire 2014‐2015, Turkey ‐ Erdem 2010). Most initiatives started relatively recently; only three started before the year 2000 (Canada ‐ McLaren 2014, Finland ‐ Laatikainen 2006, United States of America ‐ Pfeiffer 2014), and 12 started in the year 2000 or later (France ‐ Dubuisson 2010 and Japan ‐ Udagawa 2008 (2001), Ireland ‐ Perry 2010 and United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012 (2003), New Zealand ‐ New Zealand Ministry for Primary Industries (2005), China ‐ Du 2014 and Thailand ‐ Supornsilaphachai 2013 (2006), Denmark ‐ Denmark country questionnaire 2014‐2015 and Switzerland ‐ Chappuis 2011 (2008), Austria ‐ Austria country questionnaire 2014‐2015 and Turkey ‐ Erdem 2010 (2011)).
We must note that in some countries, where efforts related to sodium reduction had been ongoing for several years, we applied discretion in selecting a prominent event/effort that could be conceptualised as the start of the initiative. For example, in the United States (Pfeiffer 2014), advice to reduce salt intake to less than 6 grams/d has been provided consistently since the 1980s, and the Nutrition Labeling and Education Act of 1994 specified inclusion of the daily value of < 2400 mg of sodium as part of the new nutrition label. Thus, we assigned a start year of the United States intervention as late 1980s to early 1990s (Pfeiffer 2014). Other efforts in the United States, at national, state and municipal levels, have been made since the time that we defined to represent the start of the intervention. Similarly, in Canada (McLaren 2014), we identified the beginning of that country's national sodium reduction initiative as a major revision to the Food Guide, which appeared in 1982 and included a moderation statement about salt, even though other activities have occurred since then, such as establishment in 2007 of the national Sodium Working Group (SWG 2010) and the requirement that pre‐packaged foods contain nutrition labelling (http://www.hc‐sc.gc.ca/fn‐an/label‐etiquet/nutrition/index‐eng.php). Data are not currently available to permit evaluation of the national impact of these latter initiatives in Canada (i.e. no national post‐intervention data point), but we expect that these data will become available for inclusion in a later update of this review.
The study designs represented in our review include uncontrolled pre‐post design and open cohort design. Most (n = 14/15) initiatives were evaluated via an uncontrolled pre‐post design (Austria ‐ Austria country questionnaire 2014‐2015, Canada ‐ McLaren 2014, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, Japan ‐ Udagawa 2008, Netherlands ‐ Hendriksen 2013, New Zealand ‐ New Zealand Ministry for Primary Industries, Switzerland ‐ Chappuis 2011, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014). One initiative (China ‐ Du 2014) was evaluated via an open cohort design. Some initiatives had multiple pre‐intervention and post‐intervention data points (thereby fitting the definition of an interrupted time series design) but were classified as uncontrolled pre‐post because, once comparability of jurisdiction and measurement method was taken into account, only one useable pre‐intervention and/or post‐intervention data point remained.
Our primary, and only, outcome variable was dietary sodium consumption, assessed by any measure of salt/sodium intake.
Across all data points identified for each initiative (see Characteristics of included studies and Table 2 through Table 3), we observed a variety of measures: 24‐hour dietary recall (Austria ‐ Austria country questionnaire 2014‐2015, Canada ‐ McLaren 2014, China ‐ Du 2014, Netherlands ‐ Hendriksen 2013, New Zealand ‐ New Zealand Ministry for Primary Industries), 48‐hour dietary recall (Finland ‐ Laatikainen 2006), seven‐day food record or diet diary (Denmark ‐ Denmark country questionnaire 2014‐2015, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012), four‐day food record (Ireland ‐ Perry 2010), food frequency questionnaire (Ireland ‐ Perry 2010), unspecified "nutritional intake survey" (Japan ‐ Udagawa 2008) and "dietary survey" (Thailand ‐ Supornsilaphachai 2013), spot urine (Denmark ‐ Denmark country questionnaire 2014‐2015, Ireland ‐ Perry 2010, New Zealand ‐ New Zealand Ministry for Primary Industries, Switzerland ‐ Chappuis 2011, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014), 24‐hour urine (Finland ‐ Laatikainen 2006, Ireland ‐ Perry 2010, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012). New Zealand used a Total Diet Study method (see references under New Zealand), which involved identifying and purchasing retail foods commonly consumed by the population and preparing them as for usual consumption on the basis of which population estimates of nutrients (including sodium) were calculated.
1. Summary of estimates, all data points ‐ AUSTRIA.
| Data point 1* | Data point 2* | |
| Data source | 2008 Austrian Study on Nutritional Status | 2012 Austrian Study on Nutritional Status |
| Overall estimate – as originally reported | Mean salt intake: 8.3 grams/d, SD = 3.53 (95% CI 8.2 to 8.5) | Mean salt intake: 8.15 grams/d, SD = 2.99 (95% CI 7.85 to 8.45) |
| Overall estimate – revised for comparability | See above | See above |
| Measurement tool | 24‐Hour dietary recall | Two 24‐hour dietary recalls |
| Sample size | n = 2123 | n = 380† |
| Progress indicators available | Gender | Gender |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
†This number is based only on the number of adults in the sample, so it is comparable with the estimate from 2008 (i.e. kids and elderly were not considered)
2. Summary of estimates, all data points ‐ United States.
| Data point 1* | Data point 2 | Data point 3* | |
| Data source | 1988‐1994 NHANES |
2003‐2006 NHANES |
2010 NHANES |
| Overall estimate – as originally reported | Crude geometric mean sodium intake: 3280 milligrams/d, SD = 83.3 (95% CI 3277.64 to 3282.34) |
Crude geometric mean sodium intake: 3270 milligrams/d, SD = 101 (95% CI 3267.13 to 3272.87) |
Crude geometric mean sodium intake: 3400 milligrams/d, SD = 87.6 (95% CI 3396.18 to 3403.82) |
| Overall estimate – revised for comparability | Crude geometric mean salt intake: 8.34 grams/d (95% CI 7.92 to 8.75) | Crude geometric mean salt intake: 8.31 grams/d (95% CI 7.97 to 8.65) | Crude geometric mean salt intake: 8.64 grams/d (95% CI 8.21 to 9.08) |
| Measurement tool | Estimated 24‐hour urine | Estimated 24‐hour urine | Estimated 24‐hour urine |
| Sample size | n = 1249 | n = 1235 | n = 525 |
| Progress indicators available | Gender, race‐ethnicity | Gender, race‐ethnicity | Gender, race‐ethnicity |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
Included studies also varied in terms of reporting of information on study funding sources. Of the 15 included studies, seven provided information on study funding sources for all data points. Of those seven studies, six reported non‐industry funding (Canada ‐ McLaren 2014, France ‐ Dubuisson 2010, Japan ‐ Udagawa 2008, Netherlands ‐ Hendriksen 2013, New Zealand ‐ New Zealand Ministry for Primary Industries, United States ‐ Pfeiffer 2014), and one reported industry and non‐industry funding (Ireland ‐ Perry 2010). The remaining eight studies did not provide information on funding sources for one or more data point(s). Amongst those eight studies, authors of two (China ‐ Du 2014, Switzerland ‐ Chappuis 2011) declared no conflicts of interest, and authors of the other six (Austria ‐ Austria country questionnaire 2014‐2015, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012) reported no conflicts of interest for one or more data point(s). The limited amount of information on funding and conflicts of interest reflects, at least in part, the fact that we drew much of our material from grey literature rather than from peer‐reviewed literature.
Description of information on differential impact of initiatives
We recorded axes of stratification (inequity) considered in all initiatives, using PROGRESS as a guide (place of residence (e.g. urban/rural), race/ethnicity, occupation, gender, religion, education, socio‐economic position, social capital).
Across all data points for all initiatives, a variety of axes of inequity were considered: place of residence (China ‐ Du 2014, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Switzerland ‐ Chappuis 2011, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012), race/ethnicity (United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014), occupation (France ‐ Dubuisson 2010), gender (all except Thailand ‐ Supornsilaphachai 2013), education (Canada ‐ McLaren 2014, China ‐ Du 2014, Finland ‐ Laatikainen 2006, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012), social class (Ireland ‐ Perry 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012). Income was considered in the initiatives for Canada (McLaren 2014) and China (Du 2014). All initiatives except Thailand (Supornsilaphachai 2013) considered one or more axes of stratification at one or more time points.
Unfortunately, for the most part, axes of stratification were not considered consistently across surveys (i.e. they were considered at one data point but not another). As a result, assessment of equity of impact was possible for only five initiatives: Canada ‐ McLaren 2014 (education, income); China ‐ Du 2014 (place of residence, education, income); Finland ‐ Laatikainen 2006 (place of residence, education); United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012 (race/ethnicity, social class), United States of America ‐ Pfeiffer 2014 (race/ethnicity). Further, because these indicators have different meanings and are measured differently in different countries, they do not lend themselves to quantitative synthesis across countries. Therefore, we have considered them individually and qualitatively in the review text that follows.
The only exception is sex ("g"ender in the PROGRESS framework), for which comparable pre‐initiative and post‐initiative information was available for nine countries: Austria ‐ Austria country questionnaire 2014‐2015, Canada ‐ McLaren 2014, China ‐ Du 2014, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, United Kingdom (England ‐ Millett 2012, Great Britian ‐ Wyness 2012, Scotland ‐ Scottish Centre for Social Research 2011), United States of America ‐ Pfeiffer 2014.
Excluded studies
Of the 45 initiatives that contained at least two data points on the basis of our companion review (Trieu 2015) and were assessed closely for eligibility, we excluded 18 (see Characteristics of excluded studies table). Reasons for exclusion included the following: no useable pre‐intervention data point (Argentina, Australia, Barbados, Indonesia, Italy, Portugal, Slovakia); lack of clarity regarding start year of the initiative, despite efforts to clarify (Bangladesh, Iceland, Israel, Singapore, Uruguay); and data points based on non‐comparable jurisdiction and/or measurement methods (Croatia, Malaysia, Poland, Slovenia, Sri Lanka, Vietnam). In cases for which more than one reason led to exclusion, we have listed reasons judged to be the most prominent.
Ongoing studies
We classified initiatives in 12 countries (Belgium, Brazil, Bulgaria, Chile, Costa Rica, Fiji, Hungary, Lithuania, Mongolia, Norway, Republic of South Korea, Sweden) as ongoing (see Characteristics of ongoing studies table) because, although a start date was clearly defined and one or more pre‐intervention data points were given, no post‐intervention data point was available at the time of writing.
Risk of bias in included studies
We have presented under Characteristics of included studies our judgements on each risk of bias domain for each included initiative and have provided a summary in Figure 4 (note that the United Kingdom is counted as one initiative despite three available sets of evaluations). We characterised all 15 initiatives as having high risk of bias overall because they included one or more domains characterised as presenting high risk of bias. The overall high risk of bias reflects the study designs used, which in all cases were uncontrolled. Although use of uncontrolled designs is understandable given the nature of the intervention (government initiated; evaluated as a natural experiment), we have scored those designs as presenting high risk of bias because of the difficulty involved in ruling out alternative explanations for observed effects. Accordingly, we rated all studies as having high risk of bias on the basis of the confounding domain.
4.
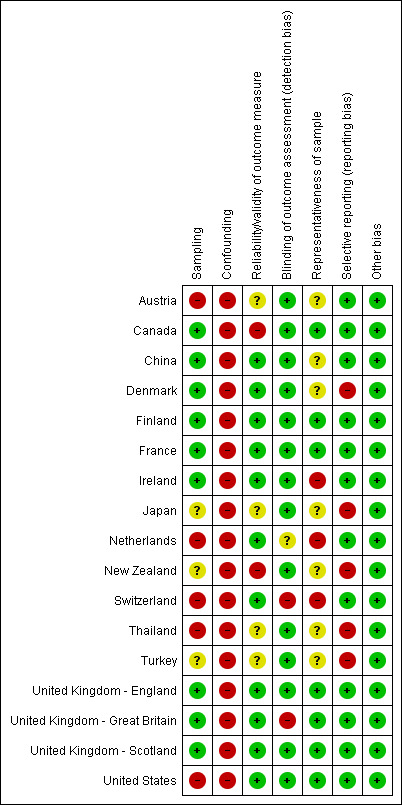
Risk of bias summary: review authors' judgements about each risk of bias item for each included initiative.
As all of our included studies had a summary rating of high risk of bias overall, we sought a means of capturing variations in methodological quality amongst them. We elected to characterise each initiative in terms of the proportion of bias domains scored as 'high' or 'uncertain', out of a total of seven domains (sampling, confounding, reliability/validity of outcome measure, blinding of outcome assessment, representativeness of sample of underlying population, risk of selective outcome reporting, other bias). Using this metric, we determined that the best studies in our sample were Finland (Laatikainen 2006) and France (Dubuisson 2010), which we scored as having 'high' or 'uncertain' risk of bias in only one of seven bias domains. We assigned high quality to the United Kingdom (Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012) on the basis of the proportion metric, which we scored as presenting 'high' or 'uncertain' risk of bias on one of seven domains according to evaluations in England (Millett 2012) and Scotland (Scottish Centre for Social Research 2011), and on two of seven domains according to evaluations of Great Britain as a whole (Wyness 2012) (for an overall metric of 2/7). The worst studies in our sample were Japan (Udagawa 2008), New Zealand (New Zealand Ministry for Primary Industries), Thailand (Supornsilaphachai 2013) and Turkey (Erdem 2010), all of which we scored as having 'high' or 'uncertain' risk of bias on five of seven domains (we scored no studies as having 'high' or 'uncertain' risk of bias on six or seven of seven domains). The remaining countries fell in between, scoring 'high' or 'uncertain' risk of bias on two of seven bias domains (Canada ‐ McLaren 2014, China ‐ Du 2014, Ireland ‐ Perry 2010, United States of America ‐ Pfeiffer 2014), or on three of seven (Denmark ‐ Denmark country questionnaire 2014‐2015) or four of seven bias domains (Austria ‐ Austria country questionnaire 2014‐2015, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011).
We next present a summary of risk of bias by domain. See Characteristics of included studies and Included studies sections for details and sources. We must acknowledge that many of our studies had important methodological strengths, including large, nationally representative samples, rigorous measurement of dietary sodium intake and use of existing survey or administrative data (not collected for the purpose of evaluating the initiative), which reduces the likelihood that outcomes are biased by knowledge of the initiative.
Sampling
We judged that seven of the 15 studies had low risk of bias on sampling, given their use of a random (simple or complex) sampling strategy (Canada ‐ McLaren 2014, China ‐ Du 2014, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012). We scored five studies (Austria ‐ Austria country questionnaire 2014‐2015, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, Thailand ‐ Supornsilaphachai 2013, United States of America ‐ Pfeiffer 2014) as having high risk of bias on sampling because they reported full or partial use of non‐random or convenience sampling. For the remaining three studies, information was insufficient to reveal the sampling method used for one or more data points (Japan ‐ Udagawa 2008, Turkey ‐ Erdem 2010), or, in the case of New Zealand (New Zealand Ministry for Primary Industries), this domain was not applicable because no sampling per se was performed (see New Zealand and Characteristics of included studies table).
Confounding
We scored all 15 studies as having high risk of bias on confounding because they used an uncontrolled study design.
Reliability/Validity of outcome measure
Methods of outcome measurement included dietary surveys (e.g. 24‐hour recall) and urinary estimates (spot urine samples, 24‐hour urine samples). In the light of significant expense and burden associated with 24‐hour urine estimates for large population‐based national samples, particularly in lower‐income and middle‐income countries, we accommodated spot urine and survey‐based methods in this literature.
Although 24‐hour urine is widely viewed as the most accurate method, all methods have both strengths and limitations (McLean 2014). For example, although some dietary surveys (e.g. 24‐hour recall using an automated multi‐pass method) have shown strong positive correlation with 24‐hour urine estimates, dietary surveys may mis‐estimate or under‐estimate sodium consumption as the result of mis‐reporting or under‐reporting and challenges associated with accurately quantifying sodium in recipes. Dietary surveys are unique amongst measurement methods in their ability to identify sources of sodium, which may be useful for informing interventions (e.g. identifying groups of foods for a possible reformulation policy). Spot urinary estimates offer pragmatic advantages (collected during a single encounter) but may not accurately reflect 24‐hour urinary sodium excretion. However, methods (e.g. formulae) have been developed to improve the correspondence between spot and 24‐hour samples, and these methods may suffice for producing reasonably accurate population‐level (but not individual‐level) estimates. Finally, although it is widely viewed as the most accurate method (approximately 90% of ingested sodium is excreted in the urine over a 24‐hour period, under 'normal' conditions of climate and physical activity), 24‐hour urine suffers from potential bias associated with low response rates (due to burden), under‐collection and limitations of methods available to accurately identify incomplete samples (McLean 2014). Accordingly, our risk of bias judgement for this domain was not based solely on the method used. Rather, all methods in studies reviewed could potentially score as introducing low risk of bias in this domain; to do so, convincing text was needed to show that the tool was administered in a careful and systematic manner and/or that reliability and validity of the tool were known from other cited literature or had been assessed within the included study.
On this basis, we judged nine of 15 studies as having low risk of bias for the reliability/validity of outcome measures (China ‐ Du 2014, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, and United States of America ‐ Pfeiffer 2014). Two countries (Canada ‐ McLaren 2014, New Zealand ‐ New Zealand Ministry for Primary Industries) were scored as having high risk of bias in this domain. In Canada (McLaren 2014), although a dietary survey was used at both time points, study authors mentioned that these surveys were not directly comparable because of changes to survey content and administration over time. New Zealand (New Zealand Ministry for Primary Industries) also received a score of high in this domain because the reliability/validity of the tools used to determine salt intake at both time points was not discussed. In the remaining four studies (Austria ‐ Austria country questionnaire 2014‐2015, Japan ‐ Udagawa 2008, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010), information provided on the measurement tool was insufficient to permit review authors to discern reliability, validity and comparability over time.
Blinding of outcome assessment
We scored studies for which pre‐existing data were used to evaluate the intervention as having low risk of bias in this domain on the basis of reasoning that absence of a direct connection between the initiative and the data constituted a form of blinding. We also scored studies in which data were collected for the purpose of evaluating the intervention but blinding was explicitly incorporated as having low risk of bias in this domain. Twelve studies satisfied the criteria for low risk of bias (Austria ‐ Austria country questionnaire 2014‐2015, Canada ‐ McLaren 2014, China ‐ Du 2014, Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, Japan ‐ Udagawa 2008, New Zealand ‐ New Zealand Ministry for Primary Industries, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010, United States of America ‐ Pfeiffer 2014). For the Netherlands (Hendriksen 2013), information about the data was insufficient to reveal risk of bias. We scored Switzerland (Chappuis 2011) as having high risk of bias in this domain. For the United Kingdom, evaluations for England (Millett 2012) and Scotland (Scottish Centre for Social Research 2011) were scored as showing low risk of bias in this domain, but the evaluation for Great Britain (Wyness 2012) was scored high (because although 24‐hour urine was used, investigators gave no explicit indication that blinding was incorporated) for an overall score of high risk of bias for the United Kingdom (Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012).
Representativeness of sample of the underlying population
We judged five initiatives (Canada ‐ McLaren 2014, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014) as having low risk of bias in this domain on the basis of efforts, such as application of sampling weights or demonstrated similarity between sample data and census data, to show that the sample resembled the underlying population. We scored Ireland (Perry 2010), Netherlands (Hendriksen 2013) and Switzerland (Chappuis 2011) as having high risk of bias in this domain on the basis of demonstrated differences between the sample and the underlying population. The remaining seven countries provided insufficient information to permit a judgement (Austria ‐ Austria country questionnaire 2014‐2015, China ‐ Du 2014, Denmark ‐ Denmark country questionnaire 2014‐2015, Japan ‐ Udagawa 2008, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010) or, in the case of New Zealand (New Zealand Ministry for Primary Industries), this domain was not applicable because no sampling per se was involved.
Risk of selective outcome reporting
We scored 10 initiatives (Austria ‐ Austria country questionnaire 2014‐2015, Canada ‐ McLaren 2014, China ‐ Du 2014, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014) as having low risk of bias in this domain because investigators reported outcome data in a useable format (i.e. means along with estimates of variance (standard deviation, standard error or 95% confidence interval)). We scored the remaining five initiatives (Denmark ‐ Denmark country questionnaire 2014‐2015, Japan ‐ Udagawa 2008, New Zealand ‐ New Zealand Ministry for Primary Industries, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010) as having high risk of bias in this domain because they did not provide estimates of variance for one or more data points, and we were unable to obtain that information through other sources or through contact with study authors.
Other sources of bias
We scored all 15 initiatives as having low risk of bias in this domain, largely because many potentially significant sources of bias are captured in the 'confounding' domain, in which all initiatives were scored as having high risk of bias.
Effects of interventions
See: Table 1
A total of 15 initiatives met the inclusion criteria. Summary statistics for all data points (reported values, as well as values converted to sodium in grams per day) are shown in Table 2; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; Table 13; Table 14; Table 15; Table 16; Table 17; Table 18; and Table 3. Note that we have provided 17 tables for 15 initiatives because separate evaluations of the United Kingdom initiative were available for Great Britain as a whole (Wyness 2012), for England only (Millett 2012) and for Scotland only (Scottish Centre for Social Research 2011).
3. Summary of estimates, all data points ‐ CANADA.
| Data point 1* | Data point 2* | |
| Data source | 1970‐1972 Nutrition Canada Survey | 2004 Canadian Community Health Survey |
| Overall estimate – as originally reported | Mean sodium intake: 2403.9 milligrams/d, SD = 1362.5 | Mean sodium intake: 3057 milligrams/d, SD = 606.2 |
| Overall estimate – revised for comparability | Mean salt intake: 6.11 grams/d, SD = 3.46 (95% CI 5.74 to 6.28) | Mean salt intake: 7.77 grams/d, SD = 1.54 (95% CI 7.69 to 7.85) |
| Measurement tool | 24‐Hour dietary recall | 24‐Hour dietary recall |
| Sample size | n = 4540 | n = 10,449 |
| Progress indicators available | Gender, education and income | Gender, education and income |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
4. Summary of estimates, all data points ‐ CHINA.
| Data point 1 | Data point 2 | Data point 3 | Data point 4 | Data point 5 | Data point 6* | Data point 7* | |
| Data source | 1991 China Health and Nutrition Survey | 1993 China Health and Nutrition Survey | 1997 China Health and Nutrition Survey | 2000 China Health and Nutrition Survey | 2004 China Health and Nutrition Survey | 2006 China Health and Nutrition Survey | 2009 China Health and Nutrition Survey |
| Overall estimate – as originally reported | Mean sodium intake: 6.6 grams/d, SD = 3.4 (95% CI 6.52 to 6.68) | Mean sodium intake: 6.6 grams/d, SD = 3.4 (95% CI 6.52 to 6.68) | Mean sodium intake: 6.2 grams/d, SD = 3.5 (95% CI 6.12 to 6.28) | Mean sodium intake: 6.0 grams/d, SD = 3.2 (95% CI 5.93 to 6.07) | Mean sodium intake: 5.2 grams/d, SD = 2.7 (95% CI 5.14 to 5.26) | Mean sodium intake: 5.0 grams/d, SD = 2.8 (95% CI 4.93 to 5.07) | Mean sodium intake: 4.7 grams/d, SD = 2.6 (95% CI 4.64 to 4.76) |
| Overall estimate – revised for comparability | Mean salt intake: 16.76 grams/d (95% CI 16.56 to 16.97) | Mean salt intake: 16.76 grams/d (95% CI 16.56 to 16.97) | Mean salt intake: 15.77 grams/d (95% CI 15.54 to 15.95) | Mean salt intake: 15.24 grams/d (95% CI 15.06 to 15.42) | Mean salt intake: 13.21 grams/d (95% CI 13.06 to 13.36) | Mean salt intake: 12.70 grams/d (95% CI 12.52 to 12.88) | Mean salt intake: 11.94 grams/d (95% CI 11.79 to 12.09) |
| Measurement tool | 3 consecutive 24‐hour dietary recalls | 3 consecutive 24‐hour dietary recalls | 3 consecutive 24‐hour dietary recalls | 3 consecutive 24‐hour dietary recalls | 3 consecutive 24‐hour dietary recalls | 3 consecutive 24‐hour dietary recalls | 3 consecutive 24‐hour dietary recalls |
| Sample size | n = 7337 | n = 6958 | n = 7241 | n = 7940 | n = 7250 | n = 6826 | n = 6932 |
| Progress indicators available | Gender, place of residence, education, income | Gender, place of residence, education, income | Gender, place of residence, education, income | Gender, place of residence, education, income | Gender, place of residence, education, income | Gender, place of residence, education, income | Gender, place of residence, education, income |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
Note: Based on all data points, “sodium intake significantly decreased over time (P‐trend, 0.001, general linear regression models)”
5. Summary of estimates, all data points ‐ DENMARK.
| Data point 1 | Data point 2 | Data point 3 | |
| Data source | 2006 Danish Health | 2008 Danish National Survey of Dietary Habits and Physical Activity | 2010 Danish Health |
| Overall estimate – as originally reported | Median salt intake: 8.93 grams/d | Mean salt intake: 8.5 grams/d, SD = 2.9 (95% CI 8.41 to 8.59) | Median salt intake: 8.27 grams/d |
| Overall estimate – revised for comparability | Same as above | Same as above | Same as above |
| Measurement tool | Spot urine | Food record for 7 consecutive days | Spot urine |
| Sample size | n = 3294 | n = 4431 | n = 1478 |
| Progress indicators available | Gender | Gender | Gender |
underlined text = computed by review authors
Denmark was not included in quantitative synthesis because of missing or unuseable information (e.g. mean, SD, n) at 1 or more data points
6. Summary of estimates, all data points ‐ FINLAND.
| Data point 1* | Data point 2 | Data point 3* | Data point 4 | Data point 5 | Data point 6 | |
| Data source | 1979 North Karelia Kuopio area |
1982 North Karelia Kuopio area |
1987 North Karelia Kuopio area |
2002 North Karelia |
2007 5 regions in Finland |
2012 5 regions in Finland |
| Overall estimate – as originally reported | Mean salt intake (North Karelia): 11.65 grams/d, SD = 4.39
(95% CI 11.28 to 12.02) Mean salt intake (Kuopio area): 11.78 grams/d, SD = 4.72 (95% CI 11.42 to 12.14) |
Mean salt intake (North Karelia): 11.94 grams/d ± 4.62
(95% CI 11.53 to 12.35) Mean salt intake (Kuopio area): 11.59 grams/d, SD = 4.50 (95% CI 11.16 to 12.02) |
Mean salt intake (North Karelia): 10.36 grams/d, SD = 4.46
(95% CI 9.93 to 10.79) Mean salt intake (Kuopio area): 10.63 grams/d, SD = 4.10 (95% CI 10.23 to 11.03) |
Mean salt intake (North Karelia): 8.43 grams/d, SD = 3.19 (95% CI 8.09 to 8.77) | Mean salt intake: 8.0 grams/d | Mean sodium intake: 3.01 grams/d, SD = 1.10 (95% CI 2.95 to 3.07) |
| Overall estimate – revised for comparability | Same as above | Same as above | Same as above | Same as above | Same as above | Mean salt intake: 7.65 grams/d (95% CI 7.49 to 7.80) |
| Measurement tool | 24‐Hour urine | 24‐Hour urine | 24‐Hour urine | 24‐Hour urine | 48‐Hour dietary recall | 48‐Hour dietary recall |
| Sample size | n = 536 (North Karelia) n = 670 (Kuopio area) |
n = 484 (North Karelia) n = 428 (Kuopio area) |
n = 409 (North Karelia) n = 400 (Kuopio area) |
n = 342 (North Karelia) | n = 1576 | n = 1295 |
| Progress indicators available | Gender and education | Gender and education | Gender and education | Gender and education | Gender | Gender, place of residence and education |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
7. Summary of estimates, all data points ‐ FRANCE.
| Data point 1a* | Data point 1b | Data point 2* | |
| Data source | 1998‐1999 Individual and National Food Consumption Surveys |
1998‐1999 Individual and National Food Consumption Surveys |
2006‐2007 Individual and National Food Consumption Surveys |
| Overall estimate – as originally reported | Mean sodium intake: 3145.7 milligrams/d, SD = 1016.4 (95% CI 3090.78 to 3199.42) | Mean sodium intake: 137.40 mmol/d, SD = 101.48 (95% CI 132.22 to 142.58) | Mean sodium intake: 2966.6 milligrams/d ± 922.4 (95% CI 2925.36 to 3007.84) |
| Overall estimate – revised for comparability | Mean salt intake: 8.00 grams/d (95% CI 7.86 to 8.13) | Mean salt intake: 7.97 grams/d (95% CI 7.67 to 8.27) | Mean salt intake: 7.54 grams/d (95% CI 7.44 to 7.65) |
| Measurement tool | 7‐Day open‐ended food record | 7‐Day open‐ended food record | 7‐Day open‐ended food record |
| Sample size | n = 1345 | n = 1474 | n = 1922 |
| Progress indicators available | Gender | Gender | Gender, place of residence and occupation |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
8. Summary of estimates, all data points ‐ IRELAND.
| Data point 1 | Data point 2 | Data point 3* | Data point 4* | Data point 4a | Data point 4b | Data point 5 | |
| Data source | 1997‐1999 North‐South Ireland Food Consumption Survey | 1998 Survey of Lifestyle Attitudes and Nutrition in Ireland | 2002 Survey of Lifestyle Attitudes and Nutrition in Ireland | 2007 Survey of Lifestyle Attitudes and Nutrition in Ireland | 2007 Survey of Lifestyle Attitudes and Nutrition in Ireland | 2007 Survey of Lifestyle Attitudes and Nutrition in Ireland | 2008‐2010 National Adult Nutrition Survey |
| Overall estimate – as originally reported | Mean salt intake: 8.3 grams/d | Mean salt intake: 8.3 grams/d, SD = 3.8 (95% CI 8.21 to 8.39) | Mean salt intake: 8.2 grams/d, SD = 5.9 (95% CI 8.05 to 8.35) | Mean salt intake: 7.85 grams/d, SD = 3.70 (95% CI 7.77 to 7.95) | Mean salt intake: 8.9 grams/d | Mean salt intake: 9.3 grams/d | Mean salt intake: 7.4 grams/d |
| Overall estimate – revised for comparability | Same as above | Same as above | Same as above | Same as above | Same as above | Same as above | Same as above |
| Measurement tool | 7‐Day diet diaries | Food frequency questionnaire | Food frequency questionnaire | Food frequency questionnaire | Spot urine | 24‐Hour urine | 4‐Day semi weighted food record |
| Sample size | n = 1379 | n = 6539 | n = 5992 | n = 9172 | n = 1207 | n = 599 | n = 1500 |
| Progress indicators available | Gender | Gender | Gender | Gender and social class | Gender | Gender | Gender |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
9. Summary of estimates, all data points ‐ JAPAN.
| Data point 1 | Data point 2 | Data point 3 | Data point 4 | Data point 5 | Data point 6 | Data point 7 | Data point 8 | Data point 9 | Data point 10 | |
| Data source | 1997 National Health and Nutrition Survey |
2003 National Health and Nutrition Survey |
2004 National Health and Nutrition Survey |
2005 National Health and Nutrition Survey |
2006 National Health and Nutrition Survey |
2007 National Health and Nutrition Survey |
2008 National Health and Nutrition Survey |
2009 National Health and Nutrition Survey |
2010 National Health and Nutrition Survey |
2012 National Health and Nutrition Survey |
| Overall estimate – as originally reported | Mean salt intake: 13.5 grams/d | Mean salt intake: 11.7 grams/d | Mean salt intake: 11.2 grams/d | Mean salt intake: 11.5 grams/d | Mean salt intake: 11.2 grams/d | Mean salt intake: 11.1 grams/d | Mean salt intake: 10.9 grams/d | Mean salt intake: 10.7 grams/d | Mean salt intake: 10.6 grams/d | Mean salt intake: 10.4 grams/d |
| Overall estimate – revised for comparability | Same as above | Same as above | Same as above | Same as above | Same as above | Same as above | Same as above | Same as above | Same as above | Same as above |
| Measurement tool | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey | Nutritional intake survey |
| Sample size | n = 13,289 | Unknown | n = 8762 | Unknown | Unknown | n = 8885 | Unknown | Unknown | n = 8815 | n = 8247 |
| Progress indicators available | ‐‐ | Gender | Gender | Gender | Gender | Gender | Gender | Gender | Gender | ‐‐ |
underlined text = computed by review authors
Japan was not included in quantitative synthesis because of missing or unuseable information (e.g. mean, SD, n) at 1 or more data points
10. Summary of estimates, all data points ‐ NETHERLANDS.
| Data point 1* | Data point 2 | Data point 3* | |
| Data source | 2006 Cross‐sectional study of adults in Doetinchem |
2007‐2010 National Food Consumption Survey |
2010 Cross‐sectional study of adults in Doetinchem |
| Overall estimate – as originally reported | Mean sodium excretion: 148 mmol/d, SD = 55
(95% CI 141.95 to 154.05) Median salt intake: 8.7 grams/d (IQR 6.7 to 11.0) |
Mean salt intake: 8.45 grams/d | Mean sodium excretion: 148 mmol/d, SD = 58
(95% CI 141.85 to 154.15) Median salt intake: 8.5 grams/d (IQR 6.6 to 10.9) |
| Overall estimate – revised for comparability | Mean salt intake: 8.58 grams/d (95% CI 8.23 to 8.93) | Same as above | Mean salt intake: 8.58 grams/d (95% CI 8.23 to 8.94) |
| Measurement tool | 24‐Hour urine | 2 non‐consecutive 24‐hour recalls | 24‐Hour urine |
| Sample size | n = 317 | n = 2160 | n = 342 |
| Progress indicators available | Gender | Gender | Gender |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
11. Summary of estimates, all data points ‐ NEW ZEALAND.
| Data point 1 | Data point 2a | Data point 2b | Data point 3 | |
| Data source | 2003‐2004 New Zealand Total Diet Study |
2008‐2009 New Zealand Adult Nutrition Survey |
2008‐2009 New Zealand Adult Nutrition Survey |
2009 New Zealand Total Diet Study |
| Overall estimate – as originally reported | N/A | Mean salt intake: 6.37 grams/d | Mean salt intake: 9 grams/d | N/A |
| Overall estimate – revised for comparability | Same as above | Same as above | ||
| Measurement tool | N/A | Multiple pass 24‐hour dietary recall | Spot urine | N/A |
| Sample size | N/A | n = 4721 | Unknown | N/A |
| Progress indicators available | Gender | ‐‐ | ‐‐ | Gender |
underlined text = computed by review authors
New Zealand was not included in quantitative synthesis because of missing or unuseable information (e.g. mean, SD, n) at 1 or more data points
12. Summary of estimates, all data points ‐ SWITZERLAND.
| Data point 1a* | Data point 1b | Data point 2* | |
| Data source | 1984 Representative sample of the Swiss population |
1984 Representative sample of the Swiss population |
2011 Swiss survey on salt intake |
| Overall estimate – as originally reported | Mean salt intake: 8.4 grams/d, SD = 3.6 (95% CI 8.12 to 9.28) | Mean salt intake: 10.3 grams/d, SD = 6.2 (95% CI 9.91 to 10.69) | Mean salt intake: 9.2 grams/d, SD = 3.8 (95% CI 9.01 to 9.39) |
| Overall estimate – revised for comparability | Same as above | Same as above | Same as above |
| Measurement tool | 24‐Hour urine | Spot urine | 24‐Hour urine |
| Sample size | n = 147 | n = 966 | n = 1448 |
| Progress indicators available | None | None | Gender and place of residence |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
13. Summary of estimates, all data points ‐ THAILAND.
| Data point 1 | Data point 2 | Data point 3 | Data point 4 | Data point 5 | |
| Data source | 1960 National Nutrition Survey |
1975 National Nutrition Survey |
2003 National Nutrition Survey |
2008 | 2008‐2009 Fourth Thai National Health Examination Survey |
| Overall estimate – as originally reported | Mean sodium intake: 2.4 grams/d | Mean sodium intake: 2.4 grams/d | Mean sodium intake: 4.0 grams/d | Mean sodium intake: 4.4 grams/d | Mean sodium intake: 3.3 grams/d |
| Overall estimate – revised for comparability | Mean salt intake: 6.10 grams/d | Mean salt intake: 6.10 grams/d | Mean salt intake: 10.16 grams/d | Mean salt intake: 11.18 grams/d | Mean salt intake: 8.38 grams/d |
| Measurement tool | Dietary survey | Dietary survey | Dietary survey (food list recall and food frequency checklist of foods/condiments) | Dietary survey (household survey) | Dietary survey (food list recall and food frequency checklist of foods/condiments) |
| Sample size | Unknown | Unknown | Unknown | Unknown | Unknown |
| Progress indicators available | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ |
Note: A 2007 data point was removed because we did not have enough information to suggest that it was national in scope (i.e. comparable with other data points)
underlined text = computed by review authors
Thailand was not included in quantitative synthesis because of missing or unuseable information (e.g. mean, SD, n) at 1 or more data points
14. Summary of estimates, all data points ‐ TURKEY.
| Data point 1a | Data point 1b | Data point 2 | |
| Data source | 2008 SALTURK 1 |
2008 SALTURK 1 |
2012 SALTURK 2 |
| Overall estimate – as originally reported | Mean salt intake: 16.6 grams/d, SD = 7.3 (95% CI 16.1 to 17.1) | Mean salt intake: 18.01 grams/d | Mean salt intake: 15.0 grams/d |
| Overall estimate – revised for comparability | Same as above | Same as above | Same as above |
| Measurement tool | 24‐Hour urine | Spot urine | 24‐Hour urine |
| Sample size | n = 816 | n = 1970 (total number of eligible participants) | n =925; “657 person (according to urine creatine levels)” |
| Progress indicators available | Gender, place of residence and education level | ‐‐ | ‐‐ |
Note: We believe that the difference between estimates 1a and 1b is that 1a is based on 24‐hour urine and 1b is based on spot urine. The overall conclusion for Turkey does not differ when 1a versus 1b is used
underlined text = computed by review authors
Turkey was not included in quantitative synthesis because of missing or unuseable information (e.g. mean, SD, n) at 1 or more data points
15. Summary of estimates, all data points ‐ U.K. ‐ ENGLAND.
| Data point 1a | Data point 1b* | Data point 2a | Data point 2b | Data point 3a | Data point 3b | Data point 4 | Data point 5a | Data point 5b | Data point 6a | Data point 6b* | Data point 7 | |
| Data source | 2003 Health Survey for England |
2003 Health Survey for England |
2004 Health Survey for England |
2004 Health Survey for England |
2005 Health Survey for England |
2005 Health Survey for England |
2005‐2006 National Diet and Nutrition Survey |
2006 Health Survey for England |
2006 Health Survey for England |
2007 Health Survey for England |
2007 Health Survey for England |
2011 National Diet and Nutrition Survey |
| Overall estimate – as originally reported | Geometric mean salt intake: 5.29 grams/d (95% CI 5.1 to 5.5) | Urinary sodium excretion: 109.03 mmol of sodium/d, SD = 20.41 (95% CI 108.05 to 110.01) |
Geometric mean salt intake: 5.99 grams/d (95% CI 5.9 to 6.1) | Urinary sodium excretion: 111.28 mmol of sodium/d, SD = 19.82 (95% CI 110.55 to 112.01) |
Geometric mean salt intake: 4.80 grams/d (95% CI 4.7 to 4.9) | Urinary sodium excretion: 99.94 mmol of sodium/d, SD = 22.17 (95% CI 99.30 to 100.58) |
Mean salt intake: 9.0 grams/d, SD = 3.7 (95% CI 8.66 to 9.34) |
Geometric mean salt intake: 4.73 grams/d (95% CI 4.7 to 4.8) | Urinary sodium excretion: 97.49 mmol of sodium/d, SD = 20.00 (95% CI 97.07 to 97.91) |
Geometric mean salt intake: 4.55 grams/d (95% CI 4.5 to 4.7) | Urinary sodium excretion: 94.16 mmol of sodium/d, SD =19.39 (95% CI 93.58 to 94.74) |
Mean salt intake: 8.1 grams/d, SD = 5.79 (95% CI 7.85 to 8.35) |
| Overall estimate – revised for comparability | Same as above | Mean salt intake:6.32 grams/d (95% CI 6.27 to 6.38) | Same as above | Mean salt intake: 6.45 grams/d (95% CI 6.41 to 6.50) | Same as above | Mean salt intake: 5.80 grams/d (95% CI 5.76 to 5.83) | Same as above | Same as above | Mean salt intake: 5.65 grams/d (95% CI 5.63 to 5.68) | Same as above | Mean salt intake: 5.46 grams/d (95% CI 5.43 to 5.49) | Same as above |
| Measurement tool | Spot urine | Spot urine | Spot urine | Spot urine | Spot urine | Spot urine | 24‐Hour urine | Spot urine | Spot urine | Spot urine | Spot urine | 24‐Hour urine |
| Sample Size | n = 1668 | n = 1668 | n = 2840 | n = 2840 | n = 4643 | n = 4643 | n = 448 | n = 8844 | n = 8844 | n = 4269 | n = 4269 | n = 547 |
| Progress indicators available | Gender, ethnicity and social class | Gender and place of residence | Gender, ethnicity and social class | Gender and place of residence | Gender, ethnicity and social class | Gender and place of residence | Gender | Gender, ethnicity and social class | Gender and place of residence | Gender, ethnicity and social class | Gender and place of residence | Gender |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
16. Summary of estimates, all data points ‐ U.K. ‐ Great Britain/UK.
| Data point 1a | Data point 1b* | Data point 1c | Data point 1d | Data point 2* | |
| Data source | 2000‐2001 National Diet and Nutrition Survey | 2000‐2001 National Diet and Nutrition Survey | 2000‐2001 National Diet and Nutrition Survey |
2000‐2001 National Diet and Nutrition Survey |
2008 Survey by National Centre for Social Research |
| Overall estimate – as originally reported | Mean sodium intake: 2794.39 milligrams/d, SD = 861.44 (95% CI 2753.76 to 2835.05) | Mean salt intake: 9.53 grams/d, SD = 4.48 (95% CI 9.27 to 9.79) | Median dietary sodium intake: 2611 milligrams/d (IQR = 1243) | Median 24‐hour sodium excretion: 140 mmol/d (IQR = 99.4) | Mean salt intake: 8.64 grams/d, SD = 4.39 (95% CI 8.31 to 8.97) |
| Overall estimate – revised for comparability | Mean salt intake: 7.01 grams/d (95% CI 7.00 to 7.21) | Same as above | Estimated salt intake: 6.5 grams/d | Estimated salt intake: 8.2 grams/d | Same as above |
| Measurement tool | 7‐Day consecutive weighted dietary record | 24‐Hour urine | 7‐Day consecutive weighted dietary record | 24‐Hour urine | 24‐Hour urine |
| Sample size | n = 1724 | n = 1147 | n = 2150 | n = 692 | |
| Progress indicators available | Gender | Gender | Gender, place of residence, education and social class | Gender, place of residence, education and social class | Gender |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
17. Summary of estimates, all data points ‐ U.K.‐Scotland.
| Data point 1* | Data point 2 | Data point 3 | Data point 4* | Data point 5 | |
| Data source | 2003 Scottish Health Survey |
2006 | 2008 Scottish Health Survey |
2009 Scottish Health Survey |
2009 |
| Overall estimate – as originally reported | Mean salt intake: 6.8 grams/d (95% CI 6.5 to 7.1) | Mean salt intake: 9.1 grams/d, SD = 4.1 | Mean salt intake: 6.4 grams/d (95% CI 6.1 to 6.7) | Mean salt intake: 6.8 grams/d (95% CI 6.5 to 7.1) | Mean salt intake: 8.8 grams/d, SD = 3.7 (95% CI 8.5 to 9.2) |
| Overall estimate – revised for comparability | Same as above | Same as above | Same as above | Same as above | Same as above |
| Measurement tool | Spot urine | 24‐Hour urine | Spot urine | Spot urine | 24‐Hour urine |
| Sample size | n = 1148 | n = 442 | n = 1041 | n = 1045 | n = 702 |
| Progress indicators available | Gender | Gender | Gender | Gender | Gender |
underlined text = computed by review authors
*Data points on which primary calculation of mean difference (pre‐intervention vs post‐intervention) is based (see Data and analyses ‐ "overall")
Of these 15 initiatives, 10 provided sufficient data for quantitative analysis of overall impact, and nine provided sufficient data for quantitative analysis of differential impact by sex. We omitted five initiatives from the quantitative synthesis of overall impact (Denmark ‐ Denmark country questionnaire 2014‐2015, Japan ‐ Udagawa 2008, New Zealand ‐ New Zealand Ministry for Primary Industries, Thailand ‐ Supornsilaphachai 2013, Turkey ‐ Erdem 2010) because variance estimates to accompany means were missing, and this could not be remedied by using other reported data or by contacting study authors.
We have used an asterisk to indicate data points that were used for analysis, for each country, Table 2; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; Table 13; Table 14; Table 15; Table 16; Table 17; Table 18; and Table 3, and we have shown these in Analysis 1.1. Countries were approximately equally split in terms of those evaluated on the basis of a dietary survey (Austria ‐ Austria country questionnaire 2014‐2015, Canada ‐ McLaren 2014, China ‐ Du 2014, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, Japan ‐ Udagawa 2008, Thailand ‐ Supornsilaphachai 2013) and those evaluated on the basis of urine samples (Denmark ‐ Denmark country questionnaire 2014‐2015, Finland ‐ Laatikainen 2006, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, Turkey ‐ Erdem 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014). The New Zealand Total Diet Survey approach does not fit into either category (New Zealand Ministry for Primary Industries).
1.1. Analysis.
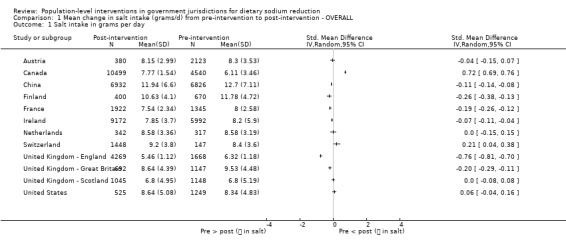
Comparison 1 Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ OVERALL, Outcome 1 Salt intake in grams per day.
We identified no adverse effects amongst these initiatives.
Comparison 1. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ OVERALL
Amongst the 10 countries (64,798 participants) included in the quantitative analysis (see Analysis 1.1), five showed a statistically significant mean decrease in salt intake from pre‐intervention to post‐intervention, ranging from Finland ‐ Laatikainen 2006 (mean decrease of 1.15, 95% confidence interval (CI) ‐1.69 to ‐0.61 grams/d) to Ireland ‐ Perry 2010 (mean decrease of 0.35, 95% CI ‐0.52 to ‐0.18 grams/d). Two initiatives (Canada ‐ McLaren 2014, Switzerland ‐ Chappuis 2011) showed a statistically significant mean increase in salt intake from pre‐intervention to post‐intervention (Canada: 1.66, 95% CI 1.56 to 1.76 grams/d; Switzerland: 0.80, 95% CI 0.19 to 1.41 grams/d).
The I2 measure of heterogeneity (between‐study variation), which ranges from 0 to 100, with higher values indicating greater heterogeneity, shows that heterogeneity for this group of 10 studies was very high (> 90%). Therefore, we did not focus on the pooled result.
Comparison 2. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ SUBSET OF MULTI‐COMPONENT INITIATIVES THAT INCLUDE STRUCTURAL ACTIVITIES
When we focused on the subset (n = 7 countries) of multi‐component initiatives that incorporated activities of a structural nature (e.g. food product reformulation, food procurement policy in specific settings; see Analysis 2.1, Figure 2 and Appendix 1), we found that most (four of seven) showed a statistically significant mean decrease in salt intake (grams/d) from pre‐intervention to post‐intervention. The significant decrease ranged from ‐1.15 (95% CI ‐1.69 to 0‐.61) grams/d in Finland (Laatikainen 2006) to ‐0.35 (95% CI ‐0.52 to ‐0.18) grams/d in Ireland (Perry 2010). One initiative (Switzerland ‐ Chappuis 2011) showed a statistically significant mean increase in salt intake (grams/d) from pre‐intervention to post‐intervention at 0.80 (95% CI 0.19 to 1.41) grams/d. Austria (Austria country questionnaire 2014‐2015) and Netherlands (Hendriksen 2013) did not show a statistically significant change in salt intake (grams/d) from pre‐intervention to post‐intervention.
2.1. Analysis.
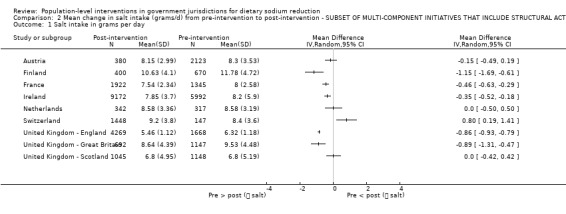
Comparison 2 Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ SUBSET OF MULTI‐COMPONENT INITIATIVES THAT INCLUDE STRUCTURAL ACTIVITIES, Outcome 1 Salt intake in grams per day.
The I2 measure revealed that heterogeneity for this group of seven studies was very high (> 90%). Therefore, we did not focus on the pooled result.
Comparisons 3 and 4. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ WOMEN ONLY (Analysis 3.1) and MEN ONLY (Analysis 4.1)
Nine countries (Austria ‐ Austria country questionnaire 2014‐2015, Canada ‐ McLaren 2014, China ‐ Du 2014, Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014) provided data that permitted quantitative analysis of differential impact by sex; that is, whether mean change in salt intake (grams/d) from pre‐intervention to post‐intervention differed between men and women (see Analysis 3.1 and Analysis 4.1). Gender‐stratified estimates are shown in Table 19.
3.1. Analysis.
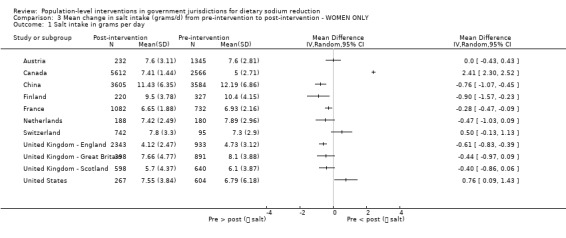
Comparison 3 Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ WOMEN ONLY, Outcome 1 Salt intake in grams per day.
4.1. Analysis.
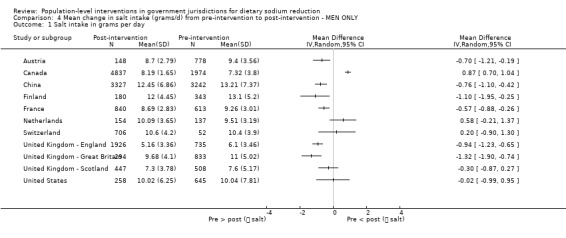
Comparison 4 Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ MEN ONLY, Outcome 1 Salt intake in grams per day.
18. Pre‐intervention and post‐intervention estimates of salt intake used for analysis of differential impact by sex (when available).
| Country | Pre‐intervention | Post‐intervention |
| AUSTRIA | ||
| Males | Data point 1 (2008) Mean salt intake = 9.4 grams/d SD = 3.56; n = 778 |
Data point 2 (2012): Mean salt intake: 8.7 grams/d SD = 2.79; n = 148 |
| Females | Data point 1 (2008) Mean salt intake = 7.6 grams/d SD = 2.81; n = 1345 |
Data point 2 (2012): Mean salt intake: 7.6 grams/d SD = 3.11; n = 232 |
| CANADA | ||
| Males | Data point 1 (1970‐1972): Mean salt intake = 7.32 grams/d SD = 3.8; n = 1974 |
Data point 2 (2004): Mean salt intake: 8.19 grams/d SD = 1.65; n = 4837 |
| Females | Data point 1 (1970‐1972): Mean salt intake = 5.00 grams/d SD = 2.71; n = 2566 |
Data point 2 (2004): Mean salt intake: 7.41 grams/d SD = 1.44; n = 5612 |
| CHINA | ||
| Males | Data point 6 (2006): Mean salt intake = 13.21 grams/d SD = 7.37; n = 3242 |
Data point 7 (2009): Mean salt intake = 12.45 grams/d SD = 6.86; n = 3327 |
| Females | Data point 6 (2006): Mean salt intake = 12.19 grams/d SD = 6.86; n = 3584 |
Data point 7 (2009): Mean salt intake = 11.43 grams/d SD = 6.35; n = 3605 |
| FINLAND – Kuopio only | ||
| Males | Data point 1 (Kuopio only 1979): Mean salt intake = 13.1 grams/d SD = 5.20; n = 343 |
Data point 3 (Kuopio only 1987): Mean salt intake = 12.0 grams/d SD = 4.45; n=180 |
| Females | Data point 1 (Kuopio only 1979): Mean salt intake = 10.4 grams/d SD = 4.15; n = 327 |
Data point 3 (Kuopio only 1987): Mean salt intake = 9.5 grams/d SD = 3.78; n=220 |
| FRANCE | ||
| Males | Data point 1 (1998‐1999): Mean salt intake = 9.26 grams/d SD = 3.01; n = 613 |
Data point 2 (2006‐2007): Mean salt intake = 8.69 grams/d SD = 2.83; n = 840 |
| Females | Data point 1 (1998‐1999): Mean salt intake = 6.93 grams/d SD = 2.16; n = 732 |
Data point 2 (2006‐2007): Mean salt intake = 6.65 grams/d SD = 1.88; n = 1082 |
| NETHERLANDS | ||
| Males | Data point 1 (2006): Mean salt intake = 9.51 grams/d SD = 3.19; n = 137 |
Data point 3 (2010): Mean salt intake = 10.09 grams/d SD = 3.65; n = 154 |
| Females | Data point 1 (2006): Mean salt intake = 7.89 grams/d SD = 2.96; n = 180 |
Data point 3 (2010): Mean salt intake = 7.42 grams/d SD = 2.49; n = 188 |
| SWITZERLAND | ||
| Males | Data point 1a (1984): Salt intake = 10.4 grams/d SD = 3.9; n = 52 |
Data point 2 (2011): Salt intake = 10.6 grams/d SD = 4.2; n = 706 |
| Females | Data point 1a (1984): Salt intake = 7.3 grams/d SD = 2.9; n = 95 |
Data point 2 (2011): Salt intake = 7.8 grams/d SD = 3.3; n = 742 |
| UNITED KINGDOM (Great Britain) | ||
| Males | Data point 1b (2000‐2001) Mean salt intake: 11.0 grams/d SD = 5.02; n = 833 |
Data point 2 (2008): Mean salt intake: 9.68 grams/d SD = 4.10; n = 294 |
| Females | Data point 1b (2000‐2001) Mean salt intake: 8.1 grams/d SD = 3.88; n = 891 |
Data point 2 (2008): Mean salt intake: 7.66 grams/d SD = 4.77; n = 398 |
| UK (England) – geometric mean, salt intake | ||
| Males | Data point 1a (2003): Geometric mean salt intake = 6.10 grams/d SD = 3.46; n = 735 |
Data point 6a (2007): Geometric mean salt intake = 5.16 grams/d SD = 3.36; n = 1926 |
| Females | Data point 1a (2003): Geometric mean salt intake = 4.73 grams/d SD = 3.12; n = 933 |
Data point 6a (2007): Geometric mean salt intake = 4.12 grams/d SD = 2.47; n = 2343 |
| UK (Scotland) | ||
| Males | Data point 1 (2003): Mean salt intake = 7.6 grams/d SD = 5.17; n = 508 |
Data point 4 (2009): Mean salt intake = 7.3 grams/d SD = 3.78; n = 447 |
| Females | Data point 1 (2003): Mean salt intake = 6.1 grams/d SD = 3.87; n = 640 |
Data point 4 (2009): Mean salt intake = 5.7 grams/d SD = 4.37; n = 598 |
| UNITED STATES | ||
| Males | Data point 1 (1988‐1994): Crude geometric mean salt intake = 10.04 grams/d SD = 7.81; n = 645 |
Data point 3 (2010): Crude geometric mean salt intake = 10.02 grams/d SD = 6.25; n = 258 |
| Females | Data point 1 (1988‐1994): Crude geometric mean salt intake = 6.79 grams/d SD = 6.18; n = 604 |
Data point 3 (2010): Crude geometric mean salt intake = 7.55 grams/d SD = 3.84; n = 267 |
For women (see Analysis 3.1), findings were split, with three initiatives showing a statistically significant mean decrease in salt intake (grams/d) from pre‐intervention to post‐intervention (China ‐ Du 2014: ‐0.76, 95% CI ‐1.07 to ‐0.45, Finland ‐ Laatikainen 2006: ‐0.90, 95% CI ‐1.57 to ‐0.23, France ‐ Dubuisson 2010: ‐0.28, 95% CI ‐0.47 to ‐0.09); two initiatives showing a statistically significant mean increase in salt intake (grams/d) from pre‐intervention to post‐cessation (Canada ‐ McLaren 2014: 2.41, 95% CI 2.3 to 2.52, United States ‐ Pfeiffer 2014: 0.76, 95% CI 0.09 to 1.43); and the remaining four countries (Austria ‐ Austria country questionnaire 2014‐2015, Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012) showing a non‐statistically significant mean change in salt intake from pre‐cessation to post‐cessation. Please note that, for women, we considered the United Kingdom as non‐statistically significant overall, because data from Great Britain as a whole (Wyness 2012) and from Scotland only (Scottish Centre for Social Research 2011) showed a non‐significant mean change in salt intake from pre‐cessation to post‐cessation. However, data from England only (Millett 2012) showed a statistically significant mean decrease in salt intake from pre‐cessation to post‐cessation (‐0.61, 95% CI ‐0.83 to ‐0.39).
For men (see Analysis 4.1), most initiatives (five of nine) showed a statistically significant mean decrease in salt intake (grams/d) from pre‐intervention to post‐intervention, ranging from United Kingdom (based on data from Great Britain as a whole ‐ Wyness 2012: ‐1.32, 95% CI ‐1.9 to ‐0.74, to France ‐ Dubuisson 2010: ‐0.57, 95% CI ‐0.88 to ‐0.26). One initiative showed a statistically significant mean increase in salt intake (grams/d) from pre‐intervention to post‐cessation (Canada: 0.87, 95% CI 0.7 to 1.04), and the remaining three countries (Netherlands ‐ Hendriksen 2013, Switzerland ‐ Chappuis 2011, United States of America ‐ Pfeiffer 2014) showed a non‐statistically significant mean change in salt intake from pre‐cessation to post‐cessation. Please note that for men, we considered United Kingdom as having a statistically significant decrease because data from Great Britain as a whole (Wyness 2012) and from England only (Millett 2012) showed a statistically significant mean decrease in salt intake from pre‐cessation to post‐cessation. However, data from Scotland only (Scottish Centre for Social Research 2011) showed a non‐statistically significant change.
The I2 measure showed that heterogeneity for this group of nine studies was very high (> 90%) for both men and women. Therefore, we did not focus on the pooled results.
Although Denmark (Denmark country questionnaire 2014‐2015) did not provide data that could be included in our analysis of differential impact by sex, information on differential impact by sex was reported within our documentation for Denmark (Denmark country questionnaire 2014‐2015); specifically, it was reported that with adjustments for body mass index (BMI) and age, a statistically significant (P value < .0001) mean decrease in salt intake from pre‐intervention to post‐intervention was found for both men (beta = ‐0.91) and women (beta = ‐0.52).
Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ differential by other axes of inequity
We recorded axes of stratification (inequity) considered in all initiatives, using PROGRESS as a guide (place of residence (e.g. urban/rural), race/ethnicity, occupation, gender, religion, education, socio‐economic position, social capital). See the Characteristics of included studies table and Table 2; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; Table 13; Table 14; Table 15; Table 16; Table 17; Table 18; and Table 3.
Information was insufficient to permit a quantitative analysis of differential impact by other axes of stratification (e.g. education, place of residence), in other words, to assess whether mean change in salt intake (grams/d) from pre‐intervention to post‐intervention differed across other axes of inequity. However, a subset of countries (Canada ‐ McLaren 2014, China ‐ Du 2014, Finland ‐ Laatikainen 2006, United Kingdom ‐ England ‐ Millett 2012, United States of America ‐ Pfeiffer 2014) incorporated an analysis of differential impact across different axes. Given that different methods were used across these studies, their equity analysis is not amenable to quantitative analysis (synthesis). Therefore, we have summarise those efforts in the following sections.
For Canada, McLaren 2014 examined inequities (by family income and highest educational attainment) in dietary sodium consumption in 1970‐1972 and in 2004. Overall, adjusted models revealed few statistically significant associations between income or education and sodium consumption. For men, an emerging inequity in use of table salt was indicated, whereby men of higher income were less likely than men of lower income to report using table salt in 2004, but no association was found in 1970‐72. For women, a negative association between education and sodium consumption (mg/d) was noted in 1970‐72, but no association in 2004. Study authors concluded that emerging inequity in reported use of table salt amongst men could reflect modest information‐based sodium reduction efforts that were implemented during the time frame considered (i.e. revision to the Food Guide in 1982). For sodium consumption in milligrams/d, no evidence of inequity was found in 2004, and in fact, in women a positive effect was observed (i.e. higher education associated with higher sodium consumption), which might reflect the very high prevalence of excess consumption.
For China, the China Health and Nutrition Survey cohort (Du 2014) permitted analysis of trends over time in sodium intake (1991‐2009) by place of residence (urban or rural), education (below high school vs high school or higher) and income (tertiles of inflation‐adjusted per capita household income). Study authors reported that sodium intake (grams/d) decreased significantly (1991‐2009) in all groups including those with higher and lower education; high, middle and low income; and urban and rural places of residence (Du 2014 ‐ Supplementary Table S1). The national sodium reduction initiative in China began in 2006.
For Finland, Laatikainen 2006 examined trends in urinary sodium excretion using surveys from 1979, 1982, 1987 and 2002 in four geographic areas: North Karelia, the Kuopio area, Southwestern Finland and the Helsinki area. Investigators observed different trends by geographical area (place of residence), such that urinary sodium excretion decreased significantly in eastern Finland between 1982 and 1987 but remained stable in southwestern Finland. Between 1982 and 2002, a significant decrease was seen in North Karelia and in southwestern Finland (Laatikainen 2006). In terms of education, the overall trend showed lowest salt intake in the highest education categories across the study period, but this effect was statistically significant only for men in North Karelia in 1979, and for women in southwestern Finland in 2002.
For the United Kingdom, Millett 2012 examined differential impact by social class (manual/non‐manual, based on the UK Registrar General's social class classification) and by ethnicity (white, black, South Asian) for the United Kingdom sodium reduction initiative, using 2003‐2007 data from the Health Survey for England. Mean salt intake decreased significantly from pre‐intervention to post‐intervention in all groups, and the reduction did not differ significantly between ethnic groups nor between social class groups, suggesting similar impact. Inequities in salt intake by social class and by ethnicity, which were noted in 2003, were thus still apparent in 2007. In other words, because reductions occurred in all social class and ethnic groups, inequities between groups remained. Another analysis of differential impact of the United Kingdom initiative was performed by Shankar in 2013 (see United Kingdom ‐ England); using econometric methods, investigators concluded that urinary sodium excretion levels were reduced following the United Kingdom initiative in almost all groups defined by birth cohort, gender and region. Stronger impact was observed amongst women than amongst men.
Finally for the United States of America, Pfeiffer 2014 examined trends in sodium intake (24‐hour urinary excretion, estimated from measured sodium concentrations in spot urine) between 1988 and 2010 using National Health and Nutrition Examination Survey (NHANES) data, including trends by race/ethnicity (Mexican‐American, Non‐Hispanic black, Non‐Hispanic white). Although cross‐sectional analysis showed differences in sodium intake between race/ethnic groups (e.g. mean estimated 24‐hour urine sodium excretion was highest in Mexican‐American and lowest in non‐Hispanic white groups in 1988‐1994 and 2003‐2006), no statistically significant changes in sodium intake were evident over time for any of these groups. In contrast, a statistically significant increase in sodium was observed across the sample as a whole.
Impact of studies that were not included in the quantitative synthesis
Initiatives in five countries could not be included in the quantitative synthesis because missing information (e.g. missing estimates of variance) could not be remedied by using other reported data or by contacting study authors. Available information from three of those countries (Japan ‐ Udagawa 2008, Denmark ‐ Denmark country questionnaire 2014‐2015, Turkey ‐ Erdem 2010) suggested a gradual decline in salt intake over the time period when the national dietary sodium reduction initiative was started. As the result of missing information, we do not know whether these apparent decreases in salt intake were statistically significant, with the exception of Denmark (Denmark country questionnaire 2014‐2015), which reported a statistically significant decrease over time in the text of their documentation. Of the other two omitted countries, the nature of change in salt intake over time in Thailand (Supornsilaphachai 2013) was mixed (appeared to be increasing on examination of one data point; appeared to be decreasing on examination of another), and data from New Zealand (New Zealand Ministry for Primary Industries) are not easily comparable because they were modelled rather than estimated, and therefore lacked key information such as sample size. Overall, it remains unknown what impact inclusion of these countries would have had on our results and conclusions.
Summary of main findings
Main findings are summarized in Table 20 .
19. Summary of main results.
| Country (initiative) | Overall impact | Impact for women only | Impact for men only |
| Austria | NS | NS | Decrease |
| Canada | Increase | Increase | Increase |
| China | Decrease | Decrease | Decrease |
| Finland | Decrease | Decrease | Decrease |
| France | Decrease | Decrease | Decrease |
| Ireland | Decrease | N/A | N/A |
| Netherlands | NS | NS | NS |
| Switzerland | Increase | NS | NS |
| United Kingdom ‐ England | Decrease | Decrease | Decrease |
| United Kingdom ‐ Great Britain | Decrease | NS | Decrease |
| United Kingdom ‐ Scotland | NS | NS | NS |
| United States | NS | Increase | NS |
Increase = Statistically significant increase in salt intake (grams/d) from pre‐intervention to post‐intervention
Decrease = Statistically significant decrease in salt intake (grams/d) from pre‐intervention to post‐intervention
NS = no statistically significant change in salt intake (grams/d) from pre‐intervention to post‐intervention
N/A = data did not permit separate analysis for males versus females
The United Kingdom is counted as one country/initiative but has three rows in the table because data were available for England only, Scotland only and Great Britain
Sensitivity analysis
Comparisons 5 and 6. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ using other available post‐intervention data points (Analysis 5.1) and using other available pre‐intervention data points (Analysis 6.1)
For initiatives with multiple available data points, analysis of impact was based on the pre‐intervention data point closest in time to the start year of the intervention, as well as the post‐intervention data point farthest away in time from the start year of the initiative. As a sensitivity check, we re‐ran analysis of impact using alternative post‐intervention data points, along with alternative pre‐intervention data points when available.
Of the 10 countries included in the overall analysis of impact, three (Finland ‐ Laatikainen 2006, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012, United States of America ‐ Pfeiffer 2014) had alternative post‐intervention data points (recall that for the United Kingdom we have data for UK/Great Britain as a whole ‐ Wyness 2012, for England only ‐ Millett 2012 and for Scotland only ‐ Scottish Centre for Social Research 2011). Finland (Laatikainen 2006), UK ‐ Scotland (Scottish Centre for Social Research 2011) and the United States of America (Pfeiffer 2014) each had one other available post‐intervention data point and UK ‐ England (Millett 2012) had three other available post‐intervention data points, as follows.
Finland: initiative started in 1979; main analysis based on post‐intervention data point from 1987; alternative post‐intervention data point available for 1982 (Laatikainen 2006).
UK ‐ Scotland: initiative started in 2003; main analysis based on post‐intervention data point from 2009; alternative post‐intervention data point available for 2006 (Scottish Centre for Social Research 2011).
United States of America: initiative started late 1980s to early 1990s; main analysis based on post‐intervention data point from 2010; alternative post‐intervention data point available for 2003‐2006 (Pfeiffer 2014).
UK‐England: initiative started in 2003; main analysis was based on post‐intervention data point from 2007; alternative post‐intervention data points available for 2004, 2005, and 2006 (Millett 2012).
We re‐ran the analysis using the only other post‐intervention data point available for Finland (Laatikainen 2006), UK ‐ Scotland (Scottish Centre for Social Research 2011) and the United States of America (Pfeiffer 2014), as well as the second most recent post‐intervention data point available for UK ‐ England (Millett 2012) (from 2006) (see Analysis 5.1). Use of these alternative post‐intervention data points did not change the effect observed in the main analysis (Analysis 1.1) for UK ‐ Scotland (Scottish Centre for Social Research 2011) (non‐significant effect based on both data points), United States of America (Pfeiffer 2014) (non‐significant effect based on both data points) or UK ‐ England (Millett 2012) (statistically significant mean decrease in salt intake from pre‐intervention to post‐intervention based on both data points). For Finland (Laatikainen 2006), the statistically significant mean decrease in salt intake (grams/d) from pre‐intervention to post‐intervention observed in Analysis 1.1 was reduced to non‐significance when the alternative post‐intervention data point was used (Analysis 5.1).
5.1. Analysis.
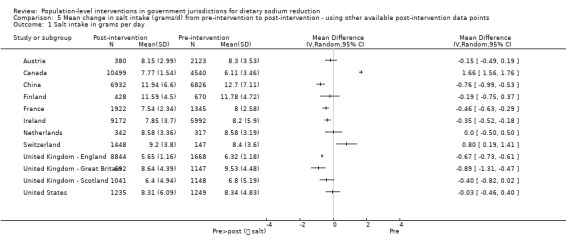
Comparison 5 Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ using other available post‐intervention data points, Outcome 1 Salt intake in grams per day.
Of the 10 countries included in the overall analysis of impact, two (China ‐ Du 2014, Ireland ‐ Perry 2010) used alternative pre‐intervention data points. China (Du 2014) included five other available pre‐intervention data points, and Ireland (Perry 2010) included one other available pre‐intervention data point, as follows.
China: initiative started in 2006; main analysis based on pre‐intervention data point from 2006; alternative pre‐intervention data points available for 1991, 1993, 1997, 2000 and 2004 (Du 2014).
Ireland: initiative started in 2003; main analysis based on pre‐intervention data point from 2002; alternative pre‐intervention data point available from 1998 (Perry 2010).
We re‐ran the overall analysis using the only other available pre‐intervention data point for Ireland (Perry 2010), as well as the alternative pre‐intervention data point for China (Du 2014) that was second‐closest to the start of the initiative (from 2004) (see Analysis 6.1). Use of these alternative pre‐intervention data points did not change the effect observed in the main analysis (Analysis 1.1), specifically, the statistically significant mean decrease in salt intake (grams/d) from pre‐intervention to post‐intervention observed in Analysis 1.1 for both China (Du 2014) and Ireland (Perry 2010) remained in the analysis when the alternative pre‐intervention data point was used (Analysis 6.1).
6.1. Analysis.
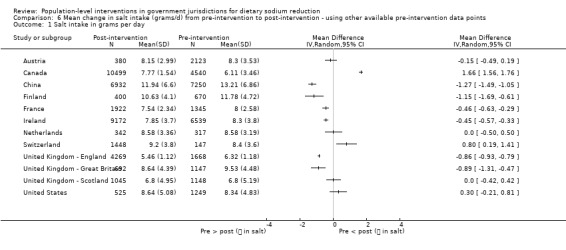
Comparison 6 Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ using other available pre‐intervention data points, Outcome 1 Salt intake in grams per day.
Methodological quality of studies and publication bias
Across the 10 studies included in the assessment of overall effect, we found no clear indication of publication bias by examining the funnel plot (Figure 5).
5.
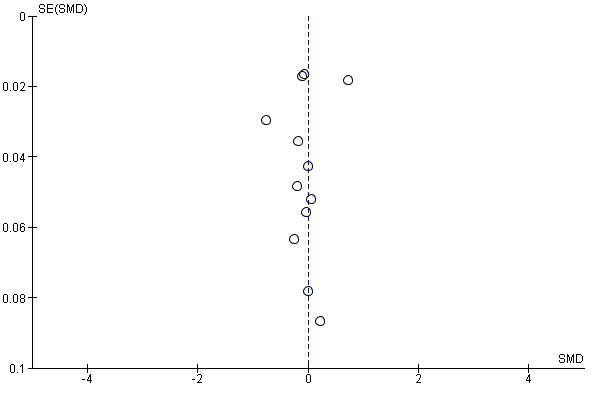
Funnel plot of comparison 1.1: Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ overall impact (men and women combined).
We rated overall quality of the evidence by using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) framework (GRADE n.d.), which is based on five considerations: risk of bias, imprecision, inconsistency, indirectness and publication bias. We first rated all of our studies as having 'low' quality because of their observational, uncontrolled nature. The relatively small number of studies and heterogeneity across them suggest the need to downgrade quality to 'very low'. See Table 1.
Discussion
Summary of main results
Of the 15 initiatives that met our inclusion criteria, 10 provided sufficient data for quantitative analysis of overall impact.
Diversity across the included studies and their effects was notable. Across the 10 studies included in the quantitative synthesis, five showed a statistically significant reduction in dietary sodium intake. These included Finland (Laatikainen 2006), where multi‐component and structural efforts have been under way since the 1970s, as well as countries where the initiative is much more recent, such as United Kingdom (Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012) and Ireland (Perry 2010) (where initiatives began in 2003). Two of the 10 studies (Canada ‐ McLaren 2014, Switzerland ‐ Chappuis 2011) showed a statistically significant increase in dietary sodium intake. In Switzerland (Chappuis 2011), although the initiative included activities of a structural nature (e.g. food product reformulation), those activities were characterised as "voluntary commitments" by companies, and thus their impact may be limited. Furthermore, the initiative in Switzerland (Chappuis 2011) is relatively new (started in 2008), and our post‐intervention data point was from 2011. At the time of data collection, Switzerland (Chappuis 2011) indicated engaging in "meetings with companies" around food product reformulation, so it is possible that those activities were in their early stages, and the 2011 data point was too early to permit capture of any impact of that initiative. In Canada (McLaren 2014), the intervention captured by available data points was very modest ‐ a single‐component initiative consisting of public education. The observed effect for Canada (McLaren 2014) may reflect an increase in salt intake that was already occurring as the result of increasing consumption of ultra‐processed food products (Moubarac 2014), which the modest intervention examined here was insufficient to offset. Because of high levels of heterogeneity across studies, we focused on individual rather than pooled study results.
When we focused on the seven multi‐component initiatives and incorporated intervention activities of a structural nature (e.g. food product reformulation, food procurement in specific settings), we found that a decrease in salt intake from pre‐intervention to post‐intervention was more apparent, with four of seven initiatives (Finland ‐ Laatikainen 2006, France ‐ Dubuisson 2010, Ireland ‐ Perry 2010, United Kingdom ‐ Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012) showing such an effect. This is consistent with Rose's (Rose 1992) population‐level strategy of prevention and further emphasises the importance of distinguishing between population‐level interventions that are more agentic and those that are more structural (McLaren 2010; Sumar 2011). Our findings indicate that structural population‐level interventions are likely more impactful in this context of national dietary sodium reduction initiatives.
In terms of the differential impact of initiatives across social groups, nine initiatives provided sufficient data for quantitative analysis of differential impact by sex ("g"ender in the PROGRESS framework). Those nine studies revealed an apparent reduction in salt intake for men, with more than half (five of the nine) the initiatives showing a statistically significant mean decrease in salt intake from pre‐intervention to post‐intervention. Findings for women were more equivocal (three initiatives showed a statistically significant mean decrease in salt intake from pre‐intervention to post‐intervention, two studies showed a statistically significant mean increase and four showed a non‐statistically significant change).
Information was insufficient to reveal differential impact of these initiatives by other axes of stratification (equity). Our qualitative synthesis of findings from the few countries that incorporated analysis of differential impact (methods and indicators were too diverse to be quantitatively synthesised) showed that in some studies inequities did not necessarily increase (worsen) in the context of a national sodium reduction initiative. However, additional studies that consistently incorporate analysis of equity of impact are needed to confirm this. Furthermore, it is important to emphasise that although it is promising to observe that inequities are not worsening, it would be preferable to demonstrate that inequities are in fact narrowing.
Overall completeness and applicability of evidence
In our companion review (Trieu 2015), 75 countries were found to have national dietary sodium reduction efforts under way. We considered all of these for inclusion in our review and retained only 15, of which only a further subset provided data amenable to quantitative analysis. Although the growing number of sodium reduction initiatives worldwide is promising, limited available data that can be used to monitor present a challenge in building the evidence base. In some cases, data limitations reflect that the initiative is relatively new, activities (including monitoring) are at an early stage and data may be forthcoming. In other cases, however, the data infrastructure is limited, for example, some initiatives were started with no baseline data in place to permit rigorous evaluation. Although initiatives in the former category were classified as 'ongoing' and may be included in updates of this review, the latter initiatives had to be classified as 'excluded' because of the impossibility of going backwards to produce pre‐intervention data.
Although our companion review (Trieu 2015) identified national sodium reduction efforts that were under way in countries at all levels of economic development and in all World Health Organization (WHO) regions, this review did not include initiatives from lower‐middle‐income nor low‐income countries, nor in African or eastern Mediterranean regions. Therefore, it is not known to what extent our findings apply to those countries and regions.
In addition to indicators of sodium consumption, we intended (see our protocol, McLaren 2013) to examine indicators of health outcomes related to sodium consumption (e.g. stroke, blood pressure, hypertension, cardiovascular disease) as well as secondary outcomes (e.g. knowledge, awareness, other health/disease outcomes). However, we were unable to include all of these outcomes because in many instances, our review involved piecing together an evaluation from existing national data sources. Ensuring a comprehensive review required that we locate, for every included country, every data source that included any of these outcomes. The potential scope of data sources accordingly became very large, and because of the unwieldy nature of the task, we made the decision to focus on indicators of sodium consumption for feasibility purposes. We made this decision reluctantly ‐ we recognise the importance of including clinical outcomes in other reviews.
Quality of the evidence
As has been noted, we found substantial between‐study variation by examining the I2 measure, which in all cases exceeded 90%. For this reason, we did not focus on the overall pooled result and we downgraded the quality of the evidence to very low. It is likely that the main reasons for heterogeneity include context (i.e. "population" in PICO ‐ countries vary substantially in social, economic, political and cultural conditions) and the nature of the initiative (i.e. "intervention" in PICO ‐ interventions vary in type and extent, which in turn reflects country‐specific attributes such as stakeholder (e.g. government) level of concern with salt, investment in salt reduction, co‐ordination with other stakeholders and so on.
Across the 10 studies included in the assessment of overall effect, we found no clear indication of publication bias by examining the funnel plot (Figure 5), which is consistent with our comprehensive search and extensive use of grey literature resources.
By using specific tools (adapted version of the Cochrane risk of bias tool and the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) method (GRADE n.d.)), review authors determined that the studies included in this review were at high risk of bias, and that overall quality of the body of evidence in terms of study limitations, consistency of effect, imprecision, indirectness and publication bias (GRADE n.d.) was very low. By examining the proportion of bias domains in which each initiative had high or uncertain risk of bias, we were able to capture variations in methodological quality across our included countries, which ranged from studies of highest methodological quality in France (Dubuisson 2010), Finland (Laatikainen 2006) and the United Kingdom (Scottish Centre for Social Research 2011; Millett 2012; Wyness 2012) (high or uncertain risk of bias in only one or two of seven bias domains) to studies of lowest methodological quality in Japan (Udagawa 2008), New Zealand (New Zealand Ministry for Primary Industries), Thailand (Supornsilaphachai 2013) and Turkey (Erdem 2010) (high or uncertain in five of seven bias domains). Notably, we included none of the four studies of lowest quality in our quantitative synthesis because investigators provided insufficient data.
There is a need to ensure that existing tools to appraise the methods used in observational studies adequately take into account the complexities associated with evaluation of national level interventions as described in this review. While the domains of GRADE assist in the identification of quality across study designs, further methodological work is needed to ensure that there is appropriate discrimination between high and low quality observational studies.
Potential biases in the review process
For feasibility reasons, we focused on a single primary outcome: dietary sodium intake. Thus we do not know ‐ on the basis of this review ‐ whether or the extent to which population‐level interventions in government jurisdictions for dietary sodium reduction impact health outcomes such as blood pressure or hypertension and stroke prevalence. Review authors need to include these outcomes in future reviews.
Although we undertook extensive efforts to accurately characterise intervention activities for each country, some uncertainty remains in terms of exposure, related to the jurisdictional administrative structure of a country. For example, a country (in the country questionnaire) may not have reported "food procurement policy in specific settings" as one of the activities within its national initiative. However, such activities may have been undertaken in smaller jurisdictions in that country such as provinces, states or municipalities, and the country contact speaking to national efforts would not necessarily be aware of activities occurring at a different level of government. We would not have captured such activities. Furthermore, to the extent that turnover of government staff is high, our method of gathering information from country contacts (see Trieu 2015) may be subject to limitations if the individual is new to the role and/or if institutional memory of the initiative is low. However, for the types of initiatives considered in this review, much information is not available in published form; thus information obtained from country contacts is extremely important, and we view its inclusion as a strength of our review.
We have no reason to believe that we missed information on serious and/or rare adverse events.
We undertook the last search in January 2015, and latency between the date of the search and publication of the review may introduce bias. Latency reflects the complexity of the review.
Although we included the Cochrane Public Health Group Specialised Register in our search, we did not search other trial registries, and this may have caused us to miss some trials (e.g. cluster‐randomised controlled designs), if indeed they existed.
We imposed no other restrictions.
Agreements and disagreements with other studies or reviews
No other comprehensive systematic reviews have examined the impact of population‐level dietary sodium reduction initiatives in government jurisdictions, including equity of impact.
Authors' conclusions
Implications for practice.
In the light of the high prevalence of excess sodium consumption reported in many countries worldwide, and the strong association between excess sodium consumption and adverse health outcomes, it is promising that a growing number of national population‐level dietary sodium reduction initiatives are being developed and implemented. Those initiatives have the potential to achieve population‐wide reductions in dietary sodium intake, particularly if they are multi‐component in nature and incorporate intervention activities of a more structural nature (e.g. food product reformulation, food procurement policy in specific settings). However, we acknowledge that wide variation in the effects across the studies reduces our confidence in the overall results.
Upon reviewing the tools used to assess study quality (adapted version of the Cochrane risk of bias tool and the GRADE method (GRADE n.d.)), we considered the studies included in this review to be at high risk of bias, and we found the overall quality of the body of evidence in terms of study limitations, consistency of effect, imprecision, indirectness and publication bias (GRADE n.d.) to be very low. However, these assessments must be interpreted in the light of the nature of the intervention (national initiatives in government jurisdictions) and corresponding use of uncontrolled study designs, for which assessment tools are not well suited.
We excluded from this review a substantial proportion of existing national sodium reduction initiatives because they lacked comparable pre‐intervention and/or post‐intervention data with which we could assess the impact of the initiative. When a national sodium reduction initiative is developed, one must consider options for monitoring the impact of the initiative (e.g. pre‐existing data sources) and/or building infrastructure to permit monitoring of the initiative if pre‐existing data are not available or suitable. Monitoring of infrastructure should permit evaluation of both overall impact and differential impact across social groups.
This review provides some evidence that national sodium reduction initiatives that are multi‐component and include activities of a structural nature (e.g. food product reformulation, food procurement policy in specific settings) appear more effective than single‐component, agentic initiatives such as information campaigns.
Implications for research.
Although we have included some excellent peer‐reviewed journal articles in our review, we note that a substantial proportion of our resources were grey literature materials, including reports, websites and communications with country contacts. In many instances, the impact of an initiative was not evaluated in a single research article, but rather the evaluation was pieced together from several discrete materials. If we are to build this evidence base, it is important and urgent that during planning of an initiative, purposive evaluations examine the impact at a level of rigour demanded by the scientific peer‐review community. Purposive evaluations of impact should use study designs that are suited to the nature of national interventions (i.e. uncontrolled pre‐post, interrupted time series, pre‐post with comparison community) and a range of important outcomes (i.e. sodium intake, clinical outcomes, secondary outcomes such as knowledge) to yield an accurate report on both overall impact and differential impact across social groups.
We noted a very high level of heterogeneity across studies, and this precluded pooled analysis. Although less heterogeneity is desirable from a research point of view, this is not a reasonable or desirable goal for population‐level initiatives. Such initiatives are embedded within their unique social, cultural, economic and political context (i.e. heterogeneity will always be present), and the initiative and its impact are inextricably related to those dimensions of context. We recommend that, rather than striving to reduce heterogeneity, researchers should focus their efforts on developing thoughtful and rigorous ways to synthesise and interpret these initiatives and their findings, when quantitative synthesis may not be feasible or desirable.
To complement this review, empirical studies of the impact of national sodium reduction initiatives, not only on sodium consumption, but on health outcomes associated with excess sodium consumption, must be accrued.
Researchers must ensure that tools used to appraise the quality of observational methods adequately take into account the complexities associated with evaluating national level interventions such as dietary sodium reduction initiatives. Studies of many public health interventions will intrinsically be judged as being at high risk of bias. This does not necessarily mean that they cannot inform policy or program level decisions. There is an important need to develop better methods for appraising studies of this nature need to collect quality information around context and implementation, to ensure research findings are of most use to decision makers.
Feedback
Comment on the review
Summary
Dear Sir,
The work “Population‐level interventions in government jurisdictions for dietary sodium reduction” of McLaren et al is focusing on the efficacy of population‐based interventions to reduce sodium intake, a health related subject of importance to governments worldwide. For various countries, authors compare results of one pre‐initiative and at least one post‐initiative study. However, this in general sound approach may lead to deceptive results, as for the case of Switzerland. The Swiss Salt Strategy started in 2008 [1] based on data available in Switzerland at that time. McLaren et al, however, are using a study from 1984 as baseline reference, which involved only 147 persons [2]. We do not consider data from more than 20 years before the actual intervention, a suitable choice. Authors obviously do not take into account important changes of the food market and dietary patterns. In 1984 many of today’s high sodium foods, such as convenience products were not even developed and dietary habits of the Swiss population have evolved as well. Further, McLaren et al selected a study of 2011 as post‐intervention data point. Knowing that a state‐of‐the‐art salt strategy has a horizon of up to 20 years to show results, the use of a study conducted three years after release of the strategy seems as well inappropriate.
My comments concern the Swiss situation but may also be applicable for other countries. We invite authors to put their results into perspective of the particular national situation throughout the entire manuscript. They have partly done so in the full text of the review, however, they have missed to do so in the results section of the abstract and especially in the plain language summary. This is indeed quite unfortunate since many readers, and in particular, journalists, politicians, etc. will only read abstract or plain language summary and may conclude that in Switzerland interventions resulted in an increase in sodium intake. Such misleading presentation renders the task of health authorities to reduce sodium intake of populations more difficult if not impossible. Authors should reconsider to amend both abstract and plain language summary.
References
1. Federal Food Safety and Veterinary Office, Salt Strategy for 2013‐2016, Bern. http://bit.ly/2dM4sAI (23.10.2016)
2. Mordasini C, Abetel G, Lauterburg H, Ludi P, Perrenoud JP, Schmid H, et al. Sodium chloride intake and supply of iodine in the Swiss population. Schweizerische Medizinische Wochenschrift 1984;114(51):1924‐9.
Reply
Thank you very much for this important comment. By way of clarification, we included any country that 1) had a sodium reduction initiative in place and 2) for which at least one pre‐initiative and at least one post‐initiative data point could be located, and 3) the two data points had to use the same method to assess dietary sodium intake (e.g., 24 hour urine samples). For the specific case of Switzerland, although the 1984 data point occurred long before the intervention began, we felt that it was a usable data point based on the objective of the study we used (translated version of Mordasini et al. 1984: "It was therefore our goal to determine with a simple scale, supported by doctors practicing in the field study, the actual salt consumption and its range within the Swiss population"). Cochrane requires authors to be comprehensive, so we only excluded countries if they did not satisfy the 3 criteria above (e.g., they did not have a pre‐ and/or a post‐ data point at all, or if the pre‐ and post‐ data points used different methods to measure salt intake). We agree that there are limitations with this approach. Limitations, including those associated with timing (which was the case for several countries included in our review, including Canada) are captured in our risk of bias assessment and GRADE scale, which pertains to the body of evidence as a whole. We also acknowledge in our abstract that “heterogeneity across studies was significant, reflecting different contexts (population and setting) and initiative characteristics”. We encourage anyone reporting the findings of this review to acknowledge the important contextual factors and sources of heterogeneity. Switzerland (among other countries) highlights one of our main conclusions which is about the importance of data infrastructure – a more recent population survey that measured urinary sodium among the Swiss population may indicate a decrease from the 2011 data point, and future updates of the review would capture this.
Contributors
Commentator: Michael Beer Federal Food Safety and Veterinary Office FSVO Head Food and Nutrition Division
Author response: Lindsay MacLaren (lead author)
What's new
| Date | Event | Description |
|---|---|---|
| 6 March 2017 | Amended | Context added to findings for Canada and Switzerland in the abstract and plain language summary. |
| 18 January 2017 | Feedback has been incorporated | Feedback and author's reply added |
History
Protocol first published: Issue 10, 2012 Review first published: Issue 9, 2016
| Date | Event | Description |
|---|---|---|
| 13 August 2013 | Amended | Protocol revised to incorporate plan to examine overall impact, as well as differential impact. Changes made to title and inclusion criteria and in various other places throughout the protocol. Jacqui Webster and Kathy Trieu added as review authors |
Notes
1To its Global Action Plan for the Prevention and Control of Non‐Communicable Diseases (NCDs) 2013–2020, the World Health Organization added a relative target for population dietary sodium reduction, namely, a 30% relative reduction in mean population intake of salt/sodium (WHO 2013; McLean 2014). The relative target is consistent with the observed linear (vs threshold) relationship between sodium intake and blood pressure, and offers the pragmatic advantage of being more achievable for some countries whose absolute values are particularly high.
Acknowledgements
We thank Ms. Chelsea Doktorchik for providing assistance with the risk of bias assessment.
We thank our external reviewers, Anthony Laverty and Eleana C. Villanueva, for providing helpful comments.
Appendices
Appendix 1. Glossary to accompany logic model
| Context | |
| Global context | Economic, political, social, cultural, demographic and technological issues, events and trends within and between countries worldwide, which define the backdrop for our review. Includes the food context: issues pertaining to growth, production, marketing and trade of food products within and between countries worldwide |
| Intervention continuum | |
| Intervention continuum | Framework for characterising population health interventions according to their implicit or explicit emphasis on agency or structure. Interventions that are more agentic target behaviour change among individuals, and interventions that are more structural target conditions in which behaviours occur. The closer an intervention is to the structural end of the continuum, the more impactful and equitable it is hypothesised to be (McLaren 2010) |
| Intervention types* | |
| Food product reformulation | Large‐scale efforts to lower the sodium content of food products at the time of production. By “large‐scale”, we mean efforts that characterise government jurisdictions (e.g. provinces, countries), transcending specific settings (see food procurement policy, below) |
| Large‐scale pricing strategies | Strategies (e.g. taxation, subsidisation) designed to manipulate the price of food products in a way that encourages the purchase of healthier foods and discourages the purchase of less healthy foods. By “large‐scale”, we mean efforts implemented by government jurisdictions (e.g. provinces, countries), transcending specific settings |
| Food procurement policy in specific settings | Nutrition policy (e.g. limits on maximum sodium content) implemented within contained food service settings or environments, particularly publicly funded environments such as schools, colleges/universities, child care settings, workplaces, recreation facilities, prisons and hospitals and long‐term care facilities |
| Restrictions on marketing to children | Efforts by government to restrict the extent or nature of promotional/marketing activities by companies. As an example, the province of Quebec, Canada, has banned television advertising to children since 1980 under sections 248 and 249 of the Consumer Protection Act (CPA 1978) |
| On‐package nutrition information | Nutrition information provided directly on food packaging. We have identified 3 subtypes of on‐package nutrition information: a) Information on calories, nutrients and % daily value of nutrients (e.g. Canada's Nutrition Facts Table) b) On‐package symbols to assist consumers with healthy food selection (e.g. United Kingdom's "traffic light" system, which tells consumers at a glance whether a food is high (red), medium (amber) or low (green) in salt, sugar, fat and saturated fat, respectively) c) On‐package high‐salt warning labels (e.g. Finland's mandatory warning labels on foods whose sodium content exceeds defined limits) |
| Information campaigns | Public information/education campaigns, which focus specifically on sodium or more broadly on diet (including sodium). Campaigns may be delivered via diverse media including television, radio, posters/billboards, newspapers, other print materials, social media (e.g. Facebook, Twitter), RSS (really simple syndication) feeds, email subscriptions, online advertising and cell phones (health "apps", text message updates), etc. |
| Intervention mechanisms** | |
| Intervention mechanisms | Processes by which intervention types are hypothesised to impact the outcomes. Intervention types are hypothesised to operate via 1 or more mechanisms, and the mechanisms are conceptualised as interacting with one another |
| Availability and accessibility | Number or proportion of lower‐sodium food products available on the market or within the setting of interest |
| Cost | Purchase price of lower‐sodium products, relative to higher‐sodium products, especially relative to higher‐sodium versions of the same product |
| Appeal and familiarity | Symbolic desirability of or attachment to a food product as experienced by consumers, established through effective marketing or some other means (e.g. personal tastes and preferences) |
| Knowledge and awareness | Consumer cognizance of dietary sodium specifically or diet generally, including associations with health |
| Axes of inequality | |
| Axes of inequality | Dimensions of socio‐economic stratification, which we hypothesise will moderate the impact of intervention types on outcomes. We will use the PROGRESS framework to identify pertinent axes of inequality: place of residence; race/ethnicity; occupation; gender; religion; education; socioeconomic position; social capital |
| Outcomes | |
| Food selection and purchase | Choice and purchase of food products by individuals, in retail facilities (e.g. grocery stores) as well as in food service settings (e.g. restaurants, cafeterias) |
| Sodium intake | Ingested dietary sodium including sodium‐related food additives. Can be measured via 24‐hour urine sample (gold standard) or via nutrition survey (e.g. 24‐hour dietary recall) |
| Disease outcomes | Diseases or risk factors for which epidemiological research has demonstrated an association with excess dietary sodium consumption. Examples include cerebrovascular outcomes (e.g. stroke); cardiovascular outcomes (e.g. blood pressure/hypertension, cardiovascular disease, myocardial infarction); and other outcomes (e.g. stomach cancer, osteoporosis, renal outcomes) |
* Additional comments about intervention types
Some of the intervention types (e.g. food product reformulation; food procurement policy; on‐package nutrition information) are amenable to implementation on a mandatory basis (i.e. required and enforced by government) or on a voluntary basis (i.e. at the discretion of individual companies). Placement of the intervention type on the continuum assumes implementation of a mandatory nature. For a given intervention type, implementation on a voluntary basis will bring it closer to the agentic end of the continuum
Classification of an intervention type as more agentic or more structural is based on the extent to which the interventionin and of itself relies on individual agency. Thus, although mandatory nutrition labelling may ultimately lead food companies to reformulate their products (e.g. following implementation of mandatory nutrition labelling in Canada, average amounts of trans fatty acids (TFA) in margarines decreased (Ricciuto 2009)), the impact of this intervention initially depends on individuals making selections based on the information provided
Further, even if an intervention characterised as more agentic ultimately leads to change of a more structural nature, longer‐term impact may still be inequitable. For example, Ricciuto 2009 demonstrated that, although mandatory nutrition labelling was associated with a decrease in average TFA in margarines, margarines lower in TFA were more expensive than margarines higher in TFA, and this relationship was stronger following labelling regulations than before
**Additional comments about intervention mechanisms
These broad categories of mechanisms were identified by review authors on the basis of literature on population health and health promotion interventions, in general and specific to diet and sodium. Although not meant to be exhaustive, we do intend them to cover the main pathways of influence
There is not necessarily a single, one‐to‐one relationship between intervention type and mechanism. For example, large‐scale pricing strategies may facilitate selection of lower‐sodium food via "cost" but impede selection via "appeal & familiarity" if the lower sodium products are not liked by the individual
The pathway from mechanisms to outcomes (food selection and purchase, sodium intake and disease outcomes) is represented by a dotted arrow, which is intended to denote the possible presence of other steps in the pathway; for example, the pathway from "information campaigns" to "food selection and purchase" via "knowledge and awareness" may include other steps, such as reading labels and deliberately searching for lower‐salt products. On the other hand, the pathway from "food product reformulation" to "food selection and purchase" via "availability and accessibility" may occur with no other steps
Appendix 2. Search strategy used for electronic databases
NOTE: Searches were run in December 2013 and January 2015.
MEDLINE (Ovid)
MEDLINE In‐Process and Non‐Indexed Citations (Ovid)
Cochrane CENTRAL Register
1. sodium, dietary/ or sodium chloride, dietary/
2. Sodium Chloride/
3. Sodium Glutamate/
4. sodium benzoate/ or sodium nitrite/
5. Sodium Hydroxide/
6. Diet, Sodium‐Restricted/
7. (monosodium glutamate* or MSG or sodium additive* or sodium alginate* or sodium benzoate* or sodium caseinate* or sodium citrate* or sodium chloride* or sodium glutamate* or sodium hydroxide* or sodium nitrate* or sodium nitrite* or sodium phosphate* or sodium propionate* or sodium saccharin* or sodium sulfite*).tw.
8. ((salt or sodium) adj10 (reduc* or target* or cutback* or decreas* or limit* or consumption)).tw.
9. ((diet* or nutrition* or food or intake) adj10 (salt or sodium)).tw.
10. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9
11. Food, Formulated/
12. Food‐Processing Industry/
13. food technology/ or food analysis/ or food preservation/
14. Food Industry/
15. 12 or 13 or 14
16. (adjust* or alter* or change or changing or control* or decreas* or limit* or modify or modified or new or reduce or reducing or reduction* or reformulat* or redevelop* or restrict*).tw.
17. 15 and 16
18. ((adjust* or alter* or change or changing or control* or decreas* or limit* or modify or modified or new or reduce or reducing or reduction* or reformulat* or redevelop* or restrict*) adj10 (recipe* or food or foods or formula* or ingredient*)).tw.
19. 11 or 17 or 18
20. taxes/ or tax exemption/
21. Government Programs/
22. financing, organized/ or financing, government/
23. "Cost Sharing"/
24. (pricing or cost or costs or subsidi*).tw.
25. (taxation or taxes or subsid*).tw.
26. (financial adj3 (incentive* or disincentive*)).tw.
27. 20 or 21 or 22 or 23 or 24 or 25 or 26
28. Nutrition Policy/
29. exp Food Service, Hospital/
30. Food Services/
31. schools/ or schools, nursery/
32. Workplace/
33. Prisons/
34. Universities/
35. Child Day Care Centers/
36. ((food* or menu or nutrition*) adj5 (buy* or procur* or purchas* or stock*) adj5 (guideline* or policy or policies or practice* or standard*)).tw.
37. ((cafeteria* or diet or food* or menu* or nutrition*) adj10 (childcare or child‐care or college* or daycare* or day‐care* or fitness centre* or fitness center* or hospital* or leisure center* or leisure centre* or preschool* or pre‐school* or prison* or public facilit* or recreation center* or recreation centre* or recreation facilit* or school* or universit*)).tw.
38. 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37
39. Advertising as Topic/
40. ((market* or adverti* or promot*) adj10 (adolescent* or adolescence or child or children or teenager* or teens or young people or youth*)).tw.
41. 39 or 40
42. Food Labeling/
43. Food Packaging/lj, st [Legislation & Jurisprudence, Standards]
44. ((food* or nutrition* or diet*) adj10 (facts or information or label* or symbol* or warning*)).tw.
45. health check.tw.
46. 42 or 43 or 44 or 45
47. nutrition surveys/ or diet surveys/
48. communications media/ or exp mass media/
49. Social Marketing/
50. health education/ or exp consumer health information/ or health fairs/
51. exp Health Promotion/
52. Information Dissemination/
53. newspapers/ or periodicals as topic/
54. computer communication networks/ or internet/ or blogging/ or social media/
55. Electronic Mail/
56. ((communicat* adj2 campaign*) or (information adj2 campaign*) or mass media or newspaper* or television* or radio* or (public adj2 campaign*) or (national adj2 campaign*) or public information).tw.
57. (blog* or email* or facebook or internet or magazine* or mobile device* or PDA or SMS or smartphone* or social media or text messag* or twitter or web).tw.
58. (health education or health information or health promotion).tw.
59. 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58
60. 19 or 27 or 38 or 41 or 46 or 59
61. 10 and 60
62. exp animals/ not humans.sh.
63. 61 not 62
Cochrane Public Health Register
1. salt OR sodium [All non‐indexed text fields]
2. (reduc OR lower OR restrict OR adjust OR decreas OR limit OR modi OR intake OR use)[All non‐indexed text fields]
3. 1 and 2
EMBASE (Ovid)
1. sodium intake/
2. *sodium chloride/
3. *glutamate sodium/
4. *sodium nitrite/
5. *sodium hydroxide/
6. sodium restriction/
7. (monosodium glutamate* or MSG or sodium additive* or sodium alginate* or sodium benzoate* or sodium caseinate* or sodium citrate* or sodium chloride* or sodium glutamate* or sodium hydroxide* or sodium nitrate* or sodium nitrite* or sodium phosphate* or sodium propionate* or sodium saccharin* or sodium sulfite*).tw.
8. ((salt or sodium) adj10 (reduc* or target* or cutback* or decreas* or limit* or consumption)).tw.
9. ((diet* or nutrition* or food or intake) adj10 (salt or sodium)).tw.
10. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9
11. exp food industry/
12. food handling/ or canned food/ or exp food preservation/ or exp food processing/
13. food additive/
14. 11 or 12 or 13
15. (adjust* or alter* or change or changing or control* or decreas* or limit* modify or modified or new or reduce or reducing or reduction* or reformulat* or redevelop* or restrict*).tw.
16. 14 and 15
17. ((adjust* or alter* or change or changing or control* or decreas* or limit* or modify or modified or new or reduce or reducing or reduction* or reformulat* or redevelop* or restrict*) adj10 (recipe* or food or foods or formula* or ingredient*)).tw.
18. 16 or 17
19. tax/
20. exp finance/ and exp government/
21. exp economics/ and exp government/
22. (pricing or cost or costs or subsidi*).tw.
23. (taxation or taxes or subsid*).tw.
24. (financial adj3 (incentive* or disincentive*)).tw.
25. reimbursement/
26. 19 or 20 or 21 or 22 or 23 or 24 or 25
27. health care policy/
28. hospital food service/
29. catering service/
30. exp school/
31. workplace/
32. prison/
33. day care/
34. ((food* or menu or nutrition*) adj5 (buy* or procur* or purchas* or stock*) adj5 (guideline* or policy or policies or practice* or standard*)).tw.
35. ((cafeteria* or diet or food* or menu* or nutrition*) adj10 (childcare or child‐care or college* or daycare* or day‐care* or fitness centre* or fitness center* or hospital* or leisure center* or leisure centre* or preschool* or pre‐school* or prison* or public facilit* or recreation center* or recreation centre* or recreation facilit* or school* or universit*)).tw.
36. 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35
37. advertizing/
38. marketing/
39. ((market* or adverti* or promot*) adj10 (adolescent* or adolescence or child or children or teenager* or teens or young people or youth*)).tw.
40. 37 or 38 or 39
41. food packaging/
42. ((food* or nutrition* or diet*) adj10 (facts or information or label* or symbol* or warning*)).tw.
43. health check.tw.
44. 41 or 42 or 43
45. mass medium/
46. exp mass communication/
47. exp health education/ or exp consumer health information/
48. information dissemination/
49. ((communicat* adj2 campaign*) or (information adj2 campaign*) or mass media or newspaper* or television* or radio* or (public adj2 campaign*) or (national adj2 campaign*) or public information).tw.
50. (blog* or email* or facebook or internet or magazine* or mobile device* or PDA or SMS or smartphone* or social media or text messag* or twitter or web).tw.
51. (health education or health information or health promotion).tw.
52. 45 or 46 or 47 or 48 or 49 or 50 or 51
53. 18 or 26 or 36 or 40 or 44 or 52
54. 10 and 53
55. limit 54 to animal studies
56. limit 54 to human
57. 55 and 56
58. 55 not 57
59. 54 not 58
Web of Science (SCI Exp and SSCI Exp)
1. TI=(monosodium glutamate* or MSG or sodium additive* or sodium alginate* or sodium benzoate* or sodium caseinate* or sodium citrate* or sodium chloride* or sodium glutamate* or sodium hydroxide* or sodium nitrate* or sodium nitrite* or sodium phosphate* or sodium propionate* or sodium saccharin* or sodium sulfite*) OR TI=((salt or sodium) AND (reduc* or target* or cutback* or decreas* or limit* or consumption)) OR TI=((diet* or nutrition* or food or intake) AND (salt or sodium))
2. Topic=((communicat* campaign* or information campaign* or mass media or newspaper* or television* or radio* or public campaign* or national campaign* or public information)) OR Title=((communicat* campaign* or information campaign* or mass media or newspaper* or television* or radio* or public campaign* or national campaign* or public information)) OR Topic=(blog* or email* or facebook or internet or magazine* or mobile device* or PDA or SMS or smartphone* or social media or text messag* or twitter or web) OR Title=(blog* or email* or facebook or internet or magazine* or mobile device* or PDA or SMS or smartphone* or social media or text messag* or twitter or web) OR Topic=(health education or health promotion or health information) OR Title=(health education or health promotion or health information)
3. Topic=(((food* or nutrition* or diet*) and (facts or information or label* or symbol* or warning*))) OR Title=(((food* or nutrition* or diet*) and (facts or information or label* or symbol* or warning*))) OR Topic=(health check) OR Title=(health check)
4. Topic=(((market* or adverti* or promot*) and (adolescent* or adolescence or child or children or teenager* or teens or young people or youth*))) OR Title=(((market* or adverti* or promot*) and (adolescent* or adolescence or child or children or teenager* or teens or young people or youth*)))
5. Topic=((cafeteria* or diet or food* or menu* or nutrition*) and (childcare or child‐care or college* or daycare* or day‐care* or fitness centre* or fitness center* or hospital* or leisure center* or leisure centre* or preschool* or pre‐school* or prison* or public facilit* or recreation center* or recreation centre* or recreation facilit* or school* or universit*)) OR Title=((cafeteria* or diet or food* or menu* or nutrition*) and (childcare or child‐care or college* or daycare* or day‐care* or fitness centre* or fitness center* or hospital* or leisure center* or leisure centre* or preschool* or pre‐school* or prison* or public facilit* or recreation center* or recreation centre* or recreation facilit* or school* or universit*)) OR Topic=((food* or menu or nutrition*) and (buy* or procur* or purchas* or stock*) and (guideline* or policy or policies or practice* or standard*)) OR Title=((food* or menu or nutrition*) and (buy* or procur* or purchas* or stock*) and (guideline* or policy or policies or practice* or standard*))
6. Topic=(pricing or cost or costs or subsidi* or taxation or taxes or subsid* or financial incentive* or financial disincentive*) OR Title=(pricing or cost or costs or subsidi* or taxation or taxes or subsid* or financial incentive* or financial disincentive*)
7. TI=((adjust* or alter* or change or changing or control* or decreas* or limit* or modify or modified or new or reduce or reducing or reduction* or reformulat* or redevelop* or restrict*))
8. 2 or 3 or 4 or 5 or 6 or 7
9. 1 and 8
LILACS
1. monosodium glutamate* or MSG or sodium or salt
2. communicat* campaign* or information campaign* or mass media or newspaper* or television* or radio* or public campaign* or national campaign* or public information
3. facts or information or label* or symbol* or warning*
4. market* or adverti* or promot*
5. cafeteria* or diet or food* or menu* or nutrition*) and (childcare or child‐care or college* or daycare* or day‐care* or fitness centre* or fitness center* or hospital* or leisure center* or leisure centre* or preschool* or pre‐school* or prison* or public facilit* or recreation center* or recreation centre* or recreation facilit* or school* or universit*))
6. food* or menu or nutrition*) and (buy* or procur* or purchas* or stock*) and (guideline* or policy or policies or practice* or standard*)
7. pricing or cost or costs or subsidi* or taxation or taxes or subsid* or financial incentive* or financial disincentive*)
8. adjust* or alter* or change or changing or control* or decreas* or limit* or modify or modified or new or reduce or reducing or reduction* or reformulat* or redevelop* or restrict*
9. 1 and 2
10. 1 and 3
11. 1 and 4
12. 1 and 5
13. 1 and 6
14. 1 and 7
15. 1 and 8
Effective Public Health Practice Project Database
TRoPHI databases
salt OR sodium [Publications/Files]
Appendix 3. Questionnaires sent to country salt reduction program leaders (Trieu 2015)
POPULATION SALT REDUCTION COUNTRY QUESTIONNAIRE
Name of country:
YOUR NAME, ORGANISATION and POSITION:
YOUR CONTACT DETAILS:
Please answer the following questions as accurately as possible, or, if you prefer, please attach the relevant documents and web links that provides answers to the questions.
1. National salt reduction initiatives
1. Is there or has there previously been any programme, policy or initiative designed to reduce population levels of salt/sodium intake in your country?This includes initiatives led by government, industry, non‐governmental organizations (NGOs) or any other agency, and may include any of the following: regulation, product reformulation, labelling, consumer awareness/ education, dietary target development, strategy development, monitoring/surveillance, research, etc.
| ☐ YES(cont. ques 1) | ☐ NO(go to ques 2) | ☐ PLANNED(cont. ques 1) |
| Name of initiative: | Time scale: | ||
| Is there a national target for dietary salt intake? | ☐ YES ☐ NO ☐ PLANNED |
If YES, what is the target? ….…... | |
| Who is the lead agency of the national salt reduction initiative? | ☐ Government ☐ NGO ☐ Food Industry ☐ Other, please specify: ….…... |
||
| Is the initiative part of a broader programme? | ☐ YES ☐ NO, the initiative is a salt‐specific programme |
||
| Are any NGOs or advocacy organisations active on salt present in the country? | ☐ YES ☐ NO |
||
2. Population salt intake
Has any work been done to measure levels of salt/sodium intake in your country?
| ☐ YES(cont. ques 2) | ☐ NO(go to ques 3) | ☐ PLANNED(cont. ques 2) |
| Year | Method (e.g. dietary survey, 24‐hour urine collection, spot urine) | Salt intake (total average, male average and female average) | |
| Please provide details on all the measurements of population salt intake in the country (Insert additional rows if needed) | |||
Has any work been done to measure the addition of salt or salty condiments to home cooking and/or at the table?
| ☐ YES. If yes, please specify how is it measured ….…... | ☐ NO | ☐ PLANNED |
3. Salt levels in foods or meals
Has any work been done to determine the salt/sodium levels in foods or meals?
| ☐ YES(cont. ques 3) | ☐ NO(go to ques 4) | ☐ PLANNED(cont. ques 3) |
| Year | Method (e.g. food analysis, survey, database, industry self report) | Food categories collected | Reduction in salt/sodium content demonstrated | |
| Please provide details on all measurements of salt levels in foods or food categories in the country. (Insert additional rows if needed) | ☐ YES. Please specify which foods: ….…... ☐ NO |
|||
| ☐ YES. Please specify which foods: ….…... ☐ NO |
4. Consumer knowledge, attitudes and behaviour
Has any work been done to determine consumer knowledge, attitude and behaviour (KAB) in relation to salt/sodium?
| ☐ YES(cont. ques 4) | ☐ NO(go to ques 5) | ☐ PLANNED(cont. ques 4) |
| Year | Method (focus group, survey) | Improvements in consumer KAB demonstrated | |
| Please provide details on all measurements of consumer knowledge, attitudes and behaviours in relation to salt in the country (Insert additional rows if needed) | ☐ Survey
☐ Focus group ☐ Other |
☐ YES ☐ NO |
|
| ☐ Survey
☐ Focus group ☐ Other |
☐ YES ☐ NO |
5. Implementation strategies
5A. ENGAGEMENT WITH INDUSTRY AND REFORMULATION Does your strategy include work with industry to achieve salt/sodium reduction in foods?
| ☐ YES(cont. ques 5a) | ☐ NO(go to ques 5b) | ☐ PLANNED(cont. ques 5a) |
| Name of initiative and year implemented | |||
| Agency/organisation taking the lead to engage industry | ☐ Government ☐ NGO |
☐ Industry ☐ Other, please specify: ….…... |
|
| Is the approach voluntary or mandatory? | ☐ Voluntary ☐ Mandatory for all food categories (e.g. maximum salt content in food) ☐ Mandatory for certain food categories such as ……………. |
||
| Approach to work with industry | ☐ Meetings with companies ☐ Voluntary commitments to salt reduction from companies ☐ Cross‐sectoral agreements to salt reduction (e.g. all bread manufacturers) ☐ Targets for salt levels in foods ☐ Taxation for high‐salt products ☐ Other, please specify ……………. |
||
| If salt reduction targets have been used, which food categories have reformulation targets? | ☐ Breads ☐ Processed meats ☐ Convenience/Ready meals ☐ Breakfast cereals ☐ Cheeses |
☐ Butter and margarines ☐ Salty snacks ☐ Biscuits and cakes ☐ Soups and sauces, ☐ Other, please specify ……………. |
|
5B. CONSUMER EDUCATION/ BEHAVIOUR CHANGE Does your strategy include activities to raise awareness/change behaviour on salt/sodium?
| ☐ YES(cont. ques 5b) | ☐ NO(go to ques 5c) | ☐ PLANNED(cont. ques 5b) |
| Name of initiative and year implemented | ||
| Agency/Organisation taking the lead | ☐ Government ☐ NGO ☐ Industry ☐ Other, please specify: |
☐ Government ☐ NGO ☐ Industry ☐ Other, please specify: |
| Approach | ☐ Social marketing (e.g. campaigns) ☐ TV advertising ☐ Events ☐ Other, please specify: |
☐ Social marketing (e.g. campaigns) ☐ TV advertising ☐ Events ☐ Other, please specify: |
5C. FRONT OF PACK LABELLING Has your country introduced front of pack labelling to indicate nutritional or salt/sodium content of food?
| ☐ YES(cont. ques 5c) | ☐ NO(go to ques 5d) | ☐ PLANNED(cont. ques 5c) |
| Name of initiative and year implemented | |
| Agency/Organisation taking the lead | ☐ Government ☐ Industry ☐ NGO ☐ Other |
| Is the approach voluntary or mandatory? | ☐ Voluntary ☐ Mandatory for all food categories ☐ Mandatory for certain food categories such as ……………. |
| Approach/detail of the label (traffic light code, logo, % daily intake) | ☐ Traffic light code ☐ Other logo or symbol ☐ Warning labels ☐ Percentage of daily intake ☐ Other, please specify ……………. |
| ☐ YES(cont. ques 5d) | ☐ NO(go to ques 6) | ☐ PLANNED(cont. ques 5d) |
5D. WORK IN SPECIFIC SETTINGS Does the strategy include work on salt/sodium in particular settings such as schools, hospitals or workplaces?
| Name of initiative and year implemented | ||
| Setting | ☐ School ☐ Hospital |
☐ Workplace ☐ Other, please specify ……………. |
| Approach to work in particular settings | ☐ Education ☐ Procurement policy |
☐ Voluntary guidelines ☐ Other, please specify ……………. |
6. Evaluation
Has your country done any work to evaluate the overall effectiveness of salt/sodium reduction strategy, in addition to monitoring salt intake, salt levels and consumer KAB? (for example, process evaluation or cost‐effectiveness analysis)
| ☐ YES(cont. ques 6) | ☐ NO(end of survey) | ☐ PLANNED(cont. ques 6) |
For each evaluation, please specify:
(please copy and paste the table below as needed, 1 table per evaluation)
| Year evaluated | |
| Evaluation approach | |
| Results (Has it had an impact?) | |
| Has a cost‐effective analysis been undertaken? | ☐ YES ☐ NO ☐ PLANNED |
| Was the programme cost‐effective? | ☐ YES ☐ NO |
Please attach any documents and website links relevant to the questions.
THANK YOU FOR COMPLETING THIS QUESTIONNAIRE. We value your time. Please send the completed questionnaire and relevant documents to (...)
Data and analyses
Comparison 1. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ OVERALL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Salt intake in grams per day | 12 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 2. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ SUBSET OF MULTI‐COMPONENT INITIATIVES THAT INCLUDE STRUCTURAL ACTIVITIES.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Salt intake in grams per day | 9 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 3. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ WOMEN ONLY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Salt intake in grams per day | 11 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 4. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ MEN ONLY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Salt intake in grams per day | 11 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 5. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ using other available post‐intervention data points.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Salt intake in grams per day | 12 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 6. Mean change in salt intake (grams/d) from pre‐intervention to post‐intervention ‐ using other available pre‐intervention data points.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Salt intake in grams per day | 12 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Austria.
| Methods | Uncontrolled pre‐post | |
| Participants | Austrian Study on Nutritional Status 2008: individuals recruited through quota sampling Austrian Study on Nutritional Status 2012: kids, adults and elderly recruited through quota sampling |
|
| Interventions | Salt reduction initiative began in 2011. Efforts included:
|
|
| Outcomes | Austrian Study on Nutritional Status 2008: mean dietary salt intake (grams/d) estimated via 24‐hour dietary recall Austrian Study on Nutritional Status 2012: mean dietary salt intake (grams/d) estimated via two 24‐hour dietary recalls |
|
| Axes of inequality | Austrian Study on Nutritional Status 2008: gender Austrian Study on Nutritional Status 2012: gender |
|
| Sample size and response rate | Austrian Study on Nutritional Status 2008: n = 2123 (778 M; 1345 F), 48% response rate (RR) Austrian Study on Nutritional Status 2012: n = 380 (148 M; 232 F), RR not available (Note: We are focusing only on the 380 adult respondents to be comparable with Austrian Study on Nutritional Status 2008) |
|
| Funding source / Conflict of Interest (COI) | Austrian Study on Nutritional Status 2008 and 2012: funding source not provided/COI statement not provided | |
| Notes | Sources of data points and references: see Austria Austrian Study on Nutritional Status 2008: World Health Organization (WHO). Mapping of salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013;1‐50 *Austria country questionnaire and associated correspondence 2014‐2015 Austrian Study on Nutritional Status 2012: *Austria country questionnaire and associated correspondence 2014‐2015 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | Austrian Nutrition Reports 2008 and 2012 employed a non‐random quota sampling technique |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Unclear risk | The 2008 data point used a 24‐hour dietary recall, which was administered once. The 2012 data point used a 24‐hour dietary recall, which was administered twice. Reliability and validity of this dietary survey were not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data (Austrian Nutrition Reports) were used to evaluate the initiative |
| Representativeness of sample | Unclear risk | No discussion included representativeness of the sample |
| Selective reporting (reporting bias) | Low risk | Means and confidence intervals were reported for overall estimates |
| Other bias | Low risk | No other obvious sources of bias to report |
Canada.
| Methods | Uncontrolled pre‐post | |
| Participants | Nutrition Canada Survey 1970‐1972: stratified, multi‐stage probability sampling technique for individuals of all ages from the 10 provinces Canadian Community Health Survey 2004: stratified, multi‐stage probability sampling technique for residents aged 2+ from the 10 provinces |
|
| Interventions | Salt reduction initiative began in 1982. Efforts included:
|
|
| Outcomes | Nutrition Canada Survey 1970‐1972: mean sodium consumption (milligrams/d) estimated via 24‐hour dietary recall Canadian Community Health Survey 2004: mean sodium consumption (milligrams/d) estimated via 24‐hour dietary recall |
|
| Axes of inequality | Nutrition Canada Survey 1970‐1972: gender, education and income Canadian Community Health Survey 2004: gender, education and income |
|
| Sample size and response rate | Nutrition Canada Survey 1970‐1972: n = 4540 (1974 M; 2566 F); ages 25 to 64, 46% RR for overall survey Canadian Community Health Survey 2004: n = 10,449 (4837 M; 5612 F); 76.5% RR for overall survey |
|
| Funding source / Conflict of Interest (COI) | Nutrition Canada Survey 1970‐1972 and Canadian Community Health Survey 2004: Study was funded by an operating grant from the Canadian Institutes of Health Research (CIHR) Institute of Nutrition, Metabolism and Diabetes (INMD) and Institute of Population and Public Health (IPPH)/Study authors declare no COI, except Dr. Norm Campbell, who declares: received travel funds from McCain to attend a regional Dieticians of Canada meeting to talk about the importance of reducing dietary sodium (2007); received samples of Mrs DASH; asked not to send more (2008); received travel funds from Boehringer Ingelheim to attend 2 hypertension meetings (2010); receive salary from the Heart and Stroke Foundation of Canada (HSFC) and CIHR to lead and co‐ordinate efforts to prevent and control hypertension; serve as an unpaid consultant for many non‐governmental organisations (NGOs) and governmental organisations (GOs), but none with a commercial flavour; receive occasional honoraria for speaking to academic groups on sodium (e.g. Canadian Council of Cardiovascular Nurses) | |
| Notes | Sources of data points and references: see Canada Nutrition Canada Survey 1970‐1972 and Canadian Community Health Survey 2004: *McLaren L, Heidinger S, Dutton DJ, Tarasuk V, Campbell NR. A repeated cross‐sectional study of socio‐economic inequities in dietary sodium consumption among Canadian adults: implications for national sodium reduction strategies. International Journal for Equity in Health 2014;13(1):44 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Both surveys used stratified, multi‐stage probability sampling technique to ensure representation of the 10 Canadian provinces |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | High risk | Estimates of sodium intake were based on 24‐hour dietary recall data from both surveys. Study authors identified that surveys are not directly comparable because of changes to survey content and administration over time |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Low risk | Both surveys used are national nutritional surveys. Study authors applied a sampling weight to account for the complex sampling design and patterns of non‐response. Crude comparisons were made between the Nutrition Canada Survey and the Canadian census, which indicated that the populations were similar |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported for sodium intake |
| Other bias | Low risk | No other obvious sources of bias to report |
China.
| Methods | Open‐cohort study (in addition to ongoing participants, replenishment samples are recruited at each wave) | |
| Participants | 1991, 1993, 1997, 2000, 2004, 2006 and 2009: multi‐stage, random‐cluster process used to recruit adults 20 to 60 years of age from Heilongjiang, Liaoning, Jiangsu, Shandong, Henan, Hubei, Hunan, Guizhou and Guangxi | |
| Interventions | Salt reduction initiative began in 2006. Efforts included:
|
|
| Outcomes | 1991, 1993, 1997, 2000, 2004, 2006 and 2009: mean sodium intake (grams/d) estimated from dietary data obtained from 3 consecutive 24‐hour dietary recalls and condiment and food weights | |
| Axes of inequality | 1991, 1993, 1997, 2000, 2004, 2006 and 2009: gender, place of residence, education and income | |
| Sample size and response rate | 1991, 1993, 1997, 2000, 2004, 2006 and 2009: n = 16,869, ˜ 88% at inception at the individual level and 90% at the household level | |
| Funding source / Conflict of Interest (COI) | 1991, 1993, 1997, 2000, 2004, 2006 and 2009: funding source not provided/no COI declared by study authors | |
| Notes | Sources of data points and references: see China 1991, 1993, 1997, 2000, 2004, 2006 and 2009: *Du S, Neiman A, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. American Journal of Clinical Nutrition 2014;99:334‐343 2011 data point from Shandong province only: Bi Z, Liang X, Xu A, Wang L, Shi X, Zhao W et al. Hypertension prevalence, awareness, treatment, and control and sodium intake in Shadong province, China: baseline results from Shadong‐Ministry of Health Action on Salt Reduction and Hypertension (SMASH). Preventing Chronic Disease 2011;11(E88) *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Sample was selected from 9 Chinese provinces through a multi‐stage random‐cluster process |
| Confounding | High risk | Uncontrolled study designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | 3 consecutive 24‐hour dietary recalls were used to measure sodium levels, both at household and individual levels. Validation of the dietary survey method was described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Unclear risk | Representativeness of the sample of the Chinese population was not discussed |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported for all years |
| Other bias | Low risk | Changes to the Chinese food environment may contribute to decreased sodium levels, including “marked advancements in the transportation of food”, and “added salt intake has decreased faster in the North than in the South” (Du 2014, pg. 339). Refrigerator ownership, among other changes, has increased as the result of “rapid modernization and urbanization” (Du 2014, pg. 340), thus salt is no longer needed as a major food preservative. Study authors discuss these potential reasons for salt reduction but do not account for them in their analysis. However, these issues are captured under the "confounding" domain |
Denmark.
| Methods | Uncontrolled pre‐post | |
| Participants | Danish Health 2006: Participants were drawn as a random sample from a list provided by the Danish Central Personal Register; 18 to 69 years of age, living in 11 municipalities in the Southwestern part of the greater Copenhagen area Danish National Survey of Dietary Habits and Physical Activity 2008: nationwide, representative, cross‐sectional survey of individuals 15 to 75 years of age in Denmark Danish Health 2010: participants drawn as a random sample from the Danish Central Personal Register; 18 to 69 years of age, living in the Western part of the Copenhagen region |
|
| Interventions | Salt reduction initiative began in 2008. Efforts included:
|
|
| Outcomes | Danish Health 2006: median salt intake (grams/d) estimated via spot urine. “Daily salt intake was calculated using the Danish Model, a simple method based on spot urine sodium and creatinine to predict the 24‐hour sodium excretion" Danish National Survey of Dietary Habits and Physical Activity 2008: mean salt intake (grams/d) estimated via a 7‐day food record Danish Health 2010: median salt intake (grams/d) estimated via spot urine. “Daily salt intake was calculated using the Danish Model, a simple method based on spot urine sodium and creatinine to predict the 24‐hour sodium excretion” |
|
| Axes of inequality | Danish Health 2006: gender Danish National Survey of Dietary Habits and Physical Activity 2008: gender Danish Health 2010: gender |
|
| Sample size and response rate | Danish Health 2006: n = 3294 (1477 M; 1817 W); 44.7% of contacted individuals participated in study and underwent health examinations Danish National Survey of Dietary Habits and Physical Activity 2008: n = 3528 (1639 M; 1889 W); 53% RR Danish Health 2010: n = 1478 (647 M, 831 W); 40.5% participation rate |
|
| Funding source / Conflict of Interest (COI) | Danish Health 2006: funding source not provided/COI statement not provided Danish National Survey of Dietary Habits and Physical Activity 2008: funding source not provided (data collected as part of the Danish National Survey of Dietary Habits and Physical Activity)/country contact states no COI exists Danish Health 2010: funding source not provided/COI statement not provided |
|
| Notes | Sources of data points and references: see Denmark Danish Health 2006: *Denmark country questionnaire and associated correspondence. 2014‐2015 Danish National Survey of Dietary Habits and Physical Activity 2008: *Denmark country questionnaire and associated correspondence. 2014‐2015 Danish Health 2010: *Denmark country questionnaire and associated correspondence. 2014‐2015: Christensen AI, Ekholm O, Glumer C, Andreasen A, Hvidberg MF, Kristensen PL, Larsen FB, Ortiz B, Juel K. The Danish National Health Survey 2010. Study design and respondent characteristics. Scandinavian Journal of Public Health 2012;40:391‐397 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Danish Health 2006 used a random sample from the background population. Danish Health 2010 recruited participants from the Danish Central Personal Register as a random sample of the background population |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | 24‐Hour urine samples were collected for both time points. Convincing text suggests protocols were adhered to, and that the method was properly carried out for both years. Validation of the tools was described elsewhere. Completeness of the urine collection was measured |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Unclear risk | Detailed discussion of representativeness of sample is not provided |
| Selective reporting (reporting bias) | High risk | Means and standard deviations or 95% confidence intervals not reported (provides median and 5th, 95th percentiles) |
| Other bias | Low risk | No other obvious sources of bias to report |
Finland.
| Methods | Uncontrolled pre‐post; controlled pre‐post | |
| Participants | 1979: representative sample 15 to 65 years of age drawn from the population register in North Karelia and Kuopio area (Note: We are considering only those participants from North Karelia and the Kuopio area) 1982: sex‐stratified random sample 25 to 64 years of age from North Karelia, Kuopio area, Turku and Loimaa region (Note: We are considering only those participants from North Karelia and the Kuopio area) 1987: sex‐stratified random sample 25 to 64 years of age from North Karelia, Kuopio area, Turku and Loimaa region (Note: We are considering only those participants from North Karelia and the Kuopio area) 2002: sex‐stratified subsample of the population 25 to 64 years of age from North Karelia, Turku, Loimaa region and Helsinki area (Note: We are considering only those participants from North Karelia) 2007: stratified random sample of adults 24 to 64 years of age from the Finnish Population Information System in 5 regions in Finland 2012: random sample of adults 25 to 74 years of age drawn from the Population Register in 5 regions in Finland (Note: We are considering only those who are 25 to 64 years of age) |
|
| Interventions | Salt reduction initiative began in 1979. Efforts included:
|
|
| Outcomes | 1979: sodium excretion (mmol/d) and mean salt intake (grams/d) estimated via 24‐hour urine 1982: sodium excretion (mmol/d) and mean salt intake (grams/d) estimated via 24‐hour urine 1987: sodium excretion (mmol/d) and mean salt intake (grams/d) estimated via 24‐hour urine 2002: sodium excretion (mmol/d) and mean salt intake (grams/d) estimated via 24‐hour urine 2007: mean salt intake (grams/d) estimated via 48‐hour dietary recall 2012: mean sodium intake (grams/d) estimated via 48‐hour dietary recall |
|
| Axes of inequality | 1979: gender and education 1982: gender and education 1987: gender and education 2002: gender and education 2007: gender 2012: gender, place of residence and education |
|
| Sample size and response rate | 1979: n = 1206 (611 M; 595 W); 64% RR for urine sample n = 536 (268 M; 268 W) for North Karelia n = 670 (343 M; 327 W) for Kuopio area 1982: n = 1382 (692 M; 690 F); 68% provided urine sample n = 484 (247 M; 237 W) for North Karelia n = 428 (213 M; 215 W) for Kuopio area 1987: n = 1151 (529 M, 622 F); 54% provided urine sample n = 409 (199 M; 210 W) for North Karelia n = 400 (180 M; 220 W) for Kuopio area 2002: n = 909 (423 M; 486 F); 59% provided urine sample n = 342 (168 M; 174 W) for North Karelia 2007: n = 1576 (730 M; 846 F); 33% participated in dietary survey 2012: n = 1708; 33% participated in dietary survey n = 1295 (585 M; 710 W); 25 to 64 years of age |
|
| Funding source / Conflict of Interest (COI) | 1979, 1982, 1987, 2002: funded by the National Public Health Institute/COI statement not provided 2007: funding source not provided/COI statement not provided 2012: survey conducted by The National Institute for Health and Welfare/COI statement not provided |
|
| Notes | Sources of data points and references: see Finland 1979, 1982, 1987, 2002: *Laatikainen T, Pietinen P, Valsta L, Sundvall J, Reinivuo H, Tuomilehto J. Sodium in the Finnish diet: 20‐year trends in urinary sodium excretion among the adult population. European Journal of Clinical Nutrition 2006;60(8):965‐970 2007: Finland country questionnaire 2014: Pietinen P, Paturi M, Reinivuo H, Tapanainen H, Valsta LM. FINDIET 2007 Survey: energy and nutrient intakes. Public Health Nutrition 2010;13(6A):920‐924 2012: Finland country questionnaire 2014: Helldán A, Raulio S, Kosola M, Tapanainen H, Ovaskainen M, Virtanen S. Finravinto 2012 ‐ tutkimus. The National FINDIET 2012 Survey. National Institute for Health and Welfare 2013;16 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Representative sample drawn from a population register |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | 24‐Hour urine collection for all years. Convincing text indicates that data collection was administered carefully |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Low risk | Representative sample was drawn from a population register. No indication that the subsample differed from the population |
| Selective reporting (reporting bias) | Low risk | Means and confidence intervals were reported for all values |
| Other bias | Low risk | No other obvious sources of bias to report |
France.
| Methods | Uncontrolled pre‐post | |
| Participants | Individual and National Food Consumption Survey (INCA1) 1998‐1999 (a): nationally representative, stratified, random sample of individuals 15 years of age and older. *Study considers only adults 18 to 79 years of age to be comparable with INCA2 Individual and National Food Consumption Survey (INCA1) 1998‐1999 (b): “The sampling design used to select nationally representative samples of adults and children living in French households included a stratification by region of residence and community size and a distribution according to age, gender, household size and head of household socio‐professional status by the quota method” Individual and National Food Consumption Survey (INCA2) 2006‐2007: nationally representative, stratified, random sample of individuals 18 to 79 years of age |
|
| Interventions | Salt reduction initiative began in 2001. Efforts included:
|
|
| Outcomes | INCA1 1998‐1999 (a): mean sodium intake (milligrams/d) estimated via 7‐day open‐ended food records INCA1 1998‐1999 (b): mean sodium intake (mmol/d) estimated via 7‐day open‐ended food records INCA2 2006‐2007: mean sodium intake (milligrams/d) estimated via 7‐day open‐ended food records |
|
| Axes of inequality | INCA1 1998‐1999 (a): gender INCA1 1998‐1999 (b): gender, place of residence and occupation INCA2 2006‐2007: gender |
|
| Sample size and response rate | INCA1 1998‐1999 (a): n = 1985; unknown RR Analysis performed on n = 1345 (613 M; 732 W) INCA1 1998‐1999 (b): n = 1985; unknown RR Analysis performed on n = 1474 (672 M; 802 W) INCA2 2006‐2007: n = 2624; 63% RR Analysis performed on n = 1922 (840 M; 1082 W) |
|
| Funding source / Conflict of Interest (COI) | INCA1 1998‐1999 (a): "The INCA1 survey was supported by a grant from the Ministries for Health, Agriculture and Consumer Affairs"/Study authors declare no COI INCA1 1998‐1999 (b): INCA1 was performed by the French Food Safety Agency. “Joel Menard received funding from the Association Robert Debre ´pour la Recherche Medicale and Pierre Meneton from the Institut National pour la Sante´ et la Recherche Medicale”/Study authors declare no COI 2006‐07: “INCA2 [was supported] by a grant from the French Food Safety Agency (AFSSA)”/Study authors declare no COI |
|
| Notes | Sources of data points and references: see France INCA1 1998‐1999 (a): France country questionnaire 2014: *Dubuisson C, Lioret S, Touvier M, Dufour A, Calamassi‐Tran G, Volatier J‐L, Lafay L. Trends in food and nutritional intakes of French adults from 1999 to 2007: results from the INCA surveys. British Journal of Nutrition 2010;103:1035‐1048 INCA1 1998‐1999 (b): France country questionnaire 2014: Meneton P, Lafay L, Tard A, Dufour A, Ireland J, Ménard J, Volatier JL. Dietary sources and correlates of sodium and potassium intakes in the French general population. European Journal of Clinical Nutrition 2009;63:1169‐1175 INCA2 2006‐2007: France country questionnaire 2014: *Dubuisson et al., 2010 (see full citation above) *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Representative samples through stratification and “quota method” were used for INCA1 1998‐1999. Random samples used multi‐stage cluster sampling for INCA2 2005‐2007 |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | Dietary surveys were used for both time points and used comparable methods. Convincing text suggests protocols were adhered to, and that the method was properly carried out for both years |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Low risk | “Two independent samples… were made representative of the French population through stratification and use of the quota method” (pg. 1036). No indication that the sample differed from the population |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported for both men and women for all measures |
| Other bias | Low risk | No other obvious sources of bias to report |
Ireland.
| Methods | Uncontrolled pre‐post | |
| Participants | North‐South Ireland Food Consumption Survey 1997‐1999: random sample of adults 18 to 64 years of age from the electoral register as the sampling frame from the entire island of Ireland Survey of Lifestyle, Attitudes and Nutrition (SLAN) in Ireland 1998: multi‐stage sample drawn by electoral division from the Electoral Register of adults 18 years of age and older across 26 counties in Ireland Survey of Lifestyle, Attitudes and Nutrition (SLAN) in Ireland 2002: multi‐stage sample drawn by electoral division from the Electoral Register of adults 18 years of age and older across 26 counties in Ireland. *Convenience sample for some of the urine Survey of Lifestyle, Attitudes and Nutrition (SLAN) in Ireland 2007 (a): multi‐stage probability sample from the Geodirectory of adults 18 years of age and older, living in private households in the Republic of Ireland *For the food frequency questionnaire (FFQ) component, adults 18 to 90 years of age were included Survey of Lifestyle, Attitudes and Nutrition (SLAN) in Ireland 2007 (b): multi‐stage probability sample from the Geodirectory of adults 18 years of age and older, living in private households in the Republic of Ireland *For the spot urine component, samples were obtained from a subsample of adults 45 years of age and older from the larger survey Survey of Lifestyle, Attitudes and Nutrition (SLAN) in Ireland 2007 (c): multi‐stage probability sample from the Geodirectory of adults 18 years of age and older, living in private households in the Republic of Ireland *For the 24‐hour urine component, samples were obtained from adults 18 to 81 years of age from 3 subsamples: (1) a general population sample from 2007 SLAN and participants of the 1998 Cork and Kerry Diabetes and Heart Disease Study, (2) student volunteers and (3) an occupational group National Adult Nutrition Survey 2008‐2010: representative sample of adults 18 years of age and older in the Republic of Ireland |
|
| Interventions | Salt reduction initiative started in 2003. Efforts included:
|
|
| Outcomes | North‐South Ireland Food Consumption Survey 1997‐1999: mean salt intake (grams/d) estimated via 7‐day diet diaries 1998: mean salt intake (grams/d) estimated via food frequency questionnaire – does not include discretionary salt 2002: mean salt intake (grams/d) estimated via food frequency questionnaire – does not include discretionary salt 2007 (a): mean salt intake (grams/d) estimated via food frequency questionnaire – does not include discretionary salt 2007 (b): mean salt intake (grams/d) estimated via spot urine samples 2007 (c): mean salt intake (grams/d) estimated via 24‐hour urine samples National Adult Nutrition Survey 2008‐2010: mean salt intake (grams/d) estimated via 4‐day semi weighted food record – does not include discretionary salt |
|
| Axes of inequality | North‐South Ireland Food Consumption Survey 1997‐1999: gender SLAN of Ireland 1998: gender SLAN of Ireland 2002: gender SLAN of Ireland 2007 (a): gender and social class SLAN of Ireland 2007 (b): gender SLAN of Ireland 2007 (c): gender National Adult Nutrition Survey 2008‐2010: gender |
|
| Sample size and response rate | North‐South Ireland Food Consumption Survey 1997‐1999: n = 1379 (662 M; 717 W); 63% RR SLAN of Ireland 1998: n = 6539; 62% RR SLAN of Ireland 2002: n = 5992; 53% RR SLAN of Ireland 2007 (a): n = 10,364 overall; 62% RR (for larger survey); n = 9172 (4511 M; 4661 W) (89%); provided complete information for FFQ SLAN of Ireland 2007 (b): n = 1207 (spot urine sample); 62% RR (for larger survey) SLAN of Ireland 2007 (c): n = 599 (24‐hour urine sample); 62% RR (for larger survey) National Adult Nutrition Survey 2008‐2010: n = 1500 (740 M; 760 W); 60% RR |
|
| Funding source / Conflict of Interest (COI) | North‐South Ireland Food Consumption Survey 1997‐1999: Funders of the survey include “the Department of Agriculture, Food and Rural Development in Dublin through the Non Commissioned Food Research Programme, part financed by the European Regional Development Fund. The Food Safety Authority of Ireland and its predecessor, the Food Safety Advisory Board. The Northern Ireland Centre for Diet and Health at the University of Ulster, which is assisted by the European Regional Development Fund through the IRTU Technology Development Programme. Industrial partners: Kelloggs, Bord Bia, Coca‐Cola, Cadburys, Dairy Council for Northern Ireland, Irish Sugar, Kerry Group, Mars Confectionery, Meat and Livestock Commission UK, National Dairy Council, Nestlé Ireland, Tesco Ireland and the Irish Business and Employers Confederation (IBEC)”/COI statement not provided SLAN of Ireland 1998: “The 1998 SLÁN survey was conducted by the Centre for Health Promotion Studies at NUI Galway on behalf of the Health Promotion Unit of the Department of Health”/COI statement not provided in report by Perry 2010, where estimate was obtained SLAN of Ireland 2002: “…commissioned by the Health Promotion Unit of the Department of Health & Children and carried out at the Centre for Health Promotion Studies at NUI Galway and at the Department of Public Health Medicine and Epidemiology, University College Dublin”/COI statement not provided in report by Perry 2010, where estimate was obtained SLAN of Ireland 2007 (a), 2007 (b) and 2007 (c): “The SLÁN 2007 survey was commissioned by the Health Promotion Unit of the Department of Health & Children and carried out by Royal College of Surgeons (RCSI), The Economic and Social Research Institute (ESRI), University College Cork (UCC) and The National University of Ireland Galway (NUIG)”/COI statement not provided in report by Perry 2010, where estimate was obtained National Adult Nutrition Survey 2008‐2010: “The funding to carry out this survey was provided under the Food for Health Research Initiative (FHRI). The FHRI is a joint initiative established by the Department of Agriculture, Fisheries & Food, the Department of Health & Children and the Health Research Board. The FHRI is supported by funds provided under the Strategy for Science, Technology and Innovation 2006‐2013 for linked public sector research, the Food Institutional Research Measure and the HRB. The team is also grateful to the Food Safety Authority of Ireland for funding additional analysis of the survey to address jet issues on food safety and nutrition”/no COI statement provided |
|
| Notes | Sources of data points and references: see Ireland North‐South Ireland Food Consumption Survey 1997‐1999: Ireland country questionnaire and associated correspondence. 2014‐2015; Irish Universities Nutrition Alliance. North/South Ireland food consumption survey. Irish Universities Nutrition Alliance 2011 SLAN of Ireland 1998, 2002, 2007 (a), 2007 (b) and 2007 (c): Ireland country questionnaire and associated correspondence. 2014‐2015: *Perry IJ, Browne G, Loughrey M, Harrington J, Lutomski J, Fitzgerald AP. Dietary salt intake and related risk factors in the Irish population. A report for safe food. 2010. ISBN: 978‐1‐905767‐13‐7. Irish Social Science Data Archive Website. http://www.ucd.ie/issda/: Harrington J, Perry I, Lutomski J, Morgan K, McGee H, Shelley E, Watson D, Barry M. SLÁN 2007: Survey of Lifestyle, Attitudes and Nutrition in Ireland. Dietary Habits of the Irish Population. Dublin: Department of Health and Children, 2008; Morgan K, McGee H, Watson D, Perry I, Barry M, Harrington SE et al. SLAN 2007: Survey of Lifestyle, Attitudes & Nutrition in Ireland. Main Report. 2008 National Adult Nutrition Survey 2008‐2010: Ireland country questionnaire and associated correspondence. 2014‐2015. Irish Universities Nutrition Alliance. North/South Ireland food consumption survey. Irish Universities Nutrition Alliance 2011 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | SLAN 1998 and 2002 used Electoral Register. SLAN 2007 used a nationally representative household sample (the Geodirectory). Both methods used random samples |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | Food frequency questionnaires. Convincing text suggests protocols were adhered to, and that the method was properly carried out for both years. The survey and methods of collection were described in detail (Perry 2010, pg. 34; Harrington 2008) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | High risk | Harrington et al. ‐ SLAN 2002 and 2007. Both used similar methods of sample weighting to account for differences in sampling methods. However, "there are potentially significant volunteer biases in both the SLÁN‐07 and the Phase II study, due to declining response rates for health and nutritional surveys…elderly and individuals from socially and economically disadvantaged backgrounds…were underrepresented. Thus it is likely that we are underestimating average salt intakes in the population” (Perry 2010, pg. 65) |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported for overall estimates |
| Other bias | Low risk | No other obvious sources of bias to report |
Japan.
| Methods | Uncontrolled pre‐post | |
| Participants | National Nutrition Survey 1997: individuals from randomly selected households in the National Nutrition Survey National Health and Nutrition Survey 2003‐2010, 2012: individuals 1+ years of age from households in 300 randomly selected districts in the National Health and Nutrition Survey |
|
| Interventions | Salt reduction initiative started in 2001. Efforts included:
|
|
| Outcomes | National Nutrition Survey 1997 and National Health and Nutrition Survey 2003‐2010, 2012: mean salt intake (grams/d) estimated via a nutritional intake survey | |
| Axes of inequality | National Nutrition Survey 1997: none National Health and Nutrition Survey 2003‐2010: gender National Health and Nutrition Survey 2012: none |
|
| Sample size and response rate | National Nutrition Survey 1997: n = 13,289; RR for dietary intake survey not officially reported National Health and Nutrition Survey 2003: 11,105 (dietary survey); RR for dietary intake survey not officially reported National Health and Nutrition Survey 2004: n = 8762 (dietary survey); RR for dietary intake survey not officially reported National Health and Nutrition Survey 2005: 8895 (dietary survey); RR for dietary intake survey not officially reported National Health and Nutrition Survey 2006: 9423 (dietary survey); RR for dietary intake survey not officially reported National Health and Nutrition Survey 2007: 8885 (dietary survey); RR for dietary intake survey not officially reported National Health and Nutrition Survey 2008: 9129 (dietary survey); RR for dietary intake survey not officially reported National Health and Nutrition Survey 2009: 9006 (dietary survey); RR for dietary intake survey not officially reported National Health and Nutrition Survey 2010: n = 8815 (dietary survey); 69% RR for dietary survey National Health and Nutrition Survey 2012: n = 32,228 (dietary survey); 52% RR for dietary survey |
|
| Funding source / Conflict of Interest (COI) | National Nutrition Survey 1997: survey conducted by Ministry of Health, Labour and Welfare/authors of published study declare no COI National Health and Nutrition Survey 2003‐2010: survey conducted by Ministry of Health, Labour and Welfare/authors of published study declare no COI National Health and Nutrition Survey 2012: survey conducted by Ministry of Health, Labour and Welfare/no COI statement provided |
|
| Notes | Sources of data points and references: see Japan National Nutrition Survey 1997: Japan country questionnaire 2014: *Udagawa K, Miyoshi M, Yoshiike N. Mid‐term evaluation of “Health Japan 21”: focus area for the nutrition and diet. Asia Pacific Journal of Clinical Nutrition 2008;17(S2):445‐452 National Health and Nutrition Survey 2003, 2005‐2007, 2009: Miura K, Ando K, Tsuchihashi T, Yoshita K, Watanabe Y, Kawarazaki H, Matsuura H, Kusaka M, Kai M, Kawamura M, Kawano Y. [Scientific Statement] Report of the Salt Reduction Committee of the Japanese Society of Hypertension (2): goal and strategies of dietary salt reduction in the management of hypertension. Hypertension Research 2013;36:1020‐1025 National Health and Nutrition Survey 2004 and 2010: Japan country questionnaire 2014; Miura et al., 2013 (see above) National Health and Nutrition Survey 2008: Miura et al., 2013 (see above) National Health and Nutrition Survey 2012: Japan country questionnaire 2014 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Sampling methods not discussed |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Unclear risk | Study authors do not discuss the methods by which sodium was measured |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Unclear risk | Articles do not discuss how representative the sample is of Japan |
| Selective reporting (reporting bias) | High risk | No standard deviations or confidence intervals reported |
| Other bias | Low risk | No other obvious sources of bias to report |
Netherlands.
| Methods | Uncontrolled pre‐post | |
| Participants | 2006: Half of the study population was recruited from individuals (35 to 70 years of age) participating in a long‐term monitoring study on chronic risk factors (the Doetinchem Cohort Study (DCS)), and half of the participants (19 to 45 years of age) were randomly drawn from the municipal register of Doetinchem (General Doetinchem Population Sample (GDPS)) National Food Consumption Survey 2007‐2010: nationally representative sample of participants 7 to 69 years of age 2010: Half of the study population was recruited from individuals (35 to 70 years of age) participating in a long‐term monitoring study on chronic risk factors (the Doetinchem Cohort Study (DCS)), and half of the participants (19 to 45 years of age) were randomly drawn from the municipal register of Doetinchem (General Doetinchem Population Sample (GDPS)) |
|
| Interventions | Salt reduction initiative began in 2007. Efforts included:
|
|
| Outcomes | 2006: median sodium excretion (mmol/d) and median salt intake (grams/d) estimated via 24‐hour urine collections National Food Consumption Survey 2007‐2010: mean salt intake (grams/d) estimated via 2 non‐consecutive 24‐hour recalls 2010: median sodium excretion (mmol/d) and median salt intake (grams/d) estimated via 24‐hour urine collections |
|
| Axes of inequality | 2006: gender National Food Consumption Survey 2007‐2010: gender 2010: gender |
|
| Sample size and response rate | 2006: n = 317 (137 M; 180 W); 68% from DCS and 19% RR from GDPS National Food Consumption Survey 2007‐2010: n = 3819; 69.4% RR. *Analysis was performed on 2106 men and women 19 to 69 years of age (1055 M; 1051 W) 2010: n = 342 (154 M; 188 W); 69% from DCS and 15% RR from GDPS |
|
| Funding source / Conflict of Interest (COI) | 2006 and 2010: funding provided by the Dutch Ministry of Health, Welfare and Sport and Wageningen University/authors stated no COI National Food Consumption Survey 2007‐2010: funded by the Dutch Ministry of Health, Welfare and Sports/no COI exists |
|
| Notes | Sources of data points and references: see Netherlands 2006 and 2010: Netherlands country questionnaire and associated correspondence 2014‐2015: *Hendriksen MAH, van Raaij JMA, Geleijnse JM, Wilson‐van den Hooven C, Ocké MC, van der A DL. Monitoring salt and iodine intakes in Dutch adults between 2006 and 2010 using 24 hour urinary sodium and iodine excretions. Public Health Nutrition 2013. doi:10.1017/S1368980013001481 National Food Consumption Survey 2007‐2010: Netherlands country questionnaire and associated correspondence 2014‐2015 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | Two different sources were used to obtain data for the age range of interest (independent, random samples of both the general population and the Doetinchem Cohort Study) |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | Both 24‐hour urine collections and questionnaires were used. Identical protocols and procedures were used between both years. Convincing text suggests protocols were adhered to, and that the method was properly carried out for both years. Investigators noted that they did not have a reliable method to assess the completeness of 24‐hour urine collections, but they provide reason to believe that this is not an issue |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information was provided |
| Representativeness of sample | High risk | Education and smoking differences between the sample and the population were reported |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported for overall estimates |
| Other bias | Low risk | No other obvious sources of bias to report |
New Zealand.
| Methods | Uncontrolled pre‐post | |
| Participants | New Zealand Total Diet Study 2003‐2004: simulated diet developed from listed foods for different population groups of New Zealanders New Zealand Adult Nutrition Survey 2008‐2009 (a): civilian population 15 years of age and older living in permanent private dwellings in New Zealand New Zealand Adult Nutrition Survey 2008‐2009 (b): civilian population 15 years of age and older living in permanent private dwellings in New Zealand. *In addition to the multiple‐pass 24‐hour dietary recall, consenting participants provided a urine sample New Zealand Total Diet Study 2009: simulated diet developed from listed foods for different population groups of New Zealanders |
|
| Interventions | Salt reduction initiative began in 2005. Efforts included:
|
|
| Outcomes | New Zealand Total Diet Study 2003‐2004: mean sodium intake (milligrams/d) New Zealand Adult Nutrition Survey 2008‐2009 (a): mean salt intake (grams/d) estimated via multiple‐pass 24‐hour dietary recall New Zealand Adult Nutrition Survey 2008‐2009 (b): mean salt intake (grams/d) estimated via spot urine samples New Zealand Total Diet Study 2009: mean sodium intake (milligrams/d) |
|
| Axes of inequality | New Zealand Total Diet Study 2003‐2004: gender New Zealand Adult Nutrition Survey 2008‐2009 (a) and (b): none New Zealand Total Diet Study 2009: gender |
|
| Sample size and response rate | New Zealand Total Diet Study 2003‐2004: N/A New Zealand Adult Nutrition Survey 2008‐2009 (a): n = 4721 for overall survey; 61% RR for overall survey New Zealand Adult Nutrition Survey 2008‐2009 (b): n = unknown for urine sample; 44% RR for urine sample New Zealand Total Diet Study 2009: N/A |
|
| Funding source / Conflict of Interest (COI) | New Zealand Total Diet Study 2003‐2004: undertaken by New Zealand Food Safety Authority/no COI statement provided New Zealand Adult Nutrition Survey 2008‐2009 (a) and (b): survey funded by New Zealand Ministry of Health/no COI statement provided New Zealand Total Diet Study 2009: undertaken by New Zealand Food Safety Authority, with management and technical input from Institute of Environmental Science & Research/no COI statement provided |
|
| Notes | Sources of data points and references: see New Zealand New Zealand Total Diet Study 2003‐2004 and 2009: New Zealand country questionnaire 2014: *New Zealand Ministry for Primary Industries. New Zealand Total Diet Study (NZTDS). http://www.foodsafety.govt.nz/policy‐law/food‐monitoring‐programmes/total‐diet‐study/ New Zealand Adult Nutrition Survey 2008‐2009 (1) and (2): New Zealand country questionnaire 2014: University of Otago and Ministry of Health. Methodology Report for the 2008/09 New Zealand Adult Nutrition Survey. Wellington: Ministry of Health, 2011 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | N/A ‐ used Total Diet Study method with no sample per se |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | High risk | Sodium intake levels were estimated on the basis of consumption of food groups in specific age and gender cohorts. Reliability and validity are not described. Sodium intake levels were based on the 123 foods that New Zealanders most commonly ate, but sodium levels were only approximated from this and were not measured |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Unclear risk | N/A ‐ used Total Diet Study method with no sample per se |
| Selective reporting (reporting bias) | High risk | Sodium intake means are reported without standard deviations or confidence intervals |
| Other bias | Low risk | No other obvious sources of bias to report |
Switzerland.
| Methods | Uncontrolled pre‐post | |
| Participants | 1984 (a): representative sample of adults (men and women 18 to 75 years of age) living in different regions of Switzerland provided a spot urine sample 1984 (b): of (a), a subset provided 24‐hour urine sample 2011: Swiss survey on salt intake 2011: nationwide survey obtained from a random sample of individuals 15 years of age and older at 11 centres from 9 cantons, covering 3 linguistic regions of Switzerland. “Participants were recruited using a two level sampling strategy, similar to the one used in the Swiss Health Surveys. The Swiss Federal Statistical Office provided a list of randomly selected household from the Swisscom fixed line directory (first level), separately for each canton.” “…one person per household was randomly selected (second level) and invited to participate in the study.” “Because of important difficulties in recruiting young participants and given budgetary constraints, we had to complete the study sample by recruiting volunteers in some of the centres, mainly in the 15‐29 years old strata, notably from Universities and professional schools” |
|
| Interventions | Salt reduction initiative began in 2008. Efforts included:
|
|
| Outcomes | 1984 (a): mean salt intake estimated via sodium‐to‐creatinine ratio in spot urine (grams/d) 1984 (b): mean salt intake estimated via 24‐hour urine 2011: Swiss survey on salt intake 2011: mean salt intake (grams/d) estimated via 24‐hour urine |
|
| Axes of inequality | 1984 (a) and (b): gender. 2011: Swiss survey on salt intake 2011: gender and place of residence (linguistic region) |
|
| Sample size and response rate | 1984 (a): n = 966; unknown RR 1984 (b): n = 147; unknown RR 2011: Swiss survey on salt intake 2011: n = 1448; 9.7% of contacted households provided a participant |
|
| Funding source / Conflict of Interest (COI) | 1984 (a) and (b): funding source unknown/country contact states no COI exists 2011: Swiss survey on salt intake 2011: “Survey was mandated and financed by the Swiss Federal Office of Public Health (contract numbers: 09.004165/404.0101/‐2 and 09.005791/414.0000/‐74). The Division of Nephrology and the Institute of Social and Preventive Medicine, both of the Centre Hospitalier Universitaire Vaudois (Lausanne, Switzerland) provided additional logistic and financial support”/country contact states no COI exists |
|
| Notes | Sources of data points and references: see Switzerland 1984: Switzerland country questionnaire and associated correspondence 2014‐2015: World Health Organization. Mapping Salt Reduction Initiatives in the WHO European Region. WHO Regional Office for Europe 2013;1‐50; Mordasini C, Abetel G, Lauterburg H, Ludi P, Perrenoud JP, Schmid H, Studer H. Sodium chloride intake and supply of iodine in the Swiss population. Schweizerische Medizinische Wochenschrift 1984;114(51):1924‐1929 Swiss survey on salt intake 2011: Switzerland country questionnaire and associated correspondence 2014‐2015: *Chappuis A, Bochud M, Glatz N, Vuistiner P, Paccaud F, Burnier M. Swiss Survey on Salt Intake: Main Results. Service de Néphrologie et Institut Universitaire de Médecine Sociale et Préventive (CHUV), 2011 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | Overall ‐ high risk of bias (ROB) 1984: random selection of men and women 2011: 2‐level random sampling strategy; however, owing to low participation rates, investigators had to recruit volunteers |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | 24‐Hour urine samples collected. Convincing text suggests protocols were adhered to, and that the method was properly carried out in both 1984 and 2011 |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | 2011 data point: Although data were collected for the purpose of evaluating the intervention, participants were blinded. Investigators “paid attention not to mention salt intake, in order for them not to change their dietary habits before the urine collection” (Chappui 2011) 1984 data point: Data were collected for the purpose of estimating salt consumption of the population; no indication that blinding was performed |
| Representativeness of sample | High risk | Investigators indicate that the convenience sampling employed “limits the representativeness of the study sample” (Chappuis 2011, pg. 8). Foreigners were underrepresented (pg. 9). 1984 data point: limited information provided |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported for overall estimates |
| Other bias | Low risk | No other obvious sources of bias to report |
Thailand.
| Methods | Uncontrolled pre‐post | |
| Participants | National Nutrition Survey 1960: individuals from military and civilian populations living in households with children younger than 5 years of age National Nutrition Survey 1975: individuals from military and civilian populations living in households with children younger than 5 years of age National Nutrition Survey 2003: individuals from military and civilian populations living in households with children younger than 5 years of age Report of sodium consumption in Thai diet survey 2008: unknown Fourth Thai National Health Examination Survey 2008‐2009: multi‐stage, stratified random sample of individuals 15+ years of age based on population registers |
|
| Interventions | Salt reduction initiative started in 2006. Efforts included:
|
|
| Outcomes | National Nutrition Survey 1960: mean sodium intake (grams/d) estimated via a dietary survey National Nutrition Survey 1975: mean sodium intake (grams/d) estimated via a dietary survey National Nutrition Survey 2003: mean sodium intake (grams/d) estimated via a dietary survey (food list recall and food frequency checklist of foods/condiments) Report of sodium consumption in Thai diet survey 2008: mean sodium intake (grams/d) estimated via a dietary survey (household survey) Fourth Thai National Health Examination Survey 2008‐2009: mean sodium intake (grams/d) estimated via a dietary survey (food list recall and food frequency checklist of foods/condiments) |
|
| Axes of inequality | National Nutrition Survey 1960: none National Nutrition Survey 1975: none National Nutrition Survey 2003: none Report of sodium consumption in Thai diet survey 2008: none Fourth Thai National Health Examination Survey 2008‐2009: none |
|
| Sample size and response rate | National Nutrition Survey 1960: sample size and response rate unknown National Nutrition Survey 1975: sample size and response rate unknown National Nutrition Survey 2003: sample size and response rate unknown Report of sodium consumption in Thai diet survey 2008: sample size and response rate unknown Fourth Thai National Health Examination Survey 2008‐2009: n = 20,450; 93.1% RR (overall survey) |
|
| Funding source / Conflict of Interest (COI) | National Nutrition Survey 1960: funding source unknown/no COI statement provided National Nutrition Survey 1975: funding source unknown/no COI statement provided National Nutrition Survey 2003: funding source unknown/no COI statement provided Report of sodium consumption in Thai diet survey 2008: funding source unknown/no COI statement provided Fourth Thai National Health Examination Survey 2008‐2009: funding source unknown/no COI statement provided |
|
| Notes | Sources of data points and references: see Thailand National Nutrition Survey 1960 and 1975: *Supornsilaphachai C. Evolution of salt reduction initiatives in Thailand: lessons for other countries in the South‐East Asia Region. Regional Health Forum 2013;17(1):61‐71 National Nutrition Survey 2003 and report of sodium consumption in Thai diet survey 2008: Thailand country questionnaire 2014: *Supornsilaphachai 2013 (see full citation above) Fourth Thai National Health Examination Survey 2008‐2009: Thailand country questionnaire 2014: *Supornsilaphachai 2013 (see full citation above): Aekplakorn W, Chariyalertsak S, Kessomboon P, Sangthong R, Inthawong R, Putwatana P, Taneepanichskul S, Thai National Health Examination Survey IV Study Group. Prevalence and management of diabetes and metabolic risk factors in Thai adults: The Thai National Health Examination Survey IV, 2009. Diabetes Care 2011;34(9):1980‐1985 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | Simple random sampling reported for only 1 data point (2007) |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Unclear risk | Methods of measuring sodium levels were not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Unclear risk | Not discussed |
| Selective reporting (reporting bias) | High risk | No estimates of variance (confidence intervals or standard deviations) were provided |
| Other bias | Low risk | No other obvious sources of bias to report |
Turkey.
| Methods | Uncontrolled pre‐post | |
| Participants | Relationship between Hypertension and Salt Intake in Turkish Population (SALTURK1) 2008 (a) and (b): 2‐stage stratified sampling method to select a nationally representative sample of adults 18+ Relationship between Hypertension and Salt Intake in Turkish Population (SALTURK2) 2012: participant information unknown |
|
| Interventions | Salt reduction initiative started in 2011. Efforts include:
|
|
| Outcomes | SALTURK1 2008 (a): mean salt intake (grams/d) estimated via 24‐hour urine SALTURK1 2008 (b): mean salt intake (grams/d) estimated via spot urine (some uncertainty regarding whether this is spot or 24 hour) SALTURK2 2012: mean salt intake (grams/d) estimated via 24‐hour urine |
|
| Axes of inequality | SALTURK1 2008 (a): gender, place of residence and education level SALTURK1 2008 (b): none SALTURK2 2012: none |
|
| Sample size and response rate | SALTURK1 2008 (a): n = 1970 were deemed to be eligible, but after exclusion criteria were applied, 24–hour urine samples were obtained for n = 816 (373 M; 443 F); RR unknown SALTURK 2008 (b): n = 1970 were deemed to be eligible, but it is unclear how many spot urine samples were collected; RR unknown SALTURK2 2012: n = 925; “657 person (according to urine creatine levels)”; RR unknown |
|
| Funding source / Conflict of Interest (COI) | SALTURK1 2008 (a): sponsored by the Turkish Society of Hypertension and Renal Diseases/authors declare no COI SALTURK1 2008 (b): unknown/no COI statement provided SALTURK2 2012: unknown/no COI statement provided |
|
| Notes | Sources of data points and references: see Turkey SALTURK1 2008: *Erdem Y, Arici M, Altun B, Turgan C, Sindel S, Erbay B, Derici U, Karatan O, Hasanoglu E, Caglar S. The relationship between hypertension and salt intake in Turkish population: SALTURK study. Blood Pressure 2010;19:313‐318 SALTURK1 2008 (b): Turkey country questionnaire and associated correspondence 2014‐2015 SALTURK2: Turkey country questionnaire and associated correspondence 2014‐2015 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | SALTURK1 (Erdem 2010) – “Two‐stage stratified sampling method was used to select a nationally representative sample…Strata were selected by a proportional sampling method” (pg. 314). “Participants…were randomly allocated from 14 cities” (pg. 314) SALTURK2 ‐ unclear |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Unclear risk | SALTURK1 (Erdem 2010) – low – 24‐hour urine samples collected. Convincing text suggests protocols were adhered to, and that the method was properly carried out Staff was trained to collect 24‐hour urine samples SALTURK2 ‐ unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | SALTURK1 (Erdem 2010) – low – SALTURK1 was used (pre‐existing survey) SALTURK2 ‐ low – SALTURK2 was used (pre‐existing survey) |
| Representativeness of sample | Unclear risk | SALTURK1 (Erdem 2010) – low ‐ “The participants were representative of Turkish population, taking into account population distribution across urban and rural settings, male and female sex, and BP status” (pg. 314) SALTURK2 ‐ unclear |
| Selective reporting (reporting bias) | High risk | SALTURK1 (Erdem 2010) – low – means and standard deviations reported SALTURK2 – high – values reported only in grams/d with no standard deviations or confidence intervals |
| Other bias | Low risk | No other obvious sources of bias to report. Note limited information available about SALTURK2 |
United Kingdom ‐ England.
| Methods | Interrupted time series | |
| Participants | Health Survey for England (HSE) 2003‐2007 (a) and 2003‐2007 (b): stratified, random probability sample of individuals living in private households in England from which a subsample of respondents ≥ 16 years of age provided a spot urine sample National Diet and Nutrition Survey 2005‐2006: random sample of individuals 19 to 64 years of age living in private households in England National Diet and Nutrition Survey 2011: random sample of individuals from 43 post code sectors 19 to 64 years of age living in private households in England |
|
| Interventions | Salt reduction initiative began in 2003. Efforts included
|
|
| Outcomes | HSE 2003‐2007 (a): geometric mean salt intake (grams/d) estimated via spot urine HSE 2003‐2007 (b): urinary sodium excretion (mmol/d) estimated via spot urine National Diet and Nutrition Survey 2005‐2006: mean salt intake (grams/d) estimated via 24‐hour urine National Diet and Nutrition Survey 2011: mean salt intake (grams/d) estimated via 24‐hour urine |
|
| Axes of inequality | HSE 2003‐2007 (a): gender, ethnicity and social class HSE 2003‐2007 (b): gender and place of residence National Diet and Nutrition Survey 2005‐2006: gender National Diet and Nutrition Survey 2011: gender |
|
| Sample size and response rate | HSE 2003 (a) and 2003 (b): n = 1668; 9.0% of adult respondents provided a urine sample HSE 2004 (a) and 2004 (b): n = 2840; 28.1% of adult respondents provided a urine sample HSE 2005 (a) and 2005 (b): n = 4643; 34.9% of adult respondents provided a urine sample National Diet and Nutrition Survey 2005‐2006: n = 448 (188 M; 260 F); “The aggregate response to the urine collection study was therefore 19.7%, the product of the first stage response and response to the urine collection stage" HSE 2006 (a) and 2006 (b): n = 8844; 41.3% of adult respondents provided a urine sample HSE 2007 (a) and 2007 (b): n = 4269; 29.7% of adult respondents provided a urine sample National Diet and Nutrition Survey 2011: n = 547; overall RR not provided |
|
| Funding source / Conflict of Interest (COI) | HSE 2003‐2007 (a): “CM is funded by the Higher Education Funding Council for England and the National Institute for Health Research. AL is funded by the National Institute for Health Research. The Department of Primary Care and Public Health at Imperial College is grateful for support from the National Institute for Health Research Biomedical Research Centre Funding scheme, the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care scheme, and the Imperial Centre for Patient Safety and Service Quality. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript”/all authors declared no COI HSE 2003‐2007 (b): "This research was funded by the European Union’s Framework 7 programme under the ‘EATWELL’ (Interventions to Promote Healthy Eating Habits: Evaluations and Recommendations) project"/all authors declared no COI National Diet and Nutrition Survey 2005‐2006: funding source of study not provided/no COI statement provided National Diet and Nutrition Survey 2011: survey carried out by the UK Department of Health/no COI statement provided |
|
| Notes | Sources of data points and references: see United Kingdom ‐ England HSE 2003‐2007 (a): *Millett C, Laverty AA, Stylianou N, Bibbins‐Domingo K, Pape UJ. Impacts of a national strategy to reduce population salt intake in England: serial cross sectional study. PLoS ONE 2012;7(1):e29836. doi:10.1371/journal.pone.0029836 HSE 2003‐2007 (b): Shankar B, Brambila‐Macias J, Traill B, Mazzocchi M, Capacci S. An evaluation of the UK Food Standards Agency's salt campaign. Health Economics 2013;22:243‐250 National Diet and Nutrition Survey 2005‐2006: National Centre for Social Research. An assessment of dietary sodium levels among adults (aged 19‐64) in the UK general population in 2008, based on analysis of dietary sodium in 24 hour urine samples. MRC Human Nutrition Research 2008;1‐16; Wyness LA, Butriss JL, Stanner SA. Reducing the population's sodium intake: the UK Food Standards Agency's salt reduction programme. Public Health Nutrition 2012;15(2):254‐261; He FJ, Pombo‐Rodrigues S, MacGregor GAS. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014;4(4):e004549 National Diet and Nutrition Survey 2011: United Kingdom country questionnaire 2014: Sadler K, Nicholson S, Steer T, Gill V, Bates B, Tipping S, Cox L, Lennox A, Prentice A. National Diet and Nutrition Survey ‐ assessment of dietary sodium in adults (aged 19 to 64 years) in England, 2011: a survey carried out on behalf of the Department of Health, 2011; He et al., 2014 (see full citation above) *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | The Health Survey for England (HSE) was used, which employed stratified random sampling from households |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | Spot urine samples were collected, and internal and external quality control was assessed. Convincing texts suggests protocols were adhered to, and that the method was properly carried out |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Low risk | Although participants in the survey volunteered to provide spot urine samples, investigators concluded that volunteers who provided a sample “did not differ from those that did not in terms of age, sex, ethnicity and class” (pg. 6). As well, investigators used weights provided by the survey to correct for issues of voluntary participation. Participants volunteered for spot urine samples; however, “analyses using the weights provided by the HSE to correct for these issues did not influence the results found” (pg. 6) |
| Selective reporting (reporting bias) | Low risk | Means and confidence intervals were reported for overall estimates |
| Other bias | Low risk | Investigators indicate that they “were unable to isolate the impacts of the salt reduction strategy from other primary and secondary prevention interventions, including the provision of financial incentives to general practitioners, to improvements in blood pressure control over the study period” (pg. 6). However these issues are captured under the "confounding" domain |
United Kingdom ‐ Great Britain.
| Methods | Uncontrolled pre‐post | |
| Participants | National Diet and Nutrition Survey (NDNS) 2001 (a): multi‐stage random probability sample of adults 19 to 64 years of age living in private households in mainland Great Britain. Participants were requested to complete a 7‐day weighted dietary record National Diet and Nutrition Survey (NDNS) 2001 (b): multi‐stage random probability sample of adults 19 to 64 years of age living in private households in mainland Great Britain. In addition to completing a 7‐day weighted dietary record, participants were asked to provide a 24‐hour urine sample National Diet and Nutrition Survey (NDNS) 2001 (c) and (d): multi‐stage random probability sample of adults 19 to 64 years of age living in private households in mainland Great Britain. Participants were requested to complete a 7‐day weighted dietary record. Ji et al., 2014, performed additional analyses on these data using only white respondents because of small sample sizes for other ethnic groups Survey by the National Centre for Social Research 2008: random sample of individuals from 45 post code sectors 19 to 64 years of age living in private households in the United Kingdom. “A random sample of 45 postcode sectors was selected initially, and within these a random sample of telephone numbers was drawn using random digit dialling.” “8,100 telephone numbers were generated (after removing non‐working numbers). A reserve sample 4,500 numbers was also generated in case the required number of completed urine samples was not obtained from the initial sample” |
|
| Interventions | Salt reduction initiative began in 2003. Efforts included
|
|
| Outcomes | NDNS 2001 (a): mean (average value) of daily intake of sodium (milligrams/d) estimated via a 7‐day consecutive weighted dietary record NDNS 2001 (b): mean (average value) of salt intake (grams/d) estimated via 24‐hour urine NDNS 2001 (c): median dietary sodium intake (milligrams/d) estimated via a 7‐day consecutive weighted dietary record. Study authors also provide an equivalent estimated salt intake (grams/d) NDNS 2001 (d): median 24‐hour urinary sodium excretion (mmol/d) estimated via 24‐hour urine. Study authors also provide an equivalent estimated salt intake (grams/d) Survey by the National Centre for Social Research 2008: mean salt intake (grams/d) estimated via 24‐hour urine |
|
| Axes of inequality | NDNS 2001 (a) and (b): gender NDNS 2001 (c) and (d): gender, place of residence, education and social class Survey by the National Centre for Social Research 2008: gender |
|
| Sample size and response rate | NDNS 2001 (a): n = 1724 (833 M; 891 W) for 7‐day food record; “Overall, 66% of the responding sample and 83% of the diary sample consented to making a 24‐hour urine collection. A urine sample was obtained for 98% of those who consented to making the 24‐hour urine collection (65% of the responding and 81% of the diary samples)" NDNS 2001b: n = 1147 (567 M; 580 W) for 24‐hour urine sample; “Overall, 66% of the responding sample and 83% of the diary sample consented to making a 24‐hour urine collection. A urine sample was obtained for 98% of those who consented to making the 24‐hour urine collection (65% of the responding and 81% of the diary samples)" NDNS 2001 (c) and (d): “A total of 2251 respondents from 11 regions completed an interview (60.8% of the total eligible sample). In this survey population, 76.6% (N=1724) completed a 7‐day dietary record and 64.8% (N=1459) provided completed 24‐h urine collections. Respondents came from different ethnic groups, white representing the majority (93.6%). Since estimation based on a few respondents may not be representative for those minority ethnic groups, especially when compared by region, only white respondents were included in this analysis (N=2105)” Survey by the National Centre for Social Research 2008: n = 692 (294 M; 398 W); 30% from first issued sample and 32% from reserve sample agreed to participation in a telephone interview (31% combined) |
|
| Funding source / Conflict of Interest (COI) | NDNS 2001 (a) and (b): funded by Food Standards Agency and the Department of Health the Office for National Statistics and the Medical Research Council Human Nutrition Research/no COI statement provided NDNS 2001 (c) and (d): funded by the BUPA Foundation (MR‐12‐002)/“FPC is unpaid member of CASH, WASH, unpaid technical advisor to the WHO and the PAHO, individual member of the National Heart Forum, past member of the Executive Committee and Trustee of the British Hypertension Society, past member of the NICE CVD population prevention guideline development group” Survey by the National Centre for Social Research 2008: funding source of study not provided/no COI statement provided |
|
| Notes | Sources of data points and references: see United Kingdom ‐ Great Britain NDNS 2001 (a) and (b): United Kingdom country questionnaire 2014: Henderson L, Irving K, Gregory J, Bates CJ, Prentice A, Perks J, Swan G, Farron M. The National Diet & Nutrition Survey: adults aged 19 to 64 years: vitamin and mineral intake and urinary analytes. National Diet and Nutrition Survey 2003;3 (Her Majesty’s Stationery Office (HMSO); *Wyness LA, Butriss JL, Stanner SA. Reducing the population's sodium intake: the UK Food Standards Agency's salt reduction programme. Public Health Nutrition 2012;15(2):254‐261; He FJ, Pombo‐Rodrigues S, MacGregor GAS. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014;4(4):e004549 NDNS 2001 (c) and (d): Ji C, Kandala NB, Cappuccio FP. Spatial variation of salt intake in Britain and association with socioeconomic status. BMJ Open 2031;3(1):e002246 Survey by the National Centre for Social Research 2008: United Kingdom country questionnaire 2014; National Centre for Social Research. An assessment of dietary sodium levels among adults (aged 19‐64) in the UK general population in 2008, based on analysis of dietary sodium in 24 hour urine samples. MRC Human Nutrition Research 2008;1‐16; *Wyness et al., 2012 (see full citation above); He et al., 2014 (see full citation above) *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Complex random samples were used |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | 24‐Hour urine samples were collected. Convincing texts suggests protocols were adhered to, and that the method was properly carried out for both years. Completeness of urine collection was measured. Similar protocols were used to measure 24‐hour urine sodium levels between time points indicating comparable data points |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Although the National Diet and Nutrition Survey (2000/2001) was pre‐existing, survey data used by the National Centre for Social Research were collected for the purpose of evaluating the initiative, and we found no indication of blinding (NCSR 2008) |
| Representativeness of sample | Low risk | NDNS (2000/01): “data weighted to compensate for the differential probabilities of selection and non‐response” (pg. viii). This ensures that the sample is representative of the population NCSR (2008): weighting used to “make the sample distribution match the UK population by age, sex, and country” (pg. 5) |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported for overall estimates |
| Other bias | Low risk | No other obvious sources of bias to report |
United Kingdom ‐ Scotland.
| Methods | Uncontrolled pre‐post | |
| Participants | Scottish Health Survey 2003, 2008 and 2009: multi‐stage stratified probability sample of individuals of all ages living in private households in Scotland, from which a subsample 16 years of age and older provided spot urine sample during a second stage visit with a nurse 2006: representative sample of individuals 19 to 64 years of age living in Scotland, including the Highlands and Islands. Sample was obtained through 2 sources: (1) a subsample of respondents from the 2003 Scottish Health Survey who agreed to be re‐contacted, and (2) a representative sample of the Scottish population obtained via random digit dialling 2009: representative sample of individuals 19 to 64 years of age living in Scotland, including the Highlands and Islands. Survey used the main 2009 Scottish Health Survey household survey as a sampling frame to obtain an additional sample for salt intake via 24‐hour urine estimates |
|
| Interventions | Salt reduction initiative began in 2003. Efforts included
|
|
| Outcomes | Scottish Health Survey 2003: mean salt intake (grams/d) estimated via spot urine 2006: mean salt intake (grams/d) estimated via 24‐hour urine Scottish Health Survey 2008 and 2009: mean salt intake (grams/d) estimated via spot urine 2009: mean salt intake (grams/d) estimated via 24‐hour urine |
|
| Axes of inequality | Scottish Health Survey 2003: gender 2006: gender Scottish Health Survey 2008 and 2009: gender 2009: gender |
|
| Sample size and response rate | Scottish Health Survey 2003: n = 1148 (for spot urine sample); 67% household RR and 60% individual RR among adults 20 to 64 years of age (overall survey) 2006: n = 442 (for 24‐hour urine sample); multiple levels of response rates but no overall response rate provided Scottish Health Survey 2008: n = 1041 (for spot urine sample); 61% household RR and 54% individual RR among adults 20 to 64 years of age (overall survey) Scottish Health Sodium Survey 2009: n = 1045 (for spot urine sample); 64% household RR and 56% individual RR among adults 20 to 64 years of age (overall survey) 2009: n = 702 (for 24‐hour urine sample); multiple levels of response rates but no overall response rate provided |
|
| Funding source / Conflict of Interest (COI) | Scottish Health Survey 2003: Survey was conducted by the Joint Health Surveys Unit (JHSU) of the National Centre for Social Research (NatCen) and the Department of Epidemiology and Public Health at University College London (UCL). The JHSU collaborated with the Medical Research Council/Chief Scientist Office (MRC/CSO) Social and Public Health Sciences Unit in Glasgow/no COI statement provided 2006: funding source of study not provided/no COI statement provided Scottish Health Survey 2008 and 2009: survey conducted by collaboration between the Scottish Centre for Social Research (part of NatCen), the MRC/CSO Social and Public Health Sciences Unit in Glasgow and the University London College/no COI statement provided 2009: funding source of study not provided/no COI statement provided |
|
| Notes | Sources of data points and references: see United Kingdom ‐ Scotland Scottish Health Survey 2003: *Scottish Centre for Social Research. A survey of 24 hour urinary sodium excretion in a representative sample of the Scottish population as a measure of salt intake. 2011;1‐25; Government of Scotland website (www.gov.scot) 2006: National Centre for Social Research. A survey of 24 hour and spot urinary sodium and potassium excretion in a representative sample of the Scottish population. Joint Health Surveys Unit 2007;1‐30 Scottish Health Survey 2008 and 2009: *Scottish Centre for Social Research. A survey of 24 hour urinary sodium excretion in a representative sample of the Scottish population as a measure of salt intake. 2011;1‐25; Government of Scotland website (www.gov.scot) 2009: *Scottish Centre for Social Research. A survey of 24 hour urinary sodium excretion in a representative sample of the Scottish population as a measure of salt intake. 2011;1‐25 *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Scottish Health Surveys (SHeS) 2006 and 2009, which employed a multi‐stage stratified probability sampling design, were used. An additional sample from this same survey was used to collect 24‐hour urine samples |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | “Very similar protocols and procedures” were used between the 2 time points (2006 and 2009) (pg. 5). Convincing text suggests protocols were adhered to, and that the method was properly carried out for both years. Staff was trained to collect 24‐hour urine samples |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Low risk | Sample weights were used to ensure the sample corresponded to that of the Scottish population |
| Selective reporting (reporting bias) | Low risk | Means and confidence intervals were reported for overall estimates |
| Other bias | Low risk | No other obvious sources of bias to report |
United States.
| Methods | Uncontrolled pre‐post | |
| Participants | NHANES 1988‐1994: “[NHANES] has a stratified, multistage, probability sample design an is representative of the civilian, noninstitutionalized U.S. population.” “The current cross‐sectional study is based on a surplus sample proposal approved by NCHS to measure urine sodium in randomly selected spot urine samples…” “We selected 1249 participants from 1992 samples who met our criteria in NHANES 1988‐1994 [aged 20‐59])” NHANES 2003‐2006: “[NHANES] has a stratified, multistage, probability sample design and is representative of the civilian, noninstitutionalized U.S. population.” “The current cross‐sectional study is based on a surplus sample proposal approved by NCHS to measure urine sodium in randomly selected spot urine samples…” “We selected 1241 participants in NHANES 2003‐2006: 853 non hypertensive participants from a one‐third urine random sub sample and 388 participants with hypertension from the full examination sub sample [aged 20‐59])” NHANES 2010: “[NHANES] has a stratified, multistage, probability sample design and is representative of the civilian, noninstitutionalized U.S. population.” “The current cross‐sectional study is based on a surplus sample proposal approved by NCHS to measure urine sodium in randomly selected spot urine samples…” “For NHANES 2010, we selected 525 persons aged 20‐59 years who met our criteria from a one‐third urine random sub sample” |
|
| Interventions | Salt reduction initiative began in the late 1980s to the early 1990s. Efforts included
|
|
| Outcomes | NHANES 1988‐1994, 2003‐2006 and 2010: mean sodium intake (milligrams/d) estimated from measured sodium concentrations in spot urine samples using calibration equations (for men and women) | |
| Axes of inequality | NHANES 1988‐1994, 2003‐2006, 2010: gender and race/ethnicity | |
| Sample size and response rate | NHANES 1988‐1994: n = 1249 (645 M; 604 W); “The unweighted examination response rates for the overall sample (and for ages 20‐59 years) were 78% (73%) for 1998‐1994…” NHANES 2003‐2006: n = 1235 (725 M; 510 W); “The unweighted examination response rates for the overall sample (and for ages 20‐59 years) were… 77% (73%) for 2003‐2006…” NHANES 2010: n = 525 (258 M; 267 W); “The unweighted examination response rates for the overall sample (and for ages 20‐59 years) were… 77% (77%) for 2010” |
|
| Funding source / Conflict of Interest (COI) | NHANES 1988‐1994, 2003‐2006 and 2010: “No specific sources of financial support were received”/all authors declare no COI | |
| Notes | Sources of data points and references: see United States NHANES 1988‐1994, 2003‐2006 and 2010: *Pfeiffer CM, Hughes JP, Cogswell ME, Burt VL, Lacher DA, LaVoie DJ, Rabinowitz DJ, Johnson CL, Pirkle JL. Urine sodium excretion increased slightly among U.S. adults between 1988 and 2010. The Journal of Nutrition 2014;144:698‐705 Note: We are aware that other papers (e.g. Cogswell 2012; Centers for Disease Control and Prevention 2013) have discussed trends in dietary sodium intake based on the 24‐hour dietary recall component of the NHANES survey. However, data points provided in these papers are all 'post‐intervention' data points in terms of how we are conceptualising the initiative *Indicates main publication used for in‐text citation purposes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | Convenience sample used for years 1988‐1994; random samples taken in years 2003‐2006 and 2010 |
| Confounding | High risk | Uncontrolled pre‐post designs always score 'high' |
| Reliability/validity of outcome measure | Low risk | Investigators estimated 24‐hour urine samples collected from spot urine samples. 24‐Hour dietary recalls were also used. Urine and dietary surveys were collected in the same way for each time point. “The correlations between the estimated 24hUNa excretion and the dietary sodium intake in our study were comparable to other studies, particularly if one considers that they were derived from a single spot urine and a single 24‐hr dietary recall” (pg. 703). One limitation reported was that they were “not able to account for within‐person variability” (pg. 704) due to diurnal fluctuations in spot urine samples and 24hUNa estimations. However, the study authors do not think this is a large limitation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pre‐existing data were used to evaluate the initiative |
| Representativeness of sample | Low risk | This survey “is representative is the civilian, non‐institutionalised U.S. population” (pg. 699). One limitation reported was the convenience sample from 1988‐1994, which “presents the question of whether the sample is representative of the US population and how much confidence can be placed in the statistical testing for temporal trends” (pg. 704). However, participants “did not differ from participants in the full NHANES sample with regards to demographic characteristics or in the central tendency of key variables used in our study” (pg. 704) |
| Selective reporting (reporting bias) | Low risk | Means and standard deviations were reported |
| Other bias | Low risk | No other obvious sources of bias to report |
Abbreviations:
CIHR: Canadian Institutes of Health Research
COI: conflict of interest
DCS: Doetinchim Cohort Study
FFQ: food frequency questionnaire
GDPS: General Doetinchem Population Sample
GO: governmental organisation
HSFC: Heart and Stroke Foundation of Canada
INMD: Institute of Nutrition, Metabolism and Diabetes
IPPH: Institute of Population and Public Health
JHSU: Joint Health Surveys Unit
KNHANES: Korea National Health and Nutrition Examination Survey
MRC/CSO: Medical Research Council/Chief Scientist Office
NatCen: National Centre for Social Research
NGO: non‐governmental organisation
ROB: risk of bias
RR: response rate
UCL: University College London
WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Argentina | No pre‐intervention data point (identified 2004‐2005 data point includes only females) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Argentina |
| Australia | No pre‐intervention data point We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Australia |
| Bangladesh. | Unknown start date of initiative (despite efforts to clarify) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Bangladesh. |
| Barbados | No pre‐intervention data point We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Barbados |
| Croatia | Lack of information to indicate whether comparable pre‐post data are available We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Croatia |
| Iceland | Unknown start date of initiative (despite efforts to clarify) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Iceland |
| Indonesia | No pre‐intervention data point We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Indonesia |
| Israel | Unknown start date of initiative (despite efforts to clarify) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Israel |
| Italy | No pre‐intervention data point We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Italy |
| Malaysia | No suitable data points (data points identified were based on non‐comparable subsets of the population) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Malaysia |
| Poland | Data points based on non‐comparable jurisdiction and/or methods We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Poland |
| Portugal | No pre‐intervention data point We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Portugal |
| Singapore | Unknown start date of initiative (despite efforts to clarify) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Singapore |
| Slovakia | No pre‐intervention data point We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Slovakia |
| Slovenia | Information insufficient to indicate whether we had 2 comparable data points (despite efforts to clarify) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Slovenia |
| Sri Lanka | Information insufficient to indicate whether we had 2 comparable data points (despite efforts to clarify) We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Sri Lanka |
| Uruguay | Unknown start date of initiative (despite efforts to clarify) and only 1 data point We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Uruguay |
| Vietnam | Data points based on non‐comparable jurisdiction and/or methods We considered this country because of its inclusion in the companion review (Trieu 2015) sources: see Vietnam |
Characteristics of ongoing studies [ordered by study ID]
Belgium.
| Trial name or title | Belgium |
| Methods | Uncontrolled pre‐post (only 1 pre‐intervention data point identified) |
| Participants | Belgian National Food Consumption Survey 2004: multi‐stage procedure used to select participants from the National Register 15 years of age and older 2009: adult population 45 to 65 years of age living in 2 regions of Belgium (Ghent and Liege) |
| Interventions | Initiative includes
|
| Outcomes | Belgian National Food Consumption Survey 2004: mean salt intake (grams/d) estimated via non‐consecutive 24‐hour recalls in combination with a self administered food frequency questionnaire 2009: mean salt intake (grams/d) estimated via 24‐hour urine |
| Starting date | May 2009 |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Belgium |
Brazil.
| Trial name or title | Brazil |
| Methods | Uncontrolled pre‐post or Interrupted time series |
| Participants | 2002‐2003 and 2008‐2009 Brazilian Household Budget Survey: probabilistic sample of households in Brazil |
| Interventions | Initiative includes
|
| Outcomes | 2002‐2003 and 2008‐2009 Brazilian Household Budget Survey: mean daily sodium available for consumption in Brazilian households (grams per 2000 kcal per day). “Records of food purchases of households were converted into nutrients using food composition tables. Mean sodium availability per person per day and mean adjusted availability for a 2,000 kcal daily energy intake were calculated. The contribution of food groups to the total household sodium availability was calculated and compared to results estimated from the 2002‐2003 Household Budget Survey” (Sarno et al., 2013, pg. 571) |
| Starting date | 2011 |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Brazil |
Bulgaria.
| Trial name or title | Bulgaria |
| Methods | Uncontrolled pre‐post (only 1 pre‐intervention data point identified) |
| Participants | National Survey of Food Intake and Nutritional Status 2004: individuals 19 to 75+ years of age |
| Interventions | Initiative includes
|
| Outcomes | National Survey of Food Intake and Nutritional Status 2004: mean salt intake (grams/d) estimated via 24‐hour dietary recall |
| Starting date | 2007 |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Bulgaria |
Chile.
| Trial name or title | Chile |
| Methods | Uncontrolled pre‐post (only 1 pre‐intervention data point identified) |
| Participants | 2009‐2010 National Health Survey: random household sample (stratified, multi‐stage, conglomerate sample) to obtain participants 15 years of age and older 2010‐2011 National Food Consumption Survey: probability sample (stratified and multi‐staged) to obtain participants 2 years of age and older representative of 5 zones in the country |
| Interventions | Initiative includes
|
| Outcomes | 2009‐2010 National Health Survey: salt intake estimated via urine collections (unclear whether collections were spot or 24‐hour) 2010‐2011 National Food Consumption Survey: salt intake estimated via a quantified food frequency questionnaire and 24‐hour recall |
| Starting date | 2011: voluntary reduction strategy sodium/salt in bread 2012: law 20,606 on nutritional composition of food and advertising |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Chile |
Costa Rica.
| Trial name or title | Costa Rica |
| Methods | Uncontrolled pre‐post or Interrupted time series |
| Participants | 2001: unknown 2004‐2005: unknown |
| Interventions | Initiative includes
|
| Outcomes | 2001: average national intake of table salt in the households of Costa Rica 2004‐2005: mean salt intake (grams/d) estimated via household budget survey |
| Starting date | 2011‐2021: National Plan to Reduce the Consumption of Salt/Sodium in the Population of Costa Rica within the National Policy on Food Security and Nutrition |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Costa Rica |
Fiji.
| Trial name or title | Fiji |
| Methods | Uncontrolled pre‐post or Interrupted time series |
| Participants | 2004 Fiji National Nutrition Survey: participants from households across the 4 administrative divisions within the Republic of Fiji Islands representing the 3 major ethnic groups from 45 randomly selected enumeration areas as survey sites 2009: unknown |
| Interventions | Initiative includes
|
| Outcomes | 2004 Fiji National Nutrition Survey: salt intake (grams/d) estimated via 24‐hour dietary recall 2009: salt intake (grams/d) estimated via Fiji food balance sheet |
| Starting date | 2012: National Salt Reduction Campaign |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Fiji |
Hungary.
| Trial name or title | Hungary |
| Methods | Uncontrolled pre‐post or Interrupted time series |
| Participants | 1985‐1988, 1992‐1994, 2003‐2004 Hungarian Diet and Nutritional Status Survey: professionally planned survey with wide geographical distribution that targeted the whole population of Hungary 2009 Hungarian Diet and Nutritional Status Survey: 2‐stage stratified sampling design to recruit participants representative of the Hungarian adult population by gender and age 2010: unknown |
| Interventions | Initiative includes
|
| Outcomes | 1985‐1988, 1992‐1994, 2003‐2004 Hungarian Diet and Nutritional Status Survey: mean salt intake (grams/d) estimated via a dietary survey 2009: Hungarian Diet and Nutritional Status Survey: mean salt intake (grams/d) estimated via a dietary survey 2010: mean salt intake (grams/d) estimated via 24‐hour urine |
| Starting date | 2010: STOP SALT! National Salt Reduction Program |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Hungary |
Lithuania.
| Trial name or title | Lithuania |
| Methods | Uncontrolled pre‐post or Interrupted time series |
| Participants | 1997 and 2007 National Nutrition Survey: unknown |
| Interventions | Initiative includes
|
| Outcomes | 1997 and 2007 National Nutrition Survey: mean salt intake (grams/d) estimated via dietary survey |
| Starting date | 2012: Project on Promotion of Reduction of Salt Consumption |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Lithuania |
Mongolia.
| Trial name or title | Mongolia |
| Methods | Uncontrolled pre‐post or Interrupted time series |
| Participants | 1998: participants 15 to 44 years of age from the capital city Ulaanbaatar and 4 other randomly selected provinces (Uvurkhangai, Huvsgol, Dornod and Huvd) located in the upper south, north, east and west of the country. Within a province, 5 to 18 villages were selected by the probability proportionate to size method 2010: participants 15 to 49 years of age 2011: salt intake of the population survey: participants 25 to 64 years of age randomly selected from the 4 economic regions of Mongolia |
| Interventions | Initiative includes
|
| Outcomes | 1998: mean salt intake (grams/d) estimated via second‐voided morning urine for 3 consecutive days 2010: mean salt intake (grams/d) estimated via spot urine 2011: mean salt intake (grams/d) estimated via 24‐hour urine |
| Starting date | 2011‐2013: pinch salt |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Mongolia |
Norway.
| Trial name or title | Norway |
| Methods | Uncontrolled pre‐post (only 1 pre‐intervention data point identified) |
| Participants | 2010‐2011: participants 18 to 70 years of age |
| Interventions | Initiative includes
|
| Outcomes | 2010‐2011: salt intake (grams/d) estimated via a food propensity questionnaire after completion of two 24‐hour dietary recalls |
| Starting date | 2014 |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Norway |
Republic of South Korea.
| Trial name or title | Republic of South Korea |
| Methods | Uncontrolled pre‐post or Interrupted time series |
| Participants | 1998, 2005, 2009 and 2012 Korean National Health and Nutrition Examination Surveys (KNHANES): “…nationally representative samples of noninstitutionalized South Korean civilians ages 1 year and older. KNHANES is based on a multistage, stratified area probability sample of noninstitutionalized South Korean households in different geographic areas and in different age and sex groups” (Lee, Duffey & Popkin, 2013, pg. 299) |
| Interventions | Initiative includes
|
| Outcomes | 1998, 2005, 2009 and 2012 KNHANES: mean sodium intake (grams/capita/d) estimated via a detailed 24‐hour dietary recall |
| Starting date | 2012; http://www.worldactiononsalt.com/worldaction/asia/53956.html |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Republic of South Korea |
Sweden.
| Trial name or title | Sweden |
| Methods | Uncontrolled pre‐post (only 1 pre‐intervention data point identified) |
| Participants | 1997 Second National Food Consumption Survey: unknown |
| Interventions | Initiative includes
|
| Outcomes | 1997 Second National Food Consumption Survey: mean salt intake (grams/d) via 7‐day dietary recording methods |
| Starting date | 2014‐2015: Keyhole Nordic Salt Reduction Project |
| Contact information | (review authors have information on file) |
| Notes | No post‐intervention data point, at the time of writing We considered this country because of its inclusion in the companion review (Trieu 2015) Sources: see Sweden |
Differences between protocol and review
Background: The content of this section is substantively the same as that provided in the protocol. We made minor changes to make this section more concise, to incorporate updated literature and to better reflect our dual goal of assessing overall impact as well as differential impact of population‐level sodium reduction initiatives. This dual goal is reflected in the evolution from our original protocol (published in The Cochrane Library, 2012 Issue 10) to our revised protocol (published in The Cochrane Library, 2013 Issue 8).
Types of studies: In our protocol, we indicated that we would include the following study designs: cluster‐randomised studies, controlled pre‐post studies, interrupted time series studies and uncontrolled pre‐post studies (McLaren 2013). It became apparent during the review process that most if not all of our studies had an uncontrolled pre‐post design. We therefore added the requirement that studies must include at least one pre‐intervention data point and at least one post‐intervention data point from the same or a comparable jurisdiction (e.g. both pre‐intervention and post‐intervention data points were national estimates).
Types of interventions: During the review process, we identified dietary sodium reduction initiatives for which the start date and whether/the extent to which intervention activities were under way (vs in planning phases) was not clear. We took efforts to gain clarity on these issues by directly contacting programme representatives, but sometimes we did not receive a clear answer to those questions. Accordingly, we amended our inclusion criteria to include population‐level interventions for dietary sodium reduction for which:
we received confirmation that activities were under way (vs in planning stages) at the time of writing; and
a start date could be identified (for the purpose of confirming pre‐intervention and post‐intervention data points).
Types of outcome measures: In our protocol (McLaren 2013), we indicated that we would examine indicators of sodium consumption (dietary survey, urine samples), indicators of health outcomes related to sodium consumption (e.g. stroke, blood pressure, hypertension, cardiovascular disease) and secondary outcomes (e.g. knowledge, awareness; other health/disease outcomes). However, we were unable to include all of these outcomes because in many instances, our review involved piecing together an evaluation by using existing national data sources. Ensuring a comprehensive review required that we locate, for every included country, every data set that included any of those outcomes. Because of the unwieldy nature of this task, we made the decision to focus on indicators of sodium consumption for feasibility purposes. We recognise the importance of including other outcomes in other reviews.
Searching other resources: This section is considerably improved by our collaboration with authors Webster and Trieu (Trieu 2015). Specifically, on the basis of grey literature searches, Webster and Trieu established a list of national sodium reduction initiatives and sent it to international experts and representatives of the World Health Organization (WHO) to identify whether any countries with initiatives had been missed. Then, they prepared a questionnaire (Appendix 3) and sent it to 87 country programme leaders identified through the expert review. They followed up queries with country programme leaders, the relevant WHO regional expert or a targeted search. Those findings are published in our companion review (Trieu 2015), and we considered all 75 initiatives reported in that paper for inclusion in this review.
Assessment of risk of bias in included studies: To assess risk of bias, we intended to use a hybrid risk of bias tool (that we created for our review) that incorporated domains from the Cochrane risk of bias tool (Higgins 2011), the EPOC (Cochrane Effective Practice and Organisation of Care) risk of bias tool and additional items. We attempted to use that hybrid tool but found it to was very difficult and cumbersome to apply and score. We were inspired by the adapted Cochrane risk of bias tool used in a recently published systematic review (Iheozor‐Ejiofor 2015), which seemed straightforward to apply and score, and appeared to be a good fit for population‐level interventions in government jurisdictions. Accordingly, we changed our plans and used an amended version of the Cochrane risk of bias tool, which is an amended version of the tool used by Iheozor‐Ejiofor 2015.
Furthermore, because all studies in our review are characterised as having high risk of bias overall (which reflects the uncontrolled, observational nature of studies) on the basis of the Cochrane tool, we sought a means of capturing variations in methodological quality amongst them. Our approach was to characterise each initiative in terms of the proportion of bias domains scored as 'high' or 'uncertain' out of a total of seven domains. Our studies provided desired variations on that metric, ranging from the best studies, which were scored as having 'high' or 'uncertain' risk of bias in one of seven domains, to the worst studies, which were scored as having 'high' or 'uncertain' risk of bias in five of seven domains.
Measures of treatment effect: This section has been shortened to reflect the small quantity and limited nature of data ultimately included in the review. For example, we had only continuous variables (no categorical data). We did not compute rate difference and rate ratio because we found an insufficient number of studies to permit quantitative analysis of differential impact by any axis other than sex. Also, as the result of high levels of study heterogeneity (I2 > 90%), we did not present pooled results but instead focused on results of individual studies.
Data synthesis, Subgroup analysis and investigation of heterogeneity and Sensitivity analysis: We intended to stratify studies by intervention type (see our intervention continuum under Description of the intervention), economic status of the country and duration of the initiative. However, studies were insufficient to permit any of this. For initiatives with multiple available data points, analysis of impact was based on the pre‐intervention data point closest in time to the start year of the intervention, as well as the post‐intervention data point farthest away in time from the start year of the initiative. As a sensitivity check, we re‐ran the analysis of impact by using alternative post‐intervention data points, along with alternative pre‐intervention data points when available.
Contributions of authors
LM: contributed to conceptualisation of the review; led data gathering, analysis, interpretation and writing.
NS: contributed to conceptualisation of the review; provided substantive input to data gathering, analysis, interpretation and writing.
AMB: co‐led data gathering and analysis; and provided substantive input to interpretation and writing.
KT: contributed to conceptualisation of the review; provided substantive input to data gathering, analysis, interpretation and writing; and co‐led the companion review (Trieu 2015).
DLL: contributed to conceptualisation of the review; provided substantive input to data gathering, analysis, interpretation and writing.
VT: contributed to conceptualisation of the review; provided substantive input to data gathering, analysis, interpretation and writing.
JW: contributed to conceptualisation of the review; provided substantive input to data gathering, analysis, interpretation and writing; and led the companion review (Trieu 2015).
NRCC: contributed to conceptualisation of the review; provided substantive input to data gathering, analysis, interpretation and writing.
All review authors have read and approved the final submitted version of this review.
Sources of support
Internal sources
No sources of support supplied
External sources
CIHR operating grant # SOK 116970, Canada.
Alberta Innovates ‐ Health Solutions Population Health Investigator Award (L. McLaren), Canada.
HSFC and CIHR Chair in Hypertension Prevention and Control (N. Campbell), Canada.
Applied Public Health Chair award funded by CIHR (Institute of Population and Public Health; Institute of Musculoskeletal Health and Arthritis), Public Health Agency of Canada, and Alberta Innovates ‐ Health Solutions (L. McLaren), Canada.
Declarations of interest
Lindsay McLaren: lead author on the only Canadian study included in this review. No other interests to declare.
Nureen Sumar: no interests to declare.
Amanda M Barberio: no interests to declare.
Kathy Trieu: no interests to declare.
Diane L Lorenzetti: no interests to declare.
Valerie Tarasuk: author on the only Canadian study included in this review. No other interests to declare.
Jacqui Webster discloses the following.
I am currently Director of the World Health Organization Collaborating Centre on Population Salt Reduction and co‐ordinator of the Australian Division of World Action on Salt and Health and have been supported in my work by grants from the National Health and Medical Research Council, the Victorian Health Promotion Foundation and headquarters and various regional offices of the World Health Organization. My Division receives funding support from Bupa Australia to develop and promote a nutritional phone application. The Food Policy Division also receives a small contribution (5k per year) from the Australian Food and Grocery Council as part of a much larger partnership project to reduce Australian salt intake. From 2003 to 2006, I managed the Salt Reduction programme of the UK government whilst working for the Food Standards Agency. I have just been awarded a four‐year co‐funded National Health and Medical Research Council and National Heart Foundation Career Development Fellowship to study international strategies to reduce salt.
Dr. Norman RC Campbell discloses the following.
2007: received travel funds from Dieticians of Canada, which were obtained from McCain to attend a regional meeting to talk about the importance of reducing dietary sodium.
2008: received samples of Mrs. DASH (a no‐salt salt substitute).
2010: received travel funds from Boehringer Ingelheim to attend two hypertension meetings.
2008: received samples of NuTek salt (a low salt substitute).
Receives salary from the Heart and Stroke Foundation of Canada and the Canadian Institutes of Health Research to lead and co‐ordinate efforts to prevent and control hypertension.
Serves as an unpaid consultant for many non‐government organisations and government organisations, none with a commercial flavour.
Receives occasional honoraria for speaking to academic groups on sodium (e.g. Canadian Council of Cardiovascular Nurses).
Dr Campbell was an author on the only Canadian study included in this review.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Austria {published and unpublished data}
- *Austria country questionnaire and associated correspondence. Country questionnaire 2014‐2015. [Google Scholar]
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Canada {published and unpublished data}
- *McLaren L, Heidinger S, Dutton DJ, Tarasuk V, Campbell NR. A repeated cross‐sectional study of socio‐economic inequities in dietary sodium consumption among Canadian adults: implications for national sodium reduction strategies. International Journal for Equity in Health 2014;13(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
China {published and unpublished data}
- *Du S, Neiman A, Batis C, Wang H, Zhang B, Zhang J, et al. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. American Journal of Clinical Nutrition 2014;99:334‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi Z, Liang X, Xu A, Wang L, Shi X, Zhao W, et al. Hypertension prevalence, awareness, treatment, and control and sodium intake in Shadong province, China: baseline results from Shadong‐Ministry of Health Action on Salt Reduction and Hypertension (SMASH). Preventing Chronic Disease 2011;11:E88. doi: 10.5888/pcd11.130423. [DOI] [PMC free article] [PubMed] [Google Scholar]
Denmark {published and unpublished data}
- *Denmark country questionnaire and associated correspondence. Country questionnaire 2014‐2015. [Google Scholar]
- Christensen AI, Ekholm O, Glumer C, Andreasen A, Hvidberg MF, Kristensen PL, et al. The Danish National Health Survey 2010. Study design and respondent characteristics. Scandinavian Journal of Public Health 2012;40:391‐7. [DOI] [PubMed] [Google Scholar]
Finland {published and unpublished data}
- Finland country questionnaire. Country questionnaire 2014.
- *Laatikainen T, Pietinen P, Valsta L, Sundvall J, Reinivuo H, Tuomilehto J. Sodium in the Finnish diet: 20‐year trends in urinary sodium excretion among the adult population. European Journal of Clinical Nutrition 2006;60(8):965‐70. [DOI] [PubMed] [Google Scholar]
- Helldán A, Raulio S, Kosola M, Tapanainen H, Ovaskainen M, Virtanen S. Finravinto 2012 ‐ tutkimus The National FINDIET 2012 Survey. National Institute for Health and Welfare 2013; Vol. 16.
- Pietinen P, Paturi M, Reinivuo H, Tapanainen H, Valsta LM. FINDIET 2007 Survey: energy and nutrient intakes. Public Health Nutrition 2010;13(6A):920‐4. [DOI] [PubMed] [Google Scholar]
- Puska P. The North Karelia Project: 30 years successfully preventing chronic diseases. Diabetes Voice 2008;53(Special issue):26‐9. [Google Scholar]
France {published and unpublished data}
- France country questionnaire. Country questionnaire 2014. [Google Scholar]
- *Dubuisson C, Lioret S, Touvier M, Dufour A, Calamassi‐Tran G, Volatier J‐L, et al. Trends in food and nutritional intakes of French adults from 1999 to 2007: results from the INCA surveys. British Journal of Nutrition 2010;103:1035‐48. [DOI] [PubMed] [Google Scholar]
- Meneton P, Lafay L, Tard A, Dufour A, Ireland J, Ménard J, et al. Dietary sources and correlates of sodium and potassium intakes in the French general population. European Journal of Clinical Nutrition 2009;63:1169‐75. [DOI] [PubMed] [Google Scholar]
Ireland {published and unpublished data}
- Ireland country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- Irish Social Science Data Archive [Survey on Lifestyle and Attitude to Nutrition (SLÁN)]. http://www.ucd.ie/issda/ Accessed May 2015.
- *Perry IJ, Browne G, Loughrey M, Harrington J, Lutomski J, Fitzgerald AP. Dietary salt intake and related risk factors in the Irish population. A report for safefood. Report 2010:ISBN: 978‐1‐905767‐13‐7.
- Harrington J, Perry I, Lutomski J, Morgan K, McGee H, Shelley E, et al. SLÁN 2007: Survey of Lifestyle, Attitudes and Nutrition in Ireland. Dietary Habits of the Irish Population. Dublin: Department of Health and Children, 2008.
- Irish Universities Nutrition Alliance (ed. Dr. Janette Walton). National Adult Nutrition Survey. Summary Report on Food and Nutrient Intakes, Physical Measurements, Physical Activity Patterns, and Food Choice Motives.. Irish Universities Nutrition Alliance, 2011.
- Morgan K, McGee H, Watson D, Perry I, Barry M, Shelly E, et al. SLAN 2007: Survey of Lifestyle, Attitudes & Nutrition in Ireland: Main Report. Report. Dublin: Department of Health and Children, 2008.
Japan {published and unpublished data}
- Japan country questionnaire. Country questionnaire 2014.
- *Udagawa K, Miyoshi M, Yoshiike N. Mid‐term evaluation of “Health Japan 21”: focus area for the nutrition and diet. Asia Pacific Journal of Clinical Nutrition 2008;17(S2):445‐52. [PubMed] [Google Scholar]
- Ikeda N, Takimoto H, Imai S, Miyachi M, Nishi N. Data Resource Profile: The Japan National Health and Nutrition Survey (NHNS). International Journal of Epidemiology 2015;44:1842‐9. [DOI] [PubMed] [Google Scholar]
- Miura K, Ando K, Tsuchihashi T, Yoshita K, Watanabe Y, Kawarazaki H, et al. [Scientific Statement] Report of the Salt Reduction Committee of the Japanese Society of Hypertension. (2) Goal and strategies of dietary salt reduction in the management of hypertension. Hypertension Research 2013;36:1020‐5. [DOI] [PubMed] [Google Scholar]
Netherlands {published and unpublished data}
- Netherlands country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- *Hendriksen MAH, Raaij JMA, Geleijnse JM, Wilson‐van den Hooven C, Ocké MC, A DL. Monitoring salt and iodine intakes in Dutch adults between 2006 and 2010 using 24 h urinary sodium and iodine excretions. Public Health Nutrition 2013;17:1431‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
New Zealand {published and unpublished data}
- New Zealand country questionnaire. Country questionnaire 2014.
- *New Zealand Ministry for Primary Industries. New Zealand Total Diet Study (NZTDS). http://www.foodsafety.govt.nz/policy‐law/food‐monitoring‐programmes/total‐diet‐study/ Accessed May 2015.
- University of Otago and Ministry of Health. Methodology Report for the 2008/09 New Zealand Adult Nutrition Survey. Wellington: Ministry of Health, 2011.
Switzerland {published and unpublished data}
- Switzerland country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- *Chappuis A, Bochud M, Glatz N, Vuistiner P, Paccaud F, Burnier M. Swiss survey on salt intake: main results. Service de Néphrologie et Institut Universitaire de Médecine Sociale et Préventive (CHUV),. Lausanne: Federal Office of Public Healh, 2011.
- Mordasini C, Abetel G, Lauterburg H, Ludi P, Perrenoud JP, Schmid H, et al. Sodium chloride intake and supply of iodine in the Swiss population. Schweizerische Medizinische Wochenschrift 1984;114(51):1924‐9. [PubMed] [Google Scholar]
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Thailand {published and unpublished data}
- Thailand country questionnaire. Country questionnaire 2014.
- *Supornsilaphachai C. Evolution of salt reduction initiatives in Thailand: lessons for other countries in the South‐East Asia Region. Regional Health Forum 2013; Vol. 17, issue 1:61‐71.
- Aekplakorn W, Chariyalertsak S, Kessomboon P, Sangthong R, Inthawong R, Putwatana P, et al. the Thai National Health Examination Survey IV Study Group. Prevalence and Management of Diabetes and Metabolic Risk Factors in Thai Adults: The Thai National Health Examination Survey IV, 2009. Diabetes Care 2011;34(9):1980‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turkey {published and unpublished data}
- Turkey country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- *Erdem Y, Arici M, Altun B, Turgan C, Sindel S, Erbay B, et al. The relationship between hypertension and salt intake in Turkish population: SALTURK study. Blood Pressure 2010;19:313‐8. [DOI] [PubMed] [Google Scholar]
United Kingdom ‐ England {published and unpublished data}
- United Kingdom country questionnaire. Country questionnaire 2014.
- *Millett C, Laverty AA, Stylianou N, Bibbins‐Domingo K, Pape UJ. Impacts of a national strategy to reduce population salt intake in England: serial cross sectional study. PLoS ONE 2012;7(1):e29836. doi:10.1371/journal.pone.0029836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He FJ, Pombo‐Rodrigues S, MacGregor GAS. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014;4(4):e004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Centre for Social Research. An assessment of dietary sodium levels among adults (aged 19‐64) in the UK general population in 2008, based on analysis of dietary sodium in 24 hour urine samples. MRC Human Nutrition Research 2008:1‐16.
- Sadler K, Nicholson S, Steer T, Gill V, Bates B, Tipping S, et al. National Diet and Nutrition Survey ‐ assessment of dietary sodium in adults (aged 19 to 64 years) in England, 2011: a survey carried out on behalf of the Department of Health. Report 2011.
- Shankar B, Brambila‐Macias J, Traill B, Mazzocchi M, Capacci S. An evaluation of the UK Food Standards Agency's salt campaign. Health Economics 2013;22:243‐50. [DOI] [PubMed] [Google Scholar]
- Wyness LA, Butriss JL, Stanner SA. Reducing the population's sodium intake: the UK Food Standards Agency's salt reduction programme. Public Health Nutrition 2012;15(2):254‐61. [DOI] [PubMed] [Google Scholar]
United Kingdom ‐ Great Britain {published and unpublished data}
- United Kingdom country questionnaire. Country questionnaire 2014.
- *Wyness LA, Butriss JL, Stanner SA. Reducing the population's sodium intake: the UK Food Standards Agency's salt reduction programme. Public Health Nutrition 2012;15(2):254‐61. [DOI] [PubMed] [Google Scholar]
- He FJ, Pombo‐Rodrigues S, MacGregor GAS. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014;4(4):e004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson L, Irving K, Gregory J, Bates CJ, Prentice A, Perks J, et al. The National Diet & Nutrition Survey: adults aged 19 to 64 years: vitamin and mineral intake and urinary analytes. National Diet and Nutrition Survey 2003; Vol. 3, issue Her Majesty’s Stationery Office (HMSO).
- Ji C, Kandala NB, Cappuccio FP. Spatial variation of salt intake in Britain and association with socioeconomic status. BMJ Open 2031;3(1):e002246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Centre for Social Research. An assessment of dietary sodium levels among adults (aged 19‐64) in the UK general population in 2008, based on analysis of dietary sodium in 24 hour urine samples. MRC Human Nutrition Research 2008:1‐16.
United Kingdom ‐ Scotland {published and unpublished data}
- United Kingdom country questionnaire. Country questionnaire 2014.
- *Scottish Centre for Social Research. A survey of 24 hour urinary sodium excretion in a representative sample of the Scottish population as a measure of salt intake. Report 2011:1‐25.
- National Centre for Social Research. A survey of 24 hour and spot urinary sodium and potassium excretion in a representative sample of the Scottish population. Joint Health Surveys Unit 2007:1‐30.
United States {published and unpublished data}
- United States of America country questionnaire. Country questionnaire 2014.
- *Pfeiffer CM, Hughes JP, Cogswell ME, Burt VL, Lacher DA, LaVoie DJ, et al. Urine sodium excretion increased slightly among U.S. adults between 1988 and 2010. The Journal of Nutrition 2014;144:698‐705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Trends in the prevalence of excess dietary sodium intake — United States, 2003–2010. MMWR ‐ Morbidity and Mortality Weekly Report 2013; Vol. 62, issue 50:1021‐5. [PMC free article] [PubMed]
- Cogswell ME, Zhang Z, Carriquiry AL, Gunn JP, Kuklina EV, Saydah SH, et al. Sodium and potassium intakes among US adults: NHANES 2003–2008. American Journal of Clinical Nutrition 2012;96:647‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G, Bowman BA. Recent economic evaluations of interventions to prevent cardiovascular disease by reducing sodium intake. Current Atherosclerosis Reports 2013;15(9):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Argentina {published and unpublished data}
- Argentina country questionnaire. Country questionnaire 2014.
- Legetic B, Campbell N. Reducing salt intake in the Americas: Pan American Health Organization actions. Journal of Health Communication 2011;16(Suppl 2):37‐48. [DOI] [PubMed] [Google Scholar]
Australia {published data only}
- Australia country questionnaire. Country questionnaire 2014.
- Australian Bureau of Statistics. Australian Health Survey 2011‐2013. http://www.abs.gov.au/australianhealthsurvey. [Australian Bureau of Statistics]
- Beard TC, Woodwork DR, Ball PJ, Hornsby H, Dwyer T. The Hobart Salt Study 1995: few meet national sodium intake target. The Medical Journal of Australia 1997;166(8):404. [DOI] [PubMed] [Google Scholar]
- Grimes CA, Campbell KJ, Riddell LJ, Nowson CA. Is socioeconomic status associated with dietary sodium intake in Australian children? A cross‐sectional study. BMJ Open 2013;3:doi:10.1136/bmjopen‐2012‐002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Land MA, Webster J, Christoforou A, Praveen D, Jeffery P, Chalmers J, et al. Salt intake assessed by 24‐hour urinary sodium excretion in a random and opportunistic sample in Australia. BMJ 2014;4(1):doi: 10.1136/bmjopen‐2013‐003720.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margerison C, Nowson C. Dietary intake and 24‐hour excretion of sodium and potassium. Asia Pacific Journal of Clinical Nutrition 2006;15(Suppl 3):S37. [Google Scholar]
Bangladesh. {published and unpublished data}
- Bangladesh country questionnaire. Country questionnaire 2014.
- World Health Organization. Regional Health Forum – WHO South East Asia Region: special issue on blood pressure – take control. Report 2013; Vol. 17, issue 1:1‐83.
Barbados {published and unpublished data}
- Barbados country questionnaire. Country questionnaire 2014.
- World Health Organization. Strategies to monitor and evaluate population sodium consumption and sources of sodium in the diet; report of a joint technical meeting convened by the WHO and the Government of Canada, October 2010. Report 2011:1‐40.
Croatia {published and unpublished data}
- World Health Organization. Mapping salt reduction initiatives in the European Region. WHO Regional Office for Europe 2013:1‐50.
Iceland {published and unpublished data}
- World Health Organization. Mapping salt reduction initiatives in the European Region. WHO Regional Office for Europe 2013:1‐50.
Indonesia {published and unpublished data}
- Indonesia country questionnaire. Country questionnaire 2014.
- World Health Organization. Expert Meeting on Population Sodium Reduction Strategies for Prevention and Control of Noncommunicable Diseases in the South‐East Asia Region. WHO Regional Office for South‐East Asia 2012:1‐43.
Israel {published and unpublished data}
- Israel country questionnaire. Country questionnaire 2014.
- Keinan Boker, Lital. (CM). Mabat First Israeli National Health and Nutrition Survey, 1999‐2001. Report.
- World Health Organization. Mapping salt reduction initiatives in the European Region. WHO Regional Office for Europe 2013:1‐50.
Italy {published and unpublished data}
- Italy country questionnaire and associated correspondence. Country questionnaire 2014.
- Donfrancesco C, Ippolito R, Noce CL, Palmieri L, Iacone R, Russo O, et al. Excess dietary sodium and inadequate potassium intake in Italy: results of the MINISAL study. Nutrition, Metabolism and Cardiovascular Diseases 2013;23(9):850‐6. [DOI] [PubMed] [Google Scholar]
- European Commission. Implementation of the European Union Salt Reduction Framework; Results of Member States Survey. Report 2012:1‐15.
- World Health Organization. Mapping salt reduction initiatives in the European Region. WHO Regional Office for Europe 2013:1‐50.
Malaysia {published and unpublished data}
- Malaysia country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- Mohd Shariff Z, Mohd Yusof S, My KZ. Energy and nutrient intakes: findings from the Malaysian Adult Nutrition Survey (MANS). Malaysian Journal of Nutrition 2008;14(1):1‐24. [PubMed] [Google Scholar]
Poland {published and unpublished data}
- Poland country questionnaire. Country questionnaire 2014.
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Portugal {published and unpublished data}
- Portugal country questionnaire. Country questionnaire 2014.
- Polonia J, Martins L, Pinto F, Nazare J. Prevalence, awareness, treatment and control of hypertension and salt intake in Portugal: changes over a decade. The PHYSA study. Journal of Hypertension 2014;32(6):1211‐21. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Singapore {published and unpublished data}
- Singapore country questionnaire. Country questionnaire 2014.
- Batcagan‐Abueg AP, Lee JJ, Chan P, Rebello SA, Amarra MSV. Salt intakes and salt reduction initiatives in Southeast Asia: a review. Asia Pacific Journal of Clinical Nutrition 2013;22(4):683. [DOI] [PubMed] [Google Scholar]
Slovakia {published and unpublished data}
- World Health Organization. Mapping salt reduction initiatives in the European Region. WHO Regional Office for Europe 2013:1‐50.
- World Health Organization. Nutrition, Physical Activity and Obesity ‐ Slovakia. Report 2013:1‐5.
Slovenia {published and unpublished data}
- Slovenia country questionnaire. Country questionnaire 2014.
- Ribič CH, Zakotnik JM, Vertnik L, Vegnuti M, Cappuccio FP. Salt intake of the Slovene population assessed by 24 h urinary sodium excretion. Public Health Nutrition 2010;13(11):1803‐9. [DOI] [PubMed] [Google Scholar]
Sri Lanka {published and unpublished data}
- Sri Lanka country questionnaire. Country questionnaire 2014.
- Jayawardena R, Thennakoon S, Byrne N, Soares M, Katulanda P, Hills A. Energy and nutrient intakes among Sri Lankan adults. International Archives of Medicine 2014;7(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Regional Office for South‐East Asia. Expert Meeting on Population Sodium Reduction Strategies for Prevention and Control of Noncommunicable Diseases in the South‐East Asia Region SEARO, New Delhi, 11‐13 December 2012. Report 2013.
Uruguay {published and unpublished data}
- Uruquay country questionnaire. Country questionnaire 2014.
- Penney S. Dropping the salt: practical steps countries are taking to prevent chronic non‐communicable diseases through population‐wide dietary salt reduction. Prepared for the Public Health Agency of Canada 2009.
Vietnam {published and unpublished data}
- Vietnam country questionnaire. Country questionnaire 2014.
References to ongoing studies
Belgium {published and unpublished data}
- Belgium country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- European Commission. Implementation of the European Union Salt Reduction Framework; Results of Member States Survey. Luxembourg: Publications Office of the European Union 2012:1‐15.
- Vandevijvere S. Study report: estimation of salt intake in two regions in Belgium through analysis of sodium in 24‐hour urine samples. Scientific Institute of Public Health, Unit of Epidemiology 2009:1‐23.
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Brazil {published and unpublished data}
- Brazil country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- Sarno F, Claro RM, Levy RB, Bandoni DH, Monteiro CA. [Estimated sodium intake for the Brazilian population, 2008‐2009]. Revista de Saúde Pública 2013;47(3):571‐8. [DOI] [PubMed] [Google Scholar]
Bulgaria {published and unpublished data}
- Bulgaria country questionnaire. Country questionnaire 2014.
- European Commission. Implementation of the European Union Salt Reduction Framework; Results of Member States Survey. Luxembourg: Publications Office of the European Union 2012:1‐15.
- World Health Organization. Mapping sodium reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Chile {published and unpublished data}
- Chile country questionnaire. Country questionnaire 2014.
Costa Rica {published and unpublished data}
- Costa Rica country questionnaire. Country questionnaire 2014.
- Blanco‐Metzler A, Montero‐Campos MDLÁ, Núñez‐Rivas H, Gamboa‐Cerda C, Sánchez G. Advances in reducing salt and sodium intake in Costa Rica. Revista Panamericana de Salud Pública 2012;32(4):316‐20. [DOI] [PubMed] [Google Scholar]
Fiji {published and unpublished data}
- Fiji country questionnaire. Country questionnaire 2014.
Hungary {published and unpublished data}
- Hungary country questionnaire. Country questionnaire 2014.
- European Commission. Implementation of the European Union Salt Reduction Framework; Results of Member States Survey. Luxembourg: Publications Office of the European Union 2012:1‐15.
- Martos É, Bakacs M, Sarkadi‐Nagy E, Ráczkevy T, Zentai A, Baldauf Z, et al. Hungarian Diet and Nutritional Status Survey – the OTAP2009 study. IV. Macroelement intake of the Hungarian population. Orvosi Hetilap 2012;153(29):1132‐41. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Lithuania {published and unpublished data}
- Lithuania country questionnaire. Country questionnaire 2014.
Mongolia {published and unpublished data}
- Mongolia country questionnaire. Country questionnaire 2014.
- Ministry of Health, Mongolia, National Center for Public Health, Mongolia, World Health Organization, Mongolia Country Office, Millennium Challenge Account – Mongolia, Health Project. Salt Intake of the Population, Survey report, Ulaanbaatar. Report 2013:1‐82.
- Yamada C, Oyunchimeg D, Erdenbat A, Enkhtuya P, Buttumur D, Naran G, et al. Estimation of salt intake and recommendation for iodine content in iodized salt in Mongolia. Asia‐Pacific Journal of Public Health 2000;12(1):27‐31. [DOI] [PubMed] [Google Scholar]
Norway {published and unpublished data}
- Norway country questionnaire and associated correspondence. Country questionnaire 2014‐15.
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Republic of South Korea {published and unpublished data}
- South Korea country questionnaire. Country questionnaire 2014.
- Rhee MY, Shin SJ, Park SH, Kim SW. Sodium intake of a city population in Korea estimated by 24‐h urine collection method. European Journal of Clinical Nutrition 2013;67(8):875‐80. [DOI] [PubMed] [Google Scholar]
- Shim E, Ryu HJ, Hwang J, Kim SY, Chung EJ. Dietary sodium intake in young Korean adults and its relationship with eating frequency and taste preference. Nutrition Research and Practice 2013;7(3):192‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sweden {published and unpublished data}
- Sweden country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
- European Commission. Implementation of the European Union Salt Reduction Framework; Results of Member States survey. Luxembourg: Publications Office of the European Union 2012:1‐15.
- World Health Organization. Mapping salt reduction initiatives in the WHO European Region. WHO Regional Office for Europe 2013:1‐50.
Additional references
Andersen 2009
- Andersen L, Rasmussen LB, Larsen EH, Jakobsen J. Intake of household salt in a Danish population. European Journal of Clinical Nutrition 2009;63:598‐604. [DOI] [PubMed] [Google Scholar]
Asaria 2007
- Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 2007;370(9604):2044‐53. [DOI] [PubMed] [Google Scholar]
Austria country questionnaire 2014‐2015
- Austria country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
Bambra 2010
- Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. Journal of Epidemiology and Community Health 2010;64:284‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bibbins‐Domingo 2010
- Bibbins‐Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, et al. Projected effect of dietary salt reductions on future cardiovascular disease. New England Journal of Medicine 2010;362:590‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chappuis 2011
- Chappuis A, Bochud M, Glatz N, Vuistiner P, Paccaud F, Burnier M. Swiss survey on salt intake: main results. Service de Néphrologie et Institut Universitaire de Médecine Sociale et Préventive (CHUV), 2011.
CPA 1978
- Consumer Protection Act, RSQ, c P‐40.1. Government of Quebec. Quebec, 1978:ss248‐9.
CSDH 2008
- Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on the Social Determinants of Health.. Geneva: World Health Organisation, Geneva: World Health Organization, 2008.
Dall 2009
- Dall TM, Fulgoni VL III, Zhang Y, Reimers KJ, Packard PT, Astwood JD. Potential health benefits and medical cost savings from calorie, sodium, and saturated fat reductions in the American diet. American Journal of Health Promotion 2009;23:412‐22. [DOI] [PubMed] [Google Scholar]
Denmark country questionnaire 2014‐2015
- Denmark country questionnaire and associated correspondence. Country questionnaire 2014‐2015.
Du 2014
- Du S, Neiman A, Batis C, Wang H, Zhang B, Zhang J, et al. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. American Journal of Clinical Nutrition 2014;99:334‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dubuisson 2010
- Dubuisson C, Lioret S, Touvier M, Dufour A, Calamassi‐Tran G, Volatier J‐L, et al. Trends in food and nutritional intakes of French adults from 1999 to 2007: results from the INCA surveys. British Journal of Nutrition 2010;103:1035‐48. [DOI] [PubMed] [Google Scholar]
Erdem 2010
- Erdem Y, Arici M, Altun B, Turgan C, Sindel S, Erbay B, et al. The relationship between hypertension and salt intake in Turkish population: SALTURK study. Blood Pressure 2010;19:313‐8. [DOI] [PubMed] [Google Scholar]
Ezzati 2002
- Ezzati M, Lopez AD, Vander Hoorn S, Murray CJ. Comparative risk assessment collaborating group. Lancet 2002;360(9343):1347‐60. [DOI] [PubMed] [Google Scholar]
Frohlich 2008
- Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. American Journal of Public Health 2008;98:216‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaziano 2009
- Gaziano TA, Bitton A, Anand S, Weinstein MC, International Society of Hypertension. The global cost of nonoptimal blood pressure. Journal of Hypertension 2009;27:1472‐7. [DOI] [PubMed] [Google Scholar]
GRADE n.d.
- GRADE Working Group. Grading of Recommendations Assessment, Development and Evaluation. http://www.gradeworkinggroup.org/ Accessed December 2015.
He 2009
- He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. Journal of Human Hypertension 2009;23:363‐84. [DOI] [PubMed] [Google Scholar]
Hendriksen 2013
- Hendriksen MAH, Raaij JMA, Geleijnse JM, Wilson‐van den Hooven C, Ocké MC, A DL. Monitoring salt and iodine intakes in Dutch adults between 2006 and 2010 using 24 h urinary sodium and iodine excretions. Public Health Nutrition 2013;17:1431‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, The Cochrane Collaboration, 2011. www.cochrane‐handbook.org. [Google Scholar]
Hooper 2004
- Hooper L, Bartlett C, Davey Smith G, Ebrahim S. Advice to reduce dietary salt for prevention of cardiovascular disease. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD003656.pub2] [DOI] [PubMed] [Google Scholar]
Iheozor‐Ejiofor 2015
- Iheozor‐Ejiofor Z, Worthington HV, Walsh T, O’Malley L, Clarkson JE, Macey R, et al. Water fluoridation for the prevention of dental caries. Cochrane Database of Systematic Reviews 2015, Issue 6. [DOI: 10.1002/14651858.CD010856.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ji 2014
- Ji C, Cappuccio FP. Socioeconomic inequality in salt intake in Britain 10 years after a national salt reduction programme. BMJ Open 2014;4(8):doi: 10.1136/bmjopen‐2014‐005683. [DOI] [PMC free article] [PubMed] [Google Scholar]
Joffres 2007
- Joffres MR, Campbell NR, Manns B, Tu K. Estimate of the benefits of a population‐based reduction in dietary sodium additives on hypertension and its related health care costs in Canada. Canadian Journal of Cardiology 2007;23:437‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laatikainen 2006
- Laatikainen T, Pietinen P, Valsta L, Sundvall J, Reinivuo H, Tuomilehto J. Sodium in the Finnish diet: 20‐year trends in urinary sodium excretion among the adult population. European Journal of Clinical Nutrition 2006;60(8):965‐70. [DOI] [PubMed] [Google Scholar]
Lopez 2006
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367:1747‐57. [DOI] [PubMed] [Google Scholar]
Mattes 1991
- Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. Journal of the American College of Nutrition 1991;10:383‐93. [DOI] [PubMed] [Google Scholar]
McLaren 2010
- McLaren L, McIntyre L, Kirkpatrick S. Rose's population strategy of prevention need not increase social inequalities in health. International Journal of Epidemiology 2010;39:372‐7. [DOI] [PubMed] [Google Scholar]
McLaren 2013
- McLaren L, Sumar N, Lorenzetti DL, Campbell NRC, Tarasuk V. Population‐level interventions in government jurisdictions for dietary sodium reduction. Cochrane Database of Systematic Reviews 2013, Issue 8. [DOI: 10.1002/14651858.CD010166] [DOI] [PMC free article] [PubMed] [Google Scholar]
McLaren 2014
- McLaren L, Heidinger S, Dutton DJ, Tarasuk V, Campbell NR. A repeated cross‐sectional study of socio‐economic inequities in dietary sodium consumption among Canadian adults: implications for national sodium reduction strategies. International Journal for Equity in Health 2014;13(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
McLean 2014
- McLean RM. Measuring population sodium intake: a review of methods. Nutrients 2014;6:4651‐62; doi:10.3390/nu6114651. [DOI] [PMC free article] [PubMed] [Google Scholar]
Millett 2012
- Millett C, Laverty AA, Stylianou N, Bibbins‐Domingo K, Pape UJ. Impacts of a national strategy to reduce population salt intake in England: serial cross sectional study. PLoS ONE 2012;7(1):e29836. doi:10.1371/journal.pone.0029836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohan 2009
- Mohan S, Campbell NR. Salt and high blood pressure. Clinical Science 2009;117:1‐11. [DOI] [PubMed] [Google Scholar]
Moubarac 2014
- Moubarac JC, Batal M, Martins AP, Claro R, Levy RB, Cannon G, et al. Processed and ultra‐processed food products: consumption trends in Canada from 1938 to 2011. Canadian Journal of Dietetic Practice and Research 2014;75(1):15‐21. [DOI] [PubMed] [Google Scholar]
New Zealand Ministry for Primary Industries
- New Zealand Ministry for Primary Industries. New Zealand Total Diet Study (NZTDS). Report. http://www.foodsafety.govt.nz/policy‐law/food‐monitoring‐programmes/total‐diet‐study/.
Ottawa Charter 1986
- World Health Organization, Health and Welfare Canada, Canadian Public Health Association. Ottawa Charter for Health Promotion. http://www.phac‐aspc.gc.ca/ph‐sp/docs/charter‐chartre/pdf/charter.pdf. Ottawa, Ontario, Canada, 1986. Accessed June 2016.
Penney 2011
- Penney S. Dropping the Salt 2: a database of global activities and plans to prevent chronic non‐communicable diseases through population‐wide dietary salt reduction. Prepared for the Public Health Agency of Canada, 2011.
Perry 2010
- Perry IJ, Browne G, Loughrey M, Harrington J, Lutomski J, Fitzgerald AP. Dietary salt intake and related risk factors in the Irish population. A report for safefood. Report 2010:ISBN: 978‐1‐905767‐13‐7.
Pfeiffer 2014
- Pfeiffer CM, Hughes JP, Cogswell ME, Burt VL, Lacher DA, LaVoie DJ, et al. Urine sodium excretion increased slightly among U.S. adults between 1988 and 2010. The Journal of Nutrition 2014;144:698‐705. [DOI] [PMC free article] [PubMed] [Google Scholar]
PHAC 2006
- Public Health Agency of Canada. Canada’s response to WHO Commission on Social Determinants of Health. http://www.phac‐aspc.gc.ca/sdh‐dss/crg‐grc‐eng.php Accessed June 2016.
Powles 2013
- Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. on behalf of the Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE). Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3:e003733 doi:10.1136/bmjopen‐2013‐003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
Puska 2008
- Puska P. The North Karelia Project: 30 years successfully preventing chronic diseases. Diabetes Voice 2008;53(Special issue):26‐9. [Google Scholar]
Raphael 2009
- Raphael D (ed). Social Determinants of Health. 2nd Edition. Toronto: Candian Scholars' Press Inc, 2009. [Google Scholar]
Rehfuess 2013
- Rehfuess EA, Akl EA. Current experience with applying the GRADE approach to public health interventions: an empirical study. BMC Public Health 2013;13(9):doi: 10.1186/1471‐2458‐13‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ricciuto 2009
- Ricciuto L, Lin K, Tarasuk V. A comparison of the fat composition and prices of margarines between 2002 and 2006, when new Canadian labelling regulations came into effect. Public Health Nutrition 2009;12(8):1270‐5. [DOI] [PubMed] [Google Scholar]
Rose 1992
- Rose G. The Strategy of Preventive Medicine. Oxford: Oxford University Press, 1992. [Google Scholar]
Scottish Centre for Social Research 2011
- Scottish Centre for Social Research. A survey of 24 hour urinary sodium excretion in a representative sample of the Scottish population as a measure of salt intake. Report 2011:1‐25.
Smith‐Spangler 2010
- Smith‐Spangler CM, Juusola JL, Enns EA, Owens DK, Garber AM. Population strategies to decrease sodium intake and the burden of cardiovascular disease: a cost‐effectiveness analysis. Annals of Internal Medicine 2010;152:481‐7. [DOI] [PubMed] [Google Scholar]
Strazzullo 2009
- Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta‐analysis of prospective studies. BMJ 2009;339:b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sumar 2011
- Sumar N, McLaren L. Impact on social inequalities of population strategies of prevention for folate intake in women of childbearing age. [Review]. American Journal of Public Health 2011;101:1218‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Supornsilaphachai 2013
- Supornsilaphachai C. Evolution of salt reduction initiatives in Thailand: lessons for other countries in the South‐East Asia Region. Regional Health Forum 2013;17(1):61‐71. [Google Scholar]
SWG 2010
- Sodium Working Group (SWG). Sodium reduction strategy for Canada – recommendations of the Sodium Working Group, 2010. http://www.hc‐sc.gc.ca/fn‐an/nutrition/sodium/related‐info‐connexe/strateg/reduct‐strat‐eng.php 2010. Accessed June 2016.
Taylor 2011
- Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009217] [DOI] [PMC free article] [PubMed] [Google Scholar]
Trieu 2015
- Trieu K, Neal B, Hawkes C, Dunford E, Campbell N, Rodriguez‐Fernandez R, et al. Salt reduction initiatives around the world – a systematic review of progress towards the global target. PLOS ONE 2015;10:DOI:10.1371/journal.pone.0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
Udagawa 2008
- Udagawa K, Miyoshi M, Yoshiike N. Mid‐term evaluation of “Health Japan 21”: focus area for the nutrition and diet. Asia Pacific Journal of Clinical Nutrition 2008;17(52):445‐52. [PubMed] [Google Scholar]
USDHHS
- U.S. Department of Health and Human Services. Healthy People 2020. http://www.healthypeople.gov Accessed June 2016.
Vasan 2002
- Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D'Agostino RB, et al. Residual lifetime risk for developing hypertension in middle‐aged women and men: the Framingham Heart Study. JAMA 2002;287:1003‐10. [DOI] [PubMed] [Google Scholar]
Webster 2011
- Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. Journal of Hypertension 2011;29:1043‐50. [DOI] [PubMed] [Google Scholar]
Whitehead 2007
- Whitehead M. A typology of actions to tackle social inequalities in health. Journal of Epidemiology & Community Health 2007;61:473‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2003
- World Health Organization (WHO). Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation. Report. Geneva: WHO, 2003.
WHO 2007
- World Health Organization. Reducing salt intake in populations: report of a WHO forum and technical meeting. Paris 2006. Accessed June 2016; Vol. p3., issue www.who.int/dietphysicalactivity/Salt_Report_VC_april07.pdf.
WHO 2013
- World Health Organization. Follow‐up to the Political Declaration of the High‐Level Meeting of the General Assembly on the Prevention and Control of Non‐Communicable Diseases: Sixty‐Sixth World Health Assembly (WHA66.10). Geneva, Switzerland: World Health Organization, 2013.
World Bank
- World Bank. Country and lending groups. http://data.worldbank.org/about/country‐and‐lending‐groups Accessed June 2016.
Wyness 2012
- Wyness LA, Butriss JL, Stanner SA. Reducing the population's sodium intake: the UK Food Standards Agency's salt reduction programme. Public Health Nutrition 2012;15(2):254‐61. [DOI] [PubMed] [Google Scholar]