Abstract
Background:
In King County, Washington, the HIV prevalence among men who have sex with men (MSM) who inject methamphetamine is high, while it is low among other people who inject drugs (PWID). Local drug problem indicators suggest that methamphetamine use is increasing. The extent to which this increase affects MSM and non-MSM, and whether MSM and non-MSM networks are connected through injection equipment sharing, is unknown.
Methods:
We used data from two serial cross-sectional surveys of PWID including five biannual surveys of Public Health–Seattle and King County Needle and Syringe Exchange Program clients (NSEP, N=2,135, 2009–2017) and three National HIV Behavioral Surveillance IDU surveys (NHBS, N=1,709, 2009–2015).
Results:
The proportion of non-MSM PWID reporting any recent methamphetamine injection increased significantly from approximately 20% in 2009 to 65% in 2017. Most of this increase was attributable to injecting methamphetamine in combination with heroin (goofballs). PWID who injected goofballs were more likely to be younger, homeless or unstably housed, report daily injection, and self-report an opioid overdose in the past year than other PWID. The majority of PWID who injected methamphetamine reported sharing any injection equipment. Among these PWID, 43% of MSM had last shared injection equipment with a non-MSM. Eight percent of non-MSM men and 15% of women had last shared equipment with an MSM.
Conclusions:
Given non-trivial rates of sharing injection equipment with methamphetamine-using MSM, a population with an HIV prevalence of 40%, non-MSM who inject methamphetamine could be an emerging population at risk for acquiring HIV.
Keywords: injection drug use, methamphetamine, HIV, men who have sex with men, surveillance
1. INTRODUCTION
A notable success in HIV prevention has been the substantial decrease in HIV/AIDS incidence among people who inject drugs (PWID) in the United States. The number of AIDS diagnoses among PWID peaked in 1993 at approximately 23,000 new diagnoses and by 2016 had declined by nearly 90% (Centers for Disease Control and Prevention, 2017). This is in contrast to an approximately 70% decline in AIDS cases among men who have sex with men (MSM) during the same time period (Centers for Disease Control and Prevention;Viral Hepatitis, Sexual Transmitted Diseases and Tuberculosis Prevention, Division of HIV/AIDS Prevention, 2017). In addition to the use of antiretroviral therapy, this reduction in risk among PWID is likely due to expanded harm reduction services like needle and syringe exchange programs (NSEP), decreased needle and syringe sharing among PWID, and decreased transmission risk from HIV-infected persons due to antiretroviral therapy (Aspinall et al., 2014; Burt and Thiede, 2016; Montaner et al., 2010). However, the recent HIV outbreak among PWID injecting pharmaceutical opioids in Scott County, Indiana, demonstrated the ongoing potential for explosive transmission when HIV is introduced in the context of injection equipment sharing and uncontrolled HIV viral load (Peters et al., 2016).
Despite the overall reduction in new HIV diagnoses among PWID, in some U.S. jurisdictions HIV risk has been strongly associated with methamphetamine use (both injection and non-injection use) among men who have sex with men (MSM) (Buchacz et al., 2005; Plankey et al., 2007; Thiede et al., 2009). For example, in King County, Washington, HIV prevalence among MSM who have used methamphetamine in the past year is approximately 40%, higher than any other subgroup (Glick et al., 2016, 2015). This is in contrast to the prevalence among all MSM (15–20%) and non-MSM men and women who inject drugs (~3%) (Glick et al., 2016). Moreover, methamphetamine use has been associated with lower levels of viral suppression among HIV-infected persons (Fairbairn et al., 2011; Feldman et al., 2015).
There have been recent signals of increased methamphetamine use in King County, Washington. The number of methamphetamine-involved overdose deaths, the number of police cases involving methamphetamine, and wastewater measures have all indicated an increase in methamphetamine use (Banta-Green et al., 2016). Recently published data from Denver also reported an increase in methamphetamine use over the past decade, especially methamphetamine injected with heroin (goofballs) (Al-Tayyib et al., 2017). However, these reports have not indicated if the increase in methamphetamine use was among MSM, where use has historically been concentrated in King County, or among non-MSM. An increase in methamphetamine use among MSM would suggest the need for more targeted HIV prevention efforts. An increase in methamphetamine use among non-MSM men and women – particularly in the context of injection equipment sharing – could predict an emerging population at risk for HIV.
1.1. Aims
To identify the populations in which methamphetamine use is increasing and potential HIV transmission risk across MSM and non-MSM networks, we investigated temporal trends in methamphetamine use and injection equipment sharing in King County among MSM and non-MSM who inject drugs. We also evaluated characteristics of people who inject methamphetamine – alone and in combination with other drugs – as well as characteristics of recent equipment sharing partners.
2. METHODS
2.1. Data and Measures
We analyzed data from two serial cross-sectional surveys of PWID in King County.
2.1.1. Public Health – Seattle & King County Needle and Syringe Exchange Program Survey (NSEP).
This is an attempted census of NSEP clients that has been conducted on an approximately biannual basis since 2003. Survey methods and cross-sectional findings from earlier surveys have been published elsewhere (Cedarbaum and Banta-Green, 2016; Jenkins et al., 2011; Peavy et al., 2012). Briefly, over a two week period in early summer, NSEP staff attempted to invite every client seeking services at the NSEP to participate. There were no other inclusion or exclusion criteria. The survey includes questions about client demographics, drug use and drug-related behaviors, sexual behavior, and health conditions and needs. Interviewers administered the surveys by reading aloud each question and recording responses on paper (2003–2013 surveys) or directly into a laptop computer or tablet using REDCap (Research Electronic Data Capture) electronic data capture tools (2015–2017 surveys) (Harris et al., 2009). The survey is anonymous and most clients completed it in about 10 minutes. Clients were offered a piece of candy for their participation. When collected, participation rates have ranged from 51% to 82%. (These response rates are likely underestimates since NSEP clients may have been approached multiple times to participate. Given the anonymous nature of the survey, there was no way to link participation data for participants who initially declined but later agreed to participate.) Because the NSEP survey was conducted for purposes of public health surveillance and program evaluation, and did not include any identifiable data, it was not considered human subjects research and it did not require IRB approval.
For this analysis, we used data from the five most recent surveys – 2009, 2011, 2013, 2015, 2017 – due to the inclusion of questions about gender of sexual partners and methamphetamine use. Participants were asked about the gender of their sex partners in the past year: male, female, both male and female, or no sex in the past year. Clients were defined as MSM if they reported male gender and any male partners in the past year. To measure recent methamphetamine injection, we used responses from a series of questions that asked clients about the drugs they had injected in the past 3 months (2011–2017) or since the beginning of the year (2009). (Surveys are typically conducted in June, so this would equate to approximately 5–6 months in 2009.) The questions asked about both injecting methamphetamine alone and in combination with heroin. To measure any methamphetamine injection, we included any reported methamphetamine injection, either alone or in goofballs. There were separate questions that asked about the number of persons with whom a client shared syringes or other injection sharing equipment (cottons, cookers, or rinse water) in the past 3 months. If clients reported sharing any injection equipment with one or more other people, we classified them as sharing. The survey also included questions about client demographics (age, race/ethnicity), current housing status, average number of injections per day, and any self-reported opioid overdose in the past 12 months.
2.1.2. Seattle-area National HIV Behavioral Surveillance Injection Drug Use Survey (NHBS-IDU).
NHBS is a CDC-funded surveillance system of HIV and risk behaviors, and we used data from the three most recent NHBS-IDU cycles conducted in the Seattle area (2009, 2012, 2015). NHBS-IDU survey methods have been previously described (Burt et al., 2017; Burt and Thiede, 2014, 2012). Briefly, participants were recruited using respondent-driven sampling, a coupon-based incentivized peer referral method. To be eligible for the NHBS-IDU cycles, participants must have been age 18 years or older, a resident of King or Snohomish Counties, able to complete the survey in English, alert enough to complete the survey, and reported any injection drug use in the past 12 months. Trained interviewers administered the 60–90 minute anonymous behavioral survey which included questions about participant demographics, drug use and drug-related behaviors, sexual behaviors, and health conditions including HIV and hepatitis C. Participants received $50 for completing the survey and an HIV test, and an additional $10 for each other eligible participant recruited. All survey procedures were approved by the Washington State Institutional Review Board (IRB). The data used in the analysis did not include any identifiers, thus this analysis did not require IRB approval.
The measures used from NHBS-IDU were very similar to those in the NSEP surveys, although the time frame for most questions was 12 months as opposed to 3 months. Participants were asked separately about their number of male and female sex partners in the past 12 months and categorized as MSM if they identified as male and reported any male partners in the past year. The survey included questions about the frequency of individual drug and drug combinations injected in the past 12 months, which allowed us to measure any methamphetamine injection. The NHBS-IDU survey did not include a question specifically about goofball injection. Syringe and other equipment sharing in the past 12 months were measured in separate questions. In the NHBS-IDU surveys, there was a module regarding the participant’s most recent injection equipment sharing partner which included questions about that person’s gender and whether that person was ever a MSM. For this analysis, we also included questions on participant demographics (age, race/ethnicity), current housing status, average number of injections per day, and overdose in the past 12 months.
2.2. Analysis
Participants who did not answer questions about their gender or the gender of their sex partners were excluded from analysis (32 in the NSEP survey, 15 in the NHBS-IDU survey). We excluded persons who identified as transgender due to small sample size (8 in each survey). We used descriptive statistics to describe the demographic characteristics, reported methamphetamine use, and injection equipment sharing of each sample. Participant characteristics were compared between surveys using t-tests and chi-square tests. To evaluate temporal trends for any methamphetamine injection and any goofball injection, we tested for linear trends using Poisson regression with a log link and robust standard errors. Due to variation in sample characteristics between years for each survey, we adjusted models for participant age, race, and interview site (Seattle or South King County). For NHBS-IDU, we further adjusted these models for injection network size and clustered on RDS seed to account for potential correlation within recruitment chains. Using NSEP survey data only, we used Poisson regression with a log link and robust standard errors to evaluate characteristics of goofball injectors compared to all other PWID. Analyses of self-reported opioid overdose were limited to persons reporting any opioid use in the past year (injection or non-injection). Analyses related to injection equipment sharing were restricted to participants reporting any methamphetamine injection. Results were stratified between MSM and non-MSM. There were no consistent, meaningful differences between non-MSM and women, so these groups were combined for most analyses. Using NHBS-IDU data only, we estimated the proportion of recent equipment sharing partners who were MSM, other men, or women.
3. RESULTS
3.1. Sample Characteristics
The characteristics of participants in the NSEP and NHBS-IDU surveys are shown in Table 1. Comparing all NSEP clients to all NHBS-IDU participants, NSEP clients were more likely to be younger (mean age, 37.7 vs. 42.6 years, P < 0.01), male (69% vs. 65%, P = 0.01) and non-Hispanic White (71.7% vs. 61.0%, P <0.01). Approximately 16% of all men reported sex with a man in the past year. Homelessness and unstable housing were very common in both samples. The majority of participants reported injecting drugs at least once a day, although daily injection was less likely among NSEP clients (68% vs. 74%, P < 0.01). Among PWID who reported any opioid use, 19% of NSEP clients and 16% of NHBS participants self-reported an opioid overdose in the past year (P = 0.01). Seven percent of NHBS-IDU participants were HIV-infected and 71% had a reactive hepatitis C antibody test.
Table 1.
Characteristics of Public Health – Seattle and King County Needle and Syringe Exchange Program (NSEP) clients, 2009–2017, and Seattle-area National HIV Behavioral Surveillance Injection Drug Use Cycle (NHBS-IDU) participants, 2009–2015
| Characteristic | NSEP Clients 2009–2017 N=2,135 N (%) | NHBS-IDU Participants 2009–2015 N=l,709 N (%) | p-value7 |
|---|---|---|---|
| Age, mean [SD] | 37.7 [11.8] | 42.6 [11.5] | <0.01 |
| Gender | 0.01 | ||
| Female | 669 (31.3) | 606 (35.5) | |
| Male | 1,466 (68.7) | 1,103 (64.5) | |
| Men who have sex with men1 | 241 (16.4) | 184 (16.7) | 0.87 |
| White, non-Hispanic | 1,525 (71.7) | 1,044 (61.2) | <0.01 |
| Homeless or unstably housed2 | 1,248 (58.7) | 835 (48.9) | <0.01 |
| Injects drugs daily | 1,419 (67.6) | 1,249 (74.0) | <0.01 |
| Opioid overdose, past year3,4 | 367 (19.4) | 256 (16.1) | 0.01 |
| HIV-infected5 | -- | 119 (7.0) | -- |
| HCV-antibodies6 | -- | 1,027 (70.6) | -- |
Abbreviations: NSEP, Needle and Syringe Exchange program; NHBS, National HIV Behavioral Surveillance; IDU, injection drug use; HIV, human immunodeficiency virus; HCV, hepatitis C virus
Restricted to male participants
NSEP survey asked if participants were “homeless or unstably housed,” while NHBS defined being homeless as “living on the street, in a shelter, in a Single Room Occupancy hotel (SRO), or in a car.”
Based on self-report
Restricted to participants reporting any opioid use in the past three months (91% of all NSEP clients, 96% of NHBS participants)
Based on serological confirmatory testing
Based on rapid antibody screening. This was implemented mid-way through the 2009 NHBS cycle, so only 271 (54%) participants were screened that year; in 2012 and 2015, 99% and 97% of participants were screened, respectively.
Based on a t-test for continuous variables and a chi-square test for categorical variables.
3.2. Temporal Trends in Methamphetamine Injection
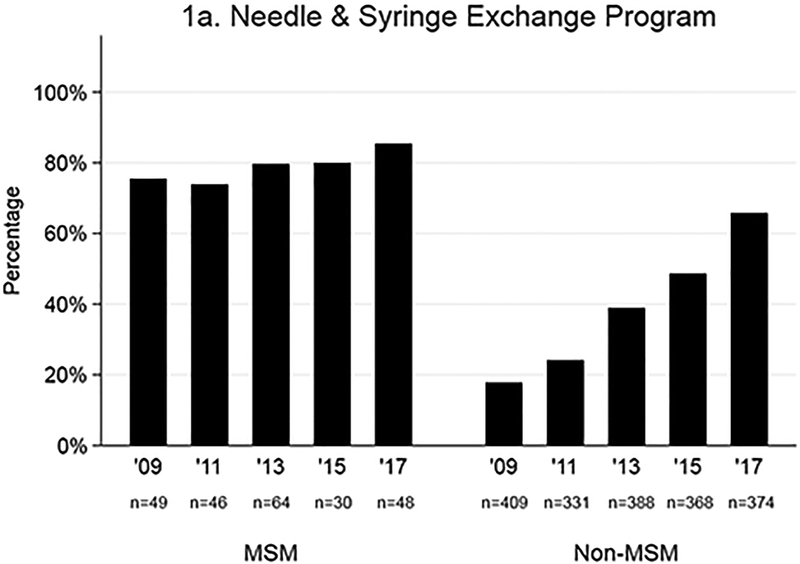
As shown in Figure 1, the proportion of NSEP clients reporting any recent methamphetamine injection increased significantly among non-MSM in both the NSEP survey (2009–2017) and the NHBS-IDU survey (2009–2015). In the NSEP survey, the proportion of non-MSM PWID reporting any methamphetamine injection increased from a low of 18% in 2009 to a high of 66% in 2017 (P < 0.01). The trend among NHBS-IDU non-MSM participants was nearly identical with a low of 23% in 2009 to a high of 62% in 2015 (P < 0.01). Methamphetamine injection was always higher among MSM than among non-MSM with 85% of MSM reporting this in the most recent (2017) NSEP survey and 88% of MSM reporting this in the most recent (2015) NHBS-IDU survey. However, there was no evidence of a statistically significant increase in methamphetamine injection among PWID who were MSM since 2009 in either survey.
Fig. 1.
Temporal trends in any methamphetamine injection (a) in the past 3 months among Public Health – Seattle and King County Needle and Syringe Exchange Program (NSEP) clients, 2009–2017, and (b) in the past year among Seattle-area National HIV Behavioral Surveillance Injection Drug Use Cycle (NHBS-IDU) participants, 2009–2015
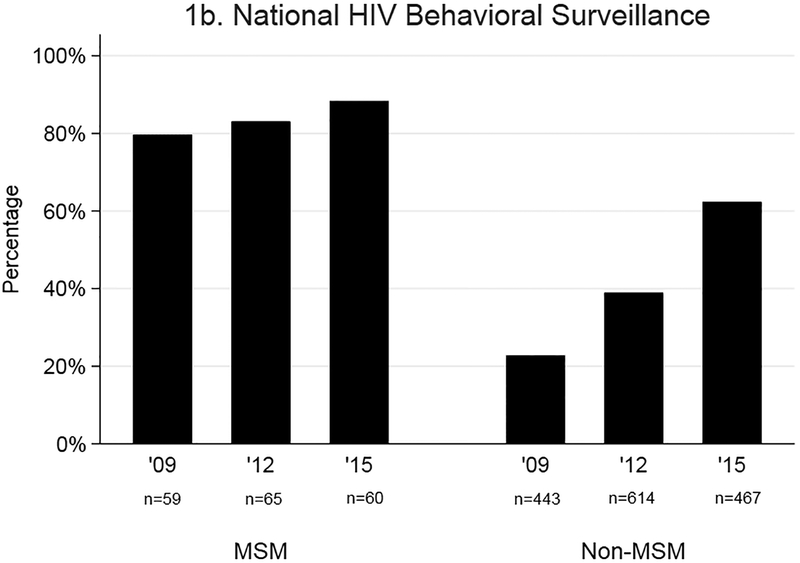
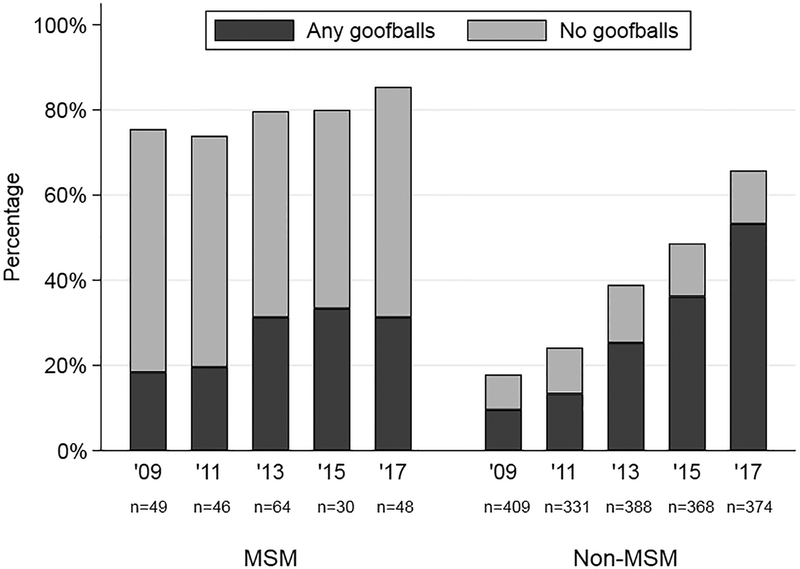
Using data available in the NSEP surveys only, we explored temporal trends in methamphetamine injected alone or in goofballs. As shown in Figure 2, the proportion of MSM reporting any goofballs in the past three months increased from 18% to 31% between 2009 and 2017 (P = 0.04). Increased reporting of goofballs accounted for nearly all of the linear increase in methamphetamine injection among non-MSM during the same time period. There was a nearly five-fold increase in the proportion of non-MSM reporting any goofball injection: 10% in 2009 to 53% in 2017 (P < 0.01). Among non-MSM, the proportion reporting injecting methamphetamine alone remained relatively constant over time between 8–14%.
Fig. 2.
Temporal trends in injecting methamphetamine with heroin (goofballs) in the past 3 months among Public Health – Seattle and King County Needle and Syringe Exchange Program (NSEP) clients, 2009–2017
3.3. Characteristics of Goofball Injectors
We compared characteristics between non-MSM NSEP clients who reported injecting any goofballs to those who reported injecting other drugs (Table 2). Non-MSM who injected goofballs were more likely to be younger than people who injected other drugs (prevalence ratio [PR]=0.7 per 10 years, 95% CI: 0.7–0.8). PWID who reported goofball injection were also more likely to be homeless or unstably housed (PR=2.2, 95% CI: 1.9–2.7) and report injecting daily (PR=1.7, 95% CI: 1.4–2.1). Among PWID reporting any opioid use, goofball injection was association with self-reported opioid overdose in the past year (PR=1.7, 95% CI: 1.5–1.9). In a multivariable model that also adjusted for survey year, all variables remained significantly associated with goofball injection (data not shown).
Table 2.
Characteristics of Public Health – Seattle and King County Needle and Syringe Exchange Program (NSEP) non-MSM clients who reported injecting methamphetamine with heroin (goofballs) compared to those who reported injecting other drugs in the past three months, 2009–2017
| Characteristic | Injected Goofballs N=576 N (%) | Injected Other Drugs N=l,559 N (%) | Unadjusted Prevalence Ratio (95% CI) |
|---|---|---|---|
| Age, mean [SD] | 33.7 [9.4] | 39.2 [12.3] | 0.7 (0.7–0.8)3 |
| Gender | |||
| Female | 172 (29.9) | 497 (31.9) | Reference |
| Male | 404 (70.1) | 1,062 (68.1) | 1.1 (0.9–1.2) |
| White, non-Hispanic | 423 (74.0) | 1,102 (70.9) | 1.1 (0.95–1.3) |
| Homeless or unstably housed | 438 (76.2) | 810 (52.3) | 2.2 (1.9–2.7) |
| Injects drugs daily | 449 (78.2) | 970 (63.6) | 1.7 (1.4–2.1) |
| Opioid overdose, past year1,2 | 166 (28.9) | 201 (15.2) | 1.7 (1.5–1.9) |
Abbreviations: SD, standard deviation
Based on self-report
Restricted to participants reporting any opioid use in the past three months (91% of all clients)
Prevalence ratio is for 10 year increments
3.4. Injection Equipment Sharing among People Who Inject Methamphetamine
Sharing injection equipment was common among both NSEP and NHBS-IDU participants with the majority of participants in both surveys reported sharing any injection equipment (Table 3). Reported sharing was more common among NHBS-IDU participants as compared to NSEP clients: 69% vs. 53% for any injection equipment and 39% vs. 27% for sharing syringes, respectively (P < 0.01 for both). MSM consistently reported lower levels of injection equipment sharing than non-MSM. In the NSEP survey, sharing any injection equipment was reported by 36% of MSM, as compared with 58% of non-MSM men and 57% of women. In NHBS, these estimates were 51%, 71%, and 77%, respectively. Sharing syringes specifically was reported by 18% of MSM, 27% of non-MSM men, and 34% of women in the NSEP survey. These estimates were slightly higher in NHBS: 25%, 39%, and 47%.
Table 3.
Injection equipment sharing in the past 3 months among Public Health – Seattle and King County Needle and Syringe Exchange Program (NSEP) clients, 2009–2017, and in the past year among Seattle-area National HIV Behavioral Surveillance Inject Drug Use Cycle (NHBS-IDU) participants, 2009–2015
| Characteristic | NSEP Clients 2009–2017 N=916 % (n/N) | NHBS-IDU Participaints 2009–2015 N=785 % (n/N) | p-value1 |
|---|---|---|---|
| Any injection equipment sharing | 53.1% (485/913) | 69.3% (543/784) | <0.01 |
| Men who had sex with men | 35.5% (66/186) | 51.0% (78/153) | |
| Non-MSM men | 57.9% (272/470) | 71.4% (274/384) | |
| Women | 57.2% (147/257) | 77.3% (191/247) | |
| Any syringe sharing | 27.2% (249/914) | 39.1% (307/785) | <0.01 |
| Men who had sex with men | 17.7% (33/186) | 25.3% (39/154) | |
| Non-MSM men | 27.2% (128/471) | 39.3% (151/384) | |
| Women | 34.2% (88/257) | 47.4% (117/247) |
Based on a chi-square test
Abbreviations: NSEP, Needle and Syringe Exchange program; NHBS, National HIV Behavioral Surveillance; MSM, men who have sex with men
Note: Row counts may not sum to column totals due to missing data.
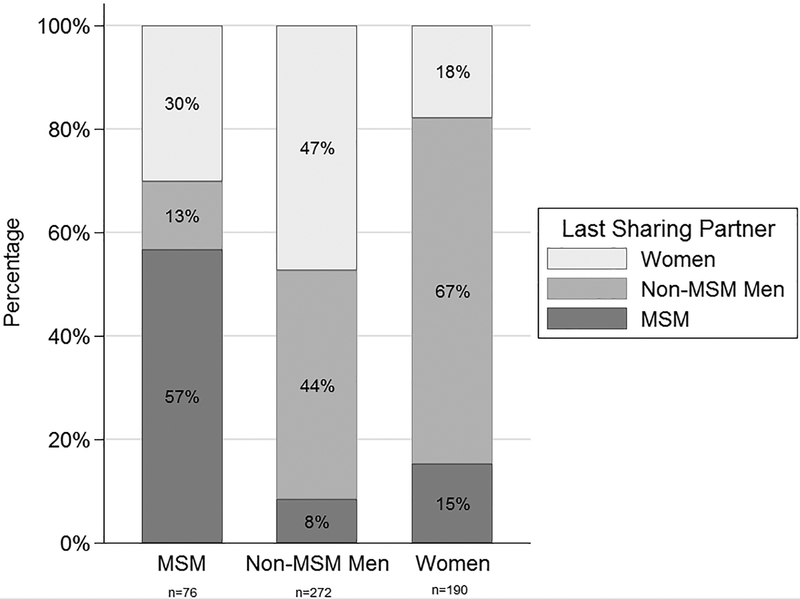
Among NHBS-IDU participants who reported both methamphetamine injection in the past year and sharing any injection equipment, we looked at the characteristics of a participant’s last equipment sharing partner (Figure 3). Among MSM, 43% had last shared any injection equipment with a non-MSM (30% women, 13% men). Eight percent of non-MSM men and 15% of women had last shared equipment with an MSM.
Fig. 3.
Characteristics of last injection equipment sharing partner among National HIV Behavioral Surveillance Injection Drug Use Cycle (NHBS-IDU) participants who injected methamphetamine in the past year and reported any equipment sharing, 2009–2015
4. DISCUSSION
In King County, Washington, non-MSM who inject methamphetamine may be an emerging population at risk for HIV infection. Our data present clear evidence of a dramatic increase in methamphetamine injection among PWID, with the most significant increase occurring among non-MSM. Based on data from our NSEP study population, most of this increase among non-MSM can be attributable to PWID injecting methamphetamine and heroin together (goofballs) and this is likely to be the case in the NHBS-IDU study population as well. Although King County has a well-established syringe exchange program, sharing injection equipment was relatively common, including sharing between MSM and non-MSM methamphetamine users. This pattern of sharing in an expanding population of PWID suggests that a new bridge for potential HIV transmission has formed in King County, one that has the potential to foster HIV transmission in a population of PWID who have traditionally been at very low risk for HIV infection.
There have been few published reports of increases in methamphetamine injection in the United States. In their analysis of Denver area NHBS-IDU data, Al-Tayyib and colleagues found that the proportion of PWID reporting that methamphetamine was their primary drug increase from 2% in 2005 to 30% in 2015 (Al-Tayyib et al., 2017). In 2015, nearly half of all Denver PWID reported using goofballs in the past 12 months. Similar to our findings in Seattle, these PWID were more likely to be younger, be currently homeless, report injecting at least daily, and report an overdose in the past year (Al-Tayyib et al., 2017). Reports of goofball use have also been sparse. In addition to goofball use reported in Denver (Al-Tayyib et al., 2017), cross-sectional data from San Diego (Meacham et al., 2016) and San Francisco (Ochoa et al., 2005) have also been published. Therefore, to date, these methamphetamine-related trends appear to be primarily a West Coast phenomenon. This is plausible given drug trafficking patterns in the United States (Center for Substance Absue Research, 2016; U.S. Department of Justic Drug Enforcement Administration, 2016). Similar to other regions of the West Coast, heroin in the Pacific Northwest tends to be “black tar” heroin, which is primarily produced in Mexico (Ciccarone, 2009). Methamphetamine production is also largely based in Mexico and drug trafficking patterns appear to be interconnected (Brouwer et al., 2006). Using heroin in combination with a stimulant is not novel, although traditionally its more common form has been with cocaine (speedballs). Indeed, speedball use declined at the same time as goofball use increased among PWID in King County, although not at the same levels of increased goofball injection (Kummer et al., 2016). Additional research is needed to further elucidate longitudinal drug use trajectories among goofball users to understand reasons for this polydrug use and identify targets for prevention interventions.
The increase in methamphetamine injection among non-MSM has occurred in the context of relatively high levels of reported injection equipment sharing, even among a sample of NSEP clients. Perhaps our most striking finding was non-trivial rates of equipment sharing between MSM and non-MSM who inject methamphetamine. Approximately 40% of MSM reporting sharing equipment with non-MSM, and 9–15% of non-MSM sharing equipment with MSM. Notably, to date in King County, we have not seen any evidence of an increase in HIV diagnoses among non-MSM PWID, with only 7 new cases of HIV identified in 2015 in this group based on local HIV surveillance data (Public Health - Seattle and King County HIV/AIDS Epidemiology Program and Washington State Department of Health Infectious Disease Assessment Unit, 2016). HIV viral suppression among PWID in King County is high at 76%, (Public Health - Seattle and King County HIV/AIDS Epidemiology Program and Washington State Department of Health Infectious Disease Assessment Unit, 2016) which substantially reduces the risk of HIV transmission.
Our local surveillance data are supported by previous analyses that found evidence of secular trends in HIV risk reduction among PWID in King County, including a reduction in sharing injection equipment and an increase in HIV testing among MSM who inject methamphetamine (Burt and Thiede, 2014), as well as a community-wide long-term reduction in syringe sharing (Burt and Thiede, 2016). Other jurisdictions with lower rates of HIV viral suppression among PWID and/or higher rates of syringe sharing should carefully monitor rates of methamphetamine use among both MSM and non-MSM in an effort to identify potential HIV transmission risk within and across populations. Our findings support the importance of conducting ongoing surveillance of injection-related behaviors among PWID.
4.1. Strengths and Limitations
The primary strength of this paper was the consistency in findings across two independent serial cross-sectional surveys of PWID in King County. Our study also has several limitations. First, because our estimate of injection equipment sharing between MSM and non-MSM was based on the last reported sharing encounter, we anticipate that this is almost certainly an underestimate of how common this behavior is. Second, we had only limited data and sample size to evaluate the characteristics of recent injection equipment sharing partners and were unable to assess partners’ HIV status, viral load among HIV-infected partners, and duration and frequency of equipment sharing. These data would provide more accurate estimates of the likelihood of HIV transmission risk across networks. Third, the estimates of self-reported overdose are subject to survival bias. These findings would be underestimates if those at highest risk for overdose already had a fatal outcome. Fourth, because all measures used in this analysis were based on self-report, there is also the possibility of social desirability bias, especially in the context of a survey conducted at a NSEP. Finally, there was some variability in survey measures both within and across surveys which somewhat limits comparability across surveys.
5. CONCLUSIONS
These findings highlight the profound importance of maintaining and expanding evidence-based HIV prevention efforts among PWID. King County has housed one of the longest-running and most robust NSEPs in the United States, and is likely one of the reasons that HIV prevalence has remained low among local PWID. Maintaining, if not increasing, these services is critical for preventing HIV transmission. Routine HIV testing, keeping HIV-infected PWID virally suppressed, and efforts to diminish injection drug use are also essential components of HIV prevention efforts in this population. MSM who use methamphetamine remain a priority population for HIV pre-exposure prophylaxis (PrEP), yet PrEP use and adherence in this population can be challenging (Storholm et al., 2017). Data from the present study suggest that non-MSM who inject methamphetamine may also benefit from PrEP. Substance use disorder and mental health treatment may also lead to reduced drug use, HIV risk behaviors, and improved health outcomes (National Institute on Drug Abuse, 2013).
Footnotes
Portions of these data were presented at the 24th Conference on Retroviruses and Opportunistic Infections, Seattle WA. February 15–16, 2017.
REFERENCES
- Al-Tayyib A, Koester S, Langegger S, Raville L, 2017. Heroin and methamphetamine injection: an emerging drug use pattern. Subst. Use Misuse 52, 1051–1058. doi: 10.1080/10826084.2016.1271432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, Palmateer N, Doyle JS, Hellard ME, Hutchinson SJ, 2014. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int. J. Epidemiol 43, 235–248. doi: 10.1093/ije/dyt243 [DOI] [PubMed] [Google Scholar]
- Banta-Green C, Kingston S, Ohta J, Taylor M, Sylla L, Tinsley J, Smith R, Couper F, Harruff R, Freng S, Von Derau K, 2016. 2015 Drug Use Trends in King County, Washington. URL: http://adai.uw.edu/pubs/pdf/2015drugusetrends.pdf. Accessed October 3, 2017 [Google Scholar]
- Brouwer KC, Case P, Ramos R, Magis-Rodríguez C, Bucardo J, Patterson TL, Strathdee SA, 2006. Trends in production, trafficking, and consumption of methamphetamine and cocaine in Mexico. Subst. Use Misuse 41, 707–27. doi: 10.1080/10826080500411478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchacz K, McFarland W, Kellogg TA, Loeb L, Holmberg SD, Dilley J, Klausner JD, 2005. Amphetamine use is associated with increased HIV incidence among men who have sex with men in San Francisco. AIDS 19, 1423–1424. doi:00002030-200509020-00011 [DOI] [PubMed] [Google Scholar]
- Burt RD, Thiede H, 2016. Reduction in needle sharing among Seattle-area injection drug users across 4 surveys, 1994–2013. Am. J. Public Health 106, 301–307. doi: 10.2105/AJPH.2015.302959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt RD, Thiede H, 2014. Evidence for risk reduction among amphetamine-injecting men who have sex with men; results from national HIV behavioral surveillance surveys in the Seattle area 2008–2012. AIDS Behav. 18, 1998–2008. doi: 10.1007/s10461-014-0769-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt RD, Thiede H, 2012. Evaluating consistency in repeat surveys of injection drug users recruited by respondent-driven sampling in the Seattle Area: results from the NHBS-IDU1 and NHBS-IDU2 surveys. Ann. Epidemiol 22, 354–363. doi: 10.1016/j.annepidem.2012.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt RD, Tinsley J, Glick SN, 2017. A decline in HIV testing among persons who inject drugs in the Seattle area, 2004–2015. J Acquir Immune Defic Syndr 75, S346–S351. doi: 10.1097/QAI.0000000000001409 [DOI] [PubMed] [Google Scholar]
- Cedarbaum ER, Banta-Green CJ, 2016. Health behaviors of young adult heroin injectors in the Seattle area. Drug Alcohol Depend. 158, 102–109. doi: 10.1016/j.drugalcdep.2015.11.011 [DOI] [PubMed] [Google Scholar]
- Center for Substance Absue Research, 2016. National Drug Early Warning System Sentinel Community Site Advance Report 2016: Selected Findings for Heroin, Fentanyl, and Methamphetamine. URL: https://ndews.umd.edu/sites/ndews.umd.edu/files/u1424/2016_ndews_scs_advance_report_final.pdf. Accessed October 3, 2017. [Google Scholar]
- Centers for Disease Control and Prevention;Viral Hepatitis, Sexual Transmitted Diseases and Tuberculosis Prevention, Division of HIV/AIDS Prevention, National Center for HIV/AIDS, 2017. HIV Surveillance among Persons Who Inject Drugs (slide set). URL: https://www.cdc.gov/hiv/pdf/library/slidesets/cdc-hiv-surveillance-persons-who-inject-drugs-2015.pdf. Accessed October 3, 2017. [Google Scholar]
- Centers for Disease Control and Prevention;Viral Hepatitis, Sexual Transmitted Diseases and Tuberculosis Prevention, Division of HIV/AIDS Prevention, N.C. for H., 2017. HIV Surveillance - Men Who Have Sex with Men (MSM) through 2015 (slide set). URL: https://www.cdc.gov/hiv/pdf/library/slidesets/cdc-hiv-surveillance-slides-msm.pdf. Accessed October 3, 2017. [Google Scholar]
- Ciccarone D, 2009. Heroin in brown, black and white: structural factors and medical consequences in the US heroin market. Int. J. Drug Policy 20, 277–282. doi: 10.1016/j.drugpo.2008.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbairn N, Kerr T, Milloy MJ, Zhang R, Montaner J, Wood E, 2011. Crystal methamphetamine injection predicts slower HIV RNA suppression among injection drug users. Addict. Behav 36, 762–763. doi: 10.1016/j.addbeh.2011.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman MB, Thomas JA, Alexy ER, Irvine MK, 2015. Crystal methamphetamine use and HIV medical outcomes among HIV-infected men who have sex with men accessing support services in New York. Drug Alcohol Depend 147, 266–271. doi: 10.1016/j.drugalcdep.2014.09.780 [DOI] [PubMed] [Google Scholar]
- Glick S, Burt R, Moreno C, Ketchum J, Thiede H, 2016. Highlights from the 2015 Seattle area National HIV Behavioral Surveillance survey of injection drug use. HIV/AIDS Epidemiology Unit, Public Healh – Seattle & King County and the Infectious Disease Assessment Unit, Washington State Department of Health HIV/AIDS Epidemiology Report. 85, 51–58. URL: http://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/patients/epidemiology/annual-reports.aspx. Accessed October 3, 2017 [Google Scholar]
- Glick S, Burt R, Shiver C, Moreno C, Thiede H, 2015. Highlights from the 2014 Seattle area National HIV Behavioral Surveillance survey of men who have sex with men. HIV/AIDS Epidemiology Unit, Public Health – Seattle & King County and the Infectious Disease Assessment Unit, Washington State Department of Health HIV/AIDS Epidemiology Report. 84, 55–68. URL: http://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/patients/epidemiology/annual-reports.aspx. Accessed October 3, 2017 [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, 2009. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform 42, 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins LM, Banta-Green CJ, Maynard C, Kingston S, Hanrahan M, Merrill JO, Coffin PO, 2011. Risk factors for nonfatal overdose at seattle-area syringe exchanges. J. Urban Heal. 88, 118–128. doi: 10.1007/s11524-010-9525-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kummer K, Thiede H, Hanrahan M, 2016. Needle exchange client surveys 2011, 2013, and 2015: drugs used, risk and protective behaviors, overdose, health insurance coverage, and health concerns. HIV/AIDS Epidemiology Unit, Public Health – Seattle & King County and the Infectious Disease Assessment Unit, Washington State Department of Health HIV/AIDS Epidemiology Report. 85, 39–48. URL: http://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/patients/epidemiology/annual-reports.aspx. Accessed October 3, 2017 [Google Scholar]
- Meacham MC, Strathdee SA, Rangel G, Armenta RF, Gaines TL, Garfein RS, 2016. Prevalence and correlates of heroin-methamphetamine co-injection among persons who inject drugs in San Diego, California, and Tijuana, Baja California, Mexico. J. Stud. Alcohol Drugs 77, 774–81. doi: 10.15288/jsad.2016.77.774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montaner JS, Lima VD, Barrios R, Yip B, Wood E, Kerr T, Shannon K, Harrigan PR, Hogg RS, Daly P, Kendall P, 2010. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet (London, England) 376, 532–539. doi: 10.1016/S0140-6736(10)60936-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse, 2013. Methamphetamine. URL: https://www.drugabuse.gov/publications/drugfacts/methamphetamine. Accessed October 3, 2017. [Google Scholar]
- Ochoa KC, Davidson PJ, Evans JL, Hahn JA, Page-Shafer K, Moss AR, 2005. Heroin overdose among young injection drug users in San Francisco. Drug Alcohol Depend. 80, 297–302. doi: 10.1016/j.drugalcdep.2005.04.012 [DOI] [PubMed] [Google Scholar]
- Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO, 2012. “Hooked on” prescription-type opiates prior to using heroin: results from a survey of syringe exchange clients. J. Psychoactive Drugs 44, 259–265. doi: 10.1080/02791072.2012.704591 [DOI] [PubMed] [Google Scholar]
- Peters PJ, Pontones P, Hoover KW, Patel MR, Galang RR, Shields J, Blosser SJ, Spiller MW, Combs B, Switzer WM, Conrad C, Gentry J, Khudyakov Y, Waterhouse D, Owen SM, Chapman E, Roseberry JC, McCants V, Weidle PJ, Broz D, Samandari T, Mermin J, Walthall J, Brooks JT, Duwve JM, Team IHIVOI, 2016. HIV infection linked to injection use of Oxymorphone in Indiana, 2014–2015. N. Engl. J. Med 375, 229–239. doi: 10.1056/NEJMoa1515195 [DOI] [PubMed] [Google Scholar]
- Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, Jacobson LP, 2007. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr 45, 85–92. doi: 10.1097/QAI.0b013e3180417c99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Public - Seattle and King County HIV/AIDS Epidemiology Program, Washington State Department of Health Infectious Disease Assessment Unit, 2016. HIV/AIDS Epidemiology Report. URL: http://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/patients/epidemiology/annual-reports.aspx. Accessed October 3, 2017 [Google Scholar]
- Storholm ED, Volk JE, Marcus JL, Silverberg MJ, Satre DD, 2017. Risk perception, sexual behaviors, and PrEP adherence among substance-using men who have sex with men: a qualitative study. Prev. Sci 1–11. doi: 10.1007/s11121-017-0799-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiede H, Jenkins RA, Carey JW, Hutcheson R, Thomas KK, Stall RD, White E, Allen I, Mejia R, Golden MR, 2009. Determinants of recent HIV infection among Seattle-area men who have sex with men. Am J Public Heal. 99 Suppl 1, S157–64. doi: 10.2105/AJPH.2006.098582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Justic Drug Enforcement Administration, 2016. 2016 National Drug Threat Assessment Summary. URL: https://www.dea.gov/resource-center/2016NDTASummary.pdf. Accessed October 3, 2017. [Google Scholar]