Abstract
Background
Despite the existence of effective interventions and best‐practice guideline recommendations for childcare services to implement policies, practices and programmes to promote child healthy eating, physical activity and prevent unhealthy weight gain, many services fail to do so.
Objectives
The primary aim of the review was to examine the effectiveness of strategies aimed at improving the implementation of policies, practices or programmes by childcare services that promote child healthy eating, physical activity and/or obesity prevention. The secondary aims of the review were to:
1. describe the impact of such strategies on childcare service staff knowledge, skills or attitudes; 2. describe the cost or cost‐effectiveness of such strategies; 3. describe any adverse effects of such strategies on childcare services, service staff or children; 4. examine the effect of such strategies on child diet, physical activity or weight status.
Search methods
We searched the following electronic databases on 3 August 2015: the Cochrane Central Register of Controlled trials (CENTRAL), MEDLINE, MEDLINE In Process, EMBASE, PsycINFO, ERIC, CINAHL and SCOPUS. We also searched reference lists of included trials, handsearched two international implementation science journals and searched the World Health Organization International Clinical Trials Registry Platform (www.who.int/ictrp/) and ClinicalTrials.gov (www.clinicaltrials.gov).
Selection criteria
We included any study (randomised or non‐randomised) with a parallel control group that compared any strategy to improve the implementation of a healthy eating, physical activity or obesity prevention policy, practice or programme by staff of centre‐based childcare services to no intervention, 'usual' practice or an alternative strategy.
Data collection and analysis
The review authors independently screened abstracts and titles, extracted trial data and assessed risk of bias in pairs; we resolved discrepancies via consensus. Heterogeneity across studies precluded pooling of data and undertaking quantitative assessment via meta‐analysis. However, we narratively synthesised the trial findings by describing the effect size of the primary outcome measure for policy or practice implementation (or the median of such measures where a single primary outcome was not stated).
Main results
We identified 10 trials as eligible and included them in the review. The trials sought to improve the implementation of policies and practices targeting healthy eating (two trials), physical activity (two trials) or both healthy eating and physical activity (six trials). Collectively the implementation strategies tested in the 10 trials included educational materials, educational meetings, audit and feedback, opinion leaders, small incentives or grants, educational outreach visits or academic detailing. A total of 1053 childcare services participated across all trials. Of the 10 trials, eight examined implementation strategies versus a usual practice control and two compared alternative implementation strategies. There was considerable study heterogeneity. We judged all studies as having high risk of bias for at least one domain.
It is uncertain whether the strategies tested improved the implementation of policies, practices or programmes that promote child healthy eating, physical activity and/or obesity prevention. No intervention improved the implementation of all policies and practices targeted by the implementation strategies relative to a comparison group. Of the eight trials that compared an implementation strategy to usual practice or a no intervention control, however, seven reported improvements in the implementation of at least one of the targeted policies or practices relative to control. For these trials the effect on the primary implementation outcome was as follows: among the three trials that reported score‐based measures of implementation the scores ranged from 1 to 5.1; across four trials reporting the proportion of staff or services implementing a specific policy or practice this ranged from 0% to 9.5%; and in three trials reporting the time (per day or week) staff or services spent implementing a policy or practice this ranged from 4.3 minutes to 7.7 minutes. The review findings also indicate that is it uncertain whether such interventions improve childcare service staff knowledge or attitudes (two trials), child physical activity (two trials), child weight status (two trials) or child diet (one trial). None of the included trials reported on the cost or cost‐effectiveness of the intervention. One trial assessed the adverse effects of a physical activity intervention and found no difference in rates of child injury between groups. For all review outcomes, we rated the quality of the evidence as very low. The primary limitation of the review was the lack of conventional terminology in implementation science, which may have resulted in potentially relevant studies failing to be identified based on the search terms used in this review.
Authors' conclusions
Current research provides weak and inconsistent evidence of the effectiveness of such strategies in improving the implementation of policies and practices, childcare service staff knowledge or attitudes, or child diet, physical activity or weight status. Further research in the field is required.
Keywords: Child; Humans; Health Knowledge, Attitudes, Practice; Motor Activity; Program Development; Child Care; Child Care/methods; Child Care/organization & administration; Child Day Care Centers; Diet; Diet/standards; Eating; Guidelines as Topic; Health Promotion; Health Promotion/methods; Health Promotion/organization & administration; Obesity; Obesity/prevention & control; Randomized Controlled Trials as Topic
Improving the implementation of healthy eating, physical activity and/or obesity prevention policies, practices or programmes in childcare services
The review question This review aimed to look at the effects of strategies to improve the implementation (or correct undertaking) of policies, practices or programmes by childcare services that promote children's healthy eating, physical activity and/or obesity prevention. We also looked at whether these strategies improved childcare service staff knowledge, skills or attitudes. We also wanted to determine the cost or cost‐effectiveness of providing implementation support, whether support strategies were associated with any adverse effects and whether there was an impact on child nutrition, physical activity or weight status. Background A number of childcare service‐based interventions have been found to be effective in improving child diet, increasing child physical activity and preventing excessive weight gain. Despite the existence of such evidence and best‐practice guideline recommendations for childcare services to implement these policies and practices, many childcare services fail to do so. Without proper implementation, children will not benefit from these child health‐directed policies and practices. Study characteristics The review identified 10 trials, eight of which examined implementation strategies versus usual practice, and two that compared different types of implementation strategies. The trials sought to improve the implementation of policies and practices targeting healthy eating (two trials), physical activity (two trials) or both healthy eating and physical activity (six trials). Collectively the implementation strategies tested in the 10 trials included educational materials, educational meetings, audit and feedback, opinion leaders, small incentives or grants, educational outreach visits or academic detailing. The strategies tested were only a small number of those that could be applied to improve implementation in this setting. Search date The evidence is current to August 2015. Key results None of the strategies identified in the review improved implementation of all the targeted policies or practices. However, most strategies reported improvement for at least one policy or practice. The findings provide weak and inconsistent evidence of the effects of these strategies on improving the implementation of policies, practices and programmes, childcare service staff knowledge or attitudes, or child diet, physical activity or weight status. The lack of consistent terminology in this area of research may have meant some relevant studies were not picked up in our search. Nonetheless, the few identified trials suggest that research to implement such policies and practices in childcare services is only in the early stages of development. Quality of the evidence We rated the evidence for all outcomes as very low quality and thus we cannot be overly confident in the findings.
Summary of findings
Summary of findings for the main comparison.
| Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services | |||
|
Patient or population: children up to the age of 6 years Settings: centre‐based childcare services that cater for children prior to compulsory schooling Intervention: any strategy (including educational materials, educational meetings, audit and feedback, opinion leaders, small incentives or grants, educational outreach visits or academic detailing) with the primary intent of improving the implementation (by usual service staff) of policies, practices or programmes in centre‐based childcare services to promote healthy eating, physical activity or prevent unhealthy weight gain Comparison: no intervention (8 studies) or alternate intervention (2 studies) | |||
| Outcomes | Impact | No of participants (studies) | Quality of the evidence (GRADE) |
| Implementation of policies, practices or programmes that promote child healthy eating, physical activity and/or obesity prevention | We are uncertain whether strategies improve the implementation of policies, practices or programmes that promote child healthy eating, physical activity and/or obesity prevention | 1053 participants (childcare services), 10 studies | ⊕⊝⊝⊝ very lowa |
| Childcare service staff knowledge, skills or attitudes related to the implementation of policies, practices or programmes that promote child healthy eating, physical activity | We are uncertain whether strategies to improve the implementation of policies, practices or programmes that promote child healthy eating, physical activity and/or obesity prevention improve childcare service staff knowledge, skills or attitudes | 457 participants (childcare service staff), 2 studies | ⊕⊝⊝⊝ very lowa |
| Cost or cost‐effectiveness of strategies to improve the implementation of policies, practices or programmes in childcare services | No studies were found that looked at the cost or cost‐effectiveness of strategies to improve the implementation of policies, practices or programmes in childcare services | Nil | N/A |
| Adverse consequences of strategies to improve the implementation of policies, practices or programmes in childcare services | We are uncertain whether strategies to improve the implementation of policies, practices or programmes that promote child healthy eating, physical activity and/or obesity prevention impact on adverse consequences | 20 participants (childcare services), 1 study | ⊕⊝⊝⊝ very lowb |
| Measures of child diet, physical activity or weight status | We are uncertain whether strategies to improve the implementation of policies, practices or programmes that promote child healthy eating, physical activity and/or obesity prevention improve child diet, physical activity or weight status | 2829 participants (children), 3 studies | ⊕⊝⊝⊝ very lowa |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
aTriple downgraded due to limitations in the design, imprecision of evidence and unexplained heterogeneity. bTriple downgraded due to indirectness, inconsistency and imprecision of evidence.
Background
Description of the condition
Internationally, the prevalence of being overweight and obesity has increased across every region of the world in recent decades (Finucane 2011). Currently over 1.5 billion adults and 170 million children are overweight or obese (Finucane 2011; Lobstein 2004). While obesity rates in high‐income countries remain higher, prevalence rates in low‐ and middle‐income countries are accelerating (Swinburn 2011). In Africa, for example, the prevalence of being overweight among children under five years is expected to increase from 4% in 1990 to 11% by 2025 (Black 2013). Excessive weight gain increases the risk of a variety of chronic health conditions. Between the years 2010 and 2030, up to 8.5 million cases of diabetes, 7.3 million cases of heart disease and stroke, and 669,000 cases of cancer attributable to obesity have been projected in the USA and UK alone (Wang 2011). In Australia, between the years 2011 and 2050, 1.75 million lives and over 10 million premature years of life will be lost due to excessive weight gain (Gray 2009).
Description of the intervention
Physical inactivity and poor diet are key drivers of excessive weight gain. As excessive weight gain in childhood tracks into adulthood, interventions targeting children's diet and physical activity have been recommended to mitigate the adverse health effects of obesity on the population (World Health Organization 2012). A recently published World Health Organization report into population‐based approaches to childhood obesity prevention identified centre‐based childcare services (including preschools, long daycare services and kindergartens that provide educational and developmental activities for children prior to formal compulsory schooling) as an important setting for public health action to reduce the risk of unhealthy weight gain in childhood. Such settings provide an opportunity to access large numbers of children for prolonged periods of time (World Health Organization 2012). Further, randomised and quasi‐experimental trials have identified a number of interventions, delivered in childcare services, which have increased child physical activity and fundamental movement skill proficiency, improved child diet quality and prevented excessive weight gain (Adams 2009; De Silva‐Sanigorski 2010; Hardy 2010; Trost 2008). As such, regulations and best practice guidelines for the childcare sector recommend implementation of a number of healthy eating and physical activity policies and practices, such as restricting sedentary screen time opportunities; ensuring meals provided by childcare services or foods packed by parents for consumption in care are consistent with dietary guidelines; and the provision of programmes to promote physical activity and fundamental movement skill development (Commonwealth of Australia; McWilliams 2009; Tremblay 2012).
Despite the existence of evidenced‐based best‐practice guidelines for childcare services, implementation of obesity prevention policies and practices that are consistent with such guidelines is poor (McWilliams 2009; Story 2006). In the USA, research suggests that 75% of meat consumed in childcare is fried or high in fat, and that children consume less than 13% of dietary guideline recommendations for whole grains and 7% for dark vegetables (Ball 2008). Childcare service adherence to dietary guidelines in other countries has also been reported to be poor (Yoong 2014). Similarly, adherence to best‐practice recommendations for physical activity is also suboptimal. For example, only 14% of USA childcare services provided 120 minutes of active play per day, 57% to 60% did not have a written physical activity policy (McWilliams 2009; Sisson 2012), and in 18% of childcare services, children were seated for more than 30 minutes at a time (McWilliams 2009). In Australia, it has been reported that just 48% to 50% of centre‐based childcare services had a written physical activity policy, 46% to 60% had programmed time each day for fundamental movement skill development (Wolfenden 2010), and 60% of child lunch boxes contained more than one serving of high‐fat, salt or sugar foods or drinks (Kelly 2010).
Without adequate implementation across the population of childcare services, the potential public health benefits of initiatives to improve child diet or physical activity, or prevent obesity, will not be fully realised. 'Implementation' is described as the use of strategies to adopt and integrate evidence‐based health interventions and to change practice patterns within specific settings (Glasgow 2012). Implementation research, specifically, is the study of strategies designed to integrate health policies, practices or programmes within specific settings (for example, primary care, community centres or childcare services) (Schillinger 2010). The National Institutes of Health recognises implementation research as a fundamental component of the third stage of the research translation process ('T3') and that it is a necessary pre‐requisite for research to yield public health improvements (Glasgow 2012). While staff of centre‐based childcare services are responsible for providing educational experiences and an environment supportive of healthy growth and development, including initiatives designed to reduce the risk of excessive weight gain, it may be the childcare services themselves, government or other agencies (such as for licensing and accreditation requirements) that undertake strategies aimed at enhancing the implementation of such initiatives.
There are a range of potential strategies that can improve the likelihood of implementation of healthy eating, physical activity and obesity prevention policies and practices in childcare services. The Cochrane Effective Practice and Organisation of Care (EPOC) taxonomy is a framework for characterising educational, behavioural, financial, regulatory and organisational interventions (EPOC 2015); it includes three categories with 22 subcategories within the topic of 'implementation strategies'. Examples of such subcategories include continuous quality improvement, educational materials, performance monitoring, local consensus processes and educational outreach visits (EPOC 2015).
How the intervention might work
The determinants of policy and practice implementation are complex and the mechanisms by which support strategies facilitate implementation are not well understood. Implementation frameworks have identified a large number of factors operating at multiple macro and micro levels that can influence the success of implementation (Damschroder 2009). However, few studies have been conducted in the childcare setting to identify key determinants of implementation in this setting. A study by Wolfenden and colleagues of over 200 childcare services in Australia examined associations between the existence of healthy eating and physical activity policies and practices and 13 factors suggested by Damschroder's Consolidated Framework for Implementation Research to impede or promote implementation (Wolfenden 2015a). The study reported that implementation policy and practice implementation was more likely when service managers, management committee and parents were supportive, and where external resources to support implementation were accessible. Applied implementation frameworks, such as the Theoretical Domains Framework (Michie 2008), suggest that strategies to facilitate implementation may be most likely to be effective with a thorough understanding of implementation context and barriers, and when theoretical frameworks are applied to select implementation support strategies to address key determinants of implementation. For example, knowledge barriers to implementation may be best overcome with education meetings or materials, while activity reminders, such as decision support systems, may be particularly important in instances where staff forgetfulness is identified as a local implementation barrier.
Why it is important to do this review
A number of large systematic reviews have been undertaken to assess the effectiveness of such implementation strategies in improving the professional practice of clinicians. For example Ivers and colleagues reviewed the effectiveness of audit and feedback on the behaviour of health professionals and the health of their patients and found it generally resulted in small but important improvements in professional practice (Ivers 2012). Giguère and colleagues reviewed the effectiveness of printed education materials on the practice of healthcare professionals and patient health outcomes and found a small beneficial effect on professional practice outcomes (Giguère 2012). Additional systematic reviews have assessed the effectiveness of additional implementation strategies including reminders (Arditi 2012), education meetings and workshops (Forsetlund 2009; O'Brien 2007), and incentives (Scott 2011). Despite the existence of such reviews, implementation research in non‐clinical community settings remains limited (Buller 2010). While several implementation strategies have been used to improve the implementation of healthy eating, physical activity and obesity prevention policies and practices in childcare services (Finch 2012; Ward 2008), a systematic synthesis of the effects reported in such trials has not been undertaken in this setting.
To our knowledge, just one systematic review of implementation interventions in non‐clinical settings (for example, schools) has been published to date (Rabin 2010). The review, which was an update of an earlier Agency for Healthcare Research and Quality report (Agency for Healthcare Research and Quality 2003), investigated the effectiveness of strategies in any community setting to implement policies or practices to reduce behavioural risks for cancer, including healthy eating, physical activity, smoking and sun protection. The review included studies published between 1980 and 2008 and did not identify any implementation trials targeting healthy eating or physical activity in childcare services. An up‐to‐date, comprehensive review of such literature is therefore warranted.
Objectives
The primary aim of the review was to examine the effectiveness of strategies aimed at improving the implementation of policies, practices or programmes by childcare services that promote child healthy eating, physical activity and/or obesity prevention.
The secondary aims of the review were to:
describe the impact of such strategies on childcare service staff knowledge, skills or attitudes;
describe the cost or cost‐effectiveness of such strategies;
describe any adverse effects of such strategies on childcare services, service staff or children;
examine the effect of such strategies on child diet, physical activity or weight status.
Methods
Criteria for considering studies for this review
Types of studies
Any study (randomised, including cluster‐randomised, or non‐randomised trials) with a parallel control group that compared:
a strategy to improve the implementation of any healthy eating, physical activity or obesity prevention policy, practice or programme in centre‐based childcare services compared with no intervention or 'usual' practice;
two or more alternative strategies to improve the implementation of any healthy eating, physical activity or obesity prevention policy, practice or programme in centre‐based childcare services.
We excluded studies that did not include implementation of policy, practices or programmes as a specific aim (primary or secondary), as well as studies that did not report baseline measures of the primary outcome. There was no restriction on the length of the study follow‐up period, language of publication or country of origin.
Types of participants
Centre‐based childcare services such as preschools, nurseries, long daycare services and kindergartens that cater for children prior to compulsory schooling (typically up to the age of five to six years). We excluded studies of childcare services provided in the home.
Types of interventions
Any strategy with the primary intent of improving the implementation of policies, practices or programmes in centre‐based childcare services to promote healthy eating, physical activity or prevent unhealthy weight gain was eligible. To be eligible strategies must have sought to improve the implementation of policies, practices or programmes by usual childcare service staff. Strategies could have included quality improvement initiatives, education and training, performance feedback, prompts and reminders, implementation resources, financial incentives, penalties, communication and social marketing strategies, professional networking, the use of opinion leaders or implementation consensus processes. Interventions may have been singular or multi‐component.
Types of outcome measures
Primary outcomes
We included any measure of either the completeness or the quality of the implementation of childcare service policies, practices or programmes (for example, the percentage of childcare services implementing a food service consistent with dietary guidelines or the mean number of physical activity practices implemented). To assess the review outcomes, data may have been collected from a variety of sources including teachers, managers, cooks or other staff of centre‐based childcare services; or administrators, officials or other health, education, government or non‐government personnel responsible for encouraging or enforcing the implementation of health‐promoting initiatives in childcare services. Such data may have been obtained from audits of service records, questionnaires or surveys of staff, service managers, other personnel or parents; direct observation or recordings; examination of routine information collected from government departments (such as compliance with food standards or breaches of childcare service regulations) or other sources. Additionally, children, parents or childcare service staff may have provided information regarding child diet, physical activity or child weight status.
Secondary outcomes
Any measure of childcare service staff knowledge, skills or attitudes related to the implementation of policies, practices or programmes that promote child healthy eating, physical activity and/or obesity prevention.
Estimates of absolute costs or any assessment of the cost‐effectiveness of strategies to improve the implementation of policies, practices or programmes in childcare services.
Any reported adverse consequences of a strategy to improve the implementation of policies, practices or programmes in childcare services. This could include impacts on child health (for example, an increase in child injury following the implementation of physical activity‐promoting practices) or development, service operation or staff attitudes (for example, impacts on staff motivation or cohesion) or the displacement of other key programmes, curricula or practices.
Any measure of child diet, physical activity (including sedentary behaviours) or weight status. Such measures could be derived from any data source including direct observation, questionnaire, or anthropometric or biochemical assessments. We excluded studies focusing on malnutrition/malnourishment.
Search methods for identification of studies
We conducted searches for peer‐reviewed articles in electronic databases. We also undertook handsearching of relevant journals and the reference lists of included trials.
Electronic searches
We searched the following electronic databases: the Cochrane Central Register of Controlled trials (CENTRAL) (2015, Issue 7), MEDLINE (1950 to 2015), MEDLINE In Process (up to 2015), EMBASE (1947 to 2015), PsycINFO (1950 to 2015), ERIC (up to 2015), CINAHL (up to 2015) and SCOPUS (up to 2015).
We adapted the MEDLINE search strategy for the other databases and we included filters used in other systematic reviews for population (childcare services) (Zoritch 2000), physical activity (Dobbins 2013), healthy eating (Jaime 2009), and obesity (Waters 2011). A search filter for intervention type (implementation interventions) was based on previous reviews (Rabin 2010), and a glossary of terms in implementation and dissemination research (Rabin 2008). See Appendix 1 for the detailed search strategy.
An experienced librarian (DB) searched the electronic databases.
Searching other resources
We searched the reference lists of all included trials for citation of other potentially relevant trials. We conducted handsearches of all publications for the past five years in the journal Implementation Science and the Journal of Translational Behavioural Medicine as they are the leading implementation journals in the field. We also performed handsearches of the reference lists of included trials. Furthermore, we conducted searches of the World Health Organization International Clinical Trials Registry Platform (www.who.int/ictrp/) and ClinicalTrials.gov (www.clinicaltrials.gov). We included studies identified in such searches, which have not yet been published, in the 'Characteristics of ongoing studies' table. We also made contact with the authors of included trials, experts in the field of implementation science and key organisations to identify any relevant ongoing or unpublished trials or grey literature publications.
Data collection and analysis
Selection of studies
Two review authors (from pool of six authors: JJ, LW, CMW, AJW, KS and SLY) independently screened abstracts and titles. Review authors were not blind to the author or journal information. We conducted the screening of studies using a standardised screening tool developed based on the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), which we piloted before use. We obtained the full texts of manuscripts for all potentially eligible trials for further examination. For all manuscripts, we recorded information regarding the primary reason for exclusion and documented this in the 'Characteristics of excluded studies' table. We included the remaining eligible trials in the review. We resolved discrepancies between review authors regarding study eligibility by consensus. In instances where the study eligibility could not be resolved via consensus, a third review author made a decision.
Data extraction and management
Two review authors (from pool of five authors: JJ, MF, RW, FT, TS), unblinded to author or journal information, independently extracted information from the included trials. We recorded the information extracted from the included trials in a data extraction form that we developed based on the recommendations of the Cochrane Public Health Group Guide for Developing a Cochrane Protocol (Cochrane Public Health Group 2011). We piloted the data extraction form before the initiation of the review. We resolved discrepancies between review authors regarding data extraction by consensus and, where required, via a third review author.
We extracted the following information:
Study eligibility as well as the study design, date of publication, childcare service type, country, participant/service demographic/socioeconomic characteristics and number of experimental conditions, as well as information to allow assessment of study risk of bias.
Characteristics of the implementation strategy, including the duration, number of contacts and approaches to implementation, the theoretical underpinning of the strategy (if noted in the study), information to allow classification against the EPOC taxonomy, and to enable an assessment of the overall quality of evidence using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach, as well as data describing consistency of the execution of the intervention with a planned delivery protocol.
Trial primary and secondary outcomes, including the data collection method, validity of measures used, effect size and measures of outcome variability.
Source(s) of research funding and potential conflicts of interest.
Assessment of risk of bias in included studies
Overall risk of bias
Two review authors (MK and FT) assessed risk of bias independently using the 'Risk of bias' tool described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We provided an overall risk of bias ('high', 'low' or 'unclear') for each included study based on consideration of study methodological characteristics (sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and 'other' potential sources of bias). Where required, a third review author adjudicated discrepancies regarding the risk of bias that could not be resolved via consensus. We included an additional criterion 'potential confounding' for the assessment of the risk of bias in non‐randomised trial designs (Higgins 2011). We also included additional criteria for cluster‐randomised controlled trials including 'recruitment to cluster', 'baseline imbalance', 'loss of clusters', 'incorrect analysis' and 'compatibility with individually randomised controlled trials' (Higgins 2011). We documented the risk of bias of the included studies in 'Risk of bias' tables.
Measures of treatment effect
Differences in measures and the primary and secondary outcomes reported in the included studies precluded the use of summary statistics to describe treatment effects. As such, the methods and outcomes of the included trials are comprehensively described in narrative form according to broad implementation strategy characteristics.
Unit of analysis issues
Clustered studies
We examined clustered trials for unit of analysis errors. We identified trials with unit of analysis errors in the 'Risk of bias' tables.
Dealing with missing data
We contacted the authors of included trials to provide additional information if any outcome data were unclear or missing. All information we received was included in the results of the review. We noted any instances of potential selective or incomplete reporting of outcome data in the 'Risk of bias' tables.
Assessment of heterogeneity
We were unable to perform an assessment of heterogeneity due to considerable variability in terms of study interventions, outcomes, measures and comparators. Therefore we were unable to explore heterogeneity via box plots, forest plots and/or the I2statistic (Higgins 2011). Instead the potential implications of trial heterogeneity are outlined in the Discussion.
Assessment of reporting biases
The comprehensive search strategy for this review helped to reduce the risk of reporting bias. We also conducted comparisons between published reports and trial protocols, and trial registers where such reports were available. Instances of potential reporting bias are documented in the 'Risk of bias' tables.
Data synthesis
We narratively synthesised trial findings according to the implementation strategies employed and the outcome measures reported. We used the EPOC taxonomy to classify implementation strategies (EPOC 2015). As the trial heterogeneity precluded meta‐analysis we described the effects of interventions by reporting the absolute effect size of the primary outcome measure for policy or practice implementation for each study. We calculated the effect size by subtracting the change from baseline on the primary implementation outcome for the control or comparison group from the change from baseline in the experimental or intervention group. If data to enable calculation of the change from baseline were unavailable, we used the differences between groups post‐intervention. Where there were two or more primary implementation outcome measures, we used the median effect size of the primary outcomes. Where the primary outcome measure was not explicitly identified by the study authors in the published manuscripts we used the implementation outcome on which the trial sample size calculation was based or, in its absence, we took the median effect size of all measures of policy or practice outcomes reported in the manuscript. Such an approach was previously used in the Cochrane Review of the effects of audit and feedback on professional practices published by the Cochrane EPOC Group (Ivers 2012). In instances where a number of subscales of an overall implementation score were reported in addition to a total scale score, we used the total score as the primary outcome to provide a more comprehensive measure of implementation. We reverse scored implementation measures that did not represent an improvement (for example, the proportion of services without a nutrition policy). We present the effects of interventions according to the implementation strategies (classified using the EPOC taxonomy) employed by included studies and, within such grouping, based on the outcome data (continuous or dichotomous) reported.
We included a 'Summary of findings' table to present the key findings of the review (Table 1). We generated the table based on the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions and the EPOC Group and included i) a list of all primary and secondary outcomes in the review, ii) a description of intervention effect, iii) the number of participants and studies addressing each outcome, and iv) a grade for the overall quality of the body of evidence for each outcome. In particular, the table provides key information concerning the quality of evidence, the magnitude of effect of the interventions examined and the sum of available data on the main outcomes.
Two review authors (LW and JJ) rated the overall quality of evidence for each outcome using the GRADE system (Guyatt 2010), with any disagreements resolved via consensus or, where required, by a third review author. The GRADE system defines the quality of the body of evidence for each review outcome regarding the extent to which one can be confident in the review findings. The GRADE system required an assessment of methodological quality, directness of evidence, heterogeneity, precision of effect estimates and risk of publication bias. We used the GRADE quality ratings (from 'very low' to 'high') to describe the quality of the body of evidence for each review outcome and we included these in 'Table 1'.
Subgroup analysis and investigation of heterogeneity
Data were insufficient to conduct subgroup analysis or enable quantitative exploration of heterogeneity. Nonetheless clinical and methodological heterogeneity of included studies is described narratively. To describe the impact of implementation strategies delivered 'at scale' (defined as involving 50 or more childcare services) we performed subgroup analyses narratively for the primary implementation outcomes. Specifically we performed subgroup analyses where included studies sought to improve implementation of policies, practices or programmes across 50 or more services.
Sensitivity analysis
We did not perform sensitivity analysis by removing studies with a high risk of bias or by removing outliers contributing to statistical heterogeneity as marked heterogeneity precluded pooled analysis.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies
Results of the search
The electronic search, conducted on 3 August 2015, yielded 6188 citations (Figure 1). We identified an additional 1102 records from handsearching key journals and checking reference lists of included trials. We identified no additional records through our contact with the authors of included trials, experts in the field of implementation science and key organisations. Following screening of titles and abstracts, we obtained the full texts of 134 manuscripts for further review, of which we included 17 manuscripts describing 10 individual trials. We contacted the authors of five included trials to provide additional information where any outcome data were unclear or missing. All authors responded and the information we received was included in the results of the review. We identified four studies as ongoing studies that have not yet been published through searches of clinical trial registration databases.
Figure 1.
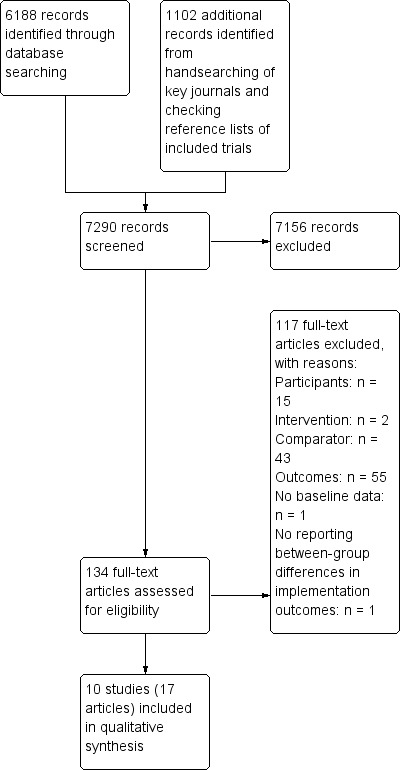
Study flow diagram.
Included studies
Types of studies
The trials were predominantly conducted in the USA (n = 5) (Alkon 2014; Benjamin 2007; Gosliner 2010; Ward 2008; Williams 2002), and Australia (n = 4) (Bell 2014; Finch 2012; Finch 2014; Hardy 2010), but also included a study from Ireland (n = 1) (Johnston Molloy 2013). Studies were conducted between 1995 and 2012, although two studies did not report the years of data collection (Benjamin 2007; Gosliner 2010). There was considerable heterogeneity in the participants, interventions and outcomes (clinical heterogeneity), and the study design characteristics (methodological) of included studies.
Participants
Of the 10 included trials, seven recruited childcare services located in disadvantaged areas or specifically serving disadvantaged low‐income or minority children (Alkon 2014; Bell 2014; Finch 2012; Finch 2014; Gosliner 2010; Johnston Molloy 2013; Williams 2002). The socio‐economic characteristics of the service locality or the children attending was not described in the remaining three trials. There was considerable variability in the number of participating childcare services in the included studies. The largest trial recruited 583 preschools (Bell 2014). However, most trials recruited 20 or fewer childcare services (Alkon 2014; Benjamin 2007; Finch 2014; Gosliner 2010; Williams 2002), with the smallest trial recruiting just nine services. Three trials sought to improve implementation of policies, practices or programmes in 50 or more services (Bell 2014; Finch 2012; Ward 2008). Six of the 10 included trials were conducted by two research groups in the USA and Australia and all were conducted in high‐income countries (Alkon 2014; Bell 2014; Benjamin 2007; Finch 2012; Finch 2014; Ward 2008).
Interventions
Two trials targeted the implementation of healthy eating policies or practices only (Bell 2014; Williams 2002), two targeted the implementation of physical activity policies and practices only (Finch 2012; Finch 2014), and six targeted both healthy eating and physical activity policies and practices (Alkon 2014; Benjamin 2007; Gosliner 2010; Hardy 2010; Johnston Molloy 2013; Ward 2008). All trials used multiple implementation strategies. The strategies tested examined only a small number of those described in the EPOC taxonomy that could be applied to improve implementation in the setting. The definitions of each of the EPOC subcategories used to classify implementation strategies employed by studies included in the review are provided in Table 2. Using the EPOC taxonomy descriptors, all trials included educational meetings and educational materials (Alkon 2014; Bell 2014; Benjamin 2007; Finch 2012; Finch 2014; Gosliner 2010; Hardy 2010; Johnston Molloy 2013; Ward 2008; Williams 2002). One trial utilised these strategies with the addition of audit and feedback (Johnston Molloy 2013). Three trials combined educational meetings and educational materials with educational outreach visits or academic detailing (Alkon 2014; Benjamin 2007; Ward 2008), and three trials utilised these strategies with the addition of small incentives of financial grants not otherwise specified (Gosliner 2010; Hardy 2010; Williams 2002). Two studies tested an intervention consisting of educational meetings and educational materials with audit and feedback, the use of opinion leaders and small incentives (Bell 2014; Finch 2012), and one study tested the impact of an implementation strategy comprising educational meetings and educational materials, academic detailing, audit and feedback, opinion leaders and small incentives (Finch 2014). Four studies reported that strategies to support implementation were theoretically based (Bell 2014; Benjamin 2007; Finch 2014; Ward 2008), and the theories adopted included components of social cognitive theory against a social‐ecologic framework (Benjamin 2007; Ward 2008), practice change and capacity building theoretical frameworks (Bell 2014), and social‐ecological models of health behaviour change (Finch 2014).
Table 1.
Definition of EPOC subcategories utilised in the review
| EPOC subcategory | Definition |
| Educational materials | Distribution to individuals, or groups, of educational materials to support clinical care, i.e. any intervention in which knowledge is distributed. For example, this may be facilitated by the internet, learning critical appraisal skills; skills for electronic retrieval of information, diagnostic formulation; question formulation |
| Educational meetings | Courses, workshops, conferences or other educational meetings |
| Educational outreach visits or academic detailing | Personal visits by a trained person to health workers in their own settings, to provide information with the aim of changing practice |
| Small incentives or grants | Transfer of money or material goods to healthcare providers conditional on taking a measurable action or achieving a predetermined performance target, for example incentives for lay health workers |
| Audit and feedback | A summary of health workers’ performance over a specified period of time, given to them in a written, electronic or verbal format; the summary may include recommendations for clinical action |
| Opinion leaders | The identification and use of identifiable local opinion leaders to promote good clinical practice |
Outcomes
Implementation was primarily assessed using telephone interview, surveys/questionnaires completed by childcare service staff or audits of service documents conducted by researchers (Bell 2014; Benjamin 2007; Finch 2012; Gosliner 2010; Hardy 2010; Williams 2002), or by direct observation (Alkon 2014; Finch 2014; Johnston Molloy 2013; Ward 2008). The validity of four of the five trials utilising a survey/questionnaire to assess implementation was not reported (Bell 2014; Finch 2012; Gosliner 2010; Hardy 2010). In one trial outcome assessments were conducted immediately post‐intervention, and one and four months post‐intervention (Benjamin 2007), while the remaining studies included follow‐up ranging from up to five to six months (Hardy 2010), 22 months (Bell 2014), or four years after initiation of the intervention (Johnston Molloy 2013). Three trials reported outcomes of both implementation and a measure of child healthy eating, physical activity or weight status (Alkon 2014; Finch 2014; Williams 2002), two trials included measures of childcare service staff knowledge, skills or attitudes (Finch 2012; Hardy 2010), one trial included a measure of potential adverse effects (Finch 2014), and none reported costs or cost‐effectiveness analyses.
Study design characteristics
Seven of the included studies were randomised trials (or cluster‐randomised trials) (Alkon 2014; Benjamin 2007; Finch 2014; Gosliner 2010; Hardy 2010; Johnston Molloy 2013; Ward 2008), and three were non‐randomised trials with a parallel control group (Bell 2014; Finch 2012; Williams 2002).
Eight trials compared an implementation strategy to usual practice or a no intervention control (Alkon 2014; Bell 2014; Benjamin 2007; Finch 2012; Finch 2014; Hardy 2010; Ward 2008; Williams 2002). Two trials directly compared two different implementation strategies (Gosliner 2010; Johnston Molloy 2013). Four studies utilised a convenience sample of childcare services (JAlkon 2014; Benjamin 2007; Johnston Molloy 2013; Ward 2008). Four trials attempted to recruit all eligible services in the study region (Bell 2014; Finch 2012; Hardy 2010), or randomly approached services within a study region to participate (Finch 2014), the service level participation rate of such studies ranging from 48% (Hardy 2010) to 91% (Bell 2014). The sampling procedures of two trials were unclear (Gosliner 2010; Williams 2002).
We judged implementation to be the primary outcome in seven trials (Alkon 2014; Bell 2014; Benjamin 2007; Finch 2012; Gosliner 2010; Johnston Molloy 2013; Ward 2008), and a secondary outcome in the remaining three trials (Finch 2014; Hardy 2010; Williams 2002), based on the stated aims of the trial. A variety of outcome measures were employed by the included studies. Seven trials included continuous measures of implementation outcomes including policy or environment scores (Alkon 2014; Benjamin 2007; Johnston Molloy 2013; Ward 2008), minutes of policy or programme implementation (Finch 2012; Finch 2014; Hardy 2010), frequency of policy or programme implementation (Finch 2014; Hardy 2010), or quantity of food or beverages or macronutrients provided to children (Bell 2014; Williams 2002). Six trials reported a dichotomous measure of implementation, including the percentage of staff or childcare services that implemented a policy, practice or programme (Alkon 2014; Bell 2014; Finch 2012; Finch 2014; Gosliner 2010; Hardy 2010). Assessment of implementation included observation of childcare environments (Alkon 2014; Finch 2014; Johnston Molloy 2013; Ward 2008), audits of menus (Bell 2014; Williams 2002), or telephone interviews or surveys/questionnaires completed by staff of childcare services (Bell 2014; Benjamin 2007; Finch 2012; Gosliner 2010; Hardy 2010) (see Table 3).
Table 2.
Summary of intervention, measures and absolute intervention effect size in included studies
| Study | Implementation strategies | Comparison group | Primary implementation outcome measures | Effect sizea |
| Alkon 2014 | Educational materials, educational meetings and audit and feedback | Usual practice |
Score: nutrition and physical activity policy quality using the CHPHSPC and nutrition and physical activity practices using the EPAO assessed via observation (5 measures) % of staff or services implementing a practice: foods offered to children assessed using the DOCC tool assessed via observation (10 measures) |
Median (range)d: 1.4 (0 to 4.29) Median (range): 0% (0% to 25%)c |
| Bell 2014 | Educational materials, educational meetings, audit and feedback, opinion leaders, and small incentives or grants | Usual practice |
% of staff or services implementing a practice: percentage of services implementing nutrition policies and practices and menus consistent with nutrition recommendations (10 measures) Quantity of food served (servings/items): mean number of items or servings of healthy/unhealthy foods on service menus (4 measures) |
Median (range): 9.5% (2% to 36%) Median (range): 0.5 serves/items (‐0.4 to 0.8) |
| Benjamin 2007 | Educational materials, educational meetings, and audit and feedback | Usual practice | Score: nutrition, physical activity environments assessed via questionnaire (NAPSACC) completed by service managers (total score) | Mean difference (95% CI)d: 5.10 (‐2.80 to 13.00) |
| Finch 2012 | Educational materials, educational meetings, audit and feedback, opinion leaders and small incentives | Usual practice |
% of staff or services implementing a practice: percentage of services implementing physical activity policies and practices (11 measures) Minutes of service or staff implementation of a policy of practice: time (hours/day) spent on structured physical activities (1 measure) |
Median (range): 2.5% (‐4% to 41%) Mean: 6 minutes |
| Finch 2014 | Educational materials, educational meetings, audit and feedback, opinion leaders and small incentives | Usual practice |
Frequency of staff or service implementation of a practice: occasions of implementation of fundamental movement skill activities, staff role modelling and verbal prompts and positive comments (4 measures) Minutes of service or staff implementation of a policy of practice (per session or day): minutes of fundamental movement skill activities, structured time, television viewing or seated time (4 measures) % of staff or services implementing a practice: services with seated time > 30 minutes or with an activity policy (2 measures) Mean number of resources or equipment per service: (3 measures) |
Median (range): 2.6 (12.1 to 0.6) Median (range)d: 4.3 minutes (‐12 minutes to 39 minutes) Median (range): 5 (30 to ‐20) Median (range): ‐01 (‐0.6 to ‐0.1) |
| Gosliner 2010 | Educational materials, educational meetings, educational outreach visits or academic detailing with small incentives or grants with staff wellness programme | Educational materials, educational meetings, educational outreach visits or academic detailing | % of staff or services implementing a practice: Provision of food items by staff 'more often' assessed via staff completed questionnaire (8 measures) | Median (range): 17% (0% to 23%) |
| Hardy 2010 | Educational materials, educational meetings, educational outreach visits or academic detailing with small incentives or grants | Usual practice |
Minutes of service or staff implementation of a policy of practice: Minutes (per week or session) of structured and unstructured play or fundamental movement skills activities (3 measures) Frequency of staff or service implementation of a practice: Frequency (per week or day) of structured or unstructured play, and of fundamental movement skill activities (3 measures) % of staff or services implementing a practice: conduct of food based activities, development of new rules around food and drink bought from home, and the provision of health information to families (3 measures) |
Median (range): 7.7 minutes (6.5 minutes to 10.1 minutes) Median (range): 0.2 (‐0.9 to 1.9) Median (range)d: 11% (‐7% to 31%) |
| Johnston Molloy 2013 | Educational materials, manager and staff educational meetings and audit and feedback | Educational materials, manager educational meetings, and audit and feedback | Score: On the Health Promotion Evaluation Activity Scored Evaluation form assessed via observation (total score) | Difference in median score: ‐2b |
| Ward 2008 | Educational materials, educational meetings, and audit and feedback | Usual practice | Score: nutrition and physical activity practices using the EPAO assessed via observation (total score) | Mean difference (95% CI)d: 1.01 (0.18 to 1.84) |
| Williams 2002 | Educational materials, educational meetings, educational outreach visits or academic detailing with small incentives or grants | Usual practice | Quantity of food served (servings/grams): Primary outcome – grams of saturated fat assessed via menu audit (one measure) | Median (range): 17% (0% to 23%) |
aEffect size calculated first using the primary outcome (where a single primary outcome was reported); otherwise using a total score (when total and subscale scores were provided); otherwise using the median effect size across measures (where more than one outcome measure was reported and not specified as primary).
bMean not reported. Represents the difference in median score between manager and staff trained versus manager only trained group.
cEffect size of measures reported as non‐significant (but where data are not reported in manuscript) assumed to be '0'.
dAdditional data obtained from study authors where unclear or missing.
CHPHSPC: Californian Childcare Health Programme Health and Safety Checklist; DOCC: Diet Observation in Child Care; EPAO: Environment and Policy Assessment and Observation; NAPSACC: Nutrition and Physical Activity Self‐Assessment for Child Care
Excluded studies
Following screening of titles and abstracts, we obtained the full texts of 134 manuscripts for further review for study eligibility (Figure 1). Of these, we considered 115 studies ineligible following the trial screening process (reasons for exclusion included: participants n = 15; intervention n = 2; comparator n = 43; outcomes n = 55). We excluded a study based on 'inappropriate outcomes' if it did not report implementation outcomes, if it did not report implementation outcomes for both intervention and control groups and if it did not report between‐group differences in implementation outcomes. We excluded an additional study following the commencement of data extraction as it did not report between‐group differences in implementation outcomes (Korwanich 2008). A further two studies did not collect baseline data (De Silva‐Sanigorski 2012; Gosliner 2010). We retained one of these studies as it was a randomised trial and therefore the examination of post‐intervention differences between groups was considered to be valid (Gosliner 2010).
Risk of bias in included studies
See Characteristics of included studies. The level of risk of bias is presented separately for each study in Figure 2 and as a combined study assessment of risk of bias in Figure 3.
Figure 2.
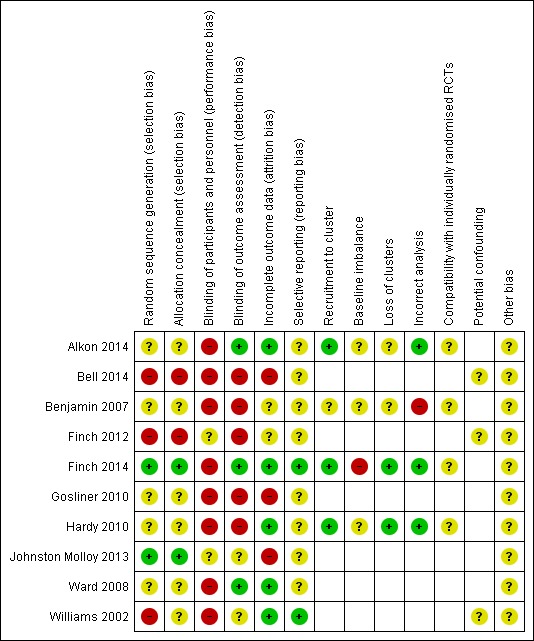
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Figure 3.
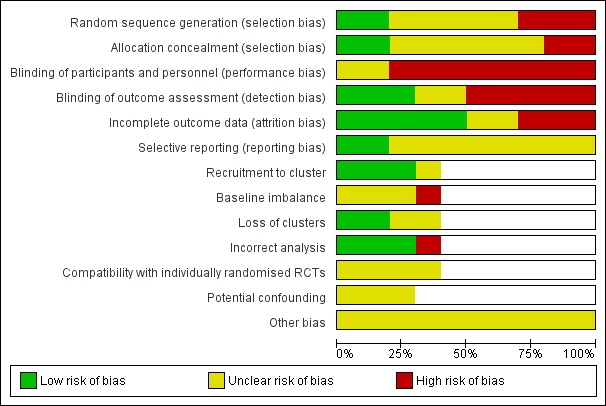
'Risk of bias graph': review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Risk of selection bias differed across studies. Only two of the studies were low risk as computerised random number functions and tables were used to generate random sequences and allocation was undertaken automatically in a single batch, preventing allocation from being pre‐empted (Finch 2014; Johnston Molloy 2013). For the three studies with quasi‐experimental, non‐randomised designs, the risk of selection bias was high (Bell 2014; Finch 2012; Williams 2002). For the remaining five studies, such bias was unclear as these studies did not report on random sequence generation or concealment of allocation.
Blinding
For the majority of studies (n = 8), the risk of performance bias was high due to participants and research personnel not being blind to group allocation. For the remaining two studies the risk of performance bias was unclear as in both studies the control group also received some form of intervention (Finch 2012; Johnston Molloy 2013). Detection bias differed across studies based on whether outcome measures were objective (e.g. body mass index (BMI)) (low risk) or self‐reported (high risk), and whether research personnel were blind to group allocation when conducting outcome assessment (low risk). For three studies, the risk of detection bias was low for all outcomes included in this review (Alkon 2014; Finch 2014; Ward 2008). For the remainder of the studies (n = 7), the risk of detection bias was high, low or unclear across one or more outcome measures.
Incomplete outcome data
For half the studies (n = 5), the risk of attrition bias was low as either all or most participating services were followed up and/or sensitivity analysis was conducted to assess the impact of missing data. For two studies the risk of such bias was high due to a large difference in the proportion of participating services lost to follow‐up between groups (Bell 2014; Johnston Molloy 2013). Risk of attrition bias was also high for the study conducted by Gosliner and colleagues (Gosliner 2010), as participants who did not complete the intervention were excluded from the analysis. For the remaining studies the risk of attrition bias was unclear as it was unclear whether incomplete outcome data had been addressed adequately.
Selective reporting
For the majority of the studies (n = 8) a published protocol paper or trial registration record was not identified and therefore it was unclear whether reporting bias had occurred. For the remaining two studies the risk of reporting bias was low as protocol papers were available and all a priori determined outcomes were reported (Finch 2014; Williams 2002).
Other potential sources of bias
For the four studies that were cluster‐randomised controlled trials, we assessed the potential risk of additional biases (Alkon 2014; Benjamin 2007; Finch 2014; Hardy 2010).
For the potential risk of recruitment (to cluster) bias, three of these studies were low risk as either a random, quasi‐random or census approach was used for recruitment (Alkon 2014; Finch 2014; Hardy 2010).
Regarding risk of bias due to baseline imbalances, three studies were at unclear risk (Alkon 2014; Benjamin 2007; Hardy 2010), while one study was at high risk due to baseline imbalances in service characteristics, with no mention of adjustments within the analysis (Finch 2014).
Two studies were low risk for loss of clusters as either all children were followed up or there was no loss of clusters (Finch 2014; Hardy 2010).
For incorrect analysis, three studies were low risk (Alkon 2014; Finch 2014; Hardy 2010), while the remaining study was high risk as no statistical analysis was undertaken due to the small sample size (Benjamin 2007).
All four cluster‐randomised controlled trials were at unclear risk for compatibility with individually randomised controlled trials as we were unable to determine whether a herd effect existed (Alkon 2014; Benjamin 2007; Finch 2014; Hardy 2010).
For the three studies with quasi‐experimental, non‐randomised designs (Bell 2014; Finch 2012; Williams 2002), we also considered the potential risk of bias due to confounding factors. For all three studies it was unclear whether confounders were adequately adjusted for.
Effects of interventions
See: Table 1
Most studies reported improvement in at least one of the policies or practices targeted by the implementation support strategy. Of the eight trials that compared an implementation strategy to usual practice or a no intervention control, seven reported statistically significant improvements in the implementation of at least one of the targeted policies or practices relative to control (Alkon 2014; Bell 2014; Finch 2012; Finch 2014; Hardy 2010; Ward 2008; Williams 2002). For trials comparing implementation strategies against a non‐intervention or usual practice control, the absolute effect of the primary implementation outcome was as follows: among the three trials that reported score‐based measures of implementation the scores ranged from 1 to 5.1 (Alkon 2014; Benjamin 2007; Ward 2008); across four trials reporting the proportion of staff or services implementing a specific policy or practice this ranged from 0% to 9.5% (Alkon 2014; Bell 2014; Finch 2012; Finch 2014; Hardy 2010); and in three trials reporting the time (per day or week) staff or services spent implementing a policy or practice this was 4.3 minutes to 7.7 minutes (Table 3). Two trials reported comparing two different implementation strategies: the first reported no significant improvement on any measure of implementation (Johnston Molloy 2013), while the second reported significant improvements in two of the eight implementation outcomes reported (Gosliner 2010).
The effects of interventions are presented according to the implementation strategies (classified using the Cochrane Effective Practice and Organisation of Care (EPOC) Group taxonomy) employed by included studies and, within such grouping, based on the outcome data (continuous or dichotomous) reported.
Primary outcome
1. Education materials, manager and staff educational meetings, and audit and feedback versus educational materials, manager educational meetings, and audit and feedback
Continuous outcomes
Johnston Molloy and colleagues conducted a randomised, parallel‐group trial testing two training‐based interventions to improve implementation of nutrition and health‐related activity practices in Irish full daycare services (preschools) (Johnston Molloy 2013). Services were randomised to a 'manager and staff trained' group (n = 31) or a 'manager trained' only group (n = 30). Eighteen services in the 'manager and staff training' group and 24 in the 'manager trained' group provided follow‐up data and were included in the main analysis. There was no single primary implementation outcome reported in the trial, however the total Preschool Health Promotion Activity Scored Evaluation score did not differ significantly between groups (absolute difference in median scores between 'manager and staff trained' versus 'manager trained' only group = ‐2), with median total scores improving from 15 to 34 in the 'manager and staff trained group' and 13 to 34 in the 'manager trained' only group (P = 0.84). Similarly, there were no significant between‐group differences on any of the four subscale measures of nutrition environment, food service, meals or snacks.
2. Educational materials, educational meetings and educational outreach visits or academic detailing versus usual practice control
Continuous outcomes
Three trials assessed the impact of implementation strategies using self‐assessment or observational assessment scores of the childcare environment, or childcare policies and practices (Alkon 2014; Benjamin 2007; Ward 2008). All trials assessed the effects of implementation strategies consisting of educational materials, education meetings and educational outreach visits or academic detailing (Alkon 2014; Benjamin 2007; Ward 2008). The absolute effect size for the primary implementation outcome (based on a total scale score where provided, or the median absolute effect size where multiple implementation outcomes are reported) ranged from 1 for the implementation strategies tested by Ward and colleagues and assessed via researcher observation of childcare environment (Ward 2008), to a 5.09 point improvement in Nutrition and Physical Activity Self‐Assessment for Child Care (NAPSACC) self‐assessment score among services receiving implementation support in a trial by Benjamin and colleagues (Benjamin 2007).
All three studies, Alkon 2014, Benjamin 2007 and Ward 2008, assessed the effectiveness of implementation of the NAPSACC programme (Ammerman 2007). The first was a randomised pilot study to assess the feasibility, acceptability and impact of the programme, which targeted implementation of 15 key service nutrition and physical activity policies and practices (Benjamin 2007). A convenience sample of eight counties in North Carolina, USA were randomised to an intervention group or control (six intervention counties and two control). Between two and five childcare services were approached per county and 15 services in the intervention and four in the control region participated. Implementation support was delivered by childcare health consultants (typically registered nurses) who were provided a NAPSACC tool kit and resources. Changes in policy and practice implementation were re‐assessed using the NAPSACC self‐assessment survey completed by service managers immediately following the six‐month intervention. At follow‐up, two intervention services had withdrawn and one had closed. The trial found no significant change in the NAPSACC self‐assessment survey score completed by service managers in the intervention relative to the control group between baseline and immediately post‐intervention (mean difference (MD) 5.10, 95% confidence interval (CI) ‐2.80 to 13.00, P = 0.21) (Benjamin 2007).
The second evaluation of the NAPSACC programme utilised a randomised controlled trial design (Ward 2008). A convenience sample of 30 childcare health consultants in North Carolina were randomised to an intervention (n = 20) or delayed intervention control group (n = 10). A convenience sample of 84 licensed childcare services associated with participating health consultants were then recruited. The primary trial outcome (change in nutrition and physical activity environment score) data were collected at baseline and immediately following the six‐month intervention using the Environment and Policy Assessment and Observation (EPAO) tool. There were significant improvements in total EPAO score among services receiving implementation support (MD 1.01, 95% CI 0.18 to 1.84, P = 0.02). There were no significant differences between groups at follow‐up for either the nutrition (MD 0.90, 95% CI 0.19 to 1.61, P = 0.06) or physical activity (MD 1.15, 95% CI ‐0.21 to 2.51, P = 0.19) environment subscales.
In the third study, Alkon and colleagues reported the findings of a randomised controlled trial of the NAPSACC programme conducted in 17 childcare services serving predominantly low‐income families (Alkon 2014). Nutrition and physical activity policies were evaluated by a research assistant using the California Childcare Health Program Health and Safety Policy Checklist (CCHPHSPC), while a modified version of the EPAO tool was completed by a research assistant to assess nutrition and physical activity practices during a one‐day observation. The trial found a significant increase in the mean policy scores, reflecting improvements in quantity and quality of nutrition and physical activity policies among intervention services at follow‐up. The mean nutrition policy score increased from 0.89 at baseline to 5.17 at follow‐up, with no change (0.0) in the mean score within the control group. The mean physical activity policy score increased from 0 at baseline to 2.82 at follow‐up, with no change in the mean score within the control group (0.0). There were no significant differences in unadjusted nutrition (MD 0.07, 95% CI ‐0.16 to 0.30, P = 0.55) or physical activity (MD 0.00, 95% CI ‐0.29 to 0.29, P = 1.00) EPAO scores between groups at follow‐up. Total EPAO score was not reported.
Dichotomous outcomes
The trial by Alkon and colleagues also assessed the impact of such an implementation strategy on the types and portions of all foods and beverages served to children in care. Assessments were conducted by direct observations conducted by researchers using the Diet Observation in Child Care (DOCC) tool, a validated instrument (Alkon 2014). At follow‐up there were no significant differences between groups on 10 measures of the types and portions of foods and beverages offered to children. Non‐significant improvements favouring intervention services were observed in the offering of: healthy foods (intervention +8%, control +1%); low‐ or non‐fat milk (intervention +10%, control +2%); and low‐fat meats and beans (intervention +17%, control ‐8%) (no other data reported).
3. Educational materials, educational meetings, educational outreach visits or academic detailing with small incentives or grants versus usual practice control
Continuous outcomes
Two trials assessed the effectiveness of implementation strategies consisting of educational materials, educational meetings, educational outreach visits or academic detailing and incentives, and utilised continuous measures of implementation (Hardy 2010; Williams 2002). However, the measures used in each trial differed. Hardy and colleagues utilised a number of implementation measures including the duration (in minutes) (three measures) or frequency (three measures) of staff or service implementation of practices or programmes (Hardy 2010). Williams and colleagues reported changes in the macronutrients of foods served to children (Williams 2002). The primary outcome for the trial conducted by Williams was the fat content of childcare meals. The effect size of the primary implementation outcome for both trials can be seen in Table 3.
Hardy and colleagues conducted a cluster‐randomised controlled trial to evaluate the 'Munch and Move' programme in one state of Australia (New South Wales) (Hardy 2010). All 61 government services (preschools) in the study region were invited to participate in the trial and 29 consented and were randomised. To assess policy and practice implementation, interviews with all service managers occurred at baseline and immediately following the five‐month intervention. The frequency of service provided in fundamental movement skill activities for children increased from 1.3 sessions per week to 3.2 sessions per week in the intervention group whilst remaining unchanged among control services, a difference that was statistically significant (difference at follow‐up of 1.5, 95% CI 0.01 to 2.9, P = 0.05). There were no significant differences between groups in the frequency of structured play sessions per week (adjusted difference 0.02, 95% CI ‐1.5 to 1.5), or unstructured play sessions per week (adjusted difference not reported). There were significant differences for the three measures assessing minutes per session of structured play (adjusted difference 0.09, 95% CI ‐11.6 to 11.8), unstructured play (adjusted difference 7.7, 95% CI ‐15.6 to 31.0) or fundamental movement skill sessions (adjusted difference 3.4, 95% CI ‐9.7 to 16.5). There were no significant differences between groups on any of the four measures of nutrition policy or practice implementation including food‐based activities, rules around food and food policies (effect sizes not reported).
Williams and colleagues conducted a quasi‐experimental trial of a preschool education and food service intervention conducted in Head Start Centers in upstate New York (Bollella 1999; D'Agostino 1999; Spark 1998; Williams 1998; Williams 2002; Williams 2004). The primary aim was to reduce the saturated fat content of service meals and to reduce consumption of saturated fat by children. Six services received either a food service intervention with nutrition classroom education curricula or an identical food service intervention with a classroom safety component. Both of these groups received implementation support to improve food service. Three other childcare services with food operations not amenable to modification served as a control and received safety education curricula. Implementation of menus with nutrient content consistent with guideline recommendations was assessed by obtaining menu recipes and food labels over a five‐day period. The trial found statistically significant within‐group reductions in grams of saturated fat of food listed on menus, the primary implementation outcome, reducing from 11.3 grams (standard deviation (SD) ± 1.9) to 7.6 grams (SD ± 1.7) at the 18‐month follow‐up. Significant within‐group changes were also identified for percentage of energy (kcal) from fat, reducing from 31.0 (SD ± 2.6) to 27.6 (SD ± 2.8) at six months (P < 0.05) and to 25.0 (SD ± 2.6) at 18 months (P < 0.01). Similarly, the percentage of energy (kcal) from saturated fat reduced from 12.5 (SD ± 1.4) to 10.3 (SD ± 1.4) at six months (not significant) and to 8.0 (SD ± 1.2) at the 18‐month follow‐up (P < 0.05) within the intervention group. There were no significant changes in these measures within the control group. Statistical comparisons between groups were not conducted. No other statistically significant changes were reported within either group for the 15 other nutrients measured at 18‐month follow‐up.
Dichotomous outcomes
Hardy and colleagues also reported trial outcomes using dichotomous measures (Hardy 2010). There were no significant differences between groups on any measures of nutrition policy or practice implementation including the conduct of food‐based activities, development of new rules around food and drinks bought from home, and the provision of health information to families, with the effect sizes relative to control ranging from ‐7% to 31% (P > 0.05).
4. Educational materials, educational meetings, educational outreach visits or academic detailing with small incentives or grants with staff wellness programme versus educational materials, educational meetings, educational outreach visits or academic detailing
Dichotomous outcomes
Gosliner and colleagues conducted a randomised trial with staff from childcare services in California, USA to assess the impact of an intervention on the nutrition and physical activity environment of childcare services (Gosliner 2010). Childcare services that were participating in a health education and policy development project (Child Health and Nutrition Center Enhancement) were matched on city of location and randomised to an intervention or control group. All services received multi‐strategic implementation support. In addition, staff of intervention services received a wellness programme consisting of individual health assessments (conducted by the research team); monthly newsletters and information with pay‐checks promoting healthy eating and nutrition; a group walking programme where staff received collective incentive rewards as they reached milestones; and staff follow‐up support visits. At 10‐month follow‐up there were significant improvements in two of the eight implementation measures. Specifically, staff at intervention services were significantly more likely to report providing fruit 'more often' to children in children's meals or snacks during the past year (74% of staff) compared to staff at control services (41% of staff) (P = 0.004). Similarly, staff at intervention services were significantly more likely to report providing vegetables 'more often' to children in children’s meals or snacks during the past year (64% of staff) compared to staff at control services (38% of staff) (P = 0.03). There were no significant differences between groups in the provision of sweetened beverages (intervention 7%, control 8%) and sweetened foods (intervention and control 5%) (P values not reported). At children’s celebrations during the past year, staff at intervention services were significantly more likely to report providing fresh fruit (39% of staff) compared to staff at control services (24% of staff) (P = 0.05). Further, intervention staff reported providing fewer sweetened beverages (7% of staff) compared to control (27% of staff) (P = 0.05) and fewer sweetened foods (intervention 15%, control 34%) (P = 0.025). There were no differences between groups in the provision of vegetables at children's celebrations (intervention 32%, control 24%) (P value not reported).
5. Educational materials, educational meetings, audit and feedback, opinion leaders and small incentives versus usual practice control
Two trials assessed the effectiveness of implementation strategies consisting of educational materials, educational meetings, audit and feedback, opinion leaders and small incentives (Bell 2014; Finch 2012). Bell and colleagues reported the impact of the implementation strategy on four continuous measures of the quantity (number of food items or food served) of food served to children (Bell 2014). The absolute effect size of the primary implementation outcome for this measure (calculated as the median effect across the four measures) was 0.5 serves/items (range 0.4 to 0.8). Finch and colleagues reported a single continuous measure assessing the impact of an implementation strategy on the time spent in structured physical activities (Finch 2012). Both trials also report dichotomous measures of the proportion of services implementing a policy or practice. The absolute effect size of the primary implementation outcome for these measures was 1% (range ‐4% to 41%) in the trial by Finch and colleagues (calculated as the median across 10 measures) and 9.5% (range 2% to 36%) in the trial by Bell and colleagues (calculated as the median across 10 measures).
Continuous outcomes
Finch and colleagues conducted a quasi‐experimental trial of a strategy to increase implementation of physical activity‐promoting policies and practices in centre‐based childcare services (Finch 2012). All services located within the Hunter New England geographic area of New South Wales, Australia (n = 338) were invited to participate in the intervention and received support to implement a number of policies and practices to promote child physical activity in care. A 10% sample of services in the rest of the state (n = 268) were randomly selected to serve as a comparison group. Services in the comparison region had the opportunity to receive government support to implement 'Munch and Move' (described above), a programme targeting similar policies and practices but utilising a less intensive series of implementation support (Hardy 2010). Implementation of physical activity practices was assessed at baseline and between eight and 12 months post‐intervention via a telephone interview administered to service managers. At follow‐up there was no significant difference between groups in time spent in structured physical activities (intervention +0.2 hours, control +0.1 hours, P = 0.65).
In Australia, Bell and colleagues conducted a quasi‐experimental trial to determine the impact of an implementation intervention to improve healthy eating policies and practices in centre‐based childcare services (Bell 2014). All services in one geographic region of the state of New South Wales, Australia (Hunter New England) were offered the intervention (n = 287) and provided implementation support. A random sample of 10% of childcare services located in all other regions of New South Wales were invited to participate in the evaluation and served as a control group (n = 296). The trial was conducted in the context of the 'Good for Kids. Good for Life' programme but occurred over a different period to the trial by Finch and colleagues (Finch 2012). Services allocated to the control group received usual care that may have included exposure to a government childcare programme to support healthy eating and physical activity offered to services. Baseline measures were collected between December 2006 and May 2007, while the follow‐up assessment occurred between March and August 2009. An audit of menus revealed that, relative to control services, intervention services were significantly more likely to have fewer high‐fat, salt or sugar processed meal items (intervention ‐0.9 items, control ‐0.2 items, P = 0.001), fewer sweetened drinks (intervention ‐0.4 items, control ‐0.1 items, P < 0.001), fewer servings of fruit (intervention ‐0.5 serves, control ‐0.1 serves, P = 0.05) and more servings of vegetables (intervention +1.0 serves, control +0.2 serves, P < 0.001).
Dichotomous outcomes
In the trial by Finch and colleagues (Finch 2012), data collected via telephone interview revealed service managers in the intervention region were significantly more likely to report a physical activity policy (intervention +28%, control +4%, P < 0.01) with a physical activity policy that referred to limits on small screen recreation (intervention +37%, control +5%, P < 0.01) and with staff trained in physical activity (intervention +47%, control +6%, P < 0.01). There were no significant differences between intervention and control services at follow‐up in the proportion that conducted daily fundamental movement sessions with recommended components (intervention +8%, control ‐1%, P = 0.08); with a policy that referred to physical activity training for staff (intervention +23%, control +8%, P = 0.07), where all staff usually participate in free active play (intervention +7%, control +8%), where all staff usually provide verbal prompts for physical activity (intervention +2%, control +3%), where children watch small screen recreation less than once per week (intervention ‐1%, control ‐2%), and where children participate in seated activities for no longer than 30 minutes at a time (intervention +1%, control +3%) (P = 0.65 to 0.95).
A number of improvements in implementation assessed using dichotomous measures were reported in the trial by Bell and colleagues (Bell 2014). Relative to the services in the control group, data from interviews with service managers found a significant increase in the proportion of services providing only water and plain milk to children (non‐sweetened drinks). Within the intervention group this increased from 68% at baseline to 95% at follow‐up, compared with changes from 58% to 82% in control services (P = 0.02). The proportion of services where parents participate in nutrition programmes or policy development significantly increased from 65% at baseline to 77% at follow‐up for intervention services compared with a change from 65% to 59% in the control group (P < 0.01). There were no significant differences between groups in three other policies or practices examined and assessed via telephone interview with service managers. Furthermore, consistent with dietary guidelines, intervention services were significantly more likely than control services to have no sweetened drinks listed on their menu (intervention +46%, control +10%, P < 0.001) and the appropriate servings of fruit (intervention +34%, control +4%, P = <0.001) and vegetables (intervention +20%, control +4%, P = 0.01) listed on the menu. There were no significant differences between groups in service guideline adherence to recommendations regarding provision of high‐fat, salt and sugar processed foods or water (intervention effect sizes +9% to +10%, P = 0.11 to 1.00).
6. Educational materials, educational meetings, audit and feedback, opinion leaders and small incentives versus usual practice control
Continuous outcomes
Finch and colleagues conducted a randomised controlled trial with 20 centre‐based childcare services in the Hunter region of the state of New South Wales, Australia (Finch 2014; Finch 2010). The intervention primarily sought to determine the effectiveness of a physical activity intervention, implemented by childcare service staff on the physical activity levels of children attending childcare. Secondary outcomes included assessment of the effectiveness of implementation strategies and the impact of the intervention on rates of child injury. The trial found that time spent by intervention services in structured physical activities increased from 23.67 (SD ± 6.03) minutes at baseline to 52.40 (SD ± 45.29) minutes at follow‐up, whereas control services decreased from 37.80 (SD ± 13.33) at baseline to 27.00 (SD ± 1.41) at follow‐up. This difference was significant (P < 0.02). There were no significant differences between groups in the number of occasions of fundamental movement skill development activity sessions (intervention +0.8 sessions, control +0.2 sessions), the number of times staff participated in active play (intervention +1.4 times, control ‐1.6 times); or the number of times staff provided positive statements about physical activity (intervention +1.7 times, control ‐10.4 times) (P = 0.07 to 0.08). There was little difference between groups in nine other measures of policy and practice implementation including: total minutes of fundamental movement skill development activity sessions, number of times staff prompted physical activity, total minutes of television viewing, total minutes of seated time, or the number of physical activity‐promoting resources or equipment.
Dichotomous outcomes
The trial by Finch included two measures assessing the proportion of services implementing a policy or practice (Finch 2014; Finch 2010). At follow‐up there was no difference between groups in the proportion of services that had a physical activity policy or that had children seated for a period exceeding 30 minutes.
Subgroup analyses of strategies to improve implementation 'at scale'
Three trials sought to implement policies or practices 'at scale', defined as more than 50 services (Bell 2014; Finch 2012; Ward 2008). The randomised trial of multiple strategies to implement the NAPSACC programme by Ward and colleagues was conducted in 56 intervention services and reported significant improvements in total EPAO score among services receiving implementation support (MD 1.01, 95% CI 0.18 to 1.84) (Ward 2008). A quasi‐experimental trial of implementation support provided to more than 200 childcare services reported significant improvement, favouring the intervention group, in the proportion of intervention services with a physical activity policy (percentage change in telephone interview measure: intervention +28%, control +4%, P < 0.01) with a physical activity policy that referred to limits on small screen recreation (percentage change in telephone interview measure: intervention +37%, control +5%, P < 0.01) and with staff trained in physical activity (percentage change in telephone interview measure: intervention +47%, control +6%, P < 0.01), but not eight other measures (Finch 2012). Across all 11 practices the median improvement of intervention relative to control was 2.5% (range ‐4% to 41%). Similarly, Bell and colleagues found, relative to the services in the control group, significant increase among services receiving implementation support in the proportion of services providing only water and plain milk to children (non‐sweetened drinks) and a number of measures of the proportion of service menus with foods consistent with dietary guidelines (Bell 2014). Across 10 such measures, however, the median effect was 9.5% (range 2% to 36%). An audit of menus revealed that intervention services had fewer high‐fat, salt or sugar processed meal items (intervention ‐0.9 items, control ‐0.2 items, P = 0.001), fewer sweetened drinks (intervention ‐0.4 items, control ‐0.1 items, P < 0.001), and more servings of vegetables (intervention +1.0 serves, control +0.2 serves, P < 0.001).
Secondary outcomes
Impact on childcare service staff knowledge, skills or attitudes
Two studies reported changes, relative to a comparator, in attitudes or knowledge of childcare service staff following multi‐component interventions. First, surveys of service managers participating in the intervention trialled by Hardy and colleagues found no differences between groups in any of the seven items assessing staff attitudes regarding encouraging healthy eating or physical activity in children at care (P = 0.07 to 0.39), or three items assessing staff knowledge of recommendations regarding child intake of fruit, vegetables or recreational screen time (Hardy 2010) (P = 0.22 to 0.79). Second, a telephone interview of managers of services receiving the intervention in the study conducted by Finch and colleagues found a greater increase in the proportion of managers at intervention services knowing the recommendations for child participation in physical activity (from 14% at baseline to 21% at follow‐up), compared to managers at control services (magnitude of increase not reported) (P < 0.01), but not in knowledge of the recommendations for maximum time preschool‐aged children should spend in small screen recreation or being sedentary (effect sizes not reported) (P > 0.05) (Finch 2012).
Estimates of absolute costs or assessments of cost‐effectiveness
None of the included studies reported on the costs or reported any cost analyses for the interventions.
Reported adverse consequences
One study explicitly assessed whether the intervention had unintended adverse effects. The study, by Finch and colleagues, compared the number of child injuries in the month prior assessment among intervention and comparison childcare services as reported by childcare managers at baseline and follow‐up (Finch 2014). The rate of injury per month at intervention services at baseline was 0.18 (95% CI 0.09 to 0.27) and 0.17 (95% CI 0.08 to 0.27) at follow‐up, and at control services was 0.12 (95% CI 0.04 to 0.20) at baseline and 0.11 (95% CI 0.03 to 0.19) at follow‐up. This difference was not statistically significant (P = 0.85).
Effects on child diet, physical activity or weight status
Diet
In the quasi‐experimental trial comparing child education curricula and a one‐day food service modification training for cooks with a child curricula only control, Williams and colleagues assessed child dietary intake via direct observation during meal and snack periods (Williams 2002). The intervention was primarily focused on reducing fat, saturated fat and energy. The trial found that children attending intervention services consumed significantly less energy (‐81.33 kcal), fat (‐3.6 grams), saturated fat (‐1.86 grams), as well as less fat as a percentage of energy (‐4.48), and saturated fat as a percentage of energy (‐2.87) relative to the control at the six‐month follow‐up during attendance at care (all P < 0.001). At the 18‐month follow‐up, the saturated fat (‐2.56 grams) and fat as a percentage of energy (‐10.92), and saturated fat as a percentage of energy (‐5.15), remained significantly lower relative to the control group (P < 0.001 to 0.01). The trial also assessed changes in 13 other nutrients. Of these, intake of iron and magnesium were found to be higher among children in intervention compared with control services at the 18‐month follow‐up.
Physical activity
In a randomised trial of a multi‐component intervention to facilitate implementation of the NAPSACC programme, Alkon and colleagues found no significant changes in the intensity or type of physical activity of children in care as assessed by the Observation System for Recording Activity in Preschools (OSRAP) tool (effect sizes and P value not reported) (Alkon 2014). There was, however, a non‐significant decrease in the intervention group in the proportion of sedentary/quiet time, from 60% at baseline to 56% at follow‐up, and a non‐significant increase in the control group from 53% at baseline to 58% at follow‐up (P value not reported). In the randomised trial of a multi‐component intervention of 20 childcare services by Finch and colleagues, there was no significant difference between groups at follow‐up in the step counts per minute as assessed by pedometer (Finch 2014). Mean child step counts in the intervention group were 17.20 (95% CI 15.94 to 18.46) at baseline and 16.12 (95% CI 14.86 to 17.30) at follow‐up, and in the control group were 13.78 (95% CI 12.76 to 14.80) at baseline and 13.87 (95% CI 12.57 to 15.17) at follow‐up.
Weight status
Analyses of the impact of the intervention on centre‐level child adiposity revealed a significant reduction in body mass index (BMI) z‐score relative to the control group (coefficient ‐0.26, standard error (SE) 0.1, P = 0.02) in the trial by Alkon and colleagues (Alkon 2014). The analyses were conducted in children who provided both baseline and follow‐up data (n = 209) and excluded extreme outliers. There were no significant changes within the intervention or control group in the proportion of children in the underweight, healthy weight, overweight or obese categories (P = 0.22 to 1.00). Between‐group comparisons for this measure were not reported (Alkon 2014). An intervention focused on improving childcare menus by Williams and colleagues assessed change in child weight to height ratio at six‐month follow‐up. The trial found no significant intervention effect (f‐value 1.18, P value not reported) (Williams 2002).
Discussion
Summary of main results
This review sought to assess the impact of strategies to support the implementation of policies, practices or programmes to promote physical activity, healthy eating or prevent excessive weight gain among children in centre‐based childcare services. The review identified just 10 trials, most of which were randomised controlled trials testing multi‐component implementation support strategies. Collectively, the findings suggest that the impact of trialled strategies to facilitate implementation is equivocal. None of the included trials improved, relative to a comparison group, implementation of all of the targeted policies and practices. However, most trials reported a significant benefit of implementation support for at least one measure of policy or practice implementation (Alkon 2014; Bell 2014; Finch 2012; Finch 2014; Gosliner 2010; Hardy 2010; Williams 2002). The impact of such interventions on the knowledge or attitudes of childcare service staff, or on the diet, physical activity or weight status of children was also equivocal in the few trials that reported such outcomes.
There were a number of challenges in conducting and synthesising the findings of included studies. There was considerable heterogeneity in the policies and practices targeted, interventions tested, measures used and outcomes reported among included trials. Such heterogeneity precluded meta‐analysis and quantitative exploration of heterogeneity and potential effect modifiers. The degree of clinical and methodological heterogeneity also presented challenges for the narrative synthesis. The 10 included trials reported the effects of six types of implementation strategy, often targeting different nutrition, physical activity or obesity prevention policies and practices, and using different measures of implementation. Classification of implementation strategies was also difficult. The Cochrane Effective Practice and Organisation of Care (EPOC) Group taxonomy has been developed to describe strategies to improve implementation or professional practice of health services or practitioners, which were often not relevant for the childcare setting (EPOC 2015). Other strategies employed by included trials to facilitate implementation, including small incentives such as lotteries or wellness initiatives, did not fit with the current EPOC taxonomy descriptors. To address such issues we included full descriptions of trials, study context and implementation strategies, and reported median and range of effects of included studies. A revision of the EPOC taxonomy and descriptors to align more with the implementation strategies used in non‐clinical settings may improve EPOC strategy coverage and facilitate classification for studies undertaken in childcare and other community settings. Interpretation of the findings therefore represents a considerable challenge.
Among studies aiming to target childcare healthy eating or nutrition policies and practices, improvements were often reported on measures of food provision by childcare service staff. For example, relative to control services, implementation of the majority of practices pertaining to the types of foods served to children were reported in the multi‐component intervention conducted by Bell and colleagues (Bell 2014), and the staff wellness programme conducted by Gosliner and colleagues (Gosliner 2010). Significant effects were also reported for measures of food energy and fat (the primary macronutrients targeted by the intervention) following a one‐day workshop for cooks and ongoing support from a registered dietitian in the study by Williams and colleagues (Williams 2002). Similarly, within‐group improvements were reported on all measures of food provision among both implementation training support strategies trialled by Johnston Molloy and colleagues (Johnston Molloy 2013). Childcare services may be particularly amenable to making changes to improve food provision given that in most jurisdictions providing food consistent with nutrition guidelines is required under service licensing and accreditation standards, as food provision is typically the primary responsibility of a single staff member (Froehlich Chow 2011) (i.e. the service cook), and given strong interest among staff to provide healthy foods to children (Derscheid 2010; Pagnini 2007). Furthermore, barriers to provision of healthy foods by services typically pertain to limited knowledge and skills of cooks (Froehlich Chow 2011; Moore 2005; Pollard 1999), with it being suggested such barriers be overcome through training (Michie 2008). The findings of this review suggest that the multi‐component interventions targeting food service provision, many of which included implementation support focusing on professional development and training of cooks, may have successfully overcome such reported barriers.
In contrast, improvements were not consistently reported on other measures of healthy eating or physical activity policy or practice implementation. Support from childcare executive committees, the service manager or parents (Wolfenden 2015a), as well as staff members' own healthy eating or physical activity behaviours, self‐efficacy in facilitating healthy eating or physical activity, and negative staff attitudes (Cashmore 2008; Copeland 2011; Froehlich Chow 2011), have all been identified as impediments to implementing healthy eating or physical activity‐promoting policies and practices. Furthermore, for the implementation of physical activity policies, practices and programmes in particular, structural barriers, such as a preference for child‐directed rather than teacher‐led structured physical activity by childcare service staff, a lack of space, inclement weather or lack of broader policy framework (Cashmore 2008; Copeland 2011), have been noted as implementation barriers. Such a complex range of potential determinants to implementation in this setting may require carefully considered and targeted support strategies in order for them to be overcome.
Only three of the included studies examined the impact of interventions on measures of child nutrition, physical activity or adiposity and effects were mixed. Improvements in both the implementation of nutrition practices regarding food service and in child diet were reported following the multi‐component intervention conducted by Williams and colleagues (Williams 2002). However, the multi‐component support provided in the trial by Finch and colleagues did not improve child physical activity while in care (Finch 2014), nor did intensive implementation support strategies to facilitate implementation of the Nutrition and Physical Activity Self‐Assessment for Child Care (NAPSACC) programme (Alkon 2014). Such findings are likely to reflect limited improvements in implementation of physical activity practices for both trials. Providing intensive implementation support did, however, reduce child body mass index (BMI) z‐score in the evaluation of the NAPSACC programme conducted by Alkon and colleagues (Alkon 2014). Such a finding was surprising given that improvements in healthy eating and physical activity policies, but not practices, were reported. Potentially, the implementation support may have facilitated the implementation of other obesity prevention practices by staff of intervention childcare services, or in the home. Further research is warranted to assess such effects in future trials.
Overall completeness and applicability of evidence
Six of the 10 included trials were conducted by two research groups in the USA and Australia (Alkon 2014; Bell 2014; Benjamin 2007; Finch 2012; Finch 2014; Ward 2008). Furthermore, all of the included studies were conducted in high‐income countries. The applicability of study findings to lower and middle‐income countries, where the operational, philosophical and cultural contexts may differ substantially, is unknown (Rosemburg 2003). Future research, conducted by a greater range of research groups in different research contexts, would strengthen the applicability of the evidence base.
Quality of the evidence
The overall rating of the quality of the body of evidence reported in this review across all GRADE domains was very low, suggesting that the effects of interventions reported in the review may differ from the true effects. 'Risk of bias' assessments identified a number of limitations of the existing trials, particularly among the non‐randomised designs. Risk of performance bias (due to lack of blinding of participants or personnel), detection bias (due to use of self‐assessment measures in some studies) and reporting bias (due to a lack of prospective registration or published trial protocols) were particularly prevalent among included studies. The comparison groups used limited the directness of the assembled evidence. A number of studies included comparison groups that included some active implementation support (Johnston Molloy 2013), or 'usual' implementation support (Bell 2014; Finch 2012), which may not have been well defined. Finally, there were concerns regarding the precision of the estimates of included studies for the primary outcomes of this review. Most studies included samples of fewer than 15 per trial arm, which is likely to be insufficient to detect small but meaningful effects. Similarly, seven of the 10 trials included a measure of implementation as the primary trial outcome (Alkon 2014; Bell 2014; Benjamin 2007; Finch 2012; Gosliner 2010; Johnston Molloy 2013; Ward 2008), and only one of these performed a sample size calculation to justify the included sample (Finch 2012). As trial data could not be pooled in meta‐analysis, under‐powering of individual studies in this review may mask important effects.
Potential biases in the review process
The review included a comprehensive search strategy for peer‐reviewed and grey literature and examined over 6000 citations. We also sought relevant studies from screening of citations of included studies, and from contact with experts in the field. While the search strategy was rigorous, as a field in which terminology for implementation constructs are developing, it is possible that not all studies that report implementation outcomes were identified. For example, it has been estimated that 15% of studies use implementation strategies that cannot be classified using implementation taxonomies (Mazza 2013). Potentially relevant studies may have been missed based on the implementation strategy search terms used in this review. However, a previous review conducted by the Agency for Healthcare Research and Quality failed to identify any studies of implementation strategies targeting healthy eating and physical activity in the childcare setting (Rabin 2010), and contact with other experts in the field did not yield any additional studies to those identified in the primary search. Such findings provide some evidence to suggest that the search strategy may have provided reasonable coverage of the relevant literature. Nonetheless, we will assess the appropriateness of search terms in future updates of the review to ensure that the search terms are inclusive of relevant implementation terminology and newly released taxonomies. The method for describing effects across studies may have also introduced bias. In instances where a primary implementation outcome was not identified in included trials we utilised a median effect size across implementation outcomes. Such analyses are inconsiderate of the robustness of individual measures, and may mask important effects on single implementation outcomes. Consideration of the narrative description of each trial included in the review is therefore important when interpreting trial findings.
Agreements and disagreements with other studies or reviews
Contextualising the findings of the review with those conducted previously is difficult given that few reviews have examined the effectiveness of implementation strategies in community settings. A comprehensive review conducted in 2008 identified just one study in the childcare setting, which targeted implementation of policies and practices to reduce the risk of skin cancer (Rabin 2010). The review found mixed evidence of the effectiveness of strategies to support implementation of health promotion policies and practices in other settings, such as schools and sporting clubs: findings that are similar to the conclusions of this review (Rabin 2010). In healthcare settings, systematic reviews have found that multi‐component implementation strategies may not be more effective than single component strategies (Squires 2014). However, small positive improvements in implementation or professional practice have been found in large systematic review of strategies including audit and feedback (Ivers 2012), training (Forsetlund 2009), and academic detailing (O'Brien 2007). More trials are required in the childcare setting to determine if such strategies are similarly effective in this setting.
Authors' conclusions
The review highlights how little guidance is available for policy makers and practitioners interested in supporting the implementation of healthy eating, physical activity or obesity prevention policies, practices and programmes in centre‐based childcare services. Collectively the findings suggest that implementation strategies can have a positive impact, albeit limited, on the implementation of healthy eating, physical activity and obesity prevention policies, practices and programmes in this setting. With a small number of trials to date and in the absence of high‐quality evidence, formative work to achieve a comprehensive understanding of the setting, context and barriers to implementation, and careful selection of support strategies to address these, may be particularly important for practitioners to maximise the potential for successful implementation (French 2012).
The findings of this review suggest that there is considerable scope to improve the evidence base to guide future efforts to support implementation of healthy eating, physical activity and obesity prevention programmes in centre‐based childcare services. The limited number of trials is surprising given the large numbers of trials testing interventions in to improve healthy eating, physical activity or obesity prevention interventions in recent systematic reviews in this setting (Finch 2016; Mikkelsen 2014; Sisson 2016). The findings confirm bibliographic studies that indicate that trials examining the effects of strategies to implement evidence‐based programmes or polices represent a fraction of public health research trials (Wolfenden 2016a; Wolfenden 2016c; Yoong 2015). Greater investment in research, and research infrastructure to support trials to improve dissemination and implementation of effective childcare‐based interventions, is therefore warranted (Wolfenden 2016b). Additionally, the review identified a number of ongoing studies in the area, which will further contribute to the evidence base (see Characteristics of ongoing studies).
In many instances the trials included in the review had small samples (Alkon 2014; Benjamin 2007; Finch 2014; Gosliner 2010; Hardy 2010; Williams 2002), which may be unable to detect important improvements in policy or practice, or they used self‐reported measures of implementation. The cost of practice improvements was not assessed in any included trials and few trials assessed the impact of interventions on child health behaviours or weight status (Alkon 2014; Finch 2014; Williams 2002). Comprehensive evaluations of future efforts to improve the implementation of health‐promoting initiatives targeting excessive weight gain or its determinants in this setting are required to address the limitations identified within the existing evidence base. The use of hybrid designs in future trials, in which implementation outcomes as well as impacts on health behaviours or weight status have been recommended, is one means of achieving this (Cohen 2015).
With a few exceptions, most included studies developed implementation support strategies without the aid of relevant theory or theoretical frameworks (Alkon 2014; Finch 2012; Gosliner 2010; Hardy 2010; Johnston Molloy 2013; Williams 2002). Perhaps unsurprisingly, the use of the range of potential strategies, as described in the EPOC taxonomy, was relatively limited by the included studies, and focused often on one‐off training or resource provision. The factors that influence policy or practice implementation are typically complex. Improvements in implementation may require ongoing changes to systems and processes rather than fixed discrete support. However, none of the trials included strategies to address other fiscal, political, regulatory or governance factors that could potentially influence the success of implementation efforts. The use of comprehensive theoretical frameworks could assist in considering a broad range of implementation barriers and designing appropriate support strategies to address these (Cane 2012; Damschroder 2009).
Further, given that the impact of current implementation support strategies appears equivocal, future theoretically informed research to identify the mechanism by which support strategies may facilitate implementation would be of particular value to guide future strategy design. The Theoretical Domains Framework is supported by documented processes to identify impediments to implementation, selection of support strategies to overcome such barriers, and validated instruments to assess implementation constructs (French 2012; Michie 2008). The framework has been successfully applied in clinical settings to improve professional practice (Cane 2012; Phillips 2015). Application of implementation‐specific frameworks such as the Theoretical Domains Framework in the childcare setting seems warranted to examine whether this improves the impact of implementation interventions in this setting. Furthermore, adaptation and revalidation of tools to assess implementation constructs in future trials in the setting would provide valuable insights into mechanisms of effect to progress the field.
Acknowledgements
We would like to acknowledge the support provided by the University of Newcastle, Hunter New England Population Health, the Hunter Medical Research Institute and Cochrane Public Health and comments received from the external referees Dianne Stanton Ward, Emily Hill Guseman and Aron Shlonsky.
Appendices
Appendix 1. Search strategy
MEDLINE search strategy
1. exp obesity/ 2. Weight Gain/ 3. exp Weight Loss/ 4. obes*.mp. 5. (weight gain or weight loss).mp. 6. (overweight or over weight or overeat* or over eat*).mp. 7. weight change*.mp. 8. ((bmi or body mass index) adj2 (gain or loss or change)).mp. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. exp Exercise/ 11. physical inactivity.mp. 12. physical activity.mp. 13. exp Motor Activity/ 14. (physical education and training).mp. 15. exp "Physical Education and Training"/ 16. Physical Fitness/ 17. sedentary.mp. 18. exp Life Style/ 19. exp Leisure Activities/ 20. exp Sports/ 21. Dancing/ 22. (exercise* adj2 aerobic*).mp. 23. sport*.mp. 24. ((life style or life style) adj5 activ*).mp. 25. (dance* or dancing).mp. 26. 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 27. exp Diet/ 28. nutrition*.mp. 29. (health* adj2 eat*).mp. 30. Child Nutrition Sciences/ 31. Fruit/ or fruit*.mp. 32. Vegetables/ or vegetable*.mp. 33. canteen*.mp. 34. Food Services/ 35. menu.mp. 36. (calorie or calories or kilojoule*).mp. 37. Energy Intake/ 38. energy density.mp. 39. Eating/ 40. Feeding Behavior/ or feeding behaviour.mp. 41. dietary intake.mp. 42. Food Habits/ 43. Food/ 44. Carbonated Beverages/ or soft drink*.mp. 45. soda.mp. 46. sweetened drink*.mp. 47. Dietary Fats/ 48. confectionary.mp. 49. (school adj2 (lunch* or meal*)).mp. 50. Menu Planning/ 51. feeding program*.mp. 52. food program*.mp. 53. (nutrition* adj2 program*).mp. 54. cafeteria*.mp. 55. Nutritional Status/ 56. 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 57. 9 or 26 or 56 58. Child, Preschool/ 59. (pre‐school* or preschool*).mp. 60. Child Day Care Centers/ 61. (childcare* or child care*).mp. 62. (daycare* or day care*).mp. 63. early child*.mp. 64. (nursery or nurseries).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] 65. Kinder*.mp. 66. 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 67. randomized controlled trial.pt. 68. controlled clinical trial.pt. 69. clinical trials as topic.sh. 70. trial*.tw. 71. double blind.tw. 72. single blind.tw. 73. experiment*.tw. 74. (pretest or pre test).tw. 75. (posttest or post test).tw. 76. (pre post or prepost).tw. 77. before after.tw. 78. qua?i randomi?ed.tw. 79. stepped wedge.tw. 80. (non randomi?ed or nonrandomi?ed).tw. 81. interrupted time series.tw. 82. multiple baseline.tw. 83. regression discontinuity.tw. 84. comprehensive cohort.tw. 85. random*.ab. 86. 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 87. implement*.mp. 88. dissemin*.mp. 89. adopt*.mp. 90. practice*.mp. 91. organi?ational change*.mp. 92. diffus*.mp. 93. (system* adj2 change*).tw. 94. quality improvement*.mp. 95. transform*.mp. 96. translat*.mp. 97. transfer*.mp. 98. uptake*.mp. 99. sustainab*.mp. 100. institutionali*.mp. 101. routin*.mp. 102. maintenance.mp. 103. capacity.mp. 104. incorporat*.mp. 105. adher*.mp. 106. ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).mp. 107. integrat*.mp. 108. scal* up.mp. 109. 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 110. 57 and 66 and 86 and 10
CENTRAL search strategy
1. MeSH descriptor: [Obesity] explode all trees 2. MeSH descriptor: [Weight Gain] this term only 3. MeSH descriptor: [Weight Loss] explode all trees 4. obes* 5. weight gain or weight loss 6. overweight or "over weight" or overeat* or "over eat*" 7. "weight change*" 8. ((bmi or body mass index) near/2 (gain or loss or change)) 9. {or #1‐#8} 10. MeSH descriptor: [Exercise] explode all trees 11. "physical inactivity" 12. "physical activity" 13. MeSH descriptor: [Motor Activity] explode all trees 14. "physical education and training" 15. MeSH descriptor: [Physical Education and Training] explode all trees 16. MeSH descriptor: [Physical Fitness] this term only 17. sedentary 18. MeSH descriptor: [Life Style] explode all trees 19. MeSH descriptor: [Leisure Activities] explode all trees 20. MeSH descriptor: [Sports] explode all trees 21. MeSH descriptor: [Dancing] this term only 22. exercis* near/2 aerobic* 23. sport* 24. (life style or lifestyle) near/5 activ* 25. dance* or dancing 26. {or #10‐#25} 27. MeSH descriptor: [Diet] explode all trees 28. nutrition* 29. health* near/2 eat* 30. MeSH descriptor: [Child Nutrition Sciences] this term only 31. fruit* 32. MeSH descriptor: [Fruit] this term only 33. vegetable* 34. MeSH descriptor: [Vegetables] this term only 35. canteen* 36. MeSH descriptor: [Food Services] this term only 37. menu 38. calorie or calories or kilojoule* 39. MeSH descriptor: [Energy Intake] this term only 40. "energy density" 41. MeSH descriptor: [Eating] this term only 42. MeSH descriptor: [Feeding Behavior] this term only 43. "feeding behaviour" 44. "dietary intake" 45. MeSH descriptor: [Food Habits] this term only 46. MeSH descriptor: [Food] this term only 47. MeSH descriptor: [Carbonated Beverages] this term only 48. "soft drink*" 49. soda 50. "sweetened drink*" 51. MeSH descriptor: [Dietary Fats] this term only 52. confectionary 53. school near/2 (lunch* or meal*) 54. MeSH descriptor: [Menu Planning] this term only 55. "feeding program*" 56. "food program*" 57. nutrition* near/2 program* 58. cafeteria* 59. MeSH descriptor: [Nutritional Status] this term only 60. {or #27‐#59} 48804 61. MeSH descriptor: [Child, Preschool] this term only 62. pre‐school* or preschool* 63. MeSH descriptor: [Child Day Care Centers] this term only 64. childcare* or "child care*" 65. daycare* or "day care*" 66. "early child*" 67. nursery or nurseries 68. Kinder* 69. {or #61‐#68} 70. randomized controlled trial.pt 71. controlled clinical trial.pt 72. clinical trials as topic.sh 73. trial*:ti,ab 74. double blind:ti,ab 75. single blind:ti,ab 76. experiment*:ti,ab 77. pretest or "pre test":ti,ab 78. posttest or "post test":ti,ab 79. pre post or "prepost":ti,ab 80. "before after":ti,ab 81. "qua?i randomi?ed":ti,ab 82. "stepped wedge":ti,ab 83. "non randomi?ed" or nonrandomi?ed:ti,ab 84. "interrupted time series":ti,ab 85. "multiple baseline":ti,ab 86. "regression discontinuity":ti,ab 87. "comprehensive cohort":ti,ab 88. random*:ab 89. {or #70‐#88} 90. implement* 91. dissemin* 92. adopt* 93. practice* 94. "organi?ational change*" 95. diffus* 96. system* near/2 change* 97. "quality improvement*" 98. transform* 99. translat* 100. transfer* 101. uptake* 102. sustainab* 103. institutionali* 104. routin* 105. maintenance 106. capacity 107. incorporat* 108. adher* 109. (polic* or practice* or program* or innovation*) near/5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*) 10599 110. integrat* 111. "scal* up" 112. {or #90‐#111} 113. #9 or #26 or #60 114. #69 and #89 and #112 and #113
MEDLINE In Process search strategy
1. obes*.mp. 2. (weight gain or weight loss).mp. 3. (overweight or over weight or overeat* or over eat*).mp. 4. weight change*.mp. 5. ((bmi or body mass index) adj2 (gain or loss or change)).mp. 6. 1 or 2 or 3 or 4 or 5 7. exercis*.mp. 8. physical inactivity.mp. 9. physical activity.mp. 10. motor activity.mp. 11. (physical education and training).mp. 12. Physical Fitness.mp. 13. sedentary.mp. 14. Leisure Activit*.mp. 15. sport*.mp. 16. ((life style or lifestyle) adj5 activ*).mp. 17. (dance* or dancing).mp. 18. 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 19. diet.mp. 20. nutrition*.mp. 21. (health* adj2 eat*).mp. 22. fruit*.mp. 23. vegetable*.mp. 24. canteen*.mp. 25. Food Service*.mp. 26. menu.mp. 27. (calorie or calories or kilojoule*).mp. 28. Energy Intake.mp. 29. energy density.mp. 30. Eating.mp. 31. feeding behavio?r*.mp. 32. dietary intake.mp. 33. Food.mp. 34. ((carbonated or sweetened or soft) adj (drink* or beverage*)).mp. 35. soda.mp. 36. Dietary Fat*.mp. 37. confectionary.mp. 38. (school adj2 (lunch* or meal*)).mp. 39. feeding program*.mp. 40. food program*.mp. 41. (nutrition* adj2 program*).mp. 42. cafeteria*.mp. 43. 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 44. (pre‐school* or preschool*).mp. 45. (childcare* or child care*).mp. 46. (daycare* or day care*).mp. 47. early child*.mp. 48. (nursery or nurseries).mp. 49. Kinder*.mp. 50. 44 or 45 or 46 or 47 or 48 or 49 51. randomized controlled trial.pt. 52. controlled clinical trial.pt. 53. trial*.tw. 54. double blind.tw. 55. single blind.tw. 56. experiment*.tw. 57. (pretest or pre test).tw. 58. (posttest or post test).tw. 59. (pre post or prepost).tw. 60. before after.tw. 61. qua?i randomi?ed.tw. 62. stepped wedge.tw. 63. (non randomi?ed or nonrandomi?ed).tw. 64. interrupted time series.tw. 65. multiple baseline.tw. 66. regression discontinuity.tw. 67. comprehensive cohort.tw. 68. random*.tw. 69. 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 70. implement*.mp. 71. dissemin*.mp. 72. adopt*.mp. 73. practice*.mp. 74. organi?ational change*.mp. 75. diffus*.mp. 76. (system* adj2 change*).tw. 77. quality improvement*.mp. 78. transform*.mp. 79. translat*.mp. 80. transfer*.mp. 81. uptake*.mp. 82. sustainab*.mp. 83. institutionali*.mp. 84. routin*.mp. 85. maintenance.mp. 86. capacity.mp. 87. incorporat*.mp. 88. adher*.mp. 89. ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).mp. 90. integrat*.mp. 91. scal* up.mp. 92. 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 93. 6 or 18 or 43 94. 50 and 69 and 92 and 93
EMBASE search strategy
1. exp obesity/ 2. weight gain/ 3. Weight Loss.mp. or exp weight reduction/ 4. obes*.mp. 5. (weight gain or weight loss).mp. 6. (overweight or over weight or overeat* or over eat*).mp. 7. weight change*.mp. 8. ((bmi or body mass index) adj2 (gain or loss or change)).mp. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. exp exercise/ 11. physical inactivity.mp. or physical inactivity/ 12. exp physical activity/ 13. exp motor activity/ 14. "physical education and training".mp. 15. physical education/ 16. physical fitness.mp. or fitness/ 17. sedentary.mp. 18. lifestyle/ 19. Leisure Activities.mp. or leisure/ 20. exp sport/ 21. dancing/ 22. (exercise* adj2 aerobic*).mp. 23. sport*.mp. 24. ((life style or lifestyle) adj5 activ*).mp. 25. (dance* or dancing).mp. 26. 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 27. exp diet/ 28. nutrition*.mp. or nutrition/ 29. (health* adj2 eat*).mp. 30. Child Nutrition Sciences.mp. or nutritional science/ 31. fruit*.mp. or fruit/ 32. vegetable*.mp. or vegetable/ 33. canteen*.mp. 34. Food Services.mp. or catering service/ 35. menu.mp. 36. (calorie or calories or kilojoule*).mp. 37. Energy Intake.mp. or caloric intake/ 38. energy density.mp. 39. eating/ 40. feeding behaviour.mp. or feeding behavior/ 41. dietary intake.mp. or dietary intake/ 42. Food Habits.mp. or feeding behavior/ 43. food/ 44. carbonated beverage/ or soft drink*.mp. or soft drink/ 45. soda.mp. 46. sweetened drink*.mp. 47. Dietary Fats.mp. or fat intake/ 48. confectionary.mp. 49. (school adj2 (lunch* or meal*)).mp. 50. Menu Planning.mp. 51. feeding program*.mp. 52. food program*.mp. 53. (nutrition* adj2 program*).mp. 54. cafeteria*.mp. 55. nutritional status/ 56. 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 57. 9 or 26 or 56 58. Child, Preschool/ 59. (pre‐school* or preschool*).mp. 60. day care/ 61. child care/ or childcare*.mp. 62. (daycare* or day care*).mp. 63. early child*.mp. 64. nurseries.mp. or nursery/ 65. Kinder*.mp. 66. 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 67. randomized controlled trial/ 68. controlled clinical trial/ 69. "clinical trial (topic)"/ 70. trial*.tw. 71. double blind.tw. 72. single blind.tw. 73. experiment*.tw. 74. (pretest or pre test).tw. 75. (posttest or post test).tw. 76. (pre post or prepost).tw. 77. before after.tw. 78. qua?i randomi?ed.tw. 79. stepped wedge.tw. 80. (non randomi?ed or nonrandomi?ed).tw. 81. interrupted time series.tw. 82. multiple baseline.tw. 83. regression discontinuity.tw. 84. comprehensive cohort.tw. 85. random*.ab. 86. 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 87. implement*.mp. 88. dissemin*.mp. 89. adopt*.mp. 90. organi?ational change*.mp. 91. diffus*.mp. 92. (system* adj2 change*).tw. 93. quality improvement*.mp. 94. practice*.mp. 95. transform*.mp. 96. translat*.mp. 97. transfer*.mp. 98. uptake*.mp. 99. sustainab*.mp. 100. institutionali*.mp. 101. routin*.mp. 102. maintenance.mp. 103. capacity.mp. 104. incorporat*.mp. 105. adher*.mp. 106. ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).mp. 107. integrat*.mp. 108. scal* up.mp. 109. 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 110. 57 and 66 and 86 and 109
PsychINFO search strategy
1. Obesity/ 2. Weight Gain/ 3. Weight Loss/ 4. obes*.mp. 5. (weight gain or weight loss).mp. 6. (overweight or over weight or overeat* or over eat*).mp. 7. weight change*.mp. 8. ((bmi or body mass index) adj2 (gain or loss or change)).mp. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. exp Exercise/ 11. physical inactivity.mp. 12. physical activity.mp. or Physical Activity/ 13. Motor Activity.mp. 14. (physical education and training).mp. 15. Physical Education/ 16. Physical Fitness/ 17. sedentary.mp. 18. exp Lifestyle/ 19. leisure time/ or recreation/ 20. exp Sports/ 21. Dance/ 22. (exercise* adj2 aerobic*).mp. 23. sport*.mp. 24. ((life style or lifestyle) adj5 activ*).mp. 25. (dance* or dancing).mp. 26. 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 27. Diets/ 28. exp Nutrition/ or Nutrition*.mp. 29. (health* adj2 eat*).mp. 30. Child Nutrition Sciences.mp. 31. fruit*.mp. 32. vegetable*.mp. 33. canteen*.mp. 34. Food Services.mp. 35. menu.mp. 36. (calorie or calories or kilojoule*).mp. 37. Food Intake/ or Energy Intake.mp. 38. energy density.mp. 39. Eating.mp. 40. Eating Behavior/ 41. feeding behavio?r.mp. 42. dietary intake.mp. 43. Food/ 44. ((carbonated or sweetened or soft) adj (drink* or beverage*)).mp. 45. soda.mp. 46. Dietary Fat*.mp. 47. confectionary.mp. 48. (school adj2 (lunch* or meal*)).mp. 49. feeding program*.mp. 50. food program*.mp. 51. (nutrition* adj2 program*).mp. 52. cafeteria*.mp. 53. 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 54. 9 or 26 or 53 55. preschool students/ or nursery school students/ 56. (pre‐school* or preschool*).mp. 57. Day Care Centers/ or Child Day Care/ 58. (childcare* or child care*).mp. 59. (daycare* or day care*).mp. 60. early child*.mp. 61. (nursery or nurseries).mp. 62. Kindergarten Students/ or Kinder*.mp. 63. 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 64. randomi?ed controlled trial*.mp. 65. Clinical Trials/ 66. trial*.tw. 67. double blind.tw. 68. single blind.tw. 69. experiment*.tw. 70. (pretest or pre test).tw. 71. (posttest or post test).tw. 72. (pre post or prepost).tw. 73. before after.tw. 74. qua?i randomi?ed.tw. 75. stepped wedge.tw. 76. (non randomi?ed or nonrandomi?ed).tw. 77. interrupted time series.tw. 78. multiple baseline.tw. 79. regression discontinuity.tw. 80. comprehensive cohort.tw. 81. random*.ab. 82. 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 83. implement*.mp. 84. dissemin*.mp. 85. adopt*.mp. 86. practice*.mp. 87. organi?ational change*.mp. 88. diffus*.mp. 89. (system* adj2 change*).tw. 90. quality improvement*.mp. 91. transform*.mp. 92. translat*.mp. 93. transfer*.mp. 94. uptake*.mp. 95. sustainab*.mp. 96. institutionali*.mp. 97. routin*.mp. 98. maintenance.mp. 99. capacity.mp. 100. incorporat*.mp. 101. adher*.mp. 102. ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).mp. 103. integrat*.mp. 104. scal* up.mp. 105. 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 or 104 106. 54 and 63 and 82 and 105
ERIC search strategy
(lobes* OR "weight gain" OR "weight loss" OR overweight OR "over weight" OR overeat* OR over eat* OR "weight change*" OR ((bmi OR body mass index) AND (gain OR loss OR change)) OR Exercise* OR "physical inactivity" OR "physical activity" OR "Motor Activity" OR "physical education" OR "Physical Fitness" OR sedentary OR "leisure activit*" OR sport* OR dance* OR ((life style OR lifestyle) AND activ*) OR Diet OR nutrition* OR (health* AND eat*) OR "Child Nutrition*" OR fruit* OR vegetable* OR canteen* OR menu OR calorie OR calories OR kilojoule* OR "Energy Intake" OR "energy density" OR Eating OR "feeding behaviour" OR "Feeding Behavior" OR "dietary intake" OR food OR ((carbonated OR sweetened OR soft) AND (drink* OR beverage*)) OR soda OR "Dietary Fat*" OR confectionary OR (school AND (lunch* OR meal*)) OR "feeding program*" OR cafeteria*)
AND (pre‐school* or preschool* or childcare* or “child care*” or daycare* or “day care*” or “early child*” or nursery or nurseries or Kinder*)
AND (Random* or trial* or “double blind” or “single blind” or experiment* or pretest or “pre test” or posttest or “post test” or “pre post” or prepost or “before after” or “stepped wedge” or nonrandomi?ed or “interrupted time series” or “multiple baseline” or “regression discontinuity” or “comprehensive cohort”)
AND (Implement* or dissemin* or adopt* or practice* or “organi?ational change*” or diffuse* or (system* and change*) or “quality improvement*” or transform* or translat* or transfer* or uptake* or sustainab* or institutionali* or routin* or maintenance or capacity or incorporate* or adher* or ((polic* or practice* or program* or innovation*) and (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)) or integrat* or “scal* up”)
CINAHL search strategy
S111. S58 AND S68 AND S87 AND S110 S110. S88 OR S89 OR S90 OR S91 OR S92 OR S93 OR S94 OR S95 OR S96 OR S97 OR S98 OR S99 OR S100 OR S101 OR S102 OR S103 OR S104 OR S105 OR S106 OR S107 OR S108 OR S109 S109. incorporat* S108. scal* up S107. integrat* S106. ((polic* or practice* or program* or innovation*) n5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)) S105. adher* S104. capacity S103. maintenance S102. routin* S101. institutionali* S100. sustainab* S99. uptake* S98. transfer* S97. translat* S96. transform* S95. quality improvement* S94. system* n2 change* S93. diffus* S92. organi?ational change* S91. practice* S90. adopt* S89. dissemin* S88. implement* S87. S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 OR S85 OR S86 S86. AB random* S85. TI comprehensive cohort OR AB comprehensive cohort S84. TI regression discontinuity OR AB regression discontinuity S83. TI multiple baseline OR AB multiple baseline S82. TI interrupted time series OR AB interrupted time series S81. TI ( non randomi?ed or nonrandomi?ed ) OR AB ( non randomi?ed or nonrandomi?ed ) S80. TI stepped wedge OR AB stepped wedge S79. TI qua?i randomi?ed OR AB qua?i randomi?ed S78. TI before after OR AB before after S77. TI ( pre post or prepost ) OR AB ( pre post or prepost ) S76. TI ( posttest or post test ) OR AB ( posttest or post test ) S75. TI ( pretest or pre test ) OR AB ( pretest or pre test ) S74. (MH "Experimental Studies") OR "experiment*" S73. (MH "Single‐Blind Studies") OR "single blind" S72. (MH "Double‐Blind Studies") OR "double blind" S71. TI trial* OR AB trial* S70. (MH "Clinical Trials") S69. (MH "Randomized Controlled Trials") S68. S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 S67. Kinder* S66. nursery or nurseries S65. (MH "Schools, Nursery") S64. "early child*" S63. daycare* or day care* S62. childcare* or child care* S61. (MH "Child Day Care") OR (MH "Child Care Providers") OR (MH "Child Care (Saba CCC)") OR (MH "Child Care") S60. pre‐school* or preschool* S59. (MH "Child, Preschool") S58. S9 OR S26 OR S57 S57. S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 S56. (MH "Nutritional Status") S55. cafeteria* S54. (nutrition* n2 program*) S53. "food program*" S52. "feeding program*" S51. school n2 (lunch* or meal*) S50. "confectionary" OR (MH "Candy") S49. (MH "Dietary Fats") S48. "sweetened drink*" S47. soda S46. (MH "Carbonated Beverages") OR "soft drink*" S45. (MH "Food") S44. (MH "Food Habits") OR "Food Habits" S43. dietary intake S42. (MH "Eating") OR (MH "Eating Behavior") S41. "feeding behavio?r" S40. (MH "Energy Density") OR "Energy Density" S39. (MH "Energy Intake") OR (MH "Food Intake") S38. calorie or calories or kilojoule* S37. (MH "Menu Planning") OR "menu" S36. (MH "Food Services") S35. "canteen*" S34. fruit* S33. (MH "Vegetables") OR "vegetable*" S32. (MH "Fruit+") S31. (MH "Child Nutrition") S30. health* n2 eat* S29. (MH "Nutrition") S28. "nutrition*" S27. (MH "Diet+") S26. S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 S25. dance* or dancing S24. (life style or lifestyle) n5 activ* S23. sport* S22. exercis* n2 aerobic* S21. (MH "Dancing+") S20. (MH "Sports+") S19. (MH "Leisure Activities+") S18. (MH "Life Style+") S17. (MH "Life Style, Sedentary") OR "sedentary" S16. (MH "Physical Fitness") S15. (MH "Physical Education and Training+") S14. physical education and training S13. (MH "Motor Activity+") S12. (MH "Physical Activity") OR "physical activity" S11. physical inactivity S10. (MH "Exercise+") S9. S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 S8. obes* S7. ((bmi or body mass index) n2 (gain or loss or change)) S6. weight change* S5. overweight or over weight or overeat* or over eat* S4. weight gain or weight loss S3. (MH "Weight Loss+") S2. (MH "Weight Gain") S1. (MH "Obesity+")
SCOPUS search strategy
TITLE‐ABS‐KEY ( obes* OR "weight gain" OR "weight loss" OR overweight OR "over weight" OR overeat* OR over eat* OR "weight change*" OR ( ( bmi OR body mass INDEX ) AND ( gain OR loss OR change ) ) OR exercise* OR "physical inactivity" OR "physical activity" OR "Motor Activity" OR "physical education" OR "Physical Fitness" OR sedentary OR "leisure activit*" OR sport* OR danc* OR ( ( life style OR lifestyle ) AND activ* ) OR diet OR nutrition* OR ( health* AND eat* ) OR "Child Nutrition*" OR fruit* OR vegetable* OR canteen* OR menu OR calorie OR calories OR kilojoule* OR "Energy Intake" OR "energy density" OR eating OR "feeding behaviour" OR "Feeding Behavior" OR "dietary intake" OR food OR ( ( carbonated OR sweetened OR soft ) AND ( drink* OR beverage* ) ) OR soda OR "Dietary Fat*" OR confectionary OR ( school AND ( lunch* OR meal* ) ) OR "feeding program*" OR cafeteria* )
AND TITLE‐ABS‐KEY ( pre‐school* OR preschool* OR childcare* OR "child care*" OR daycare* OR "day care*" OR "early child*" OR nursery OR nurseries OR kinder* )
AND TITLE‐ABS‐KEY ( random* OR trial* OR "double blind" OR "single blind" OR experiment* OR pretest OR "pre test" OR posttest OR "post test" OR "pre post" OR prepost OR "before after" OR "stepped wedge" OR nonrandomi?ed OR "interrupted time series" OR "multiple baseline" OR "regression discontinuity" OR "comprehensive cohort" )
AND TITLE‐ABS‐KEY ( implement* OR dissemin* OR adopt* OR practice* OR "organi?ational change*" OR diffuse* OR ( system* AND change* ) OR "quality improvement*" OR transform* OR translat* OR transfer* OR uptake* OR sustainab* OR institutionali* OR routin* OR maintenance OR capacity OR incorporate* OR adher* OR ( ( polic* OR practice* OR program* OR innovation* ) AND ( performance OR feedback OR prompt* OR reminder* OR incentive* OR penalt* OR communicat* OR social market* OR professional development OR network* OR leadership OR opinion leader* OR consensus process* OR change manage* OR train* OR audit* ) ) OR integrat* OR "scal* up" )
Data and analyses
This review has no analyses.
Differences between protocol and review
The review included an additional subgroup analysis that was not specified in the protocol. Specifically the review included examination of the impact of implementation strategies that have been conducted 'at scale', defined as 50 or more childcare services.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alkon 2014
| Methods | Study design: cluster‐randomised controlled trial Intervention duration: 7 months Length of follow‐up from baseline: 7 months Differences in baseline characteristics: reported Unit of allocation: childcare service Unit of analysis: childcare service (child behaviour and weight status were assessed at the level of the individual) | |
| Participants |
Service type: childcare centres Region: California, Connecticut and North Carolina, USA Demographic/socioeconomic characteristics: children between the ages of 3 and 5 years of age from racial/ethnically diverse backgrounds and primarily of low‐income families Inclusion/exclusion criteria: inclusion criteria: English‐speaking service manager, on‐site kitchen, racial/ethnic diversity among the children, participation by at least 60% of families, and a population of children in care primarily comprised of low‐income children between the ages of 3 and 5 years of age Number of services randomised: 18 (9 intervention, 9 control) Numbers by trial group: n (controls baseline) = 9 n (controls follow‐up) = 9 (2 small services under same ownership analysed as 1 service) n (interventions baseline) = 9 n (interventions follow‐up) = 9 Recruitment: Service: 42 childcare services were recruited, of which 24 services did not meet the inclusion criteria. Childcare health consultants from California and North Carolina recruited the convenience sample of services for their respective states while Connecticut services were recruited by the Connecticut principal investigator. Child: Physical activity: 8 children at each service, randomly selected by a statistician BMI: the research assistants selected children at the pre‐intervention period for height and weight measurements from service‐specific randomly ordered lists of enrolled children. Those with pre‐intervention measurements (268) were prioritised for measurement post‐intervention (336); 209 children had useable data at both time points. Recruitment rate: 43% |
|
| Interventions |
Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: Nutrition and Physical Activity Self‐Assessment for Child Care (NAPSACC) programme including: ‐ Childhood obesity ‐ Healthy eating for young children ‐ Physical activity for young children ‐ Personal health and wellness ‐ Working with families to promote healthy behaviours Implementation strategies: ‐ Workshop: the childcare health consultants facilitated 5 x 1‐hour NAPSACC workshops for child care providers and other staff (e.g. cooks, administrators) at each of the intervention services on i) childhood obesity; ii) healthy eating for young children; iii) physical activity for young children; iv) personal health and wellness; and iv) working with families to promote healthy behaviours ‐ Consultation: childcare health consultants provided at least monthly on‐site consultations and additional phone or email consultations and materials and resources (posters and information sheets on nutrition and physical activities). The childcare health consultants conducted a mean of 11 on‐site visits and 8 off‐site consultations per service over the 7‐month intervention, in addition to the provider and parent workshops. ‐ Policy support: childcare health consultants worked with the service managers to write or update the service nutrition and physical activity policies ‐ Parent workshop: 7 of the intervention services also received the parent workshop “Raising Healthy Kids” Who delivered the intervention: previously trained nurse childcare health consultants Theoretical underpinning: not reported Description of control: delayed NAPSACC intervention in year 2 of the study |
|
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: Service nutrition and physical activity policies: Data collection method: Californian Childcare Health Programme Health and Safety Checklist (CHPHSPC) completed by blinded research assistants and used to determine if the service’s written policies adhered to national guidelines Validity of measures used: unclear ‐ this policy measurement technique was used in another study and was shown to be a valid measure of the effect of childcare health consultant interventions on childcare service environments Provider nutrition and physical activity practices: Data collection method: modified version of the Environment and Policy Assessment and Observation (EPAO) was completed by a research assistant. Mean scores for the nutrition and physical activity scales were calculated for each service then aggregated by intervention and control services Validity of measures used: although these items were modified from a reliable instrument, they were not previously validated in the format included in this study Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: Child physical activity: Data collection method: the Observation System for Recording Activity in Preschools (OSRAP) ‐ Data collection was completed by a trained research assistant. Children were observed in 15‐second intervals for a total of 12 to 16 minutes per child; the observations were conducted over an 8‐hour day. Data were aggregated as the mean percentage of physical activity intensity (1 = stationary to 5 = fast) Validity of measures used: the OSRAP has been validated and has been compared favourably with accelerometer data Child weight status: Data collection method: BMI z‐score ‐ the research assistants used a portable foldable stadiometer to measure height and a digital scale to measure weight. Pre/post BMI z‐score and % underweight, healthy weight, overweight and obese children Validity of measures used: unclear – appears to be an objective measure | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors indicate that the services were randomly assigned to treatment groups, but the sequence generation procedure was not described. One control group service that was not able to adequately complete baseline data collection was replaced by a matched service (unclear if this was randomly chosen). |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessment was undertaken by blinded research personnel and therefore the risk of detection bias is considered to be low. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete data collected for all services (8 control and 9 intervention), with no services excluded from the analysis ‐ therefore risk of attrition bias is considered to be low. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it is unclear whether there was selective outcome reporting. |
| Recruitment to cluster | Low risk | Selection of participants from each service for measurement of child diet, physical activity and BMI outcomes was random, so risk of bias through selection to cluster is considered to be low. |
| Baseline imbalance | Unclear risk | There is baseline imbalance in parent and child care provider characteristics but they adjust for some of these in the analysis. |
| Loss of clusters | Unclear risk | In the control group replaced 1 cluster with a matched cluster and then merged 2 clusters (services that came under same management) for analysis. |
| Incorrect analysis | Low risk | Hierarchical linear models conducted to assess child‐level BMI z‐score outcomes (accounting for clustering within the service). |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Other bias | Unclear risk | — |
Bell 2014
| Methods | Study design: quasi‐experimental trial Intervention duration: average of 22 months between initiation of intervention and collection of follow‐up data Length of follow‐up from baseline: average 22 months (between initiation of intervention and collection of follow‐up data) Differences in baseline characteristics: reported Unit of allocation: childcare service Unit of analysis: childcare service | |
| Participants |
Service type: preschools and long daycare services Region: Intervention: Hunter New England region, New South Wales, Australia; Control: New South Wales, Australia Demographic/socioeconomic characteristics: Intervention: the Hunter New England region ‐ a geographically large area (130,000 km2) with a demographically diverse population including metropolitan urban and suburban areas, regional services, and rural and isolated remote communities. The region included pockets of wealth and poverty, and an overall socioeconomic status lower than the New South Wales state average. Control: not reported Inclusion/exclusion criteria: all services located within the intervention region were invited to participate. Services were excluded that catered for children with special needs such as intellectual or physical disabilities. Number of services randomised: 583 (287 intervention, 296 control) Numbers by trial group: n (control baseline) = 251 n (control follow‐up) = 191 n (intervention baseline) = 261 n (intervention follow‐up) = 240 Recruitment: Intervention: all services (n = 287) located within the intervention region were invited to participate. Control: a simple random sample of eligible centre‐based childcare services in all other regions of the state of New South Wales were invited to participate in the study as the comparison group (n = 296) Recruitment rate: Intervention: 91%; Control: 85% |
|
| Interventions | Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: Healthy eating policies and practices of childcare services including: ‐ Staff training in nutrition ‐ Policy guiding the content of food and drinks provided to children by the service ‐ Policy guiding the content of food and drinks packed for children by parents ‐ Provision of non‐sweetened drinks (milk and water) only to children during care ‐ Parent participation in nutrition policy or programmes ‐ Provision of foods to children consistent with dietary guidelines (for services that provide meals to children) and accreditation requirements Implementation strategies: ‐ Identifying leaders and obtaining their support and endorsement of the programme and targeted policy and practices ‐ Provision of professional development for staff (2 x 6‐hour workshops (1 for staff and service managers, 1 for cooks and service managers) ‐ Small incentives ‐ Resource provision ‐ Performance monitoring and feedback ‐ Follow‐up support (20‐minute phone call once, 5 newsletters) Who delivered the intervention: the intervention was delivered by health service staff who worked with regional representatives of the Department of Community Services and childcare service staff to implement the intervention strategies Theoretical underpinning: the intervention was based on practice change and capacity‐building theoretical frameworks Description of control: from July 2008 onwards, preschool services (not including long daycare services) in New South Wales were able to access implementation support via a government‐supported programme that aimed to promote physical activity and healthy eating for children | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: Service healthy eating policies and practices: ‐ Staff with nutrition training ‐ Services with a policy guiding the content of food and drinks provided to children by the service ‐ Services with a policy guiding the content of food and drinks packed for children by parents ‐ Services providing only water or plain milk to children ‐ Parent participation in nutrition policy or programmes Data collection method: computer‐assisted telephone interview with service managers Validity of measures used: not reported Nutritional quality of lunch menus: ‐ Number of times processed foods high in fat, salt and/or sugar were listed on the menu each day ‐ Number of times sweetened drinks were listed on the menu each day ‐ Number of times water was listed on the menu each day ‐ Number of ‘child size’ servings of fruit listed on the menu each day ‐ Number of ‘child size’ servings of vegetables listed on the menu each day Classification into the following categories: ‐ No high‐fat, ‐salt and/or ‐sugar processed food menu items ‐ No sweetened drink menu items ‐ Water with every eating occasion ‐ 1 child‐size serving of fruit listed on the menu each day ‐ The number of child‐size servings of vegetables listed on the menu each day Data collection method: all services were invited to submit a copy of their current 2‐week menu Validity of measures used: not reported Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: not applicable | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐experimental design. High risk of selection bias as intervention services were recruited from a selected area. Control services were randomly selected from a comparison region. There were no details provided regarding the sequence generation procedure used to randomise control services for selection. |
| Allocation concealment (selection bias) | High risk | Quasi‐experimental design. Intervention services were recruited from a selected area, therefore high risk of bias as no concealment of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported policies and practices. There was no blinding of research personnel or participants (service managers) and due to the self‐report of this outcome, risk of bias is considered to be high. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There was a large difference in the proportion of services followed up amongst intervention and control groups and the proportion that provided a menu for assessment: Intervention group: 91% of services surveyed at baseline were followed up and 61% provided a menu Control group: 76% of services from the control area (NSW) were followed up and 49% provided a menu Due to the magnitude of difference in the proportions of participants followed up between groups, the risk of bias is assessed as high |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it is unclear whether there was selective outcome reporting. |
| Potential confounding | Unclear risk | Authors state that "Characteristics of services were not adjusted for in the logistic regression model as we were looking at change within services and the baseline score of the services effectively controlled for potential differences in baseline characteristics between the two regions." It is unknown whether this was adequate to reduce bias due to known confounders. |
| Other bias | Unclear risk | — |
Benjamin 2007
| Methods | Study design: cluster‐randomised controlled trial (counties randomly allocated into either the intervention (n = 6) or comparison (n = 2) group; all eligible services were approached and services enrolled on a first‐come first‐served basis) Intervention duration: 6 months Length of follow‐up from baseline: approximately 10 months (assessments occurred 4 months after the 6‐month intervention) Differences in baseline characteristics: not reported Unit of allocation: county Unit of analysis: childcare service | |
| Participants |
Service type: childcare centres Region: North Carolina, USA Demographic/socioeconomic characteristics: not reported Inclusion/exclusion criteria: inclusion criteria: size of the childcare service (between 20 and 150 children); participation in the Child and Adult Care Food Program; rating of 3, 4 or 5 stars on the NC1‐5 Star Rating System for quality child care. Exclusion criteria: open case of child abuse or neglect; service provided services to a special population of children only; Head Start service; classified as a family child care home Number of services randomised: 19 (15 intervention, 4 control) Numbers by trial group: n (control baseline) = 4 n (control follow‐up) = 4 n (intervention baseline) = 15 (2 intervention services withdrew because their manager had left their position) n (intervention follow‐up) = 13 Recruitment: convenience sampling – the North Carolina childcare regulatory agency provided a list of eligible childcare services for each intervention and comparison county. 2 services were selected per county, except for 1 large county where 5 services participated. Recruitment rate: not reported |
|
| Interventions | Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: NAPSACC programme. The programme focused on 15 nutrition and physical activity areas. Nutrition areas of focus included: fruits and vegetables; fried food and high‐fat meats; beverages; menus and variety; meals and snacks; food items outside of regular meals and snacks; supporting healthful eating; nutrition education for children, parents and staff; and nutrition policy. Key physical activity areas of focus included: active play and inactive time; TV use and TV viewing; play environment; supporting physical activity; physical activity education for children, parents and staff; and physical activity policy. Implementation strategies: ‐ Self‐assessment: childcare service managers, with assistance from key service staff, completed the self‐assessment instrument to identify current service nutrition and physical activity policies and practices ‐ Action plan: NAPSACC trained childcare health consultants worked with the services to develop an action plan to improve at least 3 areas identified from the self‐assessment instrument. Childcare service managers were asked to select their priority areas for improvement in order to facilitate the most fitting and lasting environmental changes at the service. ‐ Workshops: the trained childcare health consultants delivered 3 x 30‐minute workshops on being overweight, healthful eating and physical activity ‐ Provision of technical assistance: ongoing technical assistance (visits and calls) were provided by the childcare health consultants to service managers to support policy and practice changes Who delivered the intervention: NAPSACC trained childcare health consultants Theoretical underpinning: NAPSACC is a theory‐based programme that employs components of social cognitive theory against a backdrop of the socio‐ecological framework. The inherent relationship between environment and behaviour has proven useful in intervention research. Social cognitive theory identifies several factors that influence behaviour change, including expectancies, observational learning, self‐efficacy, behavioural capability, reinforcement and reciprocal determinism, which were all principles used to guide the NAPSACC intervention. Description of control: the comparison services did not receive any training or technical assistance from a childcare health consultant but completed only the pre‐ and post‐self‐assessment instrument. | |
| Outcomes |
Outcome relating to the implementation of childcare service policies, practices or programmes: Total nutrition and physical activity score assessed using the self‐assessment instrument, which included 29 nutrition and 15 physical activity questions with either a demonstrated or a perceived relationship to childhood overweight. Each question had 3 response categories, assigned 1, 2 or 3 points (1 = minimum standard, 2 = good, 3 = best practice) Data collection method: self‐assessment instrument Validity of measures used: not established at time of study ‐ additional work tests the reliability and validity of the NAPSACC self‐assessment instrument in a sample of childcare services Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: not applicable |
|
| Notes | Given the small sample size (n = 4) in the comparison group, no between‐group comparisons were made | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Counties were matched and randomly allocated to control or intervention groups. The sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | Unclear as to whether concealment of allocation occurred. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐assessment conducted by childcare service staff for nutrition and physical activity policies and practices. No blinding of research personnel or participants (service managers) and due to the self‐report of this outcome the risk of bias is considered high. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 17 of the 19 intervention group services had full data available and 4 of 4 control services. No information is provided on the characteristics of the services that dropped out, nor sensitivity analysis undertaken to test assumptions regarding missing data. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it is unclear whether there was selective outcome reporting. |
| Recruitment to cluster | Unclear risk | All services within the county invited to participate and chosen to participate on first‐come basis – 2 per county, but 1 county was given permission to have 5 services participate. |
| Baseline imbalance | Unclear risk | A convenience sample of 6 intervention and 2 comparison counties, matched on urban/rural status randomly allocated to intervention or comparison group. Unclear if baseline characteristic imbalances are present as this was not reported. Outcome measures at baseline were similar. |
| Loss of clusters | Unclear risk | Unclear whether the 2 lost services were from the same county. |
| Incorrect analysis | High risk | No statistical analysis completed due to small sample size. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Other bias | Unclear risk | — |
Finch 2012
| Methods | Study design: quasi‐experimental study Intervention duration: 3 months (staggered) Length of follow‐up from baseline: 18 months (follow‐up was conducted approximately 12 months after the initiation of the intervention with wave 1 services, and approximately 6 months after the initiation of the intervention for wave 2 services) Differences in baseline characteristics: reported Unit of allocation: childcare service Unit of analysis: childcare service | |
| Participants |
Service type: long daycare services and preschools Region: Intervention: Hunter New England region, New South Wales, Australia; Control: New South Wales, Australia Demographic/socioeconomic characteristics: Intervention: the intervention region included a large non‐metropolitan area (more than 130,000 km2) encompassing urban and rural communities with a population of 60,970 children aged 0 to 5 years. Control: the comparison region of New South Wales had an area of 801,305 km2 and included major cities, inner regional services, outer regional services, remote and very remote areas. New South Wales has a population of 506,095 children aged 0 to 5 years Inclusion/exclusion criteria: inclusion criteria: long daycare services and preschools in the Hunter New England area (intervention group) or the remainder of New South Wales (comparison group) as recorded by the licensing agency for such services. Exclusion criteria: services catering solely for children with special needs such as intellectual or physical disabilities Number of services randomised: 484 services participated in baseline measures. Intervention: 275 (not randomised, those services approached who agreed to participate and completed baseline data collection). Control: 209 (of those randomly approached and who took part in baseline evaluation). Numbers by trial group: n (control baseline) = 209 n (control follow‐up) = 164 n (intervention baseline) = 275 n (intervention follow‐up) = 228 Recruitment: Intervention: all services (n = 338) located within the intervention region were invited to participate. Control: a simple random sample of eligible centre‐based childcare services in all other regions of the state of New South Wales were invited to participate in the study as the comparison group (n = 298). Recruitment rate: Intervention: 81%; Control: 83% |
|
| Interventions | Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: ‐ Physical activity policy ‐ Conducting daily fundamental movement sessions with recommended components ‐ Time spent on structured physical activities ‐ All staff usually participate in free active play ‐ All staff usually provide verbal prompts for physical activity ‐ Children are allowed to watch small screen recreation less than once per week ‐ Children participate in seated activities for no longer than 30 minutes at a time ‐ Staff trained in physical activity Implementation strategies: ‐ Offer of staff training (1 x 6‐hour workshop) ‐ Offer of information programme resources and instructional materials: ‐ Offer of follow‐up support (2 x 15‐minute support calls, 2 support emails/faxes, 6 project newsletters) ‐ Provision of performance monitoring and feedback regarding policy and practice adoption ‐ Offer of incentives Who delivered the intervention: the staff training was delivered by external experts and follow‐up support and performance monitoring and feedback (telephone) was delivered by health service staff Theoretical underpinning: not reported Description of control: ‐ Childcare service staff were invited to attend a full day workshop provided by a non‐government organisation ‐ Provision of a printed resource folder ‐ Provision of a small financial grant to support staff attendance at training or the purchase of equipment ‐ Opportunity for additional support strategies to be provided by local health services at their discretion | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: ‐ Services with a physical activity policy that referred to: ‐ Child fundamental movement skills development ‐ Limits on small screen recreation and TV ‐ Physical activity training for staff ‐ Services conducting daily fundamental movement sessions with recommended components ‐ Time spent on structured physical activities ‐ Services where all staff usually participate in free active play (role modelling) ‐ Services where all staff usually provide verbal prompts for physical activity ‐ Services where children are allowed to watch small screen recreation less than once per week ‐ Services where children participate in seated activities for no longer than 30 minutes at a time ‐ Services with staff trained in physical activity Data collection method: service manager self‐report via computer‐assisted telephone interview Validity of measures used: unclear (developed following review of existing validated tools and pre‐tested prior to use) Outcome relating to staff knowledge, skills or attitudes: Service manager knowledge of: ‐ The recommended time children should be sedentary ‐ Child physical activity recommendations ‐ The recommended maximum time children should watch television Data collection method: service manager self‐report via computer‐assisted telephone interview Validity of measures used: unclear Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: not applicable | |
| Notes | The study had multiple outcomes but did not appear to adjust the P value for multiple comparisons | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐experimental design. High risk of selection bias as the intervention services were recruited from a selected area. Control services were randomly selected from a comparison region. No detail is provided regarding the sequence generation procedure used to randomise control services for selection. Table 2 shows that services within the intervention and comparison sites differed significantly in terms of socio‐economic areas, geographic locality and services with children of an Aboriginal background. |
| Allocation concealment (selection bias) | High risk | Quasi‐experimental design. Intervention services were recruited from a selected area, therefore high risk of bias as there was no concealment of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation, however, as the control group may have also received some form of intervention, systematic bias between groups in terms of performance bias is unknown. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported physical activity policies and practices. No blinding of research personnel or participants (service managers) and due to the self‐report of this outcome, the risk of bias is considered to be high. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 83% of intervention group services included in final post‐test data analysis; 78% of comparison group services included in final post‐test data analysis. While these proportions are similar, it is unclear whether the services lost to follow‐up differed between groups. No sensitivity analysis reported to test assumptions regarding missing data. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it is unclear whether there was selective outcome reporting. |
| Potential confounding | Unclear risk | Authors state that "Characteristics of services were not adjusted for in the logistic regression model as we were looking at change within services and the baseline score of the services effectively controlled for potential differences in baseline characteristics between the two regions." It is unknown whether this was adequate to reduce bias due to known confounders. |
| Other bias | Unclear risk | — |
Finch 2014
| Methods | Study design: cluster‐randomised controlled trial Intervention duration: 7 months Length of follow‐up from baseline: 8 months Differences in baseline characteristics: reported Unit of allocation: childcare service Unit of analysis: childcare service (child physical activity was assessed at the level of the individual) | |
| Participants |
Service type: centre‐based long daycare services Region: Hunter region, New South Wales Demographic/socioeconomic characteristics: the Hunter region encompasses non‐metropolitan ‘major cities’ and ‘inner regional’ areas with 14,061 children aged 3 to 5 years residing in the area. 5% of residents speak languages other than English and 2% of residents are of Aboriginal or Torres Strait Islander origin. The Hunter region has lower indices of socioeconomic status than the New South Wales state average. Inclusion/exclusion criteria: inclusion criteria: centre‐based long daycare services (providing care for a minimum of 8 hours a day). Services were required to have at least 25 enrolled children aged between 3 to 5 years. Children aged 3 to 5 years attending participating services were eligible for the study if they attended on the day of the week nominated by the service manager for baseline data collection. Number of services randomised: 20 services (10 intervention (242 children), 10 control (215 children) Numbers by trial group: n (controls baseline) = 10 services n (controls follow‐up) = 10 services n (interventions baseline) = 10 services n (interventions follow‐up) = 10 services Recruitment: a total of 70 childcare services in the study region served as the sampling frame Recruitment rate: 54% |
|
| Interventions | Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: ‐ Fundamental movement skill development activity sessions ‐ Staff delivery of structured physical activity ‐ Staff role modelling of active play and delivery of verbal prompts ‐ Limiting small screen recreation and sedentary time ‐ Providing children with a physical activity‐promoting indoor and outdoor physical environment ‐ Physical activity policy Implementation strategies: ‐ Staff training (6‐hour workshop for childcare service staff) ‐ Provision of resources ‐ Follow‐up support (2 telephone support calls and a 2‐hour service visit) ‐ Performance feedback via project newsletter on 2 occasions ‐ Incentives ‐ Opinion leaders Who delivered the intervention: workshop and follow‐up component delivered by experts Theoretical underpinning: the multi‐level intervention was designed using the social ecological models of health behaviour change Description of control: wait list control group that did not receive the intervention or any intervention support or materials during the study period and were offered the intervention after collection of all follow‐up data | |
| Outcomes |
Outcome relating to the implementation of childcare service policies, practices or programmes: ‐ Fundamental movement skill development activity sessions ‐ Staff delivery of structured physical activity ‐ Staff role modelling of active play and delivery of verbal prompts ‐ Limiting small screen recreation and sedentary time ‐ Physical activity‐promoting resources and materials ‐ Portable equipment ‐ Physical activity policy Data collection method: observational audit ‐ EPAO was conducted by 2 trained research staff Validity of measures used: unclear – EPAO has reported high inter‐observer agreement but other psychometric properties of this tool are not reported Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: The number of child injuries recorded at the service in the month of data collection at baseline and follow‐up Data collection method: service manager self‐report via interview Validity of measures used: unclear Outcome relating to child diet, physical activity or weight status: Child step count: Data collection method: pedometer worn for 1 day during attendance at the childcare service Validity of measures used: a valid measure of physical activity in preschool age children |
|
| Notes | The trial had multiple outcomes but did not appear to adjust the P value for multiple comparisons | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number function in Microsoft Excel was used to generate random number sequence. |
| Allocation concealment (selection bias) | Low risk | Statistician not involved in the project allocated the services to groups using a computerised program. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Implementation of policies and practices measured using observational audit ‐ research staff undertaking audits were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Implementation of policies and practices ‐ no loss to follow‐up (10 intervention services; 10 control services). |
| Selective reporting (reporting bias) | Low risk | There are no unreported outcomes according to those planned in the published protocol. |
| Recruitment to cluster | Low risk | For the child physical activity measure, children were recruited by service managers at the service selecting a day of the week for measurement to occur. Allocation was not revealed to services until after baseline data collection. |
| Baseline imbalance | High risk | Baseline imbalance in services in areas of higher socio‐economic status (intervention 90%, control 60%) and average years of operation (intervention 8 years, control 20 years) and no mention of adjustment within analysis. |
| Loss of clusters | Low risk | 100% followed up. |
| Incorrect analysis | Low risk | Generalised linear mixed model accounting for children nested within services. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Other bias | Unclear risk | — |
Gosliner 2010
| Methods | Study design: randomised trial Intervention duration: not reported Length of follow‐up from baseline: 10 months Differences in baseline characteristics: not reported by group Unit of allocation: childcare service Unit of analysis: childcare service staff | |
| Participants |
Service type: childcare centres Region: California, USA Demographic/socioeconomic characteristics: childcare services were located in low‐income neighbourhoods in Northern California Inclusion/exclusion criteria: inclusion criteria: services that were already participating in a health education and policy development project (Child Health and Nutrition Service Enhancement) with the Contra Costa Child Care Council Number of services randomised: 18 (9 intervention, 9 control) Numbers by trial group: n (controls baseline) = 7 n (controls follow‐up) = 7 n (interventions baseline) = 6 n (interventions follow‐up) = 6 Recruitment: 9 pairs of eligible services were matched on city of location and programme size and were randomised to either the intervention or control group Recruitment rate: 84% entered the study |
|
| Interventions | Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: Nutrition and physical activity policies, children's food and physical activity environment Implementation strategies: ‐ Training and technical assistance regarding children's health and nutrition ‐ Received a set of nutrition and physical activity policies ‐ Staff wellness programme consisting of: ‐ Kick‐off wellness training with individual health consultations including education, individual health assessments ‐ Monthly newsletters and information with pay‐checks promoting healthy eating and physical activity ‐ Group walking programme with awards for reaching milestones ‐ Staff follow‐up support visits Theoretical underpinning: not reported Description of control: control services received training and technical assistance regarding children's health and nutrition and received a set of nutrition and physical activity policies | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: ‐ Staff providing fresh fruits in children’s meals and snacks more often during the past year ‐ Staff providing fresh vegetables in children’s meals and snacks more often during the past year ‐ Staff providing sweetened beverages in children’s meals and snacks more often during the past year ‐ Staff providing sweetened foods in children’s meals and snacks more often during the past year ‐ Staff providing fresh fruits in children’s celebrations more often during the past year ‐ Staff providing fresh vegetables in children’s celebrations more often during the past year ‐ Staff providing sweetened beverages in children’s celebrations more often during the past year ‐ Staff providing sweetened foods in children’s celebrations more often during the past year Data collection method: childcare service staff self‐report via questionnaire Validity of measures used: unclear Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: not applicable | |
| Notes | The study did not report baseline values for the implementation outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Services were matched on city of location and programme size and were randomised to intervention or control group. The sequence generation procedure was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Whether pending allocation was concealed is unclear as no information was provided on concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported by service managers, therefore high risk of bias due to managers being aware of allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data were available for 50 (56%) participants in the intervention group and 39 (44%) in the control group. Of those not returning at endpoint, most had changed employment (80%) or were on leave or vacation (14%). 7 intervention staff who reported participating in less than half of the intervention activities were considered inadequately exposed and were excluded from the analysis, leaving 43 staff in the intervention group. Therefore the intention‐to‐treat principle was not applied. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it is unclear whether there was selective outcome reporting. |
| Other bias | Unclear risk | — |
Hardy 2010
| Methods | Study design: cluster‐randomised controlled trial Intervention duration: 5 months Length of follow‐up from baseline: 5 months Differences in baseline characteristics: reported Unit of allocation: childcare service Unit of analysis: childcare service (staff knowledge and attitudes were assessed at the level of the individual) | |
| Participants |
Service type: preschools Region: Sydney, New South Wales, Australia Demographic/socioeconomic characteristics: not described Inclusion/exclusion criteria: inclusion criteria: preschools operating under the auspices of the New South Wales Department of Education and Training located in the Sydney, Western Sydney and South Western Sydney education regions of New South Wales Number of services randomised: 29 (15 intervention, 14 control) Numbers by trial group: n (controls baseline) = 14 n (controls follow‐up) = 14 n (interventions baseline) = 15 n (interventions follow‐up) = 15 Recruitment: all eligible preschools were invited to participate in the study (n = 61) Recruitment rate: 48% |
|
| Interventions | Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: 'Munch and Move' programme: ‐ Healthy eating and ways of incorporating food‐based activities into the education programme ‐ Physical activity and ways of incorporating fun, games‐based skills activities into the programme ‐ Strategies to encourage children to limit their recreational screen time ‐ Providing opportunities for children to engage in unstructured physically active play ‐ Developing and implementing healthy nutrition and physical activity fundraising policies Implementation strategies: ‐ 1‐day professional development workshop for up to 2 staff, delivered by a specialised early childhood training organisation ‐ Resources for preschools that included a manual and a small grant to support staff to attend training or purchase physical activity equipment for the service ‐ Contact with health promotion professionals from the local health service, to provide additional advice to preschools to support the delivery of the programme including 2 visits post‐workshop Who delivered the intervention: experts and health service staff Theoretical underpinning: not reported Description of control: control preschools received health information on unrelated topics (road safety and sun safety) during the intervention period | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: ‐ Structured play time (minutes per session) ‐ Frequency of structured play (sessions per week) ‐ Unstructured play time (minutes per session) ‐ Frequency of unstructured play (sessions per week) ‐ Fundamental movement skill activities (minutes per session) ‐ Frequency of fundamental movement skill activities (sessions per week) ‐ Conduct of food‐based activities ‐ Rules concerning food and drink brought in from home ‐ Food policies ‐ Communicating food rules and policies to parents Data collection method: interview with the service manager Validity of measures used: unclear Outcome relating to staff knowledge, skills or attitudes: Knowledge of recommended guidelines for children: ‐ Daily serves of fruit ‐ Daily serves of vegetables ‐ Recreational screen time (TV/DVDs) (hours per day) Attitudes (agreement with statement): ‐ Teachers do not need to act as role models for being active ‐ It is not the role of the teacher to teach movement skills ‐ It is not important that children participate in structured active play ‐ Safety concerns limit active play opportunities in the preschool setting ‐ It is not the role of the teacher to teach about healthy eating ‐ Parents should be able to send any type of food to school with their child ‐ It is alright to sell chocolates and sweets for fundraising Data collection method: childcare service staff self‐report via questionnaire Validity of measures used: unclear Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: not applicable | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The procedure for random sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Whether pending allocation was concealed is unclear as no information is provided on concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Policies and practices ‐ self‐reported by service managers in interviews with research staff, therefore high risk of bias due to managers being aware of allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All service managers followed up in both groups ‐ therefore low risk of bias for outcome regarding implementation of policies and practices. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it is unclear whether there was selective outcome reporting. |
| Recruitment to cluster | Low risk | All parents of participating services were invited to allow their children to participate. |
| Baseline imbalance | Unclear risk | Unclear response rate of children in each group – imbalance in numbers of students (intervention 263, control 167); some imbalances in baseline characteristics (mean years teaching experience: intervention 4.5 years, control 6 years; teacher’s aide: intervention 11.1 years, control 8.9 years; children attending 2 days per week: intervention 22%, control 11%; children attending 3 days per week: intervention 21%, control 42%; English speaking: intervention 58%, control 41%) – unknown if any were significant. Adjustment of some characteristics in analysis. |
| Loss of clusters | Low risk | No loss of clusters. |
| Incorrect analysis | Low risk | CSPlan procedure used to allow for clustering within service class. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Other bias | Unclear risk | — |
Johnston Molloy 2013
| Methods | Study design: randomised parallel‐group trial Intervention duration: not specified Length of follow‐up from baseline: not specified Differences in baseline characteristics: not reported Unit of allocation: childcare service Unit of analysis: childcare service | |
| Participants |
Service type: preschools Region: Republic of Ireland Demographic/socioeconomic characteristics: preschools were situated in towns, villages and the countryside across 4 midland counties in a geographical area defined as disadvantaged Inclusion/exclusion criteria: inclusion criteria: preschools providing a "full day care service" (i.e. for more than 5 hours per day). Exclusion criteria: preschools that provided only sessional (less than 3.5 hours per session) or part‐time care for children; preschools designated as ineligible by the Preschool Inspection Team due to insufficient standard in other pre‐defined areas of inspection; preschools that had not been inspected by the Preschool Inspection Team in the previous 12‐month period. Number of services randomised: 61 (30 intervention group 'manager trained', 31 intervention group 'manager and staff trained') Numbers by trial group: n (intervention group 'manager trained' baseline) = 30 n (intervention group 'manager trained' follow‐up) = 24 n (intervention group 'manager and staff trained' baseline) = 31 n (intervention group 'manager and staff trained' follow‐up) = 18 Recruitment: convenience sampling was undertaken. An up‐to‐date list of preschools (n = 100) providing a 'full daycare service' was obtained and these preschools were invited to participate Recruitment rate: 61% |
|
| Interventions | Number of experimental conditions: 2 (intervention group 'manager trained', intervention group 'manager and staff trained') Policies, practices or programmes targeted by the intervention: ‐ Adequate meal and snack composition ‐ Healthy foods and fluids ‐ Appropriate serving size provision ‐ Family‐style food service ‐ Healthy preschool policy development Implementation strategies: Intervention 'manager trained': ‐ 1‐hour manager training session with a research dietitian ‐ Provision of resources (Preschool Nutrition and Health Education Resource) and best practice criterion (Preschool Health Promotion Activity Scored Evaluation Form) ‐ Provision of individualised 'written feedback record' from a pre‐intervention observation visit, suggested strategies for improvement discussed with the manager Who delivered the intervention: dietitians Theoretical underpinning: not reported Implementation strategies: Intervention 'manager and staff trained': ‐ 1‐hour manager training session with a research dietitian ‐ 1.5‐hour structured staff education session with a research dietitian including presentation, group work exercises and discussion ‐ Provision of resources (Preschool Nutrition and Health Education Resource) and best practice criterion (Preschool Health Promotion Activity Scored Evaluation Form) ‐ Provision of individualised 'written feedback record' from a pre‐intervention observation visit and suggested strategies for improvement discussed with the manager and staff Who delivered the intervention: dietitians Theoretical underpinning: adult learning methodologies | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: ‐ Environment ‐ Food service ‐ Meals ‐ Snacks ‐ Overall score Data collection methods: 1 day observation, preschool manager self‐report Validity of measures used: used the validated Preschool Health Promotion Activity Scored Evaluation Form Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: not applicable | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random‐number table was used to allocate services to treatment groups. |
| Allocation concealment (selection bias) | Low risk | We assumed that allocation was conducted in a single, automated process via the random‐number table and therefore allocation could not be pre‐empted. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to nature of the intervention (training), childcare service staff and study personnel delivering the intervention were not blind to study allocation, however as both groups received some form of intervention it is unknown if there is a systematic difference in the potential for performance enhancement and therefore bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided on whether the individuals conducting the outcome assessment (audits) were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of 31 services allocated to the 'manager and staff training' intervention, only 18 received the intervention and had follow‐up data collected. Of the 30 services allocated to the 'manager training' group, 27 received the intervention and 24 had follow‐up data collected. Although data are provided to demonstrate no significant difference between those who participated and did not, this analysis is conducted for all services, not by group. Rated as high risk of bias due to the magnitude of differences in participants lost to follow‐up between groups. |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial protocol or trial registration so it is unclear whether there was selective outcome reporting. |
| Other bias | Unclear risk | — |
Ward 2008
| Methods | Study design: randomised controlled trial Intervention duration: 6 months Length of follow‐up from baseline: 6 months Differences in baseline characteristics: reported Unit of allocation: childcare service Unit of analysis: childcare service | |
| Participants |
Service type: childcare centres Region: North Carolina, USA Demographic/socioeconomic characteristics: not described Inclusion/exclusion criteria: inclusion criteria: current enrolment of 15 to 150 children. Exclusion criteria: services with an open case of abuse or neglect or served only a special population. Number of services randomised: 84 (56 intervention, 26 control, 2 excluded following randomisation) Numbers by trial group: n (controls baseline) = 26 n (controls follow‐up) = 26 n (interventions baseline) = 56 n (interventions follow‐up) = 56 Recruitment: all childcare health consultants working in North Carolina were invited to participate. A convenience sample was selected by recruiting the first 30 childcare health consultants (only 1 per county) who indicated an interest in participation, worked with at least 3 childcare services meeting eligibility requirements, and had not participated in the previous pilot project. Recruitment rate: not reported |
|
| Interventions | Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: NAPSACC programme. Best practices for the promotion of proper nutrition and regular physical activity at childcare. The programme focused on 15 nutrition and physical activity areas. Nutrition areas of focus included: fruits and vegetables; fried food and high‐fat meats; beverages; menus and variety; meals and snacks; food items outside of regular meals and snacks; supporting healthful eating; nutrition education for children, parents and staff; and nutrition policy. Key physical activity areas of focus included: active play and inactive time; TV use and TV viewing; play environment; supporting physical activity; physical activity education for children, parents and staff; and physical activity policy Implementation strategies: ‐ Provision of educational materials ‐ Self‐assessment instrument completed by service managers ‐ Action planning to improve at least 3 target areas identified from the self‐assessment ‐ Education workshops on child being overweight, healthy eating and physical activity for children delivered by childcare health consultants ‐ Provision of technical assistance to service staff via in‐person visits and telephone contact ‐ Re‐assessment using the self‐assessment tool Who delivered the intervention: trained childcare health consultants Theoretical underpinning: social cognitive theory against a social‐ecologic framework Description of control: delayed intervention control group | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: ‐ Total nutrition score ‐ Total physical activity score Data collection method: EPAO tool including 1‐day observation and a review of pertinent service documents conducted by trained observers. 75 items were selected to evaluate the impact of the intervention. All 75‐item responses were converted to a 3‐point scale (0, 1 and 2), averaged within a given subscale, and multiplied by10, with the average of all subscale scores representing total nutrition and physical activity scores. Validity of measures used: not established at time of study ‐ additional work tests the reliability and validity of the NAPSACC self‐assessment instrument in a sample of childcare services Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: not applicable | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided on the method for generating random sequence for allocation of childcare health consultants to treatment groups. |
| Allocation concealment (selection bias) | Unclear risk | No information provided on concealment of allocation of childcare health consultants to groups. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blind to group allocation of services and the tool used was observational. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 82 of 84 services recruited were followed up ‐ 2 services were lost to follow‐up due to closure. |
| Selective reporting (reporting bias) | Unclear risk | Authors state that the outcome measures were determined a priori but unknown if these are listed in a study protocol or trial registry. |
| Other bias | Unclear risk | — |
Williams 2002
| Methods | Study design: quasi‐experimental trial Intervention duration: 3 years Length of follow‐up from baseline: 6 months, 18 months Differences in baseline characteristics: not reported Unit of allocation: childcare service Unit of analysis: childcare service (child diet and weight status was assessed at the level of the individual) | |
| Participants |
Service type: Head Start Services ‐ preschools Region: Upstate New York, USA Demographic/socioeconomic characteristics: low‐income, predominantly minority preschool children Inclusion/exclusion criteria: not reported Number of services randomised: 9 (3 intervention: food service modification plus classroom education with nutrition modules, 3 intervention: food service modification plus classroom safety education, 3 control) Numbers by trial group: n (controls baseline) = 3 n (controls follow‐up) = 3 n (interventions: food service modification plus classroom education baseline) = 3 n (interventions: food service modification plus classroom education follow‐up) = 3 n (interventions: food service modification plus classroom safety education baseline) = 3 n (interventions: food service modification plus classroom safety education follow‐up) = 3 Recruitment: not reported Recruitment rate: not reported |
|
| Interventions | Number of experimental conditions: 3 (intervention: food service modification plus classroom education with nutrition modules, intervention: food service modification plus classroom safety education, control) Policies, practices or programmes targeted by the intervention: Food service modification: ‐ Achieving a 5 day a week meal/snack plan that provided no more than 30% energy from total fat and no more than 10% energy from saturated fat ‐ Increased offering of fruit, vegetables, breads and grains in meals, decreased total and saturated fat content of foods purchased for the service and decreased total and saturated fat due to alterations in food preparation techniques Implementation strategies: Intervention: food service modification plus classroom education with nutrition modules: ‐ Healthy Start Comprehensive Preschool Health Education Curriculum ‐ core curriculum plus nutrition‐related units ‐ 1‐day training programme for cooks, which covered the major food service intervention areas: menu planning, recipe development, food purchasing and food preparation ‐ A list of objectives was developed together with the cooks ‐ Ongoing support from registered dietitian ‐ Manual, newsletters and incentives Intervention: food service modification plus classroom safety education: ‐ Healthy Start Comprehensive Preschool Health Education Curriculum ‐ core curriculum plus safety‐related unit ‐ 1‐day training programme for cooks, which covered the major food service intervention areas: menu planning, recipe development, food purchasing and food preparation ‐ A list of objectives was developed together with the cooks ‐ Ongoing support from registered dietitian ‐ Manual, newsletters and incentives Who delivered the intervention: registered dietitians Theoretical underpinning: not reported Description of control: Healthy Start Comprehensive Preschool Health Education Curriculum ‐ core curriculum plus safety‐related units | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: Change in service menu: ‐ kcal ‐ Total fat ‐ Saturated fat ‐ % kcal from total fat ‐ % kcal from saturated fat Data collection method: service menus were analysed for nutrient content by obtaining menus, recipes and food labels for 5 days at each data collection time point Validity of measures used: unclear Outcome relating to staff knowledge, skills or attitudes: not applicable Outcome relating to cost: not applicable Outcome relating to adverse consequences: not applicable Outcome relating to child diet, physical activity or weight status: Change in child school meal dietary intake: ‐ Energy (kcal) ‐ Total fat ‐ Saturated fat ‐ % kcal from total fat ‐ % kcal from saturated fat Data collection method: direct observation of children during attendance at the service with plate waste measurement to determine amounts of foods and beverages consumed Validity of measures used: the complete dietary intake assessment protocol was adapted from existing protocols proven to be reliable and valid Child weight status: Data collection method: measurements of child weight (using digital scale) and height (using telescopic measuring rod) obtained by trained staff. Weight to height ratio calculated at baseline and at 6 months Validity of measures used: unclear – appears to be an objective measure | |
| Notes | For the analysis, all services assigned to the food service intervention arm of the study were grouped together, as were the services assigned to the control condition | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No random allocation to control and intervention conditions (random allocation to 1 of 2 intervention conditions). |
| Allocation concealment (selection bias) | Unclear risk | Unclear as to whether concealment of allocation occurred. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | We assumed that due to the nature of the intervention childcare service staff and study personnel delivering the intervention were not blind to the study allocation and therefore there is a potential high risk of performance bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information is provided on whether research personnel undertaking menu assessment and other data collection were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Implementation data collected on all intervention (n = 6) and control services (n = 3) pre‐ and post‐intervention. |
| Selective reporting (reporting bias) | Low risk | Methodology paper also lists physiological measures ‐ these have been published elsewhere. |
| Potential confounding | Unclear risk | No information provided. |
| Other bias | Unclear risk | — |
BMI: body mass index EPAO: Environment and Policy Assessment and Observation NAPSACC: Nutrition and Physical Activity Self‐Assessment for Child Care OSRAP: Observation System for Recording Activity in Preschools RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adamo 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Adams 2012 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Agrawal 2012 | Non‐controlled study |
| Alhassan 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Alhassan 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Androutsos 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Antoine 2012 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Bammann 2007 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Battista 2014 | Non‐controlled study |
| Bellows 2007 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Bellows 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Benjamin 2008 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Bisceglie 2010 | Non‐controlled study |
| Bonis 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Bryars 2012 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Buscemi 2014 | Inappropriate participants |
| Carpenter 2010 | Non‐controlled study |
| Crowley 2009 | Non‐controlled study |
| Céspedes 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| D'agostino 1999 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Davis 2013 | Non‐controlled study |
| De Bock 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| De Craemer 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| De Silva‐Sanigorski 2010 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| De Silva‐Sanigorski 2011 | Inappropriate participants |
| De Silva‐Sanigorski 2012 | No baseline data |
| Duncan 2011 | Non‐controlled study |
| Endres 2003 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Falbe 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Farfan‐Ramirez 2011 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Ferrer 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Fitzgerald 2014 | Non‐controlled study |
| Fitzgibbon 2002 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Fitzgibbon 2005 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Fitzgibbon 2006 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Fitzgibbon 2011 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Foltz 2012 | Non‐controlled study |
| Foulkes 2014 | Non‐controlled study |
| Fritz 2007 | Non‐controlled study |
| Gallois 2011 | Non‐controlled study |
| Gannon 2013 | Non‐controlled study |
| Gannon 2014 | Non‐controlled study |
| Girardet 2009 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Goldberg 2010 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Goldfield 2012 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Goldfield 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Golley 2011 | Non‐controlled study |
| Graham 2008 | Inappropriate participants |
| Hammons 2013 | Non‐controlled study |
| Hanna 2012 | Inappropriate intervention |
| Harvey 2008 | Non‐controlled study |
| Helland 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Herbert 2013 | Non‐controlled study |
| Herman 2012 | Non‐controlled study |
| Isbell 2013 | Non‐controlled study |
| Jones 2010 | Inappropriate participants |
| Jouret 2009 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Kain 2012 | Inappropriate participants |
| Korwanich 2008 | No reporting of between‐group differences in implementation outcomes |
| Lent 2012 | Inappropriate participants |
| Lerner‐Geva 2015 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Manios 2012 | Non‐controlled study |
| Manios 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Mazzeo 2012 | Non‐controlled study |
| Metcalf 2012 | Non‐controlled study |
| Mier 2005 | Non‐controlled study |
| Mo‐suwan 1998 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Najjar 2013 | Non‐controlled study |
| NAPNAP 2006 | Non‐controlled study |
| Natale 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Nemet 2011 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Nemet 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Niederer 2009 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Niederer 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Organizational Research Services 2003 | Non‐controlled study |
| Page 2011 | Non‐controlled study |
| Partington 2012 | Non‐controlled study |
| Passehl 2004 | Non‐controlled study |
| Patel 2010 | Non‐controlled study |
| Peregrin 2001 | Non‐controlled study |
| Phillips 2004 | Non‐controlled study |
| Prosper 2009 | Inappropriate participants |
| Ramsay 2013 | Inappropriate intervention |
| Requena 2010 | Non‐controlled study |
| Roth 2011 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Roths 2002 | Non‐controlled study |
| Rudolf 2010 | Non‐controlled study |
| Sanigorski 2008 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Santos‐Beneit 2013 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Savage 2006 | Inappropriate participants |
| Schindler 2013 | Non‐controlled study |
| Schwarz 2013 | Non‐controlled study |
| Sekhobo 2012 | Inappropriate participants |
| Skouteris 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Small 2007 | Inappropriate participants |
| Smiciklas‐Wright 1978 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Stock 2007 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Stolley 2003 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Story 2012 | Inappropriate participants |
| Strauß 2011 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Summerbell 2012 | Non‐controlled study |
| Thibault 2010 | Non‐controlled study |
| Thomas 2012 | Inappropriate participants |
| Trost 2008 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Trost 2012 | Inappropriate participants |
| Van Stan 2013 | Non‐controlled study |
| Vanderwall 2012 | Inappropriate participants |
| Vasquez 2008 | Non‐controlled study |
| Verbestel 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Watt 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Whaley 2010 | Inappropriate participants |
| Wilken 2013 | Inappropriate participants |
| Williams 2009 | Non‐controlled study |
| Witt 2012 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Yin 2012 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Zask 2012 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
| Zhou 2014 | Inappropriate outcomes ‐ does not aim to improve implementation of a policy, practice or programme |
Characteristics of ongoing studies [ordered by study ID]
Baby NAPSACC Intervention Study
| Trial name or title | Baby NAPSACC Intervention Study |
| Methods | Study design: randomised trial |
| Participants |
Service type: childcare centres Region: North Carolina, USA Number of services participating: not specified |
| Interventions |
Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: not specified Implementation strategies: ‐ Service and family self‐assessment ‐ Targeted technical assistance provided by Baby NAPSACC consultant for providers and parents ‐ Training workshops for child care providers ‐ Parent outreach and support |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: change in childcare service policies and practices |
| Starting date | 2013 |
| Contact information | Sara Benjamin Neelon, sara.benjamin@dm.duke.edu |
| Notes | ClinicalTrials.gov Identifier: NCT01890681 |
Finch 2015
| Trial name or title | A pragmatic randomised controlled trial of an implementation intervention to increase healthy eating and physical activity‐promoting policies, and practices in centre‐based childcare services |
| Methods | Study design: randomised controlled trial |
| Participants |
Service type: childcare services (preschools and long daycare services) Region: Hunter New England region, New South Wales, Australia Number of services participating: 165 |
| Interventions |
Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: ‐ Having a service policy (nutrition, physical activity and small screen recreation) ‐ Service providing information to families (healthy eating, physical activity, small screen time and breast feeding, where relevant) ‐ Service providing structured and specific learning experiences about healthy eating at least 2 times per week ‐ Service supplying age‐appropriate drinks to children (only water and age‐appropriate milk) ‐ Service conducting fundamental movement skills activities for children aged 3 to 5 years every day to at least 90% of children ‐ Service limiting use of small screen recreation by children aged 3 to 5 years to only educational purposes and for learning experiences Implementation strategies: performance review intervention with other resources |
| Outcomes |
Outcome relating to the implementation of childcare service policies, practices or programmes: proportion of services implementing all of the recommended healthy eating and physical activity‐promoting practices |
| Starting date | 2013 |
| Contact information | Meghan Finch, meghan.finch@hnehealth.nsw.gov.au |
| Notes | Australian Clinical Trials Registry ACTRN12614000972628 |
Jones 2014
| Trial name or title | A randomised controlled trial of an intervention to facilitate the implementation of healthy eating and physical activity policies and practices in childcare services |
| Methods | Study design: randomised controlled trial |
| Participants |
Service type: childcare services (preschools and long daycare services) Region: Hunter region, New South Wales, Australia Number of services participating: 128 |
| Interventions |
Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: ‐ Written nutrition and physical activity policies ‐ Staff monitoring of children’s lunch boxes against written nutritional guidelines and provision of feedback to parents when a non‐compliant food is packed ‐ Provision of water or reduced fat milk only to children ‐ Staff role modelling of physically active play and healthy eating ‐ Staff provision of prompts and positive comments to children to encourage physical activity and healthy eating ‐ Provision of adult‐guided fundamental movement skill development activities ‐ Restriction of sedentary screen time Implementation strategies: ‐ Implementation support staff ‐ Executive support ‐ Consensus processes ‐ Staff training ‐ Academic detailing visits ‐ Performance monitoring and feedback ‐ Tools and resources ‐ Communications strategy |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: change in prevalence of services implementing all healthy eating and physical activity policies and practices |
| Starting date | 2012 |
| Contact information | Jannah Jones, jannah.jones@hnehealth.nsw.gov.au |
| Notes | Australian Clinical Trials Registry ACTRN12612000927820 |
The Healthy Start Study
| Trial name or title | A multilevel intervention to increase physical activity and improve healthy eating among young children (ages 3 to 5) attending early childcare centres: the Healthy Start Study |
| Methods | Study design: randomised controlled trial |
| Participants |
Service type: early childcare centre Region: Canada Number of services participating: not specified |
| Interventions |
Number of experimental conditions: 2 (intervention, control) Policies, practices or programmes targeted by the intervention: not specified Implementation strategies: ‐ Intersectoral partnerships that leads to promoting healthy weights in communities and childcare services ‐ The Healthy Start guide for educators ‐ Customized training ‐ Role modelling and monitoring ‐ An evidence‐based resource for both families and educators and supplementary resources from governmental partners ‐ Knowledge development and exchange ‐ Communication strategy |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programmes: early childcare centre practices and policies for physical activity and nutrition |
| Starting date | 2015 |
| Contact information | Holly Hallikainen, hlh664@mail.usask.ca |
| Notes | ClinicalTrials.gov Identifier: NCT02375490 |
NAPSACC: Nutrition and Physical Activity Self‐Assessment for Child Care
Contributions of authors
Luke Wolfenden and Jannah Jones led the development of the review. Debbie Booth developed the search strategy. All authors have contributed to the conception and conduct of the research. Jannah Jones, Luke Wolfenden, Christopher M Williams, Amanda J Williams, Kirsty Seward and Sze Lin Yoong screened titles and abstracts and determined study eligibility. Jannah Jones, Meghan Finch, Rebecca Wyse, Flora Tzelepis and Tameka Small extracted data from eligible trials. Melanie Kingsland and Flora Tzelepis assessed risk of bias. Luke Wolfenden and Jannah Jones led the drafting of the manuscript. All authors provided critical comment on drafts.
Sources of support
Internal sources
-
University of Newcastle, Australia.
Salary support for review authors
-
Hunter New England Population Health, Australia.
Salary support for review authors
-
Hunter Medical Research Institute, Australia.
Salary support for review authors
-
University of Melbourne, Australia.
Salary support for review authors
External sources
-
The Australian Prevention Partnership Centre, Australia.
This research was supported by The Australian Prevention Partnership Centre through the NHMRC partnership centre grant scheme (Grant ID: GNT9100001) with the Australian Government Department of Health, NSW Ministry of Health, ACT Health, HCF and the HCF Research Foundation.
Declarations of interest
Luke Wolfenden, Jannah Jones, Meghan Finch, Rebecca Wyse, John Wiggers, Kirsty Seward and Sze Lin Yoong are currently undertaking a series of randomised trials aiming to facilitate the implementation of healthy eating and physical activity policies and practices by childcare services. The authors have not received any benefit, in cash or kind, any hospitality, or any subsidy derived from any source perceived to have an interest in the outcome of the review. Christopher Williams, Melanie Kingsland, Flora Tzelepis, Amanda J Williams, Tameka Small, Vivian Welch and Debbie Booth declare no conflict of interest.
New
References
References to studies included in this review
- Alkon A, Crowley AA, Benjamin Neelon SE, Hill S, Pan Y, Nguyen V, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children's body mass index. BMC Public Health 2014;14(215):1‐13. [DOI: 10.1186/1471-2458-14-215] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell AC, Davies L, Finch M, Wolfenden L, Francis JL, Sutherland R, et al. An implementation intervention to encourage healthy eating in centre‐based child‐care services: impact of the Good for Kids Good for Life programme. Public Health Nutrition 2014;18(9):1610‐9. [DOI: 10.1017/S1368980013003364] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin SE, Ammerman A, Sommers J, Dodds J, Neelon B, Ward DS. Nutrition and physical activity self‐assessment for child care (NAP SACC): results from a pilot intervention. Journal of Nutrition Education and Behavior 2007;39(3):142‐9. [DOI: 10.1016/j.jneb.2006.08.027] [DOI] [PubMed] [Google Scholar]
- Finch M, Wolfenden L, Falkiner M, Edenden D, Pond N, Hardy LL, et al. Impact of a population based intervention to increase the adoption of multiple physical activity practices in centre based childcare services: a quasi experimental, effectiveness study. International Journal of Behavioral Nutrition and Physical Activity 2012;9(101):1‐13. [DOI: 10.1186/1479-5868-9-101] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch M, Wolfenden L, Morgan PJ, Freund M, Jones J, Wiggers J. A cluster randomized trial of a multi‐level intervention, delivered by service staff, to increase physical activity of children attending center‐based childcare. Preventive Medicine 2014;58:9‐16. [DOI: 10.1016/j.ypmed.2013.10.004] [DOI] [PubMed] [Google Scholar]
- Gosliner WA, James P, Yancey AK, Ritchie L, Studer N, Crawford PB. Impact of a worksite wellness program on the nutrition and physical activity environment of child care centers. American Journal of Health Promotion 2010;24(3):186‐9. [DOI: 10.4278/ajhp.080227l9] [DOI] [PubMed] [Google Scholar]
- Hardy LL, King L, Kelly B, Farrell L, Howlett S. Munch and Move: evaluation of a preschool healthy eating and movement skill program. International Journal of Behavioral Nutrition and Physical Activity 2010;7(80):1‐11. [DOI: 10.1186/1479-5868-7-80] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston Molloy C, Kearney J, Hayes N, Glennon Slattery C, Corish C. Pre‐school manager training: a cost‐effective tool to promote nutrition‐ and health‐related practice improvements in the Irish full‐day‐care pre‐school setting. Public Health Nutrition 2013;18(9):1554‐64. [DOI: 10.1017/S1368980013002760] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward DS, Benjamin SE, Ammerman AS, Ball SC, Neelon BH, Bangdiwala SI. Nutrition and physical activity in child care. Results from an environmental intervention. American Journal of Preventive Medicine 2008;35(4):352‐6. [DOI: 10.1016/j.amepre.2008.06.030] [DOI] [PubMed] [Google Scholar]
- Williams CL, Bollela MC, Strobino BA, Spark A, Nicklas TA, Tolosi LB, et al. "Healthy‐Start": outcome of an intervention to promote a heart healthy diet in preschool children. Journal of the American College of Nutrition 2002;21(1):62‐71. [DOI: 10.1080/07315724.2002.10719195] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Adamo KB, Barrowman N, Naylor PJ, Yaya S, Harvey A Grattan KP, et al. Activity Begins in Childhood (ABC) ‐ inspiring healthy active behaviour in preschoolers: study protocol for a cluster randomized controlled trial. Trials 2014;15(305):1‐12. [DOI: 10.1186/1745-6215-15-305] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams AK, LaRowe TL, Cronin KA, Prince RJ, Wubben DP, Parker T, et al. The Healthy Children, Strong Families intervention: design and community participation. Journal of Primary Prevention 2012;33(4):175‐85. [DOI: 10.1007/s10935-012-0275-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal T, Hoffman JA, Ahl M, Bhaumik U, Healey C, Carter S, et al. Collaborating for impact: a multilevel early childhood obesity prevention initiative. Family and Community Health 2012;35(3):192‐202. [DOI] [PubMed] [Google Scholar]
- Alhassan S, Nwaokelemeh O, Lyden K, Goldsby T, Mendoza A. A pilot study to examine the effect of additional structured outdoor playtime on preschoolers' physical activity levels. Child Care in Practice 2013;19(1):23‐35. [Google Scholar]
- Alhassan S, Whitt‐Glover MC. Intervention fidelity in a teacher‐led program to promote physical activity in preschool‐age children. Preventive Medicine 2014;69:S34‐6. [DOI] [PubMed] [Google Scholar]
- Androutsos O, Apostolidou E, Iotova V, Socha P, Birnbaum J, Moreno L, et al. Process evaluation design and tools used in a kindergarten‐based, family‐involved intervention to prevent obesity in early childhood. The ToyBox‐study. Obesity Reviews 2014;15(S3):74‐80. [DOI] [PubMed] [Google Scholar]
- Antoine B, Jerome B, Susi K, Pedro MV, Tanja K, Jardena P. Effects of a physical activity intervention in children attending child care (youp'la bouge program): a cluster‐randomized controlled trial. Obesity Facts 2012;5:55‐79. [Google Scholar]
- Bammann K, Peplies J, Pigeot I, Ahrens W. IDEFICS: A multicenter European project on diet‐ and lifestyle‐related disorders in children. Medizinische Klinik (Munich, Germany: 1983) 2007;102(3):230‐5. [DOI] [PubMed] [Google Scholar]
- Battista RA, Oakley H, Weddell MS, Mudd LM, Greene JB, West ST. Improving the physical activity and nutrition environment through self‐assessment (NAP SACC) in rural area child care centers in North Carolina. Preventive Medicine 2014;67:S10‐6. [DOI] [PubMed] [Google Scholar]
- Bellows LL. Development and Evaluation of Food Friends get Movin' with Mighty Moves (TM), a Physical Activity Program to Prevent Obesity in Low‐income Preschoolers. Colorado State University: Fort Collins, CO, 2007. [Google Scholar]
- Bellows LL, Johnson SL, Davies PL, Anderson J, Gavin WJ, Boles RE. The Colorado LEAP study: rationale and design of a study to assess the short term longitudinal effectiveness of a preschool nutrition and physical activity program. BMC Public Health 2013;13:1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin SE, Tate DF, Bangdiwala SI, Neelon BH, Ammerman AS, Dodds JM, et al. Preparing child care health consultants to address childhood overweight: a randomized controlled trial comparing web to in‐person training. Maternal and Child Health Journal 2008;12:662‐9. [DOI] [PubMed] [Google Scholar]
- Bisceglie R. Improving academics through better school health practices encouraging good nutrition and physical activity at school. NASN School Nurse 2010;25(5):226‐8. [DOI] [PubMed] [Google Scholar]
- Bonis M, Loftin M, Ward D, Tseng TS, Clesi A, Sothern M. Improving physical activity in daycare interventions. Childhood Obesity 2014;10:334‐41. [DOI] [PubMed] [Google Scholar]
- Bryars T, Mouttapa M, McMahan S, Park TS. Results of a school‐based obesity prevention program targeting early childhood students. Californian Journal of Health Promotion 2012;10:91‐102. [Google Scholar]
- Buscemi J, Odoms‐Young A, Stolley ML, Blumstein L, Schiffer L, Berbaum ML, et al. Adaptation and dissemination of an evidence‐based obesity prevention intervention: design of a comparative effectiveness trial. Contemporary Clinical Trials 2014;38:355‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter L, Silva‐Sanigorski A, Prosser L, Honisett S, Gibbs L, Swinburn B, et al. The impacts of the Kid's ‐ 'Go for your life' obesity prevention program in Australian preschools. Obesity Research and Clinical Practice 2010;4:S70. [Google Scholar]
- Céspedes J, Briceño G, Farkouh ME, Vedanthan R, Baxter J, Leal M, et al. Targeting preschool children to promote cardiovascular health: cluster randomized trial. American Journal of Medicine 2013;126(1):27‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley AA, Kulikowich JM. Impact of training on child care health consultant knowledge and practice. Pediatric Nursing 2009;35(2):93. [PubMed] [Google Scholar]
- D'agostino C, D'andrea T, Nix ST, Williams CL. Increasing nutrition knowledge in preschool children: the Healthy Start project, year 1. Journal of Health Education 1999;30(4):217‐21. [Google Scholar]
- Davis SM, Sanders SG, FitzGerald CA, Keane PC, Canaca GF, Volker‐Rector R. CHILE: an evidence‐based preschool intervention for obesity prevention in Head Start. Journal of School Health 2013;83:223‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock F, Genser B, Raat H, Fischer JE, Renz‐Polster H. A participatory physical activity intervention in preschools: a cluster randomized controlled trial. American Journal of Preventive Medicine 2013;45:64‐74. [DOI] [PubMed] [Google Scholar]
- Craemer M, Decker E, Verloigne M, Bourdeaudhuij I, Manios Y, Cardon G. The effect of a kindergarten‐based, family‐involved intervention on objectively measured physical activity in Belgian preschool boys and girls of high and low SES: the ToyBox‐study. International Journal of Behavioral Nutrition and Physical Activity 2014;11:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva‐Sanigorski A, Kremer P, Elea D, Boak R, Swinburn B. Romp & Chomp: Improving young children's eating and activity behaviours through an environmental intervention in family day care. Obesity Reviews 2010;11:59. [Google Scholar]
- Silva‐Sanigorski A, Elea D, Bell C, Kremer P, Carpenter L, Nichols M, et al. Obesity prevention in the family day care setting: impact of the Romp & Chomp intervention on opportunities for children's physical activity and healthy eating. Child: Care, Health & Development 2011;37:385‐93. [DOI] [PubMed] [Google Scholar]
- Silva‐Sanigorski A, Bell AC, Kremer P, Park J, Demajo L, Smith M, et al. Process and impact evaluation of the Romp & Chomp obesity prevention intervention in early childhood settings: lessons learned from implementation in preschools and long day care settings. Childhood Obesity 2012;8(3):205‐15. [DOI: 10.1089/chi.2011.0118] [DOI] [PubMed] [Google Scholar]
- Duncan S. Improving fitness and reducing obesity in preschool children. BMJ 2011;343:1‐2. [DOI] [PubMed] [Google Scholar]
- Endres J, Barter S, Theodora P, Welch P. Soy‐enhanced lunch acceptance by preschoolers. Journal of the American Dietetic Association 2003;103(3):346‐51. [DOI] [PubMed] [Google Scholar]
- Falbe J, Davison KK, Taveras EM, Gortmaker SL, Anand SG, Blaine RE, et al. Evaluating mass in motion kids (MiM Kids): a multi‐sector intervention to reduce childhood obesity using a community‐clinical partnership. FASEB Journal 2013;27:36. [Google Scholar]
- Farfan‐Ramirez L, Diemoz L, Gong EJ, Lagura MA. Curriculum intervention in preschool children: Nutrition Matters!. Journal of Nutrition Education and Behavior 2011;43:S162‐5. [DOI] [PubMed] [Google Scholar]
- Ferrer R, Arellano‐Jimenez MR, Rangel D, Hernandez R, Caamaño M, Reyes L, et al. Effect of an education nutrition program in anthropometry, eating habits and physical activity in preschool children from Querétaro, México. The FASEB Journal 2014;28:626‐9. [Google Scholar]
- Fitzgerald N, Mueller C, Willems C, Zhang Y. A school‐based intervention’s influence on food knowledge, food preference and gross motor skills among preschoolers. The FASEB Journal 2014;28:252‐5. [Google Scholar]
- Fitzgibbon ML, Stolley MR, Dyer AR, Horn L, Kaufer Christoffel K. A community‐based obesity prevention program for minority children: rationale and study design for Hip‐Hop to Health Jr. Preventive Medicine 2002;34:289‐97. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Horn L, KauferChristoffel K, Dyer A. Two‐year follow‐up results for Hip‐Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. Journal of Pediatrics 2005;146(5):618‐25. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Horn L, KauferChristoffel K, Dyer A. Hip‐Hop to Health Jr. for Latino preschool children. Obesity 2006;14(9):1616‐25. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer LA, Braunschweig CL, Gomez SL, Horn L, et al. Hip‐Hop to Health Jr. obesity prevention effectiveness trial: postintervention results. Obesity 2011;19(5):994‐1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foltz JL, May AL, Belay B, Nihiser AJ, Dooyema CA, Blanck HM. Population‐level intervention strategies and examples for obesity prevention in children. Annual Review of Nutrition 2012;32:391‐415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foulkes C. Lessons from Healthy Together Geelong: delivering systems change at scale across two levels of government. Obesity Research and Clinical Practice 2014;8:33. [Google Scholar]
- Fritz K. Fighting obesity in 4‐year‐olds ‐ 'Move to Improve/Catch the Energy'. Strategies 2007;21(2):17‐20. [Google Scholar]
- Gallois KM, Henauw S, Hassel H, Hebestreit A, Pigeot I, Zeeb H. Standardized development of the IDEFICS intervention and its implementation in Germany. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 2011;54:330‐8. [DOI] [PubMed] [Google Scholar]
- Gannon AM, Olson R. Assessing the effectiveness of pre‐school nutrition education in West Virginia: a pilot program. Journal of the Academy of Nutrition and Dietetics 2013;9(113):A77. [Google Scholar]
- Gannon AM, Jeffrey J, Dice L. Evaluating the impact of a group education obesity intervention in early child care. 2014 Food & Nutrition Conference & Expo, October 18‐21, 2014, Atlanta, GA. Journal of the Academy of Nutrition & Dietetics 2014;114:A81. [Google Scholar]
- Girardet JP, Bocquet A, Bresson JL, Chouraqui JP, Darmaun D, Dupont C, et al. French national program for nutrition and health: effects on children's health. Archives de Pédiatrie 2009;16(1):3. [DOI] [PubMed] [Google Scholar]
- Goldberg P. A Comparison of BMI Percentiles and Predictor Variables for Two Head Start Childhood Obesity Prevention Programs. George Mason University, 2010. [Google Scholar]
- Goldfield GS, Harvey A, Grattan K, Colley R, Alberga AS, Ferraro ZM, et al. The preschoolers activity trial (PAT): a randomized controlled trial of physical activity intervention in the early years. Archives of Disease in Childhood 2012;97:A114. [Google Scholar]
- Goldfield G, Harvey A, Grattan K, Colley R, Alberga A, Ferraro Z, et al. The Preschoolers Activity Trial (PAT): a randomized controlled trial evaluating the effects of physical activity on adiposity in the early years. Obesity Facts 2014;7:121. [Google Scholar]
- Golley RK, Hendrie GA, Slater A, Corsini N. Interventions that involve parents to improve children's weight‐related nutrition intake and activity patterns: what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness?. Obesity Reviews 2011;12:114‐30. [DOI] [PubMed] [Google Scholar]
- Graham D, Appleton S, Rush E, McLennan S, Reed P, Simmons D. Increasing activity and improving nutrition through a schools‐based programme: Project Energize. 1. Design, programme, randomisation and evaluation methodology. Public Health Nutrition 2008;11:1076‐84. [DOI] [PubMed] [Google Scholar]
- Hammons AJ, Wiley AR, Fiese BH, Teran‐Garcia M. Six‐week Latino family prevention pilot program effectively promotes healthy behaviors and reduces obesogenic behaviors. Journal of Nutrition Education and Behavior 2013;45(6):745‐50. [DOI] [PubMed] [Google Scholar]
- Hanna H, Mathews R, Southward LH, Cross GW, Kotch J, Blanchard T, et al. Use of paid child care health care consultants in early care and education settings: results of a national study comparing provision of health screening services among Head Start and non‐Head Start centers. Journal of Pediatric Health Care 2012;26(6):427‐35. [DOI] [PubMed] [Google Scholar]
- Harvey H, Coleman G. Raising healthy eaters: a parenting and nutrition curriculum. Journal of Nutrition Education and Behavior 2008;40(1):52‐3. [DOI] [PubMed] [Google Scholar]
- Helland S, Bere E, Overby N. Food for preschoolers. Annals of Nutrition and Metabolism 2013;63:621. [Google Scholar]
- Herbert B, Strauß A, Mayer A, Duvinage K, Mitschek C, Koletzko B. Implementation process and acceptance of a setting based prevention programme to promote healthy lifestyle in preschool children. Health Education Journal 2013;72(3):363‐72. [Google Scholar]
- Herman A, Nelson BB, Teutsch C, Chung PJ. "Eat Healthy, Stay Active!": a coordinated intervention to improve nutrition and physical activity among Head Start parents, staff, and children. American Journal of Health Promotion 2012;27:e27‐36. [DOI] [PubMed] [Google Scholar]
- Isbell P, Kotch J, Savage E, Gunn E, Lu L, Weber D. Improvement of child care programs' health and safety policies, and practices, and children's access to health care, linked to child care health consultation. NHSA Dialog 2013;16(2):34‐52. [Google Scholar]
- Jones RA, Warren JM, Okely AD, Collins CE, Morgan PJ, Cliff DP. Process evaluation of the Hunter Illawarra Kids Challenge Using Parent Support study: a multisite randomized controlled trial for the management of child obesity. Health Promotion Practice 2010;11(6):917‐27. [DOI] [PubMed] [Google Scholar]
- Jouret B, Ahluwalia N, Dupuy M, Cristini C, Negre‐Pages L, Grandjean H, et al. Prevention of overweight in preschool children: results of kindergarten‐based interventions. International Journal of Obesity 2009;33:1075‐83. [DOI] [PubMed] [Google Scholar]
- Kain J, Uauy R, Concha F, Leyton B, Bustos N, Salazar G, et al. School‐based obesity prevention interventions for Chilean children during the past decades: lessons learned. Advances in Nutrition 2012;3:616S‐21S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korwanich K, Sheiham A, Srisuphan W, Srisilapanan P. Promoting healthy eating in nursery school children: a quasi‐experimental intervention study. Health Education Journal 2008;67(1):16‐30. [DOI: 10.1177/0017896907083153] [DOI] [Google Scholar]
- Lent M, Hill TF, Dollahite JS, Wolfe WS, Dickin KL. Healthy children, healthy families: parents making a difference! A curriculum integrating key nutrition, physical activity, and parenting practices to help prevent childhood obesity. Journal of Nutrition Education And Behavior 2012;44(1):90‐2. [DOI] [PubMed] [Google Scholar]
- Lerner‐Geva L, Bar‐Zvi E, Levitan G, Boyko V, Reichman B, Pinhas‐Hamiel O. An intervention for improving the lifestyle habits of kindergarten children in Israel: a cluster‐randomised controlled trial investigation. Public Health Nutrition 2015;18:1537‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manios Y, Grammatikaki E, Androutsos O, Chinapaw MJ, Gibson EL, Buijs G, et al. A systematic approach for the development of a kindergarten‐based intervention for the prevention of obesity in preschool age children: the ToyBox‐study. Obesity Reviews 2012;13(s1):3‐12. [DOI] [PubMed] [Google Scholar]
- Manios Y, Androutsos O, Katsarou C, Bourdeaudhuij I, Koletzko B, Moreno L, et al. Early prevention of childhood obesity: review of the literature and the first results of the ToyBox‐study. Annals of Nutrition And Metabolism 2013;63:64‐5. [Google Scholar]
- Mazzeo D, Arens SA, Germeroth C, Hein H. Stopping childhood obesity before it begins. Phi Delta Kappan 2012;93(7):10‐5. [Google Scholar]
- Metcalf B, Wilkin T. Lifestyle intervention in preschool children has little effect on obesity. BMJ 2012;344:1. [DOI] [PubMed] [Google Scholar]
- Mier N, Piziak V, Valdez L. Ultimate nutrition game for Mexican American preschoolers. Journal of Nutrition Education and Behavior 2005;37(6):325‐6. [DOI] [PubMed] [Google Scholar]
- Mo‐suwan L, Pongprapai S, Junjana C, Puetpaiboon A. Effects of a controlled trial of a school‐based exercise program on the obesity indexes of preschool children. American Journal of Clinical Nutrition 1998;68:1006‐11. [DOI] [PubMed] [Google Scholar]
- Najjar RH, Docherty A, Adita, L, Bergstro N, Larson E, Seitzinger A. Examining the effectiveness of the classroom portion of the 5‐2‐1‐0 program. Communicating Nursing Research 2013;46:694. [Google Scholar]
- National Association of Pediatric Nurse Associates and Practitioners. NAPNAP healthy eating and activity together (HEAT) initiative. Journal of Pediatric Health Care 2006;20:S3‐63. [PubMed] [Google Scholar]
- Natale RA, Messiah SE, Asfour L, Uhlhorn SB, Delamater A, Arheart KL. Role modeling as an early childhood obesity prevention strategy: effect of parents and teachers on preschool children's healthy lifestyle habits. Journal of Developmental and Behavioral Pediatrics 2014;35:378‐87. [DOI] [PubMed] [Google Scholar]
- Nemet D, Geva D, Pantanowitz M, Igbaria N, Meckel Y, Eliakim A. Health promotion intervention in Arab‐Israeli kindergarten children. Journal of Pediatric Endocrinology and Metabolism 2011;24:1001‐7. [DOI] [PubMed] [Google Scholar]
- Nemet D, Geva D, Pantanowitz M, Igbaria N, Meckel Y, Eliakim A. Long term effects of a health promotion intervention in low socioeconomic Arab‐Israeli kindergartens. BMC Pediatrics 2013;13:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederer I, Kriemler S, Zahner L, Bürgi F, Ebenegger V, Hartmann T, et al. Influence of a lifestyle intervention in preschool children on physiological and psychological parameters (Ballabeina): study design of a cluster randomized controlled trial. BMC Public Health 2009;9:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederer I, Bürgi F, Ebenegger V, Marques‐Vidal P, Schindler C, Nydegger A, et al. Effects of a lifestyle intervention on adiposity and fitness in overweight or low fit preschoolers (Ballabeina). Obesity 2013;21(3):E287‐93. [DOI] [PubMed] [Google Scholar]
- Organizational Research Services. Pilot Evaluation Report, Executive Summary, Healthy Child Care Washington. Seattle, WA: Organizational Research Services, 2003. [Google Scholar]
- Page AS, Winklhofer‐Roob BM. Five‐minutes‐to‐twelve for implementation of early changes in dietary and lifestyle behaviour across Europe. International Journal of Obesity 2011;35:S1‐2. [DOI] [PubMed] [Google Scholar]
- Partington S, Murphy E, Bowen E, Lacombe D, Piras G, Carson L, et al. Choose to Change: The West Virginia Early Childhood Obesity Prevention Project. Journal of Nutrition Education and Behavior 2012;44(4):S82‐3. [Google Scholar]
- Passehl B, McCarroll C, Buechner J, Gearring C, Smith AE, Trowbridge F. Preventing childhood obesity: establishing healthy lifestyle habits in the preschool years. Journal of Pediatric Health Care 2004;18:315‐9. [DOI] [PubMed] [Google Scholar]
- Patel AI, Cabana MD. Encouraging healthy beverage intake in child care and school settings. Current Opinion in Pediatrics 2010;22:779‐84. [DOI] [PubMed] [Google Scholar]
- Peregrin T. Take 10! Classroom‐based program fights obesity by getting kids out of their seats. Journal of the American Dietetic Association 2001;101:1409. [DOI] [PubMed] [Google Scholar]
- Phillips F. Nutrition and pre‐school children. Nutrition Bulletin 2004;29:64‐6. [Google Scholar]
- Prosper M, Moczulski VL, Qureshi A, Weiss M, Bryars T. Healthy for Life/PE4ME: assessing an intervention targeting childhood obesity. Californian Journal of Health Promotion 2009;7:1‐10. [Google Scholar]
- Ramsay S, Safaii S, Croschere T, Branen LJ, Wiest M. Kindergarteners' entree intake increases when served a larger entree portion in school lunch: a quasi‐experiment. Journal of School Health 2013;83:239‐42. [DOI] [PubMed] [Google Scholar]
- Requena Ayala I. Wednesday, fruit day at the American School of Valencia. Metas de Enfermería 2010;13:56‐9. [Google Scholar]
- Roth K, Mauer S, Obinger M, Lenz D, Hebestreit H. Activity and health prevention in preschools ‐ contents of an activity‐based intervention programme (PAKT ‐ Prevention through Activity in Kindergarten Trial). Journal of Public Health 2011;19:293‐303. [Google Scholar]
- Roths B, Fees BS, Bailey G, Fitzgerald K. Let's move, learn, and have fun!. Journal of Nutrition Education and Behavior 2002;34:343‐4. [DOI] [PubMed] [Google Scholar]
- Rudolf MCJ, Hunt C, George J, Hajibagheri K, Blair M. HENRY: development, pilot and long‐term evaluation of a programme to help practitioners work more effectively with parents of babies and pre‐school children to prevent childhood obesity. Child: Care, Health and Development 2010;36:850‐7. [DOI] [PubMed] [Google Scholar]
- Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity‐building: results of a quasi‐experimental intervention program, Be Active Eat Well. International Journal of Obesity 2008;32:1060‐7. [DOI] [PubMed] [Google Scholar]
- Santos‐Beneit G, Sotos‐Prieto M, Penalvo JL, Pocock S, Redondo J, Fuster V. Anthropometry and blood pressure in 3‐5 year old children of Madrid: Program si! study. Annals of Nutrition and Metabolism 2013;63:921. [Google Scholar]
- Savage AI, Koch T. A pediatric healthy lifestyle program. AAACN Viewpoint 2006;28:9‐11. [Google Scholar]
- Schindler JM, Corbett D, Forestell CA. Assessing the effect of food exposure on children's identification and acceptance of fruit and vegetables. Eating Behaviors 2013;14:53‐6. [DOI] [PubMed] [Google Scholar]
- Schwarz DF, Mallya G. The Philadelphia experience: actionable strategies for childhood obesity prevention. Childhood Obesity 2013;9:282‐5. [DOI] [PubMed] [Google Scholar]
- Sekhobo JP, Egglefield K, Edmunds LS, Shackman G. Evidence of the adoption and implementation of a statewide childhood obesity prevention initiative in the New York State WIC Program: the NY Fit WIC process evaluation. Health Education Research 2012;27:281‐91. [DOI] [PubMed] [Google Scholar]
- Skouteris H, Edwards S, Rutherford L, Cutter‐MacKenzie A, Huang T, O'Connor A. Promoting healthy eating, active play and sustainability consciousness in early childhood curricula, addressing the Ben10TM problem: a randomised control trial. BMC Public Health 2014;14:548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small L. PLAY! To tackle obesity in preschoolers. Parents Leading Active Youth. Nurse Practitioner World News 2007;12:16‐7. [Google Scholar]
- Smiciklas‐Wright H, D'Augelli AR. Primary prevention for overweight: Preschool Eating Patterns (PEP) Program. Journal of the American Dietetic Association 1978;72(6):626. [PubMed] [Google Scholar]
- Stock S, Miranda C, Evans S, Plessis S, Ridley J, Yeh S, et al. Healthy Buddies: a novel, peer‐led health promotion program for the prevention of obesity and eating disorders in children in elementary school. Pediatrics 2007;120:e1059‐68. [DOI] [PubMed] [Google Scholar]
- Stolley MR, Fitzgibbon ML, Dyer A, Horn L, KauferChristoffel K, Schiffer L. Hip‐Hop to Health Jr., an obesity prevention program for minority preschool children: baseline characteristics of participants. Preventive Medicine 2003;36:320‐9. [DOI] [PubMed] [Google Scholar]
- Story M, Hannan PJ, Fulkerson JA, Rock BH, Smyth M, Arcan C, et al. Bright Start: description and main outcomes from a group‐randomized obesity prevention trial in American Indian children. Obesity 2012;20:2241‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauß A, Herbert B, Mitschek C, Duvinage K. TigerKids. Bundesgesundheitsblatt‐Gesundheitsforschung‐Gesundheitsschutz 2011;54(3):322‐9. [DOI] [PubMed] [Google Scholar]
- Summerbell CD, Moore HJ, Vogele C, Kreichauf S, Wildgruber A, Manios Y, et al. Evidence‐based recommendations for the development of obesity prevention programs targeted at preschool children. Obesity Reviews 2012;13 Suppl 1:129‐32. [DOI] [PubMed] [Google Scholar]
- Thibault H, Boulard S, Carriere C, Ruello M, Atchoarena S, Delmas C, et al. Prevention and treatment of childhood obesity in the Aquitaine region (France). International Journal of Pediatric Obesity 2010;5:39‐40. [Google Scholar]
- Thomas R. Conditional cash transfers to improve education and health: an ex ante evaluation of red de protección social, Nicaragua. Health Economics 2012;21:1136‐54. [DOI] [PubMed] [Google Scholar]
- Trost SG, Fees B, Dzewaltowski D. Feasibility and efficacy of a 'Move and Learn' physical activity curriculum in preschool children. Journal of Physical Activity and Health 2008;5(1):88. [DOI] [PubMed] [Google Scholar]
- Trost SG, Gunter K, Rice K. Promotion of healthy eating and regular physical activity in children attending family child care homes. Journal of Nutrition Education and Behavior 2012;44:S83. [Google Scholar]
- Vanderwall C, Mullen M, Keim K, Sowa D. Parents Learn about Thoughtful Eating (PLATE) Program: school‐based intervention to prevent obesity in preschool‐aged children. Journal of Nutrition Education and Behavior 2012;44:S49. [Google Scholar]
- Stan S, Lessard L, Dupont Phillips K. The impact of a statewide training to increase child care providers' knowledge of nutrition and physical activity rules in Delaware. Childhood Obesity 2013;9:43‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasquez F, Andrade M, Rodriguez M, Salazar G. Effect of educational nutrition program on the energy and macronutrients intake of preschoolers attending Junji day care centres in the eastern sector of Santiago, Chile. Archivos Latinoamericanos de Nutricion 2008;58:241‐8. [PubMed] [Google Scholar]
- Verbestel V, Coen V, Winckel M, Huybrechts I, Maes L, Bourdeaudhuij I. Prevention of overweight in children younger than 2 years old: a pilot cluster‐randomized controlled trial. Public Health Nutrition 2014;17:1384‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt RG, Draper AK, Ohly HR, Rees G, Pikhart H, Cooke L, et al. Methodological development of an exploratory randomised controlled trial of an early years' nutrition intervention: the CHERRY programme (Choosing Healthy Eating when Really Young). Maternal and Child Nutrition 2014;10(2):280‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley SE, McGregor S, Jiang L, Gomez J, Harrison G, Jenks E. A WIC‐based intervention to prevent early childhood overweight. Journal of Nutrition Education and Behavior 2010;42:S47‐51. [DOI] [PubMed] [Google Scholar]
- Wilken LR, Novotny R, Fialkowski MK, Boushey CJ, Nigg C, Paulino Y, et al. Children's Healthy Living (CHL) Program for remote underserved minority populations in the Pacific region: rationale and design of a community randomized trial to prevent early childhood obesity. BMC Public Health 2013;13:944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CL, Carter BJ, Kibbe DL, Dennison D. Increasing physical activity in preschool: a pilot study to evaluate animal trackers. Journal of Nutrition Education and Behavior 2009;41:47‐52. [DOI] [PubMed] [Google Scholar]
- Witt KE, Dunn C. Increasing fruit and vegetable consumption among preschoolers: evaluation of Color Me Healthy. Journal of Nutrition Education and Behavior 2012;44:107‐13. [DOI] [PubMed] [Google Scholar]
- Yin Z, Parra‐Medina D, Cordova A, He M, Trummer V, Sosa E, et al. Miranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Childhood Obesity 2012;8:429‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zask A, Barnett LM, Rose L, Brooks LO, Molyneux M, Hughes D, et al. Three year follow‐up of an early childhood intervention: is movement skill sustained?. International Journal of Behavioral Nutrition and Physical Activity 2012;9:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z, Ren H, Yin Z, Wang L, Wang K. A policy‐driven multifaceted approach for early childhood physical fitness promotion: impacts on body composition and physical fitness in young Chinese children. BMC Pediatrics 2014;14:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
- Duke University. Baby NAP SACC Intervention Study. https://clinicaltrials.gov/ct2/show/NCT01890681?term=childcare&rank=15.
- Finch M, Yoong SL, Thomson RJ, Seward K, Cooney M, Jones J, et al. A pragmatic randomised controlled trial of an implementation intervention to increase healthy eating and physical activity‐promoting policies, and practices in centre‐based childcare services: study protocol. BMJ Open 2015;5(5):e006706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J, Wolfenden L, Wyse R, Finch M, Yoong SL, Dodds P, et al. A randomised controlled trial of an intervention to facilitate the implementation of healthy eating and physical activity policies and practices in childcare services. BMJ Open 2014;4(4):e005312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Université de Sherbrooke. Healthy Start to Increase Physical Activity and Improve Healthy Eating in Early Childcare Centres. https://clinicaltrials.gov/show/NCT02375490/.
Additional references
- Adams J, Zask A, Dietrich U. Tooty Fruity Vegie in Preschools: an obesity prevention intervention in preschools targeting children's movement skills and eating behaviours. Health Promotion Journal of Australia 2009;20:112‐9. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. Diffusion and dissemination of evidence‐based cancer control interventions. Agency for Healthcare Research and Quality2003.
- Ammerman AS, Ward DS, Benjamin SE, Ball SC, Sommers JK, Molloy M, et al. An intervention to promote healthy weight: nutrition and physical activity self‐assessment for child care (NAP SACC) theory and design. Preventing Chronic Disease 2007;4(3):1‐12. [PMC free article] [PubMed] [Google Scholar]
- Arditi C, Rège‐Walther M, Wyatt JC, Durieux P, Burnand B. Computer‐generated reminders delivered on paper to healthcare professionals; effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD001175.pub3] [DOI] [PubMed] [Google Scholar]
- Ball SC, Benjamin SE, Ward DS. Dietary intakes in North Carolina child‐care centers: are children meeting current recommendations. Journal of the American Dietetic Association 2008;108(4):718‐21. [DOI] [PubMed] [Google Scholar]
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, Onis M, et al. Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet 2013;382(9890):427‐51. [DOI] [PubMed] [Google Scholar]
- Bollella MC, Boccia LA, Nicklas TA, Lefkowitz KB, Pittman BP, Zang EA, et al. Assessing dietary intake in preschool children: the Healthy Start project ‐ New York. Nutrition Research 1998;19(1):37‐48. [Google Scholar]
- Buller DB. Continuing issues for dissemination and implementation of cancer prevention interventions. American Journal of Preventive Medicine 2010;38(4):462‐3. [DOI] [PubMed] [Google Scholar]
- Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Science 2012;7:1‐17. [DOI: 10.1186/1748-5908-7-37] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cashmore AW, Jones SC. Growing up active: a study into physical activity in long day care centers. Journal of Research in Childhood Education 2008;12:179‐91. [DOI: 10.1080/02568540809594654] [DOI] [Google Scholar]
- Cochrane Public Health Group. Guide for Developing a Cochrane Protocol. http://ph.cochrane.org/sites/ph.cochrane.org/files/uploads/Guide%20for%20PH%20protocol_Nov%202011_final%20for%20website.pdf2011.
- Cohen AN, Hamilton AB, Ritchie M, Mittman BS, Kirchner JE, Wyatt GE, et al. Improving care quality through hybrid implementation/effectiveness studies: best practices in design, methods, and measures. Implementation Science 2015;10 Suppl 1(A29):1‐3. [DOI: 10.1186/1748-5908-10-S1-A29] 25567289 [DOI] [Google Scholar]
- Commonwealth of Australia. Get Up and Grow Healthy Eating and Physical Activity for Early Childhood. http://www.health.gov.au/internet/main/publishing.nsf/Content/phd‐gug‐staffcarers2013.
- Copeland KA, Kendeigh CA, Saelens BE, Kalkwarf HJ, Sherman SN. Physical activity in child‐care centers: do teachers hold the key to the playground?. Health Education Research 2012;27(1):81‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Agostino C, D'Andrea T, Lieberman L, Sprance L, Williams CL. Healthy Start: a new comprehensive preschool health education program. Journal of Health Education 1999;30(1):9‐12. [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science 2009;4(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derscheid LE, Umoren J, Kim S, Henry BW, Zittel LL. Early childhood teachers' and staff members' perceptions of nutrition and physical activity practices for preschoolers. Journal of Research in Childhood Education 2010;24(3):248‐65. [DOI: 10.1080/02568543.2010.487405] [DOI] [Google Scholar]
- Dobbins M, Husson H, DeCorby K, LaRocca RL. School‐based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database of Systematic Reviews 2013, Issue 2. [DOI: 10.1002/14651858.CD007651.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effective Practice, Organisation of Care (EPOC). EPOC Taxonomy. https://epoc.cochrane.org/epoc‐taxonomy2015.
- Finch M, Wolfenden L, Morgan PJ, Freund M, Wyse R, Wiggers J. A cluster randomised trial to evaluate a physical activity intervention among 3‐5 year old children attending long day care services: study protocol. BMC Public Health 2010;10(534):1‐10. [DOI: 10.1186/1471-2458-10-534] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch M, Jones J, Yoong S, Wiggers J, Wolfenden L. Effectiveness of centre‐based childcare interventions in increasing child physical activity: a systematic review and meta‐analysis for policymakers and practitioners. Obesity Reviews 2016;17(5):412‐28. [DOI] [PubMed] [Google Scholar]
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body‐mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country‐years and 9.1 million participants. Lancet 2011;377:557‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsetlund L, Bjørndal A, Rashidian A, Jamtvedt G, O'Brien MA, Wolf FM, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD003030.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SD, Green SE, O'Connor DA, McKenzie JE, Francis JJ, Michie S, et al. Developing theory‐informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implementation Science 2012;7(1):1‐8. [DOI: 10.1186/1748-5908-7-38] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froehlich Chow A, Humbert L. Physical activity and nutrition in early years care centers: barriers and facilitators. Canadian Children 2011;36(1):26‐30. [Google Scholar]
- Giguère A, Légaré F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A, et al. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews 2012, Issue 10. [DOI: 10.1002/14651858.CD004398.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science; current and future directions. American Journal of Public Health 2012;107(7):1274‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray V, Holman CDJ. Deaths and premature loss of life caused by overweight and obesity in Australia in 2011‐2050: benefits from different intervention scenarios. Report for the Australian Preventive Health Taskforce. Commonwealth of Australia2009.
- Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knotterus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 2010 Dec 24 [Epub ahead of print]. [DOI] [PubMed]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
- Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard‐Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD000259.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaime PC, Lock K. Do school based food and nutrition policies improve diet and reduce obesity?. Preventive Medicine 2009;48(1):45‐53. [DOI] [PubMed] [Google Scholar]
- Kelly B, Hardy LL, Howlett S, King L, Farrell L, Hattersley L. Opening up Australian preschoolers’ lunchboxes. Australian and New Zealand Journal of Public Health 2010;34:288‐92. [DOI] [PubMed] [Google Scholar]
- Lobstein T, Baur L, Uauy R for the IASO International Obesity Taskforce. Obesity in children and young people: a crisis in public health. Obesity Reviews 2004;5(Suppl 1):4‐104. [DOI] [PubMed] [Google Scholar]
- Mazza D, Bairstow P, Buchan H, Paubrey Chakraborty S, Hecke O, Grech C, et al. Refining a taxonomy for guideline implementation: results of an exercise in abstract classification. Implementation Science 2013;8(32):1‐10. [DOI: 10.1186/1748-5908-8-32] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliams C, Ball SC, Benjamin SE, Hales D, Vaughn A, Ward DS. Best‐practice guidelines for physical activity at childcare. Pediatrics 2009;124:1650‐9. [DOI] [PubMed] [Google Scholar]
- Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Applied Psychology 2008;57(4):660‐80. [Google Scholar]
- Mikkelsen MV, Husby S, Skov LR, Perez‐Cueto FJ. A systematic review of types of healthy eating interventions in preschools. Nutrition Journal 2014;13(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore H, Nelson P, Marshall J, Cooper M, Zambas H, Brewster K, et al. Laying foundations for health: food provision for under 5s in day care. Appetite 2005;44(2):207‐13. [DOI] [PubMed] [Google Scholar]
- O'Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard‐Jensen J, Kristoffersen DT, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD000409.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagnini D, Wilkenfield R, King L, Booth M, Booth S. Early childhood sector staff perceptions of child overweight and obesity: the Weight of Opinion Study. Health Promotion Journal of Australia 2007;18(2):149‐54. [DOI] [PubMed] [Google Scholar]
- Phillips CJ, Marshall AP, Chaves NJ, Jankelowitz SK, Lin IB, Loy CT, et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: a qualitative study. Journal of Multidisciplinary Healthcare 2015;8:139‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard CM, Lewis JM, Miller MR. Food service in long day care centres ‐ an opportunity for public health intervention. Australian and New Zealand Journal of Public Health 1999;23:606‐11. [DOI] [PubMed] [Google Scholar]
- Rabin BA, Brownson RC, Haire‐Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. Journal of Public Health Management Practice 2008;14(2):117‐23. [DOI] [PubMed] [Google Scholar]
- Rabin BA, Galsgow RE, Kerner JF, Klump MP, Brownson RC. Dissemination and implementation research on community‐based cancer prevention. American Journal of Preventive Medicine 2010;38(4):443‐56. [DOI] [PubMed] [Google Scholar]
- Rosemburg F. Multilateral organizations and early child care and education policies for developing countries. Gender and Society 2003;17(2):250‐66. [DOI: 10.1177/0891243202250831] [DOI] [Google Scholar]
- Schillinger D. An introduction to effectiveness, dissemination and implementation research. In: Fleisher P, Goldstein E editor(s). UCSF Clinical and Translational Science Institute (CTSI) Resource Manuals and Guides to Community‐Engaged Research. San Francisco: Clinical Translational Science Institute Community Engagement Program, University of California, 2010. [Google Scholar]
- Scott A, Sivey P, Ait Ouakrim D, Willenberg L, Naccarella L, Furler J, et al. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database of Systematic Reviews 2011, Issue 9. [DOI: 10.1002/14651858.CD008451.pub2] [DOI] [PubMed] [Google Scholar]
- Sisson S, Campbell JE, May KB, Brittain DR, Monrie LA, Guss SH, et al. Assessment of food, nutrition, and physical activity practices in Oklahoma child‐care centers. Journal of the Academy of Nutrition and Dietetics 2012;112:1230‐40. [DOI] [PubMed] [Google Scholar]
- Sisson SB, Krampe M, Anundson K, Castle S. Obesity prevention and obesogenic behavior interventions in child care: a systematic review. Preventive Medicine 2016;87:57‐69. [DOI] [PubMed] [Google Scholar]
- Spark A, Pfau J, Nicklas TA, Williams CL. Reducing fat in preschool meals: description of the foodservice intervention component of Healthy Start. Journal of Nutrition Education 1998;30(3):170‐7. [Google Scholar]
- Squires JE, Sullivan K, Eccles MP, Worswick J, Grimshaw JM. Are multifaceted interventions more effective than single‐component interventions in changing health‐care professionals' behaviours? An overview of systematic reviews. Implementation Science 2014;9(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M, Kaphingst K, French S. The role of child care settings in obesity prevention. Future of Children 2006;16(1):143‐68. [DOI] [PubMed] [Google Scholar]
- Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet 2011;378(9793):804‐14. [DOI] [PubMed] [Google Scholar]
- Tremblay L, Boudreau‐Lariviere C, Cimon‐Lambert K. Promoting physical activity in pre‐schoolers: a review of the guidelines, barriers, and facilitators for implementation of policies and practices. Canadian Psychology 2012;53(4):280‐90. [Google Scholar]
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815‐25. [DOI] [PubMed] [Google Scholar]
- Waters E, Silva‐Sanigorski A, Burford BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD001871.pub3] [DOI] [PubMed] [Google Scholar]
- Williams CL, Squillace MM, Bollela MC, Brotanek J, Campanaro L, D'Agostino C, et al. Healthy Start: a comprehensive health education program for preschool children. Preventive Medicine 1998;27:216‐23. [DOI] [PubMed] [Google Scholar]
- Williams CL, Strobino BA, Bollela M, Brotanek J. Cardiovascular risk reduction in preschool children: the "Healthy Start" project. Journal of the American College of Nutrition 2004;23(2):117‐23. [DOI: 10.1080/07315724.2004.10719351] [DOI] [PubMed] [Google Scholar]
- Wolfenden L, Neve M, Farrell L, Lecathelinais C, Bell AC, Milat A, et al. Physical activity policies and practices of childcare centres in Australia. Journal of Paediatrics and Child Health 2010;47:73‐6. [DOI] [PubMed] [Google Scholar]
- Wolfenden L, FInch M, Nathan N, Weaver N, Wiggers J, Yoong SL, et al. Factors associated with early childhood education and care service implementation of healthy eating and physical activity policies and practices in Australia: a cross‐sectional study. Translational Behavioural Medicine 2015;5(3):327‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfenden L, Milat AJ, Lecathelinais C, Sanson‐Fisher RW, Carey ML, Bryant J, et al. What is generated and what is used: a description of public health research output and citation. European Journal of Public Health 2016;26(3):523‐5. [DOI] [PubMed] [Google Scholar]
- Wolfenden L, Finch M, Wyse R, Clinton‐McHarg T, Yoong SL. Time to focus on implementation: the need to re‐orient research on physical activity in childcare services. Australian and New Zealand Journal of Public Health 2016;40(3):209‐10. [DOI] [PubMed] [Google Scholar]
- Wolfenden L, Milat AJ, Lecathelinais C, Skelton E, Clinton‐McHarg T, Williams C, et al. A bibliographic review of public health dissemination and implementation research output and citation rates. Preventive Medicine Reports 2016;4:441‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Population based approaches to childhood obesity prevention. http://www.who.int/dietphysicalactivity/childhood/WHO_new_childhoodobesity_PREVENTION_27nov_HR_PRINT_OK.pdf2012.
- Yoong SL, Skelton E, Jones J, Wolfenden L. Do childcare services provide foods in line with the 2013 Australian Dietary guidelines? A cross‐sectional study. Australian and New Zealand Journal of Public Health 2014;38(6):595‐6. [DOI] [PubMed] [Google Scholar]
- Yoong SL, Clinton‐Mcharg T, Wolfenden L. Systematic reviews examining implementation of research into practice and impact on population health are needed. Journal of Clinical Epidemiology 2015;68(7):788‐91. [DOI] [PubMed] [Google Scholar]
- Zoritch B, Roberts I, Oakley A. Day care for pre‐school children. Cochrane Database of Systematic Reviews 2000, Issue 3. [DOI: 10.1002/14651858.CD000564] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Wolfenden L, Jones J, Finch M, Wyse RJ, Yoong SL, Steele EJ, et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD011779] [DOI] [PMC free article] [PubMed] [Google Scholar]


