Abstract
Background/Objectives:
A lower risk of falls is commonly cited as a reason to treat hypertension conservatively in older individuals. We examined the effect of hypertension treatment and control status and measured blood pressure (BP) level on the risk of falls in older women.
Design/Setting:
Prospective cohort study
Participants:
5971 women (mean age 79 years; 50.4% White, 33.1% Black, 16.5% Hispanic/Latina) enrolled in the Women’s Health Initiative and Objective Physical Activity and Cardiovascular Health study
Measurements:
BP was measured by trained nurses and hypertension treatment was assessed by medication inventory. Participants mailed in monthly calendars to self-report falls for one year.
Results:
Overall, 70% of women had hypertension at baseline (53% treated and controlled, 12% treated and uncontrolled, 5% untreated). There were 2582 (43%) women who reported falls in the one year of surveillance. Compared with non-hypertensive women, when adjusted for fall risk factors and lower limb physical function the incidence rate ratio and 95% confidence interval for falls was 0.82 (0.74–0.92) in women with treated controlled hypertension (p=0.0008) and 0.73 (0.62–0.87) in women with treated uncontrolled hypertension (p=0.0004). Neither measured systolic nor diastolic BP were associated with falls in the overall cohort. In women treated with antihypertensive medication, higher diastolic BP was associated with a lower risk of falls in a model adjusted for fall risk factors (incidence rate ratio 0.993 per mm Hg, 95% confidence interval 0.987– 1.000, p=0.04). The only class of antihypertensive medication that was associated with an increased risk of falls compared with all other types of antihypertensive drugs was beta blockers.
Conclusion:
Women in this long-term research study with treated hypertension have lower risk of falls compared with non-hypertensive women. Diastolic BP (but not systolic BP) is weakly associated with fall risk in women on antihypertensive treatment (<1% decrease in risk per mm Hg increase).
Keywords: hypertension, blood pressure, falls, older adults, cohort study
INTRODUCTION
Evidence from clinical trials shows that treatment of hypertension prevents cardiovascular events, especially stroke.1–3 Counterbalancing the benefits of antihypertensive treatment is the concern that it may place patients at risk for hypotension, falls and fractures, particularly when more stringent control of blood pressure (BP) is the goal. Falls are a serious problem in older Americans; in 2014 they resulted in 2.8 million emergency room visits, 800,000 hospitalizations, 27,000 deaths and an estimated $31.3 billion in Medicare expenditures.4
It is a common belief that long-term antihypertensive treatment is causally linked to falls and fractures, but there is little supporting evidence. Two randomized trials that achieved substantial BP reduction and collected data on self-reported falls did not find an elevated risk in the intervention group.5,6 The recent Systolic Blood Pressure Intervention Trial (SPRINT) also found no increase in injurious falls with mean systolic BP 121 mm Hg in the intensive treatment group compared with 136 mm Hg in the standard treatment group.7 Similarly, hypertension trials have not shown an increase in fracture risk, and some have suggested that fractures may be reduced with antihypertensive treatment.5,6,8 Prospective observational studies also have not generally shown that individuals on antihypertensive treatment have an increased risk of fractures and other serious injuries.9–13 In contrast to the findings from long-term clinical trials and observational studies, recent observational studies using large national databases have consistently found a short-term increased risk of injurious falls and hip fracture in the 14–45 day period immediately following initiation of antihypertensive or diuretic therapy in elderly patients.14–18
In this paper we present data on the association of prospectively collected data on falls with hypertension, measured BP, and antihypertensive treatment in a large and diverse population of older women enrolled in the Women’s Health Initiative (WHI) Objective Physical Activity and Cardiovascular Health (OPACH) study. The objectives of this report are to compare the risk of falls in older women with adjustment for important covariates 1) by hypertension status (no hypertension, untreated hypertension, treated controlled hypertension, treated uncontrolled hypertension), 2) across a range of measured systolic and diastolic BP, and 3) by antihypertensive drug class.
METHODS
Participants
The study participants were enrolled in the Women’s Health Initiative (WHI), a long-term study of postmenopausal women aged 50–79 recruited in 1993–1998 from centers across the United States.19,20 In 2012–2013 home visits were conducted in a subset of older WHI participants as part of the ancillary Long Life Study. Ambulatory women in the Long Life Study were invited to enroll in the OPACH study. 21 All of the studies were approved by the Fred Hutchinson Cancer Research Center institutional review board. The 5971 women included in this analysis completed the Long Life Study home visit, consented to OPACH, and returned at least one fall calendar.
Measurements
Physical measurements (BP, height, and weight) were performed by trained nurses during a home visit using a standard protocol.22 After determining the correct cuff size by measuring the upper arm circumference, and after sitting quietly with legs uncrossed for at least five minutes, BP was taken twice with a 30 second interval between measurements using an anaeroid sphygmomanometer. In analyses, the average of the two BP measurements was used. Lower limb physical function was assessed by the Short Physical Performance Battery (SPPB), consisting of tests of balance, gait speed, and ability to stand from a seated position.23,24
Antihypertensive treatment was determined from a medication inventory conducted in 2012–2013 and matched to the corresponding item in a pharmacy database (Master Drug Data Base, Medi-Span) and further categorized according to antihypertensive drug class. Hypertension status was classified based on measured BP at the Long Life Study visit and antihypertensive treatment from the medication inventory as follows: no hypertension (BP<140/90 mm Hg and not treated with antihypertensive drugs), treated controlled hypertension (BP<140/90 mm Hg and treated with antihypertensive drugs), treated uncontrolled hypertension (BP≥140/90 mm Hg and treated with antihypertensive drugs), and untreated hypertension (BP≥140/90 mm Hg and not treated with antihypertensive drugs).
Comorbidities, including diabetes, were self-reported by the participants from a list of 10 chronic conditions.25 Other self-reported items included demographics, alcohol use, history of fracture, number of falls in the past year, difficulty walking for more than 30 minutes, use of assistive devices for walking, balance, vision, and bodily pain.
Outcomes
Incident falls were collected prospectively from monthly calendars completed by OPACH participants for 13 months after starting the study. Women were instructed to report a fall if they lost balance and fell to the ground or a lower level or if they had to use a wall, rail or other object to prevent themselves from falling to the ground.
Statistical Analysis
Characteristics of the study participants were stratified by self-reported number of falls in the year prior baseline. Incident fall rates were calculated as the number of falls reported from the fall calendars divided by the number of person-months of calendar pages received. Since fall incidence is highly right-skewed, negative binomial regression models were used to examine the association of the hypertension-related exposures (hypertension status, measured systolic and diastolic BP, and antihypertensive drug class in treated women) with the incidence rate of falling in the 12-month period. Incidence rate ratio (IRR) was calculated as the natural log transformed coefficient; 95% percent confidence intervals (CI) were calculated by similar means using the standard error of the coefficient.
Covariates were entered into models adjusting for age, race/ethnicity, and education (Model 1). Model 2 additionally adjusted for selected fall risk factors (alcohol use, BMI, chronic conditions, vision, and bodily pain). Model 3 added SPPB score to Model 2. We did not adjust for self-reported fall risk factors (use of assistive devices, difficulty walking, and balance) that were more directly measured by the SPPB. We also analyzed Model 2 stratified by SPPB score (1–8 vs. 9–12), since worse lower limb physical function could represent a biologic mechanism through which BP or antihypertensive therapy operates to affect falls risk differently than that in women with higher levels of physical functioning. Models with measured BP as the exposure were examined in the entire study population and in the subgroup of women with treated hypertension. Models with antihypertensive drugs class as the exposure were examined in the subgroup of women with treated hypertension. Each drug class was coded as a categorical variable (1=drug class was in the medication inventory, 0=all other drug class(es) were in the medication inventory.) Hypothesis tests were conducted at alpha .05 with two-sided P-values <0.05 considered nominally significant. All analyses were performed using R 3.3.0 (R Foundation for Statistical Computing, Vienna, Austria.)
RESULTS
The study sample (n=5971) had a mean age of 79 years; 50.4% were non-Hispanic White, 33.1% were Black, and 16.5% were Hispanic (Table 1). During prospective follow-up, 57% reported no falls, while 23% reported 1 fall and 21% reported 2 or more falls. Compared with women with no falls, women who reported falls during the prospective observation period were older, were more likely to be non-Hispanic white, had a slightly higher level of education, were slightly more likely to drink alcohol, and had lower BMI. Women with falls had more chronic conditions and had lower SBBP scores compared with women remaining free of falls during follow-up. Those experiencing incident falls also were more likely to have had fractures and falls prior to OPACH baseline, to use an assistive device for walking, and to report difficulty walking, poorer balance, worse vision, and more bodily pain than non-fallers.
Table 1.
Participant characteristics by no fall vs. fall
| Total sample |
No fall | 1 fall | 2+ falls | |
|---|---|---|---|---|
| Characteristic | N=5971 | N=3389 | N=1355 | N=1227 |
| Age, years, mean (SD) | 78.8 (6.7) | 78.3 (6.7) | 78.7 (6.6) | 80.3 (6.6) |
| Race/Ethnicity, n (%) | ||||
| White | 3011 (50.4) | 1528 (45.1) | 704 (52.0) | 779 (63.5) |
| Black | 1976 (33.1) | 1264 (37.3) | 426 (31.4) | 286 (23.3) |
| Hispanic/Latina | 984 (16.5) | 597 (17.6) | 225 (16.6) | 162 (13.2) |
| Highest education level high school or less, n (%) | 1846 (30.9) | 1080 (31.9) | 411 (30.3) | 355 (28.9) |
| No or rare alcohol intake past 3 mo, n (%) [494 (8.3%) missing] | 4504 (75.4) | 2537 (74.9) | 1043 (77.0) | 924 (75.3) |
| Body mass index, kg/m2, mean (SD) | 28.1 (5.8) | 28.3 (5.8) | 28.1 (5.8) | 27.7 (5.5) |
| Diabetes, n (%) | 668 (11.2) | 394 (11.6) | 133 (9.8) | 141 (11.5) |
| Number of chronic conditions, n (%) [375 (6.3%) missing] | ||||
| Zero | 991 (16.6) | 606 (17.9) | 214 (15.8) | 171 (13.9) |
| One | 2082 (34.9) | 1166 (34.4) | 501 (37.0) | 415 (33.8) |
| Two or more | 2523 (42.3) | 1391 (41.0) | 562 (41.5) | 570 (46.5) |
| SPPB* Score (Range 0–12), mean (SD) [543 (9.1%) missing] | 8.2 (2.5) | 8.3 (2.4) | 8.3 (2.5) | 7.8 (2.7) |
| SPPB Score 9–12, n (%) [543 (9%) missing] | 2665 (44.6) | 1571 (46.4) | 632 (46.6) | 462 (37.7) |
| History of fracture, n (%) | 1226 (20.5) | 618 (18.2) | 287 (21.2) | 321 (26.2) |
| Self-reported fall history, n (%) [246 (4.1%) missing] | ||||
| No fall | 3905 (65.4) | 2483 (73.3) | 870 (64.2) | 552 (45) |
| 1 fall | 1161 (19.4) | 531 (15.7) | 336 (24.8) | 294 (24.0) |
| 2+ falls | 659 (11.0) | 196 (5.8) | 121 (8.9) | 342 (27.9) |
| Use of assistive device for walking, n (%) | 1760 (29.5) | 866 (25.6) | 406 (30.0) | 488 (39.8) |
| No difficulty walking 30 minutes, n (%) [231 (3.9%) missing] | 4009 (67.1) | 2339 (69.0) | 931 (68.7) | 739 (60.2) |
| Excellent or very good balance, n (%) [524 (8.8%) missing] | 2175 (36.4) | 1356 (40.0) | 500 (36.9) | 319 (26.0) |
| Excellent or very good vision, n (%) [516 (8.6%) missing] | 2838 (47.5) | 1608 (47.4) | 662 (48.9) | 568 (46.3) |
| No or mild body pain, n (%) [501 (8.4%) missing] | 3625 (60.7) | 2079 (61.3) | 857 (63.2) | 689 (56.2) |
| Hypertension, n (%) [2 (<1%) missing] | ||||
| No hypertension | 1797 (30.1) | 1041 (30.7) | 383 (28.3) | 373 (30.4) |
| Treated controlled hypertension | 3191 (53.4) | 1785 (52.7) | 754 (55.6) | 652 (53.1) |
| Treated uncontrolled hypertension | 709 (11.9) | 403 (11.9) | 150 (11.1) | 156 (12.7) |
| Untreated uncontrolled hypertension | 272 (4.6) | 159 (4.7) | 67 (4.9) | 46 (3.7) |
Short Physical Performance Battery
Of the 5969 women whose hypertension status could be categorized based on measured BP and medication inventory, 30.1% had no hypertension, 53.4% had treated controlled hypertension, 11.9% had treated uncontrolled hypertension, and 4.6% had untreated hypertension (Table 1). There was no clear evidence for increased risk of falls among women with treated hypertension (regardless of control) compared to those without hypertension (Figure 1). In all models, women with treated controlled hypertension had a statistically significant 15%−20% lower risk of falls than women with no hypertension. Women with treated uncontrolled hypertension also had a significantly lower risk of falls than women with no hypertension in models adjusted for fall risk factors (Model 2), including SBBP (Model 3). Compared with women with no hypertension, fall risk was higher in women with untreated uncontrolled hypertension in Model 2 only, but confidence intervals around the point estimates were wide in all the models in this small subgroup. Among 3900 treated women 1516 (39%) were treated with 1 drug, 1429 (37%) were treated with 2 drugs, and 955 (24%) were treated with 3 or more drugs. The lower point estimate of the risk of falls in women with treated hypertension was qualitatively similar regardless of whether treatment was with 1, 2, or 3 or more antihypertensive drugs and also in strata of SPPB scores 1–8 and 9–12 in Model 2 (IRR for falls in women with treated controlled hypertension 0.79 [95% CI 0.67–0.94] for SPPB scores 1–8 and 0.86 [95% CI 0.74–1.00] for SBBP scores 9–12; IRR for falls in women with treated uncontrolled hypertension 0.76 [95% CI 0.60–0.97] for SPPB scores 1–8 and 0.73 [95% CI 0.57–0.94] for SBBP scores 9–12.)
Figure 1: Association of Hypertension Status with Fall Incidence (N=5969).
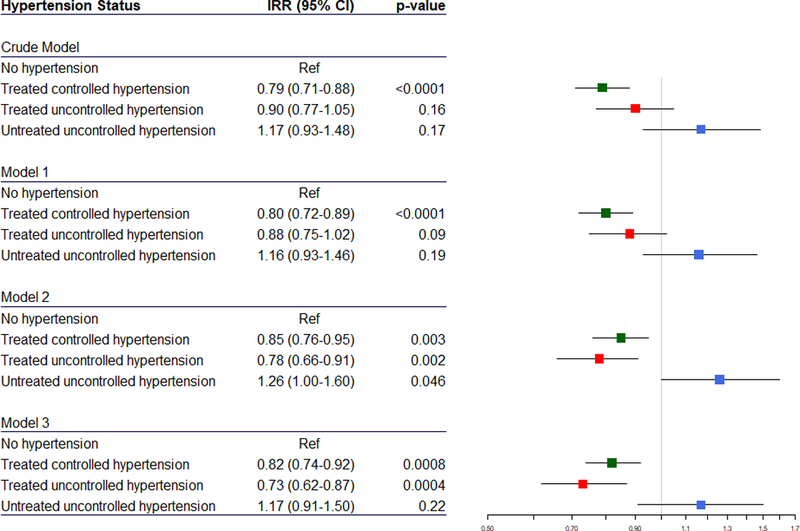
The point estimate of the incidence rate ratio (IRR, colored squares) and 95% confidence interval (CI, horizontal lines) for fall incidence compared to women with no hypertension (reference, vertical grey line) is shown for treated controlled hypertension (green), treated uncontrolled hypertension (red), and untreated uncontrolled hypertension (blue). There are two participants with missing blood pressure. Model 1 adjusts for age, race/ethnicity, and education. Model 2 additionally adjusts for alcohol use, body mass index, number of chronic conditions, vision (excellent, very good, good, fair, poor), and bodily pain (none, very mild, mild, moderate, severe). Model 3 additionally adjusts for Short Physical Performance Battery (SPPB) score.
In the overall study sample the median BP was 124/72 mm Hg. There was no association of systolic or diastolic BP with risk of incident falls, either as a continuous variable or in lower BP categories compared with systolic BP ≥140 mm Hg or diastolic BP >80 mm Hg in any of the adjusted models (Table 2). In Model 2 there was no association of BP with risk of falls in women with worse lower limb function (SPPB scores 9–12): IRR 0.997 (95% CI 0.992–1.002) per mm Hg increase in systolic BP and IRR 0.994 (95% CI 0.986–1.002) per mm Hg increase in diastolic BP.
Table 2.
Association of Blood Pressure with Fall Incidence (N=5969)*
| Crude Model | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N (%) | IRR† (95% CI) | p values |
IRR (95% CI) | p values |
IRR (95% CI) | p values |
IRR (95% CI) | p values |
|
| Systolic Blood Pressure | |||||||||
| continuous | 0.999 (0.996–1.002) | 0.52 | 0.999 (0.996–1.002) | 0.53 | 0.998 (0.994–1.001) | 0.20 | 0.998 (0.994–1.001) | 0.19 | |
| <120 mm Hg | 2003 (33.6) | 0.95 (0.83–1.09) | 0.50 | 0.96 (0.84–1.10) | 0.57 | 1.05 (0.91–1.21) | 0.52 | 1.06 (0.91–1.24) | 0.44 |
| 120–129 mm Hg | 1886 31.6) | 0.85 (0.74–0.98) | 0.02 | 0.89 (0.77–1.02) | 0.09 | 0.97 (0.83–1.12) | 0.64 | 1.01 (0.86–1.17) | 0.94 |
| 130–139 mm Hg | 1159 (19.4) | 0.87 (0.75–1.02) | 0.09 | 0.86 (0.74–1.01) | 0.06 | 0.96 (0.82–1.13) | 0.62 | 1.01 (0.86–1.2) | 0.87 |
| >=140 mm Hg | 921 (15.4) | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Diastolic Blood Pressure | |||||||||
| continuous | 0.994 (0.989–1.00) | 0.04 | 1.000 (0.995–1.005) | 0.92 | 0.997 (0.992–1.003) | 0.29 | 0.998 (0.992–1.003) | 0.42 | |
| <60 mm Hg | 327 (5.4) | 1.13 (0.91–1.4) | 0.28 | 0.94 (0.76–1.17) | 0.60 | 0.98 (0.79–1.23) | 0.87 | 0.97 (0.77–1.22) | 0.80 |
| 60–69 mm Hg | 1742 (29.2) | 1.08 (0.95–1.23) | 0.22 | 1.00 (0.88–1.14) | 0.95 | 1.06 (0.93–1.21) | 0.40 | 1.04 (0.90–1.20) | 0.57 |
| 70–79 mm Hg | 2586 (43.3) | 1.09 (0.97–1.23) | 0.16 | 1.03 (0.91–1.16) | 0.65 | 1.05 (0.92–1.19) | 0.48 | 1.03 (0.90–1.17) | 0.67 |
| >=80 mm Hg | 1314 (22.0) | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
There are two participants with missing blood pressure. Model 1 adjusts for age, race/ethnicity, and education. Model 2 additionally adjusts for alcohol use, body mass index, number of chronic conditions, vision (excellent, very good, good, fair, poor), and bodily pain (none, very mild, mild, moderate, severe). Model 3 additionally adjusts for Short Physical Performance Battery (SPPB) score. Results in bold font are statistically significant at p<0.05.
Incidence rate ratio, for continuous represents change in fall risk associated with 1 mm Hg increase in blood pressure
In the subgroup of 3900 women who were treated with antihypertensive drugs, distribution and range of BP was similar to the overall sample (median BP 125/72 mm Hg.) As in the overall study sample, the treated subgroup of women showed no significant associations of systolic BP with a risk of falls in any of the models (Table 3). In the crude model, higher diastolic BP as a continuous variable was associated with a decreased risk of falls. In the adjusted models, higher diastolic BP as a continuous variable was weakly associated with a decreased risk of falls in Model 2 (IRR 0.993 per mm Hg, 95% confidence interval 0.987– 1.000, p=0.04), and was similar in both strata of SPPB (score 1–8, IRR= 0.994, 95% CI 0.986–1.002; score 9–16, IRR= 0.992, 95% CI 0.982–1.002). After adjustment for SPPB score, the point estimate for fall risk associated with diastolic BP in Model 3 was similar to model 2, but was no longer statistically significant. In the crude model for the categorical analysis, compared to diastolic BP ≥80 mm Hg, BP 60–69 mm Hg was associated with a 22% increased fall risk and BP <60 mm Hg was associated with a 30% increase in fall risk. In the adjusted models, lower diastolic BP categories had IRR point estimate above unity, but the only significantly increased risk of falls compared to diastolic BP ≥80 mm Hg was in Model 2 in women with diastolic BP 60–69 mm Hg. However, only 6% of women had diastolic BP <60 mm Hg, so confidence intervals were wide for this category.
Table 3.
Association of Blood Pressure with Fall Incidence (treated hypertension, N=3900)*
| Crude Model | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N (%) | IRR† (95% CI) | p values |
IRR (95% CI) | p values |
IRR (95% CI) | p values |
IRR (95% CI) | p values |
|
| Systolic Blood Pressure | |||||||||
| continuous | 1.001 (0.998–1.005) | 0.50 | 1.00 (0.997–1.004) | 0.84 | 0.997 (0.993–1.001) | 0.13 | 0.997 (0.993–1.001) | 0.14 | |
| <120 mm Hg | 1177 (30.2) | 0.86 (0.73–1.01) | 0.06 | 0.89 (0.76–1.04) | 0.15 | 1.07 (0.90–1.26) | 0.45 | 1.07 (0.89–1.27) | 0.47 |
| 120–129 mm Hg | 1230 (31.5) | 0.88 (0.75–1.03) | 0.11 | 0.93 (0.79–1.09) | 0.35 | 1.01 (0.85–1.19) | 0.95 | 1.04 (0.88–1.24) | 0.62 |
| 130–139 mm Hg | 825 (21.2) | 0.90 (0.75–1.06) | 0.21 | 0.88 (0.75–1.05) | 0.15 | 1.05 (0.88–1.25) | 0.60 | 1.10 (0.91–1.32) | 0.31 |
| >=140 mm Hg | 668 (17.1) | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Diastolic Blood Pressure | |||||||||
| continuous | 0.992 (0.986–0.997) | 0.006 | 0.997 (0.991–1.003) | 0.31 | 0.993 (0.987–1.000) | 0.04 | 0.994 (0.988–1.000) | 0.07 | |
| <60 mm Hg | 223 (5.7) | 1.30 (1.02–1.65) | 0.03 | 1.09 (0.86–1.39) | 0.46 | 1.13 (0.89–1.44) | 0.33 | 1.12 (0.88–1.44) | 0.36 |
| 60–69 mm Hg | 1104 (28.3) | 1.22 (1.05–1.42) | 0.01 | 1.14 (0.98–1.32) | 0.09 | 1.17 (1.00–1.37) | 0.04 | 1.14 (0.97–1.34) | 0.11 |
| 70–79 mm Hg | 1656 (42.4) | 1.03 (0.89–1.18) | 0.69 | 1.00 (0.87–1.15) | 0.95 | 1.01 (0.88–1.17) | 0.85 | 1.00 (0.86–1.16) | 0.95 |
| >=80 mm Hg | 907 (23.2) | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
Model 1 adjusts for age, race/ethnicity, and education. Model 2 additionally adjusts for alcohol use, body mass index, number of chronic conditions, vision (excellent, very good, good, fair, poor), and bodily pain (none, very mild, mild, moderate, severe). Model 3 additionally adjusts for Short Physical Performance Battery (SPPB) score. Results in bold font are statistically significant at p<0.05. Results in bold font are statistically significant at p<0.05.
Incidence rate ratio, continuous represents change in fall risk associated with 1 mm Hg increase in blood pressure
Among the 3864 women who were treated with antihypertensive drugs in known classes, 42% were treated with thiazide diuretics, 41% with beta blockers, 37% with calcium channel blockers, 31% with angiotensin converting enzyme inhibitors, and 27% with angiotensin receptor blockers. In Model 1, after adjustment for demographics several drug classes were significantly associated with falls: thiazide diuretics had a 14% lower risk and beta blockers had a 23% increased risk (Table 4). After adjustment for other fall risk factors in Model 2, the higher fall risk in users of beta blockers persisted, but was no longer associated with falls after further adjustment for SPPB.
Table 4.
Association of falls with hypertension drug class and confounders (for treated hypertension subjects with known drugs, N=3864)*
| Drugs | N (%) | IRR† (95% CI) | p value | IRR (95% CI) | p value | IRR (95% CI) | p value | IRR (95% CI) | p value |
|---|---|---|---|---|---|---|---|---|---|
| Aldosterone inhibitor | 128 (3.3) | 1.06 (0.79–1.43) | 0.72 | 1.18 (0.88–1.59) | 0.26 | 1.05 (0.77–1.44) | 0.77 | 1.12 (0.81–1.54) | 0.50 |
| Alpha blocker | 34 (0.9) | 1.40 (0.82–2.47) | 0.22 | 1.29 (0.76–2.25) | 0.36 | 1.16 (0.66–2.07) | 0.62 | 1.22 (0.68–2.25) | 0.51 |
| Angiotensin converting enzyme inhibitor | 1192 (30.8) | 0.99 (0.87–1.13) | 0.86 | 0.97 (0.85–1.10) | 0.62 | 0.95 (0.83–1.09) | 0.45 | 0.94 (0.82–1.09) | 0.42 |
| Angiotensin receptor blocker | 1024 (26.5) | 0.97 (0.85–1.1) | 0.65 | 1.00 (0.87–1.13) | 0.99 | 1.08 (0.94–1.24) | 0.28 | 1.08 (0.93–1.25) | 0.29 |
| Beta blocker | 1572 (40.7) | 1.29 (1.15–1.44) | <0.0001 | 1.23 (1.10–1.37) | 0.0003 | 1.14 (1.01–1.28) | 0.03 | 1.06 (0.94–1.20) | 0.34 |
| Centrally acting | 86 (2.2) | 0.95 (0.66–1.38) | 0.79 | 1.07 (0.74–1.56) | 0.71 | 0.69 (0.44–1.07) | 0.09 | 0.69 (0.43–1.10) | 0.11 |
| Dihydropyridine calcium channel blocker | 1122 (29.0) | 0.85 (0.76–0.97) | 0.01 | 0.91 (0.81–1.03) | 0.13 | 0.98 (0.86–1.11) | 0.72 | 0.98 (0.86–1.12) | 0.79 |
| Direct Renin Inhibitor | 13 (0.3) | 1.08 (0.45–2.77) | 0.87 | 1.09 (0.46–2.74) | 0.84 | 1.39 (0.58–3.52) | 0.47 | 1.01 (0.38–2.74) | 0.99 |
| Nondihydropyridine calcium channel blocker | 309 (8.0) | 1.00 (0.82–1.23) | 1.00 | 1.01 (0.82–1.23) | 0.95 | 1.01 (0.82–1.25) | 0.91 | 1.00 (0.80–1.25) | 0.99 |
| Potassiumsparing diuretic | 282 (7.3) | 1.08 (0.86–1.35) | 0.51 | 1.10 (0.88–1.38) | 0.41 | 1.14 (0.91–1.4) | 0.26 | 1.13 (0.89–1.44) | 0.32 |
| Thiazide diuretic | 1625 (42.1) | 0.81 (0.72–0.91) | 0.0004 | 0.86 (0.77–0.97) | 0.01 | 0.90 (0.80–1.02) | 0.10 | 0.96 (0.85–1.09) | 0.53 |
| Vasodilator | 72 (1.9) | 0.95 (0.64–1.43) | 0.81 | 0.96 (0.65–1.43) | 0.85 | 1.10 (0.73–1.67) | 0.67 | 1.18 (0.78–1.80) | 0.44 |
Model 1 adjusts for age, race/ethnicity, and education. Model 2 additionally adjusts for alcohol use, body mass index, number of chronic conditions, vision (excellent, very good, good, fair, poor), and bodily pain (none, very mild, mild, moderate, severe). Model 3 additionally adjusts for Short Physical Performance Battery (SPPB) score. Results in bold font are statistically significant at p<0.05.
Incidence rate ratio
DISCUSSION
This analysis of a large, diverse cohort of community-dwelling ambulatory women with a mean age of 79 years did not show an association of hypertension or hypertension treatment with falls assessed prospectively on a monthly basis for about one year. The level of systolic BP was not associated with falls in either the overall sample or in women treated with antihypertensive medication. In women treated with antihypertensive medication, higher diastolic BP was associated with a lower risk of falls in the unadjusted model and in the model adjusted for demographics, alcohol use, BMI, chronic conditions, vision, and bodily pain (<1% decrease in risk per mm Hg increase in BP). The categorical analysis also suggested an increased fall risk in women with diastolic BP <70 mm Hg. This association was attenuated with further control for SPPB score, suggesting that physical function could be part of the mechanistic pathway between diastolic BP and falls. Beta blockers were the only class of antihypertensive medication that was associated with an increased risk of falls compared with all other types of antihypertensive drugs. The increased risk was attenuated after adjustment for fall risk factors, and became non-significant after adjusting for lower limb physical function, suggesting that the association may be related to differential use of beta blockers among women with fall risk factors.
Given the lack of evidence for an association of long-term antihypertensive treatment with falls, why do clinicians commonly cite the risk of falls as a reason not to treat to lower BP targets in older individuals? In contrast to the weak inverse association of seated diastolic BP with self-reported falls in the current study among treated women treated for hypertension, Bromfield, et al did not find an association of either seated systolic or diastolic BP with serious fall injuries ascertained via a claims algorithm.13 Further study is needed on whether low levels of treated diastolic BP are associated with an increased risk of falls, and whether a different mechanism links diastolic versus systolic BP with fall propensity.
Orthostatic hypotension (a drop in blood pressure on standing), which becomes more prevalent with aging and is more common in individuals with hypertension, might be another link between antihypertensive treatment and falls.26–28 Juraschek, et al reported that orthostatic hypotension in middle-aged adults was positively associated with falls, fractures, and syncope during a median of 23 years of follow-up.29 Finucane, et al also found a 40% increased risk of falls at 2 years of follow-up in people with orthostatic hypotension in a population-based study prospective study in Irish adults.30 The SPRINT study also supports this finding,31 as do smaller and cross-sectional studies, 28,32 although one moderately large prospective study does not.33
Some observational studies, but not others, found an association of antihypertensive treatment with orthostatic hypotension.26,32,34,35 However, there is little evidence that antihypertensive treatment itself results in a greater degree of orthostatic hypotension than would otherwise be found in a given hypertensive person. Two trials that achieved substantial BP reduction through intensive treatment, Action to Control Cardiovascular Risk in Diabetes (ACCORD) and SPRINT, did not observe any difference in the presence or degree of documented orthostatic hypotension in the intensive and standard treatment groups.7,36,37 In these trials, few participants with dizziness on standing had orthostatic hypotension, and conversely most orthostatic hypotension was not accompanied by symptoms of dizziness on standing. Two other randomized trials comparing different BP lowering strategies did not report measures of orthostatic hypotension, but the Stop Atherosclerosis in Native Diabetics Study (SANDS) found that 35% of participants in the intensive BP group (mean systolic BP 116 mm Hg achieved on treatment) reported generalized dizziness, compared with 17% in the standard group (mean systolic BP 128 mm Hg).38 In contrast, in the Secondary Prevention of Subcortical Strokes Study (SPS3), there were no differences in reports of dizziness, unsteadiness, or lightheadedness on standing between the treatment groups (mean systolic BP 127 and 138 mm Hg.)39 In summary, little evidence supports an association of antihypertensive treatment with falls that is mediated by low levels of seated blood pressure or orthostatic hypotension.
The current study has many strengths including its large, racially and geographically diverse study population in which 43% reported one or more falls. There was detailed information on antihypertensive treatment from a medication inventory and BP was measured according to a standardized protocol by trained technicians. Follow-up was prospective and falls were recorded daily and reported on a monthly basis to minimize the chance of unreported falls. However, some limitations of the study need to be acknowledged. Although repeated BP measures were averaged, BP was measured only on a single day and was performed manually using an anaeroid sphygmomanometer. Some antihypertensive medications may be used for other indications (eg, migraines, heart failure.) While it is possible that usual BP and hypertension treatment status could have been misclassified, it is unlikely that misclassification was differential in those who eventually experienced a fall and those who did not. Some of the antihypertensive medication classes were uncommonly used, but the classes that are commonly used in clinical practice were well-represented. We did not include duration of treatment in our analysis, but it is likely that most antihypertensive drugs listed in the medication inventory had been used for longer than the 14–45 day period where falls may be increased following initiation or titration of antihypertensive treatment. The study included only women participating in WHI and OPACH, and data on cognitive function were not available for most women. Thus, it is unknown if findings would be similar in men or patients with frailty, cognitive impairment, or multiple co-morbidities so severe that they would be unlikely to participate in research.
In conclusion, there is little evidence for a causal mechanism or an association of chronic antihypertensive treatment with falls in the literature9–13 or in this study, even in the subgroup of women with increased falls risk due to low measured physical function. However, there is a growing body of evidence that the risk of falls and fractures is increased in the first several weeks following initiation or intensification of antihypertensive therapy.14–18 To ensure that antihypertensive treatment initiation or intensification is needed, care should be taken to measure BP accurately in the office setting. In patients who are suspected of having isolated elevated office BP, out-of-office BP measurements should be considered to confirm the need for additional treatment in accordance with current guidelines.40 While the risk of a serious fall injury is low, it is reasonable to monitor patients in the early period following starting a new antihypertensive or dose intensification. For patients who are doing well and tolerating a new treatment regimen after the first several weeks, it seems likely that the long-term benefits of improved hypertension control can be achieved without an increased risk for falls.
Acknowledgements
WHI Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Joan McGowan, Leslie Ford, and Nancy Geller. Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg. Investigators and Academic Centers: (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Jennifer Robinson; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker; (University of Nevada, Reno, NV) Robert Brunner; (University of Minnesota, Minneapolis, MN) Karen L. Margolis. Women’s Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Mark Espeland. For a list of all the investigators who have contributed to WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
Sources of Funding: The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, and HHSN268201600004C. This work was additionally supported by National Heart, Lung and Blood Institute (grant R01HL105065).
Sponsor’s role
The sponsor had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Footnotes
Clinical Trials Registration: ClinicalTrials.gov identifier NCT00000611.
Conflict of interest
The authors have no conflicts of interest to disclose.
Contributor Information
Karen L. Margolis, HealthPartners Institute.
David M. Buchner, University of Illinois at Urbana Champaign.
Michael J. LaMonte, University at Buffalo.
Yuzheng Zhang, Fred Hutchinson Cancer Research Center.
Chongzhi Di, Fred Hutchinson Cancer Research Center.
Eileen Rillamas-Sun, Fred Hutchinson Cancer Research Center.
Julie Hunt, Fred Hutchinson Cancer Research Center.
Farha Ikramuddin, University of Minnesota.
Wenjun Li, University of Massachusetts.
Steve Marshall, University of North Carolina.
Dori Rosenberg, Kaiser Permanente Washington Health Research Institute.
Marcia L. Stefanick, Stanford University.
Robert Wallace, University of Iowa.
Andrea Z. LaCroix, University of California San Diego.
References
- 1.Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet 1990;335(8693):827–838, [DOI] [PubMed] [Google Scholar]
- 2.Turnbull F, Blood Pressure Lowering Treatment Trialists C. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003;362(9395):1527–1535, [DOI] [PubMed] [Google Scholar]
- 3.Czernichow S, Zanchetti A, Turnbull F, et al. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. J Hypertens 2011;29(1):4–16, 10.1097/HJH.0b013e32834000be. [DOI] [PubMed] [Google Scholar]
- 4.Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged >/=65 Years - United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65(37):993–998, 10.15585/mmwr.mm6537a2. [DOI] [PubMed] [Google Scholar]
- 5.Curb JD, Applegate WB, Vogt TM, et al. Antihypertensive therapy and falls and fractures in the systolic hypertension in the elderly program. J Am Geriatr Soc 1993;41(SA15), [Google Scholar]
- 6.Margolis KL, Palermo L, Vittinghoff E, et al. Intensive blood pressure control, falls, and fractures in patients with type 2 diabetes: the ACCORD trial. J Gen Intern Med 2014;29(12):1599–1606, 10.1007/s11606-014-2961-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Group SR, Wright JT Jr., Williamson JD, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med 2015;373(22):2103–2116, 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters R, Beckett N, Burch L, et al. The effect of treatment based on a diuretic (indapamide) +/− ACE inhibitor (perindopril) on fractures in the Hypertension in the Very Elderly Trial (HYVET). Age Ageing 2010;39(5):609–616, 10.1093/ageing/afq071. [DOI] [PubMed] [Google Scholar]
- 9.Tinetti ME, Han L, Lee DS, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med 2014;174(4):588–595, 10.1001/jamainternmed.2013.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc 1999;47(1):40–50, [DOI] [PubMed] [Google Scholar]
- 11.Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 2009;169(21):1952–1960, 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 12.Butt DA, Harvey PJ. Benefits and risks of antihypertensive medications in the elderly. J Intern Med 2015;278(6):599–626, 10.1111/joim.12446. [DOI] [PubMed] [Google Scholar]
- 13.Bromfield SG, Ngameni CA, Colantonio LD, et al. Blood Pressure, Antihypertensive Polypharmacy, Frailty, and Risk for Serious Fall Injuries Among Older Treated Adults With Hypertension. Hypertension 2017;70(2):259–266, 10.1161/HYPERTENSIONAHA.116.09390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berry SD, Zhu Y, Choi H, Kiel DP, Zhang Y. Diuretic initiation and the acute risk of hip fracture. Osteoporos Int 2013;24(2):689–695, 10.1007/s00198-012-2053-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med 2012;172(22):1739–1744, 10.1001/2013.jamainternmed.469. [DOI] [PubMed] [Google Scholar]
- 16.Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of falls on initiation of antihypertensive drugs in the elderly. Osteoporos Int 2013;24(10):2649–2657, 10.1007/s00198-013-2369-7. [DOI] [PubMed] [Google Scholar]
- 17.Gribbin J, Hubbard R, Gladman J, Smith C, Lewis S. Risk of falls associated with antihypertensive medication: self-controlled case series. Pharmacoepidemiol Drug Saf 2011;20(8):879–884, 10.1002/pds.2176. [DOI] [PubMed] [Google Scholar]
- 18.Shimbo D, Barrett Bowling C, Levitan EB, et al. Short-Term Risk of Serious Fall Injuries in Older Adults Initiating and Intensifying Treatment With Antihypertensive Medication. Circ Cardiovasc Qual Outcomes 2016;9(3):222–229, 10.1161/CIRCOUTCOMES.115.002524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Design of the Women’s Health Initiative clinical trial and observational study. The Women’s Health Initiative Study Group. Control Clin Trials 1998;19(1):61–109, [DOI] [PubMed] [Google Scholar]
- 20.Anderson GL, Manson J, Wallace R, et al. Implementation of the Women’s Health Initiative study design. Ann Epidemiol 2003;13(9 Suppl):S5–17, [DOI] [PubMed] [Google Scholar]
- 21.LaCroix AZ, Rillamas-Sun E, Buchner D, et al. The Objective Physical Activity and Cardiovascular Disease Health in Older Women (OPACH) Study. BMC Public Health 2017;17(1):192, 10.1186/s12889-017-4065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Life Study Materials/Long Life Study Table of Data Collection Activities 2017; https://www.whi.org/studies/SitePages/Long%20Life%20Study.aspx.
- 23.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000;55(4):M221–231, [DOI] [PubMed] [Google Scholar]
- 24.Simonsick EM, Gardner AW, Poehlman ET. Assessment of physical function and exercise tolerance in older adults: reproducibility and comparability of five measures. Aging (Milano) 2000;12(4):274–280, [DOI] [PubMed] [Google Scholar]
- 25.Rillamas-Sun E, LaCroix AZ, Bell CL, Ryckman K, Ockene JK, Wallace RB. The Impact of Multimorbidity and Coronary Disease Comorbidity on Physical Function in Women Aged 80 Years and Older: The Women’s Health Initiative. J Gerontol A Biol Sci Med Sci 2016;71 Suppl 1:S54–61, 10.1093/gerona/glv059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finucane C, O’Connell MD, Fan CW, et al. Age-related normative changes in phasic orthostatic blood pressure in a large population study: findings from The Irish Longitudinal Study on Ageing (TILDA). Circulation 2014;130(20):1780–1789, 10.1161/CIRCULATIONAHA.114.009831. [DOI] [PubMed] [Google Scholar]
- 27.Fedorowski A, Stavenow L, Hedblad B, Berglund G, Nilsson PM, Melander O. Orthostatic hypotension predicts all-cause mortality and coronary events in middle-aged individuals (The Malmo Preventive Project). Eur Heart J 2010;31(1):85–91, 10.1093/eurheartj/ehp329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension 1992;19(6 Pt 1):508–519, [DOI] [PubMed] [Google Scholar]
- 29.Juraschek SP, Daya N, Appel LJ, et al. Orthostatic Hypotension in Middle-Age and Risk of Falls. Am J Hypertens 2017;30(2):188–195, 10.1093/ajh/hpw108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finucane C, O’Connell MD, Donoghue O, Richardson K, Savva GM, Kenny RA. Impaired Orthostatic Blood Pressure Recovery Is Associated with Unexplained and Injurious Falls. J Am Geriatr Soc 2017;65(3):474–482, 10.1111/jgs.14563. [DOI] [PubMed] [Google Scholar]
- 31.Sink KM, Evans GW, Shorr RI, et al. Syncope, Hypotension, and Falls in the Treatment of Hypertension: Results from the Randomized Clinical Systolic Blood Pressure Intervention Trial. J Am Geriatr Soc 2018;66(4):679–686, 10.1111/jgs.15236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heitterachi E, Lord SR, Meyerkort P, McCloskey I, Fitzpatrick R. Blood pressure changes on upright tilting predict falls in older people. Age Ageing 2002;31(3):181–186, [DOI] [PubMed] [Google Scholar]
- 33.Gangavati A, Hajjar I, Quach L, et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc 2011;59(3):383–389, 10.1111/j.1532-5415.2011.03317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Verwoert GC, Mattace-Raso FU, Hofman A, et al. Orthostatic hypotension and risk of cardiovascular disease in elderly people: the Rotterdam study. J Am Geriatr Soc 2008;56(10):1816–1820, 10.1111/j.1532-5415.2008.01946.x. [DOI] [PubMed] [Google Scholar]
- 35.Hajjar I Postural blood pressure changes and orthostatic hypotension in the elderly patient: impact of antihypertensive medications. Drugs Aging 2005;22(1):55–68, [DOI] [PubMed] [Google Scholar]
- 36.Fleg JL, Evans GW, Margolis KL, et al. Orthostatic Hypotension in the ACCORD (Action to Control Cardiovascular Risk in Diabetes) Blood Pressure Trial: Prevalence, Incidence, and Prognostic Significance. Hypertension 2016;68(4):888–895, 10.1161/HYPERTENSIONAHA.116.07474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs Standard Blood Pressure Control and Cardiovascular Disease Outcomes in Adults Aged >/=75 Years: A Randomized Clinical Trial. JAMA 2016;315(24):2673–2682, 10.1001/jama.2016.7050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weir MR, Yeh F, Silverman A, et al. Safety and feasibility of achieving lower systolic blood pressure goals in persons with type 2 diabetes: the SANDS trial. J Clin Hypertens (Greenwich) 2009;11(10):540–548, 10.1111/j.1751-7176.2009.00121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Group SPSS, Benavente OR, Coffey CS, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet 2013;382(9891):507–515, 10.1016/S0140-6736(13)60852-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017, 10.1161/HYP.0000000000000065. [DOI]


