Abstract
The majority of studies investigating the relationship between racism/racial discrimination and birth outcomes have focused on perceived experiences of racism/racial discrimination directed at oneself (personal racism). However, evidence suggests individuals report with greater frequency racism/racial discrimination directed at friends, family members, or other members of their racial/ethnic group (group racism). We examined how much African American (AA) women report lifetime experiences of perceived racism or racial discrimination, both personal and group, varied by maternal age. We also investigated whether reports of personal and group racism/racial discrimination were associated with the risk of delivering a small-for-gestational age (SGA) infant and how much maternal age in relation to developmental life stages (adolescence [≤ 18 years], emerging adulthood [19–24 years], and adulthood [≥ 25 years]) moderated the relationship. Data stem from the Baltimore Preterm Birth Study, a hybrid prospective/retrospective cohort study that enrolled 872 women between March 2000 and July 2004 (analyzed in 2016–2017). Spline regression analyses demonstrated a statistically significant (p value for overall association < 0.001) and non-linear (p value = 0.044) relationship between maternal age and the overall racism index. Stratified analysis showed experiences of racism overall was associated with a higher odds ratio of delivering an SGA infant among AA women aged ≥ 25 years (OR = 1.45, 95% CI 1.02–2.08). The overall racism index was not associated with the SGA infant odds ratio for emerging adults (OR = 0.86, 95% CI 0.69–1.06) or adolescents (OR = 0.92, 95% CI 0.66–1.28). Multiple aspects of racism and the intersection between racism and other contextual factors need to be considered.
Keywords: Life course, Emerging adults, Racism, African Americans, Adverse birth outcomes, Birth weight, Gestational age
Introduction
In 2014, the United States of America (USA) reached a historic low rate in infant mortality (5.82 deaths/1000 live births) [1]; however, substantial racial disparities in infant health persist. Since the early 1970s, African American (AA) infants have had a persistent infant mortality rate more than twice the rate of Whites; 2014 data show 10.93 deaths/1000 live births for non-Hispanic Blacks/AA and 4.89 deaths/1000 live births for non-Hispanic Whites [2]. Racial disparities of similar magnitude are also seen for preterm birth (PTB; born < 37 weeks of gestation) and low birth weight (BW; born < 2500 g) [3, 4], both are leading infant mortality causes [5, 6]. Fetal growth restriction, an adverse birth outcome seen in preterm and term infants that is independently associated with infant mortality [7], also disproportionately affects AAs [8–10]. While national rates are not available, studies examining racial/ethnic disparities in fetal growth report the risk of delivering a small-for-gestational age (SGA) infant for AA women is twofold greater than that for non-Hispanic White women [8, 9, 11–13]. Most recently, Grobman et al. [13] report the frequency of SGA infant for AA women in a large multisite US study (N = 9470) was 2.2 times (95% confidence interval 1.9–2.6) the frequency for non-Hispanic Whites (17.2 vs 8.6%).
Considerable effort has been devoted to trying to understand the reasons behind the racial/ethnic disparity in birth outcomes. However, a relatively small portion of this disparity can be attributed to Black-White differentials in exposure to pre- and perinatal risk factors (e.g., social disadvantage, infection, medical comorbidities, smoking, prenatal care, health insurance) that are traditionally incorporated in health disparity studies [14–18]. Despite widespread acknowledgement of race, not as a biological but as a social construct, the implications of race on health and health policy in race-conscious societies have not been fully studied [19]. In the USA, racial classification is a life course phenomenon [20–22] and a system for continued maintenance of social dominance [23]. Thus, race is a proxy for limited access to resources, systemic oppression, intergenerational social exclusion, and life challenges in marginalized communities. As a lived experience, racial hierarchies and discrimination are a common part of daily AA life experiences [21, 24].
In fact, in their most recent meta-analytic review of health literature, Paradies et al. [25] established racism as a major determinant of health for marginalized Americans with both systemic and interpersonal routes. They reported that racism is associated with poorer health overall (general, physical health, mental health, anxiety, depression, psychological stress). However, while ethnicity buffered some of the effects of racism on health outcomes for Latino and Asian populations, sadly this was not the case for AAs. In relation to birth outcomes, the literature on racism/racial discrimination provides both null and adverse findings [26–31]. Studies documenting an adverse relationship show perceived experiences of racism/racial discrimination increased AA women’s risk of having an adverse birth outcome with the increase ranging from 30% to threefold. In one of the few studies investigating fetal growth specifically as a birth outcome, Hilmert and colleagues [10] found experiences of racism occurring in childhood interacted with maternal blood pressure to predict fetal growth restriction among AAs. The heterogeneity in findings for birth outcome studies may be due in part to the conceptualization and measurement of AA’s lived experiences of racism/racial discrimination [30, 32].
Harrell [22], in her multidimensional conceptualization of racism-related stress, defines racism-related stress as “the race-related transactions between individuals or groups and their environment that emerge from the dynamics of racism, and are perceived to tax or exceed existing individual or collective resources or threaten well-being,” (p. 44) and posits that racism may exert its influences on a person through direct and vicarious daily life experiences and micro stressors, as well as through the collective experiences of the racial/ethnic group with whom an individual self-identifies. The majority of studies investigating racism/racial discrimination and the risk of poor birth outcomes have studied only perceived racism experiences directed at oneself (personal racism) [29, 32]. Yet, evidence suggests that individuals report with greater frequency of racism/racial discrimination directed at friends, family members, or other members of their racial or ethnic group (group racism) [29, 33–37].
Principles central to the life course perspective are concepts of age-patterned exposures, sensitive periods, and linked lives [20]. Recently, Gee et al. [20] emphasized the importance of using a life course framework to illustrate how the effects of racism on health could be minimized if lived experiences of racism/racial discrimination from birth to death and through different developmental stages are incompletely acknowledged. In reviewing the current literature on birth outcomes, we found considerable heterogeneity in timeframe when exposure to racism/racial discrimination was measured (e.g., past year, during pregnancy, lifetime) [10, 26, 29, 30, 38–42]. To our knowledge, only two studies [42, 43] have assessed whether racism/racial discrimination and its impact on birth outcomes were associated with age and time; both variables have biologic, developmental, and social significance [20]. However, both studies focused solely on women aged 14 to 21 years [42].
The purpose of this study is to examine reports of perceived racism/racial discrimination and its impact on the lives of childbearing AA women from a life course perspective. First, we examined whether AA women’s reports of lifetime racism experiences (overall, personal, and group) varied by maternal age. Second, using the biopsychosocial model [44], we investigated whether personal and group racism experiences were associated with the risk of delivering an SGA infant and how much maternal age in relation to developmental life stages (adolescence [≤ 18 years], emerging adulthood [19–24 years], and adulthood [≥ 25 years]) moderated the relationship.
Materials and Methods
Study Design and Data Collection
Details about the Baltimore PTB Study have been previously published [29, 41, 45] in brief, a hybrid prospective/retrospective cohort design was utilized to enroll women over a 41-month period (March 2001–July 2004). Women were recruited either prenatally from a Johns Hopkins Medical Institution (JHMI) satellite prenatal clinic or postnatally (during the postpartum hospitalization) if they delivered a live-born infant. Eligibility was further restricted to women who resided in Baltimore City, Maryland, and self-identified as Black or African American since 95% of women receiving care at the participating JHMI satellite clinics were residents of Baltimore City, Maryland, and 90% of all JHMI deliveries were to Black or African American women.
This study was approved by the institutional review board at Johns Hopkins University. Of women who received prenatal care from participating JHMI clinics, 677 women were eligible for the study; 485 (72%) consented and were enrolled between 22 and 28 weeks of gestation. With respect to postpartum recruitment, 606 women with intermittent or no prenatal care who delivered at JHMI met study eligibility criteria; 387 (64%) consented and were enrolled during their postpartum hospitalization. Trained study staff collected information on social, psychosocial, and biomedical factors via structured interview and medical record review. Women who were enrolled prenatally were interviewed between 22 and 28 weeks of gestation and again during their postpartum hospitalization; those who were enrolled postnatally were interviewed only during their hospitalization stay, and postpartum interviews typically occurred within 24–48 h after delivery. To reduce the possibility of bias in participants’ responses on interview questions related to race or racism, also known as race-of-interviewer effect, all interviewers for this study were Black or African American and female [46].
A total of 872 women consented and were enrolled and interviewed for the Baltimore Preterm Birth Study—a 68% response rate. Women served by JHMI had a median age of 20 years, their median year of education was 11.2, and the preterm birth rate was 15%. Women who were enrolled in the Baltimore Preterm Birth Study had a median age of 22 years, their median year of education was 11, and the preterm birth rate was 16.4%.
Sample
For this analysis, we excluded women who delivered a multiple birth (n = 24) since the birth weight-for-gestational age distributions differ for singleton and multiple births [47]. We also excluded 22 women who were enrolled and interviewed prenatally, but then lost to follow-up in 2001 when the university had a shutdown of all research. Lastly, women with missing data on the exposure, experiences of personal or group racism (n = 42), gestational age (GA; n = 16), or BW (n = 8) were excluded. The final analytic sample included 778 women. Women who were enrolled prenatally did not significantly differ from those who were enrolled postnatally on exposure or outcome variables [48].
Measures
Exposure
Using methods by Caughy et al. [49] and applying them in our publication on prenatal care and racism [29], we created an index of overall racism and two sub-indices using items from the Racism and Lifetime Experience Scale (RaLES)-Brief questionnaire developed by Harrell et al. (Harrell S, Merchant M, Young S 1997. Psychometric properties of the racism and life experiences scales (RaLES). Unpublished manuscript; Harrell SP 1997. Development and initial validation of scales to measure racism-related stress. Unpublished manuscript). The RaLES-Brief questionnaire includes nine items assessing direct, vicarious, and collective experiences of racism in addition to information on the stressfulness of those experiences (Harrell S, Merchant M, Young S 1997. Psychometric properties of the racism and life experiences scales (RaLES). Unpublished manuscript; Harrell SP 1997. Development and initial validation of scales to measure racism-related stress. Unpublished manuscript). In particular, we used four items to distinguish personal experiences from group-related experiences including the following: (1) overall, during your lifetime, how much have you personally experienced racism, racial prejudice, or racial discrimination [personal]; (2) during the past year, how much have you personally experienced racism, racial prejudice, or racial discrimination [personal]; (3) how much racism had affected the life experiences of people close to them [group]; (4) and how much they thought racism affected the lives of others belonging to their racial/ethnic group [group]. Each question was answered using a 5-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”).
The overall racism index was created by summing women’s responses on each of the four items together ranging from 0 to 16; a higher score reflected greater amounts of experienced racism. The following two sub-indices were created: one reflective of personal racism and another reflective of group racism; each ranged from 0 to 8. Internal reliability, measured using Cronbach’s α, for the overall racism index and the personal and group sub-indices was 0.73, 0.82, and 0.61, respectively.
Outcome
SGA was operationalized using the cut point defined for the BW ratio continuous measure [50] defined as the observed BW divided by the expected BW for the infant’s GA. The expected BW was determined using a sex-specific U.S. fetal growth curve by Talge et al. [51].
Potential Effect Modifier
Our cohort included adolescents in substantial numbers (~ 11%, ≤ 18 years) as there was no lower limit for age eligibility. It has been reported that age may influence reporting about racism experiences; younger individuals are more likely to state they have not experienced racism or racial discrimination [20]. Hence, maternal age (continuous) was examined as a potential modifier. Maternal age was also stratified into three groups which align with the developmental literature and the concept of emerging adulthood [52, 53]: adolescence (≤ 18 years), emerging adulthood (19–24 years), and adulthood (≥ 25 years).
Covariates
Potential confounding variables considered for inclusion were parity (number of live births), recruitment status (prenatal or postnatal), and socioeconomic variables as follows: years of education, employment during pregnancy (yes/no), receipt of Medicaid insurance during pregnancy, maternal height (cm), and the Family Resource Scale (FRS) [54]. The 25-item FRS assesses the adequacy of household resources in relation to time and money (e.g., having enough money to “buy food for 2 meals/day” and to “pay the rent/mortgage” and/or having “time to socialize with friends and family”) [51]. Women responded using a 5-point Likert scale ranging from 1 (“almost always”) to 5 (“almost never”). The FRS theoretically ranges from 25 to 125; a lower score reflects greater adequacy in household resources. The FRS has three subscales: essential money, non-essential money, and leisure time [29, 55]. The internal reliability, estimated by Cronbach’s α, was high (≥ 0.80) for the FRS and its subscales. Each covariate was assessed for missing values. Due to the degree of missing data exhibited in the analytic sample for maternal height (12.6%), the FRS (5%), and Medicaid status (5%), expectation-maximization algorithm [56] was used to impute missing values for these items.
Statistical Analysis
Stata version 14 (College Station, TX) was used to conduct statistical analyses (June 2016–May 2017). Bivariate analyses were used to compare the mean and SD for each racism index and maternal characteristics of the analytic sample and by age group. As mentioned previously, one’s age may influence the reporting and exposure to racism or experiences of unfair treatment related to race. Hence, we used spline regression to assess the age-racism association and examine the relationship for any non-linearities. We used restricted cubic spline transformations as they permit a high degree of flexibility when modeling potential non-linear relationships between two variables; they also administer constraints that ensure a smooth curve as well as linearity in the tails of the function [57, 58]. Spline transformation of maternal age with 4 df was employed using the Stata package POSTRCSPLINE [59] and knots placed at the 5th, 35th, 65th, and 95th percentiles of maternal age [60]. The spline transformations were then incorporated as predictor variables into linear regression models where the racism measure served as the outcome.
Logistic regression was used to assess associations between each racism measure and SGA odds ratio, allowing for calculation of ORs and their corresponding 95% CIs. To account for the possibility of maternal age moderating the relationship between racism and delivery of an SGA infant, an interaction term between the racism measure and maternal age, as a continuous variable, was included into the regression model. Significance of the interaction term was evaluated using the likelihood ratio test; a p value < 0.10 was used for a level of statistical significance. Next, regression models were stratified by maternal age (≤ 18, 19–24, and ≥ 25 years) to further explore interactions. The final age-stratified models were adjusted for maternal education, Medicaid status, essential money, parity, and recruitment status.
Results
Sample Characteristics
Table 1 displays maternal characteristics for this study’s 778 AA women. Women were relatively young with a mean age of 23.3 years (SD 5.7), and nearly half (48.1%) had ≤ 12 years of education and no diploma/GED. In terms of household resources for themselves and their family, more than half (54.1%) reported having unmet or inadequate needs met for essential resources.
Table 1.
Distribution of racism indices and maternal characteristics for the Baltimore Preterm Birth Study (N = 778), Baltimore City, Maryland, 2001–2004
| Sample characteristics | Total sample (N = 778) | Maternal age | p valuec | ||
|---|---|---|---|---|---|
| ≤ 18 years (n = 167) | 19–24 years (n = 354) | ≥ 25 years (n = 257) | |||
| N (%) | n (%) | n (%) | n (%) | ||
| Overall racism index | |||||
| Mean (SD) | 2.5 (1.2) | 2.2 (1.2) | 2.5 (1.3) | 2.7 (1.2) | < 0.01 |
| 0 item acknowledged | 48 (6.2) | 15 (9.0) | 22 (6.2) | 11 (4.4) | |
| 1 item acknowledged | 127 (16.3) | 32 (19.2) | 61 (17.2) | 34 (13.2) | |
| 2 items acknowledged | 205 (26.4) | 53 (31.7) | 83 (23.5) | 69 (26.9) | |
| 3 items acknowledged | 169 (21.7) | 32 (19.2) | 77 (21.8) | 60 (23.4) | |
| 4 items acknowledged | 229(29.4) | 35 (21.0) | 111 (31.4) | 83 (32.3) | |
| Personal racism sub-index | |||||
| Mean (SD) | 0.9 (0.9) | 0.7 (0.8) | 0.9 (0.9) | 1.0 (0.9) | 0.01 |
| 0 item acknowledged | 333 (42.8) | 87 (52.1) | 149 (42.1) | 97 (38.5) | |
| 1 item acknowledged | 181 (23.3) | 37 (22.2) | 80 (22.6) | 64 (24.9) | |
| 2 item acknowledged | 264 (33.9) | 43 (25.8) | 125 (35.3) | 96 (37.4) | |
| Group racism sub-index | |||||
| Mean (SD) | 1.6 (0.6) | 1.5 (0.7) | 1.6 (0.6) | 1.7 (0.6) | 0.02 |
| 0 item acknowledged | 55 (7.1) | 18 (10.8) | 25 (7.1) | 12 (4.7) | |
| 1 item acknowledged | 195 (25.1) | 47 (28.1) | 86 (24.9) | 62 (24.1) | |
| 2 items acknowledged | 528 (67.9) | 102 (61.1) | 243 (68.6) | 183 (71.2) | |
| Recruitment status | 0.30 | ||||
| Prenatal | 429 (55.1) | 74 (44.3) | 150 (42.4) | 125 (48.6) | |
| Postpartum | 349 (44.9) | 93 (55.7) | 204 (57.6) | 132 (51.4) | |
| Maternal age (years) | |||||
| Mean (SD) | 23.3 (5.7) | 17.0 (1.3) | 21.4 (1.6) | 29.8 (4.4) | – |
| Maternal education | < 0.001 | ||||
| Mean grade level (SD) | 11.2 (1.7) | 10.3 (1.5) | 11.3 (1.4) | 11.7 (1.9) | |
| ≤ 12 years, no diploma/GEDa | 374 (48.1) | 123 (73.5) | 155 (43.8) | 96 (37.4) | |
| ≤ 12 years, diploma/GEDb | 326 (41.9) | 41 (24.7) | 169 (47.7) | 116 (45.1) | |
| > 12 years | 78 (10.0) | 3 (1.9) | 30 (8.5) | 45 (17.5) | |
| Family Resource Scale | |||||
| Essential money | |||||
| Mean (SD) | 20.1 (6.9) | 19.0 (5.9) | 20.5 (6.7) | 20.3 (7.7) | |
| Quartile 1 (more) | 154 (19.8) | 37 (22.2) | 52 (14.7) | 65 (25.3) | 0.01 |
| Quartile 2 | 203 (26.1) | 45 (27.0) | 101 (28.5) | 57 (22.2) | |
| Quartile 3 | 219 (28.2) | 52 (31.1) | 101 (28.5) | 66 (25.7) | |
| Quartile 4 (less) | 202 (26.0) | 33 (19.8) | 100 (28.3) | 69 (26.9) | |
| Non-essential money | |||||
| Mean (SD) | 13.7 (5.2) | 13.1 (4.9) | 14.0 (5.1) | 13.5 (5.6) | |
| Quartile 1 (more) | 145 (18.6) | 29 (17.4) | 57 (16.1) | 59 (23.0) | 0.01 |
| Quartile 2 | 235 (30.2) | 67 (40.1) | 105 (29.7) | 63 (24.5) | |
| Quartile 3 | 198 (25.5) | 39 (23.4) | 92 (26.0) | 67 (26.1) | |
| Quartile 4 (less) | 200 (25.7) | 32 (19.2) | 100 (28.3) | 68 (26.5) | |
| Marital status | < 0.001 | ||||
| Single/separated/divorced | 428 (55.0) | 44 (26.4) | 164 (46.3) | 142 (55.3) | |
| Married/cohabitating | 350 (45.0) | 123 (73.7) | 190 (53.7) | 115 (44.8) | |
| Previous live births | < 0.001 | ||||
| Nulliparous | 279 (35.9) | 143 (85.6) | 111 (31.4) | 25 (9.7) | |
| Primiparous | 206 (26.3) | 20 (12.0) | 139 (39.3) | 47 (18.3) | |
| ≥ 2 live births | 293 (37.7) | 4 (2.4) | 104 (29.4) | 185 (72.0) | |
| Medicaid (yes) | 509 (65.4) | 106 (63.5) | 246 (69.5) | 157 (61.1) | 0.08 |
| Maternal height (cm) | |||||
| Mean (SD) | 162.7 (7.6) | 162.2 (7.1) | 162.2 (7.3) | 163.9 (8.2) | 0.02 |
| Preterm birth | 125 (16.1) | 25 (15.0) | 60 (17.0) | 40 (15.6) | 0.82 |
| SGA | 147 (18.9) | 35 (21.0) | 75 (21.2) | 37 (14.4) | 0.08 |
aOnly 13 women had 12 years of education and no diploma or GED
bThirty-six women had less than 12 years of education but had obtained a GED
cp values estimated with the chi-square test, except for the racism measures which were estimated with ANOVA
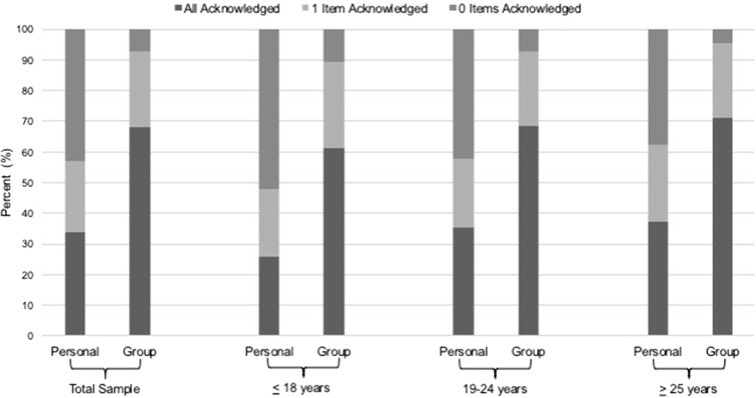
Personal Versus Group Racism and Maternal Age
Table 1 also provides the sample distribution for the overall racism index and the personal and group racism sub-indices. The personal-group discrimination discrepancy was exhibited in our sample (Fig. 1); women acknowledged with more frequency items representing group racism than items representing personal racism. Two thirds (67%) of the women stated they had experienced both types of group racism: vicarious and collective, whereas only 34% acknowledged all items representing personal racism. Less than 10% of these women reported having never experienced group racism, while 43.7% reported having never experienced personal racism. The personal-group discrimination discrepancy was also exhibited within each age group in varying degrees (Fig. 1).
Fig. 1.
Distribution of personal and group experiences of racism stratified by maternal age group in the Baltimore Preterm Birth Study, 2001–2004
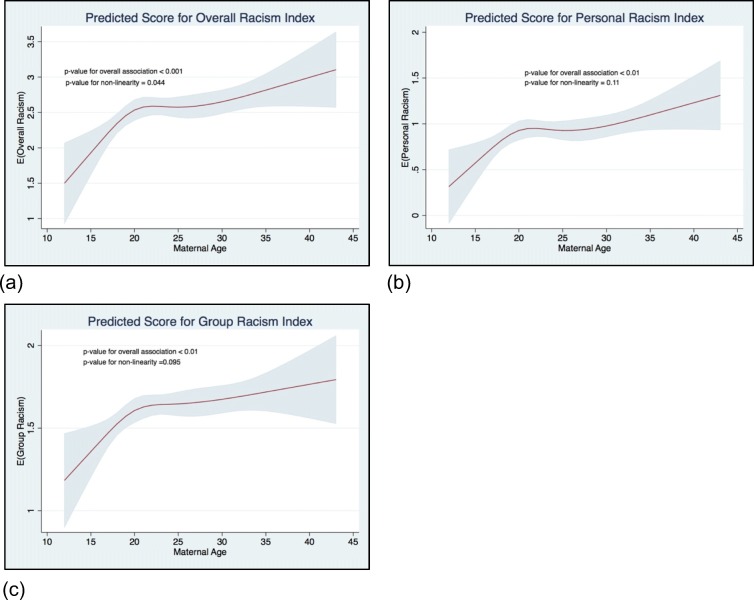
Spline regression analyses demonstrated a statistically significant (p value for overall association < 0.001) and non-linear (p value = 0.04) relationship between maternal age and overall racism. Figure 2a illustrates this non-linear relationship showing the predicted overall racism index score steeply increases until about 20 years, then plateaus until approximately 30 years of age, then continuously increases. Similar patterns were demonstrated between maternal age and the racism sub-indices (Fig. 2b, c). However, the non-linear relationship was only marginally significant for the sub-indices.
Fig. 2.
Relationship between maternal age and reports of perceived racism. a Overall racism index. b Personal racism. c Group racism. The X-axis represents the maternal age (years). The Y-axis represents the predicted score for the racism index. Red line represents the predicted score for each racism index. Gray fill represents the 95% confidence interval
Perceived Racism and SGA
The SGA prevalence in the sample was 18.6%, with younger women having the highest SGA prevalence (Table 1). Table 2 presents results from the logistic regression examining the association between perceived racism and SGA. In the full sample, unadjusted main effects models showed neither the overall racism index nor the sub-indices were significantly associated with the odds ratio of SGA. Next, we tested for effect modification by maternal age. In separate models, the overall racism-maternal age and the group racism-maternal age interaction terms were deemed statistically significant (p = 0.03 and p = 0.01, respectively). However, the personal racism-maternal age interaction term was not statistically significant (p = 0.17).
Table 2.
Personal and group racism and SGA stratified by maternal age (≤ 18, 19–24, and ≥ 25 years)
| Measure | Total sample (N = 778) | Interaction p valuea | Maternal developmental age group | ||
|---|---|---|---|---|---|
| Unadjusted | ≤ 18 yearsb (n = 167) | 19–24 yearsb (n = 354) | ≥ 25 yearsb (n = 257) | ||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Overall racism | 0.95 (0.82, 1.10) | 0.03 | 0.92 (0.66, 1.28) | 0.86 (0.69, 1.06) | 1.45 (1.02, 2.08) |
| Personal racism | 0.92 (0.74, 1.13) | 0.17 | 0.96 (0.58, 1.58) | 0.86 (0.64, 1.18) | 1.33 (0.86, 2.09) |
| Group racism | 0.97(0.73, 1.30) | 0.01 | 0.83 (0.47, 1.45) | 0.72 (0.47, 1.10) | 2.84 (1.10, 7.32) |
We further explored effect modification via stratification by developmental age groups: ≤ 18, 19–24, and ≥ 25 years. Overall racism was not associated with SGA among women aged ≤ 18 years (OR = 0.92, 95% CI 0.66–1.28) and women aged 19–24 years (OR = 0.86, 95% CI 0.69–1.06); however, among women aged ≥ 25 years, one-unit increase in the overall racism index was associated with a higher SGA odds ratio (OR = 1.45, 95% CI 0.1.02–2.08).
With the personal racism sub-index, age-stratified models did not show a significant association between personal racism and the SGA odds ratio among women aged ≤ 18 years (OR = 0.96, 95% CI 0.58–1.58) and 19–24 years (OR = 0.86, 95% CI 0.64–1.18). In women aged ≥ 25 years, again there was no association seen, but the trend was suggestive (OR = 1.33, 95% CI 0.86–2.09). For the group racism sub-index, age-stratified models showed an increase in SGA odds ratio associated with the group racism among women aged ≥ 25 (OR = 2.84, 95% CI 1.10–7.32). However, group racism was not significantly associated with SGA odds ratio in women aged ≤ 18 years (OR = 0.83, 95% CI 0.48–1.45) or in women aged 19–24 years old (OR = 0.72, 95% CI 0.47–1.10).
Discussion
Few investigators have examined the importance of personal versus group exposure to racism or racial discrimination in relation to health outcomes, much less with regard to birth outcomes. We examined the personal-group discrimination discrepancy in a cohort of urban low-income AA women. We found that AA women were less likely to acknowledge that racism affects them through direct personal experiences than to acknowledge that racism affects the lives of other AAs, family, and friends. We also showed, in varying degrees, that this pattern of differential reporting is present across major developmental stages that intersect with women’s childbearing period. The personal-group discrepancy found in our study may be the result of people’s ability to perceive racism occurring on multiple levels and in multiple contexts with equal ability [22]. Researchers have also suggested this discrepancy may reflect maladaptive strategies that individuals use to minimize the distress of acknowledging and coping with discrimination [22, 34, 35].
As noted in the “Introduction” section, age may influence the experience and/or reporting of racism for self or vicariously. However, few studies about racism, much less studies about racism and health, have reported on the distribution of racism by age. In all of our analyses, we found a lower endorsement of racism scale items in both the personal and group domain for the younger mothers in our cohort. Late adolescence through emerging adulthood are periods of rapid developmental change [53]. These developmental shifts impact individuals’ perception of racism and parenting attitudes and behaviors [61]—two salient factors in the context of Black Motherhood. When our data were stratified (i.e., informed by a developmental life course perspective), findings demonstrated that maternal developmental stage (≤ 18 years, adolescence; 19–24 years, emerging adulthood; ≥ 25 years, adulthood) served as a moderator for perceived racism and racial life experiences [22, 51]. Moreover, the significant interaction between group racism and SGA, when stratified by developmental stage of the mother, may demonstrate the impact that an increased awareness of race may have on birth outcomes. This confirms prior evidence for emerging adults as a distinct developmental group in maternal and child health research [61].
For some of the comparisons, the proportion of women not reporting racism in the younger age groups is substantial. This could suggest that fewer reports of racism or racial discrimination may be more normative for younger women. This would be consistent with the effect modification we report by maternal age for the apparently protective effect of racism on fetal growth. Alternatively, differences in reports of racism and subsequent effect modification by maternal age could be due to generational changes in the sociopolitical climate of the USA [62]. Comparison of our findings with other published studies on racism and birth outcomes is somewhat difficult. First, we appear to have the only such study that recruited women with maternal ages spanning across adolescence, emerging adulthood, and adulthood (Maryland law considers minors emancipated if pregnant). Second, even among adult cohorts, the published studies on racism and birth outcomes have not reported on whether maternal age moderated the impact of racism on the risk of adverse outcomes.
More broadly, our results suggest that context is important when considering the impact of psychosocial exposures. Maternal age appears to be an important contextual factor. Community and time may be other factors; however, our study could not explore these factors. As noted above, very few studies have been published on racism and birth outcomes. Among the pregnancy cohorts reporting on racism, the women have been recruited from the Baltimore, MD [29, 41]; Chicago, IL [63, 64]; and Central NC [65, 66]. The studies of racism in which women retrospectively reported their birth outcomes include a wider range of communities—the Black Women’s Health Study (a national sample) and the CARDIA study (Birmingham, AL; Chicago, IL; Oakland, CA; Minneapolis, MN). Future studies might more explicitly examine how differences or changes in community and sociopolitical context over time relate to the impact of racism.
Limitations
As with every study, ours has some limitations which should be considered. As have most birth outcome studies, we used BW-standardized growth curves to assess fetal growth; these curves can be biased at the lower end of the distribution [67]. The use of SGA as an indicator of poor fetal growth implies that every infant in the tail of end of the BW-for-gestational age distribution experienced impaired fetal growth, yet some infants may be just constitutionally small [51]. Our hybrid prospective/retrospective design could be perceived as a limitation. However, recruitment of women prenatally and postnatally may increase the generalizability of our study findings to urban low-income AA women since we were able to include women with late, interrupted, or sporadic PNC. Indeed, prospective pregnancy cohorts often report lower PTB or lower BW rates than those reported for the general population [68, 69].
In relation to our racism measures, the difference in reports of personal and group experiences of racism may be confounded by the difference in phrasing of items. For example, personal items ask women about the amount of racism, but group items ask women to report on an effect of racism. Furthermore, the sub-index of group racism is limited, as Cronbach’s α was somewhat low; this may be related to the fact that each item represented a different type of potential group-level racism-related stress. Future research should focus on increasing the reliability of this measure by incorporating additional questions representative of vicarious and collective racism.
Conclusions
Rates of reported racism among women in the Baltimore PTB Study were higher for group than for personal experiences of racism overall and by maternal developmental age group. In our sample of low-income urban AA women, racism, whether personal or group, had a consistently adverse impact, increasing the SGA risk among the women aged ≥ 25 years though not among emerging adults or adolescents. Future studies should examine maternal age as a contextual factor in the study of racism and consider the role of domain-specific race-related stress [70] in SGA and other perinatal health outcomes. Similarly, contributing factors to racial awareness such as racial identity [71], racial socialization [72, 73], and race-based traumatic stress [74, 75] should be assessed to identify stronger pathways for public health interventions.
Abbreviations
- AA
African American
- BW
Birth weight
- CI
Confidence interval
- FRS
Family Resource Scale
- GA
Gestational age
- OR
Odds ratio
- PNC
Prenatal care
- PTB
Preterm birth
- SD
Standard deviation
- SGA
Small-for-gestational age
Funding Information
This research was supported by NIH grant R01 HD038098 to Dr. Misra. The NIH took no role in any part of the study, including the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. Support was also provided by the Drexel University to Dr. Slaughter-Acey.
Contributor Information
Jaime C. Slaughter-Acey, Phone: 504-231-5215, Email: jcs396@drexel.edu, Email: jslaughts@gmail.com
Lloyd M. Talley, Email: ltalley@gse.upenn.edu
Howard C. Stevenson, Email: howards@gse.upenn.edu
Dawn P. Misra, Email: dmisra@med.wayne.edu
References
- 1.Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: final data for 2014. Natl Vital Stat Rep. 2016;65(4):1–122. [PubMed] [Google Scholar]
- 2.Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep. 2017;66(1):1. [PubMed] [Google Scholar]
- 3.Mathews T, MacDorman MF. Infant mortality statistics from the 2010 period linked birth/infant death data set. Natl Vital Stat Rep. 2013;62(8):1–26. [PubMed] [Google Scholar]
- 4.Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: final data for 2013. Natl Vital Stat Rep. 2016; 64(2):1–19. [PubMed]
- 5.Hamilton BE, Martin JA, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2014. Natl Vital Stat Rep. 2015;64(12):1–64. [PubMed] [Google Scholar]
- 6.Mathews T, MacDorman MF, Thoma ME. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl Vital Stat Rep. 2015;64(9):1–28. [PubMed] [Google Scholar]
- 7.Catov JM, Lee M, Roberts JM, Xu J, Simhan HN. Race disparities and decreasing birth weight: are all babies getting smaller? Am J Epidemiol. 2016;183(1):15–23. doi: 10.1093/aje/kwv194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bediako SM, Griffith DM. Eliminating racial/ethnic health disparities: reconsidering comparative approaches. J Racial Ethn Health Disparities. 2012;2(1):5. [Google Scholar]
- 9.Kramer MS, Ananth CV, Platt RW, Joseph K. US Black vs White disparities in foetal growth: physiological or pathological? Int J Epidemiol. 2006;35(5):1187–1195. doi: 10.1093/ije/dyl125. [DOI] [PubMed] [Google Scholar]
- 10.Hilmert CJ, Dominguez TP, Schetter CD, Srinivas SK, Glynn LM, Hobel CJ, Sandman CA. Lifetime racism and blood pressure changes during pregnancy: implications for fetal growth. Health Psychol. 2014;33(1):43–51. doi: 10.1037/a0031160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elo IT, Culhane JF, Kohler IV, O’Campo P, Burke JG, Messer LC, Kaufman JS, Laraia BA, Eyster J, Holzman C. Neighbourhood deprivation and small-for-gestational-age term births in the United States. Paediatr Perinat Epidemiol. 2009;23(1):87–96. doi: 10.1111/j.1365-3016.2008.00991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Love C, David RJ, Rankin KM, Collins JW. Exploring weathering: effects of lifelong economic environment and maternal age on low birth weight, small for gestational age, and preterm birth in African-American and white women. Am J Epidemiol. 2010;172(2):127–134. doi: 10.1093/aje/kwq109. [DOI] [PubMed] [Google Scholar]
- 13.Grobman WA, Parker CB, Willinger M, Wing DA, Silver RM, Wapner RJ, Simhan HN, Parry S, Mercer BM, Haas DM, Peaceman AM, Hunter S, Wadhwa P, Elovitz MA, Foroud T, Saade G, Reddy UM, Eunice Kennedy Shriver National Institute of Child Health and Human Development Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b) Network* Racial disparities in adverse pregnancy outcomes and psychosocial stress. Obstet Gynecol. 2018;131(2):328–335. doi: 10.1097/AOG.0000000000002441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gennaro S. Overview of current state of research on pregnancy outcomes in minority populations. Am J Obstet Gynecol. 2005;192(5 Suppl):S3–S10. doi: 10.1016/j.ajog.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 15.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willis E, McManus P, Magallanes N, Johnson S, Majnik A. Conquering racial disparities in perinatal outcomes. Clin Perinatol. 2014;41(4):847–875. doi: 10.1016/j.clp.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 18.Misra DP, Guyer B, Allston A. Integrated perinatal health framework. A multiple determinants model with a life span approach. Am J Prev Med. 2003;25(1):65–75. doi: 10.1016/s0749-3797(03)00090-4. [DOI] [PubMed] [Google Scholar]
- 19.Smedley A, Smedley BD. Race as biology is fiction, racism as a social problem is real: anthropological and historical perspectives on the social construction of race. Am Psychol. 2005;60(1):16–26. doi: 10.1037/0003-066X.60.1.16. [DOI] [PubMed] [Google Scholar]
- 20.Gee GC, Walsemann KM, Brondolo E. A life course perspective on how racism may be related to health inequities. Am J Public Health. 2012;102(5):967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones CP. Invited commentary: “race,” racism, and the practice of epidemiology. Am J Epidemiol. 2001;154(4):299–304. doi: 10.1093/aje/154.4.299. [DOI] [PubMed] [Google Scholar]
- 22.Harrell SP. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthop. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- 23.Omi M, Winant H. Racial formation in the United States. New York, NY: Routledge; 2014.
- 24.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511. doi: 10.1371/journal.pone.0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giurgescu C, McFarlin BL, Lomax J, Craddock C, Albrecht A. Racial discrimination and the black-white gap in adverse birth outcomes: a review. J Midwifery Womens Health. 2011;56(4):362–370. doi: 10.1111/j.1542-2011.2011.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Acevedo-Garcia D, Rosenfeld LE, Hardy E, McArdle N, Osypuk TL. Future directions in research on institutional and interpersonal discrimination and children’s health. Am J Public Health. 2013;103(10):1754–1763. doi: 10.2105/AJPH.2012.300986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 29.Slaughter-Acey JC, Caldwell CH, Misra DP. The influence of personal and group racism on entry into prenatal care among African American women. Womens Health Issues. 2013;23(6):e381–e387. doi: 10.1016/j.whi.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Slaughter-Acey JC, Sealy-Jefferson S, Helmkamp L, Caldwell CH, Osypuk TL, Platt RW, Straughen JK, Dailey-Okezie RK, Abeysekara P, Misra DP. Racism in the form of micro aggressions and the risk of preterm birth among black women. Ann Epidemiol. 2016;26(1):7–13. doi: 10.1016/j.annepidem.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alhusen JL, Bower KM, Epstein E, Sharps P. Racial discrimination and adverse birth outcomes: an integrative review. J Midwifery Womens Health. 2016;61(6):707–720. doi: 10.1111/jmwh.12490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med. 2013;95:115–127. doi: 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 33.Hagiwara N, Alderson CJ, Mezuk B. Differential effects of personal-level vs group-level racial discrimination on health among Black Americans. Ethn Dis. 2016;26(3):453–460. doi: 10.18865/ed.26.3.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruggiero KM. The personal/group discrimination discrepancy. J Soc Issues. 1999;55(3):519–536. [Google Scholar]
- 35.Taylor DM, Wright SC, Moghaddam FM, Lalonde RN. The personal/group discrimination discrepancy perceiving my group, but not myself, to be a target for discrimination. Personal Soc Psychol Bull. 1990;16(2):254–262. [Google Scholar]
- 36.Crosby F. The denial of personal discrimination. Am Behav Sci. 1984;27(3):371–386. [Google Scholar]
- 37.Dominguez TP, Dunkel-Schetter C, Glynn LM, Hobel C, Sandman CA. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychol. 2008;27(2):194–203. doi: 10.1037/0278-6133.27.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethn Health. 2014;19(5):479–499. doi: 10.1080/13557858.2013.846300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Giurgescu C, Zenk SN, Dancy BL, Park CG, Dieber W, Block R. Relationships among neighborhood environment, racial discrimination, psychological distress, and preterm birth in African American women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E51–E61. doi: 10.1111/j.1552-6909.2012.01409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rankin KM, David RJ, Collins JW., Jr African American women’s exposure to interpersonal racial discrimination in public settings and preterm birth: the effect of coping behaviors. Ethn Dis. 2011;21(3):370–376. [PubMed] [Google Scholar]
- 41.Misra D, Strobino D, Trabert B. Effects of social and psychosocial factors on risk of preterm birth in black women. Paediatr Perinat Epidemiol. 2010;24(6):546–554. doi: 10.1111/j.1365-3016.2010.01148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosenthal L, Earnshaw VA, Lewis TT, Reid AE, Lewis JB, Stasko EC, Tobin JN, Ickovics JR. Changes in experiences with discrimination across pregnancy and postpartum: age differences and consequences for mental health. Am J Public Health. 2015;105(4):686–693. doi: 10.2105/AJPH.2014.301906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Earnshaw VA, Rosenthal L, Lewis JB, Stasko EC, Tobin JN, Lewis TT, Reid AE, Ickovics JR. Maternal experiences with everyday discrimination and infant birth weight: a test of mediators and moderators among young, urban women of color. Ann Behav Med. 2013;45(1):13–23. doi: 10.1007/s12160-012-9404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 45.Misra DP. Racial disparities in perinatal health: a multiple determinants perinatal framework with a lifespan approach. Harvard Health Policy Rev. 2006;7(1):72–90. [Google Scholar]
- 46.Davis RE, Couper MP, Janz NK, Caldwell CH, Resnicow K. Interviewer effects in public health surveys. Health Educ Res. 2010;25(1):14–26. doi: 10.1093/her/cyp046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu YC, Blair EM. Predicted birthweight for singletons and twins. Twin Res. 2002;5(6):529–537. doi: 10.1375/136905202762341991. [DOI] [PubMed] [Google Scholar]
- 48.Misra DP, Slaughter-Acey JC, Giurgescu C, Sealy-Jefferson S, Nowak A. Why do black women experience higher rates of preterm birth? Curr Epidemiol Rep. 2017;4(2):83–97. [Google Scholar]
- 49.Caughy MOB, O’Campo PJ, Muntaner C. Experiences of racism among African American parents and the mental health of their preschool-aged children. Am J Public Health. 2004;94(12):2118–2124. doi: 10.2105/ajph.94.12.2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Voskamp BJ, Kazemier BM, Schuit E, Mol BWJ, Buimer M, Pajkrt E, Ganzevoort W. Birth weight ratio as an alternative to birth weight percentile to express infant weight in research and clinical practice: a nationwide cohort study. Obstet Gynecol Int. 2014;2014:1–9. doi: 10.1155/2014/749476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Talge NM, Mudd LM, Sikorskii A, Basso O. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics. 2014;133(5):844–853. doi: 10.1542/peds.2013-3285. [DOI] [PubMed] [Google Scholar]
- 52.Arnett JJ. Conceptions of the transition to adulthood: perspectives from adolescence through midlife. J Adult Dev. 2001;8(2):133–143. [Google Scholar]
- 53.Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 54.Dunst CJ, Leet HE. Measuring the adequacy of resources in households with young children. Child Care Health Dev. 2006;13(2):111–125. doi: 10.1111/j.1365-2214.1987.tb00528.x. [DOI] [PubMed] [Google Scholar]
- 55.Misra DP, O’Campo P, Strobino D. Testing a sociomedical model for preterm delivery. Paediatr Perinat Epidemiol. 2001;15(2):110–122. doi: 10.1046/j.1365-3016.2001.00333.x. [DOI] [PubMed] [Google Scholar]
- 56.Allison PD. Missing data. Thousand Oaks, CA: Sage Publications, Inc; 2001. [Google Scholar]
- 57.Stone CJ, Koo C-Y. Additive splines in statistics. Proc Stat Comp Sect Am Statist Assoc. 1985;27:45–48. [Google Scholar]
- 58.Harrell F. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. New York, NY: Springer; 2015. [Google Scholar]
- 59.Buis ML. POSTRCSPLINE: Stata module containing post-estimation commands for models using a restricted cubic spline. https://EconPapers.repec.org/RePEc:boc:bocode:s456928; https://econpapers.repec.org/software/bocbocode/S456928.htm. Accessed April 10, 2017.
- 60.Harrell F. SAS macros for assisting with survival and risk analysis, and some SAS procedures useful for multivariable modeling. January 31, 2003. Available at: http://biostat.mc.vanderbilt.edu/wiki/Main/SasMacros. Accessed May 20, 2012, 2014.
- 61.Lewin A, Mitchell SJ, Ronzio CR. Developmental differences in parenting behavior: comparing adolescent, emerging adult, and adult mothers. Merrill-Palmer Q. 2013;59(1):23–49. [Google Scholar]
- 62.Beckfield J, Krieger N. Epi + demos + cracy: linking political systems and priorities to the magnitude of health inequities—evidence, gaps, and a research agenda. Epidemiol Rev. 2009;31:152–177. doi: 10.1093/epirev/mxp002. [DOI] [PubMed] [Google Scholar]
- 63.Collins JW, Jr, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94(12):2132–2138. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Collins JW, Jr, David RJ, Symons R, Handler A, Wall SN, Dwyer L. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology. 2000;11(3):337–339. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 65.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157(1):14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 66.Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotto I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and White women in Central North Carolina. Am J Public Health. 2004;94(8):1358–1365. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hutcheon JA, Platt RW. The missing data problem in birth weight percentiles and thresholds for “small-for-gestational-age”. Am J Epidemiol. 2008;167(7):786–792. doi: 10.1093/aje/kwm327. [DOI] [PubMed] [Google Scholar]
- 68.Kramer MS. Socioeconomic disparities in preterm birth. Paediatr Perinat Epidemiol. 2015;29(3):169–171. doi: 10.1111/ppe.12186. [DOI] [PubMed] [Google Scholar]
- 69.Osypuk TL, Slaughter-Acey JC, Kehm RD, Misra DP. Life-course social mobility and reduced risk of adverse birth outcomes. Am J Prev Med. 2016;51(6):975–982. doi: 10.1016/j.amepre.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carter RT. Racism and psychological and emotional injury: recognizing and assessing race-based traumatic stress. Couns Psychol. 2007;35(1):13–105. [Google Scholar]
- 71.Sellers RM, Smith MA, Shelton JN, Rowley SA, Chavous TM. Multidimensional model of racial identity: a reconceptualization of African American racial identity. Personal Soc Psychol Rev. 1998;2(1):18–39. doi: 10.1207/s15327957pspr0201_2. [DOI] [PubMed] [Google Scholar]
- 72.Bentley-Edwards KL, Stevenson HC. The multidimensionality of racial/ethnic socialization: scale construction for the Cultural and Racial Experiences of Socialization (CARES) J Child Fam Stud. 2015;25(1):96–108. [Google Scholar]
- 73.Hughes D, Rodriguez J, Smith EP, Johnson DJ, Stevenson HC, Spicer P. Parents’ ethnic-racial socialization practices: a review of research and directions for future study. Dev Psychol. 2006;42(5):747–770. doi: 10.1037/0012-1649.42.5.747. [DOI] [PubMed] [Google Scholar]
- 74.Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Carter RT, Forsyth JM, Mazzula SL, Williams B. Racial discrimination and race-based traumatic stress: an exploratory investigation. Handbook of Racial-Cultural Psychology and Counseling. 2005;2:447–476. [Google Scholar]