Abstract
Introduction
The prevalence of obesity continues to rise in parallel with demand for total hip arthroplasty (THA). This study aims to report obesity trends in primary THA and its effects on procedure outcomes in the United States, stratifying based on Body Mass Index (BMI).
Methods
Primary THA procedures were identified in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database (2008–2016). Patient demographic (including BMI), primary outcomes (death; serious morbidity), and secondary outcome variables were analyzed. Using BMI comparison groups (Obese: BMI > 30 [O]; Morbidly Obese: BMI > 40 [MO]) for case populations, univariate, propensity score-matched, and multivariate logistic regression analyses were performed.
Results
The prevalence of obesity increased among primary THA (2008: 546/1200 [45.5%], 2016: 16,078/34,137 [47.1%]) cases. Data on 135,013 primary THA cases were analyzed. Propensity score-matched analyses demonstrated that both serious morbidity (O: OR = 0.73, p < 0.001; MO: OR = 0.84, p = 0.001) and frequency of discharges home (O: OR = 0.90, p < 0.001; MO: OR = 0.71, p < 0.001) were significantly reduced. Instead, long operative times (O: OR = 1.30, p < 0.001; MO: OR = 1.53, p < 0.001), readmission (O: OR = 1.27, p < 0.001; MO: OR = 1.49, p < 0.001), and reoperation (O: OR = 1.44, p < 0.001, MO: OR = 1.96, p < 0.001) were all significantly increased in both obese and morbidly obese cases. Death (OR = 0.29; p = 0.016) was decreased in the MO cohort, while length of stay (OR = 1.19, p = 0.004) was increased in the MO cohort.
Conclusion
Both obese and morbidly obese primary THA patient populations were associated with variably increased complication risks; morbidly obese patients had higher complication rates relative to obese patients. Orthopaedic surgeons should continue to consider obesity as a risk factor for THA complications. However, given similar functional outcomes and satisfaction levels as non-obese patients, denying patients THA surgery based on BMI alone may merit reconsideration.
Keywords: Obesity, Total hip arthroplasty, NSQIP, Complications, Outcomes, Propensity score-matching
1. Introduction
In recent decades, obesity has been identified as an epidemic in the United States; over one-third of the current adult population is obese, and its prevalence continues to rise.1,2 Moreover, obesity is associated with various orthopaedic health risks, such as osteoarthritis, resulting in debilitating joint pain and hindered mobility. Osteoarthritis of the hip is a significant factor contributing to the risk of requiring total hip arthroplasty (THA); the rise in demand for THA parallels the national obesity trend.1,3,4
Prior studies have identified obesity as a risk factor for complications following THA procedures, including infection, instability and subsequent revision surgery.5,6 In morbidly obese patients, the risk for complications includes acute kidney injury, cardiac arrest, venous thromboembolism, and reintubation.7 Nonetheless, obese patients self-report similar improvement and satisfaction levels as non-obese patients when surveyed.8,9 Therefore, utilization of THA for the treatment of obese patients will unlikely decrease, making it paramount to understand changes in the prevalence of obesity at a national level, allowing physicians to best serve a growing population of patients seeking THA.
Prior investigations regarding the prevalence of obesity among THA patients at the national level are sparse, and have even been recently disputed. For example, Odum et al.10 determined the THA population obesity prevalence to be just 11–20% between 2002 and 2009 using the National Inpatient Sample database. Overall, this result was unconvincing because it fell far below the national overall population prevalence of obesity: nearly 40%.2 Furthermore, prior institutional studies yielding values over 50%.11, 12, 13 George et al.14 utilized complex statistical methods and generalized relative risks to estimate the national prevalence of obesity in THA cases, but faced scrutiny since relative risks likely changed over time and differed amongst patient populations, making the findings inaccurate. The ideal method for evaluating the prevalence of obesity among patients undergoing THA is through the use of a database that is able to provide patient-level data on body mass index (BMI).15
In this study, we investigated the changing prevalence of obesity among THA patients in the United States from 2008 to 2016 using a national database with patient-level BMI data. The demographic characteristics and health statuses of patients were subsequently analyzed for their effect on procedural outcomes. We hypothesized that the prevalence of obesity among THA patients has been rising in parallel with that of the overall United States population trend, and that complication rates would be increased in both obese and morbidly obese patients as compared to non-obese patients.
2. Methods
The American College of Surgeons National Surgical Quality Improvement (ACS-NSQIP) database was used to evaluate the change in BMI among patients who underwent primary THA (135,013 cases) between 2008 and 2016. Patients were identified by Current Procedural Terminology (CPT) code for primary THA, 27,130. Patients were excluded if the admission International Classification of Disease diagnosis code indicated proximal femoral or pelvic fracture.
Obese patients were analyzed in two groups: first, outcomes were assessed by comparing obese (BMI > 30) patients to non-obese patients; a subsequent analysis was performed comparing morbidly obese (BMI > 40) patients to non-morbidly obese patients. Covariates are depicted in Table A.1; the primary and secondary outcomes for each of these patient cohorts are represented in Table B.2.
2.1. Statistical methods
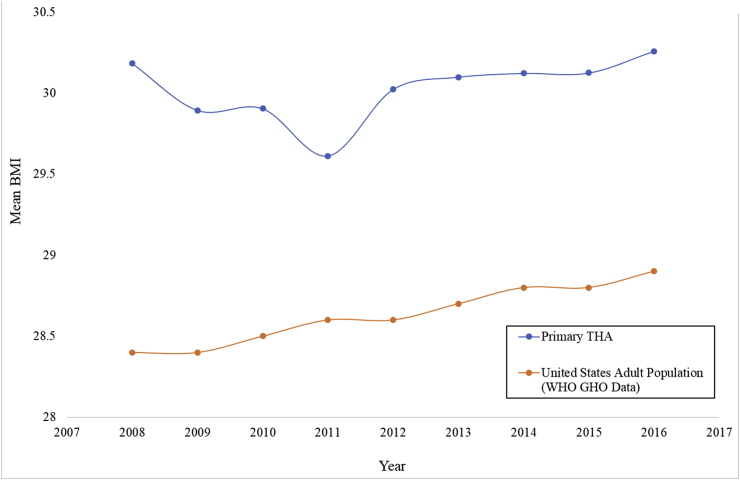
The prevalence of obesity was evaluated in the overall NSQIP population using two-sample t-tests between 2008 and 2016. Trends in BMI were evaluated using linear regression from 2008 to 2016, while changes in obesity group proportions were evaluated by Chi Square test. For reference, this was compared to the mean BMI of the adult population in the United States using estimates from the World Health Organization: in 2008, the mean adult BMI was 28.4, which increased to 28.9 by 2016.16
Successful propensity score-matching yielding no significant differences between both obese and morbidly obese comparison groups was demonstrated in Table C.3, resulting in cohorts of equal case numbers (39,293 matched pairs of obese and non-obese patients; 8492 matched pairs of morbidly obese and non-morbidly obese patients). Bonferroni correction was used to account for testing seven outcomes; thus, associations were considered significant for p-values ≤ 0.007 (0.05/7).
Propensity score-matched logistic regression modeling was performed using the same covariates from Table A.1, Table B.2 to control for confounding effects. Nearest neighbor 1:1 matching was used, with the caliper set to 1 × 10−7. A new set of matched obese and non-obese pairs was generated, from which covariates were assessed using Pearson chi-squared or Fischer's exact test to assess success of the matching algorithm. Primary and secondary outcomes were then assessed using logistic regression on this propensity-matched cohort. All statistics were performed using Stata IC 14.2 (StataCorp LLC, College Station, TX).17
2.2. Source of funding
No outside funding was utilized to support this research project.
3. Results
3.1. Trends in the prevalence of obesity
Data on 135,013 primary THA cases performed between 2008 and 2016 was available for analysis through the NSQIP database, and is detailed in Table 1. In 2008, primary THA patients had a mean BMI of 30.18 (n = 1,200, Standard Deviation [SD] = 6.84, 45.5% obese), which did not differ significantly from that of the overall NSQIP patient population (p = 0.396). By 2016, the mean BMI of primary THA patients had risen to 30.26 (n = 34,137, [SD] = 6.30, 47.1% obese), which was significantly higher than the mean BMI of 30.32 for the overall NSQIP population (n = 980,441, p = 0.004, 43.9% obese).
Table 1.
Trends in mean BMI and proportion of obese patients undergoing total hip arthroplasty, 2008–2016.
| Year | Number of Patients | Mean BMI | Standard Deviation | Proportion Obese |
|---|---|---|---|---|
| 2008 | 1200 | 30.18 | 6.84 | 45.47% |
| 2009 | 2487 | 29.89 | 6.43 | 43.79% |
| 2010 | 3822 | 29.90 | 6.76 | 43.55% |
| 2011 | 9158 | 29.61 | 6.48 | 41.65% |
| 2012 | 14,188 | 30.02 | 6.56 | 44.17% |
| 2013 | 19,111 | 30.10 | 6.59 | 44.91% |
| 2014 | 22,361 | 30.12 | 6.43 | 45.70% |
| 2015 | 28,549 | 30.13 | 6.28 | 46.30% |
| 2016 | 34,137 | 30.26 | 6.30 | 47.11% |
Among primary THA patients, mean BMI increased by 0.032 points per year from 2008 to 2016 (p = 0.228, adjusted R-square 0.08) (Fig. 1). The proportion of obese primary THA patients increased at 0.36% per year during this time (p = 0.088, adjusted R-square 0.26). In contrast, the mean adult BMI in the overall United States population was 28.4 in 2008, which increased to 28.9 by 2016.16
Fig. 1.
Trends in the mean Body Mass Index (BMI) values for primary THA patients in the overall NSQIP population between 2008 and 2016, compared to that of the U.S. adult population (based on data from the World Health Organization).
3.2. Propensity score-matched analyses
Univariate analyses using propensity-matched cohorts (Table 2) generally agreed with the results from the multivariate regression (Table 3). Specifically, multivariate analysis showed that that serious morbidity (Obese: OR = 0.73, p < 0.001; Morbidly Obese: OR = 0.84, p = 0.001) and frequency of discharges home (Obese: OR = 0.90, p < 0.001; Morbidly Obese: OR = 0.71, p < 0.001) were significantly reduced, while long operative times (Obese: OR = 1.30, p < 0.001; Morbidly Obese: OR = 1.53, p < 0.001), readmission (Obese: OR = 1.27, p < 0.001; Morbidly Obese: OR = 1.49, p < 0.001), and reoperation (Obese: OR = 1.44, p < 0.001, Morbidly Obese: OR = 1.96, p < 0.001) were all significantly increased in both obese and morbidly obese cases. The morbidly obese cohort demonstrated association with decreased risk of death (OR = 0.29; p = 0.016) and increased length of stay (OR = 1.19, p = 0.004) compared with the non-obese matched group.
Table 2.
Univariate analysis for primary total hip arthroplasty procedures grouped by BMI after propensity score-matching.
| Characteristic | Obese (BMI > 30) |
Morbidly Obese (BMI > 40) |
||||||
|---|---|---|---|---|---|---|---|---|
| Overall (no. [%]) | Obese, BMI > 30 (no. [%]) | Normal Weight, BMI < 30 (no. [%]) | P Value | Overall (no. [%]) | Morbidly Obese, BMI > 40 (no. [%]) | Non-Morbidly Obese, BMI < 40 (no. [%]) | P Value | |
| Death or serious morbidity | 8274 (10.5) | 3566 (9.1) | 4708 (12.0) | <0.001 | 1849 (10.9) | 853 (10.0) | 996 (11.7) | <0.001 |
| Death | 90 (0.1) | 43 (0.1) | 47 (0.1) | 0.673 | 22 (0.1) | 5 (0.1) | 17 (0.2) | 0.010 |
| Serious morbidity | 8253 (10.5) | 3558 (9.1) | 4695 (12.0) | <0.001 | 1839 (10.8) | 850 (10.0) | 989 (11.7) | 0.001 |
| Surgical Site Infection | 4 (0.0) | 4 (0.0) | 0 (0.0) | 0.046 | 2 (0.0) | 2 (0.0) | 0 (0.0) | 0.158 |
| Respiratory | 134 (0.2) | 82 (0.2) | 52 (0.1) | 0.009 | 31 (0.2) | 16 (0.2) | 15 (0.2) | 0.857 |
| Cardiac | 732 (0.9) | 394 (1.0) | 338 (0.9) | 0.038 | 147 (0.9) | 75 (0.9) | 72 (0.9) | 0.804 |
| Bleeding (bleeding transfusion intraop/postop) | 7460 (9.5) | 3083 (7.9) | 4377 (11.1) | <0.001 | 1645 (9.7) | 736 (8.7) | 909 (10.7) | <0.001 |
| Sepsis | 193 (0.3) | 127 (0.3) | 66 (0.2) | <0.001 | 67 (0.4) | 45 (0.5) | 22 (0.3) | 0.005 |
| Time variables | ||||||||
| Operative Time | <0.001 | <0.001 | ||||||
| Expected Operative Time | 67,043 (85.3) | 32,874 (83.7) | 34,169 (87.0) | 13,794 (81.2) | 6622 (78.0) | 7172 (84.5) | ||
| Long Operative Time (1 SD > Mean) | 11,543 (14.7) | 6419 (16.3) | 5124 (13.0) | 3190 (18.8) | 1870 (22.0) | 1320 (15.5) | ||
| Total length of stay | 0.763 | 0.004 | ||||||
| −5 days | 74,393 (94.7) | 37,187 (94.6) | 37,206 (94.7) | 15,740 (92.7) | 7821 (92.1) | 7919 (93.3) | ||
| >5 days | 4193 (5.3) | 2106 (5.4) | 2087 (5.3) | 1244 (7.3) | 671 (7.9) | 573 (6.8) | ||
| Discharge | <0.001 | <0.001 | ||||||
| Discharged to Non-Home Facility | 17,426 (22.9) | 9064 (23.8) | 8362 (22.0) | 4426 (27.0) | 2491 (30.3) | 1935 (23.7) | ||
| Discharged to Home | 58,720 (77.1) | 29,073 (76.2) | 29,647 (78.0) | 11,975 (73.0) | 5729 (69.7) | 6246 (76.4) | ||
| Readmission Within 30 Days | 2643 (3.5) | 1476 (3.9) | 1167 (3.1) | <0.001 | 763 (4.7) | 454 (5.6) | 309 (3.8) | <0.001 |
| Required Reoperation | 1480 (2.0) | 873 (2.3) | 607 (1.6) | <0.001 | 472 (2.9) | 311 (3.8) | 161 (2.0) | <0.001 |
Table 3.
Multivariate analysis on the effect of obesity and morbid obesity on total hip arthroplasty postoperative outcomes after propensity score matching.
| Outcomes | Obese (BMI > 30) |
Morbidly Obese (BMI > 40) |
||
|---|---|---|---|---|
| OR | P Value | OR | P Value | |
| Complications | ||||
| Death or serious morbidity | 0.73 | <0.001 | 0.84 | <0.001 |
| Death | 0.91 | 0.673 | 0.29 | 0.016 |
| Serious morbidity | 0.73 | <0.001 | 0.84 | 0.001 |
| Time Variables | ||||
| Long Operation Time | 1.30 | <0.001 | 1.53 | <0.001 |
| Long Length of Stay | 1.01 | 0.763 | 1.19 | 0.004 |
| Discharge Home | 0.90 | <0.001 | 0.71 | <0.001 |
| Reoperation | 1.44 | <0.001 | 1.96 | <0.001 |
| Readmission | 1.27 | <0.001 | 1.49 | <0.001 |
Post-hoc power analysis demonstrated a sample of 229,510 would be required to detect a significant difference in obesity rates with 80% power or an alpha of 0.05, if one truly existed. Additional post-hoc analysis confirmed that a sample of at least 13,268 was needed to detect a difference in the readmission rate and at least 9612 to detect a difference in the reoperation rate observed between groups in this study.
4. Discussion
This study is the first to use patient-level BMI data to show that the prevalence of obesity among primary THA patients is significantly higher than that of the general United States population, rising from 45.5% to 47.1% between 2008 and 2016 in the overall ACS-NSQIP patient population. This is in agreement with our initial hypothesis. We employ unique propensity score-matching in order to control for confounding demographic and comorbidity characteristics when comparing complication rates between groups. This statistical approach revealed variably increased complication rates for obese and morbidly obese THA patients relative to non-obese patients.
Our finding that the prevalence of obesity in primary THA patients is slightly greater than that of the overall United States population agrees with prior results from single-institution studies.11, 12, 13 These previous studies estimated the prevalence of obesity among primary THA patients to be about 50%, whereas the CDC estimates that the current prevalence of obesity in the U.S. adult population is about 36%.2,11, 12, 13 This may be explained by the fact that patients undergoing THA procedures tend to be higher in age, which is associated with reduced resting metabolic rates as well as decreased levels of physical activity contributing to increased body mass.18,19 Similarly, the prevalence of obesity has been shown to be higher among patients with hip osteoarthritis, a major risk factor for THA.20 However, we did not observe a significant increase in mean BMI among primary THA patients over the study period. This could be due to increasing pressure from arthroplasty groups and medical payors to place BMI limits on THA eligibility given the risk for increased complications.21 Thus, careful patient selection by clinicians and payor refusal may limit the extent to which the average BMI of primary THA patients will rise over time, and may even lead to a decrease in patient BMI moving forward.
This study uses an ideal method for evaluating the prevalence of obesity among patients undergoing THA by using a database that provides patient-level data on BMI. We believe that this methodology improves upon those used by the two prior studies that investigated the national prevalence of obesity among THA patients. First, Odum et al.10 determined the prevalence of obesity in the primary THA population prevalence to be uncharacteristically low, between 11% and 20% from 2002 to 2009 using the National Inpatient Sample database. This deviation from the expected prevalence is likely due to underreporting of obesity diagnoses in the NIS database. The NIS database is derived from patient discharge records, which relies on the submission of obesity and other diseases as a diagnosis code for calculation of comorbidities. Coding for obesity is not directly reimbursable resulting in a limited incentive to report the diagnosis, making the database an imperfect source for evaluating obesity prevalence among arthroplasty patients.
Secondly, George et al.14 estimated the prevalence of obesity among THA cases using complex statistical methods. As noted by Sloan and Sheth in a previous letter, complex methods for calculating obesity among populations appear to overestimate obesity prevalence and should not be considered accurate for incorporation into risk models or health policy predictions.15 Relative risk of obesity among THA patients may change over time, and the cited relative risks may not apply to different patient populations. For these reasons, we consider our use of the ACS-NSQIP database, which contains patient-level information and more accurate BMI figures, to be the main strength of this study and its ability to accurately ascertain the prevalence of obesity in the THA population.
We found that obese and morbidly obese primary THA patients are at variably increased risks for complications relative to non-obese patients, but have no significant differences with respect to mortality risk. For example, obese primary THA patients experienced a prolonged operative time, more frequent discharges to non-home facilities, and more often required readmission and reoperation; morbidly obese patients also experienced increased lengths of stay. Complication risk was higher overall for morbidly obese patients relative to obese patients in our study. This again confirms prior single-institution studies which found increased complications for obese and morbidly obese THA patients.5, 6, 7 Interestingly, we found that both obese and morbidly obese primary THA patients were at a reduced risk for serious morbidity. Breaking down this more broadly defined morbidity variable into its specific possible causes (Table 2) reveals that this finding is mainly driven by a significantly reduced risk of blood transfusion; all other causes of morbidity were expectedly higher in these patients. Considering the comparative rarity of all other types of complications in this study, the paradoxical decrease in apparent morbidity for obese and morbidly obese THA patients is suggested to instead be an artifact of selection bias resultant from clinicians choosing “the healthiest” obese patients for elective hip surgery.21 Combined with the fact that higher BMI is associated with higher starting blood volume and thus both lower rates of required blood transfusion due to reduced percentages of blood volume loss, the finding that obese and morbidly obese patients have decreased overall morbidity may not best reflect the actual risks of medical complications for these patient.22
These findings align closely with the singular prior study using the NSQIP database to investigate surgical complications of THA in obese patients. Specifically, Zusmanovich, Kester, and Schwarzkopf demonstrated increased risks for complications in obese and morbidly obese patients, though not an increased risk of mortality.23 However, our analysis benefited not only from more recent data – which contributed an additional 30,000 THA patients – but also from the use of propensity score-matching prior to multivariate logistic regression in order to control for confounding patient health and demographic factors. Relative to other statistical techniques used to minimize confounding variable bias, propensity score-matching is regarded as less biased, more robust, and more precise than regression techniques alone whenever the number of events per confounder is less than eight.24 Given that our analysis required controlling for over thirty potential confounding variables for several events that were exceedingly rare, we consider our decision to use propensity score-matching prior to multivariate regression as a substantial methodological strength assuring the validity and reliability of our results.25
This study has several limitations associated with the nature of the ACS-NSQIP database. First, given that the data does not follow patients beyond 30 days after surgery, we were unable to track outcomes for longer time periods. Second, the database does not contain institutional-level details. Therefore, models did not account for geographic variability in risk or the volume of complicated cases that a particular institution may see in a given period. Third, it is impossible to randomize patients by BMI who undergo any procedure. While we aimed to account for differences in demographic and comorbid variables using propensity score-matching, this significantly reduced the number of cases available for analysis. Despite these limitations, our use of a large national administrative database with patient-level data for this risk-adjusted analysis gives us confidence in our ability to accurately determine the prevalence of obesity in THA patient populations across time.
Obese and morbidly-obese patients face variably increased complication risks following THA procedures. However, they do not appear to be at increased risk for mortality, and both functional outcomes and satisfaction levels are often similar to those reported in non-obese patients. Therefore, patients should not necessarily be denied from THA procedures based on high BMI alone. Instead, surgeons should counsel obese and morbidly obese patients of these increased perioperative complication risk in order to enhance patient decision making. Moreover, clinicians may encourage certain patients for whom it is safe and feasible to consider diet and exercise regimens in order to reduce their BMI prior to elective surgeries. By holistically considering these factors, the rising demand for THA in an increasingly obese United States population may be more effectively met without negatively impacting procedural complication rates. Randomized prospective studies regarding the impact of preoperative weight loss in mitigating some of these observed risks are necessary.
Footnotes
Table A.1.
| Advanced Age (>70 Years) | Use of General Anesthesia for the Procedure |
|---|---|
| Sex | Chronic Obstructive Pulmonary Disease (COPD) |
| Race | Steroid Use |
| Functional Status | Renal Failure Requiring Dialysis |
| American Society of Anesthesiologists (ASA) Classification | History of Malignancy |
| Diabetes Mellitus Requiring Insulin | High Creatinine Levels (Defined as ≥2 mg/dL) |
| History of Hypertension Requiring Medication | Low Albumin Levels (Defined as < 3.5 g/dL) |
| History of Osteoarthritis or Rheumatoid Arthritis | Low Platelet Count (Defined as < 100 Billion cells/L) |
| Smoking | High Bilirubin Levels (Defined as ≥ 2 mg/dL) |
Table B.2.
| Primary Outcomes |
| Readmission within 30 Days |
| Reoperation within 30 Days |
| Secondary Outcomes |
| Death within 30 Days of Surgery |
| Serious Medical Morbidity within 30 Days of Surgery (Including: Postoperative Surgical Site Infection, Respiratory Event, Cardiac Event, Bleeding with Need for Transfusion, Sepsis) |
| Discharge to Home (Rather Than a Non-Home Facility) |
| Total Operative Time from Incision to Closure (Long Operative Time Defined as One Standard Deviation Greater than Mean) |
| Total Length of Stay (Prolonged Length of Stay Defined as >5 Days) |
| American Society of Anesthesiologists (ASA) Classification |
| Diabetes Mellitus Requiring Insulin |
| History of Hypertension Requiring Medication |
| History of Osteoarthritis or Rheumatoid Arthritis |
| Smoking |
Table C.3.
| Characteristic | Obese (BMI > 30) |
Morbidly Obese (BMI > 40) |
||||
|---|---|---|---|---|---|---|
| Obese, BMI > 30 (no. [%]) | Normal Weight, BMI < 30 (no. [%]) | P Value | Morbidly Obese, BMI > 40 (no. [%]) | Non-Morbidly Obese, BMI < 40 (no. [%]) | P Value | |
| Total | 39,293 (50.0) | 39,293 (50.0) | 8492 (50.0) | 8492 (50.0) | ||
| Sex | 1.000 | 0.988 | ||||
| Male | 18,280 (46.5) | 18,280 (46.5) | 3527 (41.5) | 3528 (41.5) | ||
| Female | 21,013 (53.5) | 21,013 (53.5) | 4965 (58.5) | 4964 (58.5) | ||
| Age | 0.994 | 0.984 | ||||
| <70 yr | 26,308 (67.0) | 26,307 (67.0) | 6953 (81.9) | 6952 (81.9) | ||
| ≥70 yr | 12,985 (33.1) | 12,986 (33.1) | 1539 (18.1) | 1540 (18.1) | ||
| Race | 1.000 | 1.000 | ||||
| White | 35,500 (90.4) | 35,500 (90.4) | 7339 (86.4) | 7336 (86.4) | ||
| Black | 3211 (8.2) | 3211 (8.2) | 1061 (12.5) | 1063 (12.5) | ||
| Hispanic | 356 (0.9) | 356 (0.9) | 33 (0.4) | 33 (0.4) | ||
| Hawaiian | 70 (0.2) | 70 (0.2) | 18 (0.2) | 19 (0.2) | ||
| American Indian | 156 (0.4) | 156 (0.4) | 41 (0.5) | 41 (0.5) | ||
| Functional status | 1.000 | 0.930 | ||||
| Independent | 38,706 (98.5) | 38,706 (98.5) | 8299 (97.7) | 8301 (97.8) | ||
| Partially Dependent | 581 (1.5) | 581 (1.5) | 189 (2.2) | 188 (2.2) | ||
| Totally Dependent | 6 (0.0) | 6 (0.0) | 4 (0.1) | 3 (0.0) | ||
| ASA class | 1.000 | 1.000 | ||||
| Low (Class < 3) | 23,193 (59.0) | 23,193 (59.0) | 2165 (25.5) | 2165 (25.5) | ||
| High (Class ≥ 3) | 16,100 (41.0) | 16,100 (41.0) | 6327 (74.5) | 6327 (74.5) | ||
| Comorbidities | ||||||
| Diabetes | 3706 (9.4) | 3706 (9.4) | 1.000 | 1990 (23.4) | 1989 (23.4) | 0.986 |
| Hypertension Medication | 23,317 (59.3) | 23,317 (59.3) | 1.000 | 6284 (74.0) | 6287 (74.0) | 0.958 |
| Smoker | 5351 (13.6) | 5351 (13.6) | 1.000 | 1006 (11.9) | 1005 (11.8) | 0.981 |
| General Anesthesia | 14,124 (61.6) | 15,100 (57.5) | <0.001 | 5382 (63.0) | 5009 (58.6) | <0.001 |
| COPD | 1477 (3.8) | 1478 (3.8) | 0.985 | 357 (4.2) | 354 (4.2) | 0.908 |
| Chronic steroid | 1215 (3.1) | 1214 (3.1) | 0.984 | 280 (3.3) | 279 (3.3) | 0.966 |
| Dialysis | 31 (0.1) | 31 (0.1) | 1.000 | 5 (0.1) | 5 (0.1) | 1.000 |
| Cancer | 62 (0.2) | 62 (0.2) | 1.000 | 9 (0.1) | 9 (0.1) | 1.000 |
| Low Hematocrit (<30) | 206 (0.5) | 205 (0.5) | 0.961 | 41 (0.5) | 43 (0.5) | 0.827 |
| High Creatinine (≥2 mg/dL) | 2488 (6.3) | 2488 (6.3) | 1.000 | 503 (5.9) | 506 (6.0) | 0.922 |
| Low Albumin (<3.5 g/dL) | 682 (1.7) | 681 (1.7) | 0.978 | 236 (2.8) | 236 (2.8) | 1.000 |
| Low Platelets (<100 billion cells/L) | 127 (0.3) | 127 (0.3) | 1.000 | 32 (0.4) | 30 (0.4) | 0.799 |
| High Bilirubin (≥2 mg/dL) | 19,809 (50.4) | 19,810 (50.4) | 0.994 | 4137 (48.7) | 4133 (48.7) | 0.951 |
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization (WHO . Health; 2017. Obesity and Overweight Factsheet from the WHO. [Google Scholar]
- 2.Ogden C.L., Carroll M.D., Fryar C.D., Flegal K.M. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2015. Prevalence of Obesity Among Adults and Youth: United States, 2011-2014. [Google Scholar]
- 3.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. doi: 89/4/780 [pii] [DOI] [PubMed] [Google Scholar]
- 4.Kulkarni K., Karssiens T., Kumar V., Pandit H. Obesity and osteoarthritis. Maturitas. 2016;89:22–28. doi: 10.1016/j.maturitas.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Liu W., Wahafu T., Cheng M., Cheng T., Zhang Y., Zhang X. The influence of obesity on primary total hip arthroplasty outcomes: a meta-analysis of prospective cohort studies. Orthop Traumatol: Surg Res. 2015;101(3):289–296. doi: 10.1016/j.otsr.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 6.Ward D.T., Metz L.N., Horst P.K., Kim H.T., Kuo A.C. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplast. 2015;30(9):42–46. doi: 10.1016/j.arth.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 7.Ward D.T., Metz L.N., Horst P.K., Kim H.T., Kuo A.C. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplast. 2015;30(9):42–46. doi: 10.1016/j.arth.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 8.Stickles B., Phillips L., Brox W.T., Owens B., Lanzer W.L. Defining the relationship between obesity and total joint arthroplasty. Obesity. 2001;9(3):219–223. doi: 10.1038/oby.2001.24. [DOI] [PubMed] [Google Scholar]
- 9.Lash H., Hooper G., Hooper N., Frampton C. Should a patients BMI status be used to restrict access to total hip and knee arthroplasty? functional outcomes of arthroplasty relative to BMI - single centre retrospective review. Open Orthop J. 2013;7:594–599. doi: 10.2174/1874325001307010594. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Odum S.M., Springer B.D., Dennos A.C., Fehring T.K. National obesity trends in total knee arthroplasty. J Arthroplast. 2013;28(8):148–151. doi: 10.1016/j.arth.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 11.Fehring T.K., Odum S.M., Griffin W.L., Mason J.B., McCoy T.H. The obesity epidemic: its effect on total joint arthroplasty. J Arthroplast. 2007;22(6):71–76. doi: 10.1016/j.arth.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Namba R.S., Paxton L., Fithian D.C., Stone M.L. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplast. 2005;20:46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 13.Collins J.E., Donnell-Fink L.A., Yang H.Y. Effect of obesity on pain and functional recovery following total knee arthroplasty. J Bone Joint Surg Am. 2017;99(21):1812–1818. doi: 10.2106/JBJS.17.00022. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.George J., Klika A.K., Navale S.M., Newman J.M., Barsoum W.K., Higuera C.A. Obesity epidemic: is its impact on total joint arthroplasty underestimated? an analysis of national trends. Clin Orthop Relat Res. 2017:1–9. doi: 10.1007/s11999-016-5222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sloan M., Sheth N.P. Letter to the editor: obesity epidemic is its impact on total joint arthroplasty underestimated? an analysis of national trends. Clin Orthop Relat Res. 2018;476(5):1122–1123. doi: 10.1007/s11999.0000000000000238. Accessed 7/3/2018 2:27:06 PM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO) 2017. Mean Body Mass Index Trends Among Adults, Age-Standardized (Kg/m2): Estimates by WHO Region. [Google Scholar]
- 17.StataCorp L.P. Vol. 14.2. 2015. (Stata Statistical Software). [Google Scholar]
- 18.Maradit Kremers H., Larson D.R., Crowson C.S. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386–1397. doi: 10.2106/JBJS.N.01141. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johannsen D.L., Ravussin E. Obesity in the elderly: is faulty metabolism to blame? Aging Health. 2010;6(2):159–167. doi: 10.2217/ahe.10.12. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jiang L., Rong J., Wang Y. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2011;78(2):150–155. doi: 10.1016/j.jbspin.2010.04.011. [doi] [DOI] [PubMed] [Google Scholar]
- 21.Zhang J.C., Matelski J., Gandhi R., Jackson T., Urbach D., Cram P. Can patient selection explain the obesity paradox in orthopaedic hip surgery? an analysis of the ACS-NSQIP registry. Clin Orthop Relat Res. 2018;476(5):964–973. doi: 10.1007/s11999.0000000000000218. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao G., Huang Z., Huang Q., Zhang S., Xu B., Pei F. Incidence and risk factors for blood transfusion in simultaneous bilateral total joint arthroplasty: a multicenter retrospective study. J Arthroplast. 2018;33(7):2087–2091. doi: 10.1016/j.arth.2018.02.041. doi: S0883-5403(18)30172-4 [pii] [DOI] [PubMed] [Google Scholar]
- 23.Zusmanovich M., Kester B.S., Schwarzkopf R. Postoperative complications of total joint arthroplasty in obese patients stratified by BMI. J Arthroplast. 2018;33(3):856–864. doi: 10.1016/j.arth.2017.09.067. Accessed 11/9/2018 12:03:29 AM. doi: S0883-5403(17)30878-1 [pii] [DOI] [PubMed] [Google Scholar]
- 24.Cepeda M.S., Boston R., Farrar J.T., Strom B.L. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158(3):280–287. doi: 10.1093/aje/kwg115. Accessed 11/8/2018 11:57:51 PM. [DOI] [PubMed] [Google Scholar]
- 25.Biondi-Zoccai G., Romagnoli E., Agostoni P. Are propensity scores really superior to standard multivariable analysis? Contemp Clin Trials. 2011;32(5):731–740. doi: 10.1016/j.cct.2011.05.006. Accessed 11/8/2018 11:57:51 PM. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.