Summary
Optimizing diabetes management in patients with complex type 2 diabetes (T2DM) and obesity presents challenges. This study evaluates weight and HbA1c at 12 months (primary outcomes) and blood pressure, lipids, medication and lifestyle changes (secondary outcomes) in patients referred by a diabetes specialist (DSN) to the weight management intervention (Slimming World). Patients attended up to 12 or 24 funded weekly group sessions. The DSN recorded baseline and 12‐month primary and secondary outcome data. A post‐intervention questionnaire explored the lifestyle changes made. 69 patients achieved a mean weight loss of 5.5 (5.16) %, reduction in BMI [37.7(6.11) to 35.9 (6.30) kg/m2, P < 0.001] and HbA1c levels [62.8 (12.85) to 55.0 (13.02) mmol/mol, P < 0.001] at 12 months. 81.2% reduced their HbA1c levels. Small reductions were observed in SBP, DBP and triglycerides, and six patients reduced their diabetes medications. Twenty patients completed the questionnaire: unhealthy snacking reduced (P < 0.001) and going for walks increased (P < 0.001) with fewer people avoiding moderate activity (P < 0.05). Despite being a chronic, progressive condition, referral to a community‐based programme was successful in supporting patients with established T2DM improve their diet and activity levels, lose weight and improve their glycaemic control 12 months later with a small number able to reduce their medication.
Keywords: diabesity, evaluation, glycaemic control, primary care, weight management
1. INTRODUCTION
Managing the patient with complex type 2 diabetes (T2DM) who is overweight or obese presents a number of challenges in primary care. Poor glycaemic control, the presence of co‐morbidities such as hypertension and dyslipidaemia and the associated use of polypharmacy all contribute to the difficulties in optimizing outcomes.
Whilst a HbA1c level of ≤48 mmol/mol signifies a prediabetes state, for most adults with established diabetes the HbA1c target is below 53 mmol/mol as this can reduce the risk of developing micro‐ and macrovascular complications1. Tight glycaemic control combined with lowering blood pressure can slow the progression of associated conditions.2 However, less stringent targets (≤58 mmol/mol) are considered appropriate in patients where 53 mmol/mol is difficult to attain despite intensive self‐management education, intensive clinical support and glucose‐lowering multi‐pharmacotherapy. For this group of patients, any sustained reduction in HbA1c levels will be of clinical benefit, and indeed, 53‐58 mmol/mol may be more appropriate in reducing the risk of all‐cause mortality.3
An increasing number of pharmacological agents are available to improve glycaemic control but with some concerns about both their side effects and uncertainties associated with intensive glycaemic control including an increased risk of hypoglycaemia.4 The increasing costs of some of the newer medications require practitioners to determine whether less costly options for reducing glycaemia may be more appropriate for some individual patients (NICE, 2015‐2017 update). Non‐adherence to medications may be an issue, and this risk increases with the number of medications prescribed and higher dosing frequency in the patient with complex diabetes.5
Cardiovascular disease remains the major cause of death in people with diabetes.6 Central adiposity is associated with an inferior metabolic profile.7 The foundations for managing diabetes and cardiovascular disease are diet, physical activity and weight management. A modest weight loss of 5%‐10% can contribute to improved management, and smaller degrees of weight loss may still be of benefit. Larger amounts of weight loss in the longer term will have greater metabolic impact.8 Patients who eventually lose and keep weight off may do so after many cycles of weight loss and relapse. Whilst it is challenging for the healthcare professional, they need to remain non‐judgemental, persistent in supporting lifestyle changes and be able to sign‐post patients to appropriate forms of support.
Slimming World (SW) offers weekly weight management groups in local communities where individuals needing to lose weight can either self‐refer or be referred by their local healthcare team. The weight management programme is in line with current NICE guidelines offering dietary, activity and behavioural change strategies.9, 10 People with diabetes can choose to attend a SW group, and reported data from an online survey suggest that this population can benefit both in terms of their weight loss and a reduction in HbA1c levels with a mean self‐reported change of 18 mmol/mol in HbA1c after attending a group for a number of weeks.11 However, only around 25% of the 620 participants in this online retrospective study provided self‐reported HbA1c levels.
This study evaluates the weight, BMI and HbA1c changes at 12 months (primary outcomes) and the blood pressure, lipid and medication changes (secondary outcomes) in a group of people with diabetes referred by the diabetes specialist nurse (DSN) to a SW group held within the practice building. A questionnaire was used to determine patient experiences of the intervention and to explore the lifestyle changes made as further secondary outcomes. The referred population were people with obesity/central adiposity and established diabetes who, for various reasons, were struggling to achieve optimal glycaemic control or requiring significant changes to the medications prescribed to achieve optimal glycaemic management.
2. METHODS
2.1. Patient recruitment
The DSN identified patients who were struggling to optimize glycaemic control who could benefit from weight loss rather than increasing medication.
2.2. Intervention
A new SW group was established by an experienced local SW facilitator to be held early evening, the same day of the week an evening surgery was being run by a GP with a specialist interest in diabetes. The identified patients were referred to one of five groups; one group commenced March 2015, one June 2015, one September 2015, one February 2016 and one June 2016. Referred patients were able to attend the weekly group sessions for up to 12 weeks at no cost to themselves. Once the referral programme had been completed, patients were offered a second 12‐week referral, if they had achieved a ≥ 3% weight loss, to attend a locally run SW group or able to self‐fund and attend for as long as they wished.
2.3. Data collection
The DSN electronically recorded baseline data (before intervention) for weight, height, HbA1c, systolic and diastolic blood pressure (SBP & DBP), total cholesterol (TC), LDL cholesterol (LDLc) and HDL cholesterol (HDLc) and triglycerides (TG). These measures were then repeated at 3‐6 months and 12 months post‐intervention.
Waist circumference was recorded for some but not all of the patients at baseline. Patients’ date of birth and gender were also noted.
Electronic data from SW were used to capture number of group attendances.
A questionnaire developed to be used for SW referral schemes ( https://sw.checkboxonline.com/Audley), collecting quantitative and qualitative data, was sent to patients at the end of the first 12‐week intervention period. The questionnaire determined how useful the patients found the group and their feelings having had attended, the support they received, accessibility of the group and dietary and lifestyle changes made using either a 5‐point Likert scale, one question a 1‐10 scale or yes/no responses. To report the changes in eating and physical activity habits, the five‐point Likert scale of agree very much, agree quite a lot, moderately agree, agree a little, do not agree was changed to ordinal data with agree very much =5.
2.4. Handling of missing data
For three patients, with only baseline data reported by the DSN available, last data observed carried forward were used for the analyses of the primary outcomes, with the SW weight data, electronically captured each week direct from the scales, used.
2.5. Data analysis
This service evaluation reports outcomes for all identified patients who attended at least one SW group session. BMI values at baseline and at 12 months post‐referral were calculated from weight (kg) and height (m) data (wt/ht2). Mean (SD) changes in BMI at 12 months and mean% weight loss are reported and mean changes in HbA1c, blood pressure and lipids. Paired t tests were used to compare statistical differences between the parameters at baseline and 12 months post‐referral. Regression analyses were used to determine the influence of % weight change on 12‐month HbA1c levels.
Changes in diabetes‐related medications 12 months post‐referral were reported by the DSN using the practice database.
The results section refers to statistical rather than clinically significant changes, the latter considered in the discussion.
3. RESULTS
Sixty‐nine patients were referred by the DSN and attended at least one group running at the practice between March 2015 and June 2016 resulting in group sizes between 12 and 17 people. The mean attendance was 9.0 (3.74) with 40 patients attending 10‐12 sessions. Mean age at the time of referral was 60.5 (10.05) (range 34.8 to 83.7) years with 47 females and 22 males referred. Mean BMI was 37.7 (6.11) (range 26.1 to 53.2) kg/m2, and baseline HbA1c was 62.9 (12.77) mmol/mol (range 45‐106) with 78.3% having a HbA1c > 53 mol/mol at baseline. Only 21 patients had a waist circumference reported at baseline with a mean 112 (16.67) cm: females 84‐130 cm and males (n = 8) 107‐142 cm. None of the patients had a recorded waist circumference at 12 months.
Reductions in weight and significant reductions in BMI and HbA1c levels were achieved at 12 months and across both genders. A mean weight loss of 5.7 (5.52) kg was achieved with an overall mean weight loss of 5.5 (5.16) % with female patients achieving 5.7 (5.10) % (range 18.3 to +3.7%) and the male patients 5.0 (5.38) % (range 22.6 to +1.6%). Fourteen patients achieved >10% weight reduction. In total, just three patients gained weight during the study period despite good attendances at the weekly weight management group. Two of these patients commenced on insulin during this period, and the third patient commenced the intervention on triple therapy, without metformin due to poor tolerance, and this pharmacotherapy regime did not change during the study period.
Mean BMI reduced from 37.7 (6.11) at baseline to 35.9 (6.30) kg/m2 at 12 months (P < 0.001).
81.2% of patients achieved a reduction in their HbA1c levels, with 36 (52.2%) achieving a HbA1c level <53 mmol/mol compared to 17 (24.6%) at baseline and 24 (34.8%) achieving a HbA1c level <48 mmol/mol compared to five (7.2%) at baseline. Mean reduction in HbA1c levels for the total population was 7.7 (10.84) mmol/mol.
Figure 1 illustrates the mean changes in BMI (kg/m2 ) and HbA1c (mmol/mol) at 12 months by gender and Table 1 the actual values for the primary and secondary outcomes.
Figure 1.
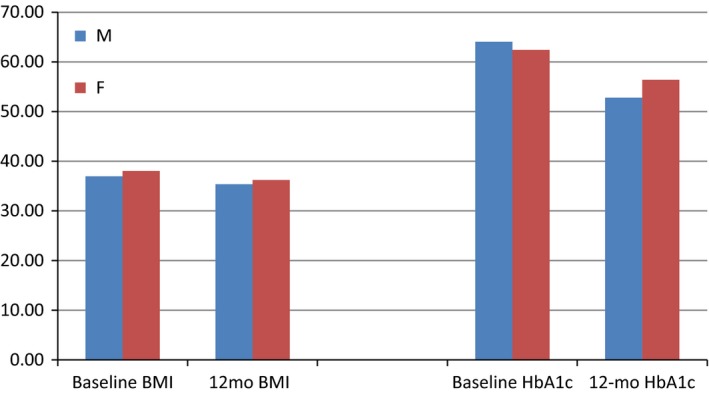
Mean changes in BMI (kg/m2 ) and HbA1c (mmol/mol) at 12 months by gender
Table 1.
Mean (SD) baseline and 12‐month post‐referral data for all parameters reported (all, n = 69; female, n = 47; and male, n = 22 unless stated)
| Baseline | 12 month post‐referral | Sig (2‐tailed) | |
|---|---|---|---|
| BMI (all) kg/m2 | 37.7 (6.11) | 35.9 (6.30) | 0.000 |
| BMI (female) | 38.1 (6.82) | 36.2 (6.89) | 0.000 |
| BMI (male) | 37.0 (4.44) | 35.4 (4.91) | 0.001 |
| HbA1c (all) mmol/mol | 62.8 (12.85) | 55.0 (13.02) | 0.000 |
| HbA1c (female) | 62.2 (11.48) | 56.1 (14.02) | 0.000 |
| HbA1c (male) | 64.1 (15.60) | 52.8 (10.54) | 0.000 |
| SBP (all) mmHg (n = 53) | 132.2 (12.65) | 130.6 (11.87) | 0.480 |
| SBP (female) (n = 36) | 133.0 (12.92) | 132.2 (11.19) | 0.755 |
| SBP (male) (n = 17) | 130.2 (12.20) | 127.1 (12.95) | 0.415 |
| DBP (all) mmHg (n = 53) | 76.1 (9.29) | 73.7 (9.38) | 0.138 |
| DBP (female) (n = 36) | 76.7 (9.91) | 73.5 (8.73) | 0.126 |
| DBP (male) (n = 17) | 75.1 (7.97) | 74.1 (10.91) | 0.730 |
| TC (all) mmol (n = 55) | 4.1 (0.82) | 4.3 (0.92) | 0.171 |
| TC (female) (n = 40) | 4.2 (0.88) | 4.5 (0.94) | 0.065 |
| TC (male) (n = 15) | 3.9 (0.65) | 3.7 (0.61) | 0.123 |
| LDLc (all) mmol (n = 48) | 1.9 (0.51) | 2.2 (0.71) | 0.006 |
| LDlc (female) (n = 33) | 2.0 (0.55) | 2.4 (0.79) | 0.011 |
| LDlc (male) (n = 15) | 1.8 (0.40) | 1.9 (0.34) | 0.256 |
| HDLc (all) mmol (n = 48) | 1.1 (0.26) | 1.2 (0.31) | 0.000 |
| HDLc (female) (n = 33) | 1.1 (0.27) | 1.3 (0.32) | 0.000 |
| HDlc (male) (n = 15) | 0.98 (0.18) | 1.0 (0.20) | 0.512 |
| TG (all) mmol (n = 48) | 2.0 (0.75) | 1.8 (0.81) | 0.052 |
| TG (female) (n = 33) | 1.8 (0.71) | 1.8 (0.88) | 0.914 |
| TG (male) (n = 15) | 2.2 (0.80) | 1.7 (0.64) | 0.004 |
DBP, diastolic blood pressure; HDLc, high‐density lipoprotein cholesterol; LDLc, low‐density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TG, triglycerides.
Regression analyses showed that 12‐mth HbA1c values were significantly (P < 0.001) affected by the level of weight loss following adjustment for baseline BMI.
Thirty‐three patients (n = 21F, 12 M; mean age 62.5 SD 9.66 years) accepted a second referral to go to a local SW group of their choice for a further 12 weeks. This group of patients achieved a mean reduction in BMI of 2.2 kg/m2 (36.2 SD 5.81 to 34.0 SD 6.22; P < 0.000) at 12 months with a mean % weight change of −6.9 (5.35) %. These patients achieved weight loss ranging from 1.0% to 22.6%. For this patient group, HbA1c levels fell from 61.3 (12.68) to 52.8 (12.31) mmol/mol (P = 0.000). For ten patients, their 12‐month HbA1c levels remained within ±5 mol/mol of their baseline level; for twelve (36%) of these patients, their 12‐month HbA1c reduced ≤48 mmol/mol and for three patients their HbA1c at 12 months fell to ≤42 mmol/mol. Five of these patients who took the opportunity to accept a second referral were able to reduce their oral medications for glycaemic control. Sixteen of these people then went on to self‐fund their weekly attendance with a mean attendance of 28 (16.67) self‐funded weeks [range 2‐52 weeks]. Of the participants who continued their weight loss journey, five people achieved their personal target weight.
3.1. Secondary outcomes for total patient group
Reductions, but not statistically significant, in both SBP and DBP for both genders were reported at 12 months. An increase, but not significant, in total cholesterol was observed in female patients and a decrease, but not significant, in males. An increase in LDL cholesterol but improvements in HDL cholesterol was observed for both females and males but only statistically significant for the females. For triglyceride levels at 12 months, there was no change for the females but significant reductions for the male patients (Table 1).
For all those participants (n = 40) where the pharmacotherapy data have been reported, 15 patients were just on metformin, 10 were on more than one oral hypoglycaemic agent, 8 were on multi‐pharmacotherapy including insulin and 3 were on insulin at baseline. Whilst six patients reduced/stopped their diabetes medication, two patients had commenced insulin by 12 months post‐referral.
3.2. Questionnaire results
Twenty (29%) patients completed the questionnaire. All found the group either very enjoyable (60%) or enjoyable (40%) with the other people in the group being either very friendly (75%) or friendly (25%), and 95% found the group facilitator very supportive with just one person indicating that the support was okay (Table 2).
Table 2.
Qualitative data from the post‐intervention questionnaire
| “My blood sugars have reduced immensely I am so happy about this! My waist line has reduced fab!!!! Want to continue with this my asthma consultant is so proud of me!!!!! After years of steroid weight.” (female, aged 50) |
| “It was an incentive to change—mildly competitive but mutually supportive” (male, aged 58) |
| “It has been a tremendous kick start to getting back on track so many thanks for the opportunity” (female, aged 67) |
| “Quick referral good, also a friendly group, with an approachable and knowledgeable consultant. Meeting room was well spaced.” (male, aged 58) |
| “Feel proud I have got there! But feel I learned more from the online site than group leader! But found attending the group helpful because of peer support!” (female, aged 50) |
| “I feel very pleased after completing my three months; I have gained a lot of useful information to help me on my weight loss journey.” (female, aged 61) “the nurse was at hand if we needed to talk, there was a lot of support, more so than any other group’'ve been” (female, aged 47) |
Sixteen people (80%) had no difficulties getting to the group. One person indicated that it was occasionally difficult to access the group because of shift work and another because of caring responsibilities.
Fourteen people (70%) found the information gained from attending the group very useful.
When asked how they felt once the 12‐week referral came to an end, no one indicated that they were glad it was over with all participants saying that they would continue going to a SW group. Sixteen (80%) expressed a sense of achievement with 65% reporting feeling healthier. For those who wished to state specific feelings following the intervention, the following feelings were expressed:
Sense of achievement
More healthy
Proud
Gained lots of useful information to start weight loss journey
Enjoyment
Grateful for the opportunity
3.2.1. Eating habits
For the questions asking about changes to eating habits, nine people (45%) indicated that they had reduced their intake of takeaways and fast food following the intervention, although eight of the eleven people who indicated that they had not made any changes did not eat a lot of these foods at baseline and on the scale used were not able to express any further reduction. These changes were reflected in a mean reduction in intake (scale data) from 2.05 (1.10) before to 1.15 (0.37) after the intervention (P = 0.003).
Whilst two people indicated that they ate more unhealthy snacks at home or work after the intervention, five people indicated no change and thirteen (65%) people indicated a reduction in unhealthy snacking habits. These changes were reflected in a mean reduction in unhealthy snacking habits from 2.55 (1.05) to 1.25 (0.64) after the intervention (P = 0.000).
Only one person suggested that they did not eat the recommended five portions of fruit and vegetables before they joined the SW group. Ten people indicating that they did not change their consumption level as a consequence of the intervention, seven people indicated an increase and three people a reduction in fruit and vegetable intake. These changes were reflected in the number of people agreeing that they met the recommendations for fruit and vegetable intake from 3.50 (1.36) before to 4.10 (1.07) after the intervention (P = 0.069).
Twelve people (60%) indicated a reduction in the number of processed foods in their diets, seven people no change and one person, with caring responsibilities, an increase in processed foods following the intervention (2.30 SD 1.17 to 1.40 SD 0.68; P = 0.003) and this was reflected in the responses to cooking meals from scratch with twelve (60%) indicating an increase, five (25%) no change and three people (15%) a reduction (mean score 3.15 SD 1.46 to 4.05 SD 1.43; P = 0.046). Participants indicated very little change in sugary drink consumption (P = 0.110).
3.2.2. Activity habits
Whilst thirteen people suggested no change in their avoidance of moderate activity, seven people did indicate that they were less likely to avoid moderate activity after the intervention with fourteen people (70%) indicating an increase in going out for walks, six people no change and one person a reduction in their walking levels. This corresponded to a reduction in sedentary behaviour with the mean score for watching a lot of TV significantly reducing from 3.15 (1.23) to 2.5 (1.10). Table 3 and Figure 2 reflect the changes in physical activity and sedentary behaviours.
Table 3.
Changes in physical activity and sedentary behaviour following the intervention
| Activity habit (n = 20) | Mean score before (SD) (5‐point Likert scale) | Mean score after (SD) (5‐point Likert scale) | P value (paired) |
|---|---|---|---|
| Played a lot of sport/used the gym | 1.4 (0.75) | 1.75 (1.07) | 0.069 |
| Watched a lot of TV | 3.15 (1.23) | 2.5 (1.10) | 0.004 |
| Went for walks a lot | 2.6 (1.47) | 3.35 (1.35) | 0.000 |
| Did a lot of physical work around the house/garden | 2.95 (1.43) | 3.25 (1.52) | 0.163 |
| Avoided intense activity | 2.4 (1.39) | 2.15 (1.53) | 0.330 |
| Avoided moderate activity | 2.25 (1.25) | 1.65 (1.18) | 0.024 |
Figure 2.
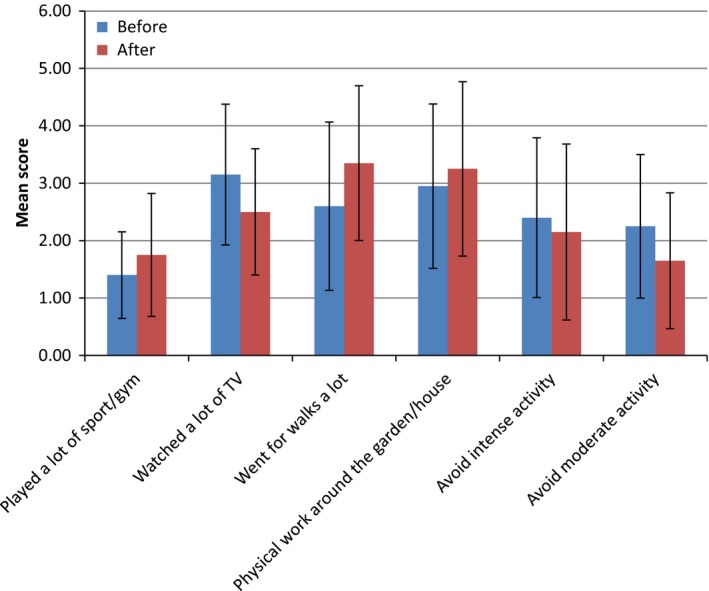
Physical activity levels and sedentary behaviours pre‐ and post‐intervention
4. DISCUSSION
This service evaluation found that referral from primary care to a community‐based weight management programme was successful in both supporting female and male patients with established diabetes to lose weight and improve their glycaemic control over a 12‐month period, with some of the patients being able to reduce their medication. Furthermore, some of the patients achieved their personally chosen target weight, around a third achieved glycaemic levels of 48 mmol/mol or below. These changes go against what one would expect to see in this patient group—diabetes is a chronic condition and routinely glycaemic control deteriorates in people with established diabetes unless medication increases. Small reductions were also observed in blood pressure levels and, whilst not significantly reduced, the changes are still likely to be of clinical benefit in reducing micro‐ and macrovascular complications in this patient group. The patients were generally all on statins and lipid profiles remained largely the same apart from the improvements seen in HDL cholesterol levels in the female patients, although also with increases in LDL levels, and triglyceride levels in the male patients. The reduction in weight at one year could be expected to result in a decrease in cardiovascular events over a period of ten years, based on adjusted observations from the Look AHEAD trial where results of the post hoc analysis suggest an association between the size of weight loss and incidence of cardiovascular disease in people with T2DM.12 In this trial, individuals who lost at least 10% of their bodyweight in the first year had a 21% lower risk of cardiovascular disease.
Attendance at the group, held within the practice building, was good. The intervention was found to be easy to access and acceptable to the patients responding to the follow‐up survey with more than a half of the patients attending either 11 or 12 of the twelve funded sessions and almost half of the total sample taking the opportunity to attend a local SW group for a further 12 weeks and then some continuing to self‐fund their weight management journey.
Whilst there was a significant correlation between the weight loss achieved at 12 months and HbA1c reduction, weight loss only contributed 60% of the variance seen in glycaemic control. Other factors such as the improvements in dietary habits and physical activity levels may also have contributed.
The SW approach to long‐term weight management is based on evidence‐based principles including behavioural strategies to improve dietary and physical activity habits.9, 10 Almost a third of the patients responded to the follow‐up survey, and these participants indicated that they had reduced their intake of takeaway and processed foods, which are often energy dense, reduced their intake of unhealthy snacks, increased their fruit and vegetable intake and cooked more meals from scratch as a consequence of the intervention. They also increased their activity levels, particularly walking with less avoidance of moderately intense activity and less time spent watching TV. These changes are sustainable, can fit in with family lifestyle being based on “normal” foods of lower energy density and activities suitable for the wider family. Generally, the respondents found the practical advice about healthy food choices and recipe ideas to be helpful. The intervention does not require any commercial dietary product or complex food reintroduction phase.
Of importance to the patients was the mutual support offered by the group intervention. The support of the group facilitator, the additional online support, the support from the diabetes special nurse and from peers was all highlighted as beingimportant. Individuals valued some of the support components more than others implying that individuals respond differently. Clearly, there were benefits of the partnership between the primary care practitioner and the commercial weight management organization which have been highlighted previously.13 The weekly group support was achieved with minimal NHS resource in terms of time, and if costed, the 12‐week intervention would be £60/patient. It is a model which could easily be replicated elsewhere, particularly referring to local SW groups rather than a bespoke group held within the surgery premises. 19 000 SW community‐based groups run each week facilitated by trained SW consultants although the partnership with the primary care practitioner is so important in ensuring that medication is appropriately reduced alongside weight loss.
An independent study investigating the cost‐effectiveness of primary care referral to SW groups14 reported that referral to the weight management programme fared more favourably than usual care, being both cheaper and more clinically effective. Their model adjusted quality‐of‐life simulations estimated lower lifetime rates for T2DM, stroke and MI as a consequence of the weight loss achieved.
Whilst the weight losses reported are less than for the DiRECT study, where the 137 subjects in the intervention group achieved a 10% weight loss at 12 months, the intervention requires less clinical supervision. The rapid early weight loss associated with the use of a low energy formula diet, and the composition of the formula used in the DiRECT study requires that all antihypertensive medications need to be withdrawn due to the risk of postural hypertension if antihypertensive drugs are continued.8 It has also been suggested that bariatric surgery offers the only solution to effective weight management in people with diabetes, and yet, this invasive intervention comes at a considerably higher financial cost and with the risk of long‐term clinical problems including micronutrient deficiencies15 and postprandial hypoglycaemia particularly after Roux‐en‐Y gastric bypass surgery16 and a postcode lottery as to who can access the surgery17.
The findings presented do support the conclusions of the Cochrane review18 where group‐based interventions encouraging self‐management strategies were found to be effective in significantly improving glycated haemoglobin levels, significantly reducing systolic blood pressure, body weight and the need for diabetes medications. The review concluded that for every five patients attending a group‐based lifestyle education programme, one patient could be expected to be able to reduce their diabetes medication.
4.1. Study limitations
The primary outcome data presented in this service evaluation were obtained from practice records with no self‐reported data included. Some of the secondary outcome data were missing with not all the patients going back for all their follow‐up appointments as requested, but other than the free referral to the SW group, the patients were offered no other incentive to participate in the study. One limitation is that we did not record how many patients were offered the intervention in order to calculate the take‐up rate or to be able to undertake intention‐to‐treat analysis, and thus, there is more potential for bias in this service evaluation compared to a controlled trial. The DSN undertook all of the additional reporting as an additional activity within this busy practice.
The service evaluation was undertaken at one practice in North Staffordshire, and thus, the patients included in the study were a relatively homogenous group, representative of the 10 000 patients attending this six‐partner practice just outside of the Potteries, an area of relatively low socio‐economic status.
This was a relatively low‐intensity intervention, welcomed by the DSN. The dietary approach included normal everyday foods which can be incorporated into family eating. Similarly, the changes in physical activity encouraged are sustainable. Despite being a chronic, progressive condition, this service evaluation found that referral from primary care to a weight management programme was successful in supporting patients with established diabetes to improve their diet and physical activity levels and lose weight and improve their glycaemic control 12 months later. Improvements in cardiovascular risk factors with some patients being able to reduce their medication were also seen. Given the low intensity and small gradual reductions in both weight and HbA1c levels, the risks of associated adverse effects are minimized. Patients who attended valued the support, and many continued to access support after the referral programme had ended.
CONFLICT OF INTERESTS
AA, RC, CP and JL all receive salaries from SW.
AUTHOR CONTRIBUTIONS
All authors were involved in designing the study and reviewing the manuscript. AA analysed the data and wrote the manuscript. JG referred patients and recorded the data at each time‐point.
ACKNOWLEDGEMENTS
Slimming World (SW) provided the 12‐ or 24‐week group support to patients referred by the DSN at no cost to the practice. The referred patients had access to all of the supporting materials available to self‐funding members.
Avery A, Griffin J, Stokes J, Coulton R, Pallister C, Lavin J. The benefits of non‐surgical weight management on weight and glycaemic control in people with complex type 2 diabetes: A primary care service evaluation of clinical outcomes at 12 months. Endocrinol Diab Metab. 2019;2:e00045 10.1002/edm2.45
DATA ACCESSIBILITY
This was a service evaluation, and thus due to ethical concerns, supporting data cannot be made openly available. Additional details relating to other aspects of the anonymized data are available from the corresponding author with the permission of the practice.
REFERENCES
- 1. NICE . NICE guideline 28 Type 2 diabetes in adults: management; 2015. https://www.nice.org.uk/guidance/ng28. Accessed September 17, 2018.
- 2. Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Currie CJ, Peters JR, Tynan A, et al. Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;2010:22‐24. 10.1016/S0140-6736(09)61969-3 [DOI] [PubMed] [Google Scholar]
- 4. Hemmingsen B, Lund SS, Gluud C, Vaag A, Almdal TP, Wetterslev J. Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2015;(7):CD008143 10.1002/14651858.CD008143.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kennedy M, Roberts A. Complex type 2 diabetes mellitus‐management challenges and pitfalls. Aust Fam Physician. 2013;42:207‐210. [PubMed] [Google Scholar]
- 6. Huxley R, Balzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta‐analysis of 37 prospective cohort studies. BMJ. 2006; 332(7533):73‐78. 10.1136/bmj.38678.389583.7C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Papaetis GS, Papakyriakou P, Panagiotou TN. Central obesity, type 2 diabetes and insulin: exploring a pathway full of thorns. Arch Med Sci. 2015;11(3):463‐482. 10.5114/aoms.2015.52350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lean M, Leslie WS, Barnes AC, et al. Primary care‐led weight management for remission of type 2 diabetes (DiRECT): an open‐label, cluster‐randomised trial. Lancet. 2018;391(10120):541‐551. 10.1016/S0140-6736(17)33102-1. [DOI] [PubMed] [Google Scholar]
- 9. NICE . Weight management: lifestyle services for overweight or obese adults Public health guideline [PH53]; 2014. https://www.nice.org.uk/guidance/ph53. Accessed September 17, 2018.
- 10. Stubbs J, Morris L, Pallister C, Horgan G, Lavin J. Weight outcomes audit in 1.3 million adults during their first 3 months’ attendance in a commercial weight management programme. BMC Public Health. 2015;15:822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Avery A, Nagar R, Hillier S, Pallister C, Lavin J, Mellor D. Studying the impact on weight and glycaemic control in adults with diabetes attending a group‐based commercial weight management programme. Practice Nursing. 2017;28(2):60‐66. [Google Scholar]
- 12. The Look AHEAD Research Group . Association of the magnitude of weight loss and changes in physical fitness with long‐term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post‐hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016;4:913‐921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lavin JH, Avery A, Whitehead SM, et al. Feasibility and benefits of implementing a Slimming on Referral service in primary care using a commercial weight management partner. Public Health. 2006;120(9):872‐881. [DOI] [PubMed] [Google Scholar]
- 14. Meads DM, Hulme CT, Hall P, Hill AJ. The cost‐effectiveness of primary care referral to a UK commercial weight loss programme. Clinical Obesity. 2014;4:324‐332. [DOI] [PubMed] [Google Scholar]
- 15. Shankar P, Boylan M, Sriram K. Micronutrient deficiencies after bariatric surgery. Nutrition. 2010;26(11–12):1031‐1037. 10.1016/j.nut.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 16. Millstein R, Lawler HM. Hypoglycemia after gastric bypass: An emerging complication. Clevel Clin J Med. 2017;84(4):319‐328. [DOI] [PubMed] [Google Scholar]
- 17. Kmietowicz Z. Postcode lottery persists over weight loss surgery despite NICE guidance. BMJ. 2010;340:c427. [Google Scholar]
- 18. Deakin T, McShane C, Cade J, Williams R. Group based training for self‐management strategies in people with type 2 diabetes mellitus. Cochrane Library. 2005:CD003417 10.1002/14651858 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This was a service evaluation, and thus due to ethical concerns, supporting data cannot be made openly available. Additional details relating to other aspects of the anonymized data are available from the corresponding author with the permission of the practice.


