Abstract
Identifying factors that affect adolescent lifestyle behaviors is essential in order to develop effective generic prevention approaches. This study aimed to investigate the association between parental monitoring, parental emotional support, parental-adolescent conflict and adolescent substance use, meal pattern and food choices. The study included data from 13,269 Norwegian adolescents aged 13–16 years collected in 2016. Multivariable logistic regression models adjusted for gender, age and parental education were applied. Results show that low parental monitoring was associated with increased substance use (Odds ratios (OR) ranging from 2.8; 95% Confidence intervals (CI) 2.1–3.6 to OR 3.8; 95% CI, 2.7–5.3) and irregular meal patterns (1.7; 1.3–2.1 to 2.6; 2.1–3.3), low fish intake (1.3;1.0–1.7), and high intake of sugar-sweetened beverages, diet beverages and energy drinks (1.4;1.1–1.7 to 2.1;1.6–2.8). Low parental emotional support was associated with increased substance use (1.8;1.5–2.1 to 2.5;1.9–3.2), irregular meal patterns (2.0; 1.8–2.3 to 2.1;1.9–2.3), low intake of vegetables, fruits and fish (1.3; 1.1–1.5 to 1.5; 1.3–1.7) and high intake of salty snacks, candy, cakes, sugar-sweetened beverages, diet beverages and energy drinks (1.4; 1.2–1.6 to 2.1;1.7–2.5). Finally, high parent-adolescent conflict was associated with increased substance use (2.3; 2.0–2.7 to 2.7; 2.3–3.1), irregular meal patterns (1.6 ;1.5–1.8 to 1.9;1.7–2.1), low intake of fruits and fish (1.3; 1.1–1.5 to 1.5; 1.3–1.7) and high intake of salty snacks, candy, cakes, sugar-sweetened beverages, diet beverages and energy drinks (1.5; 1.3–1.7 to 2.1; 1.8–2.5). Overall, parenting was associated with a range of lifestyle outcomes among adolescents. Family-strengthening interventions may have an impact on multiple public health domains.
Keywords: Diet, food, and nutrition; Adolescent alcohol use; Cannabis; Parenting; Smoking; Meals
Highlights
-
•
Adolescent unhealthy lifestyle is associated with low parental monitoring.
-
•
Adolescent unhealthy lifestyle is related to low parental emotional support.
-
•
Adolescent unhealthy lifestyle is related to parent-offspring conflict level.
1. Introduction
Adolescence is a fundamental period for the development of good health, and lifestyle habits established in this period may have impact on both present and later health. Substance use and unhealthy dietary habits are two of the most serious threats to adolescent health worldwide (WHO, 2016a; Lim et al., 2012), and the risk includes both acute and long-term harm (Rehm, 2011; Siddiqi et al., 2015; Danielsson et al., 2012; WHO, 2016b; Hallstrom et al., 2013; Marlatt et al., 2016; Oellingrath et al., 2014; Sjoberg et al., 2003). Identifying factors that affect adolescent lifestyle behaviors is essential in order to develop effective, generic prevention approaches to reduce negative health outcomes and strengthen adolescent health.
Family is a universal context for adolescent development, and the influence of parenting on a range of adolescent outcomes has been well established in the literature (Pyper et al., 2016; Philips et al., 2014; Dickson et al., 2015). Research has documented that both increased substance use and unhealthy dietary habits are related to the lack of parental monitoring and supervision (Gossrau-Breen et al., 2010; Latendresse et al., 2008), (Philips et al., 2014; Gevers et al., 2015; Rhee et al., 2015; Berge et al., 2014). Furthermore, warm, caring, encouraging and supportive parenting (Morton et al., 2012; Berge et al., 2010) has also been shown to be predictive of healthy dietary habits and reduced substance use in adolescence (Pyper et al., 2016; Knight et al., 1998; Barber, 1992). Conversely, parental conflict has been implicated as a predictor of increased adolescent substance use (Farrell and White, 1998; Brody and Forehand, 1993). Several studies have also found prospective associations between low family affection or high family conflict and nutritional related issues (Berge et al., 2014; Johnson et al., 2002; May et al., 2006).
The literature above demonstrates that general parenting practices seem to impact how children and adolescents respond to specific substance use and nutritional issues during adolescence. However, the parenting factors vary between studies in terms of how the specific parental behavior is defined and measured. Most studies also address only one type of outcome, substance use or nutrition. This makes it difficult to apply existing knowledge in developing generic preventive approaches aimed at reducing both substance use and unhealthy dietary habits among adolescents. There is therefore a need for more comprehensive studies addressing the relationship between parenting and a broader spectrum of adolescent lifestyle outcomes.
Thus, the aim of this study is to explore whether parenting, such as parental monitoring and emotional support, parent - adolescent conflict level, is associated with adolescent substance use and nutrition habits.
2. Materials and methods
2.1. Design and participants
Young-data (Ungdata) is a cross-national data collection scheme, designed to conduct surveys of adolescents in Norway at the municipality level (for more information on Ungdata, see ungdata.no). The Norwegian Social Research, Oslo and Akershus University College of Applied Sciences, cooperate with regional resource centres and the counties to recruit municipalities to the survey. In the southern region, both counties and all 30 municipalities participated, and this included all 70 schools.
In this study, we included junior high school students (grades 8–10, age range 13–16 years) and high school students (grade 11, age range 16–17 years). The data collection was conducted in the period from February to March 2016, and a total of 15,651 students were invited to participate in the study; 11,042 junior high school students and 4609 high school students, respectively. Of these, 13,635 completed and returned the questionnaire; this yields a participation rate of 90% among junior high school students and 80% among high school students. Total N of 13.269 refers to the final sample of respondents after the removal of respondents that provided severely inconsistent or spurious responses. The submission of the questionnaire online did not require responses on each item, so the n per question varied. In multivariable models, only those who have completed responses to exposure variables, the outcome variable in question, and possible confounders are included.
An information letter was directed to both parents and students and sent at least 14 days before initiation of the data collection, and the schools were to inform parents and adolescents about this through established information channels. The information letter was approved by the The Norwegian Centre for Research Data (NSD) Parents were given the opportunity to withdraw their children from participation, and the students decided for themselves if they wanted to participate. All participants filled in an online questionnaire anonymously during school hours on their own computer or iPad, and this took approximately 30–45 min to complete. At least one member of the project group was available to answer questions. The study was conducted in accordance with ethical guidelines and law.
The overall legal responsibility for Young-Data survey is held by the research centre NOVA (The Norwegian Social Research, Oslo and Akershus University College of Applied Sciences). The Norwegian Centre for Research Data (NSD) is the Data Protection Official for Research for all the Norwegian universities, university colleges and several hospitals and research institutes. According to their guidelines (http://www.nsd.uib.no/nsd/english/pvo.html) this study is not subject to notification, because it does not include personal data according to the Personal Data Act. NOVA has also consulted the Regional Committee for medical and health research ethics and clarified that the Young-Data was not obligated to seek approval from this committee.
2.2. Measures
All measures were based on adolescent self-reports.
2.2.1. Outcome variables
2.2.1.1. Adolescent substance use
Intoxication was measured by asking respondents how many times they had been clearly intoxicated the past 12 months with five response alternatives: never, once, 2–5 times, 6–10 times, and >11 times (Roberts et al., 2009). The variable was categorized as a binary variable including any intoxication episodes vs. no intoxication episodes.
Cannabis use was measured by asking respondents how many times they had used hashish/marihuana/cannabis during the past 12 months with five response alternatives: never, once, 2–5 times, 6–10 times, and >11 times. The variable was categorized as a binary variable including any use vs. no use.
Smoking (tobacco) was measured by asking respondents whether they smoke (Post et al., 2005). There were five response categories: 1. Have never smoked; 2. Have smoked earlier, but have quit; 3. Smoke more seldom than once a week; 4. Weekly smoking, but not daily 5. Daily smoking. This variable was applied as a binary variable including current smoking (category 3–5) vs no current smoking (category 1–2) (Lochen et al., 2017).
Use of smokeless tobacco was retrieved by asking respondents whether they use snuff (Post et al., 2005). There were five response categories: 1. Have never used smokeless tobacco; 2. Have used smokeless tobacco earlier, but have quit; 3. Use smokeless tobacco more seldom than once a week; 4. Weekly use, but not daily 5. Daily use. This variable was applied as a binary variable including current use (category 3–5) vs no current use of smokeless tobacco (category 1–2).
2.2.1.2. Adolescent food choices
Diet and beverage intake were assessed by asking respondents how often they eat vegetables, fruits, fish, salty snacks, candy, cakes and how often they drink sugar-sweetened beverages, diet beverages and energy drinks. All items had ten different response alternatives, ranging from never to more than once a day, and the response alternatives were further dichotomized into having high or low intake of the selected food items and drinks. Having soft drinks, sweets and candy and a salty snack ≥4 times a week, respectively, was categorized as high intake. Having fruits, berries and vegetables less than once a day, and fish less than once a week was categorized as low intake. Previous studies reporting dietary habits among Norwegian adolescents have used similar questions and cut-off values which are thought to reflect dietary intake among Norwegian adolescents (Overby et al., 2013; Stea and Torstveit, 2014). In addition, these questions have shown good test-retest reliability (Stea and Torstveit, 2014).
2.2.1.3. Adolescent meal pattern
Meal frequency was assessed by asking respondents how often they have breakfast, lunch, dinner and evening meals each week (Stea and Torstveit, 2014). The items had four different response categories: 1. Never or seldom; 2. Once a week; 3. 2–5 times per week; 4. Daily. For statistical analyses, adolescents who reported a daily intake of these main meals were classified as regular breakfast-, lunch-, dinner-, and evening meal consumers, respectively (category 4), whereas those who omitted these main meals at least once a week were classified as irregular meal consumers (category 1–3).
2.2.2. Explanatory variables
Parental monitoring was measured by asking respondents to consider whether the assertion “My parents usually know where I am, and who I am with in my leisure time” 1) fits very well, 2) fits quite well 3), fits poorly or 4) fits very poorly. The variable was recoded into a dichotomous, variable, where the latter two response categories were recoded and defined as low parental monitoring and the first two categories were defined as high monitoring.
Parental emotional support was measured by asking respondent whether they would turn to parents for help if they had a personal problem and felt sad. Response categories were “certainly”, “maybe” and “no”. This variable was dichotomized into “low emotional support” (including maybe and no) vs. high emotional support (including certainly).
Parent-adolescent conflict level was attained by asking respondents to consider whether the assertion “I often quarrel with my parents” 1) fits very well, 2) fits quite well 3), fits poorly or 4) fits very poorly. The variable was dichotomized, and answers in category 1 and 2 where defined as high conflict and category 3 and 4 were defined as low conflict level.
2.2.3. Control variables
Parental education was applied as a measure of socioeconomic status (SES), and this information was retrieved by asking respondents whether their mother and whether their father had college/university education. Response categories where binary no vs. yes for both maternal education and for paternal education.
Class-level was applied as a proxy for adolescent age and was measured by asking respondents which class-level they attended. Grades 8–10 equals the age range 13–16 years, and grade 11 equals the age range 16–17 years. This was included as a continuous variable in multivariable analyses.
Adolescent gender was retrieved by asking respondents whether they were male or female.
2.3. Statistical analysis
Descriptive analyses were performed initially to get an overview of the data.
Logistic regression analyses were applied to explore possible associations between parental factors and any of the defined risk outcomes reported by the adolescents. Results were reported by odds ratios (ORs), 95% confidence intervals (CIs) with the respective p-values with a significance level set to p < .05 (P). Multivariable analyses were adjusted for parental education, adolescent age and gender.
3. Results
3.1. Descriptive analyses
Table 1 provides a descriptive overview of the prevalence related to the various background/control variables, exposure variables and outcome variables included in the multivariable analyses. Age and gender were evenly distributed among the population, and there were slightly more fathers with lower education (34%) than mothers (29%). Low parental emotional support (18%) and high level of parent-adolescent conflict (22%) were more common than low parental monitoring (4%). Prevalence of outcome risk behaviors varied from cannabis use at 3% to low intake of fruits at 74%.
Table 1.
Descriptive statistics (n = 13.269). Norway, 2016.
| Variables | % (n) | |
|---|---|---|
| Control/background variables | Gender, boys | 50.9 (6548) |
| Gender, girls | 49.1 (6318) | |
| Age, 8th grade junior high school | 24.3 (3131) | |
| Age, 9th grade junior high school | 24.1 (3105) | |
| Age, 10th grade junior high school | 25 (3223) | |
| Age, 1.th grade senior high school | 26.6 (3436) | |
| Paternal education, lower | 34 (3949) | |
| Maternal education, lower | 28.8 (3410) | |
| Exposure variables | Low parental monitoring | 4.3 (567) |
| Low parental emotional support | 18.2 (2264) | |
| High parent-offspring conflict level | 22.1 (2858) | |
| Dependent variables | Alcohol intoxication last 12 months | 17.3 (2205) |
| Cannabis use last 12 months | 3.1 (398) | |
| Currently smoking | 8.1 (1040) | |
| Currently use of smokeless tobacco | 8.6 (1103) | |
| Irregular breakfast | 31.7 (4008) | |
| Irregular lunch | 35.6 (4503) | |
| Irregular dinner | 14 (1775) | |
| Irregular evening | 53.2 (5054) | |
| Low intake of vegetables | 69.2 (7632) | |
| Low intake of fruits | 73.9 (8363) | |
| Low intake of fish | 23.3 (2664) | |
| High intake of salty snacks | 11.8 (1344) | |
| High intake of candy | 15.6 (1779) | |
| High intake of cakes | 9.3 (1060) | |
| High intake of sugar sweetened beverages | 27.1 (3138) | |
| High intake of diet beverages | 19.1 (2193) | |
| High intake of energy drinks | 7.2 (830) | |
Crude data presented in Table 2 indicate a higher prevalence of risk behavior associated with low parental monitoring and emotional support and high parent-adolescent conflict level.
Table 2.
Crude associations between exposure variables and outcome variables, percentages and chi-squarea. Norway, 2016.
| Outcomes | Exposure variables |
||
|---|---|---|---|
| Low/high parental monitoring |
Low/high parental emotional support |
High/low parent-offspring conflict level |
|
| % (n) | % (n) | % (n) | |
| Alcohol intoxication last 12 months | 53.5/17.4 (n = 13,180) | 34.2/15.4(n = 12,893) | 30.3/15.8 (n = 13,070) |
| Cannabis use last 12 months | 16.9/2.7 (n = 13,160) | 7.8/2.1 (n = 12,871) | 7.1/2.2 (n = 13,051) |
| Currently smoking | 33.5/7.3 (n = 13,264) | 17.1/6.2 (n = 12,906) | 16.4/6.2 (n = 13,146) |
| Current use of smokeless tobacco | 31.2/8.2 (n = 13,260) | 17.5/7.0 (n = 12,902) | 16.6/7.1 (n = 13,141) |
| Irregular breakfast | 58.8/30.9 (n = 13,062) | 51.5/27.7 (n = 12,829) | 47.0/27.9 (n = 12,974) |
| Irregular lunch | 59.1/34.5 (n = 13,090) | 53.5/31.4 (n = 12,824) | 49.0/31.8 (n = 12,975) |
| Irregular dinner | 37.7/13.1 (n = 13,081) | 27.1/11.0 (n = 12,817) | 23.8/11.3 (n = 12,967) |
| Irregular evening | 65.9/53.1 (n = 11,820) | 63.7/51.2 (n = 11,636) | 61.7/51.3 (n = 11,733) |
| Low intake of vegetables | 80.0/68.9 (n = 11,442) | 75.1/68.2 (n = 11,242) | 72.3/68.5 (n = 11,357) |
| Low intake of fruits | 84.1/73.8 (n = 11,734) | 79.4/73.2 (n = 11,529) | 77.7/73.2 (n = 11,644) |
| Low intake of fish | 34.7/22.9 (n = 11,858) | 32.7/21.3 (n = 11,665) | 31.3/21.1 (n = 11,769) |
| High intake of salty snacks | 19.4/11.6 (n = 11,875) | 17.2/10.6 (n = 11,685) | 17.6/10.3 (n = 11,786) |
| High intake of candy | 22.3/15.3 (n = 11,848) | 22.1/14.1 (n = 11,656) | 22.9/13.6 (n = 11,758) |
| High intake of cakes | 14.2/9.0 (n = 11,830) | 13.9/8.1 (n = 11,643) | 14.1/8.0 (n = 11,743) |
| High intake of sugar sweetened beverages | 41.8/26.8 (n = 12,006) | 34.8/25.7 (n = 11,793) | 34.9/25.3 (n = 11,912) |
| High intake of diet beverages | 28.3/18.9 (n = 11,896) | 25.7/17.8 (n = 11,689) | 25.9/17.5 (n = 11,804) |
| High intake of energy drinks | 20.7/6.6 (n = 11,943) | 13.1/5.7 (n = 11,738) | 12.4/5.8 (n = 11,850) |
Based on data from Norwegian 13.269 adolescents collected in 2016.
All associations were significant (p < .001).
3.2. Multivariable analyses
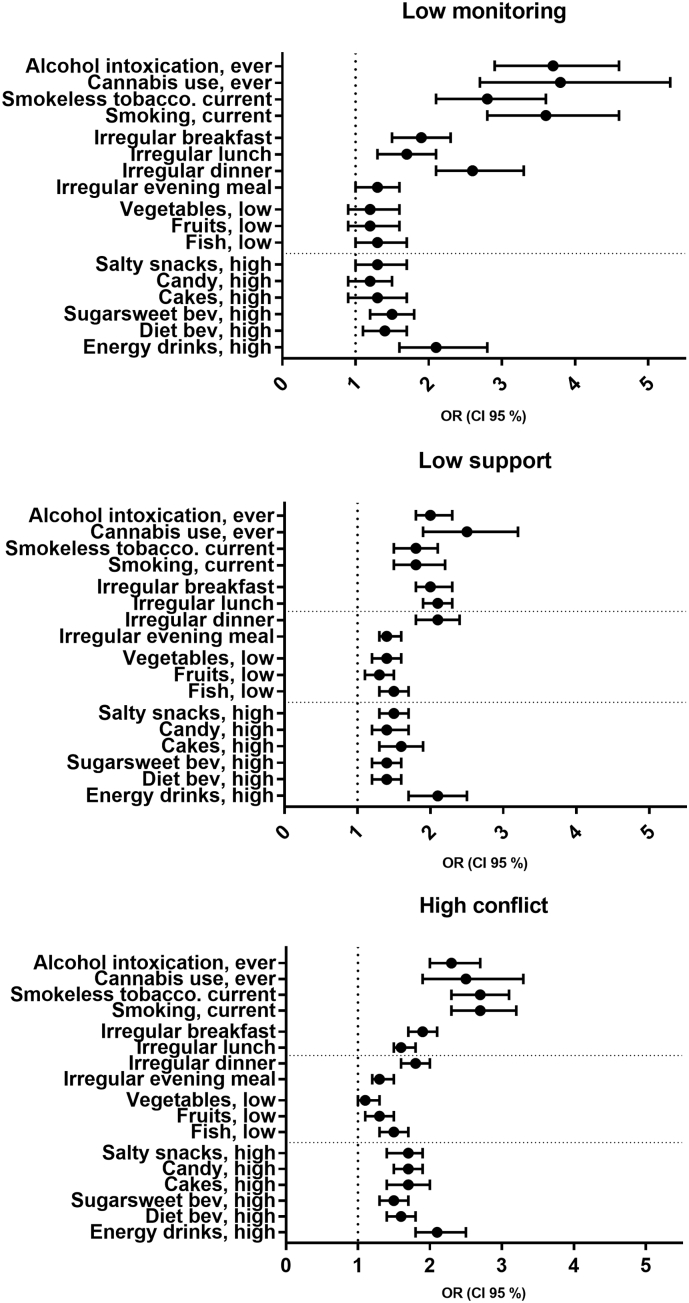
All main results are reported using Odds Ratios with 95% confidence intervals and respective p-values, and results are displayed in Fig. 1, and full models in Table 3, Table 4, Table 5, Table 6. All multivariable analyses were adjusted for age, gender and parental education.
Fig. 1.
Main adjusted results between parenting and adolescent lifestyle habits (OR and 95%). Norway, 2016. Associations between parental monitoring and substance use, meal pattern and food choices, associations between parental emotional support and substance use, meal pattern and food choices, and associations between parent-adolescent conflict level and substance use, meal pattern and food choices.
Table 3.
Associations between parenting and adolescent substance use risk behavior, adjusted for age, gender and parental education. Multivariable logistic regression. Norway, 2016.
| Alcohol, intoxication, ever |
Cannabis use, ever |
Smokeless tobacco, current |
Smoking, current |
||
|---|---|---|---|---|---|
| OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | ||
| Exposure variables | Parental monitoring (low) | 3.7 (2.9–4.6)⁎⁎⁎ | 3.8 (2.7–5.3)⁎⁎⁎ | 2.8 (2.1–3.6)⁎⁎⁎ | 3.6 (2.8–4.6)⁎⁎⁎ |
| Parental support (low) | 2.0 (1.8–2.3)⁎⁎⁎ | 2.5 (1.9–3.2)⁎⁎⁎ | 1.8 (1.5–2.1)⁎⁎⁎ | 1.8 (1.5–2.2)⁎⁎⁎ | |
| Conflicts with parents (high) | 2.3 (2.0–2.7)⁎⁎⁎ | 2.5 (1.9–3.3)⁎⁎⁎ | 2.7 (2.3–3.1)⁎⁎⁎ | 2.7 (2.3–3.2)⁎⁎⁎ | |
| Control variables | Gender (female) | 1.0 (0.9–1.1) | 0.5 (0.4–0.7)⁎⁎⁎ | 0.7 (0.6–0.8)⁎⁎⁎ | 0.6 (0.5–0.8)⁎⁎⁎ |
| Age | 2.7 (2.5–2.9)⁎⁎⁎ | 1.7 (1.5–2.0)⁎⁎⁎ | 2.0 (1.8–2.1)⁎⁎⁎ | 2.0 (1.8–2.2)⁎⁎⁎ | |
| Paternal education (low) | 1.1 (1.0–1.2) | 1.1 (0.8–1.4) | 1.2 (1.0–1.4)⁎ | 1.1 (0.9–1.3)⁎⁎ | |
| Maternal education (low) | 1.2 (1.0–1.3)⁎ | 1.3 (0.9–1.7) | 1.4 (1.2–1.7)⁎⁎⁎ | 1.4 (1.2–1.7)⁎⁎⁎ | |
p < .05.
p < .010.
p < .001.
Table 4.
Associations between parenting and meal patterns, adjusted for age, gender and parental education. Multivariable logistic regression. Norway, 2016.
| Irr. breakfast |
Irr. lunch |
Irr. dinner |
Irr. evening |
||
|---|---|---|---|---|---|
| OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | ||
| Exposure variables | Parental monitoring (low) | 1.9 (1.5–2.3)⁎⁎⁎ | 1.7 (1.3–2.1)⁎⁎⁎ | 2.6 (2.1–3.3)⁎⁎⁎ | 1.3 (1.0–1.6)⁎ |
| Parental support (low) | 2.0 (1.8–2.3)⁎⁎⁎ | 2.1 (1.9–2.3)⁎⁎⁎ | 2.1 (1.8–2.4)⁎⁎⁎ | 1.4 (1.3–1.6)⁎⁎⁎ | |
| Conflicts with parents (high) | 1.9 (1.7–2.1)⁎⁎⁎ | 1.6 (1.5–1.8)⁎⁎⁎ | 1.8 (1.6–2.0)⁎⁎⁎ | 1.3 (1.2–1.5)⁎⁎⁎ | |
| Control variables | Gender (female) | 1.5 (1.3–1.6)⁎⁎⁎ | 1.1 (1.0–1.2) | 1.5 (1.3–1.7)⁎⁎⁎ | 1.7 (1.5–1.8)⁎⁎⁎ |
| Age | 1.2 (1.2–1.3)⁎⁎⁎ | 1.0 (1.0–1.1) | 1.1 (1,0–1,1)⁎⁎ | 1.1 (1.1–1.2)⁎⁎⁎ | |
| Paternal education (low) | 1.2 (1.1–1.3)⁎⁎ | 1.1 (1.0–1.3)⁎ | 1.1 (1.0–1.3) | 1.1 (1.0–1.2) | |
| Maternal education (low) | 1.6 (1.4–1.8)⁎⁎⁎ | 1.3 (1.2–1.5)⁎⁎⁎ | 1.5 (1.3–1.7)⁎⁎⁎ | 1.1 (1.0–1.2) | |
p < .05.
p < .010.
p < .001.
Table 5.
Associations between parenting and low intake of healthy food choices, adjusted for age, gender and parental education Multivariable logistic regression. Norway, 2016.
| Vegetables, low |
Fruits, low |
Fish, low |
||
|---|---|---|---|---|
| OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | ||
| Exposure variables | Parental monitoring (low) | 1.2 (0.9–1.6) | 1.2 (0.9–1.6) | 1.3 (1.0–1.7)⁎ |
| Parental support (low) | 1.4 (1.2–1.6)⁎⁎⁎ | 1.3 (1.1–1.5)⁎⁎⁎ | 1.5 (1.3–1.7)⁎⁎⁎ | |
| Conflicts with parents (high) | 1.1 (1.0–1.3) | 1.3 (1.1–1.5)⁎⁎⁎ | 1.5 (1.3–1.7)⁎⁎⁎ | |
| Control variables | Gender (female) | 0.6 (0.5–0.6)⁎⁎⁎ | 0.5 (0.4–0.5)⁎⁎⁎ | 1.0 (0.9–1.1) |
| Age | 1.0 (1.0–1.0) | 1.1 (1.1–1.2)⁎⁎⁎ | 1.0 (0.9–1.0)⁎⁎ | |
| Paternal education (low) | 1.4 (1.3–1.6)⁎⁎⁎ | 1.3 (1.2–1.5)⁎⁎⁎ | 1.4 (1.2–1.5)⁎⁎⁎ | |
| Maternal education (low) | 1.4 (1.2–1.5)⁎⁎⁎ | 1.3 (1.1–1.5)⁎⁎⁎ | 1.3 (1.2–1.5)⁎⁎⁎ | |
p < .05.
p < .010.
p < .001.
Table 6.
Associations between parenting and high intake of unhealthy food choices, adjusted for age, gender and parental education. Multivariable logistic regression. Norway, 2016.
| Salty snacks, high |
Candy, high |
Cakes, high |
Sugarsweet. Bev, high |
Diet bev, high |
Energy drinks, high |
||
|---|---|---|---|---|---|---|---|
| OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | OR (CI 95%) | ||
| Exposure variables | Parental monitoring (low) | 1.3 (1.0–1.7) | 1.2 (0.9–1.5) | 1.3 (0.9–1.7) | 1.5 (1.2–1.8)⁎⁎ | 1.4 (1.1–1.7)⁎ | 2.1 (1.6–2.8)⁎⁎⁎ |
| Parental support (low) | 1.5 (1.3–1.7)⁎⁎⁎ | 1.4 (1.2–1.7)⁎⁎⁎ | 1.6 (1.3–1.9)⁎⁎⁎ | 1.4 (1.2–1.6)⁎⁎⁎ | 1.4 (1.2–1.6)⁎⁎⁎ | 2.1 (1.7–2.5)⁎⁎⁎ | |
| Conflicts with parents (high) | 1.7 (1.4–1.9)⁎⁎⁎ | 1.7 (1.5–1.9)⁎⁎⁎ | 1.7 (1.4–2.0)⁎⁎⁎ | 1.5 (1.3–1.7)⁎⁎⁎ | 1.6 (1.4–1.8)⁎⁎⁎ | 2.1 (1.8–2.5)⁎⁎⁎ | |
| Control variables | Gender (female) | 0.9 (0.8–1.0)⁎ | 1.1 (1.0–1.3)⁎ | 0.9 (0.8–1.0) | 0.7 (0.6–0.8)⁎⁎⁎ | 0.9 (0.8–1.0)⁎ | 0.3 (0.3–0.4)⁎⁎⁎ |
| Age | 1.0 (1.0–1.1) | 1.1 (1.1–1.2)⁎⁎⁎ | 1.1 (1.0–1.1) | 1.1 (1.0–1.1)⁎⁎⁎ | 1.2 (1.1–1.2)⁎⁎⁎ | 1.1 (1.0–1.2)⁎ | |
| Paternal education (low) | 0.9 (0.9–1.2) | 1.0 (0.9–1.1) | 1.1 (0.9–1.3) | 1.0 (1.2) | 1.0 (0.9–1.1) | 0.9 (0.8–1.1) | |
| Maternal education (low) | 1.4 (1.2–1.6)⁎⁎⁎ | 1.3 (1.2–1.5)⁎⁎⁎ | 1.3 (1.1–1.6)⁎⁎ | 1.5 (1.3–1.7)⁎⁎⁎ | 1.2 (1.1–1.4)⁎⁎ | 1.4 (1.2–1.8)⁎⁎⁎ | |
p < .05.
p < .010.
p < .001.
Table 3 presents substance use among adolescents relative to parenting practices. The results revealed consistent associations between low parental monitoring and increased odds of adolescent alcohol intoxication (OR 3.7; 95% CI 2.9–4.6), cannabis use (3.8;2.7–5.3), smokeless tobacco (2.8;2.1–3.6), and smoking (3.6;2.8–4.6). Low parental emotional support was also associated with increased adolescent alcohol intoxication (2.0;1.8–2.3), cannabis use (2.5;1.9–3.2), smokeless tobacco 1.8;1.5–2.1), and smoking (1.8;1.5–2.2). Similarly, high level of conflicts between adolescents and their parents was associated with adolescent alcohol intoxication (2.3;2.0–2.7), cannabis use (2.5;1.9–3.3), smokeless tobacco (2.7;2.3–3.1), and smoking (2.7;2.3–3.2).
Table 4 presents irregular meal pattern among adolescents relative to parenting practices. The results showed significant associations between low parental monitoring and irregular intake of breakfast (1.9;1.5–2.3), lunch (1.7;1.3–2.1), dinner (2.6;2.1–3.3), and evening meal (1.3;1.0–1.6). Low emotional support was also associated with adolescent irregular intake of breakfast (2.0;1.8–2.3), dinner 2.1;1.8–2.4), and evening meal (1.4;1.3–1.6). In addition, high level of conflicts between adolescents and their parents was associated with an irregular intake of breakfast (1.9;1.7–2.1), lunch (1.6;1.5–1.8), dinner (1.8;1.6–2.0), and evening meal (1.3;1.2–1.5).
Table 5 presents low intake of healthy food items among adolescents relative to parenting practices. The results showed significant associations between low parental monitoring and low intake of fish (1.3;1.0–1.7), but not with low intake of vegetables or fruits. However, findings revealed significant associations between low parental emotional support and low intake of vegetables (1.4;1.2–1.6), fruits (1.3;1.1–1.5) and fish (1.5;1.3–1.7). High level of conflicts between adolescents and their parents was also associated with a low intake of fruits (1.3;1.1–1.5) and fish (1.5;1.3–1.7).
Table 6 presents high intake of unhealthy food and beverages among adolescents relative to parenting practices. The results revealed significant associations between low parental monitoring and a high intake of sugar sweetened beverages (1.5;1.2–1.8), diet beverages (1.4;1.1–1.7), and energy drinks (2.1;1.6–2.8). Furthermore, the results showed a significant association between low parental emotional support and a high intake of salty snacks (1.5; 1.3–1.7), sweets and candy (1.4; 1.2–1.7), cakes (1.6;1.3–1.9), and sugar-sweetened beverages (1.4; 1.2–1.6), diet beverages (1.4;1.2–1.6), and energy drinks (2.1;1.7–2.5).
High level of conflicts between adolescents and their parents was also associated with a high intake of salty snacks (1.7;1.4–1.9), candy (1.7;1.5–1.9), cakes (1.7;1.4–2.0), sugar-sweetened beverages (1.5;1.3–1.7), diet beverages (1.6;1.4–1.8), and energy drinks (2.1;1.8–2.5).
4. Discussion
The aim of this study was to explore whether parenting, such as parental monitoring and emotional support, parent - adolescent conflict level, was associated with adolescent substance use and nutrition habits. Findings revealed a consistent pattern of associations between aspects of general parenting and a broad range of adolescent lifestyle behaviors.
A strong positive association was found between low parental monitoring and increased adolescent intoxication, cannabis use, smoking and smokeless tobacco use. These results are in line with previous research which has indicated that parental monitoring reduces juvenile alcohol use (Gossrau-Breen et al., 2010; Latendresse et al., 2008; Enstad et al., 2017). Monitoring may be regarded as an expression of concern and interest for the child, and as the opposite, neglectful parenting style is almost consistently found to be associated with higher rates of substance use (Adalbjarnardottir and Hafsteinsson, 2001; Shucksmith et al., 1997). Our study revealed mixed results regarding the relationship between parental monitoring and dietary habits. Adolescents reporting low parental monitoring were more likely to report a low intake of fish and high intake of sugar sweetened beverages, diet beverages and energy drinks. On the other hand, no associations were found between low monitoring and low intake of fruits and vegetables or high intake of salty snacks, cakes and candy. Furthermore, low parental monitoring was associated with an irregular intake of all main meals, except evening meal. Overall, the results indicate that there is a stronger relationship between parental monitoring and the regularity of meals, than consumption of healthy and unhealthy food and beverages. The inconsistent findings regarding low parental monitoring and increased adolescent substance use, unhealthy food choices and irregular meal patterns may be due to inadequate capture of the construct of parental monitoring. Some theorists have suggested that measures of parental monitoring frequently have focused on how well informed parents are rather than on actual supervision and control of youth behavior (Stattin and Kerr, 2000). In recent reexaminations of the role of parental monitoring in problem behavior prevention, categorization of potential sources of parents' knowledge of their adolescent's activities, such as youth disclosure, parental solicitation, and parental control, have been used (Stattin and Kerr, 2000; Kerr and Stattin, 2000). This current study relied solely on adolescent self-report.
Results from the present study showing that lack of parental emotional support was associated with increased risk of substance use, unhealthy dietary habits and irregular meal pattern are in line with findings from previously published studies (Pyper et al., 2016; Knight et al., 1998). The strongest associations between low parental emotional support and adolescent lifestyle choices were found in relation to increased substance use, high intake of energy drinks and irregular meal patterns. However, associations between low emotional support and high intake of unhealthy food (salty snacks, candy, cakes, sugared/diet beverages) and low intake of healthy food (vegetables, fruits, fish) were consistent.
A high level of conflict between parents and offspring was also consistently related to increased risk of substance use, irregular meal pattern and high intake of unhealthy food and beverages and low intake of healthy food choices, except fruit intake. Again, the highest point estimates were found for substance use, but the increased odds of having an irregular meal pattern and a high intake of unhealthy food and beverages were substantial if adolescents reported a high level of conflict with their parents. Several explanations could be suggested for these associations. Both substance use and a high consumption of unhealthy food may be regarded as potential regulators of negative emotions (Harrist et al., 2013), and may increase in difficult emotional situations, such as conflicted relationship. Conflicted family relationship may also contribute to avoidance of meals within the home environment, resulting in irregular meal pattern (Neumark-Sztainer et al., 1999).
A major strength of the current study is the large representative sample and the high response rate. To our knowledge, no other studies have previously examined the association between parenting practices and such a broad range of lifestyle behaviors. Thus, results from this study provide important information which could be relevant to broader public health interventions than merely towards substance use or nutrition. A limitation of the present study is the cross-sectional design, which does not allow for causal inference. Further, there is a possibility for bi-directional relationships between adolescent lifestyle behavior and some parenting practices. For instance, it may be plausible that unhealthy lifestyle behavior among adolescents may increase the conflict-level between parents and adolescents. Van Der Vorst et al. (2010) found that among young males with the highest alcohol consumption more frequency of alcohol-specific communication predicted an increase in drinking (Van Der Vorst et al., 2010). Further studies with longitudinal design are warranted to clearly establish the causal directions.
In addition, our data relies on self-reported measures which may be influenced by recall bias. Questions were self-administered, and studies have shown that respondents are more willing to disclose sensitive information when questions are self-administered than when they are administered by an interviewer (Tourangeau and Yan, 2007). Further, the data was collected in a school setting, which have been found to be a better context for collecting sensitive data (Tourangeau and Yan, 2007). The inconsistency in responses to questions of intoxication and cannabis use have been assessed to be very low (0–1%) (Kraus and Nociar, 2016). Several of the items included have also been used in other large scale surveys among adolescents (Roberts et al., 2009; Kraus and Nociar, 2016). Although categorization of outcome variables is comparable with other studies (Overby et al., 2013; Stea and Torstveit, 2014; Torstveit et al., 2018), dichotomization may lead to some loss of information. Various alternative categorization of several of the outcome variables revealed similar results.
Multivariate analyses were adjusted for parental education. Although this is a commonly used SES-measure (Callahan and Eyberg, 2010), it may only partially capture the socioeconomic status of the family. Various SES-measures may capture different aspects of the socioeconomic background and must be interpreted with care.
In addition to parental education, we have repeated the multivariate analyses applying another subjective SES-measure; “perceived financial situation”. This was measured by asking respondents how they perceived their family's finances over the past two years, with five response categories; our finances have been good/mostly good/neither good nor bad/mostly poor/have been poor for the entire period. Adjusting for this SES-measure instead of parental education did not alter the main findings concerning the relationship between parenting and adolescent lifestyle habits. We would argue that parental education may be a relevant approach when it comes to the relationship between parenting and adolescent outcomes (Roubinov and Boyce, 2017). Other researchers have conjectured that through the “knowledge gap hypothesis” parents with higher levels of education will be exposed to, acquire, and adopt information relevant to parenting practices more rapidly than parents with lower education (Radey and Randolph, 2009). Parental practices are reported by adolescents only, leaving it uncertain whether this matches actual parental behavior. Several studies have revealed discrepancies in adolescent report of parental behavior and parental own report, and findings suggests that parents' and children's reports may capture subtly various aspects of parenting behavior (Abar et al., 2015; Reynolds et al., 2011). However, findings also suggest that adolescent perception of parenting behavior is highly relevant to adolescent lifestyle and health (Pisinger et al., 2016; Aas et al., 1996), and may also have a greater predictive value over parental report in relation to adolescent lifestyle behavior (Abar et al., 2015; Aas et al., 1996; Latendresse et al., 2009).
5. Conclusions
A broad range of lifestyle outcomes among Norwegian adolescents were associated with general parenting practices such as parental monitoring, emotional support and adolescent-parental conflicts. The findings provide valuable knowledge, as the identification of general parenting factors that may affect several adolescent lifestyle behaviors is important in order to develop generic prevention approaches to reduce negative health outcomes and strengthen adolescent health. A recent research review (Petrie et al., 2007) concluded that the most effective family skills training programmes include active parental involvement, focus on the development of adolescents' social skills and responsibility among children and adolescents, and address issues related to substance abuse. Effective interventions also involve youth in family activities and strengthen family bonds. Practitioners working with families who have adolescents need to include monitoring and supervision practices and practical steps parents can take to improve their monitoring skills. Raising awareness in parents of the importance of giving emotional support to adolescents may be useful in relation to preventing substance use and unhealthy dietary habits.
Conflict of interest
Authors declare no conflict of interest.
Acknowledgements
We are grateful to all the participating adolescents. The authors thank the Norwegian Social Research (NOVA), the southern regional Drug and Alcohol Competence Centre (Korus) and the municipalities for their contributions to the data collection.
Contributor Information
Siri Håvås Haugland, Email: siri.h.haugland@uia.no.
Lindsey Coombes, Email: elcoombes@brookes.ac.uk.
Tonje Holte Stea, Email: tonje.h.stea@uia.no.
References
- Aas H., Jakobsen R., Anderssen N. Predicting 13-year-olds' drinking using parents' self-reported alcohol use and restrictiveness compared with offspring's perception. Scand. J. Psychol. 1996;37(2):113–120. doi: 10.1111/j.1467-9450.1996.tb00644.x. (PubMed PMID: WOS:A1996UR48100001) [DOI] [PubMed] [Google Scholar]
- Abar CC, Jackson KM, Colby SM, Barnett NP. Parent-child discrepancies in reports of parental monitoring and their relationship to adolescent alcohol-related behaviors. J Youth Adolescence. 2015;44(9):1688–701. doi: 10.1007/s10964-014-0143-6. PubMed PMID: WOS:(000360912200003). [DOI] [PMC free article] [PubMed]
- Adalbjarnardottir S., Hafsteinsson L.G. Adolescents' perceived parenting styles and their substance use: concurrent and longitudinal analyses. J Res Adolescence. 2001;11(4):401–423. (PubMed PMID: WOS:000172811100004) [Google Scholar]
- Barber B.K. Family, personality, and adolescent problem behaviors. J Marriage Fam. 1992;54(1):69–79. (PubMed PMID: WOS:A1992HG96300006) [Google Scholar]
- Berge J.M., Wall M., Loth K., Neumark-Sztainer D. Parenting style as a predictor of adolescent weight and weight-related behaviors. J Adolescent Health. 2010;46(4):331–338. doi: 10.1016/j.jadohealth.2009.08.004. (PubMed PMID: WOS:000275784700005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Wall M, Larson N, Eisenberg ME, Loth KA, Neumark-Sztainer D. The unique and additive associations of family functioning and parenting practices with disordered eating behaviors in diverse adolescents. J. Behav. Med.. 2014;37(2):205–17. doi: 10.1007/s10865-012-9478-1. PubMed PMID: WOS:(000332689300004). [DOI] [PMC free article] [PubMed]
- Brody G.H., Forehand R. Prospective associations among family form, family processes, and adolescents alcohol and drug-use. Behav. Res. Ther. 1993;31(6):587–593. doi: 10.1016/0005-7967(93)90110-g. (PubMed PMID: WOS:A1993LM22000006) [DOI] [PubMed] [Google Scholar]
- Callahan C.L., Eyberg S.M. Relations between parenting behavior and SES in a clinical sample: validity of SES measures. Child & Family Behavior Therapy. 2010;32(2):125–138. [Google Scholar]
- Danielsson A.K., Wennberg P., Hibell B., Romelsjo A. Alcohol use, heavy episodic drinking and subsequent problems among adolescents in 23 European countries: does the prevention paradox apply? Addiction. 2012;107(1):71–80. doi: 10.1111/j.1360-0443.2011.03537.x. Epub 2011/06/16. (PubMed PMID: 21672071) [DOI] [PubMed] [Google Scholar]
- Dickson D.J., Laursen B., Stattin H., Kerr M. Parental supervision and alcohol abuse among adolescent girls. Pediatrics. 2015;136(4):617–624. doi: 10.1542/peds.2015-1258. Epub 2015/09/24. (PubMed PMID: 26391935; PubMed Central PMCID: PMCPMC4586729) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enstad F., Pedersen W., Nilsen W., von Soest T. Predicting early onset of intoxication versus drinking-a population-based prospective study of Norwegian adolescents. Addict. Behav. Rep. 2017;6:1–7. doi: 10.1016/j.abrep.2017.04.002. Epub 2018/02/17. (PubMed PMID: 29450232; PubMed Central PMCID: PMCPMC5800584) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell A.D., White K.S. Peer influences and drug use among urban adolescents: family structure and parent-adolescent relationship as protective factors. J Consult Clin Psych. 1998;66(2):248–258. doi: 10.1037//0022-006x.66.2.248. (PubMed PMID: WOS:000073178500004) [DOI] [PubMed] [Google Scholar]
- Gevers DWM, van Assema P, Sleddens EFC, de Vries NK, Kremers SPJ. Associations between general parenting, restrictive snacking rules, and adolescent's snack intake. The roles of fathers and mothers and interparental congruence. Appetite. 2015;87:184–91. doi: 10.1016/j.appet.2014.12.220. PubMed PMID: WOS:(000350517800023). [DOI] [PubMed]
- Gossrau-Breen D, Kuntsche E, Gmel G. My older sibling was drunk - younger siblings' drunkenness in relation to parental monitoring and the parent-adolescent relationship. J. Adolesc.. 2010;33(5):643–52. doi: 10.1016/j.adolescence.2009.11.006. PubMed PMID: (20004961). [DOI] [PubMed]
- Hallstrom L, Labayen I, Ruiz JR, Patterson E, Vereecken CA, Breidenassel C, et al. Breakfast consumption and CVD risk factors in European adolescents: the HELENA (healthy lifestyle in Europe by nutrition in adolescence) study. Public Health Nutr.. 2013;16(7):1296–305. doi: 10.1017/S1368980012000973. PubMed PMID: (22494882). [DOI] [PMC free article] [PubMed]
- Harrist AW, Hubbs-Tait L, Topham GL, Shriver LH, Page MC. Emotion regulation is related to children's emotional and external eating. J. Dev. Behav. Pediatr.. 2013;34(8):557–65. PubMed PMID: WOS:(000330359300006). [DOI] [PubMed]
- Johnson J.G., Cohen P., Kasen S., Brook J.S. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. Am J Psychiat. 2002;159(3):394–400. doi: 10.1176/appi.ajp.159.3.394. (PubMed PMID: WOS:000174186400009) [DOI] [PubMed] [Google Scholar]
- Kerr M., Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: further support for a reinterpretation of monitoring. Dev. Psychol. 2000;36(3):366–380. (PubMed PMID: WOS:000086929200007) [PubMed] [Google Scholar]
- Knight D.K., Broome K.M., Cross D.R., Simpson D.D. Antisocial tendency among drug-addicted adults: potential long-term effects of parental absence, support, and conflict during childhood. Am J Drug Alcohol Ab. 1998;24(3):361–375. doi: 10.3109/00952999809016903. (PubMed PMID: WOS:000075721000002) [DOI] [PubMed] [Google Scholar]
- Kraus L., Nociar A. European Monitoring Centre for Drugs and Drug Addiction; 2016. ESPAD Report 2015: Results from the European School Survey Project on Alcohol and Other Drugs. [Google Scholar]
- Latendresse SJ, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, Dick DM. Parenting mechanisms in links between parents' and adolescents' alcohol use behaviors. Alcohol. Clin. Exp. Res.. 2008;32(2):322–30. doi: 10.1111/j.1530-0277.2007.00583.x. PubMed PMID: 18162066; PubMed Central PMCID: (PMCPMC2504716). [DOI] [PMC free article] [PubMed]
- Latendresse SJ, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, Dick DM. Parental socialization and adolescents' alcohol use behaviors: predictive disparities in parents' versus adolescents' perceptions of the parenting environment. J Clin Child Adolesc. 2009;38(2):232–44. doi: 10.1080/15374410802698404. PubMed PMID: WOS:(000264765000005). [DOI] [PMC free article] [PubMed]
- Lim S.S., Vos T., Flaxman A.D., Danaei G., Shibuya K., Adair-Rohani H. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. Epub 2012/12/19. (PubMed PMID: 23245609; PubMed Central PMCID: PMCPMC4156511) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lochen M.L., Gram I.T., Mannsverk J., Mathiesen E.B., Njolstad I., Schirmer H. Association of occasional smoking with total mortality in the population-based Tromso study, 2001–2015. BMJ Open. 2017;7(12):e019107. doi: 10.1136/bmjopen-2017-019107. Epub 2017/12/31. (PubMed PMID: 29288187; PubMed Central PMCID: PMCPMC5770901) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt K.L., Farbakhsh K., Dengel D.R., Lytle L.A. Breakfast and fast food consumption are associated with selected biomarkers in adolescents. Prev. Med. Rep. 2016;3:49–52. doi: 10.1016/j.pmedr.2015.11.014. (PubMed PMID: PMC4733061) [DOI] [PMC free article] [PubMed] [Google Scholar]
- May A.L., Kim J.Y., McHale S.M., Crouter A.C. Parent-adolescent relationships and the development of weight concerns from early to late adolescence. Int J Eat Disorder. 2006;39(8):729–740. doi: 10.1002/eat.20285. (PubMed PMID: WOS:000242196400015) [DOI] [PubMed] [Google Scholar]
- Morton KL, Wilson AH, Perlmutter LS, Beauchamp MR. Family leadership styles and adolescent dietary and physical activity behaviors: a cross-sectional study. Int J Behav Nutr Phy. 2012;9. doi: Artn 4810.1186/1479-5868-9-48. (PubMed PMID: WOS:000307765000001). [DOI] [PMC free article] [PubMed]
- Neumark-Sztainer D., Story M., Perry C., Casey M.A. Factors influencing food choices of adolescents: findings from focus-group discussions with adolescents. J. Am. Diet. Assoc. 1999;99(8):929–937. doi: 10.1016/S0002-8223(99)00222-9. (PubMed PMID: 10450307) [DOI] [PubMed] [Google Scholar]
- Oellingrath I.M., Svendsen M.V., Hestetun I. Eating patterns and mental health problems in early adolescence–a cross-sectional study of 12–13-year-old Norwegian schoolchildren. Public Health Nutr. 2014;17(11):2554–2562. doi: 10.1017/s1368980013002747. Epub 2013/10/11. (PubMed PMID: 24107233; PubMed Central PMCID: PMCPMC4173131) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overby N.C., Ludemann E., Hoigaard R. Self-reported learning difficulties and dietary intake in Norwegian adolescents. Scand J Public Health. 2013;41(7):754–760. doi: 10.1177/1403494813487449. Epub 2013/05/17. (PubMed PMID: 23676256) [DOI] [PubMed] [Google Scholar]
- Petrie J., Bunn F., Byrne G. Parenting programmes for preventing tobacco, alcohol or drugs misuse in children <18: a systematic review. Health Educ. Res. 2007;22(2):177–191. doi: 10.1093/her/cyl061. (PubMed PMID: WOS:000244962300003) [DOI] [PubMed] [Google Scholar]
- Philips N, Sioen I, Michels N, Sleddens E, De Henauw S. The influence of parenting style on health related behavior of children: findings from the ChiBS study. Int J Behav Nutr Phy. 2014;11. doi: ARTN 9510.1186/s12966-014-0095-y. (PubMed PMID: WOS:000340000600001). [DOI] [PMC free article] [PubMed]
- Pisinger VSC, Bloomfield K, Tolstrup JS. Perceived parental alcohol problems, internalizing problems and impaired parentchild relationships among 71988 young people in Denmark. Addiction. 2016;111(11):1966–74. doi: 10.1111/add.13508. PubMed PMID: WOS:(000386153700015). [DOI] [PubMed]
- Post A., Gilljam H., Rosendahl I., Meurling L., Bremberg S., Galanti M.R. Validity of self reports in a cohort of Swedish adolescent smokers and smokeless tobacco (snus) users. Tob. Control. 2005;14(2):114–117. doi: 10.1136/tc.2004.008789. Epub 2005/03/26. (PubMed PMID: 15791021; PubMed Central PMCID: PMCPMC1747998) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyper E, Harrington D, Manson H. The impact of different types of parental support behaviours on child physical activity, healthy eating, and screen time: a cross-sectional study. BMC Public Health. 2016;16. doi: ARTN 56810.1186/s12889-016-3245-0. (PubMed PMID: WOS:000381980600001). [DOI] [PMC free article] [PubMed]
- Radey M., Randolph K.A. Parenting sources: how do parents differ in their efforts to learn about parenting? Fam. Relat. 2009;58(5):536–548. [Google Scholar]
- Rehm J. The risks associated with alcohol use and alcoholism. Alcohol Res Health. 2011;34(2):135–143. (PubMed PMID: ISI:000298304600001) [PMC free article] [PubMed] [Google Scholar]
- Reynolds EK, MacPherson L, Matusiewicz AK, Schreiber WM, Lejuez CW. Discrepancy between mother and child reports of parental knowledge and the relation to risk behavior engagement. J Clin Child Adolesc. 2011;40(1):67–79. doi: Pii 93223283610.1080/15374416.2011.533406. (PubMed PMID: WOS:000286897300006). [DOI] [PMC free article] [PubMed]
- Rhee K.E., Boutelle K.N., Jelalian E., Barnes R., Dickstein S., Wing R.R. Firm maternal parenting associated with decreased risk of excessive snacking in overweight children. Eat Weight Disord-St. 2015;20(2):195–203. doi: 10.1007/s40519-014-0164-x. (PubMed PMID: WOS:000354214900007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts C., Freeman J., Samdal O., Schnohr C.W., de Looze M.E., Nic Gabhainn S. The health behaviour in school-aged children (HBSC) study: methodological developments and current tensions. Int J Public Health. 2009;54(Suppl. 2):140–150. doi: 10.1007/s00038-009-5405-9. Epub 2009/07/30. (PubMed PMID: 19639259; PubMed Central PMCID: PMCPMC2732766) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roubinov D.S., Boyce W.T. Parenting and SES: relative values or enduring principles? Curr. Opin. Psychol. 2017;15:162–167. doi: 10.1016/j.copsyc.2017.03.001. Epub 2017/05/16. (PubMed PMID: 28503655; PubMed Central PMCID: PMCPMC5423399) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shucksmith J, Glendinning A, Hendry L. Adolescent drinking behaviour and the role of family life: a Scottish perspective. J. Adolesc.. 1997;20(1):85–101. doi: 10.1006/jado.1996.0066. PubMed PMID: (9063777). [DOI] [PubMed]
- Siddiqi K, Shah S, Abbas SM, Vidyasagaran A, Jawad M, Dogar O, et al. Global burden of disease due to smokeless tobacco consumption in adults: analysis of data from 113 countries. BMC Med. 2015;13. doi: Artn 19410.1186/S12916-015-0424-2. (PubMed PMID: WOS:000359450300001). [DOI] [PMC free article] [PubMed]
- Sjoberg A., Hallberg L., Hoglund D., Hulthen L. Meal pattern, food choice, nutrient intake and lifestyle factors in the Goteborg Adolescence Study. Eur. J. Clin. Nutr. 2003;57(12):1569–1578. doi: 10.1038/sj.ejcn.1601726. Epub 2003/12/04. (PubMed PMID: 14647222) [DOI] [PubMed] [Google Scholar]
- Stattin H., Kerr M. Parental monitoring: A reinterpretation. Int. J. Psychol. 2000;35(3–4) doi: 10.1111/1467-8624.00210. (153-. PubMed PMID: WOS:000088388801488) [DOI] [PubMed] [Google Scholar]
- Stea T.H., Torstveit M.K. Association of lifestyle habits and academic achievement in Norwegian adolescents: a cross-sectional study. BMC Public Health. 2014;14:829. doi: 10.1186/1471-2458-14-829. Epub 2014/08/13. (PubMed PMID: 25112948; PubMed Central PMCID: PMCPMC4138388) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torstveit M.K., Johansen B.T., Haugland S.H., Stea T.H. Participation in organized sports is associated with decreased likelihood of unhealthy lifestyle habits in adolescents. Scand. J. Med. Sci. Sports. 2018;28(11):2384–2396. doi: 10.1111/sms.13250. [DOI] [PubMed] [Google Scholar]
- Tourangeau R, Yan T. Sensitive questions in surveys. Psychol. Bull.. 2007;133(5):859–83. doi: 10.1037/0033-2909.133.5.859. PubMed PMID: WOS:(000249065500007). [DOI] [PubMed]
- Van Der Vorst H., Burk W.J., Engels R.C.M.E. The role of parental alcohol-specific communication in early adolescents' alcohol use. Drug Alcohol Depend. 2010;111(3):183–190. doi: 10.1016/j.drugalcdep.2010.03.023. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2016. Adolescents: Health Risks and Solutions.http://www.who.int/mediacentre/factsheets/fs345/en/ [updated May 2016; cited 2016]. Available from: [Google Scholar]
- WHO . World Health Organization, Department of Mental Health and Substance Abuse W; Geneva, Switzerland: 2016. The Health and Social Effects of Nonmedical Cannabis Use. [Google Scholar]