Abstract
Background
Non-suicidal self-injury (NSSI) describes a phenomenon where individuals inflict deliberate pain and tissue damage to their bodies. Self-injurious behaviour is especially prevalent across the autism spectrum, but little is understood about the features and functions of self-injury for autistic individuals without intellectual disability, or about the risk factors that might be valuable for clinical usage in this group.
Methods
One hundred and three autistic adults who responded to an online advertisement were classified as current, historic or non-self-harmers in accordance with responses to the Non-Suicidal Self-Injury Assessment Tool (NSSI-AT). Multinomial regression aimed to predict categorisation of participants in accordance with scores on tests of autistic traits, alexithymia, depression, anxiety, mentalising and sensory sensitivity. Linear regression examined relationships between these predictors and the range, frequency, lifetime occurrence and functional purposes of NSSI. Qualitative analysis explored the therapeutic interventions that participants had found helpful, and what they wished people understood about self-injury.
Results
Current, historic and non-self-harming participants did not differ in age, age at diagnosis, male-to-female ratio, level of employment or education (the majority qualified to at least degree level). The most common function of NSSI was the regulation of low-energy affective states (depression, dissociation), followed by the regulation of high-energy states such as anger and anxiety. Alexithymia significantly predicted the categorisation of participants as current, historic or non-self-harmers, and predicted use of NSSI for regulating high-energy states and communicating distress to others. Depression, anxiety and sensory-sensitivity also differentiated participant groups, and sensory differences also predicted the range of bodily areas targeted, lifetime incidence and frequency of NSSI. Sensory differences, difficulty expressing and identifying emotions also emerged as problematic in the qualitative analysis, where participants expressed the need for compassion, patience, non-judgement and the need to recognise diversity between self-harmers, with some participants perceiving NSSI as a practical, non-problematic coping strategy.
Conclusions
Alexithymia, depression, anxiety and sensory differences may place some autistic individuals at especial risk of self-injury. Investigating the involvement of these variables and their utility for identification and treatment is of high importance, and the voices of participants offer guidance to practitioners confronted with NSSI in their autistic clients.
Electronic supplementary material
The online version of this article (10.1186/s13229-019-0267-3) contains supplementary material, which is available to authorized users.
Keywords: Self-injury, Self-harm, Autism, Alexithymia, Sensory differences, Suicidality, Qualitative
Non-suicidal self-injury (NSSI), also known as self-mutilation or self-harm, describes acts of purposeful, physical, sometimes painful damage to the body without suicidal intent [1]. These must be differentiated from what might be described as self-damaging or risky behaviours which afford some kind of pleasurable or anxiolytic effects despite known health risk (e.g. drinking, smoking, unsafe sex); cutting or burning of the skin are examples of self-injurious behaviour which reflect ‘attempts to modify one’s affective/cognitive or social experience’ [1] (p. 15.5). NSSI tends to begin in adolescence and is a common feature of a number of mental health conditions. It may serve a number of functional roles including emotion regulation (breaking through states of numbness, depression or dissociation or discharging ‘hot’ feelings of anger, frustration, agitation), self-punishment, sensory stimulation, as a means of communicating to or influencing others, or even in avoidance of more severe actions [2]. As NSSI is often associated with later suicide attempts [3–9], clinical and research attention to these behaviours is imperative.
One group at substantially higher risk of suicidality and mental illness are autistic people [10, 11]. Despite this, only recently have attempts been made to understand the occurrence and nature of non-suicidal self-injury in this group.1 NSSI in autism spectrum conditions (ASC) is challenging to define due to the presence of high-frequency self-injurious behaviours, such as head-banging and biting, which are commonly classed as ‘stereotyped’ [12], as elements of repetitive and restricted behaviours and interests (RRBI). These self-injurious behaviours, which have been the focus of autism research in children and adults [12–14], appear to differ in nature from NSSI in the typically developing populations: they occur in front of others without attempts to disguise them, being most commonly associated with intellectual disability and severe receptive and expressive language deficits. Maddox et al. [15] were recently the first to delineate a different type of NSSI, one resembling that seen in neurotypical populations, in autistic people without intellectual disability (all of whom had completed high school, the majority of whom had college qualifications). They found more similarities than differences between their small groups of autistic and non-autistic (typically developing) self-harmers; both began self-injuring in early adolescence and did not differ in the specific NSSI they engaged in. No significant differences were seen in their perceived reasons for NSSI: both groups were equally likely to engage in NSSI in attempts to modulate ‘low pressure’ emotions such as depression or dissociation, to release ‘high pressure’ emotions like agitation and anger, as a form of communication or social influence, to punish themselves or avoid more serious actions and consequences, and to seek simulation. The only suggested differences were that autistic participants were more likely than non-autistic self-harmers to engage in NSSI for the purpose of shocking or hurting others, in imitation of peers, or for the purpose of avoiding a suicide attempt. These authors also compared autistic self-harmers to autistic people who did not engage in NSSI: they found no significant differences in age, depression or emotion dysregulation, but a higher proportion of autistic women than autistic men engaged in NSSI.
This important paper was the first to explore autistic NSSI not within the RRBI domain, and not in individuals with intellectual impairment, but in individuals with IQ within the normal range and with consideration of the roles or functions of NSSI as reported within the typical population and other clinical groups. Crucially, it highlighted the increased prevalence of NSSI in autistic as compared with typically developing populations, with 50% of the autistic sample (n = 42) having engaged in at least one act of NSSI—an inflated prevalence that motivates further study of NSSI in a larger sample of these individuals within the autism spectrum.
In their analysis, Maddox et al. considered the association of depression and emotion dysregulation with NSSI by comparing these factors between autistic self-harmers and autistic non-self-harmers. They found no significant differences between groups and so suggest that these factors are not associated with increased risk of self-injury. We note, however, that the small sample did not allow the authors to differentiate between current and historic self-harmers within their NSSI group, instead categorising participants dichotomously based on lifetime incidence of NSSI. This dichotomous categorisation may have hidden group differences if, for example, current self-harmers suffer from greater depression and emotional dysregulation than those whose NSSI is in the past and who judge themselves unlikely to engage in these behaviours in future, and thus leaves open the question as to whether depression and emotional dysregulation are indeed risk factors for current engagement in NSSI.
In our consideration of potential factors of clinical relevance, the functions that NSSI serves in autistic (and typically developing) people afford vital clues for a theory-led analysis. The use of NSSI for emotion regulation, for example, does implicate current depression as a risk factor in participants who engage in NSSI to manage depressive or dissociative states [2]. NSSI is also employed for the management of high energy states such as anger, anxiety, frustration and agitation, where it seems to act as a kind of pressure valve. One common associate of NSSI that may be of relevance here is alexithymia, a difficulty understanding and identifying one’s own emotions and those of other people. Alexithymia is common in people who self-injure [16]: these individuals not only have difficulty expressing their emotions verbally [17], a key aspect of alexithymia, but tend to be less aware of their emotional states [18, 19]. Borrill et al. [20] identified alexithymia as a strong predictor of self-injury in a student sample, and noted that it was especially associated with repetitive NSSI. Others have identified alexithymia as an important mediator which increases the risk of NSSI in people who have experienced different types of life adversity, such as childhood abuse and bullying [16, 21–23]. In clinical groups, better ability to label and differentiate between negative emotions is associated with decreased likelihood of NSSI [24].
Another variable of potential relevance may relate to the function of NSSI as a means of communicating distress or anger to others [2]. Whilst the inability to verbalise one’s emotions is again of high relevance here, the use of self-injury as a means of communication when verbal means fail may reflect the interpersonal difficulties at the core of ASC. These communication difficulties have been linked to difficulties with ‘theory of mind’, also known as mentalising [25, 26], which is very important for effective communication. Whilst mentalising impairments or differences have not been previously linked to self-injury as such, they are a feature of borderline personality disorder [27–30], which is itself strongly linked with self-injury [31–33]. In this vein, some authors have hypothesised that mentalising deficits might lead to more intense negative feelings and social isolation, thus leading to manipulation and self-harm to create connection with others [34, 35]. Accordingly, interventions aiming to strengthen mentalising ability have been seen to decrease self-injury alongside borderline symptomatology [36, 37], with further trials ongoing [38]. This motivates investigation of mentalising impairments as predictive of self-injury in autism. The presence of mentalising impairments in autistic individuals, and the relationship between mentalising abilities and autistic traits [39–41], suggests that autistic symptom severity (in so far as it predicts mentalising impairment) could also be a predictor of NSSI. Indeed, the fact that autistic symptom severity predicts the severity and frequency of the ‘stereotyped’ forms of NSSI seen in adults with learning disabilities [42] motivates investigation of autistic symptom severity as a predictor of the form of NSSI described by Maddox et al.
In contrast to its role in communication, another potential variable of interest is highlighted by use of NSSI to generate sensory stimulation [2], with non-autistic self-harmers reporting a ‘rush’ or a ‘high’, a feeling of excitement, after engaging in NSSI [43, 44]. Therapeutic interventions may reroute this drive by providing alternative strategies for stimulation [45]. Sensory stimulation as a function of NSSI is highly relevant for autistic people, as different sensory-perceptual experience of the world is very common in autism (see [46, 47]). Some individuals show a pattern of low registration or under-responsivity (a weak response to stimulation due to a high neurological threshold [47]); some seek sensation for stimulation; others show sensory sensitivity or over-responsivity, a low neurological threshold leading to exaggerated and uncomfortable sensory experiences [47]; heterogeneous sensory symptoms are modulated by age, IQ and severity of autism, and individuals may show more than one pattern in different sensory modalities [48]. Importantly, sensory differences in autism are associated with ritualistic and repetitive behaviours including self-injury [49], and are even the strongest predictors of self-injury [13]. However, these studies have focused on self-injury of the type which Maddox et al. note is more characteristic of individuals with intellectual disability and language problems; consequently, investigation of whether sensory differences are also important for self-injury in individuals without intellectual disability is timely.
The aims of the present report are threefold: whilst aiming to validate Maddox et al.’s descriptive analysis of NSSI within a larger autistic population without intellectual disability, we further aimed to qualitatively analyse participants’ experiences of NSSI, and to explore predictive factors for NSSI that might thus be of clinical relevance. In a mixed methods approach, a descriptive report of the characteristics of autistic self-harmers and their self-injurious behaviour was bolstered by statistical regression in order to examine alexithymia, mentalising impairments, autistic traits and sensory differences as variables that might predict (a) the presence of self-injury; (b) the severity, range and frequency of these behaviours; and (c) the use of self-injury to meet certain functional purposes. To explore participants’ individual experience of NSSI, we employed the qualitative method of thematic analysis to examine participants’ responses to two open questions regarding their experience of therapeutic help and what they would like others to know about self-injury.
Methods
Participants
Autistic participants were recruited from support groups local to the primary researcher (Dorset) and via the Cambridge Autism Research Database (CARD) at the Autism Research Centre, Cambridge, UK. Details of the study were sent to 2264 national and international volunteers with a formal diagnosis of autism,2 and 103 participants took part in the study. The group (n = 70 females and n = 33 males) had an average age of 43 years old (SD = 13.6) and was diagnosed, on average, at 34.2 years old (SD = 16.2). The majority of them (66%) were British, but other nationalities included American, Australian, Hungarian, Finnish, Dutch, German, Swedish, Irish, Scottish, Italian, Canadian, New Zealandic, Czech and Venezualan. Although IQ was not measured, all participants had attended school to GCSE level (or equivalent) and the majority (64%) had degrees, such that it was possible to infer that participants did not have an intellectual impairment (IQ < 70). Just over half of the participants (52%) were employed. Forty-nine percent were taking some kind of psychotropic medication at the time of the study; 75% had been diagnosed with at least one comorbid psychiatric condition, the most common being depression and/or anxiety. Twenty-two participants had been diagnosed with a specific learning difficulty such as dyslexia or dyspraxia; 12 had been diagnosed with ADHD.
Participants were classified as current self-harmers (n = 49), historic self-harmers (n = 27) and non-self-harmers (n = 27) (see ‘Methods’ section): the demographic details of each group are given in the ‘Results’ section. Individuals (4) who responded to the advertisement but whose NSSI occurred in the context of suicide attempts were not included in this analysis.
Materials
Variables of interest in relation to NSSI included alexithymia, autistic traits, sensory processing differences, mentalising abilities, depression and anxiety.
Alexithymia was measured with the Toronto Alexithymia Scale (TAS-20 [50]), a self-report measure which asks participants to rate their agreement with 20 items reflecting their recognition and understanding of their own emotional states, their ability to verbalise them to others and their tendency for externally orientated thinking. The authors report good internal consistency and test-retest reliability (alexithymia is understood as a stable construct), and the instrument has been translated and used across a substantial number of countries and cultures [51]. Whilst these authors found the three distinct factors named above to be largely reliable across cultures, other findings contradict this, especially in patient groups ([52, 53], though Loas et al. showed that this may depend on the patient group [54]). We used a single overall score from the TAS-20 to reflect degree of alexithymia, which encompasses all three of the above in its clinical presentation.
The Autism-Spectrum Quotient (AQ) [55] is a quantitative measure of autistic traits that can be used in the general population as well as in clinical groups. A recent systematic review revealed the extent of its usage and confirmed normative mean scores of 16.9 for typically developing and 35 for autistic people [56]. The test has good internal consistency and test-retest reliability and has been translated into many languages [57, 58]. Whilst it consists of five subscales (social skills, attention switching, attention to detail, communication and imagination), we used a single score to reflect autistic traits in each participant.
The Adolescent-Adult Sensory Profile [59] is based on Dunn’s [47] model of sensory processing. It measures scores in four domains: low registration (weak response to stimulation due to high neurological threshold), sensation seeking (a similar weak response to stimulation coupled with a drive to counter this), sensory sensitivity (a high response to sensation due to a low neurological threshold, manifest in distractibility and discomfort), and sensory avoidant (similar low threshold coupled with behaviours limiting exposure to stimuli). The test has good construct validity in terms of skin conductivity and good internal consistency [59], and is used clinically.
The ‘Reading the Mind in the Eyes’ test (RMET) [41] is a test of mentalising (‘theory of mind’), the ability to attribute mental states (beliefs, desires) and emotions to other agents. Participants are shown 36 pairs of eyes and must identify the mental state (e.g. playful, frightened, regretful) in each depiction. The test has good internal consistency and test-retest reliability [60, 61].
Current (i.e. state) depression and anxiety were measured by the Beck Depression Inventory (BDI) [62] and the Beck Anxiety Inventory (BAI) [63] respectively. Both tests are used clinically and possess strong psychometric validity and reliability [64–66]. The BDI reflects depressive symptoms over the last fortnight; the BAI reflects symptoms of anxiety over the last month.
The Non-Suicidal Self-Injury Assessment Tool (NSSI-AT): coding and categorisation of participants
Developed by Whitlock et al. [2], this comprehensive instrument documents the nature and bodily location of any self-injurious behaviours; their functional utility; their recency, frequency and likelihood of reoccurrence; the age of onset of self-injury; the severity of injuries (based on whether these did or should have received medical attention); the social and habitual routines or context around self-injurious behaviours (if, for example, individuals always make sure they are alone); the degree to which participants are habituated to the occurrence of self-injurious behaviour; and whether individuals have sought therapy, their experiences in therapy and their experiences of telling others about their self-injury.
The NSSI-AT lends itself to in-depth qualitative exploration but several aspects of the scale were of especial interest in this analysis, and so we quantified them for comparison between participants. Whilst the scale allowed us to differentiate between participants who had and those who had never engaged in NSSI, we further categorised our self-harming group as follows: current self-harmers were those who had last engaged in NSSI between 1 week and 1 year ago, and who rated themselves as ‘very’ (4 points) or ‘somewhat likely’ (3 points) ‘unsure’ (2) or left the question blank as to whether they would harm themselves again; historic self-harmers were those who had last engaged in NSSI more than 1 year ago and classed themselves as ‘unsure’ (2 points), ‘somewhat’ (1 point) or ‘very unlikely’ (0 points) or left the question blank as to whether they were likely to harm themselves again. This categorisation system allowed us to easily categorise all but two participants who had engaged in NSSI more than 1 year ago but suggested they were ‘very’ or ‘somewhat likely’ to do it again; since NSSI was still a likely option in their behavioural repertoire, these individuals were classed as a current self-harmers.
Of descriptive interest were many of the variables explored in Maddox et al.: for example, the commonest types and bodily locations of NSSI, the typical age of onset of NSSI and the initial motivation for starting, the functional role of NSSI, the extent to which self-injury troubled participants and the ways in which it did so, and participants overall positive and negative thoughts about their experiences around NSSI.
Particular attention was paid to the functional role of self-injurious behaviours. Self-injurious behaviours fulfilled one or more of five roles, example items of each which can be seen in Table 1:
Table 1.
Functional roles of NSSI
| Functional role of NSSI | Example answers to the question ‘I hurt myself …’ |
|---|---|
| Affective imbalance-low pressure (4 items) | ‘… to feel something.’ ‘… to change my emotional pain into something physical.’ |
| Affective imbalance-high pressure (3 items) | ‘… to relieve stress or pressure.’ ‘… to deal with frustration.’ |
| Social communication and expression (3 items) | ‘… in hopes that someone would notice that something is wrong or that so others will pay attention to me.’ ‘… to shock or hurt someone.’ |
| Self-retribution and deterrence (4 items) | ‘… as a self-punishment or to atone for sins.’ ‘… so I do not hurt myself in other ways.’ |
| Sensation seeking (4 items) | ‘… because I get the urge and cannot stop it.’ ‘… to get a rush or surge of energy.’ |
Example items for the five functional roles of self-injurious behaviour outlined in the Non-Suicidal Self-Injury Assessment Tool (NSSI-AT)
As in Maddox et al. [15], participants who indicated that they engaged in NSSI only as a means of practicing or attempting suicide were excluded from analysis, though participants who included this as one reason alongside having engaged in NSSI for other reasons were included. As in Whitlock et al. and Maddox et al., responses of ‘strongly’ and ‘somewhat agree’ were collapsed to indicate affirmation of that functional role, whilst responses of ‘strongly’ or ‘somewhat disagree’ were collapsed to indicate denial of that role. We allocated each affirmation within a category a score of 1, and took an average of the number of statements endorsed in each category across participants for a descriptive analysis, but also included scores in each of the five categories as outcome measures in a regression to examine their relationship with the variables reported above.
Indeed, included in our analysis as continuous outcome variables were not only scores in each of these five functional categories, but also
The range of NSSI behaviours (quantified by giving a score of 1 for each type of NSSI engaged in, such that higher scores indicated that participants engaged in a wider range of NSSI than individuals who consistently used one or two methods)
The number of bodily locations targeted (quantified by giving each location a score of 1, with higher scores indicating that participants targeted more areas of their body for NSSI)
The lifetime incidence of NSSI (quantified by giving a score of 1 for up to five occurrences, a score of 2 for 6–20 incidents, a score of 3 for 21–50 incidents and a score of 4 for more than 50)
The frequency of NSSI in the participant’s most active period of engaging with this behaviour (quantified as follows: a score of 1 if participants engaged in NSSI once in a period of 1, 2 or more years, a score of 2 if they engaged in NSSI once every few months, a score of 3 if they engaged between once a week and 1–3 times a month and a score of 4 if they engaged in NSSI every day or 2–3 times per week).
Analysis
Following our descriptive report of the type and bodily location of NSSI, initial motivation, age of onset, functional reasons, extent and type of repercussions caused by NSSI and lasting feelings about NSSI, we conducted a number of regression analyses with categorical or continuous outcome measures. Firstly, multinomial regression was used to examine which variables could, individually, correctly categorise participants as current, historic or non-self-harmers: these variables included autistic traits (AQ), depression (BDI) and anxiety (BAI) scores, mentalising score, alexithymia score and sensory profile as reflected in scores for low registration, sensation seeking, sensory sensitivity and sensory avoidance. (We included measures of anxiety and depression in this analysis to specifically test the assertion that autistic self-harmers and non-self-harmers do not differ significantly in depression [15], but results must be interpreted with caution as these measures reflect current psychological health within the last fortnight and month respectively. As such, BDI and BAI scores were not used in the remainder of the analysis below). Regression models tested whether current self-harmers could be differentiated from non-self-harmers, and whether historic self-harmers could be differentiated from non-self-harmers. We therefore included, for each variable that was seen to be a significant predictor of group categorisation, a planned t test comparing scores between current and historic self-harmers.
Secondly, stepwise linear regression including only current and historic self-harmers was used to examine the predictive power of autistic traits (AQ), mentalising score, alexithymia score, sensory low registration, sensation seeking, sensory sensitivity and sensory avoidance on four continuous measures: the range of NSSI behaviours, the range of bodily locations targeted, the lifetime incidence of NSSI and the frequency of NSSI in the participant’s most active period of engaging with the behaviour.
In consideration of the five functional roles of NSSI as outcome measures in regression, we took a theory-driven approach in order to reduce the number of statistical tests conducted. Alexithymia was hypothesised to be associated with participants’ use of NSSI to address affective imbalances of both the high pressure and low pressure type. Use of NSSI as a means of expressing and communicating with others was hypothesised to be predicted not only by alexithymia (which relates to one’s ability to verbally communicate emotional states) but by ability to understand other people (mentalising): deficits would theoretically impair communication with others. Sensation seeking as a reason for NSSI was hypothesised to be predicted by the sensation seeking and low registration scales of the Sensory Profile. We did not have hypotheses regarding the prediction of NSSI for the purpose of self-punishment and deterrence, so entered autistic traits, mentalising score, alexithymia score and sensory profile in low registration, sensation seeking, sensory sensitivity and sensory avoidance into a stepwise linear regression.
We conducted a thematic analysis of two open items from the Non-Suicidal Self-Injury Assessment Tool (NSSI-AT). As we took the two questions directly from the questionnaire and these were loaded with prior assumptions (e.g. that something had helped reduce or prevent self-injury), our analysis could not be described as fully inductive in nature, despite our attempts to approach it without expectation as to what participants would answer to the two items. The analysis was conducted independently by two of the researchers, RLM and NJG, who pursued a thematic analysis in the style of Braun and Clarke [67]. In this conceptualization, the themes in the data do not exist there objectively but ‘reside in our heads from our thinking about our data and creating links as we understand them’ ([68], pp. 205–6). RLM’s familiarity with the quantitative data of the present study, alongside previous literature on self-injury in ASC, was expected to undoubtedly interact and influence her interpretation of the qualitative data. NJG, in contrast, performed her qualitative analysis blind to the quantitative data generated by the same participants and without familiarity with the literature on self-injury in autistic and typically developing populations. The two authors independently followed the pipeline set forward by Braun and Clarke: first, extensively familiarising themselves with the dataset as a whole, then generating initial codes for the data, with some quotations from participants fitting into multiple categories; thirdly, identifying latent themes across the codes. At this point, the authors came together to review the themes that they had identified independently. In multiple meetings over the course of several weeks, they discussed and revised their initial mind-maps and thematic tables, until they had unanimously defined and named the final themes that appear in this analysis.
Results
Group demographic information
The demographic details of each group are given in Table 2:
Table 2.
Demographic details for each group
| Percentage female | Age (years) | Age at diagnosis (years) | Percentage employed | Percentage qualified to at least degree level | Percentage with comorbid psychiatric diagnoses | Percentage taking medication | |
|---|---|---|---|---|---|---|---|
| Current self-harmers (n = 49) | 75.5% (n = 37) | 41.2 (3.4) | 33.4 (13.8) | 53% (n = 26) | 66% (n = 21) | 85.7% (n = 42) | 65.3% (n = 32) |
| Historic self-harmers (n = 27) | 63% (n = 17) | 43.5 (15.8) | 36.1 (17.1) | 37% (n = 10) | 63% (n = 17) | 81.5% (n = 22) | 37.1% (n = 10) |
| Non-self-harmers (n = 27) | 59.2% (n = 16) | 43.0 (13.6) | 34.2 (16.2) | 66.6% (n = 18) | 70.4% (n = 19) | 48.1% (n = 13) | 33.3% (n = 9) |
Average age and age at diagnosis for each group (standard deviations in brackets). Also included are percentages of female participants; participants who were employed, qualified to at least degree level, suffering from a comorbid psychiatric diagnosis, and taking medication
Participant groups did not differ with respect to current age (F [2, 102] = 1.077, p = .345) or age at diagnosis (F [1, 102] = 1.877, p = .158). Neither was the distribution of female participants across groups significantly different (χ2(2) = 1.906, p = .086) nor was the distribution of participants who were employed (χ2(2) = 4.341, p = .114), or those who had a degree (χ2(2) = .350, p = .840). However, the distribution of participants who were taking medication (χ2(2) = 7.720, p = .021) and the distribution of participants with additional psychiatric comorbidities (χ2(2) = 12.814, p = .002) were significantly different: the participants in both self-harming groups were more likely to be experiencing psychiatric comorbidities, and the current self-harming group were more likely to be taking medication at the time of the study. Group scores in each of the variables of interest are displayed in Table 3.
Table 3.
Group scores in experimental variables
| Depression (BDI) | Anxiety (BAI) | Alexithymia (TAS-20) | Autism spectrum quotient (AQ) | Number of correct answers: RMET | Sensory low registration | Sensory seeking | Sensory sensitivity | Sensory avoidant | |
|---|---|---|---|---|---|---|---|---|---|
| Current self-harmers (n = 49) | 25.6 (13) | 24.6 (11) | 65.9 (11) | 39.1 (9) | 23.6 (8) | 43.1 (10) | 35.9 (9) | 52.9 (10) | 53.0 (11) |
| Historic self-harmers (n = 27) | 22.9 (15) | 22.3 (14) | 60.4 (12) | 37.8 (8) | 24 (6) | 39.9 (10) | 37.4 (8) | 47.6 (13) | 47.2 (12) |
| Non self-harmers (n = 27) | 14.6 (10) | 13.1 (9) | 56 (15) | 35.6 (10) | 23.3 (9) | 38.8 (14) | 38.7 (12) | 44.1 (14) | 46.2 (17) |
Average scores for each group on each variable of interest (standard deviation in brackets)
BDI and BAI scores, on average, fell in the range of mild depression (10–19) and mild anxiety (8–15) for non-self-harmers and moderate to severe depression (20–30) and moderate anxiety (16–25) for current and historic self-harmers [64, 69]. Sixty-three of 103 participants (61%) scored above the 61 cut-off point for clinical levels of alexithymia [50]: the lowest score was 33, and 9 participants fell just below the cut-off by scoring 59 or 60.
On the AQ, all but 6 participants scored ≥ 26, a cut-off which correctly categorises 83% of autistic individuals [70]; on average, autistic individuals tend to receive scores of approximately 35 [56], consistent with our groups. Likewise, scores in the RMET are similar to those seen in other publications with autistic participants [41, 71].
Group averages in the subscales of the Sensory Profile suggested that participants scored above test norms (based on nearly 500 typically developing individuals) in low registration, sensory sensitivity and sensory avoiding. All groups scored below test norms for sensation seeking.
Descriptive analysis of self-injury
Of the 76 current and historic self-harmers, 60 could recall the onset of self-injury at an average age of 15.1 years (SD = 10.8). Seven others also estimated that they began self-harming in childhood or early adolescence. The reason they first engaged in self-injury, the range and bodily location of NSSI are summarised in Table 4.
Table 4.
Range and bodily location of NSSI in autistic individuals
| Type of NSSI | Percentage (%) of participants |
|---|---|
| Severely scratched or pinched with fingernails or other objects to the point that bleeding occurs or marks remain on the skin | 72.4% (n = 55) |
| Cut wrists, arms, legs, torso or other areas of the body | 50% (n = 38) |
| Banged or punched objects to the point of bruising or bleeding | 44.6% (n = 33) |
| Punched or banged yourself to the point of bruising or bleeding | 44.6% (n = 33) |
| Bitten yourself to the point that bleeding occurs or marks remain on the skin | 41.2% (n = 31) |
| Intentionally prevented wounds from healing | 38.2% (n = 29) |
| Ripped or torn skin | 34.2% (n = 25) |
| Burned wrists, hands, arms, legs, torso or other areas of the body | 30.1% (n = 22) |
| Rubbed glass into skin or stuck sharp objects such as needles, pins and staples into or underneath the skin (not including tattooing, body piercing or needles used for medication use) | 27.6% (n = 21) |
| Carved words or symbols into the skin | 20.5% (n = 15) |
| Engaged in fighting or other aggressive activities with the intention of getting hurt | 11% (n = 8) |
| Tried to break your own bones | 8.2% (n = 6) |
| Ingested a caustic substance(s) or sharp object(s) (bleach, other cleaning substances, pins, etc.) | 6.8% (n = 5) |
| Banging head against walls, hard surfaces | 6.8% (n = 5) |
| Broke your own bones | 2.7% (n = 2) |
| Dripped acid onto skin | 2.7% (n = 2) |
| Pulled out hair, eyelashes or eyebrows (with the intention of hurting yourself) | 1.7% (n = 1) |
| Other (avoided taking medication or seeking healthcare as a form of self-harm; tried to choke/strangle myself; took small overdoses of paracetamol or paracetamol; poured boiling water over hands; provoking an animal to bite; trying to get hit by traffic; tried to set myself alight; dropped heavy objects onto myself; tried dropping off heights; masturbated with metal objects that caused me to bleed) | 24.7% (n = 18) |
| Bodily site of NSSI | |
| Arms | 61.8% (n = 47) |
| Hands | 58.1% (n = 43) |
| Head | 47.4% (n = 36) |
| Wrists | 42.5% (n = 31) |
| Face | 35.1% (n = 26) |
| Fingers | 31.6% (n = 24) |
| Stomach or chest | 31.5% (n = 23) |
| Thighs | 28.8% (n = 21) |
| Calves or ankles | 14.5% (n = 11) |
| Lips or tongue | 13.7% (n = 10) |
| Shoulders or neck | 11.8% (n = 9) |
| Breasts | 9.2% (n = 7) |
| Genitals or rectum | 6.6% (n = 5) |
| Feet | 2.7% (n = 2) |
| Back | 2.7% (n = 2) |
| Eyes | 1.4% (n = 1) |
| Initial motivation for NSSI | |
| I was angry with myself. | 38.2% (n = 29) |
| I accidentally discovered it—I had never seen or heard of it before. | 38.2% (n = 29) |
| I was upset and decided to try it | 30.3% (n = 23) |
| I was angry with someone else. | 15.1% (n = 11) |
| It felt good. | 15.1% (n = 11) |
| I wanted someone to notice me and/or my injuries. | 11% (n = 8) |
| I cannot remember. | 8.2% (n = 6) |
| I wanted to shock or hurt someone. | 27.7% (n = 2) |
| It seemed to work for other people I know. | 27.7% (n = 2) |
| I did it because I had friends who did it and I wanted to fit in. | 27.7% (n = 2) |
| I saw it on a movie/television or read about it in a book and decided to try it. | 27.7% (n = 2) |
| I read about it on the internet and decided to try it. | 1.4% (n = 1) |
| It was part of a dare. | 1.4% (n = 1) |
| Other (‘Whilst not remembering the exact first time, I know it was initially an attempt to FEEL my own self-loathing—to be able to grasp and feel the feeling’; ‘It reduced my stress’; ‘I was having what I now know was a meltdown and did it in desperation to “do” something’; ‘I needed to do so something to ease the pain I felt inside’; ‘I hated myself’; ‘It just happened. It was like a compulsion and I could not control myself at all’; ‘I copied my dad’; ‘I wanted to be humiliated, “told you so”’; ‘I was so stressed’; ‘I just wanted out of the situation I was in’; ‘I was frustrated by other people’s talking and noise and rule-breaking and needed something to distract me’; ‘I was depressed’; ‘Boredom’; ‘I was so frustrated, cornered, it felt like the last resort’; ‘I was trying to understand what had happened to me at a doctor’s surgery’; ‘full of self-hatred and confusion’.) | 21.1% (n = 16) |
Participants report the their methods of self-injury, the bodily areas most commonly targeted and initial motivations for starting
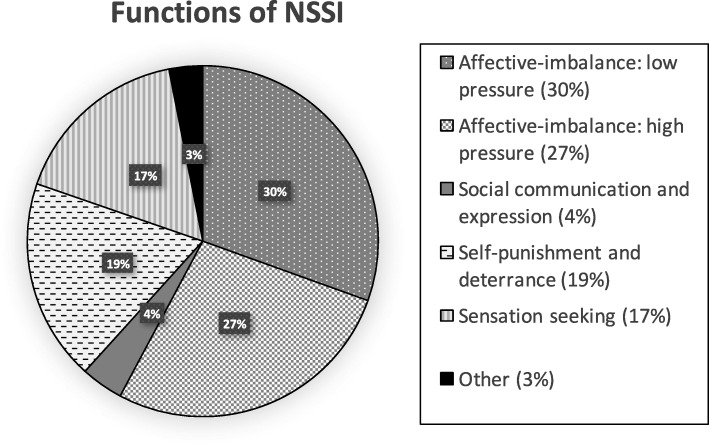
To analyse the functional role that NSSI plays or played, we took an average of the number of statements endorsed from each of the five categories. The average of each category is displayed in Fig. 1 as a percentage. On average, current and historic self-harming participants endorsed 2.6 statements from the affective-imbalance low pressure category (which has 4 statements overall), making this the most common reason for NSSI. This was followed by affective-imbalance high pressure (2.3 statements on average, out of 3 possible statements), self-punishment and deterrence (1.6 statements on average, out of 4 possible statements), sensation seeking (1.4 statements on average, out of 4 possible statements) and social communication and expression (.33 statements on average, out of 3 possible statements). A small number of additional ‘other’ reasons were offered. Some of these were rewording of items from the other categories (‘frustration’, for example, could be recoded in the affective-imbalance high pressure category; ‘punishment for incompetence’ could be recoded in the self-punishment and deterrence category). Other motivations for NSSI that were less transparent to categorise or indeed separate included ‘to stop sensory input from overwhelming me’; ‘To look ugly, deformed’; ‘I wanted to disappear from an unbearable situation’; ‘To appease voices’; ‘Because it helps me deal with my eating disorder’; ‘Over a relationship’; ‘Distraction’; ‘So I don’t hurt someone else or break something’; ‘Loneliness’; ‘To stop being lost to get out of lost the empty black where I don’t know what to do. It helps me to focus and get out of the black, to have focus to move on’.
Fig. 1.
Functions of NSSI. This chart depicts the average number of statements endorsed in each category as a percentage
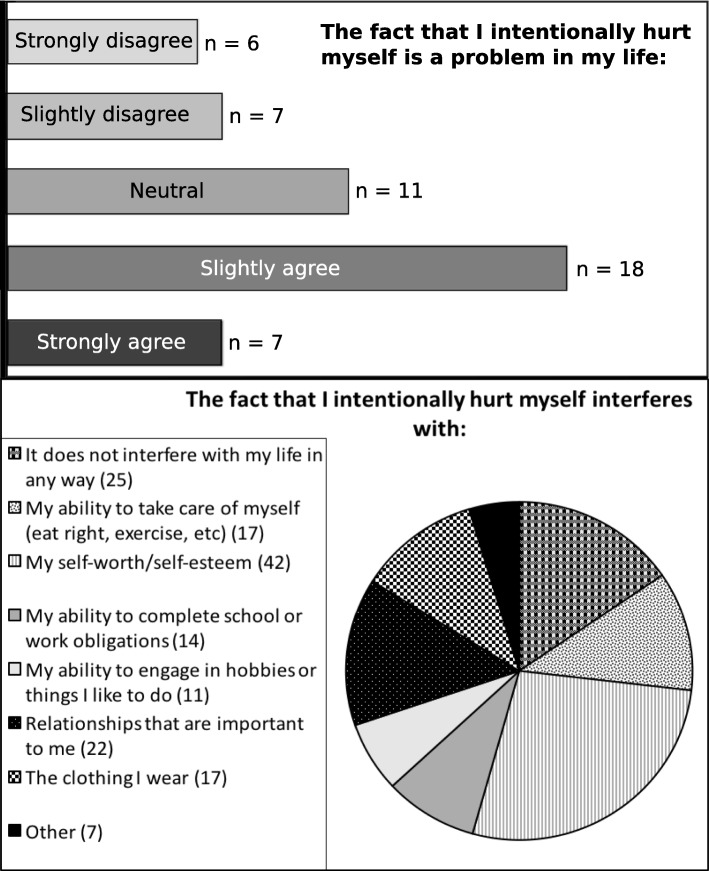
Participant responses to the query as to whether self-injury was a problem in their life, and how so, are displayed in Fig. 2.
Fig. 2.
Negative repercussions of NSSI. The chart depicts participant responses to questions on the NSSI-AT as to a whether self-injury is a problem in their life and b whether self-harm was problematic in relation to seven repercussions specified by the NSSI-AT. Several participants offered additional problems caused by NSSI (‘Other’) which included: ‘It causes anxiety in public places as I don’t want other people to watch me while I am doing it’; ‘Being a mother and role model for my son’; ‘Hiding when it hurts how I move or if touched’; ‘I’m ugly. No man would want me and people won’t want to be my friends as they’d be ashamed to be seen with me’; ‘I don’t know what the long-term effects might be and that sometimes worries me’; ‘Constant trips to A&E’ (hospital); ‘Ashamed of my appearance’
Lasting feelings about NSSI, a summary question at the end of the NSSI-AT, corroborated participants’ concern over the physical marks of NSSI. Twenty-eight participants endorsed a statement that their scars are a constant reminder of a bad time in their life; 19 that their scars are a source of embarrassment. Ten people took a more positive view of their scars as their ‘battle wounds’. Seventeen participants reported that they found it hard to think about or talk about their experience with NSSI, but surprisingly, the most commonly endorsed feeling (30 participants) was that their NSSI had not impacted on their life much at all. Nineteen participants thought that they had learnt something from their experience with NSSI and had grown emotionally/mentally; 5 that they could now help others who self-injure; 2 reported that NSSI had caused anxiety in their relationships, but 7 reported that talking about their experience with NSSI had brought them closer to people they care about.
Statistical analysis: predictors of NSSI
Variables which predicted the categorisation of participants as current, historic or non-self-harmers were alexithymia (χ2(2) = 10.677, p = .005), BDI scores (χ2(2) = 12.313, p = .002), BAI scores (χ2(2) = 19.299, p < .001) and sensory sensitivity (χ2(2) = 9.953, p = .007). Alexithymia explained 11% (Nagelkerke R2) of the variance in categorisation, with the model able to differentiate significantly between current and non-self-harmers in accordance with their alexithymia scores (b = .062, Exp [b] = 1.064, p = .002) but not between historic and non-self-harmers (p = .232); planned comparison showed that the difference between current and historic self-harmers was only marginal (t [74] = 1.968, p = .053). Scores on the depression inventory explained 13% of the variance (Nagelkerke R2), with the model able to correctly differentiate current from non-self-harmers (b = .068, Exp [b] = 1.070, p = .002) and historic from non-self-harmers (b = .053, Exp [b] = 1.055, p = .02), and planned comparison showing no significant difference between current and historic self-harmers. Scores on the anxiety inventory explained 19% of the variance (Nagelkerke R2), with the model correctly differentiating between current and historic self-harmers (b = .107, Exp [b] = 1.113, p < .001) and between historic and non-self-harmers (b = .091, Exp [b] = 1.095, p = .003), and planned comparisons showing no significant differences between current and historic self-harmers. Sensory sensitivity explained 10% of the variance (Nagelkerke R2), but the model only significantly differentiated between current and non-self-harmers (b = .063, Exp [b] = 1.065, p = .004); the planned comparison between current and historic self-harmers (t [74] = 2.005, p = .049) was only marginally significant.
This approach to regression, of course, fails to address the issue of multicollinearity, given that many of these variables would theoretically be expected to correlate with one another. As such, we added all variables (AQ, BDI, BAI, alexithymia, mentalising score and the four sensory variables) into a binomial regression. Together, they significantly predicted categorisation of participants as current, historic or non-self-harmers (χ2(2) = 34.73, p = .022), and explained 38% of the variance. However, given the correlations (i.e. shared variance) between the variables (Additional file 1: Table S1), no single variable emerged as a significant predictor in the model; greater power would be required to tease out the contributions of each variable.
Stepwise linear regression was conducted to look at several continuous outcome measures, namely the range of self-injurious behaviours, the range of bodily locations targeted, the lifetime incidence of NSSI and the frequency of NSSI in the participant’s most active period of self-injury. None of the variables significantly predicted the range of self-injurious behaviours. The only significant predictor to remain in a model of the range of bodily areas targeted (F [1, 62] = 5.157, p = .027) was sensory avoidance (b [standardised coefficient] = .279, t = 2.271, p = .027). Likewise, the only predictor to remain in a model of lifetime incidence (F [1, 62] = 7.715, p = .007) was sensory avoidance (b = .335, t = 2778, p = .007). The only predictor to remain in a model of frequency of behaviours in most active period (F [1, 62] = 4.264, p = .043) was sensory low registration (b = .256, t = 2.065, p = .043).
As regards engagement in NSSI for the purpose of regulating low-energy states such as depression or dissociation, our hypothesis was not supported: alexithymia was not a significant predictor of participants’ endorsement of statements about NSSI related to regulating these low-energy states. In contrast, the hypothesis that alexithymia would predict use of NSSI to regulate high-energy states was supported (F [1, 74] = 5.065, p = .027), with participants high in alexithymia more likely to endorse statements about engaging in NSSI for the purpose of regulating high-energy states. In a stepwise regression predicting use of NSSI for communicative purposes (F [1, 74] = 5.065, p = .027), alexithymia (b = .255, t = 2.251, p = .027) was a significant predictor but mentalising performance was not. Neither sensory low registration nor sensory seeking predicted NSSI for the purpose of sensory seeking. None of the variables predicted NSSI for the purpose of self-punishment and deterrence.
Qualitative analysis: autistic voices on self-injury
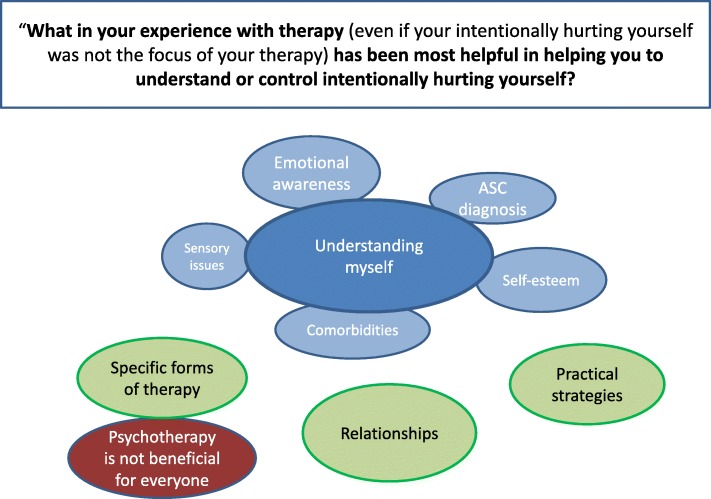
We chose to analyse two qualitative items from the NSSI-AT. The first item was: ‘What in your experience with therapy (even if your intentionally hurting yourself was not the focus of your therapy) has been most helpful in helping you to understand or control intentionally hurting yourself?’. A thematic map for this question is depicted in Fig. 3:
Fig. 3.
First thematic map. Figure depicts themes and subthemes around experiences with therapy
Sixty-three of our 76 participants responded to this question, and 4 core categories were identified within the data. The most overarching of these was understanding myself, which encompassed the themes of developing emotional awareness, understanding the roles of self-esteem and sensory issues, getting and understanding an ASC diagnosis as well as acknowledging the role of comorbidities. In addition, three further themes were found: Specific forms of therapy which helped, therapeutic and personal relationships were important and the practical strategies that therapy focussed on developing and which helped manage or reduce NSSI. Finally, a contrasting theme was found, that psychotherapy was not beneficial for everyone. Please see Additional file 1: Table S2 for a thematic table of responses.
Understanding myself
The way that therapy had helped participants to better understand themselves and their reasons for NSSI was central to the data. This understanding described in this theme took the form of five sub-themes.
Emotional awareness: Participants spoke most widely about how emotional experiences were at the root of their self-injury and that understanding what these were, what caused them and then learning strategies to manage those emotions, often helped reduce their NSSI. As this was such an important but diverse subtheme, we sub-divided it into five aspects of emotional awareness.
-
i.
Understanding the cause of emotions (e.g. ‘… starting to understand my emotions and what is “upsetting”’—P75).
-
ii.
Identifying emotions: some participants highlighted a difficulty in identifying emotions which could exacerbate NSSI (‘[Understanding] that I hurt myself out of [...] fear of showing confusing emotions’—P74) and alleviate NSSI when assisted (‘Learning to name my thoughts and feelings [...helped with my NSSI]’—P11).
-
iii.
Expressing emotions: participants mentioned how learning to articulate their feelings to others was something that had helped with NSSI (‘Reading and speaking to other people openly’—P72). The process of articulating emotions also helped one participant to understand their own feelings more fully (‘Verbalising some feelings so that I can understand them better’—P17).
-
iv.
Emotions in control: there was a sense from several participants that their emotions controlled them or were something which needed to be controlled. Increasing emotional awareness and learning strategies to manage emotions changed that dynamic so that participants were more in control, and seemed to consequently help reduce NSSI (‘Not letting them [thoughts and feelings] take control over me’—P11).
-
v.
Management strategies: once identified, it was possible for participants to put strategies in place to alter, manage or control these difficult emotions (‘Learning that I have other ways to change how I feel - or don’t feel - and learning to do those things.’—P22). The methods of managing difficult emotions which helped participants were stress-reduction techniques, such as MBSR and relaxation techniques, hypnotherapy, having regular times to check in with emotions. However, despite many strategies helping participants to ‘stop letting [their] emotional pain build up’ (P64) and thus manage their NSSI, one participant eloquently described how management strategies were in fact less helpful than seemingly more basic emotional awareness work (‘I haven’t attended therapy for over a decade, but better understanding my anger and the causes of it (not necessarily any relevant, suggested coping mechanisms/strategies) was the most constructive in regards to self-injury’—P12).
Other subthemes of ‘Understanding myself’ were:
Sensory issues: two participants acknowledged sensory stimulation can be tied up with their need to engage in NSSI, and that increasing awareness of physiological states (‘checking in with myself every few hours to know if I am hungry/too hot/too cold/thirsty/tired’—P39) and being aware of when they needed to do something to change that was helpful.
Self-esteem: several participants described how through therapy, they had become aware of the role of low self-confidence or self-esteem in their NSSI, such that building their self-esteem made NSSI less likely (‘That I hurt myself out of low self-love and low self-esteem (which did improve in time, and so did self-injuries become less possible’—P74).
Getting a diagnosis of ASC: being diagnosed with ASC was cited by several participants as beneficial to understanding and/or reducing their NSSI (‘Actually having my ASD diagnosis has been the most helpful thing’—P10). Notably, the five participants who made statements in this vein were diagnosed after the age of 30, two in their sixties.
Comorbidities: three participants also acknowledged the importance of addressing and treating their comorbidities in understanding and controlling their NSSI, naming depression, anxiety, OCD and eating disorders (P71, P13, P58).
As a theme, ‘Understanding myself’ seemed the key aspect of therapy which helped participants control and understanding their NSSI. This psychotherapeutic work appeared to enable participants to gain insight into their own feelings, behaviours and other difficulties and to reflect on these in a less judgmental, accepting way. It is possible that this more compassionate attitude to the self made NSSI less of viable option.
Practical strategies
As well as the psychotherapeutic work which was central to most participants’ experience of therapy, the next theme described learning practical strategies (the next theme) to cope with urges to self-injure, with examples given such as wearing false nails, elastic bands or drawing in red. There is a link, here, with the emotional awareness and the sensory issues subthemes of ‘Understanding myself’, as these strategies were described for the purpose of managing emotions and sensory experiences once these were identified. For example, finding an alternative sensory stimulation to NSSI was found to be helpful for one participant (‘We did however explore options of generating strong sensory input without causing injury (similar to ‘skills lists’ for BPD)’—P5). Although not aimed at eliminating NSSI itself, one participant (P44) explained how they would reduce alcohol consumption if they intended to self-harm, a sort of damage limitation strategy.
Specific forms of therapy
In this theme, participants mentioned specific forms of therapy, in addition to the relaxation techniques mentioned above, which were useful. These included occupational therapy (P32), CAT (P10) and CBT (P48); conversely, one participant expressed that CBT had made them feel much worse (P10).
Relationships
Several participants mentioned how the therapeutic relationship was itself beneficial, simply for having ‘regular time’ to ‘check in’ (P27), a safe place to talk and the feeling of ‘being heard’ (P48) by ‘someone who understood’ (P62). Similarly, three participants acknowledged the role of social connections not just within the therapeutic setting in reducing their NSSI (‘Therapy was helpful but when alone for periods in my life, I will regress to self-harming’—P8).
Psychotherapy is not always beneficial
This theme, which stands in contrast to the rest of the responses to this question, importantly reflects assertions that therapy undertaken had been at best unhelpful and at worst detrimental. Some participants expressed their confusion and difficulty knowing how to respond to questions from therapists (‘Therapy not understand autistic person they use their understanding of how they operate to judge an autistic operating system so all it does is give confusion they get cross and I feel sad and lost because I am not being good and compliant’—P23). Another participant described the group therapy they had received as ‘totally inappropriate’ and ‘traumatising’ (P46). There were many comments that therapy had been ineffective but where participants did not elaborate on why (P14, P28, P38, P41, P47, P55). It is possible that a ‘one size fits all’ approach to psychotherapy may have also been the reason that these participants found no value in the therapy they had been offered.
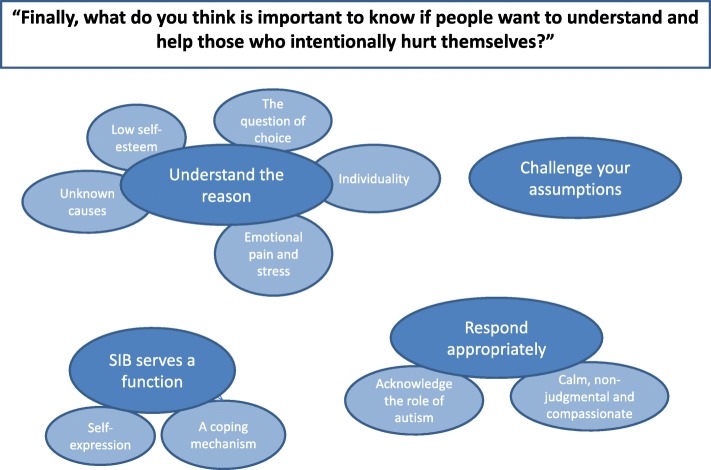
The second set of responses we analysed were in response to the following question: ‘Finally, what do you think is important to know if people want to understand and help those who intentionally hurt themselves?’. A thematic map for this question can be seen in Fig. 4.
Fig. 4.
Second thematic map. Figure depicts themes and subthemes exploring the themes and subthemes around messages for people who want to understand and help self-harmers
Four themes emerged from analysis of this item. It was clear from the data that participants wanted others to understand the reasons behind NSSI. Instead of resorting to stereotypes about people who self-injure, participants were definite that others should challenge their assumptions and seek to look beyond the behaviour itself to the underlying reasons for it. The most prominent reason, and a theme in its own right, was that NSSI served a function for most participants as a coping mechanism or a means of self-expression. With this new knowledge, others involved with those who self-injure should respond appropriately, that is calmly, non-judgmentally and compassionately, whilst acknowledging the unique role of autism in these individuals who self-injure. A full table of themes and quotes can be seen in Additional file 1: Table S3.
Understand the reason
Participants wanted others to understand that people engage in NSSI for a reason and that people should seek to understand the reason in order to better understand NSSI and help self-harmers. It was important to participants that people realise that NSSI in itself was not necessarily the problem (or indeed a problem), but rather ‘a symptom of a significant problem’ (P41), and that ‘the outer wound only hints at a much more painful inner (hidden) wound’ (P59).
Participants wanted others to know that the main reasons behind the use of NSSI were that it was a response to low self-esteem, emotional pain. It was acknowledged that that there is great individuality in the motivations to self-injure, and that sometimes there are unknown reasons behind participants’ NSSI. NSSI may or may not be a choice. We explore each subtheme in turn.
Emotional pain: The overwhelming majority of participants cited difficult emotional experiences as prompting their self-injury. Specifically, participants mentioned confusing emotions, anger, stress, anxiety, frustration, ‘pressure’, ‘emotional pain’, ‘hurting inside’ and stress as the precursors to self-injury, and one participant suggested that NSSI serves as ‘a coping mechanism to convert emotional pain into physical pain’ (P9).
Low self-esteem: One of the less frequent causes mentioned by participants was low self-esteem, which was cited by one participant as resulting from the difficulties they faced as a person with autism (‘I hurt myself because of my self-hatred and desire to punish myself for the problems I have with everything due to my Aspergers’ (P47).
Unknown causes: Whilst theoretically self-injury should always serve a functional purpose, several participants explained that people who engage in NSSI may not fully understand why they do it themselves (‘I really don’t know why I did it’—P17).
Individuality: Participants expressed the importance of recognising the individuality of the self-injurer before making assumptions about why someone is turning to NSSI (‘It’s really important to find out how to address each individual, there is a common misconception that we all fit in the same box … we really don’t’—P70).
The question of choice: This subtheme reflected an interesting dichotomy in the data. A number of participants (P6, P17, P72, P26, P65, P70, P45, P46) expressed a lack of conscious control or choice over self-injury (‘That it happened just like that; I had no control over hurting myself’—P6) and a clear aversion to the behaviour (‘They don’t want to do it’—P44). The word ‘compulsion’ was used twice (P26, P65), the word ‘addiction’ twice (P72, P46). However, the way NSSI was framed by other participants (P5, P7, P12, P16, P18, P21, P27, P39, P41, P46) suggested it was a conscious choice, a strategy that people could choose to use (‘I have no problem with intentional hurting. I know when and why … I can either not do the act [the stressful thing] or cause some pain to achieve homeostatic balance’—P7). In line with this, some explained that NSSI should not always be seen as a negative thing (‘That sometimes, if controlled appropriately, it can be a helpful way to control overwhelming feelings. As long as it is controlled and isn’t causing huge degrees of harm, then there could be many worse things the person could be doing’—P16). The words ‘choice’ or ‘choose’ were used by two participants (P7, P46), whereas others use the word ‘strategy’ (P21) or ‘outlet … a form of expression’ (P12), and mention their ability to ‘control’ or ‘resist’ it (P16, P39). Interestingly, one participant used the word ‘compulsive’ to distinguish their self-injury from ‘impulsive’ acts (P27). This participant appeared to be using the word in a different sense to those described above, who seemed to use ‘impulse’ and ‘compulsion’ in an interchangeable way that suggested they were ‘forced to do it’ (e.g. P25, P26). Participant 27’s use of the words seems to correspond to their more scientific definitions, ‘impulsive’ as ‘a predisposition toward rapid, unplanned reactions to internal or external stimuli with diminished regard to the negative consequences of these reactions’, and ‘compulsive’ as ‘a tendency to perform unpleasantly repetitive acts in a habitual or stereotyped manner to prevent perceived negative consequences’ ([72], pp. 591). The words used by some participants suggested that they might feel both elements of control and elements of helplessness: one (P46) spoke of self-injury first as a ‘choice’ and then as ‘an addiction’ (implying automaticity and lack of volition) in the same sentence.
Challenge your assumptions
Several participants believed there are public misperceptions about those who self-injure and that these should be challenged. The most commonly cited perceptions that participants thought were prevalent were that those who self-injure are ‘crazy’ (P9), ‘attention seekers’ (P50), ‘drama queens’ (P18), ‘irresponsible and over emotional’ (P18), or had a personality disorder (P50). Another participant alluded specifically to inaccurate attitudes of some health professionals regarding the motivation for NSSI (‘Not everyone who self-injures does it for attention. When medical personnel are treating these people, they deserve the same respect and treatment that anyone else would get. Don’t assume they ‘like pain’ and refuse them anaesthetic’—P22). Notably, with a link to the choice subtheme above, some participants found it unhelpful that self-injury was automatically seen as a negative thing (P5, P41).
NSSI serves a function
Participants wanted others to know that NSSI has a functional role in managing a range of difficulties. This links to the choice subtheme discussed above, where some participants expressed that NSSI was not always a negative thing—that it was not, in itself, a distressing thing, and was something they would struggle to do without (‘If anyone had tried to get me to stop, I would have been much, much worse’—P27). The first of two subthemes of this theme was the idea of NSSI as a ‘coping mechanism’ (P9), a tool participants could use to ‘self-regulate or cope with overwhelming emotions or find brief relief from suffering’ (P28), such that they could continue their day and participate in activities like work and social interactions that they would have otherwise been unable to complete (‘Some days things happen and I feel so overwhelmed that I feel like I will break completely and I have no idea how I can get through my day (I work). Seeing the blood is like flipping a switch … then I can go back and get on with meetings and talking to people’—P3). The second subtheme was the idea of NSSI as means of self-expression, ‘much like any creative or artistic outlet … a form of expression that some people turn to when words or other communicative methods do not fully convey how they feel’ (P12)—a method which served a function when participants had no alternative means of expressing themselves.
Respond appropriately
Finally, having helped others to understand the causes behind NSSI, people should use this knowledge to respond appropriately to the self-injurer in a way that will support them best: calmly, non-judgementally and compassionately, and recognising the autism-specific needs of the individual.
Calmly, non-judgmentally and compassionately: A calm, non-judgmental and compassionate approach was mentioned as an appropriate way to respond (‘Never get emotional about it with someone—P10; ‘Be patient and understanding. Non-judgemental and considerate’—P49). Above all, participants expressed that others should make the person who self-injures aware that they are not alone, that they are loved, supported and cared for (‘Be there for them. Make sure they know they’re loved. DON’T leave them alone’—P53; ‘People need relationships, love and appreciation’—P56).
Acknowledge the role of autism: Participants explained that others should acknowledge the role that autism has in NSSI, especially when trying to discuss it. They should potentially modulate their communication appropriately (‘You are speaking a different understanding and it is so hard to find a moment where understanding touches’—P23; ‘To not beat around the bush. Just try and speak openly about it’—P24). One participant conceptualised their NSSI as part of their autism, highlighting that NSSI may need to be conceptualised differently in autistic and non-autistic people (‘It’s a part of my autism - a repetitive, ritualistic, stereotyped behaviour that has developed with me for the past 20 years’—P27).
Discussion
The prediction and characterisation of self-injury in autistic people is of high clinical importance, given the relationship between self-injury and later suicidality [3–9]. Our mixed-methods approach addressed the dearth of research on self-injury in autistic people without intellectual disability by validating and extending findings from a previous investigation of self-injury in this population [15]. The features of self-injury were remarkably similar in this considerably larger dataset of autistic individuals. An adolescent age of onset of NSSI was confirmed (12.7 years in Maddox et al., 15.1 years in the present study), which mirrors the typical age of NSSI onset in neurotypical participants [1, 73]. As in Maddox, descriptive analysis showed that our participants most commonly engaged in scratching, pinching or cutting, and most often targeted the hands and arms; self-anger and upset were common initial motivators, but the largest proportion of our participants claimed to have stumbled on self-injury ‘accidentally’ without having seen or heard of it from external sources. Whilst Maddox et al. found no difference in the prevalence of self-injury in a direct comparison of autistic adults diagnosed in childhood and those diagnosed after 18, we likewise found no significant differences in age of diagnosis between current, historic and non-self-harming autistic adults, suggesting that no group is of particular risk. Our participants did differ from those in the previous study in respect of biological sex, with Maddox and colleagues reporting a greater number of autistic women than men in their self-harming group. Respondent bias might possibly have influenced these findings in both cases: most participants in the previous study were male (24 out of 42), whereas the majority of our participants (70 out of 103) were female. Sex differences in autistic self-harmers are of interest given that NSSI tends to be more prevalent in women generally, with the ratio of women to men especially greater in clinical populations [74].3 Our data suggests that this assumption cannot be extended to autism: self-injury, in ASC, should be of concern to clinicians of male and female patients.
An important goal highlighted in this study is the need to identify autistic individuals at heightened risk for self-injury, and we consequently aimed to extend the previous work in this area with consideration of the variables that might be of clinical importance in predicting the presence of self-injury.
Predictors of self-injury: alexithymia, depression, anxiety and sensory differences
Alexithymia, difficulty identifying one’s own emotional states, was a prime candidate of interest given its common presence in clinical populations who self-injure [16–20]. This construct is not entirely equivalent to emotional dysregulation (operationalised by Maddox et al. with the Emotion Regulation Scale [75]), but encapsulates the latter in combination with difficulty identifying and understanding one’s emotions [76, 77]. With this substantially larger sample, alexithymia was a significant predictor of self-injury, with current self-harmers exhibiting the highest levels of alexithymia followed by historic and then non-self-harmers. Our analysis further connected alexithymia to NSSI for the functional purpose of regulating high-energy states and as a means of social influence (communication and expression). This corroborates our theory-driven interest in this variable: individuals with alexithymia have difficulty identifying, and indeed regulating, high-energy states such as anger, agitation, frustration and anxiety, and by its nature alexithymia describes a difficulty in expressing emotional states that would make communication difficult. The importance of this variable also emerged in qualitative responses, where participants spoke about how learning to identify and express emotions, and understand the cause of emotions, was helpful. The use of NSSI to ‘control overwhelming feelings’, and the ‘traumatic’ and ‘frustrating’ difficulty of communicating how they feel, also corroborated our quantitative data around alexithymia.
A growing literature has highlighted the importance of diagnosing comorbid alexithymia, which may explain some of the socioemotional and communicative deficits of autism and be worthy of targeted intervention [78–83]. Our analysis, indeed, suggests that alexithymia may be of clinical relevance in identifying those at particular risk of self-injurious behaviour. The decreased levels of alexithymia in the historic as compared to current self-harmers does, however, create an interesting puzzle for future research. Alexithymia is generally conceptualised as a stable construct (a trait) [84–86], though the temporal stability of the factors (difficulty identifying feelings, difficulty describing feelings and externally orientated thinking) has been seen to differ, the former two to increase when patients are in depressive episodes [87]. Current self-harmers were indeed marginally more depressed than historic self-harmers, but not significantly so.
Difficulty identifying and communicating one’s own emotional states (alexithymia) is closely related to the ability to identify and understand the emotional and mental states of other people. Impairments in this latter ability, commonly known as ‘theory of mind’ or ‘mentalising’, were, like alexithymia, hypothesised to put participants at particular risk of self-injury. Interestingly, this hypothesis was not borne out: deficits in the popular ‘Reading the Mind in the Eyes’ task (RMET) [41] were unrelated to the presence of self-injury, its range or frequency or its use for the functional purpose of communicating with others. Notably, previous literature has failed to link NSSI to mentalising deficits, although these are common in clinical populations notorious for self-injury [31–33]. A tenuous link has been made between the two with therapeutic attempts to alleviate self-injury through improving mentalising ability [36–38]. Problematically, the described therapeutic approach conflates strengthening mentalising ability with alleviating alexithymia, involving as it does increasing awareness and identification of emotions and communicating about them. Importantly, mentalising and alexithymia are distinct constructs, and there is debate as to whether the RMET indexes mentalising (the common assumption and the assertion of the authors, who validated it against other mentalising tasks [88–90]) or recognition of emotional expressions [91], deficits in which are associated with alexithymia. Adopting the latter view leaves open the question as to whether mentalising deficits really do increase the risk of self-injury, but the implication from our data, given the relationship between NSSI and TAS-20 scores but not between NSSI and RMET, is that the inability to identify and express one’s emotions is of greater concern for self-injury than is the ability to recognise emotions in others, even if the latter would theoretically impair communication.
Further variables of clinical interest for the risk of self-injury were depression and anxiety. Depression was examined by Maddox et al., who found no difference between their self-harming and non-self-harming autistic groups. We suggest the likely reason for this lack of difference was their indiscriminate categorisation of self-harming participants, a group containing current self-harmers and those we would classify as ‘historic’.4 Indeed, where current depression significantly predicted the dichotomous likelihood that participants had ever engaged in NSSI, planned t tests revealed that significant differences were only evident between current and non-self-harmers, and between historic and non-self-harmers, but not, as previously mentioned, between current and historic self-harmers. The same was true of anxiety, which was significantly higher in both self-harming groups than in the non-self-harming group. Of course, the implications of these findings are tempered by the fact that depression and anxiety, as measured by the BDI and the BAI, reflect states, not traits: in this case, they reflect emotional state over the last 2 and 4 weeks respectively. State anxiety tends to correlate with trait anxiety [92], but without the inclusion of a measure of trait anxiety, we can only speculate whether trait anxiety is a risk-factor for NSSI. Nevertheless, the data corroborates the association between depression, anxiety and self-injury [73, 93–101], and highlights the risk for self-injury in autistic sufferers of anxiety and depression. The most common functional purpose of self-injury reported by our sample was the regulation of low-energy states (e.g. depression, dissociation), with the second most popular function being the alleviation of high-energy states (which include anxiety). The qualitative data, too, makes mention of depression and anxiety, which are implied by one participant as the cause of self-injury in so far as tackling these issues helps reduce NSSI.
The last variables explored as potential risks for NSSI were autistic traits as a proxy of symptom severity [42], and sensory differences [13, 49]. Interestingly, though both variables were highlighted in the literature on the ‘stereotyped’ form of NSSI often seen in individuals with autism and intellectual disability, sensory sensitivity also appeared in our group as a predictor of group categorisation, and sensory differences were the only variables to predict the range of body areas targeted (sensory avoidance), lifetime incidence of NSSI (sensory avoidance) and the frequency of NSSI in most active phase (sensory low registration). These findings are theoretically consistent with the high level of distress that autistic people report from their sensory disturbances [102–104], and are bolstered by data from our qualitative analysis, where NSSI was linked to being ‘overwhelmed’ by sensory stimulation, and could be helped by learning to identify sensory needs and/or sensory stimulation. That individuals with low registration (that is, under-responsivity to sensory stimulation) might engage in NSSI with higher frequency has alarming implications for injuries more severe than perhaps intended, and highlights self-injury as a potential deleterious association of sensory differences.
Scientists, loved ones and practitioners: what can we learn from the voices of autistic people?
Improving clinical services and mental health is a highly topical issue and a research priority for the autistic community [105–107], and here special attention should be paid to the voices of autistic people in our qualitative data [105, 108–111]. What implications can be drawn from our qualitative data to inform research and/or clinical practice? As phrased in our question to participants, what should people know if they want to understand and help?
Autistic people in our analysis placed a high importance on understanding the diverse reasons for NSSI, both for the sake of alleviating or controlling their self-injury and so that others could respond to them more appropriately. Furthermore, our analysis demonstrated a need to critically consider the meaning that autistic individuals themselves ascribe to NSSI, and we query whether it is the functions of NSSI, rather than NSSI in and of itself, which may be predictive of mental illness and suicidality. This relates back to the dichotomy seen between individuals who felt a great deal of distress and helplessness in the face of self-injury, and those who appeared to approach their self-injury quite practically and methodically as a coping mechanism. The framing of self-injury as an ‘addiction’ draws an interesting parallel with research in non-autistic participants and the lay view of self-injury [112]. Some theorists speak of it as a ‘process addiction’ with addictive features including compulsion, loss of control, difficulties stopping and increasing tolerance [113]. Biologically, the pain of injury stimulates the release of endogenous opiates which can produce analgesic and euphoric effects [114]. Others investigating NSSI alongside cravings for and abuse of substances point out that consciously, self-injury is craved for reasons of negative reinforcement (reduction of aversive emotions) rather than by positive reinforcement [115]. This is the kind of negative reinforcement described by one participant who felt ‘calm’, after feeling ‘overwhelmed’, upon seeing blood. Interestingly, non-autistic participants suggest that quite aside from pain, looking at the blood from self-injury seems particularly important for many self-harmers, serving to, likewise, ‘make [s] me feel calm’ [116].
If self-injury is powerfully reinforced by behavioural contingencies, clinicians should be aware that NSSI is not easily changed. However, they must also be aware of the latter group of participants who may see no problem with their self-injury, as a conscious choice that might be preferable to other options and one that might, in fact, cause problems if made unavailable. This view may be somewhat alien to loved ones and clinicians who quite naturally, and rightly considering its links to suicidality, view NSSI with high concern. Of course, where participants appear to express clear distress that they attribute to their self-injury, this clearly necessitates action from the conscientious practitioner. However, we suggest that a measured response, one that acknowledges a potentially functional, ‘rational’ purpose of NSSI, may be beneficial whilst clinicians ascertain the functional role and meaning ascribed to NSSI by that individual.
Both questions highlighted the great importance of how others react to the autistic individual (the need for compassion; empathy; non-judgement; patience; and open-mindedness, avoiding assumptions and emotionality). Participants appeared to place great value on the safety and regularity of the therapist’s office as a place to talk and be heard, as has also been emphasised in the treatment of self-harming non-autistic patients [32, 117]. Several participants highlighted that communication is problematic, that therapists and clinicians may be ‘speaking a different understanding’ (P23) and that misunderstandings can give rise to feelings of despair in individuals who are trying to comply. It is important that clinicians recognise the especial communicative needs of this group, and that likewise, commonly used clinical tools, designed for non-autistic people, may not be entirely fit for purpose [118–121].
Therapeutic goals that autistic adults highlighted as helpful in helping them understand and decrease self-injury included increasing poor self-esteem and low self-confidence, decreasing self-criticism, teaching practical strategies and managing sensory issues. Both low self-esteem [122, 123] and self-criticism [124–127] have been linked to NSSI; poor self-esteem, in particular, appears (along with weak coping strategies) to mediate the relationship between personality pathology and self-injury [128]. Accordingly, therapeutic interventions in non-autistic participants commonly attempt to decrease self-criticism and improve self-worth, alongside teaching more adaptive coping strategies [32, 117, 129, 130]. Teaching more adaptive means of emotional expression and regulation is also an element of these interventions, as is replacing behaviours with alternatives meeting the same functional purposes; this is concordant with our participants highlighting alternative behaviours and damage limitation strategies that are helpful for them in managing self-injury. Our participants also highlighted that identification and management of sensory issues, and understanding their self-injury within the context of their autism, had been helpful. Whether sensory interventions or so-called sensory diets of prescribed activities, the efficacy of which is debated in terms of positive outcomes [131, 132], have any positive effect on autistic NSSI in this population is yet to be determined. As so little research focuses on therapeutic interventions for autistic adults, this is an important avenue for future study.
Limitations and directions for future study
The present study aimed to advance understanding of NSSI in autistic adults without intellectual disability, an understudied group. Given the relationship of NSSI to mental ill-health and suicidality, an understanding of the particular risk factors that might improve identification and treatment of NSSI is a worthwhile goal. Lacking a control group of non-autistic participants, the present study cannot certify whether the variables that predicted classification as current, historic or non-self-harmers—alexithymia, depression, anxiety and sensory sensitivity—are especial risk factors for autistic people or would similarly indicate non-autistic individuals at greater risk of self-injury. The small sample of autistic and non-autistic self-harmers compared in previous research [15] imply many similarities in the use of NSSI between groups, but these preliminary findings require validation in a larger group, alongside examination of risk variables for self-injury.
Limitations to the current work include the variables we were unable to consider, notably IQ, which could not be operationalised in this online design. We surmise that our participants would be considered to have an IQ in the average to high range [> 70]); over half were qualified to degree level in each group, and all participants had attended school to GCSE (UK) or equivalent level. As such, our conclusions must be considered with caution as regards their relevance to autistic people with intellectual disabilities; although self-injurious behaviour in this group also seems related to sensory differences [13, 49], it remains to be investigated whether alexithymia, for instance, increases the risk of self-injury in autistic individuals with intellectual impairment. Similarly, we were unable to obtain a more thorough operationalization of autistic symptomatology, such as might be provided through use of the Autism Diagnostic Observation Schedule [133], and therefore operationalised this variable only through use of the AQ. Furthermore, given the debate described above regarding the use of RMET to measure theory of mind [91], further investigation of the role of sociocommunication difficulties related to mentalizing in NSSI might be valuable.
Limitations of our statistical approach should also be considered. We adopted an a priori analysis informed by prior literature, and did not correct significance values for multiple statistical tests. The issue of multicollinearity, overlapping variance between measures, is also one to be considered. As can be seen in our analysis and Additional Materials, many of the predictor variables explored in this study tend to correlate: previous literature has demonstrated, for example, that alexithymia is strongly associated with autism and autistic traits [82], that a relationship exists between autistic traits and depressive symptomatology [134] and that depression and anxiety often co-exist in autistic [135, 136] and non-autistic [137] populations. In an analysis of this size, it is hard to identify the unique contribution of any one of these variables, stripped of the overlapping variance with its fellows. The analysis does, however, highlight some screening tests, for example alexithymia, as being more valuable than others if clinicians are concerned about self-injury.
Much remains to be ascertained to understand the incidence of NSSI in autistic adults with and without intellectual disability and for identifying those most at risk. Given the divergence in how participants perceive their self-injury, we question the nature of the risk, the link between self-injury, suicide ideation and suicidal acts seen in non-autistic people [3–9]. Future research might investigate whether NSSI similarly increases the risk of suicide ideation and behaviours in autistic individuals, or whether this relationship is mediated by another factor/s, such as self-esteem, the function played by NSSI or the perceptions held by participants about it; whether those in whom NSSI might indicate a suicide risk can be identified. Although several variables are highlighted here as potentially important in the aetiology of self-injury, it remains to be ascertained whether, systematically and specifically targeted, alleviation of related symptoms is beneficial to those who suffer from their self-injury.
Another broader query, within this study and pertaining to general clinical use, concerns the use of measurement and assessment tools designed for non-autistic individuals. As previously mentioned, tools specific to autistic individuals are now being developed to accurately assess depression and suicidality [118, 119], but the key measures in this study were designed for use with non-autistic individuals and have never been validated with autistic groups. As one participant phrased so aptly, non-autistic clinicians ‘use their understanding of how they operate to judge an autistic operating system’, and thus are liable to make assumptions about the way psychometric items are perceived or interpreted. A very basic example, from the NSSI-AT, is the continuously used phrase ‘hurt yourself’. The instrument thoroughly assesses methods of self-injury, but at no point queries whether the participant actually experiences pain from any of these behaviours. There has been rigorous scientific debate as to whether autistic people have different pain thresholds to non-autistic people, or at least have a qualitatively different subjective experience of it [138–140]. It is plausible that an individual who does not experience pain from NSSI might be perturbed by a literal understanding of the term ‘hurt yourself’. Another instance is the TAS-20, which despite being robustly used in autism research (see, for instance, [80, 82, 141]), has never undergone a thorough examination (e.g. [118, 119]) as to whether autistic individuals understand items in the same way as non-autistic people; the very nature of the alexithymia construct might challenge comprehension of the test. Although our data suggests that the TAS-20 is a reasonable predictor of engagement in NSSI, the fact that this and other measures were not designed with autistic people in mind raises important questions about how the utility of these measures might be maximised for clinical usage.
Conclusions
The present study attempted to elucidate the features of self-injury in autistic individuals without intellectual disability, and to explore the thoughts of participants regarding their self-injury and helpful interventions. There was great diversity in the quantitative and qualitative data, with several participants signalling the disruptive effects of NSSI, their distress and lack of control over it, whilst others indicated that NSSI appeared to play a functional role in their lives, compartmentalised as a coping technique under their control. Variables that might differentiate self-harming from non-self-harming individuals were also of interest in so far as they might predict the incidence of self-injury and provide vital clues for understanding and treating the phenomenon. Current and historic self-harmers were set apart from non-self-harmers by their scores in measures of depression, anxiety, alexithymia and sensory sensitivity.
Additional File
Table S1. Pearson correlation coefficients between predictor variables. Table S2 Qualitative analysis: Experiences with therapy. Table S3 Qualitative analysis: what others should know about NSSI. (DOCX 45 kb)
Acknowledgements
We would like to acknowledge and thank our colleagues at Bournemouth University for their support, most especially Dr. Bernhard Angele, who provided invaluable statistical guidance. Our thanks go to the Dorset Adult Asperger Support group, who provide invaluable services for autistic adults in the Dorset area and who allowed us to advertise the study to their members, and to the owners of social media platforms where we were able to advertise the study. Our ultimate gratitude goes to the autistic individuals who were brave and generous enough to share their experiences. You are courageous.
Funding
RLM and NG are salaried staff of Bournemouth University and did not receive external funding for this project. SBC, PS and CA were supported by the Autism Research Trust, Autistica, and EU-AIMS during the period of this work. The research was conducted in association with the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care East of England at Cambridgeshire and Peterborough NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, NIHR or Department of Health and Social Care.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASC
Autism spectrum conditions
- NSSI
Non-suicidal self-injury
- NSSI-AT
Non-Suicidal Self-Injury Assessment Tool
- RMET
Reading the Mind in the Eyes Test
Authors’ contributions
Quantitative data was collected and analysed by RLM, the primary author of the manuscript, with access to many participants provided by PS, CA and SB-C via the Cambridge Autism Research Database (CARD). NJG and RLM analysed the qualitative data in a collaborative approach. NJG, PS, CA and SB-C all edited and contributed to the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethical approval of the study was granted by Bournemouth University Ethics Committee. All participants provided fully informed consent to take part in the study.
Consent for publication
Consent to publish anonymized data was granted by participants when consenting to take part in the study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
We choose here to use the identity-first language preferred by the majority of autistic individuals [142], but respect the right of individuals to use person-first or identity-first language.
We did not ourselves confirm the diagnostic status of participants, but confirmed the precise diagnosis they had received and the date they received it when entering the study.
Of note, studies of NSSI in typically-developing (non-autistic) participants suggest that sex differences are especially apparent in the methods that people use to self-injure, with women more likely to engage in cutting specifically [74, 143]. Some studies suggest men more likely to engage in hitting or burning [143].
Though, notably, differences could also be partially due to measures used: we employed the Beck Depression Inventory, whilst Maddox and colleagues used the Patient Health Questionnaire-9 [144].
Contributor Information
R. L. Moseley, Phone: 01202 965538, Email: rmoseley@bournemouth.ac.uk
N. J. Gregory, Email: ngregory@bournemouth.ac.uk
P. Smith, Email: pls28@cam.ac.uk
C. Allison, Email: cla29@cam.ac.uk
S. Baron-Cohen, Email: sb205@cam.ac.uk
References
- 1.Nock MK. Self-injury. Annu Rev Clin Psychol. 2010;6:339–363. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- 2.Whitlock J, Exner-Cortens D, Purington A. Assessment of nonsuicidal self-injury: development and initial validation of the Non-Suicidal Self-Injury-Assessment Tool (NSSI-AT) Psychol Assess. 2014;26:935–946. doi: 10.1037/a0036611. [DOI] [PubMed] [Google Scholar]
- 3.Cooper J, Kapur N, Webb R, Lawlor M, Guthrie E, Mackway-Jones K, et al. Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry. 2005;162:297–303. doi: 10.1176/appi.ajp.162.2.297. [DOI] [PubMed] [Google Scholar]
- 4.Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537–542. doi: 10.1192/bjp.182.6.537. [DOI] [PubMed] [Google Scholar]
- 5.Hawton K, Harriss L. Deliberate self-harm in young people: characteristics and subsequent mortality in a 20-year cohort of patients presenting to hospital. J. Clin. Psychiatry. 2007;68:1574–1583. doi: 10.4088/JCP.v68n1017. [DOI] [PubMed] [Google Scholar]
- 6.Olfson M, Wall M, Wang S, Crystal S, Gerhard T, Blanco C. Suicide following deliberate self-harm. Am J Psychiatry. 2017;174:765–774. doi: 10.1176/appi.ajp.2017.16111288. [DOI] [PubMed] [Google Scholar]
- 7.Wester KL, Ivers N, Villalba JA, Trepal HC, Henson R. The relationship between nonsuicidal self-injury and suicidal ideation. J Couns Dev. 2016;94:3–12. doi: 10.1002/jcad.12057. [DOI] [Google Scholar]
- 8.Cox LJ, Stanley BH, Melhem NM, Oquendo MA, Birmaher B, Burke A, et al. A longitudinal study of nonsuicidal self-injury in offspring at high risk for mood disorder. J Clin Psychiatry. 2012;73:821–828. doi: 10.4088/JCP.11m07250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.David Klonsky E, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. J Abnorm Psychol. 2013;122:231–237. doi: 10.1037/a0030278. [DOI] [PubMed] [Google Scholar]
- 10.Cassidy S, Bradley P, Robinson J, Allison C, McHugh M, Baron-Cohen S. Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic: a clinical cohort study. Lancet Psychiatry. 2014;1:142–147. doi: 10.1016/S2215-0366(14)70248-2. [DOI] [PubMed] [Google Scholar]
- 11.Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, et al. The health status of adults on the autism spectrum. Autism. 2015;19:814–823. doi: 10.1177/1362361315577517. [DOI] [PubMed] [Google Scholar]
- 12.Minshawi NF, Hurwitz S, Fodstad JC, Biebl S, Morriss DH, CJ MD. The association between self-injurious behaviors and autism spectrum disorders. Psychol Res Behav Manag. 2014;7:125–36. [DOI] [PMC free article] [PubMed]
- 13.Duerden EG, Oatley HK, Mak-Fan KM, McGrath PA, Taylor MJ, Szatmari P, et al. Risk factors associated with self-injurious behaviors in children and adolescents with autism spectrum disorders. J Autism Dev Disord. 2012;42:2460–2470. doi: 10.1007/s10803-012-1497-9. [DOI] [PubMed] [Google Scholar]
- 14.Matson Johnny L., LoVullo Santino V. A Review of Behavioral Treatments for Self-Injurious Behaviors of Persons With Autism Spectrum Disorders. Behavior Modification. 2008;32(1):61–76. doi: 10.1177/0145445507304581. [DOI] [PubMed] [Google Scholar]
- 15.Maddox Brenna B, Trubanova Andrea, White Susan W. Untended wounds: Non-suicidal self-injury in adults with autism spectrum disorder. Autism. 2016;21(4):412–422. doi: 10.1177/1362361316644731. [DOI] [PubMed] [Google Scholar]
- 16.Norman H, Borrill J. The relationship between self-harm and alexithymia. Scand J Psychol. 2015;56:405–419. doi: 10.1111/sjop.12217. [DOI] [PubMed] [Google Scholar]
- 17.Gratz Kim L. Targeting emotion dysregulation in the treatment of self-injury. Journal of Clinical Psychology. 2007;63(11):1091–1103. doi: 10.1002/jclp.20417. [DOI] [PubMed] [Google Scholar]
- 18.Bjärehed J, Lundh LG. Deliberate self-harm in 14-year-old adolescents: how frequent is it, and how is it associated with psychopathology, relationship variables, and styles of emotional regulation? Cogn Behav Ther. 2008;37:26–37. doi: 10.1080/16506070701778951. [DOI] [PubMed] [Google Scholar]
- 19.Zlotnick C, Shea MT, Pearlstein T, Simpson E, Costello E, Begin A. The relationship between dissociative symptoms, alexithymia, impulsivity, sexual abuse, and self-mutilation. Compr Psychiatry. 1996;37:12–16. doi: 10.1016/S0010-440X(96)90044-9. [DOI] [PubMed] [Google Scholar]
- 20.Roger D, Flynn M, Borrill J, Fox P. Students who self-harm: coping style. Rumination and Alexithymia Couns Psychol Q. 2009;22:361–372. doi: 10.1080/09515070903334607. [DOI] [Google Scholar]
- 21.Swannell S, Martin G, Page A, Hasking P, Hazell P, Taylor A, et al. Child maltreatment, subsequent non-suicidal self-injury and the mediating roles of dissociation, alexithymia and self-blame. Child Abus Negl. 2012;36:572–584. doi: 10.1016/j.chiabu.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 22.Paivio SC, McCulloch CR. Alexithymia as a mediator between childhood trauma and self-injurious behaviors. Child Abus Negl. 2004;28:339–354. doi: 10.1016/j.chiabu.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 23.Garisch JA, Wilson MS. Vulnerabilities to deliberate self-harm among adolescents: the role of alexithymia and victimization. Br J Clin Psychol. 2010;49:151–162. doi: 10.1348/014466509X441709. [DOI] [PubMed] [Google Scholar]
- 24.Zaki LF, Coifman KG, Rafaeli E, Berenson KR, Downey G. Emotion differentiation as a protective factor against nonsuicidal self-injury in borderline personality disorder. Behav Ther. 2013;44:529–540. doi: 10.1016/j.beth.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Baron-Cohen Simon. Autism: The Empathizing-Systemizing (E-S) Theory. Annals of the New York Academy of Sciences. 2009;1156(1):68–80. doi: 10.1111/j.1749-6632.2009.04467.x. [DOI] [PubMed] [Google Scholar]
- 26.Baron-Cohen Simon. Mindblindness. 1995. [Google Scholar]
- 27.Sharp C, Pane H, Ha C, Venta A, Patel AB, Sturek J, et al. Theory of mind and emotion regulation difficulties in adolescents with borderline traits. J Am Acad Child Adolesc Psychiatry. 2011;50:563–573. doi: 10.1016/j.jaac.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 28.Harari H, Shamay-Tsoory SG, Ravid M, Levkovitz Y. Double dissociation between cognitive and affective empathy in borderline personality disorder. Psychiatry Res. 2010;175:277–279. doi: 10.1016/j.psychres.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Choi-Kain LW, Gunderson JG. Mentalization: ontogeny, assessment, and application in the treatment of borderline personality disorder. Am J Psychiatry. 2008;165:1127–1135. doi: 10.1176/appi.ajp.2008.07081360. [DOI] [PubMed] [Google Scholar]
- 30.Baez S, Marengo J, Perez A, Huepe D, Font FG, Rial V, et al. Theory of mind and its relationship with executive functions and emotion recognition in borderline personality disorder. J Neuropsychol. 2015;9:203–218. doi: 10.1111/jnp.12046. [DOI] [PubMed] [Google Scholar]
- 31.Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet. 2004;364:453–461. doi: 10.1016/S0140-6736(04)16770-6. [DOI] [PubMed] [Google Scholar]
- 32.Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. 1993. [Google Scholar]
- 33.Gunderson J. G. Borderline Personality Disorder: Ontogeny of a Diagnosis. American Journal of Psychiatry. 2009;166(5):530–539. doi: 10.1176/appi.ajp.2009.08121825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bateman A, Fonagy P. Borderline personality disorder and mood disorders: mentalizing as a framework for integrated treatment. J Clin Psychol. 2015;71:792–804. doi: 10.1002/jclp.22206. [DOI] [PubMed] [Google Scholar]
- 35.Fonagy P, Luyten P, Bateman A. Translation: mentalizing as treatment target in borderline personality disorder. Personal Disord. 2015;6:380–392. doi: 10.1037/per0000113. [DOI] [PubMed] [Google Scholar]
- 36.Rossouw Trudie I., Fonagy Peter. Mentalization-Based Treatment for Self-Harm in Adolescents: A Randomized Controlled Trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(12):1304-1313.e3. doi: 10.1016/j.jaac.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 37.Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166:1355–1364. doi: 10.1176/appi.ajp.2009.09040539. [DOI] [PubMed] [Google Scholar]
- 38.Beck E, Bo S, Gondan M, Poulsen S, Pedersen L, Pedersen J, et al. Mentalization-based treatment in groups for adolescents with borderline personality disorder (BPD) or subthreshold BPD versus treatment as usual (M-GAB): study protocol for a randomized controlled trial. Trials. 2016;17 [DOI] [PMC free article] [PubMed]
- 39.Best CS, Moffat VJ, Power MJ, Owens DGC, Johnstone EC. The boundaries of the cognitive phenotype of autism: theory of mind, central coherence and ambiguous figure perception in young people with autistic traits. J Autism Dev Disord. 2008;38:840–847. doi: 10.1007/s10803-007-0451-8. [DOI] [PubMed] [Google Scholar]
- 40.Ronald A, Viding E, Happé F, Plomin R. Individual differences in theory of mind ability in middle childhood and links with verbal ability and autistic traits: a twin study. Soc Neurosci [Internet] 2006;1:412–425. doi: 10.1080/17470910601068088. [DOI] [PubMed] [Google Scholar]
- 41.Baron-Cohen S, Wheelwright S, Hill J, Raste Y, Plumb I. The “Reading the mind in the eyes” test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. J Child Psychol Psychiatry. 2001;42:241–251. doi: 10.1111/1469-7610.00715. [DOI] [PubMed] [Google Scholar]
- 42.McClintock K., Hall S., Oliver C. Risk markers associated with challenging behaviours in people with intellectual disabilities: a meta-analytic study. Journal of Intellectual Disability Research. 2003;47(6):405–416. doi: 10.1046/j.1365-2788.2003.00517.x. [DOI] [PubMed] [Google Scholar]
- 43.Klonsky ED, Glenn CR. Assessing the functions of non-suicidal self-injury: psychometric properties of the inventory of statements about self-injury (ISAS) J Psychopathol Behav Assess. 2009;31:215–219. doi: 10.1007/s10862-008-9107-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Klonsky E. David, Muehlenkamp Jennifer J. Self-injury: A research review for the practitioner. Journal of Clinical Psychology. 2007;63(11):1045–1056. doi: 10.1002/jclp.20412. [DOI] [PubMed] [Google Scholar]
- 45.Favell JE, Azrin NH, Baumeister AA, Carr EG, Dorsey MF, Forehand R, et al. The treatment of self-injurious behavior. Behav Ther. 1982;13:529–554. doi: 10.1016/S0005-7894(82)80015-4. [DOI] [Google Scholar]
- 46.Bogdashina O. Sensory theory in autism makes sense: a brief review of the past and present research. Open Access Autism. 2013;1:3. [Google Scholar]
- 47.Dunn W. The impact of sensory processing abilities on the daily lives of young children and their families: a conceptual model. Infants Young Child. 1997;9:23–35. doi: 10.1097/00001163-199704000-00005. [DOI] [Google Scholar]
- 48.Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, Gal E. A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. J Autism Dev Disord. 2009;39:1–11. doi: 10.1007/s10803-008-0593-3. [DOI] [PubMed] [Google Scholar]
- 49.Boyd BA, McBee M, Holtzclaw T, Baranek GT, Bodfish JW. Relationships among repetitive behaviors, sensory features, and executive functions in high functioning autism. Res Autism Spectr Disord. 2009;3:959–966. doi: 10.1016/j.rasd.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bagby M, Parker JDA, Taylor GJ. The twenty-item Toronto alexithymia scale—I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 51.Taylor Graeme J, Bagby R.Michael, Parker James D.A. The 20-Item Toronto Alexithymia Scale. Journal of Psychosomatic Research. 2003;55(3):277–283. doi: 10.1016/S0022-3999(02)00601-3. [DOI] [PubMed] [Google Scholar]
- 52.Kooiman CG, Spinhoven P, Trijsburg RW. The assessment of alexithymia: a critical review of the literature and a psychometric study of the Toronto alexithymia Scale-20. J Psychosom Res. 2002;53:1083–1090. doi: 10.1016/S0022-3999(02)00348-3. [DOI] [PubMed] [Google Scholar]
- 53.Müller J, Bühner M, Ellgring H. Is there a reliable factorial structure in the 20-item Toronto alexithymia scale? A comparison of factor models in clinical and normal adult samples. J Psychosom Res. 2003;55:561–568. doi: 10.1016/S0022-3999(03)00033-3. [DOI] [PubMed] [Google Scholar]
- 54.Loas G, Corcos M, Stephan P, Pellet J, Bizouard P, Venisse JL, et al. Factorial structure of the 20-item Toronto alexithymia scale confirmatory factorial analyses in nonclinical and clinical samples. J Psychosom Res. 2001;50:255–261. doi: 10.1016/S0022-3999(01)00197-0. [DOI] [PubMed] [Google Scholar]
- 55.Baron-Cohen S, Wheelwright S, Skinner R, Martin J, Clubley E. The Autism-Spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. 2001;31:5–17. doi: 10.1023/A:1005653411471. [DOI] [PubMed] [Google Scholar]
- 56.Ruzich E, Allison C, Smith P, Watson P, Auyeung B, Ring H, et al. Measuring autistic traits in the general population : a systematic review of the autism-spectrum quotient (AQ) in a nonclinical population sample of 6,900 typical adult males and females. Mol Autism. 2015;6:1–12. doi: 10.1186/2040-2392-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hurst RM, Mitchell JT, Kimbrel NA, Kwapil TK, Nelson-Gray RO. Examination of the reliability and factor structure of the autism spectrum quotient (AQ) in a non-clinical sample. Pers Individ Dif. 2007;43:1938–1949. doi: 10.1016/j.paid.2007.06.012. [DOI] [Google Scholar]
- 58.Hoekstra RA, Bartels M, Cath DC, Boomsma DI. Factor structure, reliability and criterion validity of the autism-spectrum quotient (AQ): a study in Dutch population and patient groups. J Autism Dev Disord. 2008;38:1555–1566. doi: 10.1007/s10803-008-0538-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brown C, Tollefson N, Dunn W, Cromwell R, Filion D. The adult sensory profile: measuring patterns of sensory processing. Am J Occup Ther. 2001;55:75–82. doi: 10.5014/ajot.55.1.75. [DOI] [PubMed] [Google Scholar]
- 60.Vellante Marcello, Baron-Cohen Simon, Melis Mariangela, Marrone Matteo, Petretto Donatella Rita, Masala Carmelo, Preti Antonio. The “Reading the Mind in the Eyes” test: Systematic review of psychometric properties and a validation study in Italy. Cognitive Neuropsychiatry. 2013;18(4):326–354. doi: 10.1080/13546805.2012.721728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fernández-Abascal Enrique G, Cabello Rosario, Fernández-Berrocal Pablo, Baron-Cohen Simon. Test-retest reliability of the ‘Reading the Mind in the Eyes’ test: a one-year follow-up study. Molecular Autism. 2013;4(1):33. doi: 10.1186/2040-2392-4-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio: Psychological Corporation; 1996. [Google Scholar]
- 63.Beck AT, Steer RA. Manual for the Beck anxiety inventory. San Antonio: Psychological Corporation; 1990. [Google Scholar]
- 64.Osman A, Downs WR, Barrios FX, Kopper BA, Gutierrez PM, Chiros CE. Factor structure and psychometric characteristics of the Beck depression inventory-II. J Psychopathol Behav Assess. 1997;19:359–376. doi: 10.1007/BF02229026. [DOI] [Google Scholar]
- 65.Arnau RC, Meagher MW, Norris MP, Bramson R. Psychometric evaluation of the Beck depression inventory-II with primary care medical patients. Health Psychol. 2001;20:112–119. doi: 10.1037/0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- 66.Storch EA, Roberti JW, Roth DA. Factor structure, concurrent validity, and internal consistency of the Beck depression inventory-second edition in a sample of college students. Depress. Anxiety. 2004;19:187–189. doi: 10.1002/da.20002. [DOI] [PubMed] [Google Scholar]
- 67.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 68.Ely M, Vinz RD, Downing M, Anzul M. On writing qualitative research: living by words. London: Falmer Press; 1997. [Google Scholar]
- 69.Kendall PC, Hollon SD, Beck AT, Hammen CL, Ingram RE. Issues and recommendations regarding use of the Beck depression inventory. Cognit Ther Res. 1987;11:289–299. doi: 10.1007/BF01186280. [DOI] [Google Scholar]
- 70.Woodbury-Smith MR, Robinson J, Wheelwright S, Baron-Cohen S. Screening adults for Asperger syndrome using the AQ: a preliminary study of its diagnostic validity in clinical practice. J Autism Dev Disord. 2005;35:331–335. doi: 10.1007/s10803-005-3300-7. [DOI] [PubMed] [Google Scholar]
- 71.Baron-Cohen S, Bowen DC, Holt RJ, Allison C, Auyeung B, Lombardo MV, et al. The “Reading the mind in the eyes” test: complete absence of typical sex difference in ~400 men and women with Autism. PLoS One. 2015;10:e0136521. doi: 10.1371/journal.pone.0136521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fineberg Naomi A, Potenza Marc N, Chamberlain Samuel R, Berlin Heather A, Menzies Lara, Bechara Antoine, Sahakian Barbara J, Robbins Trevor W, Bullmore Edward T, Hollander Eric. Probing Compulsive and Impulsive Behaviors, from Animal Models to Endophenotypes: A Narrative Review. Neuropsychopharmacology. 2009;35(3):591–604. doi: 10.1038/npp.2009.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nixon MK, Cloutier P, Jansson SM. Nonsuicidal self-harm in youth: a population-based survey. CMAJ. 2008;178:306–312. doi: 10.1503/cmaj.061693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bresin Konrad, Schoenleber Michelle. Gender differences in the prevalence of nonsuicidal self-injury: A meta-analysis. Clinical Psychology Review. 2015;38:55–64. doi: 10.1016/j.cpr.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 75.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26(1):41–54.
- 76.Swart Marte, Kortekaas Rudie, Aleman André. Dealing with Feelings: Characterization of Trait Alexithymia on Emotion Regulation Strategies and Cognitive-Emotional Processing. PLoS ONE. 2009;4(6):e5751. doi: 10.1371/journal.pone.0005751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen J, Xu T, Jing J, Chan RCK. Alexithymia and emotional regulation: a cluster analytical approach. BMC Psychiatry. 2011;11 [DOI] [PMC free article] [PubMed]
- 78.Costa AP, Steffgen G, Samson AC. Expressive incoherence and alexithymia in autism spectrum disorder. J Autism Dev Disord. 2017;47:1659–1672. doi: 10.1007/s10803-017-3073-9. [DOI] [PubMed] [Google Scholar]
- 79.Milosavljevic B, Carter Leno V, Simonoff E, Baird G, Pickles A, Jones CRG, et al. Alexithymia in adolescents with autism spectrum disorder: its relationship to Internalising difficulties, sensory modulation and social cognition. J Autism Dev Disord. 2016;46:1354–1367. doi: 10.1007/s10803-015-2670-8. [DOI] [PubMed] [Google Scholar]
- 80.Shah P, Catmur C, Bird G. Emotional decision-making in autism spectrum disorder: the roles of interoception and alexithymia. Mol Autism. 2016;7:43. doi: 10.1186/s13229-016-0104-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gaigg Sebastian B, Cornell Anna SF, Bird Geoffrey. The psychophysiological mechanisms of alexithymia in autism spectrum disorder. Autism. 2016;22(2):227–231. doi: 10.1177/1362361316667062. [DOI] [PubMed] [Google Scholar]
- 82.Bird G, Cook R, Mixed emotions: the contribution of alexithymia to the emotional symptoms of autism Transl Psychiatry. 2013;3:e285. doi: 10.1038/tp.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Trevisan DA, Bowering M, Birmingham E. Alexithymia, but not autism spectrum disorder, may be related to the production of emotional facial expressions. Mol Autism. 2016;7:46. doi: 10.1186/s13229-016-0108-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Salminen JK, Saarijärvi S, Ääirelä E, Tamminen T. Alexithymia-state or trait? One-year follow- up study of general hospital psychiatric consultation out-patients. J Psychosom Res. 1994;38:681–685. doi: 10.1016/0022-3999(94)90020-5. [DOI] [PubMed] [Google Scholar]
- 85.Salminen JK, Saarijärvi S, Toikka T, Kauhanen J, Äärelä E. Alexithymia behaves as a personality trait over a 5-year period in Finnish general population. J Psychosom Res. 2006;61:275–278. doi: 10.1016/j.jpsychores.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 86.Tolmunen T, Heliste M, Lehto SM, Hintikka J, Honkalampi K, Kauhanen J. Stability of alexithymia in the general population: an 11-year follow-up. Compr Psychiatry. 2011;52:536–541. doi: 10.1016/j.comppsych.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 87.Saarijärvi S, Salminen JK, Toikka T. Temporal stability of alexithymia over a five-year period in outpatients with major depression. Psychother Psychosom. 2006;75:107–112. doi: 10.1159/000090895. [DOI] [PubMed] [Google Scholar]
- 88.Baron-Cohen S, Jolliffe T, Mortimore C, Robertson M. Another advanced test of theory of mind: evidence from very high functioning adults with autism or Asperger syndrome. J Child Psychol Psychiatry Allied Discip. 1997;38:813–822. doi: 10.1111/j.1469-7610.1997.tb01599.x. [DOI] [PubMed] [Google Scholar]
- 89.Lawrence EJ, Shaw P, Baker D, Baron-Cohen S, David AS. Measuring empathy: reliability and validity of the empathy quotient. Psychol Med. 2004;34:911–919. doi: 10.1017/S0033291703001624. [DOI] [PubMed] [Google Scholar]
- 90.Chapman E, Baron-Cohen S, Auyeung B, Knickmeyer R, Taylor K, Hackett G. Fetal testosterone and empathy: evidence from the empathy quotient (EQ) and the “reading the mind in the eyes” test. Soc Neurosci. 2006;1:135–148. doi: 10.1080/17470910600992239. [DOI] [PubMed] [Google Scholar]
- 91.Oakley BFM, Brewer R, Bird G, Catmur C. Theory of mind is not theory of emotion: a cautionary note on the Reading the mind in the eyes test. J Abnorm Psychol. 2016;125:818. doi: 10.1037/abn0000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gros DF, Simms LJ, Antony MM. Psychometric properties of the state-trait inventory for cognitive and somatic anxiety (STICSA) in friendship dyads. Behav Ther. 2010;41:277–284. doi: 10.1016/j.beth.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 93.Klonsky ED, Oltmanns TF, Turkheimer E. Deliberate self-harm in a nonclinical population: prevalence and psychological correlates. Am J Psychiatry. 2003;160:1501–1508. doi: 10.1176/appi.ajp.160.8.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hawton K, Rodham K, Evans E, Weatherall R. Deliberate self harm in adolescents: self report survey in schools in England. BMJ. 2002;325:1207–1211. doi: 10.1136/bmj.325.7374.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hawton Keith, Saunders Kate EA, O'Connor Rory C. Self-harm and suicide in adolescents. The Lancet. 2012;379(9834):2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- 96.Muehlenkamp JJ, Gutierrez PM. An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide Life-Threatening Behav. 2004;34:12–23. doi: 10.1521/suli.34.1.12.27769. [DOI] [PubMed] [Google Scholar]
- 97.Gollust SE, Eisenberg D, Golberstein E. Prevalence and correlates of self-injury among university students. J Am Coll Heal. 2008;56:491–498. doi: 10.3200/JACH.56.5.491-498. [DOI] [PubMed] [Google Scholar]
- 98.Tuisku V, Pelkonen M, Karlsson L, Kiviruusu O, Holi M, Ruuttu T, et al. Suicidal ideation, deliberate self-harm behaviour and suicide attempts among adolescent outpatients with depressive mood disorders and comorbid axis I disorders. Eur Child Adolesc Psychiatry. 2006;15:199–206. doi: 10.1007/s00787-005-0522-3. [DOI] [PubMed] [Google Scholar]
- 99.Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT) Am J Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- 100.Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 101.Chartrand H, Sareen J, Toews M, Bolton JM. Suicide attempts versus nonsuicidal self-injury among individuals with anxiety disorders in a nationally representative sample. Depress Anxiety. 2012;29:172–179. doi: 10.1002/da.20882. [DOI] [PubMed] [Google Scholar]
- 102.Robledo J, Donnellan AM, Strandt-Conroy K. An exploration of sensory and movement differences from the perspective of individuals with autism. Front Integr Neurosci. 2012;6 [DOI] [PMC free article] [PubMed]
- 103.Robertson AE, Simmons DR. The sensory experiences of adults with autism spectrum disorder: a qualitative analysis. Perception. 2015;44:569–586. doi: 10.1068/p7833. [DOI] [PubMed] [Google Scholar]
- 104.Ashburner J, Bennett L, Rodger S, Ziviani J. Understanding the sensory experiences of young people with autism spectrum disorder: a preliminary investigation. Aust Occup Ther J. 2013;60:171–180. doi: 10.1111/1440-1630.12025. [DOI] [PubMed] [Google Scholar]
- 105.Pellicano E, Dinsmore A, Charman T. What should autism research focus upon? Community views and priorities from the United Kingdom. Autism. 2014;18:756–770. doi: 10.1177/1362361314529627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Parkin E, Mackley A. Mental health and suicide within the autism community. 2017. [Google Scholar]
- 107.Autistica . Personal tragedies, public crisis: the urgent need for a national response to early death in autism. 2016. [Google Scholar]
- 108.Jivraj J, Sacrey L-A, Newton A, Nicholas D, Zwaigenbaum L. Assessing the influence of researcher–partner involvement on the process and outcomes of participatory research in autism spectrum disorder and neurodevelopmental disorders: a scoping review. Autism Int J Res Pract. 2014;18:782–793. doi: 10.1177/1362361314539858. [DOI] [PubMed] [Google Scholar]
- 109.Pellicano E, Stears M. Bridging autism, science and society: moving toward an ethically informed approach to autism research. Autism Res. 2011;4:271–282. doi: 10.1002/aur.201. [DOI] [PubMed] [Google Scholar]
- 110.Wright CA, Wright SD, Diener ML, Eaton J. Autism spectrum disorder and the applied collaborative approach: a review of community based participatory research and participatory action research. J Autism. 2014;1:1. doi: 10.7243/2054-992X-1-1. [DOI] [Google Scholar]
- 111.MacLeod AG, Lewis A, Robertson C. ‘Charlie: PLEASE respond!’ Using a participatory methodology with individuals on the autism spectrum. Int J Res Method Educ. 2014;37:407–420. doi: 10.1080/1743727X.2013.776528. [DOI] [Google Scholar]
- 112.Whitlock JL, Powers JL, Eckenrode J. The virtual cutting edge: the Internet and adolescent self-injury. Dev Psychol. 2006;42:407–417. doi: 10.1037/0012-1649.42.3.407. [DOI] [PubMed] [Google Scholar]
- 113.Buser Trevor J., Buser Juleen K. Conceptualizing Nonsuicidal Self-Injury as a Process Addiction: Review of Research and Implications for Counselor Training and Practice. Journal of Addictions & Offender Counseling. 2013;34(1):16–29. doi: 10.1002/j.2161-1874.2013.00011.x. [DOI] [Google Scholar]
- 114.Sandman CA, Hetrick WP. Opiate mechanisms in self-injury. Ment Retard Dev Disabil Res Rev. 1995;1:130–136. doi: 10.1002/mrdd.1410010209. [DOI] [Google Scholar]
- 115.Victor SE, Glenn CR, Klonsky ED. Is non-suicidal self-injury an “addiction”? A comparison of craving in substance use and non-suicidal self-injury. Psychiatry Res. 2012;197:73–77. doi: 10.1016/j.psychres.2011.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Glenn CR, Klonsky ED. The role of seeing blood in non-suicidal self-injury. J Clin Psychol. 2010;66:466–473. doi: 10.1002/jclp.20661. [DOI] [PubMed] [Google Scholar]
- 117.Muehlenkamp JJ. Empirically supported treatments and general therapy guidelines for non-suicidal self-injury. J Ment Heal Couns. 2006;28:166–185. doi: 10.17744/mehc.28.2.6w61cut2lxjdg3m7. [DOI] [Google Scholar]
- 118.Cassidy SA, Bradley L, Bowen E, Rodgers J. Measurement properties of tools used to assess depression in adults with and without autism spectrum conditions: a systematic review. Autism Res. 2018;11:738–754. doi: 10.1002/aur.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cassidy SA, Bradley L, Bowen E, Wigham S, Rodgers J. Measurement properties of tools used to assess suicidality in autistic and general population adults: a systematic review. Clin Psychol Rev. 2018;62:56–70. doi: 10.1016/j.cpr.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 120.Rodgers J, Ofield A. Understanding, recognizing and treating co-occurring anxiety in autism. Curr Dev Disord Reports. 2018;5:58–64. doi: 10.1007/s40474-018-0132-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.McConachie H, Mason D, Parr JR, Garland D, Wilson C, Rodgers J. Enhancing the validity of a quality of life measure for autistic people. J Autism Dev Disord. 2018;48:1596–1611. doi: 10.1007/s10803-017-3402-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Laye-Gindhu A, Schonert-Reichl KA. Nonsuicidal self-harm among community adolescents: understanding the “whats” and “whys” of self-harm. J Youth Adolesc. 2005;34:447–457. doi: 10.1007/s10964-005-7262-z. [DOI] [Google Scholar]
- 123.Andover MS, Morris BW, Wren A, Bruzzese ME. The co-occurrence of non-suicidal self-injury and attempted suicide among adolescents: distinguishing risk factors and psychosocial correlates. Child Adolesc Psychiatry Ment Health. 2012;6:11. doi: 10.1186/1753-2000-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Claes Laurence, Soenens Bart, Vansteenkiste Maarten, Vandereycken Walter. The Scars of the Inner Critic: Perfectionism and Nonsuicidal Self-Injury in Eating Disorders. European Eating Disorders Review. 2011;20(3):196–202. doi: 10.1002/erv.1158. [DOI] [PubMed] [Google Scholar]
- 125.Gilbert P, McEwan K, Irons C, Bhundia R, Christie R, Broomhead C, et al. Self-harm in a mixed clinical population: the roles of self-criticism, shame, and social rank. Br. J. Clin. Psychol. 2010;49:563–576. doi: 10.1348/014466509X479771. [DOI] [PubMed] [Google Scholar]
- 126.Baetens I, Claes L, Hasking P, Smits D, Grietens H, Onghena P, et al. The relationship between parental expressed emotions and non-suicidal self-injury: the mediating roles of self-criticism and depression. J Child Fam Stud. 2015;24:491–498. doi: 10.1007/s10826-013-9861-8. [DOI] [Google Scholar]
- 127.Glassman LH, Weierich MR, Hooley JM, Deliberto TL, Nock MK. Child maltreatment, non-suicidal self-injury, and the mediating role of self-criticism. Behav Res Ther. 2007;45:2483–2490. doi: 10.1016/j.brat.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cawood CD, Huprich SK. Late adolescent nonsuicidal self-injury: the roles of coping style, self-esteem, and personality pathology. J Pers Disord. 2011;25:765–781. doi: 10.1521/pedi.2011.25.6.765. [DOI] [PubMed] [Google Scholar]
- 129.Washburn JJ, Richardt SL, Styer DM, Gebhardt M, Juzwin KR, Yourek A, Aldridge D. Psychotherapeutic approaches to non-suicidal self-injury in adolescents. Child Adolesc Psychiatry Ment Health. 2012;6(1):14. [DOI] [PMC free article] [PubMed]
- 130.Gonzales AH, Bergstrom L. Adolescent non-suicidal self-injury (NSSI) interventions. J Child Adolesc Psychiatr Nurs. 2013;26:124–130. doi: 10.1111/jcap.12035. [DOI] [PubMed] [Google Scholar]
- 131.Lang Russell, O’Reilly Mark, Healy Olive, Rispoli Mandy, Lydon Helena, Streusand William, Davis Tonya, Kang Soyeon, Sigafoos Jeff, Lancioni Giulio, Didden Robert, Giesbers Sanne. Sensory integration therapy for autism spectrum disorders: A systematic review. Research in Autism Spectrum Disorders. 2012;6(3):1004–1018. doi: 10.1016/j.rasd.2012.01.006. [DOI] [Google Scholar]
- 132.Case-Smith Jane, Weaver Lindy L, Fristad Mary A. A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism. 2014;19(2):133–148. doi: 10.1177/1362361313517762. [DOI] [PubMed] [Google Scholar]
- 133.Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, Dilavore PC, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–223. doi: 10.1023/A:1005592401947. [DOI] [PubMed] [Google Scholar]
- 134.Rosbrook A, Whittingham K. Autistic traits in the general population: what mediates the link with depressive and anxious symptomatology? Res Autism Spectr Disord. 2010;4:415–424. doi: 10.1016/j.rasd.2009.10.012. [DOI] [Google Scholar]
- 135.Strang JF, Kenworthy L, Daniolos P, Case L, Wills MC, Martin A, et al. Depression and anxiety symptoms in children and adolescents with autism spectrum disorders without intellectual disability. Res Autism Spectr Disord. 2012;6:406–412. doi: 10.1016/j.rasd.2011.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mazzone L, Ruta L, Reale L. Psychiatric comorbidities in asperger syndrome and high functioning autism: diagnostic challenges. Ann General Psychiatry. 2012; [DOI] [PMC free article] [PubMed]
- 137.Steer RA, Clark DA, Kumar G, Beck AT. Common and specific dimensions of self-reported anxiety and depression in adolescent outpatients. J Psychopathol Behav Assess. 2008;30:163–170. doi: 10.1007/s10862-007-9060-2. [DOI] [Google Scholar]
- 138.Allely CS. Pain sensitivity and observer perception of pain in individuals with autistic spectrum disorder. Sci World J. 2013; [DOI] [PMC free article] [PubMed]
- 139.Moore David J. Acute pain experience in individuals with autism spectrum disorders: A review. Autism. 2014;19(4):387–399. doi: 10.1177/1362361314527839. [DOI] [PubMed] [Google Scholar]
- 140.Yasuda Y, Hashimoto R, Nakae A, Kang H, Ohi K, Yamamori H, et al. Sensory cognitive abnormalities of pain in autism spectrum disorder: a case-control study. Ann General Psychiatry. 2016; [DOI] [PMC free article] [PubMed]
- 141.Shah P, Hall R, Catmur C, Bird G. Alexithymia, not autism, is associated with impaired interoception. Cortex. 2016;81:215–220. doi: 10.1016/j.cortex.2016.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kenny L, Hattersley C, Molins B, Buckley C, Povey C, Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. 2016;20:442–462. doi: 10.1177/1362361315588200. [DOI] [PubMed] [Google Scholar]
- 143.Sornberger MJ, Heath NL, Toste JR, McLouth R. Nonsuicidal self-injury and gender: patterns of prevalence, methods, and locations among adolescents. Suicide Life-Threatening Behav. 2012;42:266–278. doi: 10.1111/j.1943-278X.2012.0088.x. [DOI] [PubMed] [Google Scholar]
- 144.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Pearson correlation coefficients between predictor variables. Table S2 Qualitative analysis: Experiences with therapy. Table S3 Qualitative analysis: what others should know about NSSI. (DOCX 45 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.