Abstract
Background:
Positive-pressure air arthrography and venting of the hip capsule are techniques used to decrease the traction forces needed for joint distraction during hip arthroscopic surgery. Little is known about the effects that these techniques have on postoperative pain.
Hypothesis:
Positive-pressure air arthrography and venting during hip arthroscopic surgery will decrease patient-reported pain and narcotic requirements in the acute postoperative setting.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective cohort analysis was conducted to analyze 35 patients who underwent positive-pressure air arthrography and venting to aid joint distraction during hip arthroscopic surgery versus a group with similar demographics, pathologies, and treatments who did not undergo air arthrography. Numeric pain rating scale (NPRS) scores and medication administration including narcotic and nonnarcotic analgesia in the postanesthesia care unit (PACU) were tracked and compared.
Results:
The maximum (7.17 vs 4.97, respectively), minimum (2.43 vs 1.09, respectively), and mean (5.15 vs 3.11, respectively) NPRS scores were all higher in the control group compared with the air arthrogram group (P < .001, P = .007, and P < .001, respectively). The administration of oral morphine equivalents (OMEs) during the PACU stay was significantly lower in the air arthrogram group, with a mean of 36.75 ± 11.37 OMEs, compared with 44.53 ± 16.06 OMEs in the control group (P = .023). There was no difference in postoperative nonopioid medications, such as ketorolac or acetaminophen, given between groups.
Conclusion:
Patients undergoing hip arthroscopic surgery with air arthrography and venting used to aid distraction had significantly less postoperative pain and required a lower total dosage of opioids during their PACU stay when compared with patients who underwent hip arthroscopic surgery without air arthrography.
Keywords: hip arthroscopic surgery, venting; pain, narcotics
The arthroscopic management of hip abnormalities has been steadily increasing over the past decade.6,8,15 This increase is in part driven by high levels of patient satisfaction and return to sport at both short-term and midterm follow-up after hip arthroscopic surgery for femoroacetabular impingement (FAI).7,9 Compared with knee and shoulder arthroscopic surgery, arthroscopic techniques to manage hip abnormalities are relatively new. Unlike knee and shoulder arthroscopic surgery, hip arthroscopic surgery requires joint distraction for adequate visualization and access to the joint to avoid iatrogenic chondral and/or labral damage. Joint distraction may be a source of postoperative hip pain, but there is little research on techniques to improve postoperative pain after hip arthroscopic surgery.2
During routine hip arthroscopic surgery, adequate visualization is often obtained by applying gross and fine traction on the operative leg with a traction table. Prolonged traction or forceful distraction can lead to a number of complications, including pain and pudendal nerve injuries.12 Some authors have advocated introducing a needle into the joint before joint distraction, to allow pressure equilibration or “venting” of the hip capsule or positive-pressure air arthrography.14 These techniques break the negative pressure seal of the joint and allow for increased ease of distraction.14 To date, little or no research has specifically compared the effect of using an air arthrogram on patient pain after hip arthroscopic surgery.
The purpose of this study was to assess if using a positive-pressure air arthrogram decreases postoperative pain and analgesia requirements. To determine this, a matched-cohort analysis comparing numeric pain rating scale (NPRS) scores and opioid use in the postanesthesia care unit (PACU) in patients undergoing hip arthroscopic surgery for FAI with and without the use of an air arthrogram was performed. We hypothesized that the use of an air arthrogram will decrease postoperative pain as well as opioid use.
Methods
Patients undergoing hip arthroscopic surgery by a sports medicine fellowship–trained orthopaedic surgeon with a focus on hip preservation (A.L.Z.) at a single academic institution were prospectively enrolled in a secure database. Database records were retrospectively reviewed, and 2 groups were established. Thirty-five patients undergoing primary hip arthroscopic surgery for FAI with the use of an air arthrogram during hip distraction were matched by age, sex, body mass index (BMI), and abnormality to 35 patients who did not receive an air arthrogram during similar procedures. The appropriate institutional review board approved the study protocol, and all patients provided written consent before enrollment.
Inclusion criteria included patients with symptomatic FAI with failure of conservative management and physical therapy who consented to participate in the study and underwent surgery within a 15-month time period. All patients had undergone a minimum of 6 weeks of conservative management before the surgical intervention. Exclusion criteria included patients with osteoarthritis (Tönnis grade ≥2), hypermobility (Beighton score ≥4), and age older than 65 years. The primary outcomes evaluated were traction-related perioperative complications; maximum, minimum, and mean NPRS scores; and opioid medications administered in the PACU. Secondary outcomes included nonnarcotic analgesia administration and time from admission to discharge.
Patient demographics, including sex, age, and BMI, as well as radiographic findings were recorded along with intraoperative variables, complications, and medications administered. All patients underwent a preoperative radiographic evaluation, which included radiographs of the pelvis in the supine anteroposterior view and Dunn lateral 45° view, in addition to magnetic resonance imaging of the affected side.20 Radiographic measurements including the alpha angle and lateral center-edge angle were collected. Intraoperative variables recorded included procedures performed, cartilage condition, time spent in traction, and total procedure time.3 Intraoperative pain medications given by anesthesia were standardized for both groups.
To compare opioid administration between patients in the setting of multiple different narcotics and administration routes, a standardized calculation was used to convert all PACU narcotics administered into oral morphine equivalents (OMEs).19 All opioid administration data were recorded by PACU nursing staff and documented in the electronic medical record. Narcotic analgesia was administered for a pain score greater than 5 or for tachycardia, hypertension, or visible discomfort in patients not yet awake enough to report their pain score.
Surgical Technique
General anesthesia was used in all cases, and intraoperative medications were standardized across all patients. All patients underwent hip arthroscopic surgery on a standard hip distractor attachment table. The uninjured leg and operative leg were appropriately padded and placed into traction boots, and a well-padded perineal post was used. The hip was positioned in neutral without flexion or extension and without internal or external rotation. Gentle gross traction was performed to remove any slack from the knee joint so that the leg was suspended with the knee in extension but without any distraction of the hip joint.
After sterile preparation and draping, the hip capsule was entered anteriorly through the anterolateral portal with a sterile 17-gauge hip-length spinal needle under fluoroscopic guidance (Figure 1). Entry was away from the labrum and weightbearing articular cartilage to avoid iatrogenic injuries to these structures.
Figure 1.
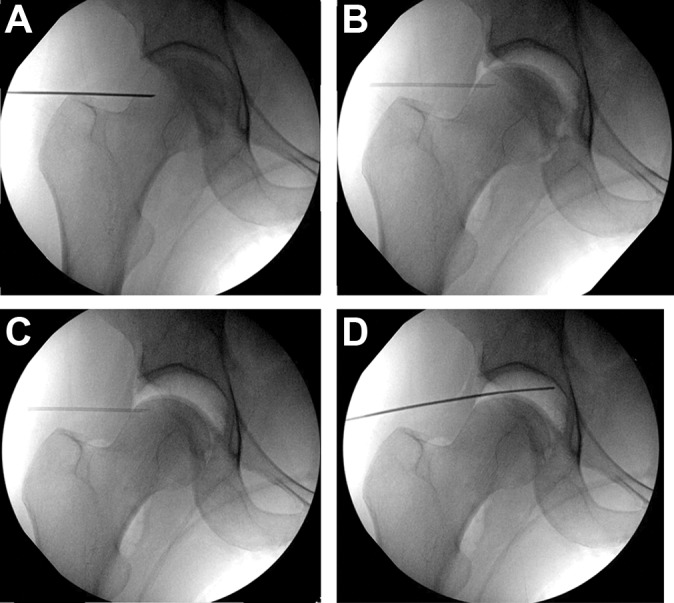
(A) A 17-gauge spinal needle is used to penetrate the hip joint capsule anteriorly, away from the labrum and weightbearing articular surface to reduce the risk of iatrogenic injuries. (B) Afterward, 25 mL of air is injected through the spinal needle. The subsequent air arthrogram confirms the intra-articular position, breaks the suction seal of the hip joint, and aids in distraction. (C) After 10 turns of fine traction is applied, the hip joint easily distracts, allowing a safe space for instrumentation without damage to the labrum or articular cartilage. (D) Redirecting the spinal needle allows a pathway for instrumentation into the joint over a guide wire, with continued fluoroscopic guidance until the arthroscope is inserted and the remainder of the procedure can be directly visualized.
Air Arthrogram Group
After localization, 25 mL of air was then injected into the joint with a sterile syringe to provide positive pressure, breaking the negative suction seal of the hip joint. Fluoroscopy was used to confirm the intra-articular position by identifying an appropriate air arthrogram site, after which the syringe was removed from the needle, allowing pressure neutralization or “venting” to occur. Fine traction was then placed on the hip, with 10 turns typically needed for adequate joint distraction before dilators and arthroscopic instruments were used for standard hip arthroscopic entry through the anterolateral and midanterior portals.
Control Group
Gross traction using the distractor and padded post was placed on the operative hip before sterile preparation and draping, followed by fine traction as needed (typically 25-30 turns) until a visible/audible pop occurred, indicating hip joint distraction. Fluoroscopy was used to evaluate the joint for adequate distraction, after which the spinal needle was used to enter the joint and a similar process of instrumentation performed.
At the end of the procedure, patients from both groups were given a 10-mL injection of 0.2% ropivacaine intra-articularly before portal closure.
Statistical Analysis
An unpaired Student t test was used to calculate the statistical significance between the 2 groups for mean values such as age, traction time, and medication administration. The Pearson chi-square test was used for categorical values such as sex and affected hip laterality. A P value <.05 was considered statistically significant. All statistical computations were conducted in StatPlus:mac (v 6; AnalystSoft). An a priori power analysis was performed based on the results of previous literature on pain scores after hip arthroscopic surgery.10 It was determined that a minimum of 26 patients per group was required to power the study to 1 – β = 0.80, and therefore, groups of 35 patients each were selected to ensure adequate power. A post hoc power analysis conducted for the postoperative pain scores between the 2 groups resulted in a power value of 100%.
Results
The demographics and intraoperative findings for the control and air arthrogram groups are shown in Table 1. There was no statistical difference between groups in demographics, including sex, laterality, age, or BMI. No statistical difference was present with regard to preoperative radiographic measurements, including the alpha angle or lateral center-edge angle. Intraoperative findings, including mean traction time (63.6 ± 19.1 vs 63.2 ± 21.2 minutes, respectively; P = .939) and mean procedure time (110.8 ± 23.7 vs 103.3 ± 24.3 minutes, respectively; P = .197) were also similar between the control and air arthrogram groups. Thirty-four of 35 (97.14%) patients in the control group and 35 of 35 (100.00%) patients in the air arthrogram group had labral tears identified at the time of arthroscopic surgery. In the control group, 8 of the 35 patients (22.86%) were on short-acting narcotic analgesia preoperatively, compared with 7 of 35 patients (20.00%) in the air arthrogram group (P = .771). No patients in either group were on long-acting narcotic medications before surgery.
TABLE 1.
Demographics and Intraoperative Findingsa
| Control | Air Arthrogram | P b | |
|---|---|---|---|
| Demographics | |||
| Sex | .229 | ||
| Male | 17 | 22 | |
| Female | 18 | 13 | |
| Side involved | .322 | ||
| Right | 24 | 20 | |
| Left | 11 | 15 | |
| Age, y | 37.3 ± 10.6 | 34.3 ± 9.9 | .208 |
| BMI, kg/m2 | 26.2 ± 4.7 | 24.4 ± 3.5 | .063 |
| Alpha angle, deg | 62.2 ± 5.7 | 59.8 ± 4.9 | .066 |
| Lateral center-edge angle, deg | 34.6 ± 7.1 | 34.1 ± 6.4 | .752 |
| Labral tears | 34 | 35 | .314 |
| Preoperative narcotic use | 8 | 7 | .771 |
| Intraoperative findings | |||
| Wave sign | 23 | 22 | |
| Median acetabular cartilage condition | 3 | 3 | |
| Median femoral cartilage condition | 2 | 2 | |
| Median labral condition | 3 | 3 | |
| Cam resection (femoroplasty) | 35 | 35 | |
| Pincer resection (acetabuloplasty) | 22 | 25 | |
| Labral repair | 32 | 33 | |
| Labral debridement | 2 | 2 | |
| Microfracture | 2 | 1 | |
| Chondroplasty | 0 | 1 | |
| Traction time, min | 63.6 ± 19.1 | 63.2 ± 21.2 | .939 |
| Procedure time, min | 110.8 ± 23.7 | 103.3 ± 24.3 | .197 |
aData are reported as mean ± SD or counts. BMI, body mass index.
bStudent unpaired-samples t test for mean values and chi-square test for categorical values.
The study outcomes are presented in Table 2. The only traction-related complication occurring in either group was transient pudendal nerve palsy lasting for 3 weeks in 1 patient of the control group, and this difference between groups was not statistically significant. The maximum (7.17 vs 4.97, respectively), minimum (2.43 vs 1.09, respectively), and mean (5.15 vs 3.11, respectively) NPRS scores were all statistically significantly different between the control and air arthrogram groups (P < .001, P = .007, and P < .001, respectively). Opioid administration during the PACU stay was significantly lower in the air arthrogram group, with a mean of 36.75 ± 11.37 OMEs versus 44.53 ± 16.06 OMEs administered for the control group (P = .023). The rate of nonnarcotic analgesia administration was not significantly different between groups and included both acetaminophen and ketorolac. In addition, the total length of stay from admission to PACU discharge was similar for both groups.
TABLE 2.
NPRS Scores and Medications Administereda
| Control | Air Arthrogram | P | |
|---|---|---|---|
| Postoperative NPRS scores | |||
| Minimum | 2.43 ± 2.37 | 1.09 ± 1.56 | .007 |
| Maximum | 7.17 ± 1.79 | 4.97 ± 1.89 | <.001 |
| Mean | 5.15 ± 1.68 | 3.11 ± 1.28 | <.001 |
| Medications | |||
| Oral morphine equivalents | 44.53 ± 16.06 | 36.75 ± 11.37 | .023 |
| Acetaminophen, mg | 515.00 ± 373.59 | 396.43 ± 275.01 | .136 |
| Ketorolac, mg | 8.57 ± 13.75 | 6.00 ± 12.18 | .41 |
aData are reported as mean ± SD. Bolded P values indicate statistically significant difference between groups (P < .05). NPRS, numeric pain rating scale.
Discussion
The primary goal of this study was to evaluate the effects of a positive-pressure air arthrogram on patient-reported pain scores after hip arthroscopic surgery. The elimination of the negative pressure seal of the hip joint using venting without air arthrography has been studied and is known to provide increased joint distraction at equal traction forces.11 This study adds to the literature by assessing the effect of the air arthrography technique in addition to venting on postoperative pain and narcotic requirements. We hypothesized that not only will an air arthrogram vent the joint, but a positive-pressure application of air into the joint will also help to further decrease surface tension and facilitate distraction. In performing this matched-cohort analysis, we found that patients undergoing hip arthroscopic surgery with air arthrography had significantly less postoperative pain and required a lower total dosage of opioids during their PACU stay when compared with patients who underwent hip arthroscopic surgery without air arthrography during distraction.
The 2 groups in this study were matched by abnormalities, procedures, and demographics. There was no significant difference with regard to their nonnarcotic analgesia. The between-group differences in NPRS scores were most notable regarding maximum pain (2.20) and mean pain (2.04) but were slightly less with respect to minimum pain (1.34). All of these, however, were greater than the minimal clinically important difference for acute pain in the hospital setting (1.3) as established by Bijur et al.5 The difference in OMEs between groups was 7.78, equivalent to approximately 5 mg of oral oxycodone or nearly 0.5 mg of hydromorphone less in the air arthrogram group.19 Decreased opioid use in the PACU may be associated with decreased opioid use after discharge, which is important in battling the current opioid epidemic.13
Techniques to decrease postoperative pain in hip arthroscopic surgery are imperative. Unlike shoulder, elbow, knee, and ankle arthroscopic surgery, there is little benefit to standard regional nerve blocks.4 The joint also requires greater forces to distract because of its thick capsule. Prolonged and greater traction is associated with an increased risk of pudendal nerve palsy17,18 and should therefore be limited. Furthermore, prolonged postoperative narcotic use has been tied to worse outcomes after hip arthroscopic surgery.1 Other valuable techniques have also been described, including hip arthroscopic surgery without a perineal post,17,18 which may work well in conjunction with the air arthrography technique. It is important for surgeons to continue to develop safe and reliable techniques to minimize postoperative pain and traction-related complications after hip arthroscopic surgery.2,12,13
The use of air arthrography or “venting” has been described as a technical pearl to aid in distraction of the hip joint.16,21 The strength and thickness of the hip capsule, combined with a patient population that tends to be young, healthy, and active, make distraction of the joint difficult. It is likely that by breaking the native vacuum suction seal of the hip joint with positive pressure, the hip distracts more easily, with less force on the soft tissue and surrounding musculature. Additionally, there is less force exerted in the perineal region as a result of decreased pressure against the perineal post. In contrast, manually distracting the joint with gross and fine traction may require increased force on the hip musculature as well as perineal area to overcome a tight negative suction seal on the hip. Therefore, using an air arthrogram may produce the effects of decreased immediate postoperative pain and narcotic requirements because of the reduced force needed on the leg to achieve adequate joint distraction.
This study is not without limitations. It was a single-surgeon, single-institution study, and because it was a retrospective review of a prospectively collected database, there was no randomization of patients. There was no group for whom venting alone was tested against positive-pressure air arthrography, and thus, the two can only be compared as a single combined strategy against traction without countermeasures to eliminate the suction seal of the hip. In addition, there is not a reliable record of patient narcotic or nonnarcotic analgesia requirements after discharge from the PACU. However, the goal of this study was to evaluate the immediate postoperative effects of using the air arthrography technique during hip arthroscopic surgery. Longer term outcomes after discharge from the PACU may be related to other factors, such as rehabilitation, that are more difficult to control for, but it is a goal of future studies to better examine this aspect. Future areas of research may also include larger multicenter studies to evaluate the effect of air arthrography on pudendal nerve palsy rates, as they are typically too infrequent to adequately power for an analysis at a single institution.
Conclusion
Patients undergoing hip arthroscopic surgery with air arthrography and venting used to aid distraction had significantly less self-reported postoperative pain and required a lower total dosage of opioids during their PACU stay when compared with patients who underwent hip arthroscopic surgery without air arthrography.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.D.H. has received reimbursement for educational material written for Johnson & Johnson. A.L.Z. has received consulting fees from Stryker, research support from Zimmer, and educational support from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of California–San Francisco Institutional Review Board (No. 14-14742).
References
- 1. Anciano Granadilo V, Cancienne JM, Gwathmey FW, Werner BC. Perioperative opioid analgesics and hip arthroscopy: trends, risk factors for prolonged use, and complications. Arthroscopy. 2018;34(8):2359–2367. [DOI] [PubMed] [Google Scholar]
- 2. Baker JF, Byrne DP, Hunter K, Mulhall KJ. Post-operative opiate requirements after hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2011;19:1399–1402. [DOI] [PubMed] [Google Scholar]
- 3. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. [DOI] [PubMed] [Google Scholar]
- 4. Behrends M, Yap EN, Zhang AL, et al. Preoperative fascia iliaca block does not improve analgesia after arthroscopic hip surgery, but causes quadriceps muscles weakness: a randomized, double-blind trial. Anesthesiology. 2018;129(3):536–543. [DOI] [PubMed] [Google Scholar]
- 5. Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10(4):390–392. [DOI] [PubMed] [Google Scholar]
- 6. Bonazza N, Liu G, Leslie D, Dhawan A. Surgical trends in arthroscopic hip surgery using a large national database. Orthop J Sports Med. 2017;5(7 suppl 6):2325967117S00406. [DOI] [PubMed] [Google Scholar]
- 7. Boykin RE, Patterson D, Briggs KK, Dee A, Philippon MJ. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med. 2013;41:2296–2301. [DOI] [PubMed] [Google Scholar]
- 8. Bozic KJ, Chan V, Valone FH, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(suppl 8):140–143. [DOI] [PubMed] [Google Scholar]
- 9. Byrd JWT. Femoroacetabular impingement in athletes: current concepts. Am J Sports Med. 2014;42:737–751. [DOI] [PubMed] [Google Scholar]
- 10. Childs S, Pyne S, Nandra K, Bakhsh W, Mustafa SA, Giordano BD. The effect of intra-articular cocktail versus femoral nerve block for patients undergoing hip arthroscopy. Arthroscopy. 2017;33(12):2170–2176. [DOI] [PubMed] [Google Scholar]
- 11. Dienst M, Seil R, Godde S, et al. Effects of traction, distension, and joint position on distraction of the hip joint: an experimental study in cadavers. Arthroscopy. 2002;18(8):865–871. [DOI] [PubMed] [Google Scholar]
- 12. Frandsen L, Lund B, Grønbech Nielsen T, Lind M. Traction-related problems after hip arthroscopy. J Hip Preserv Surg. 2017;4(1):54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Luo J, Min S. Postoperative pain management in the postanesthesia care unit: an update. J Pain Res. 2017;10:2687–2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mannava S, Howse EA, Stone AV, Stubbs AJ. Basic hip arthroscopy: supine patient positioning and dynamic fluoroscopic evaluation. Arthrosc Tech. 2015;4(4):e391–e396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maradit Kremers H, Schilz SR, Van Houten HK, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. 2017;32:750–755. [DOI] [PubMed] [Google Scholar]
- 16. Matsuda DK, Gupta N, Hanami D. Hip arthroscopy for challenging deformities: global pincer femoroacetabular impingement. Arthrosc Tech. 2014;3(2):e197–e204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mei-Dan O, Kraeutler MJ, Garabekyan T, Goodrich JA, Young DA. Hip distraction without a perineal post: a prospective study of 1000 hip arthroscopy patients. Am J Sports Med. 2018;46(3):632–641. [DOI] [PubMed] [Google Scholar]
- 18. Merrell G, Medvecky M, Daigneault J, Jokl P. Hip arthroscopy without a perineal post: a safer technique for hip distraction. Arthroscopy. 2007;23(1):107. [DOI] [PubMed] [Google Scholar]
- 19. Neilsen S, Degenhardt L, Hoban B, Gisev N. A synthesis of oral morphine equivalents (OME) for opioid utilization studies. Pharmacoepidemiol Drug Saf. 2016;25:733–737. [DOI] [PubMed] [Google Scholar]
- 20. Pfirrmann CWA, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240(3):778–785. [DOI] [PubMed] [Google Scholar]
- 21. Thomas J, Ross JR, Salata MJ, Bancroft R, Bedi A. Synovial-based disorders In: Wiesel SW, ed. Operative Techniques in Orthopedics. 2nd ed Philadelphia: Wolters-Kluwer; 2016:264–275. [Google Scholar]


