Abstract
Introduction
Inhaled nitric oxide (iNO) is a selective pulmonary vasodilator with limited indications in adults. We present a patient with hypoxemia and right ventricular dysfunction due to submassive acute pulmonary emboli where iNO was used as a bridge to thrombolysis.
Case
A 29-year-old male was admitted to the intensive care unit (ICU) for alcohol intoxication complicated with aspiration pneumonia and acute respiratory failure requiring mechanical ventilation. His medical history included morbid obesity (BMI 43) and alcohol dependence syndrome. Nine days after admission, he developed severe acute hypoxia and tachycardia with arterial oxygen tension (PaO2) of 52 mmHg requiring a positive end-expiratory pressure (PEEP) of 14 cmH2O and fraction of inspired oxygen (FiO2) of 1. Chest computed tomography (CT) revealed a large embolus in the right main pulmonary artery and transthoracic echocardiogram (TTE) reported new right ventricular dilatation with decreased right ventricular function. Due to the severe hypoxemia, he was started on iNO via the breathing circuit of the ventilator at a concentration of 20 parts per million (ppm) with steady improvement in oxygenation after 1 hour with a PaO2 of 81 mmHg on the same ventilator setting. The patient was given thrombolysis with alteplase and the iNO was slowly tapered off during the subsequent four days with concomitant successful tapering of PEEP to 8 cmH2O and FiO2 of 0.45.
Conclusion
Inhaled NO has been used to improve ventilation-perfusion matching and also to reduce pulmonary vascular resistance (PVR). Its effects on PVR may be useful in the setting of acute pulmonary emboli where vascular obstruction and vasoconstriction contribute to increased pulmonary arterial pressure and PVR which can present as acute right heart failure. We suggest that iNO, if available, could be considered in those patients with acute pulmonary emboli associated with significant hypoxemia as an adjunctive therapy or bridge to thrombolysis or thrombectomy.
1. Introduction
Nitric oxide (NO) is a naturally occurring gas, and at room temperature, it is both colorless and odorless, and when added to an inspired gas, it produces selective pulmonary vasodilation which improves pulmonary hypertension and decreases right ventricular (RV) afterload [1, 2]. This potent endogenous vasodilator can be exogenously administered via inhalation. Use of iNO in adults remains controversial. We present a patient with severe hypoxemia and acute right ventricular dysfunction due to a submassive acute pulmonary emboli where iNO was used as a bridge to diagnosis and thrombolysis.
2. Case
A 29-year-old male was admitted to the intensive care unit with acute respiratory failure requiring intubation in the field. The patient was found unresponsive on the floor of his apartment. His medical history included morbid obesity with a body mass index of 43 kg/m2 and alcohol dependence syndrome.
On initial examination he was sedated on mechanical ventilation, afebrile (98 F), hypertensive with a blood pressure of 167/69 mmHg, tachycardic with heart rate of 111 beats per minute and a respiratory rate of 20 breaths per minute synchronous to the set rate on the ventilator. Peripheral capillary oxygen saturation (SPO2) was 98% with inspired oxygen saturation (FiO2) of 0.5. Lung examination revealed rales in the mid and lower zones of the right lung field. Cardiac examination revealed tachycardia with no murmurs. Abdominal, neurologic and skin exams were unremarkable.
Relevant laboratory on admission included the following: leukocytosis (white cell count of 11.2 × 103 cells/ /μL), serum creatinine of 2.1 mg/dL (baseline 0.6 mg/dL), serum creatine kinase of 39, 552 units/L, serum lactic acid of 4.2 mmoles/L, and serum ethanol level of 316 mg/dL. Initial arterial blood gas analysis revealed a pH of 7.26, an arterial carbon dioxide (PCO2) level of 40.2 mmHg and oxygen level (PO2) of 108 mmHg on a FiO2 of 0.5, and positive end-expiratory pressure (PEEP) of 5. Chest X-ray (CXR) showed right upper, middle, and lower lobe infiltrates and computed tomography (CT) of the head demonstrated no acute infarcts or hemorrhage.
He was started on broad spectrum antibiotics including vancomycin, piperacillin-tazobactam, and azithromycin for pneumonia. On day 2 of admission, the patient underwent fiberoptic bronchoscopy which revealed thick mucopurulent secretions in all segments of right lung. The respiratory cultures from bronchoalveolar lavage were negative as well as initial blood and urine cultures. Transthoracic echocardiogram (TTE) on day 2 revealed an ejection fraction of 57% with normal right ventricular structure and function and normal pulmonary artery systolic pressure (PASP). The patient clinically and radiologically improved, he was awake and tolerating daily spontaneous breathing trials with FiO2 requirements of 0.4 to keep PO2 of 104.
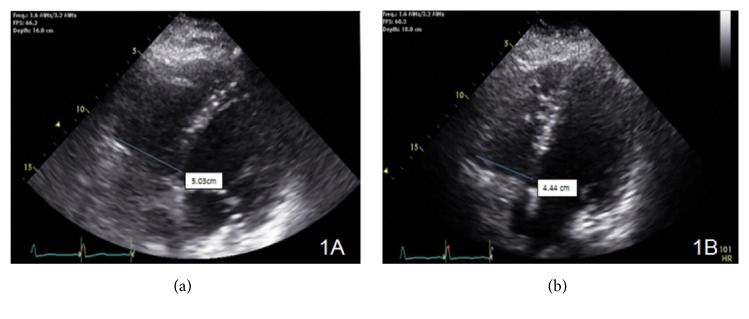
On day nine of admission, he was noted to be hypoxic with a PO2 of 52 mmHg with a SPO2 of 88%. He required a PEEP of 14 cmH20 and a FiO2 of 1 to achieve a PO2 of 66 mmHg. Due to body habitus prone position was not an option. Repeated CXR did not show any new abnormalities- resolving right-side infiltrates. In addition to the subcutaneous heparin started on admission for deep venous thrombosis (DVT) prophylaxis, a therapeutic dose of low molecular weight heparin (LMWH) at 1 mg/kg was administered with a presumptive diagnosis of acute pulmonary emboli as he was too unstable for transportation to radiology. A repeat TTE showed a PASP of 54 mmHg with new moderate dilatation of the RV and moderate tricuspid regurgitation (Figure 1(a)) with a serum troponin T of 0.204 ng/mL and proBNP of 445 pg/mL. Inhaled nitric oxide (iNO) was given via the breathing circuit of the mechanical ventilator at a concentration of 20 parts per million (ppm) with improved oxygenation noted after one hour, PO2 increased to 81 mmHg with a FiO2 of 0.8. His blood pressure during this time ranged from a systolic of 117-134 mmHg and diastolic of 68–87 mmHg.
Figure 1.
(a) Right ventricular size and function assessment was done with RV focused imaging from apical four chamber view. Initial measurement showed 5.03 cm RV basal diameter consistent with moderately dilated RV size. 2D images also showed reduced RV ejection fraction along with RV strain findings. (b) Right ventricular size and function assessment was done with RV focused imaging from apical four chamber view. RV basal diameter is measured as 4.44 cm which was consistent with mildly dilated RV size. RV ejection fraction is improved, and RV strain findings were no longer available.
Chest CT angiogram revealed large embolus in the right main pulmonary artery (Figure 2). Thrombolytic therapy with alteplase at 100 mg was administered over two hours and the iNO was slowly tapered off over the next four days with concomitant tapering of PEEP to 8 cmH20 and FiO2 of 0.45. Repeat TTE three days after thrombolytic therapy demonstrated a PASP of 32 mmHg with mild dilation of the RV without signs of strain (Figure 1(b)). The patient was weaned from mechanical ventilation and later discharged to a skilled nursing facility for rehabilitation on oral apixaban for three months with outpatient follow-up provided.
Figure 2.
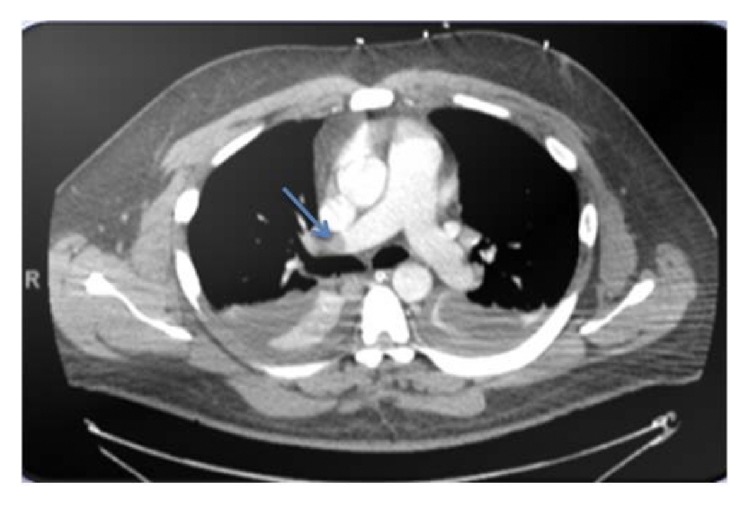
CT Chest demonstrating embolus in the right main pulmonary artery.
3. Discussion
Nitric oxide (NO) is a naturally occurring gas and at room temperature it is both colorless and odorless. It is produced endogenously from L-arginine by NO synthase and when added to an inspired gas, it produces selective pulmonary vasodilation. It activates guanylate cyclase which then activates cyclic guanosine monophosphate (cGMP). Cyclic GMP stimulates cGMP-dependent protein kinase that activates myosin light chain phosphatase, which dephosphorylates myosin light chains, leading to smooth muscle relaxation. Additionally, increased intracellular cGMP inhibits calcium entry into the cell, and decreases intracellular calcium concentrations further promoting relaxation of vascular smooth muscle [3]. In the lung it acts selectively on the pulmonary vasculature because of rapid hemoglobin-mediated inactivation as it diffuses into the pulmonary capillaries [1]. With the relaxation of the pulmonary vessels, iNO reduces pulmonary vascular resistance which translates to lower pulmonary arterial pressures and reduced right ventricular (RV) afterload [2].
There are limited therapeutic indications for iNO in adults. Currently in the United States, it is licensed only for neonates with respiratory failure and persistent pulmonary hypertension. In adults, it has an established diagnostic role in vasodilator testing in patients with pulmonary arterial hypertension. iNO has been studied in patients with acute respiratory distress syndrome (ARDS) but with conflicting results. A meta-analysis by Sokol et al. reviewed five randomized control trials with a combined total of 535 patients with acute hypoxemic respiratory failure and found no significant effect in mortality with only transient improvement in oxygenation [4]. The use of Inhaled NO in adults is based on its ability to provide selective pulmonary vasodilatation in well- ventilated lung units, to improve ventilation-perfusion mismatch and subsequently to reduce the elevated pulmonary vascular resistance and pulmonary hypertension as seen in ARDS [5]. In addition, iNO has been used in RV failure associated with cardiac surgery and sickle cell disease [6].
The estimated incidence of PE in the United States in one analysis looking at patients from 1998-2006 was 112 per 100, 000 adults with a 7.8% mortality rate [7]. Several studies have found that the presence of RV dysfunction portends a worse prognosis with at least a 2-fold increased risk of death [8–12]. An experimental model looking at pulmonary vascular reserve during experimental PE noted that increased PVR was caused to a minor degree by direct mechanical obstruction and to a greater extent by vasoconstriction [13]. A sudden increase in the RV systolic pressure caused by an acute PE promotes turbulent flow across the tricuspid and pulmonic valves leading to hemolysis and release of heme (which deactivates NO) and arginase-1, reducing L- arginine levels needed for NO production. Additionally, trapped platelets release thromboxane A2 and serotonin which are potent vasoactive mediators [14–17]. Overall, reduced levels of NO in the presence of vasoactive substances further increase pulmonary vascular resistance and RV pressures in an acute PE.
Assessing RV function is essential in the risk stratification of acute PE. In our case, we highlighted acute right ventricular dilatation with moderate tricuspid regurgitation. An emerging echocardiographic marker for patients with intermediate risk PE is the ratio of tricuspid regurgitation peak gradient (TRPG) to tricuspid annulus plane systolic excursion (TAPSE) or TRPG/TAPSE. A TAPSE of < 17 mmHg is suggestive of RV systolic dysfunction but when interpreted as a ratio to TRPG, a group of Polish researchers were able to demonstrate that a TRPG/TAPSE > 4.5 was associated with 21.1% risk of PE-related death or rescue thrombolysis [18]. This echo parameter may be of added prognostic value especially when combined with conventional parameters of RV function.
There are case reports of successful use of iNO as a therapeutic agent in patients with acute pulmonary embolism (PE). Inhaled nitric oxide may have a unique role as an adjunct to existing standard of care including anticoagulation, thrombolytics and surgery in the patient with acute PE and severe hypoxia, acute RV failure or hemodynamic instability. Its role as a selective pulmonary vasodilator may reduce RV afterload without causing systemic vasodilation which is beneficial in these critically ill patients. There are case reports of successful use of iNO as a therapeutic agent in patients with acute pulmonary embolism (PE) [19]. A review of 18 patient with acute PE receiving iNO at a dose of 10 to 50 ppm for up to 6 days revealed that 14 (78%) patients had improvement in mean arterial pressure, 16 (89%) had significant improvement in oxygenation and 14 (78%) survived hospital admission. All of the patients were anticoagulated, 12 received thrombolytic therapy and 6 received either mechanical embolectomy or intra-arterial thrombolysis [20]
Our patient has similar characteristics to patients described in other reports with refractory hypoxemia and evidence of acute RV failure. The real-world challenge for the clinician practicing in a setting similar to ours, without on-site ECMO or advanced thoracic-vascular surgery, is to be able to stabilize the patient in order for safe transportation for diagnostic or therapeutic purposes. At our institution, iNO is available for use in neonates. We extrapolated data from pediatrics and from reported use in similar cases of intermediate risk PE with RV strain in our decision to use iNO and at what dose. There has been significant interest regarding the potential therapeutic use of iNO in PE with the first phase II double-blinded, randomized trial of iNO to treat acute PE recently completed by Kline et al. with the final analysis to be reported [21].
Inhaled epoprostenol (iEPO) is another inhaled pulmonary vasodilator that like iNO has been used in patients with ARDS and refractory hypoxemia. It functions like iNO, causing selective pulmonary vasodilation when added to an inspired gas. Webb et al. described a case in 1996 where its use in a patient with massive PE resulted in a transient improvement in mean pulmonary arterial pressures but did not alter the clinical deterioration of the described patient [22]. While there have been no studies assessing the role of iEPO in acute submassive PE, the use of systemic epoprostenol was studied by Kooter et al. who conducted a randomized controlled trial comparing its use to placebo in patients with a diagnosis of acute PE and right ventricular overload. The researchers were unable to find any significant improvement in right ventricular dilatation or other objective markers of right ventricular overload with the use of systemic epoprostenol [23]. While the patients in this study did not develop hypotension, the use of a systemic vasodilator should be used with caution in this setting as it may precipitate hemodynamic collapse in patients with acute RV dysfunction. iEPO is not available at our institution and thus not considered in our patient
4. Conclusion
Our patient highlights the challenges in the evaluation and management of critically ill patients with acute pulmonary emboli and severe hypoxia and right-side failure.The use of iNO likely plays a role in the initial stabilization of these patients allowing time for more definitive therapy and may even decrease the need for more invasive therapeutic modalities. These potential benefits will need to be assessed in large prospective trials.
Abbreviations
- RV:
Right ventricle
- ICU:
Intensive care unit
- PEEP:
Positive end-expiratory pressure
- CT:
Computed tomography
- TTE:
Transthoracic echocardiogram
- iNO:
Inhaled nitric oxide
- PVR:
Pulmonary vascular resistance
- FiO2:
Fraction of inspired oxygen
- CXR:
Chest X-ray
- PASP:
Pulmonary artery systolic pressure
- PE:
Pulmonary embolism.
Disclosure
Dr. Khalida Ismailova was involved in the preparation of an abstract of this case which was presented at the annual meeting of the American College of Chest Physicians in October 2018. She was unable to provide input for this case report and thus her name was not included in this case report. She is aware of this manuscript and has given us consent for review for possible publication.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Omesh Toolsie searched the literature and wrote the manuscript. Omesh Toolsie conceived and edited the manuscript. Gilda Diaz-Fuentes supervised the patient's treatment and critically revised and edited the manuscript. Umut Gomceli provided the patient's echocardiogram pictures and commented on the images as they pertain to the patient. All authors have made significant contributions to the manuscript and have reviewed it before submission. All authors have confirmed that the manuscript is not under consideration for review at any other journal. All authors have read and approved the final manuscript. Dr. Khalida Ismailova was involved in the preparation of an abstract of this case which was presented at the annual meeting of the American College of Chest Physicians in October 2018. She was unable to provide input for this case report and thus her name was not included in this case report. She is aware of this manuscript and has given us consent for review for possible publication.
References
- 1.Rimar S., Gillis C. N. Selectivepulmonaryvasodilationbyinhalednitricoxideis due to hemoglobin inactivation. Circulation. 1993;88:2884–2887. doi: 10.1161/01.cir.88.6.2884. [DOI] [PubMed] [Google Scholar]
- 2.Pepke-Zaba J., Higenbottam T. W., Dinh-Xuan A. T., Stone D., Wallwork J. Inhaled nitric oxide as a cause of selective pulmonary vasodilatation in pulmonary hypertension. The Lancet. 1991;338(8776):1173–1174. doi: 10.1016/0140-6736(91)92033-X. [DOI] [PubMed] [Google Scholar]
- 3.Stamler J. S., Singel D. J., Loscalzo J. Biochemistry of nitric oxide and its redox-activated forms. Science. 1992;258:1898–1902. doi: 10.1126/science.1281928. [DOI] [PubMed] [Google Scholar]
- 4.Sokol J., Jacobs S. E., Bohn D. Inhalednitricoxideforacutehypoxicrespiratory failure in children and adults: a meta-analysis. Anesth Analg. 2003;97:989–998. doi: 10.1213/01.ANE.0000078819.48523.26. [DOI] [PubMed] [Google Scholar]
- 5.Hillman N. D., Meliones J. N., Black D. R., Craig D. M., Cheifetz I. M., Smith P. K. In acute lung injury, inhaled nitric oxide improves ventilation-perfusion matching, pulmonary vascular mechanics, and transpulmonary vascular efficiency. The Journal of Thoracic and Cardiovascular Surgery. 1995;110(3):593–600. doi: 10.1016/S0022-5223(95)70089-7. [DOI] [PubMed] [Google Scholar]
- 6.George I., Xydas S., Topkara V. K., et al. Clinical Indication for Use and Outcomes After Inhaled Nitric Oxide Therapy. The Annals of Thoracic Surgery. 2006;82(6):2161–2169. doi: 10.1016/j.athoracsur.2006.06.081. [DOI] [PubMed] [Google Scholar]
- 7.Wiener R. S., Schwartz L. M., Woloshin S. Timetrendsinpulmonaryembolisminthe United States: evidence of overdiagnosis. Archives of Internal Medicine. 2011;171:831–837. doi: 10.1001/archinternmed.2011.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldhaber S. Z., Visani L., de Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER) The Lancet. 1999;353(9162):1386–1389. doi: 10.1016/S0140-6736(98)07534-5. [DOI] [PubMed] [Google Scholar]
- 9.Goldhaber S. Z., Haire W. D., Feldstein M. L., et al. Alteplaseversusheparininacute pulmonary embolism: randomised trial assessing right-ventricular function and pulmonary perfusion. Lancet. 1993;341:507–511. doi: 10.1016/0140-6736(93)90274-k. [DOI] [PubMed] [Google Scholar]
- 10.Ribeiro A., Lindmarker P., Juhlin-Dannfelt A., Johnsson H., Jorfeldt L. Echocardiography Doppler in pulmonary embolism: Right ventricular dysfunction as a predictor of mortality rate. American Heart Journal. 1997;134(3):479–487. doi: 10.1016/S0002-8703(97)70085-1. [DOI] [PubMed] [Google Scholar]
- 11.Kasper W., Konstantinides S., Geibel A., Tiede N., Krause T., Just H. Prognostic significance of right ventricular afterload stress detected by echocardiography in patients with clinically suspected pulmonary embolism. Heart. 1997;77(4):346–349. doi: 10.1136/hrt.77.4.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grifoni S., Olivotto I., Cecchini P., et al. Short-term clinical outcome of patients with acute pulmonary embolism, normal blood pressure, and echocardiographic right ventricular dysfunction. Circulation. 2000;101(24):2817–2822. doi: 10.1161/01.CIR.101.24.2817. [DOI] [PubMed] [Google Scholar]
- 13.Watts J. A., Gellar M. A., Fulkerson M. K., Kline J. A. Pulmonary vascular reserve during experimental pulmonary embolism: Effects of a soluble guanylate cyclase stimulator, BAY 41-8543∗. Critical Care Medicine. 2011;39(12):2700–2704. doi: 10.1097/CCM.0b013e318226678e. [DOI] [PubMed] [Google Scholar]
- 14.Kline J. A., Steuerwald N. M., Watts J. A., Courtney M., Bonkovsky H. L. Leukocyte expression of heme oxygenase-1 [hmox1] varies inversely with severity of tricuspid regurgitation in acute pulmonary embolism. Thrombosis Research. 2015;136(4):769–774. doi: 10.1016/j.thromres.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kline J. A., Watts J., Courtney D., Lee Y. Y., Hwang S. Severe pulmonary embolism decreases plasma L-arginine. European Respiratory Journal. 2014;43(3):906–909. doi: 10.1183/09031936.00171913. [DOI] [PubMed] [Google Scholar]
- 16.Watts J. A., Gellar M. A., Fulkerson M. K., Das S. K., Kline J. A. Arginase depletes plasma l-arginine and decreases pulmonary vascular reserve during experimental pulmonary embolism. Pulmonary Pharmacology and Therapeutics. 2012;25(1):48–54. doi: 10.1016/j.pupt.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 17.Frostell C., Fratacci M. D., Wain J. C., Jones R., Zapol W. M. Inhaled nitric oxide. A selective pulmonary vasodilator reversing hypoxic pulmonary vasoconstriction. Circulation. 1991;83(6):2038–2047. doi: 10.1161/01.CIR.83.6.2038. [DOI] [PubMed] [Google Scholar]
- 18.Ciurzyński M., Kurnicka K., Lichodziejewska B., et al. Tricuspid Regurgitation Peak Gradient (TRPG)/tricuspid annulus plane systolic excursion (TAPSE) – a novel parameter for stepwise echocardiographic risk stratification in Normotensive Patients with acute pulmonary embolism. Circulation Journal. (4) 2018;82:1179–1185. doi: 10.1253/circj.CJ-17-0940. [DOI] [PubMed] [Google Scholar]
- 19.Szold O., Khoury W., Biderman P., Klausner J. M., Halpern P., Weinbroum A. A. Inhaled Nitric Oxide Improves Pulmonary Functions Following Massive Pulmonary Embolism: A Report of Four Patients and Review of the Literature. Lung. 2006;184(1):1–5. doi: 10.1007/s00408-005-2550-7. [DOI] [PubMed] [Google Scholar]
- 20.Tariq B., Adi N., Mohmad T., et al. Inhaled nitric oxide in acute pulmonary embolism: a systematic review. Reviews in Cardiovascular Medicine. 2015;16(1):1–8. doi: 10.3909/ricm0718. [DOI] [PubMed] [Google Scholar]
- 21.Kline J. A., Hall C. L., Jones A. E., Puskarich M. A., Mastouri R. A., Lahm T. Randomized trial of inhaled nitric oxide to treat acute pulmonary embolism: The iNOPE trial. American Heart Journal. 2017;186:100–110. doi: 10.1016/j.ahj.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kearon C., Akl E. A., Ornelas J., et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. CHEST. 2016;149(2):315–352. doi: 10.1016/j.chest.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 23.Webb S. A., Stott S., van Heerden P. V. The use of inhaled aerosolized prostacyclin (IAP) in the treatment of pulmonary hypertension secondary to pulmonary embolism. Intensive Care Medicine. 1996;22(4):353–355. doi: 10.1007/BF01700458. [DOI] [PubMed] [Google Scholar]