Abstract
Background
Carotid artery stenting (CAS) has been regarded as a reliable treatment approach for carotid artery stenosis. However, recurrent carotid artery stenosis after CAS affects long-term outcomes. In this study, we aimed to investigate the potential risk factors for carotid restenosis.
Material/Methods
We retrospectively analyzed the clinical data of patients diagnosed with carotid artery stenosis who underwent CAS implantation at our department from September 2012 to July 2015. Each included study patient was followed up with serial duplex ultrasound scanning. Kaplan-Meier estimates were used to evaluate freedom from restenosis and potential risk factors were analyzed.
Results
There were 33 patients enrolled in our study. The mean age was 65.5±11.5 years. The technique was successfully achieved in all patients. No death or major stroke occurred after stenting. There were 2 events of minor stroke and one myocardial infarction within 30 days after stent implantation. All the patients were followed up for 3 years. Cumulative rates of freedom from recurrent stenosis at 1, 2, and 3 years were 87.4%, 74.6%, and 68.3% respectively. Cox multivariate regression analysis revealed that male sex, smoking and hyperlipidemia were independent risk factors associated with restenosis.
Conclusions
In this study, we identified that CAS was a reliable approach for carotid artery stenosis. Male sex, smoking, and hyperlipidemia were independent risk factors associated with restenosis. Thus, hyperlipidemia should be monitored and routine follow-up with ultrasonography are recommended especially for male patients with current or history of smoking.
MeSH Keywords: Carotid Artery Diseases; Endovascular Procedures; Graft Occlusion, Vascular; Risk Factors
Background
The morbidity and mortality of stroke remains high worldwide. It is reported that extracranial carotid artery disease accounts for up to 20% of these strokes [1]. Carotid artery atherosclerosis is one of the important causes of ischemia stroke [2], which contributes to impairment of cognitive function. Thus, effective treatment strategies targeting stenosis of the carotid artery is of importance for prohibiting the progression of cognitive dysfunction in patients with ischemic cerebrovascular disease. In 1980, percutaneous transluminal carotid angioplasty was first performed by Kerber [3]. During the past decade, the rapid improvement in interventional technology and materials has transformed a technique initially developed as a palliative treatment in inoperable patients into a therapeutic alternative option to surgery. Nowadays, carotid artery stenting (CAS) has become an option for treatment with less invasion [4].
Although carotid artery stenting has been regarded as a reliable approach with lower risks of myocardial infarction, cranial nerve palsy, and access site hematoma, some studies reported that carotid artery stenting was associated with a higher risk of procedure-related stroke [5,6]. Oszkinis et al. [7] found that the incidence of restenosis following carotid interventions was up to 9.3% in a study including 16 patients underwent endovascular procedure. Sadideen et al. reported the restenosis rate reached as high as 37% [8]. So far, few studies have focused on the recurrent stenosis after carotid artery stenting [9,10]. Thus, in our study, we investigated the potential risk factors which contributed to recurrent carotid-artery stenosis following stenting treatment.
Material and Methods
Patient population
The study was a retrospective study on patients diagnosed with carotid arteries stenosis at the Department of Vascular Surgery of Jining No. 1 People’s Hospital between September 2012 and July 2015. The study was reviewed and approved by the Institutional Review Board of Jining No. 1 People’s Hospital. Informed consent was waived for this study. Before enrollment, all the patients were screened for eligibility on the basis of findings from duplex ultrasonography, contrast angiography, or both. Inclusion criteria consisted of stenosis of more than 50% on digital subtraction angiography, more than 70% on computed tomographic angiography (CTA), or duplex ultrasonography. Patients were excluded if they had any of the following comorbidities: myocardial infarction within 30 days, chronic atrial fibrillation or paroxysmal atrial fibrillation within 6 months, or unstable angina. The final selected patients were included in this study.
Carotid artery stenting procedure
Before the CAS, the brains and necks of all study patients were examined by CTA, magnetic resonance imaging, ultrasonography, and brain vessels angiography. The degree, location, and length of vessel stenosis were evaluated. From these results, the location and length of the stent could be determined before CAS procedure. The carotid artery stenting procedure was performed by an experienced surgeon after local anesthesia. Then an 8F catheter sheath was inserted through the right femoral artery via a Seldinger puncture. Contrast medium was infused through the catheter to reconfirm the stenosis of carotid artery. A guiding catheter was advanced to the common carotid artery. Before the releasing of the stent, a protective umbrella was implanted and released following a pre-expanded balloon placed at the lesion site. After that, an Acculink carotid stent (Abbott, IL, USA) was implanted and released at the stenosed portion of carotid artery.
When the protective devices were removed, immediate angiography was performed to confirm there was no contrast agent extravasation and the residual stenosis of the artery <30%. All patients received antiplatelet therapy at least for 12 weeks after stenting. Lipid lowering medication were provided in patients with hyperlipidemia.
Outcomes measure and follow-up
The primary outcome of this analysis was defined as restenosis >50% occlusion of the carotid artery detected at any stage during follow-up, namely a peak systolic velocity of >125 cm/second in ultrasonography [11]. Procedure-related complications included puncture site bleeding, vascular injury, cranial-nerve injury, and noncerebral bleeding. Additional perioperative complications were myocardial infarction, stroke, or death within 1 month after CAS. Ultrasonography was conducted 1, 3, 6, and 12 months after the procedure; and then at 6-monthly intervals for next 3 years. A follow-up telephone interview was performed at 6 months and then at 3-month intervals. Patients were followed until 3 years post-procedure. Stroke was defined as an acute neurologic event lasting for more than 1 day with diagnosis of focal cerebral ischemia via CTA. Myocardial infarction was defined by increase of a troponin or creatine kinase MB level in addition to symptoms that were consistent with electrocardiographic evidence of ischemia.
Statistical analysis
All data was analyzed using IBM SPSS Statistics Version 20 (IBM Corp., NY, USA). All missing variables were coded and omitted from analysis. Baseline variables are summarized with the use of descriptive statistics. Continuous variables are summarized as the mean, median, standard deviation, minimum and maximum values, and 95% confidence intervals and was analyzed using t-tests or Mann-Whitney U where appropriate. Categorical variables are summarized as counts, percentages, and exact 95% Clopper-Pearson confidence intervals and was assessed with chi-square and Fischer’s exact analysis. Cox regression analysis was performed taking outcome measures as dependent variables and entering the risk factors with significant P values (P<0.05) from univariate analysis as independent variables. Cox regression analysis was repeated to analyze independent variables. For time-to-event variables, Kaplan-Meier survival estimates were used.
Results
Patient population
Between September 2012 and July 2015, a total of 45 patients diagnosed with carotid artery stenosis were recruited in our department. 12 patients were excluded from this study according to the exclusion criteria. Of these 12 patients, 5 patients refused to receive CAS; 1 patient had myocardial infarction within the previous 30 days; 2 patients had chronic atrial fibrillation with anticoagulation treatment; and 4 patients were lost during follow-up. Finally, a total of 33 patients were selected for this analysis (Figure 1). Patient demographics are summarized in Table 1.
Figure 1.
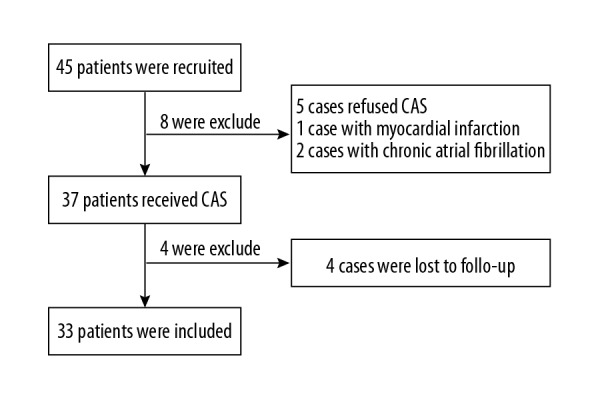
Flow chart of the trial profile.
Table 1.
Characteristics of the study population.
| Characteristic | |
|---|---|
| Age-year | |
| Mean | 65.5 |
| Range | 54–76 |
| Male sex-no. (%) | 19 (57.6) |
| Hypertension-no. (%) | 28 (84.8) |
| Hyperlipidemia-no. (%) | 27 (81.8) |
| Diabetes mellitus-no. (%) | 13 (39.3) |
| Cigarette smoking-no. (%) | 24 (72.7) |
| History of stroke-no. (%) | 5 (15.2) |
| Current contralateral carotid disease-no. (%) | 13 (39.3) |
Clinical outcomes
Mean duration of stenting procedure was 24.4±7.5 minutes and mean time from recent event to treatment was 16.5±5.5 days. Stenosis and lesion length were measured via angiography intraoperatively. Successful CAS implantation was achieved in all patients. Mean in-hospital stay of length was 6.8 days (Table 2). Clinical outcomes within 30 days post procedure are summarized in Table 3. No other complications were observed during hospitalization. Follow-up at 30 days demonstrated all carotid artery patent. The preoperative and postoperative digital subtraction angiography (DSA) images were shown in Figure 2.
Table 2.
Clinical data of patients.
| Characteristic | |
|---|---|
| Time from recent event to treatment-d | |
| Mean | 16.5 |
| Range | 5–32 |
| Stenosis of the vessel-% | 74.5±7.6 |
| Lesion length-mm | 16.7±5.5 |
| Technique success rate-% | 100 |
| Mean in-hospital stay of length-d | 6.8±2.6 |
Table 3.
Clinical outcomes within 30 days after stenting.
| Outcome | Number |
|---|---|
| Death | 0 |
| Major stroke | 0 |
| Minor stroke-no. (%) | 2 (6.1%) |
| Myocardial infarction-no. (%) | 1 (3%) |
| Noncerebral bleeding-no. (%) | 1 (3%) |
| Access-site bleeding-no. (%) | 5 (15.1%) |
| Other complications | 0 |
Figure 2.
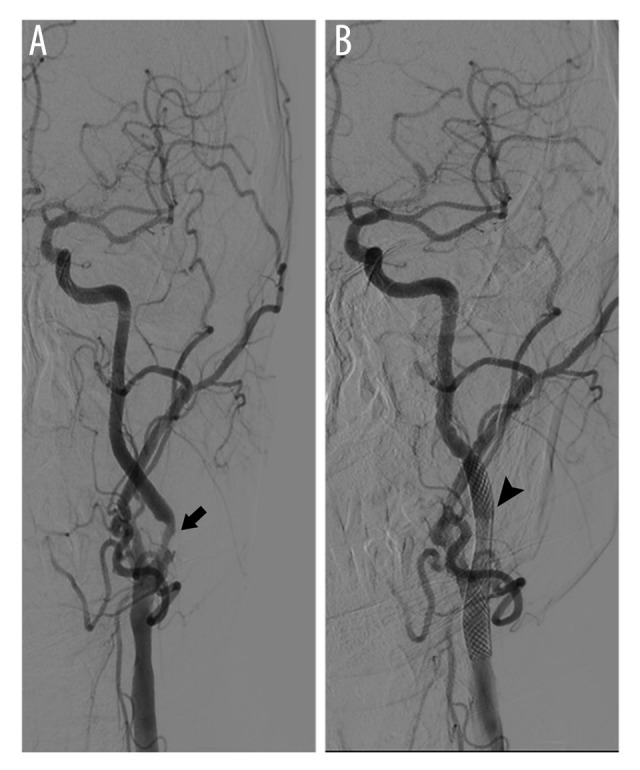
Preoperative and postoperative DSA images: (A) shows severe stenosis of left internal carotid artery (arrow); (B) shows implantation of the stent completely restored the vascular lumen (arrowhead).
Over the follow-up of 3 years, 11 patients demonstrated recurrent carotid artery stenosis. Eight of these 11 patients had no symptoms at presentation and recurrent carotid artery stenosis was diagnosed at ultrasonography during routine follow-up. Three patients with symptoms were referred to our department and received ultrasonography. Recurrent stenotic lesion ranged from 50–80%. Of these 11 patients, 8 underwent reintervention treatment while the other 3 refused revascularization. No major problems were observed in these 8 patients after a second surgery. With Kaplan-Meier estimates, cumulative rates of freedom from recurrent stenosis at 1, 2, and 3 years were 87.4%, 74.6%, and 68.3% respectively (Figure 3).
Figure 3.
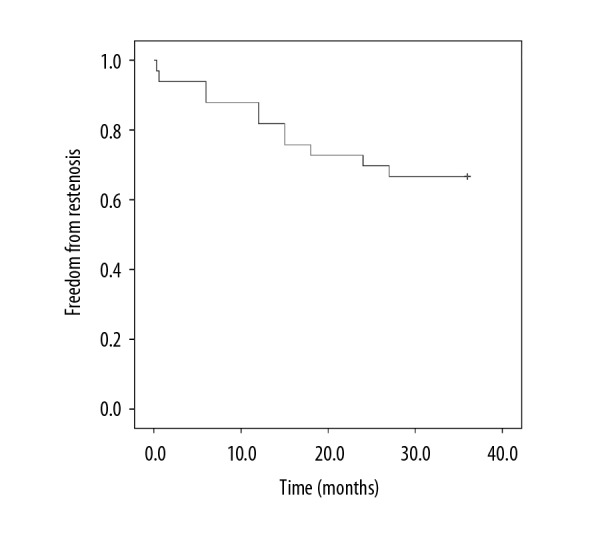
Kaplan-Meier analysis of freedom from recurrent carotid artery stenosis. Shown is the Kaplan-Meier survival curve for freedom from recurrent from carotid artery stenosis within 3 years after the procedure in the included population.
Risk factors for recurrent carotid artery stenosis
Univariate analysis revealed that 6 evaluated factors, including male sex (HR, 2.4; 95% CI, 1.1–4.5), smoking (HR, 3.0; 95% CI, 1.8–6.7), hypertension (HR, 2.1; 95% CI, 1.3–3.7), hyperlipidemia (HR, 3.8; 95% CI, 1.6–5.7), diabetes mellitus (HR, 1.9; 95% CI, 1.02–2.8) and peripheral vascular disease (HR, 1.5; 95% CI, 1.08–1.9) were associated with increased risk of recurrent carotid artery stenosis (Table 4). Furthermore, multivariate analysis showed only 3 of these 6 were independent risk factors associated with recurrent carotid artery stenosis. Factors including hypertension, diabetes mellitus, and peripheral vascular disease have no significant association with recurrent carotid artery stenosis. However, male sex (HR, 2.2; 95% CI, 1.5–3.9), smoking (HR, 3.3; 95% CI, 1.4–7.7) and hyperlipidemia (HR, 2.5; 95% CI, 1.2–5.7) were associated with restenosis (Table 5).
Table 4.
Univariate analysis for recurrent carotid artery stenosis.
| Factor | HR | 95% CI | P value |
|---|---|---|---|
| Age, >60 | 1.05 | 0.75–1.6 | 0.631 |
| Sex, male | 2.4 | 1.1–4.5 | 0.014 |
| Smoking | 3.0 | 1.8–6.7 | 0.011 |
| Hypertension | 2.1 | 1.02–3.7 | 0.034 |
| History of stroke | 1.1 | 0.8–1.6 | 0.145 |
| Hyperlipidemia | 3.8 | 1.6–5.7 | 0.021 |
| Diabetes mellitus | 1.9 | 1.02–2.8 | 0.032 |
| Peripheral vascular disease | 1.5 | 1.08–1.9 | 0.041 |
| Contralateral carotid disease | 1.06 | 0.8–1.5 | 0.221 |
Table 5.
Multivariate analysis for recurrent carotid artery stenosis.
| Factor | HR | 95% CI | P value |
|---|---|---|---|
| Sex, male | 2.2 | 1.5–3.9 | 0.025 |
| Smoking | 3.3 | 1.8–6.7 | 0.015 |
| Hypertension | 1.8 | 0.6–3.2 | 0.158 |
| Hyperlipidemia | 2.5 | 1.2–5.7 | 0.017 |
| Diabetes mellitus | 1.5 | 0.7–2.3 | 0.225 |
| peripheral vascular disease | 1.6 | 0.8–2.1 | 0.325 |
Discussion
Carotid atherosclerosis is the main cause for carotid stenosis and many previous studies have reported a series risk factor for carotid atherosclerosis [12,13]. Carotid artery stenting has emerged as an option to operation in the management of carotid artery stenosis. Previous studies have demonstrated that CAS is valuable treatment for carotid artery stenosis on long term with pleasing results on patency and death/stroke rates [14,15]. Donato et al. [16] enrolled 3179 patients underwent CAS procedure and retrospectively analyzed the 5-year freedom from death or stroke. The results showed that CAS as a reliable approach for prevention of stroke. Additionally, the procedure-related complications after CAS was comparable to that of traditional treatment. In our study, we collected the data from patients with 3-year follow-up and revealed that 3-year freedom rate from recurrent stenosis was 68.3% which is lower than that from other studies [17,18]. The explication should be the different inclusion criteria. We included a portion of patients with high-risk or having a history of stroke. In addition, the results from 30 days after CAS also proved lower procedure-related complications. We observed no death or major stroke and only 2 minor stroke, 1 myocardial infarction, and other minor complications. The types of stent used contributed to differences in adverse event rates. A number of published studies have focused on the comparison between carotid artery stenosis and carotid endarterectomy. However, for normal-risk patients, there are no randomized clinical trials demonstrating the equivalent role of stenting compared to CEA [5,19]. The SAPPHIRE trials concluded that the composite rate of death, stroke, or myocardial infarction within 30 days or death or ipsilateral stroke between 31 days and 3 years was 26.2% in the stenting group and 30.3% in the endarterectomy group [20]. In general, our results demonstrated that CAS was a reliable treatment as previous studies concluded.
In this study, we aimed to investigate the potential risk factors contributed to recurrent carotid artery stenosis. Previous reports found that some predictors such as male sex, renal insufficiency, age >70 years, and a lesion located at the bifurcation were associated with neurological complications for CAS [17]. However, to our knowledge, few researchers have focused on the risk factors associated with recurrent carotid artery stenosis. Gutierrez et al. [21] reported female sex and diabetes as risk factors for recurrent carotid artery stenosis after endarterectomy. In addition, results from other studies have shown that contralateral stenosis, and ASA grades 2 and 3 are independent predictors of carotid restenosis [22,23]. Our results were not in link with previous studies. This discrepancy can be explained by different therapeutic strategies. In our study, the patients all received CAS instead of endarterectomy. In addition, all of previous study reports were based on short follow-up. With longer follow-up and the application of Kaplan-Meier survival estimates, we were able to report more informative data on recurrent carotid artery stenosis after carotid artery stenting. The Kaplan-Meier survival estimates indicate recurrences reported relative to the patient population at risk during a given interval. Thus, these data reveal all accumulated information weighting the data in correlation with the duration of follow-up. Additionally, it is of note that we did not observe significant neurological complications in association with recurrent stenosis. In accordance with previous results, we found that most of the lesions occurred within the first 36 months after the procedure [24]. Previous reports have suggested the possibility of recurrent atherosclerotic plaque as a possible cause [25].
In conclusion, our results established that CAS was a safe and effective option for carotid artery stenosis with a low rate of neurological events and other procedure-related complications. Furthermore, the long-term follow-up showed that despite restenosis as an infrequent complication, most of events occur within the first 3 years after the procedure. Finally, we found that male sex, smoking, and hyperlipidemia were independent predictors for carotid stenosis. Thus, hyperlipidemia should be monitored and routine follow-up with ultrasonography are recommended especially for male patients with current or history of smoking.
Conclusions
This study investigated the potential risk factors for recurrent carotid-artery stenosis following stenting treatment. Our results revealed that male sex, smoking, and hyperlipidemia were independent risk factors associated with restenosis. In general, CAS was a reliable treatment for carotid artery stenosis. However, a prospective trial is needed to further evaluate the long-term effect of CAS.
Footnotes
Source of support: Departmental sources
Conflicts of interest
None.
References
- 1.Rosenfield K, Matsumura JS, Chaturvedi S, et al. Randomized trial of stent versus surgery for asymptomatic carotid stenosis. N Engl J Med. 2016;374(11):1011–20. doi: 10.1056/NEJMoa1515706. [DOI] [PubMed] [Google Scholar]
- 2.Petty GW, Brown RD, Jr, Whisnant JP, et al. Ischemic stroke subtypes: A population-based study of incidence and risk factors. Stroke. 1999;30(12):2513–16. doi: 10.1161/01.str.30.12.2513. [DOI] [PubMed] [Google Scholar]
- 3.Kerber CW, Cromwell LD, Loehden OL. Catheter dilatation of proximal carotid stenosis during distal bifurcation endarterectomy. Am J Neuroradiol. 1980;1(4):348–49. [PMC free article] [PubMed] [Google Scholar]
- 4.Spacek M, Veselka J. Carotid artery stenting – current status of the procedure. Arch Med Sci. 2013;9(6):1028–34. doi: 10.5114/aoms.2013.39216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.SPACE Collaborative Group. 30 day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: A randomised non-inferiority trial. Lancet. 2006;368(9543):1239–47. doi: 10.1016/S0140-6736(06)69122-8. [DOI] [PubMed] [Google Scholar]
- 6.International Carotid Stenting Study investigators. Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (International Carotid Stenting Study): An interim analysis of a randomised controlled trial. Lancet. 2010;375(9719):985–97. doi: 10.1016/S0140-6736(10)60239-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oszkinis G, Pukacki F, Juszkat R, et al. Restenosis after carotid endarterectomy: Incidence and endovascular management. Interv Neuroradiol. 2007;13(4):345–52. doi: 10.1177/159101990701300405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sadideen H, Taylor PR, Padayachee TS. Restenosis after carotid endarterectomy. Int J Clin Pract. 2006;60(12):1625–30. doi: 10.1111/j.1742-1241.2005.00775.x. [DOI] [PubMed] [Google Scholar]
- 9.Lal BK, Hobson RW, II, Goldstein J, et al. In-stent recurrent stenosis after carotid artery stenting: life table analysis and clinical relevance. J Vasc Surg. 2003;38(6):1162–68. doi: 10.1016/j.jvs.2003.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Pohlmann C, Höltje J, Zeile M, et al. Recurrent stenosis following carotid artery stenting treated with a drug-eluting balloon: A single-center retrospective analysis. Neuroradiology. 2018;60(1):81–87. doi: 10.1007/s00234-017-1935-7. [DOI] [PubMed] [Google Scholar]
- 11.Oates CP, Naylor AR, Hartshorne T, et al. Joint recommendations for reporting carotid ultrasound investigations in the United Kingdom. Eur J Vasc Endovasc Surg. 2009;37(3):251–61. doi: 10.1016/j.ejvs.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 12.Giaginis C, Papadopouli A, Zira A, et al. Correlation of plasma osteoprotegerin (OPG) and receptor activator of the nuclear factor κB ligand (RANKL) levels with clinical risk factors in patients with advanced carotid atherosclerosis. Med Sci Monit. 2012;18(10):CR597–604. doi: 10.12659/MSM.883485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giaginis C, Klonaris C, Katsargyris A, et al. Correlation of peroxisome proliferator-activated receptor-γ (PPAR-γ) and retinoid x receptor-α (RXR-α) expression with clinical risk factors in patients with advanced carotid atherosclerosis. Med Sci Monit. 2011;17(7):CR381–91. doi: 10.12659/MSM.881849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bosiers M, Peeters P, Deloose K, et al. Does carotid artery stenting work on the long run: 5-year results in high-volume centers (ELOCAS Registry) J Cardiovasc Surg (Torino) 2005;46(3):241–47. [PubMed] [Google Scholar]
- 15.Paniagua D, Howell M, Strickman N, et al. Outcomes following extracranial carotid artery stenting in high-risk patients. J Invasive Cardiol. 2001;13(5):375–81. [PubMed] [Google Scholar]
- 16.de Donato G, Setacci C, Deloose K, et al. Long-term results of carotid artery stenting. J Vasc Surg. 2008;48(6):1431–41. doi: 10.1016/j.jvs.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 17.Bergeron P, Roux M, Khanoyan P, et al. Long-term results of carotid stenting are competitive with surgery. J Vasc Surg. 2005;41(2):213–21. doi: 10.1016/j.jvs.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 18.Lal BK, Kaperonis EA, Cuadra S, et al. Patterns of in-stent restenosis after carotid artery stenting: Classification and implications for long-term outcome. J Vasc Surg. 2007;46(5):833–40. doi: 10.1016/j.jvs.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 19.Mas JL, Chatellier G, Beyssen B, et al. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355(16):1660–71. doi: 10.1056/NEJMoa061752. [DOI] [PubMed] [Google Scholar]
- 20.Gurm HS, Yadav JS, Fayad P, et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med. 2008;358(15):1572–79. doi: 10.1056/NEJMoa0708028. [DOI] [PubMed] [Google Scholar]
- 21.Reina-Gutierrez T, Serrano-Hernando FJ, Sanchez-Hervas L, et al. Recurrent carotid artery stenosis following endarterectomy: natural history and risk factors. Eur J Vasc Endovasc Surg. 2005;29(4):334–41. doi: 10.1016/j.ejvs.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Bonati LH, Gregson J, Dobson J, et al. Restenosis and risk of stroke after stenting or endarterectomy for symptomatic carotid stenosis in the International Carotid Stenting Study (ICSS): Secondary analysis of a randomised trial. Lancet Neurol. 2018;17(7):587–96. doi: 10.1016/S1474-4422(18)30195-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zapata-Arriaza E, Moniche F, González A. Predictors of restenosis following carotid angioplasty and stenting. Stroke. 2016;47(8):2144–47. doi: 10.1161/STROKEAHA.116.012650. [DOI] [PubMed] [Google Scholar]
- 24.Lal BK, Hobson RW, II, Goldstein J, et al. In-stent recurrent stenosis after carotid artery stenting: life table analysis and clinical relevance. J Vasc Surg. 2003;38(6):1162–68. doi: 10.1016/j.jvs.2003.08.021. [DOI] [PubMed] [Google Scholar]
- 25.Treiman GS, Jenkins JM, Edwards WH, Sr, et al. The evolving surgical management of recurrent carotid stenosis. J Vasc Surg. 1992;16(3):354–62. [PubMed] [Google Scholar]


