Abstract
Purpose
Investigation of the longitudinal effect of schizophrenia on changes in various brain-metabolite levels and their relationships with cognitive deficits that have not been fully explained yet.
Methods
Five years subsequent to their first examination for their first episode of schizophrenia, eleven patients from an original group of 30 were reexamined. Their cognitive functions were assessed with the Wisconsin Card Sorting Test. Magnetic resonance imaging and proton magnetic resonance spectroscopy were performed on a 1.5 T scanner. Voxels of 8 cm3 were positioned in the left frontal lobe, left temporal lobe, and the left thalamus. The study had a naturalistic design, and patients were treated with various antipsychotics.
Results
No significant statistical differences between the baseline and follow-up in N-acetylaspartate (NAA:creatine plus phosphocreatine [Cr] and NAA/H2O) levels were observed in any region of interest. We found a significant statistical correlation between 5-year difference in frontal NAA/Cr levels and duration of the last antipsychotic treatment in this period (R=0.908, P=0.012). We found a trend (P=0.068) toward lower choline-containing compounds (Cho/Cr ratio) in the temporal lobe over 5 years and a trend (P=0.079) in higher glutamate–glutamine– GABA (Glx/H2O) levels in the left thalamus. The patients showed social and clinical improvement at follow-up examination, and there were no changes in Wisconsin Card Sorting Test results.
Conclusion
The observed tendency toward decline in choline ratio might have been due to decreased temporal cell density or impaired neuron-membrane or myelin functions. A tendency for higher Glx levels suggest the involvement of thalamus dysfunction in the chronic schizophrenia process. The lack of NAA decrease might have been due to effective antipsychotic treatment. Further longitudinal studies on large patient groups are required to confirm these metabolic changes in schizophrenia.
Keywords: first-episode schizophrenia, proton magnetic resonance spectroscopy, longitudinal study, cognitive functioning, N-acetylaspartate, choline
Introduction
A few complex theories explaining the neurobiological processes of schizophrenia have been developed based on growing evidence, mostly from neuroimaging studies. The neurodegenerative theory of schizophrenia is based on Kraepelin’s observation on the progressive illness process. Liebermann1 proposed the hypothesis that schizophrenia involves a limited neurodegenerative process reflected by psychotic symptoms, and moreover such a process is most active in the early stages of illness. According to the neurodevelopmental theory of schizophrenia, etiologic and pathogenic factors occur early in brain development, and symptom occurrence is connected with the normal maturation of brain areas affected by early developmental pathology, particularly the dorsolateral prefrontal cortex.2 Woods3 proposed a progressive developmental mechanism of schizophrenia that can reconcile neuropathological and imaging data, while being compatible with early onset and late deterioration. With regard to these three theories, time and duration of disease are very important variables for morphological and neurochemical brain changes in schizophrenia.
Magnetic resonance spectroscopy (MRS) may allow for testing the neurobiological models of pathogenesis of psychiatric diseases.4–9 This method enables in vivo evaluation of chemical tissue composition and identification of chemical compounds. An N-acetylaspartate (NAA) signal is the most visible in proton spectra (1H MRS). The level of NAA increases during brain growth, and reflects the development of dendrites, synapses, and neuronal somata.5 A decrease in NAA concentration in stroke may indicate neuronal loss or dysfunction. The relationship between NAA levels and duration of schizophrenia has been analyzed in cross-sectional studies. A significant inverse relationship between NAA and creatine–phosphocreatine (Cr) in the left dorsolateral prefrontal cortex and disease duration has been observed.9 The mean duration of illness in that study was 6 years, so it suggests that reduced NAA concentration may occur primarily in the early years of the illness.9 Other frequently checked spectroscopic brain metabolites include: glutamate–glutamine (Glx; combined signal, with minor contribution from GABA), choline-containing compounds (Cho; a measure of cellular density), Cr, a marker of cellular energy level, and myoinositol (mI; a marker of brain osmotic balance and glial cells).5–9
Most studies in this area have been cross-sectional, while longitudinal studies allow for distinguishing the progressive aspects of illness from static ones, but few studies have been reported. Longitudinal studies (lasting up to 24 months)11,12 point to a global or frontal brain NAA decrease or increase in the cingulate cortex and to a glutamate increase in the thalamus and cingulate, whereas a longitudinal study lasting 80 months10 on schizophrenia duration/treatment, found no changes in NAA and decreased glutamate levels in the thalamus. Glutamatergic alterations and gray-matter loss in schizophrenia in longitudinal studies are consistent with neurodegeneration;10 nevertheless, results regarding NAA levels were variable in these studies: a 2-year reduction or no NAA differences in a longer study.10–12 As earlier longitudinal studies found changes only in glutamate levels, we decided to check and reexamine patients after 5 years of illness to determine whether other progressive metabolite changes would be observed in the frontal and temporal lobes, as well as in the thalamus. Our hypothesis was that NAA levels would be decreased.
Methods
Subjects
The first examination was performed during patients’ first hospitalization at the Department of Psychiatry of the Medical University of Białystok and at the Psychiatric Hospital in Choroszcz. Subjects were included in the study from consecutively admitted patients. The original group consisted of 30 patients with first-episode schizophrenia.13 For a current sample of eleven patients, there were five women and six men, with mean age 23.5±2.61 years and mean duration of illness 6 months. At baseline, patients were given the diagnosis of schizophrenia according to ICD10 criteria: paranoid type (n=9) and undifferentiated type (n=2). One patient was scanned as neuroleptic-naïve and ten received stable doses of antipsychotics (five risperidone, four olanzapine, one haloperidol). Mean antipsychotic doses (chlorpromazine equivalents) were 358 mg/day,14 and the mean number of days on antipsychotic drugs was 50 days until the neuroimaging examination. The subgroup of eleven patients did not differ from the initial group of 30 patients in terms of sex, age, education, length of illness, severity of clinical symptoms, doses of antipsychotics, or length of treatment. All the examined patients were right-handed, determined with the Edinburgh Handedness Inventory.
The follow-up examination was performed 5 years after baseline examination (mean 67.1±12.42 months, 48–87 months). Patients were scanned and underwent clinical and cognitive examination. From the initial group of 30 patients, eleven were contacted and responded (the remaining 19 were lost to medical observation). These were inpatients (n=3) and outpatients (n=8). The mean age of patients was 28.7±2.68 years and mean length of illness 5.5±1.2 years. Ten patients met the criteria for schizophrenia – eight paranoid type and two undifferentiated type – and one for schizoaffective disorder. All patients were treated with antipsychotic medication (atypical and typical antipsychotics in combination: clozapine, olanzapine, risperidone, quetiapine, zuclopenthixol, haloperidol, perphenazine). The mean duration of treatment with the last medication before the second examination was 10 months, and the mean dose (chlorpromazine equivalents) was 376 mg/day.14 Some patients were also treated with mood stabilizers (n=3) and antidepressants (n=4). Clinical symptoms at baseline and follow-up were assessed by a battery of psychiatric measures: Positive and Negative Syndrome Scale (PANSS),15 Calgary Depression Scale for Schizophrenia (CDSS),16 Clinical Global Impression (CGI),17 and Global Assessment of Functioning (GAF). Study-exclusion criteria were central nervous system organic damage confirmed on routine neurological and MR examinations, present and active alcohol and other psychoactive substance dependence, and contraindications to conduct MR examinations.
This study was carried out in accordance with the recommendations of the Declaration of Helsinki and the Bioethical Committee of the Medical University of Białystok. The protocol was approved by the Bioethical Committee of the Medical University of Białystok. All subjects provided written informed consent in accordance with the Declaration of Helsinki to participate in the baseline assessment and after 5 years at follow-up.
MR imaging and 1H MRS
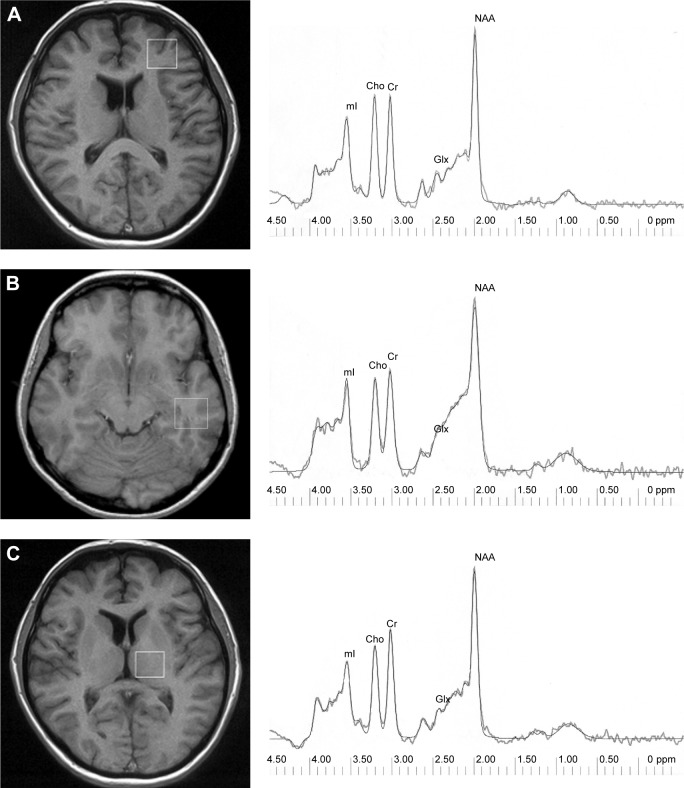
MR imaging and MRS examinations were performed at the Department of Radiology, Medical University of Białystok, on a 1.5 T scanner (Eclipse; Picker International, Highlands Heights, OH, USA) with a standard circularly polarized head coil. A description of this method has been provided by Galińska et al.18 T1-weighted fast scans and conventional fast spin–echo T2-weighted series were obtained. 1H MRS examinations were carried out by means of single-voxel point-resolved spectroscopy (PRESS) sequences with the parameters TR=1,500 ms, TE=35 ms (TE1=~17 ms), number of excitations 192, and 3,906 kHz bandwidth. Voxels of 2×2×2 cm3 were positioned in the left frontal lobe, left temporal lobe, and the left thalamus. In order to shorten the time of scanning, left-sided voxels were analyzed. A trained investigator located voxels by eye by means of T1-weighted sections in sagittal, coronal, and axial planes, and the inclusion of cerebrospinal fluid was minimized. The left frontal lobe voxel was localized in a region that included superior and middle frontal gyrus, above the anterior horns of the lateral ventricles, and comprised mostly of white matter and cortex. The left temporal lobe voxel was localized in the region that included the middle and inferior temporal gyrus. The left thalamus voxel included mostly thalamus tissue and small portions of different structures, eg, the posterior limb of the internal capsule (Figure 1). For the follow-up scan, we took into consideration the voxel position at the initial scan. This was done individually for each patient. Next, the signal over the voxel was shimmed to within a line width of 3–7 Hz and transmitter-pulse power optimized by automated procedures. The multiply optimized insensitive suppression– train method was applied to suppress the signal from water.19
Figure 1.
Voxel location: left frontal lobe (A), left temporal lobe (B), left thalamus (C), and 1H spectrum – raw and fitted data for each region.
Abbreviations: NAA, N-acetylaspartate; Glx, GABA, glutamine, glutamate; Cho, choline-containing compounds; Cr, creatine plus phosphocreatine; mI, myoinositol.
Via 2.0C software provided by Picker was used to analyze spectroscopic data. 1H MRS data were zero-filled to 8,192 points and residual water resonances removed using time-domain high-pass filtering. Exponential Gaussian transformation was applied as a time-domain apodizing Gaussian filter. Next, data were Fourier-transformed and phase-corrected. After the application of a Legendre polynomial function to approximate the baseline, automated curve fitting was performed using an iterative, nonlinear least–squares fitting procedure by means of the Levenberg–Marquardt algorithm. Line shapes of the simulated peaks used in the fitting process were fixed with 85% Gaussian and 15% Lorentzian fractions. Simulated peaks were created using a table of brain metabolites within Via 2.0. Only spectra with the best fit (exactly overlapping and adjusted raw spectrum lines) were included. Metabolites assessed were NAA at 2.01 ppm, Glx in the area from 2.11 ppm to 2.45 ppm, Cho at 3.22 ppm, Cr at 3.03 ppm, and mI at 3.56 ppm (Figure 1). Then, metabolite to creatine ratios were analyzed. The ratio of metabolites to unsuppressed water signals was also calculated:
Cognitive functions
Cognitive functions were tested by the Wisconsin Card Sorting Test (WCST), which is considered a measure of “executive function” and assesses abstract reasoning ability and flexibility in problem-solving.20 We used the WCST Computer Version 2 Research Edition,21 and analyzed the following measures: total errors, perseverative errors, nonperseverative errors, categories completed, and trials to complete first category.
Statistical analysis
Statistical analysis was performed with the Polish version of Statistica 9.0. Metabolite ratios to creatine and water and clinical and neuropsychological results of patients at baseline and follow-up were compared using Wilcoxon’s signed-rank test, due to the small sample. Relationships among all metabolites and clinical characteristics, doses, time of treatment, and neuropsychological results at start and follow-up were analyzed with Spearman’s correlations. For these results, we also performed post hoc analyses with Bonferroni corrections. In addition, dose of antipsychotics and duration of treatment were also correlated with differences in metabolite levels (last minus first day of study) without post hoc analyses. P<0.05 was taken as significant.
Results
Mean metabolite ratios at baseline and follow-up are shown in Table 1. There were no significant differences in any region studied in NAA/Cr or NAA/H2O, the main metabolite of interest. No metabolite ratios from any of the three regions studied correlated with antipsychotic dose at baseline or follow-up. There was a trend toward a lower Cho/Cr ratio in the temporal lobe (P=0.068) and a trend (P=0.079) toward a higher Glx/H2O ratio in the left thalamus over 5 years.
Table 1.
Neurochemical findings in patients with schizophrenia during index hospitalization and at 5-year follow-up
| Metabolite ratios | Baseline | Follow-up | P-value |
|---|---|---|---|
| Left frontal lobe | |||
| NAA/Cr | 2.00±0.34 | 1.68±0.26 | 0.236 |
| Cho/Cr | 1.04±0.15 | 1.02±0.15 | 0.612 |
| mI/Cr | 0.73±0.13 | 0.83±0.13 | 0.398 |
| Glx/Cr | 2.12±0.48 | 1.88±0.12 | 0.236 |
| NAA/H2O | 0.47±0.06 | 0.46±0.03 | 0.398 |
| Cho/H2O | 0.27±0.04 | 0.28±0.03 | 0.236 |
| mI/H2O | 0.19±0.04 | 0.23±0.06 | 0.176 |
| Glx/H2O | 0.54±0.09 | 0.51±0.06 | 0.612 |
| Cr/H2O | 0.25±0.04 | 0.27±0.03 | 0.345 |
| Left temporal lobe | |||
| NAA/Cr | 1.88±0.50 | 1.86±0.13 | 1.000 |
| Cho/Cr | 0.96±0.19 | 0.94±0.25 | 0.068 |
| mI/Cr | 0.69±0.13 | 0.62±0.30 | 1.000 |
| Glx/Cr | 2.41±0.44 | 2.33±0.62 | 0.285 |
| NAA/H2O | 0.40±0.05 | 0.48±0.10 | 0.179 |
| Cho/H2O | 0.24±0.03 | 0.22±0.07 | 0.592 |
| mI/H2O | 0.18±0.07 | 0.16±0.11 | 1.000 |
| Glx/H2O | 0.57±0.16 | 0.56±0.07 | 0.285 |
| Cr/H2O | 0.24±0.05 | 0.23±0.09 | 0.592 |
| Left thalamus | |||
| NAA/Cr | 1.99±0.29 | 1.86±0.28 | 0.345 |
| Cho/Cr | 0.88±0.08 | 0.90±0.20 | 0.463 |
| mI/Cr | 0.61±0.20 | 0.59±0.09 | 0.463 |
| Glx/Cr | 1.90±0.43 | 1.87±0.27 | 0.500 |
| NAA/H2O | 0.53±0.06 | 0.53±0.02 | 0.916 |
| Cho/H2O | 0.25±0.03 | 0.25±0.03 | 0.465 |
| mI/H2O | 0.15±0.04 | 0.21±0.12 | 0.345 |
| Glx/H2O | 0.48±0.12 | 0.53±0.04 | 0.079 |
| Cr/H2O | 0.28±0.03 | 0.28±0.04 | 1.000 |
Notes: Ratios given as mean ± SD. Wilcoxon’s test was used for testing group differences.
Abbreviations: NAA, N-acetylaspartate; Glx, GABA, glutamine, glutamate; Cho, choline-containing compounds; Cr, creatine plus phosphocreatine; mI, myoinositol.
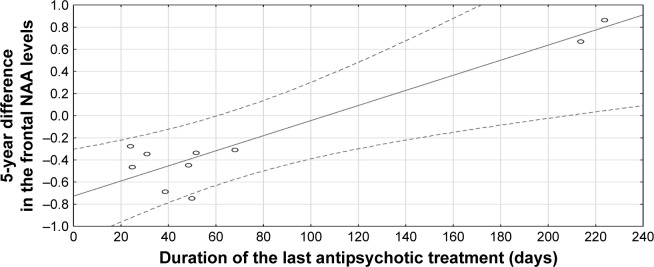
Clinical characteristics of patients and WCST results are shown in Table 2. There was a significant improvement in patients’ social, occupational, and school functioning according to the GAF scale (P<0.05). Depressive symptoms significantly decreased (P<0.05), and the general psychopathology score on the PANSS significantly improved (P<0.05). No significant differences were observed between WCST results at baseline and second evaluation. NAA/Cr ratios from the left frontal region at follow-up significantly correlated with WCST results (trials to complete first category, R=−0.942; P=0.005). Using a Bonferroni-corrected significance level of P≤0.003 (or 0.05/15), this correlation did not survive this correction. At baseline examination, we did not observe a significant correlation of the frontal NAA/Cr ratio with the WCST results. We found a significant correlation between the 5-year difference in frontal NAA levels and the duration of the last antipsychotic treatment in this period (R=0.908; P=0.012; Figure 2).
Table 2.
Clinical and cognitive findings in patients with schizophrenia during index hospitalization and at 5-year follow-up
| Baseline | Follow-up | P-value | |
|---|---|---|---|
| CGI | 4.64±0.92 | 3.91±1.22 | 0.066 |
| GAF | 49.1±9.70 | 59.5±16.80 | 0.011* |
| CDSS | 8.7±7.18 | 3.7±3.41 | 0.011* |
| PANSS total | 75.0±9.28 | 63.3±18.11 | 0.061 |
| PANSS positive | 17.8±3.25 | 14.8±5.12 | 0.059 |
| PANSS negative | 19.7±4.29 | 18.5±5.28 | 0.078 |
| PANSS general | 37.5±4.66 | 29.9±9.07 | 0.024* |
| TEs | 36.3±27.77 | 31.3±22.93 | 0.398 |
| PEs | 19.4±14.94 | 14.9±10.75 | 0.151 |
| NPEsa | 11.5 | 11.0 | 0.833 |
| CCsa | 6.0 | 6.0 | 0.422 |
| TCCsa | 11.5 | 12.0 | 0.865 |
Notes: Data given as mean ± SD or
median (variables with abnormal distribution, Shapiro–Wilk test). Wilcoxon’s test was used for testing group differences.
P<0.05.
Abbreviations: CGI, Clinical Global Impression; GAF, Global Assessment of Functioning; PANSS, Positive and Negative Syndrome Scale; CDSS, Calgary Depression Scale for Schizophrenia; TEs, total errors; PEs, perseverative errors; NPEs, nonperseverative errors; CCs, categories completed; TCCs, trials to complete first category.
Figure 2.
Correlation between 5-year difference in frontal NAA levels and duration of last antipsychotic treatment (R=0.908, P=0.012).
Abbreviation: NAA, N-acetylaspartate.
Discussion
According to our knowledge, the present study is one of few published longitudinal 1H MRS reports on schizophrenia. Aoyama et al10 followed 17 patients with schizophrenia for 80 months after diagnosis, Théberge et al11 examined 16 patients with a first episode before and after 10 and 30 months of antipsychotic treatment, and Bustillo et al12 scanned early-schizophrenia patients and repeated 1H MRS every 6 months up to 2 years (only six patients scanned at 2 years). We examined patients for a mean 67 months (~5 years) after the onset of the illness, which is one of the longest observations.
In our study, no significant differences in NAA/Cr or NAA/H2O ratios in the left frontal lobe, left temporal lobe, or left thalamus were identified between baseline and follow-up. Previous longitudinal 1H MRS studies in schizophrenia have shown conflicting short-term results: frontal NAA was reduced within the first year of treatment,22 but there were no changes in NAA in a 2-year evaluation;12 NAA reduction in the left anterior cingulate and left thalamus was found only between 10-month and 80-month assessments, but not between start point and 80 months;10 and in other 30-month study, NAA decrease was not found.11 The results of our study and others may show metabolite alterations at different stages of illness. Probably, NAA lowering develops gradually over the duration of illness and would be more noticeable in continuing observation. On the other hand, NAA reduction may be observed only within the first year of treatment,22 and potentially has a tendency to increase thereafter. It may also be that a larger group needs to be checked to show a real trend in NAA levels.
Since patients with schizophrenia have been treated with antipsychotic medications during long-term studies, NAA levels can be influenced by exposure to these medications. However, studies of patients with first-episode schizophrenia revealed no significant increase in previously lowered hippocampal and medial temporal NAA levels after 3 months of treatment.23,24 After 12 months of treatment with atypical antipsychotics, the NAA/Cr ratio in the dorsolateral prefrontal cortex did not significantly change in antipsychotic-naïve first-episode schizophrenia patients either.25 Studies of chronic patients with schizophrenia have demonstrated NAA changes associated with antipsychotic treatment.26–28 Therefore, type of antipsychotic treatment may have an impact on NAA levels. Increased NAA can be related to risperidone29 or clozapine treatment.30 On the contrary, patients receiving typical neuroleptics show lower NAA in the thalamus compared to controls.31 Moreover, there were no changes in NAA following treatment with haloperidol or quetiapine in one study.12 In two studies performed by Bustillo et al,12,32 the antipsychotic treatment was randomized-controlled.
In our study, we did not control the regimen of treatment: we used a naturalistic design, and patients were receiving various antipsychotics (atypical and typical) due to their clinical condition. Patients in our study benefited clinically from pharmacological treatment, and at followup they exhibited improvement in social functioning and clinical symptoms (better GAF and PANSS scores). Therefore, a correlation between the 5-year difference in frontal NAA/Cr levels and duration of the last antipsychotic treatment in this period shows that the lack of significant decrease in NAA levels might have been due to effective treatment of schizophrenia. A better clinical state of schizophrenia patients at follow-up might potentially also have been due to adaptation to the disease/treatment and be the reason for the result of no longitudinal decline in cognitive processes.
Inconsistent results have been found regarding choline levels in schizophrenia.33 Signals derived from choline-containing compounds are related to the concentration of phosphocholine and glycerophosphocholine, and choline level in 1H MRS is interpreted as a measure of overall cell density and alterations in neuron membrane or myelin turnover.27,33 Also, choline-containing compounds and mI connected with antigliadin antibodies may reflect brain inflammation in schizophrenia.34 In a longitudinal study by Aoyama et al,10 there was a trend of increasing thalamic choline levels at 80 months compared to the never-treated measure. In our study, we observed a trend toward a lower Cho/Cr ratio in the temporal lobe over 5 years, suggesting a longitudinal trend in cell density or impaired neuron-membrane or myelin function in this localization. In a study by Chang et al,35 choline in the right frontal white matter was shown to decrease with age in elderly schizophrenic subjects.
Earlier studies also found increased glutamate levels in the thalamus and cingulate cortex in schizophrenia, whereas after 24–80 months of treatment, glutamate levels in the thalamus had decreased.10,11 We found a trend toward a higher Glx/H2O ratio in the left thalamus over the 5 years of our study. The different result of a glutamate increase in our study might have been due to the neurodegenerative tendency of the thalamus.10 As in our study and the aforementioned,10,11 patients were treated with first- and second-generation antipsychotics, some differences in medications might not be excluded as a reason for these discrepancies in glutamate results.
In our study, cognitive function results did not significantly differ between the baseline examination performed in the first episode and after 5 years of schizophrenia. This is consistent with the results of other studies. Cognitive functions in patients with first-episode schizophrenia and recent-onset schizophrenia did not deteriorate over 5 years.36 In addition, an improvement in verbal IQ and full-scale IQ was correlated with a reduction in negative symptoms, which supports the view that negative syndrome is more strongly related to the level of cognitive functions than psychotic or disorganized syndrome. In our study, the level of negative symptoms had a tendency to improve, but not strongly enough to improve cognitive functions. In another study, there was no decline in cognitive functions over the first 2 years after a first episode of psychosis.37 In others, the cognitive decline observed in the first episode of schizophrenia remained relatively stable through at least 10 years of the illness,38 executive deficits were present in first-episode psychosis, but there was no progress over 10–12 years,39 and impairment in executive function was observed in schizophrenia through the various disease stages, and also the negative symptoms were able to be explained by that dysfunction.40 Studies of gene interactions with symptoms severity and cognitive functioning may also explain schizophrenia pathophysiology.41 We may also suggest that effective treatment might stop progression in cognitive deficit in our patients.
An important problem in longitudinal studies is to maintain the results from the same persons in subsequent examinations. The number of patients is decreasing in long-term 1H MRS examinations.12,24,25,32 In our study, subjects from the initial group (30 patients) were followed up, and only eleven (36%) were available for a second examination 5 years after the first examination (the remaining 19 patients were lost to medical observation). This problem occurs not only in neuroimaging studies but also in longitudinal studies of cognitive functions in patients with schizophrenia.38 Some factors have to be taken into consideration, eg, uncooperative patients or cooperative patients who fail to report for a follow-up or quit due to changes in their living situation. Therefore, our study has certain limitations. Firstly, the limited size of the patient group might have been insufficient to detect significant changes in NAA between two study points, because of variability measurements made by the same method in the same person.42 The absence of findings may also have been due to selection bias. However, our subsample of eleven patients did not differ clinically from the original sample of 30 patients. Secondly, we do not have results from a control group. Thirdly, we did not perform segmentation within the volume of interest. This procedure was not available in our study, and thus we cannot exclude the possibility of regional variations in metabolite concentration.43 Other limitations may also include low field strength (1.5 T) and no partial volume correction. The use of the unsuppressed water signal as an internal standard enhances the meaning of our results, because the observed creatine level was relatively stable. The strength of this study is its longitudinal design, which is one of the longest 1H MRS observations of schizophrenia patients in the literature.
Conclusion
Early-schizophrenia patients on neuroleptic treatment did not show significant regional NAA decline in the first 5 years of illness, which may have been due to the effect of schizophrenia treatment. A tendency shown toward lower Cho/Cr ratio in the temporal lobe over 5 years might point to a longitudinal trend in lower cell density or impaired neuron-membrane or myelin functions in the temporal lobe. A tendency toward higher glutamate levels might have been due to the involvement of thalamic dysfunction in the chronic schizophrenia process. Despite the choline and glutamate longitudinal changes/tendencies, these patients had no worsening of cognitive functions and a better clinical state. Further studies on large patient groups are required to check other long-term metabolic changes in different brain regions of schizophrenia patients.
Acknowledgments
This work was supported by a grant from the State Committee for Scientific Research (KBN, Poland): 3 PO5B 098 24.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Lieberman JA. Is schizophrenia a neurodegenerative disorder? A clinical and neurobiological perspective. Biol Psychiatry. 1999;46(6):729–739. doi: 10.1016/s0006-3223(99)00147-x. [DOI] [PubMed] [Google Scholar]
- 2.Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. 1987;44(7):660–669. doi: 10.1001/archpsyc.1987.01800190080012. [DOI] [PubMed] [Google Scholar]
- 3.Woods BT. Is schizophrenia a progressive neurodevelopmental disorder? Toward a unitary pathogenic mechanism. Am J Psychiatry. 1998;155(12):1661–1670. doi: 10.1176/ajp.155.12.1661. [DOI] [PubMed] [Google Scholar]
- 4.Dager SR, Oskin NM, Richards TL, Posse S. Research applications of magnetic resonance spectroscopy (MRS) to investigate psychiatric disorders. Top Magn Reson Imaging. 2008;19(2):81–96. doi: 10.1097/RMR.0b013e318181e0be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demougeot C, Marie C, Giroud M, Beley A. N-acetylaspartate: a literature review of animal research on brain ischaemia. J Neurochem. 2004;90(4):776–783. doi: 10.1111/j.1471-4159.2004.02583.x. [DOI] [PubMed] [Google Scholar]
- 6.Galińska-Skok B, Małus A, Konarzewska B, et al. Choline compounds of the frontal lobe and temporal glutamatergic system in bipolar and schizophrenia proton magnetic resonance spectroscopy study. Dis Markers. 2018 doi: 10.1155/2018/3654894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waszkiewicz N, Galińska-Skok B, Nestsiarovich A, et al. Neurobiological effects of binge drinking help in its detection and differential diagnosis from alcohol dependence. Dis Markers. 2018 doi: 10.1155/2018/5623683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iwata Y, Nakajima S, Plitman E, Mihashi Y, Caravaggio F, Chung JK. Neurometabolite levels in antipsychotic-naïve/free patients with schizophrenia: a systematic review and meta-analysis of 1H-MRS studies. Prog Neuropsychopharmacol Biol Psychiatry. 2018;30(86):340–352. doi: 10.1016/j.pnpbp.2018.03.016. [DOI] [PubMed] [Google Scholar]
- 9.Molina V, Sánchez J, Reig S, et al. N-acetyl-apartate levels in the dorsolateral prefrontal cortex in the early years of schizophrenia are inversely related to disease duration. Schizophr Res. 2005;73(2–3):209–219. doi: 10.1016/j.schres.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Aoyama N, Théberge J, Drost DJ, et al. Grey matter and social functioning correlates of glutamatergic metabolite loss in schizophrenia. Br J Psychiatry. 2011;198(6):448–456. doi: 10.1192/bjp.bp.110.079608. [DOI] [PubMed] [Google Scholar]
- 11.Théberge J, Williamson KE, Aoyama N, et al. Longitudinal grey-matter and glutamatergic losses in first-episode schizophrenia. Br J Psychiatry. 2007;191:325–334. doi: 10.1192/bjp.bp.106.033670. [DOI] [PubMed] [Google Scholar]
- 12.Bustillo JR, Rowland LM, Jung R, et al. Proton magnetic resonance spectroscopy during initial treatment with antipsychotic medication in schizophrenia. Neuropsychopharmacology. 2008;33(10):2456–2466. doi: 10.1038/sj.npp.1301631. [DOI] [PubMed] [Google Scholar]
- 13.Galińska B, Szulc A, Tarasów E, et al. Relationship between frontal N-acetylaspartate and cognitive deficits in first-episode schizophrenia. Med Sci Monit. 2007;13(Suppl 1):11–16. [PubMed] [Google Scholar]
- 14.Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64(6):663–667. doi: 10.4088/jcp.v64n0607. [DOI] [PubMed] [Google Scholar]
- 15.Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 16.Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: The Calgary Depression Scale. Br J Psychiatry Suppl. 1993;22:39–44. doi: 10.1192/S0007125000292581. [DOI] [PubMed] [Google Scholar]
- 17.Guy W. ECDEU Assessment Manual for Psychopharmacology. Washington, DC: US Department of Health, Education, and Welfare; 1976. [Google Scholar]
- 18.Galińska B, Szulc A, Tarasów E, et al. Duration of untreated psychosis and proton magnetic resonance spectroscopy (1H-MRS) findings in first-episode schizophrenia. Med Sci Monit. 2009;15(CR):82–88. [PubMed] [Google Scholar]
- 19.Murdoch JB, Lampman DA. Beyond Wet and Dry: Optimized Pulses for Water Suppression. Society of Magnetic Resonance in Medicine; New York. Twelfth Annual Meeting; 1993. p. 1191. [Google Scholar]
- 20.Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test Manual Revised and Expanded. Odessa (FL): Psychological Assessment Resources; 1993. [Google Scholar]
- 21.Heaton RK. Wisconsin Card Sorting Test: Computer Version 2 Research Edition. Odessa (FL): Psychological Assessment Resources; 1990. p. 1993. [Google Scholar]
- 22.Bustillo JR, Lauriello J, Rowland LM, et al. Longitudinal follow-up of neurochemical changes during the first year of antipsychotic treatment in schizophrenia patients with minimal previous medication exposure. Schizophr Res. 2002;58(2–3):313–321. doi: 10.1016/s0920-9964(02)00210-4. [DOI] [PubMed] [Google Scholar]
- 23.Fannon D, Simmons A, Tennakoon L, et al. Selective deficit of hippocampal N-acetylaspartate in antipsychotic-naive patients with schizophrenia. Biol Psychiatry. 2003;54(6):587–598. doi: 10.1016/s0006-3223(03)00185-9. [DOI] [PubMed] [Google Scholar]
- 24.Wood SJ, Berger GE, Wellard RM, et al. A 1H MRS investigation of the medial temporal lobe in antipsychotic-naïve early-treated first episode psychosis. Schizophr Res. 2008;102(1–3):163–170. doi: 10.1016/j.schres.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 25.Grošić V, Grošić PF, Kalember P, et al. The effect of atypical anti-psychotics on brain N-acetylaspartate levels in antipsychotic-naïve first-episode patients with schizophrenia: a preliminary study. Neuropsychiatr Dis Treat. 2014;10:1243–1253. doi: 10.2147/NDT.S61415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bertolino A, Callicott JH, Mattay VS, et al. The effect of treatment with antipsychotic drugs on brain N-acetylaspartate measures in patients with schizophrenia. Biol Psychiatry. 2001;49(1):39–46. doi: 10.1016/s0006-3223(00)00997-5. [DOI] [PubMed] [Google Scholar]
- 27.Szulc A, Galińska-Skok B, Waszkiewicz N, et al. Proton magnetic resonance spectroscopy changes after antipsychotic treatment. Curr Med Chem. 2013;20(3):414–427. [PubMed] [Google Scholar]
- 28.Choe BY, Suh TS, Shin KS, Lee CW, Lee C, Paik IH. Observation of metabolic changes in chronic schizophrenia after neuroleptic treatment by in vivo hydrogen magnetic resonance spectroscopy. Invest Radiol. 1996;31(6):345–352. doi: 10.1097/00004424-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Szulc A, Galińska B, Tarasów E, et al. The effect of risperidone on metabolite measures in the frontal lobe, temporal lobe and thalamus in schizophrenic patients. A proton magnetic resonance spectroscopy (1H MRS) study. Pharmacopsychiatry. 2005;38(5):214–219. doi: 10.1055/s-2005-873156. [DOI] [PubMed] [Google Scholar]
- 30.Ertrugrul A, Volkan-Salanci B, Koray B, et al. The effect of clozapine on regional cerebral blood flow and brain metabolite ratios in schizophrenia: relationship with treatment response. Psychiatry Res. 2009;174(2):121–129. doi: 10.1016/j.pscychresns.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 31.Szulc A, Galińska B, Tarasów E, et al. N-acetylaspartate (NAA) levels in selected areas of the brain in patients with chronic schizophrenia treated with typical and atypical neuroleptics: a proton magnetic resonance spectroscopy (1H MRS) study. Med Sci Monit. 2007;13(Suppl 1):17–22. [PubMed] [Google Scholar]
- 32.Bustillo JR, Rowland LM, Mullins P, et al. 1H MRS at 4 Tesla in minimally treated early schizophrenia. Mol Psychiatry. 2010;15(6):629–636. doi: 10.1038/mp.2009.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maddock RJ, Buonocore MH. MR spectroscopic studies of the brain in psychiatric disorders. Curr Top Behav Neurosci. 2012;11:199–251. doi: 10.1007/7854_2011_197. [DOI] [PubMed] [Google Scholar]
- 34.Rowland LM, Demyanovich HK, Wijtenburg SA, Eaton WW, Rodriguez K, Gaston F. Antigliadin antibodies (AGA IgG) are related to neurochemistry in schizophrenia. Front Psychiatry. 2017;8:104. doi: 10.3389/fpsyt.2017.00297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chang L, Friedman J, Ernst T, Zhong K, Tsopelas D, Davis K. Brain metabolite abnormalities in the white matter of elderly schizophrenic subjects: implication for glial dysfunction. Biol Psychiatry. 2007;62(12):1396–1404. doi: 10.1016/j.biopsych.2007.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gold S, Arndt S, Nopoulos P, O’Leary DS, Andreasen NC. Longitudinal study of cognitive function in first-episode and recent-onset schizophrenia. Am J Psychiatry. 1999;156(9):1342–1348. doi: 10.1176/ajp.156.9.1342. [DOI] [PubMed] [Google Scholar]
- 37.Addington J, Saeedi H, Addington D. The course of cognitive functioning in first episode psychosis: changes over time and impact on outcome. Schizophr Res. 2005;78(1):35–43. doi: 10.1016/j.schres.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 38.Hoff AL, Svetina C, Shields G, Stewart J, DeLisi LE. Ten year longitudinal study of neuropsychological functioning subsequent to first episode of schizophrenia. Schizophr Res. 2005;78(1):27–34. doi: 10.1016/j.schres.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 39.Stirling J, White C, Lewis S, et al. Neurocognitive function and outcome in first-episode schizophrenia: a 10-year follow-up of epidemiological cohort. Schizophr Res. 2003;65(2–3):75–86. doi: 10.1016/s0920-9964(03)00014-8. [DOI] [PubMed] [Google Scholar]
- 40.Orellana G, Slachevsky A. Executive functioning in schizophrenia. Front Psychiatry. 2013;4:35. doi: 10.3389/fpsyt.2013.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kandratsenka H, Nestsiarovich A, Goloenko I, et al. Association of mir137 with symptom severity and cognitive functioning in belarusian schizophrenia patients. Front Psychiatry. 2018;9:295. doi: 10.3389/fpsyt.2018.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Venkatraman TN, Hamer RM, Perkins DO, Song AW, Lieberman JA, Steen RG. Single-voxel 1H PRESS at 4.0 T: precision and variability of measurements in anterior cingulated and hippocampus. NMR Biomed. 2006;19(4):484–491. doi: 10.1002/nbm.1055. [DOI] [PubMed] [Google Scholar]
- 43.Auer DP, Wilke M, Grabner A, Heidenreich JO, Bronisch T, Wetter TC. Reduced NAA in the thalamus and altered membrane and glial metabolism in schizophrenic patients detected by 1H-MRS and tissue segmentation. Schizophr Res. 2001;52(1–2):87–99. doi: 10.1016/s0920-9964(01)00155-4. [DOI] [PubMed] [Google Scholar]