Abstract
Black/African American (black) women comprised 59% of women living with HIV at the end of 2014 and 61% of HIV diagnoses among women in 2015. Black women living with HIV infection (BWLH) have poorer health outcomes compared with women of other races/ethnicities; social and structural determinants are often cited as barriers and facilitators of care. The objective of this qualitative review was to identify social and structural barriers and facilitators of HIV treatment and care among BWLH. The systematic review was conducted in six-stages using databases such as PubMed, PsycINFO, and Google Scholar: 1) searched for studies that enrolled BWLH published between January 2005 and December 2016, 2) excluded unpublished reports and commentaries, 3) limited the search to our primary keywords, 4) limited our search to studies that included participants living with HIV infection that were >60% black and 100% female, 5) extracted and summarized the data, and 6) conducted a contextual review to identify common themes. Of 534 studies retrieved, 16 were included in the final review. Studies focused on: ART medication adherence (n = 5), engagement/retention in care (n = 4), HIV care and treatment services (n = 3), viral suppression (n = 1), and addressing multiple HIV care outcomes (n = 3). Main barrier themes included lack of family and/or social support, poor quality HIV services, and HIV-related stigma, particularly from healthcare providers; facilitator themes included resilience, positive relationships between case management and support services, high racial consciousness, and addressing mental health. Interventions that decrease these noted barriers and strengthen facilitators may help improve care outcomes for BWLH. Also, more HIV stigma-reduction training for healthcare providers may be warranted.
Keywords: HIV-positive, African Americans, women, HIV care continuum, disparities
Introduction
Black women comprised 59% of women living with HIV infection in 2014 and 61% of diagnoses among women in 2015 (CDC, 2016b). Reducing disparities in HIV diagnoses and improving the health of persons living with HIV infection (PLWH), including black women, aligns with national prevention goals (Office of National AIDS Policy, 2015). Early diagnoses, linkage to care, and retention in care are important steps for reducing HIV disparities and preventing HIV transmission (Skar- binski et al., 2015). Greater than 90% of new HIV infections are attributable to PLWH who are unaware of their status or not in care (Skarbinski et al., 2015).
Black women experience disparities in HIV treatment and care. Data from 61 health department jurisdictions indicated black women newly diagnosed with HIV and linked to HIV care within 90 days of diagnosis increased from 33.8% in 2012 to 50.1% in 2014 (Stein, Pierce, Hollis, & Smith, 2016). However, this was below the national target of 85%. Identifying factors associated with disparities in HIV treatment and care for black women is critical to increase the percentage who know their HIV status, are in HIV care, and are virally suppressed (Office of National AIDS Policy, 2015).
Thirty-six years after the identification of HIV infection in the United States (U.S.), there are no literature reviews focused exclusively on contextual factors that facilitate or limit access to HIV treatment and care among black women (Kennedy & Jenkins, 2011; Stampley, Mallory, & Gabrielson, 2005; Waite, Braw- ner, & Gipson-Jones, 2008). Such a review could identify the scant literature available regarding HIV treatment and care, support the need for more HIV research and interventions, and inform the quality of HIV treatment and care provided by healthcare professionals to black women. The purpose of this literature review is to identify possible social and structural factors related to the disparities in treatment and care among black women living with diagnosed HIV infection (BWLH).
Methods
The systematic review was conducted in six stages using PubMed, PsycINFO, Scopus, Embase, Global Health, OVID/Medline and Google Scholar. First, we searched for studies that enrolled BWLH published between January 2005 and December 2016. Second, we excluded abstracts, unpublished dissertations, editorials, commentaries and studies that were conducted outside of the U.S. Third, we limited the results to five areas of inquiry that address disparities in HIV treatment and care among black women: 1) biomedical (care, treatment, antiretroviral therapy (ART), medication adherence, viral suppression); 2) structural determinants of health (access to HIV care, patient-provider communication, quality of HIV care); 3) social determinants of health (stigma, discrimination, medical mistrust); 4) psychosocial context (peer support and mental health); and 5) social and sexual networks (sexual mixing, partner characteristics) (Office of National AIDS Policy, 2015; Maulsby et al., 2014). Fourth, we focused on studies that had majority representation of BWLH in the U.S., by requiring that the study population was >60% black and 100% female. Published quantitative and qualitative research studies that met the above inclusion criteria were included in the full-text review (Figure 1). Fifth, we extracted and summarized these data in a summary table that highlighted the author names, year, location, study design, sample size, age, HIV continuum of care category, and major findings (Hall et al., 2013) (Table 1). Sixth, we reviewed the articles and utilized direct content analysis to identify common themes for barriers and facilitators for HIV care (Hsieh & Shannon, 2005) (Table 2).
Figure 1.
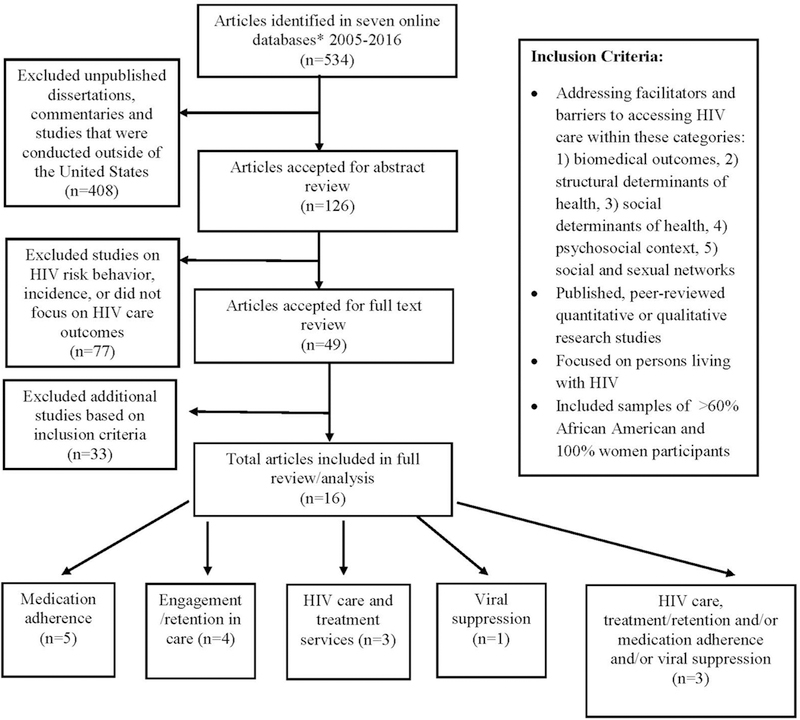
Selection process for systematic review of the literature, HIV care outcomes among HIV-Positive black women, 2005–2016. *The literature search included the following databases: PubMed, PsycINFO, Scopus, Embase, Global Health, OVID/Medline and Google Scholar.
Table 1.
Literature review findings of social and structural barriers and facilitators contributing to HIV treatment and care disparities among black women.
| First author, year | Source of the data, location |
Study population |
N, % African American, % female, age mean years (SD) or (range) |
Methodology | HIV care continuum category |
Major findings |
|---|---|---|---|---|---|---|
| Baker et al. (2014) | Secondary data analysis, Northeast U.S. | Patients of an HIV Care Clinic | N =157; 100% African Americans in the analysis; 100% female; 39.85 (SD = 8.72) | Randomized, controlled, intervention; ACASI questionnaire implemented at baseline and follow-up; baseline data used for analysis | HIV care and treatment services | • Satisfaction with medical services (88%, n = 140) • Communication with healthcare providers, detectable viral load, education, income, self-reported health status, and sexual orientation were significantly associated with satisfaction with healthcare (p <.05 for all outcomes) |
| Brody et al. (2016) | Primary data collection, Midwest, U.S. | Participants of the Interagency HIV Study (WIHS) | N = 22; 98% African Americans in the analysis; 100% female; 46.51 (SD = 13.05) | Qualitative narrative, autobiographical and interview design | Medication adherence | • Mutuality-fostering relationships involving reciprocal care and empathy • Self-awareness-recognition of personal strengths and weaknesses and multiple factors contributing to life choices and trajectories • Self-efficacy-active coping, self-advocacy, and utilizing resources |
| Buseh, Kelber, Stevens, and Park (2008) | Primary data collection, Midwest, U.S. | Community-based purposive recruitment | N = 29; 100% African American in the analysis; 100% female; 40.0 (range: 25–54)a | Qualitative narrative interview design, data collections – 2000–2003; 10 face-to-face interviews lasting 2–3 h | Retention in care | • Multi-level encounters with HIV-related stigma including family, friends, and healthcare providers |
| Dale et al. (2014) | Primary data collection, Midwest, U.S. | Ruth M. Rothstein CORE Center/ Cook County Health and WIHS | N =138; 87% African American; 100% female; 45.74 (SD = 8.38) | Cross-sectional questionnaire of a longitudinal study | Medication adherencea Viral suppression | • High resilience and increased HAART adherence (OR = 1.08, 95% CI 1.00–1.15) • High resilience and decreased detectable viral load (OR = 0.94, 0.89–0.99) |
| Dalmida, Holstad, DiIorio, and Laderman (2012) | Primary data collection, Southeast, U.S. | Patients from a large infectious disease center | N = 20; 100% African Americans in the analysis; 100% female; 46.8 (SD = 6.5) | Two group sessions using focus group methodology; Six individual interviews using a focus group guide, a semi structured interview script, and a phenomenological approach | Medication adherence | • Spirituality, when integrated with HIV care and treatment services, improved patients’ medication adherence |
| Edwards (2006) | Primary data collection, Northeast U.S. | Patients from Johns Hopkins Medical Institution - Moore Clinic | N = 20; 100% African Americans in the analysis; 100% female; (range: 20–49)a | Journal entries and semi-structured interviews | Medication adherence | • HIV-related stigma, relationship turbulence, and prioritization of caring for others over their personal care as barriers to medication adherence. • Social support from family members was facilitator to medication adherence |
| Edwards, Irving, Amutah, and Sydnor (2012) | Secondary data analysis, Northeast, U.S. | Patients from Johns Hopkins Medical Institution - Moore Clinic | N = 20; 100% African Americans in the analysis; 100% female; (range: 20–49)a | Journal entries and semi-structured interviews | Medication adherence | • Social support was a facilitator of medication adherence |
| Fletcher et al. (2016) | Secondary data analysis, Southeast, U.S. | Patients of five South Carolina clinics or AIDS organizations | N = 42; 100% African Americans in the analysis, 100% female; 37.7 (SD = 9.2) | In-depth face-to-face interviews | Retention in care | • Multilevel HIV-related stigma •Stigma subsequently complicated disclosure decisions, resulting in limited support in social, professional and medical settings |
| Halkitis, Kupprat, and Mukherjee (2010) | Retrospective data analysis, Northeast, U.S. | Analysis of case management records, support services records, and medical charts | N = 46; 63.0% African Americans in the analysis; 100% female; 46.58 (SD = 5.98) | Examined descriptive and relational data | HIV care and treatment services | • Positive relationships between case management and supportive services increased HIV care and treatment services |
| Kelso et al. (2014) | Primary data collection, Midwest, U.S. | Recruited through the CORE Center Site of the Chicago Women’s Interagency HIV Study | N = 67; 100% African Americans in the analysis; 100% female; 44.9 (SD = 8.93) | Detailed, structured interview; brief physical and gynecologic examinations; semi-annual specimens; Self-report data | Viral suppression | • Black women who perceived high racial discrimination, yet reported high critical consciousness were • Less likely to have a detectable viral load (B = −0.79, p = 0.03, odds ratio = 0.45) • More likely to have CD4 cell counts above 350 (B = 1.00, p = 0.06, odds ratio = 2.72) |
| McDoom, Bokhour, Sullivan, and Drainoni (2015) | Primary data collection, Northeast, U.S. | Patients from a primary care clinic in Metropolitan Boston Area | N = 20; 100% African Americans in the analysis; 100% female; 56 (range 50–63)a | Semi-structured interviews | Retention in care | • Social support was a facilitator for consistent • HIV care retention HIV-related stigma, particularly from healthcare providers, was a barrier to continuity of care |
| Toth, Messer, and Quinlivan (2013) | Primary data collection, Southern, U.S. | Patients from a primary care clinic | N =140; 85% African American in the analysis; 100% female; 46.1 (SD 10.43) | Cross-sectional survey | HIV care and treatment | • Depression, illness severity, and psychological abuse were associated with >5 barriers to HIV care and services |
| Vyavaharkar, Moneyham, and Corwin (2008) | Primary data collection, Southeast, U.S. | Recruited through community based organizations and university based research study of rural women with HIV disease | N = 22; 100% African Americans in the analysis; 100% female; 44 (SD 9.24) | Focus groups | HIV care and treatment services and retention in carea | • Lack of transportation, stigma, lack of support, housing and childcare, dissatisfaction with quality of care services, limited availability of services were barriers to continuity of HIV care |
| Vyavaharkar et al. (2010) | Secondary data collection, Southeast, U.S. | Recruited from community- based consortiums that provide HIV prevention and care | N = 340; 100% African Americans in the analysis; 100% female; 41.25 (9.47) | Self-reported data; cross-sectional questionnaire | Medication adherence | • Addressing depressive symptoms through social support facilitated patients’ engagement in long-term HIV care |
| Walcott, Kempf, Merlin, and Turan (2016) | Primary data collection, Southeast, U.S. | Recruitment through HIV care clinics and a residential facility for HIV-positive persons; Included service providers (n = 14) and women living with HIV (n = 46) | N = 60; 89% African American; 100% female; 44.6 (SD = 9.6) | In-depth interviews (service providers); focus groups (HIV-positive women) | Engagement/retention in care | • Structural community factors, such as poverty, poor employment opportunities, limited access to healthcare resources, stigma, transportation challenges and access to illicit substances, were barriers to engaging in HIV care |
| Wyatt, Carmona, Loeb, and Williams (2005) | Primary data collection, West, U.S. | Patients of community-based clinics, county hospitals, ethnicity- and AIDS specific organizations and drug rehabilitation centers | N =75; 100% African Americans in the analysis; 100% female; 40 (SD = N/A) | Structured interview assessment | Engagement/Retention in care HIV Care and Treatment Services | • Substance use, confidentiality issues, limited financial resources, difficulty in getting an appointment, excessive waiting for healthcare provider, caring for others (family and friends) were barriers to continuity of HIV care |
Table 2.
Emergent themes for barriers and facilitators for HIV care and treatment among black women, 2005–2016.
| Barriers to care | Facilitators for care |
|---|---|
| • HIV-related stigma among family and friends | • High resilience |
| • HIV-related stigma among healthcare providers | • Comprehensive and integrated services - including Spirituality components for enhancement of care |
| • Poor quality of HIV care services, including confidentiality concerns, difficulty in getting an appointment, excessive waiting for healthcare provider | • Positive relationships between case management and supportive services |
| • Inadequate social support | • Social support from family and friends |
| • Unmet needs beyond HIV treatment and care including, limited financial resources, lack of childcare, housing, and reliable transportation | • High racial consciousness in the context of perceived racism |
| • Relationship turbulence, and prioritization of caring for others over their personal care | • Addressing symptoms of depression |
| • Substance use | |
Results
We screened 534 relevant titles and abstracts; 49 were selected for full review; 16 articles met inclusion criteria for final analysis (Figure 1). The 16 studies were conducted throughout the U.S. including the Northeast (n = 5), Southeast (n = 6), Midwest (n = 4), and West (n = 1) (Table 1). Barriers and facilitators of care and ART adherence emerged during the review and are summarized in Table 2.
ART medication adherence
Five individual studies and one study with multiple outcomes addressed social and structural determinants of ART adherence to HIV therapy (Brody et al., 2016; Dale et al., 2014; Dalmida et al., 2012; Edwards, 2006; Edwards et al., 2012; Vyavaharkar et al., 2010). Dalmida et al. (2012) found that black women attributed the integration of spirituality with their HIV care to improvement in their ART adherence. Diagnosing and managing depressive symptoms associated with HIV diagnosis and HIV-related stigma (Vyavaharkar et al., 2010), high levels of self-awareness (Brody et al., 2016; Dale et al., 2014) and self-efficacy (Brody et al., 2016) were also noted as facilitators to improving ART adherence. Other barriers and facilitators of ART adherence included HIV-related stigma, relationship turbulence, prioritization of caring for others over their personal care (Edwards, 2006) and social support from family members (Edwards, 2006; Edwards et al., 2012; Vyavaharkar et al., 2010).
Engagement/retention in care
Four individual studies and two studies with multiple outcomes examined barriers to engagement and/or retention in care, with HIV-related stigma being the most noted barrier to consistent access to and utilization of HIV care services (Buseh & Stevens, 2007; Fletcher et al., 2016; McDoom et al., 2015; Vyavaharkar et al., 2008; Walcott et al., 2016; Wyatt et al., 2005). These studies all demonstrated that black women have multi-level encounters with HIV-related stigma, from family, friends, religious groups, healthcare providers, employers, and prison employees s. Three studies examined factors beyond the scope oftreatment, and identified unmet social and structural needs as barriers to engaging in care, including transportation, housing, childcare (Vyavahar-kar et al., 2008), caring for others (Wyatt et al., 2005), poverty, poor employment opportunities, and limited access to healthcare resources (Walcott et al., 2016).
HIV care and treatment services
Three individual studies and two studies with multiple outcomes examined quality and access to HIV care (Baker, Rodgers, Davis, Gracely, & Bowleg, 2014; Halki-tis et al., 2010; Toth et al., 2013; Vyavaharkar et al., 2008; Wyatt et al., 2005). Dissatisfaction with the quality of HIV care, and limited access, were barriers to engaging in HIV care (Baker et al., 2014; Halkitis et al., 2010; Vyavaharkar et al., 2008; Wyatt et al., 2005). Explanations for patient dissatisfaction included poor attitudes and behaviors of healthcare providers, lack of patient-provider communication, not addressing depression, and a lack of integrated services; women indicated how integrated services would increase their access to care and decrease patient burden (Toth et al., 2013; Vyavaharkar et al., 2008). Facilitators of engaging in HIV care included stable housing, childcare, transportation, and peer support (Halkitis et al., 2010; Toth et al., 2013; Vyavaharkar et al., 2008; Wyatt et al., 2005). Halkitis et al. (2010) found that women with higher utilization of support services such as transportation, primary healthcare/medical specialists, and support groups, had more encounters with their case managers and were more consistent in their HIV treatment and care.
Viral suppression
One individual study and one study with multiple outcomes examined social and structural determinants of viral suppression (Dale et al., 2014; Kelso et al., 2014). Black women who perceived high racial discrimination and reported high critical consciousness (cultural self-awareness) were significantly less likely to have a detectable viral load and more likely to have CD4 cell counts above 350 cells/mm3 (Kelso et al., 2014). Dale et al. (2014) examined resilience and viral load; black women with high levels of resilience had lower viral loads than their counterparts.
Discussion
Our review suggests that social and structural factors, including suboptimal patient-provider communication, HIV-related stigma, lack of social support, and unmet needs (e.g., transportation, financial stability, and childcare) all contribute to challenges in HIV treatment and care for black women. Available studies (Table 1) suggest that social and structural factors (Table 2) need to be considered by providers, and underscore the importance of relationships and communication between patients, providers, and the support networks of BWLH.
The finding of healthcare provider stigma as a barrier for HIV care and treatment is of concern and is aligned with a study which reported negative clinical encounters by black compared with white HIV-infected women (Beach et al., 2011). Training physicians to more effectively engage patients in non-stigmatizing dialogue and empowering black women to address specific topics with their providers may be important strategies for improving communication and satisfaction with HIV care services (Beach et al., 2011).
These studies suggest important roles for interventions through healthcare providers (Gaston, Gutierrez, & Nisanci, 2015). Culturally tailored communication strategies, developed with affected communities of black women, is also an additional tool for improving care for BWLH (Arya, Behforouz, & Viswanath, 2009). It is vital that we improve trust, increase culturally appropriate care, and actively follow-up on missed visits, to strengthen engagement and retention in care for BWLH (Aziz & Smith, 2011; El-Bassel, Caldeira, Ruglass, & Gilbert, 2009). Moreover, addressing depression, unmet needs (i.e., childcare, unemployment, and housing), and increasing peer-support may be well-received if these factors are considered as part of care for BLWH (Rao et al., 2012; Toth et al., 2013).
This review has limitations. First, nine of 16 (60%) studies included small sample sizes, larger samples of black women will be needed for future studies, to provide for more robust analyses and be generalizable to larger groups of women. Second, factors such as geographic location may play unique role for black women, especially in the southern U.S., an area which has a historical context of institutional racism (i.e., limited or no resources available due to a lack of insurance coverage) which may create additional HIV prevention and care challenges for people of color (Adimora, Ramirez, Schoenbach, & Cohen, 2014). Third, many of the studies were qualitative and included face-to-face interviews; social desirability biases may have played a role in some responses. Using computer-assisted quantitative surveys may offer additional privacy and decrease this type of bias.
Conclusion
Given the disproportionate burden of HIV infection among black women in the U.S., (CDC, 2016b) the development of social and structural interventions that increase accessibility and acceptability to services are vital. Moreover, of 84 Centers for Disease Control and Prevention evidence-based HIV interventions (CDC, 2016a), none were developed exclusively for BWLH. In order to reach national HIV prevention goals for women of color, future studies, with larger samples of BWLH, are needed to increase the number of culturally appropriate interventions and evidence-based practices for addressing social and structural factors that impede treatment and care for BWLH. Findings discussed in this manuscript support the need to address the ongoing disparities in HIV treatment and care among black women.
Acknowledgements
The authors equally contributed to the conception, data collection, data analysis, data interpretation, writing, and final development of this manuscript. The authors have no funding sources and financial conflicts to report.
Footnotes
Disclosure statement
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official views of their affiliated institute.
Geolocation
Data for this study were collected in the U.S.
No potential conflict of interest was reported by the authors.
References
- Adimora AA, Ramirez C, Schoenbach VJ, & Cohen MS (2014). Policies and politics that promote HIV infection in the Southern United States. AIDS, 28, 1393–1397. doi: 10.1097/QAD.0000000000000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arya M, Behforouz HL, & Viswanath K (2009). African American women and HIV/AIDS: A national call for targeted health communication strategies to address a disparity. The AIDS Reader, 19, 79–C3. [PMC free article] [PubMed] [Google Scholar]
- Aziz M, & Smith KY (2011). Challenges and successes in linking HIV-infected women to care in the United States. Clinical Infectious Diseases, 52(Suppl 2), S231–S237. doi: 10.1093/cid/ciq047 [DOI] [PubMed] [Google Scholar]
- Baker JL, Rodgers CR, Davis ZM, Gracely E, & Bowleg L (2014). Results from a secondary data analysis regarding satisfaction with health care among African American women living with HIV/AIDS. Journal of Obstetric, Gynecologic, & Neonatology Nursing, 43, 664–676. [DOI] [PubMed] [Google Scholar]
- Beach MC, Saha S, Korthuis PT, Sharp V, Cohn J, Wilson IB,... Moore, R. (2011). Patient-provider communication differs for black compared to white HIV- infected patients. AIDS and Behavior, 15, 805–811. doi: 10.1007/s10461-009-9664-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody LR, Jack DC, Bruck-Segal DL, Ruffing EG, Firpo-Perretti YM, Dale SK,... Cohen MH (2016). Life lessons from women with HIV: Mutuality, self-awareness, and self-efficacy. AIDS Patient Care and STDs, 30, 261–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buseh AG, Kelber ST, Stevens PE, & Park CG (2008). Relationship of symptoms, perceived health, and stigma with quality of life among urban HIV-infected African American men. Public Health Nursing, 25(5), 409–419. doi: 10.1111/phn.2008.25.issue-5 [DOI] [PubMed] [Google Scholar]
- Buseh AG, & Stevens PE (2007). Constrained but not determined by stigma: Resistance by African American women living with HIV. Women & Health, 44, 1–18. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2016a). Compendium of evidence-based interventions and best practices for HIV prevention. Retrieved from https://www.cdc.gov/hiv/research/interventionresearch/compendium/ma/index.html
- Centers for Disease Control and Prevention (CDC). (2016b). HIV surveillance report, 2015. Vol. 27. Retrieved from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- Dale S, Cohen M, Weber K, Cruise R, Kelso G, & Brody L (2014). Abuse and resilience in relation to HAART medication adherence and HIV viral load among women with HIV in the United States. AIDS Patient Care and STDs, 28, 136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalmida SG, Holstad MM, DiIorio C, & Laderman G (2012). The meaning and use of spirituality among African American women living with HIV/AIDS. Western Journal of Nursing Research, 34, 736–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards LV (2006). Perceived social support and HIV/AIDS medication adherence among African American women. Qualitative Health Research, 16, 679–691. [DOI] [PubMed] [Google Scholar]
- Edwards LV, Irving SM, Amutah NN, & Sydnor KD (2012). Am I my mother’s keeper? Children as unexpected sources of social support among African American women living with HIV-AIDS. Journal of Black Studies, 43, 571–595. [Google Scholar]
- El-Bassel N, Caldeira NA, Ruglass LM, & Gilbert L (2009). Addressing the unique needs of African American women in HIV prevention. American Journal of Public Health, 99(6), 996–1001. doi: 10.2105/AJPH.2008.140541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher F, Ingram LA, Kerr J, Buchberg M, Richter DL, & Sowell R (2016). “She told them, oh that bitch got AIDS”: Experiences of multilevel HIV/AIDS-related stigma among African American women living with HIV/ AIDS in the south. AIDS Patient Care and STDs, 30, 349–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaston GB, Gutierrez SM, & Nisanci A (2015). Interventions that retain African Americans in HIV/AIDS treatment: Implications for social work practice and research. Social Work, 60(1), 35–42. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Kupprat SA, & Mukherjee PP (2010). Longitudinal associations between case management and supportive services use among black and Latina HIV-positive women in New York City. Journal of Women’s Health, 19(1), 99–108. [DOI] [PubMed] [Google Scholar]
- Hall HI, Frazier EL, Rhodes P, Holtgrave DR, Furlow- Parmley C, Tang T,... Skarbinski J (2013). Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Internal Medicine, 173, 1337–1344. doi: 10.1001/jamainternmed.2013.6841 [DOI] [PubMed] [Google Scholar]
- Hsieh H, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15, 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Kelso GA, Cohen MH, Weber KM, Dale SK, Cruise RC, & Brody LR (2014). Critical consciousness, racial and gender discrimination, and HIV disease markers in African American women with HIV. AIDS and Behavior, 18, 1237–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy BR, & Jenkins CC (2011). Promoting African American women and sexual assertiveness in reducing HIV/AIDS: An analytical review of the research literature. Journal of Cultural Diversity, 18(4), 142–149. [PubMed] [Google Scholar]
- Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, & Holtgrave D (2014). HIV among black men who have sex with men (MSM) in the United States: A review of the literature. AIDS and Behavior, 18(1), 10–25. doi: 10.1007/s10461-013-0476-2 [DOI] [PubMed] [Google Scholar]
- McDoom MM, Bokhour B, Sullivan M, & Drainoni ML (2015). How older black women perceive the effects of stigma and social support on engagement in HIV care. AIDS Patient Care and STDs, 29, 95–101. [DOI] [PubMed] [Google Scholar]
- Office of National AIDS Policy. (2015). National HIV/AIDS Strategy for the United States: Updated to 2020. Washington, DC: Author; Retrieved from https://www.aids.gov/federalresources/national-hiv-aids-strategy/overview/index.html [Google Scholar]
- Rao D, Desmond M, Andrasik M, Rasberry T, Lambert N, Cohn SE, & Simoni J (2012). Feasibility, acceptability, and preliminary efficacy of the unity workshop: An internalized stigma reduction intervention for African American women living with HIV. AIDS Patient Care and STDs, 26 (10), 614–620. doi: 10.1089/apc.2012.0106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skarbinski J, Rosenberg E, Paz-Bailey G, Hall I, Rose CE, Abigail HV,... Mermin JH (2015). Human immunode ficiency virus transmission at each step of the care continuum in the United States. JAMA Internal Medicine, 175, 588–596. [DOI] [PubMed] [Google Scholar]
- Stampley CD, Mallory C, & Gabrielson M (2005). HIV/ AIDS among midlife African American women: An integrated review of literature. Research in Nursing & Health, 28(4), 295–305. [DOI] [PubMed] [Google Scholar]
- Stein R, Pierce T, Hollis N, & Smith J (2016). HIV testing and service delivery among black females — 61 health department jurisdictions, United States, 2012–2014. MMWR. Morbidity and Mortality Weekly Report, 65, 83–85. [DOI] [PubMed] [Google Scholar]
- Toth M, Messer LC, & Quinlivan EB (2013). Barriers to HIV care for women of color living in the southeastern US are associated with physical symptoms, social environment, and self-determination. AIDS Patient Care and STDs, 27, 613–620. doi: 10.1089/apc.2013.0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyavaharkar MV, Moneyham L, & Corwin S (2008). Health care utilization: The experiences of rural HIV-positive African American women. Journal of Health Care for the Poor and Underserved, 19(1), 294–306. [DOI] [PubMed] [Google Scholar]
- Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, & Tavakoli A (2010). Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural southeastern United States. Journal of the Association of Nurses in AIDS Care, 21, 144–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite R, Brawner B, & Gipson-Jones TL (2008). Factors that shape mental health treatment-seeking behaviors of HIV-positive African-American women with depressive symptoms: A review of the literature. Journal of National Black Nurses’ Association, 19(2), 50–58. [PubMed] [Google Scholar]
- Walcott M, Kempf MC, Merlin JS, & Turan JM (2016). Structural community factors and sub-optimal engagement in HIV care among low-income women in the deep south of the USA. Culture, Health & Sexuality, 18, 682–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt GE, Carmona JV, Loeb TB, & Williams JK (2005). HIV-positive black women with histories of childhood sexual abuse: Patterns of substance use and barriers to health care. Journal of Health Care for the Poor and Underserved, 16(4 Suppl B), 9–23. [DOI] [PubMed] [Google Scholar]


