Abstract
Among places where people living with HIV experience and anticipate HIV-related stigma, stigma in health care settings may be particularly harmful. Utilizing an exploratory sequential mixed methods approach, we conducted interviews (n = 76) and questionnaires (N = 460) with older adult women living with HIV enrolled in the Women's Interagency HIV Study in Birmingham, AL; Jackson, MS; Atlanta, GA; and San Francisco, CA. Interviews addressed facilitators and barriers to HIV treatment adherence, including HIV-related stigma. Qualitative data were coded using thematic analysis. Questionnaires assessed self-reported antiretroviral therapy (ART) adherence and experienced and anticipated HIV-related stigma from various sources (i.e., health care personnel, family, partner, and community). Covariate-adjusted logistic regression analyses examined total and mediated effects of stigma on ART adherence. Interviewees described fears and experiences of stigma in health care settings; including privacy violations, disrespect for patient autonomy, and reproductive coercion; and how these influenced their adherence to HIV treatment recommendations. Experienced and anticipated HIV-related stigma in health care settings were associated with suboptimal (or <95%) ART adherence in separate models controlling for experienced or anticipated stigma, respectively, from other sources. When entered together, only anticipated stigma in health care settings was associated with suboptimal ART adherence, controlling for anticipated and experienced stigma from other sources. The effect of anticipated stigma in health care settings on suboptimal ART adherence may work through the pathways of lower adherence self-efficacy, higher depressive symptoms, and higher coping by substance use. These findings indicate that interventions should promote cultures of acceptance within health care settings and resilience-based strategies for women to combat stigma and promote life-sustaining behaviors.
Keywords: HIV/AIDS, antiretroviral therapy, mixed methods, adherence, stigma, mental health
Introduction
HIV-related stigma is a pervasive barrier to HIV prevention and treatment, and to curbing related adverse physical health outcomes,1 by way of compromised psychological, social, and emotional well-being of people living with HIV (PLWH).2 HIV-related stigma is conceptualized as operating in multiple dimensions and includes acts of social devaluation (or experienced stigma) and fears of negative social evaluation (or anticipated stigma). Furthermore, stigma can have a variety of sources (e.g., institutions, communities, individuals, etc.).3
Experienced and anticipated stigma in health care settings may be particularly detrimental to health care engagement among PLWH, as these are the places they turn to for life-saving treatment and support services.4 PLWH in multiple settings globally have reported experiencing and anticipating HIV-related stigma in health care settings; such as undue physical distancing and avoidance,5 excessive precautionary measures,6 and care refusal.7,8 These events may undermine the delivery of quality health care services, and fears of these events among PLWH hinder subsequent HIV care utilization.9
Women living with HIV (WLWH) may be highly susceptible to the harmful consequences of HIV-related stigma in health care settings. Compared to men, WLWH in the United States have lower antiretroviral therapy (ART) adherence and higher morbidity and mortality.10 Minority women [women with social group characteristics or identities (race, ethnicity, income-level, gender, age, geographic location, etc.) that are historically subject to social disadvantage relative to majority groups],11,12 in particular, are vulnerable to adverse health outcomes associated with HIV infection.13
A recent study indicated that HIV-positive women who were newly diagnosed at several health care sites in a large metropolitan US city were predominantly African American or black, had a higher baseline CD4 count at diagnosis, and had lower odds linkage to care postdiagnosis compared with men.14 Other studies indicate that black women in the United States are less likely to be linked to HIV care and virally suppressed, compared with white and Hispanic/Latina women.15–17 US Hispanic/Latina women and women who attend public HIV clinics are also less likely to be virally suppressed compared with white women and women attending private HIV clinics, respectively.17
Women in US South may be especially burdened by the negative health effects of HIV-related stigma in health care settings. The US HIV epidemic is highly concentrated within southern US states, with most of new HIV diagnoses and deaths attributed to HIV occurring in this region.18 Gender, racial, and ethnic disparities are also more pronounced in the US South, where women and black PLWH have lower probabilities of HIV and AIDS survival once diagnosed and higher rates of death, compared with men and other racial groups.19 Further, several states in the region have taken legal and policy action or inaction that impedes access to HIV care, largely among lower income women, including restrictive Medicaid income eligibility criteria, lower Medicaid benefits, lack of Medicaid expansion, and lower contributions to state Ryan White AIDS Drug Assistance Programs.20
Minority WLWH contend with stigma in various settings due to their unique positioning at the intersections of multiple social group identities.21 Stigmas experienced by minority WLWH may produce greater stress, anxiety, or depression, ultimately compromising women's motivation to engage in life-sustaining health behaviors such as engagement in HIV care.3,22 Recent studies suggest that these pathways, from specific dimensions of HIV-related stigma to HIV treatment outcomes through psychosocial and mental health mediators, may be present only for specific population groups: for women of color and not for white women,23 and for men yet not for women.24 However, there is a dearth of research evidence regarding the unique effects of anticipated and enacted stigma in US health care settings, while controlling for other sources of stigma, among minority WLWH.
The present study seeks to address this literature gap through a mixed methods analysis of data from WLWH in four US cities, mostly in the South, regarding their experiences and anticipation of HIV stigma in health care and other settings using validated multi-item measures. Data regarding the specific health implications of stigma in health care settings for WLWH may help develop targeted strategies to reduce the negative health manifestations of stigma. This analysis in particular examines effects of stigma in health care settings on engagement in HIV care, and potential psychosocial mechanisms for these effects (i.e., adherence self-efficacy, depressive symptoms, and coping by substance use) suggested by prior literature.25–27 Findings may inform behavioral intervention strategies that serve WLWH by revealing potential opportunities for support in reaching desired health goals.
Methods
The present analysis was conducted as part of a substudy of the Women's Interagency HIV Study (WIHS), an ongoing multisite prospective cohort study.28,29 The Women's Adherence and Visit Engagement (WAVE) substudy uses an exploratory sequential approach to collect, analyze, and integrate qualitative interview and quantitative survey data from selected WIHS sites to examine how HIV-related and other intersecting stigmas affect adherence to HIV treatment recommendations and HIV clinical outcomes among WLWH, and inform future intervention studies.
From 2016 through 2017, adult WLWH were enrolled in the WAVE substudy at the Birmingham, AL and Jackson, MS site (these two locations work together as a single WIHS site), the Atlanta, GA site, and the San Francisco, CA site. These specific sites were selected to represent different parts of the country—California (San Francisco), the Deep South (Alabama/Mississippi), and the Southeast (Georgia). The southern sites in particular are newer additions to WIHS (beginning in 2013 whereas other WIHS sites began recruitment a decade earlier) and increased the presence of younger women, racial minority women, and newly diagnosed women enrolled in WIHS.
All participants provided written informed consent, and study procedures were approved by the WIHS Executive Committee and the Institutional Review Boards at each participating WIHS site. WLWH were recruited for participation in the qualitative interviews by WIHS staff using purposive sampling to achieve diverse demographic representation (by race, ethnicity, and income) and a sufficient number of participants at each site. Women who could complete questionnaires in the English were invited by WIHS staff to participate in the interviewer-administered questionnaire.
Data collection and analysis
Qualitative interviews
Interviews were conducted by researchers who have experience in qualitative methods and in-depth interviewing and identify as female. Interview guides were used to facilitate discussion around barriers and facilitators related to HIV treatment adherence, including perceptions and experiences of stigma from various sources. Sample questions included, “In what areas of life (e.g., health care, work, family) have you experienced stigma or discrimination?” and “How have the negative ways that women living with HIV are viewed or treated by others impacted your life?”
Interviews were audio recorded and transcribed by professional transcriptionists. A four-person team of coders developed a coding framework through an iterative process and applied codes using thematic analysis methods in Dedoose.30,31 Sampling, data collection, and analysis procedures for the qualitative phase of this substudy are described in greater detail elsewhere.21
Quantitative questionnaire
Preliminary findings from the qualitative data were used to inform the development of a structured questionnaire with multi-item scales assessing stigma and other relevant constructs (i.e., coping, self-efficacy, disclosure concerns, food and financial insecurity, resilience, etc.) previously validated in different study samples, in some cases, including WLWH. The questionnaire included 12 items adapted from the Earnshaw et al. HIV stigma mechanisms measure to assess whether participants experienced stigma related to HIV status within the past year from 4 sources: health care workers, family members, sexual/romantic partner, and neighbors/others in the community (3 items for each source; α = 0.92).2 An additional 12-item parallel scale assessed anticipated stigma from the same sources (α = 0.91).
Variables to represent experienced and anticipated stigma from health care workers and others (family members, sexual/romantic partner, and neighbors/others in the community) were created from the mean of the three items that measured stigma in each setting both scales (see Table 2 for item descriptions for stigma in health care settings). The adapted scales were validated previously in a different study sample of men and WLWH in the US South.26
Table 2.
Quantitative Questionnaire Items, Mean Scores, and Related Sample Qualitative Quotes by Anticipated and Experienced Stigma
| Quantitative itema | Mean (SD)b | Illustrative quote |
|---|---|---|
| Anticipated stigma | ||
| Health care workers will not listen to my concerns. | 1.83 (1.06) | “[A] lady that worked [at the clinic] had leaked my [HIV] status out. So that had me really apprehensive until I just started going back to the doctor. The [new] doctor is very kind, concerned…” (black participant, MS site) |
| Health care workers will avoid touching me. | 1.81 (1.04) | Recount of a scenario where the participant's expectation differed from reality: “I got into a car accident. I went over to the emergency room and I was ashamed to be there…. I was afraid. How are these people going to treat me? I was on guard. I even had a nurse, he went to go take blood from me and didn't have his gloves on. I [said] ‘oh, wait, I'm HIV positive…’” (black participant, AL site) |
| Health care workers will treat me with less respect. | 1.86 (1.10) | “I've put [my HIV status] on different applications … like when I had to do a mammogram….. But my sense of thinking sometimes, ‘What's she thinking?’ You know … ‘How's she going to treat me now?’ Because your attitude is all the sudden I got stink, you know. Yeah, been there.” (black participant, GA site) |
| Experienced stigma | ||
| Health care workers have not listened to my concerns. | 1.40 (0.95) | “…maybe seven or eight years into my diagnosis, I had a doctor tell me that scientists say right now that you need to start taking meds. I said well, scientists say one thing, but I'm saying that I'm not ready because I always was told that, when you start the meds, you've got to be faithful and it's nothing to play with. Me and him had some words. He told me that, since you're not going to take the meds, I'm not going to treat you. I said no problem… and I left out of his clinic.” (black participant, AL site) |
| Health care workers have avoided touching me. | 1.26 (0.73) | “I think I had like a bacterial infection or something else going on down there. So I made an appointment and I went and saw the doctor. I disclosed my status on the paperwork. The [doctor] wouldn't touch me. She was like she kind of looked at me from this distance and was like yeah, you have a yeast infection …. I liked flipped my wig. I was like ‘I know this is not what is wrong with me.” (multiracial participant, CA site) |
| Health care workers have treated me with less respect. | 1.34 (0.87) | Characterization of visits to HIV care provider: “In three words cold and calculated …. the majority of them act like they don't even want to come near you …. It's sad because that's what they're in their profession for…. but some of them they just act like they standoffish …. It just ticks me off as brilliant as they are, they can be that ignorant …. not every time, just certain doctors…. 75% [of doctors].” (white participant, MS site) |
Items measuring anticipated stigma were prefaced by the question, “For the following, please tell me how likely it is that people will treat you in the following ways, in the future, because of your HIV status?”; Items measuring experienced stigma included the question, “How often have people treated you this way in the past 12 months because of your HIV status?”
SD, standard deviation; range for anticipated stigma: 1 (Very Unlikely) −5 (Very Likely); range for enacted stigma: 1 (Never) −5 (Very Often).
ART adherence was assessed by asking participants to self-report how often they took their HIV medication(s) as prescribed over the past 6 months. Response options were “100% of the time,” “95–99% of the time,” “75–94% of the time,” “<75% of the time,” and “I haven't taken any of my prescribed medications.” As in previous peer-reviewed studies involving WIHS participants,32,33 we used the 95% cutoff for optimal versus suboptimal adherence. Depressive symptoms were assessed using the 20-item CES-D (Center for Epidemiological Studies Depression) scale,34 which has been validated among women enrolled in WIHS across all sites.23
Adherence self-efficacy was evaluated using the HIV-ASES (HIV Treatment Adherence Self-Efficacy Scale; α = 0.94),35 which has been validated among various groups of PLWH, including groups specific to the US Deep South.36 Coping by substance use was measured using two items from the Brief COPE inventory that assess the frequency of alcohol or other drug use to deal with the stress of living with HIV within the past 12 months (α = 0.88 for the full inventory; α = 0.93 for the two substance use coping items).37 The Brief Cope has also been validated among PLWH, including women in the US South.38 Participants also self-reported their age, race/ethnicity, education, income, time on ART, and illicit drug use.
We assessed sample demographic and health characteristics using descriptive analyses. Logistic regression analyses controlling for covariates examined total and mediated effects of stigma measures on ART adherence through adherence self-efficacy, depressive symptoms, and coping by substance use. All statistical models were conducted in SPSS using the Hayes' PROCESS macro with bootstrapping for mediation analyses39 and with a cutoff p-value of 0.05 and confidence intervals of 95% for significant results.
At the interpretation stage, we made comparisons between qualitative and quantitative findings. We first prepared separate reports on quantitative and qualitative results and then, for each thematic area, we examined the quantitative and qualitative data concurrently to elucidate the findings that emerged from each method and identified areas where the findings converged or added insight to one another.
Results
Participant characteristics
Approximately one-third of qualitative interview and questionnaire participants were enrolled from the San Francisco WIHS site, another third from the Atlanta site, and the last third from the combined Birmingham/Jackson site (Table 1). Qualitative interviewees were recruited from the same population who responded to the quantitative questionnaires (i.e., HIV-positive WIHS participants at the site).
Table 1.
Sociodemographic and Health Characteristics of Women Living with HIV Participants by Mode of Study Participation
| Characteristic | Qualitative interview (n = 76), n (%) | Quantitative questionnaire (n = 460) | ||||||
|---|---|---|---|---|---|---|---|---|
| n (%) | Anticipated stigma in HCS | Experienced stigma in HCS | ||||||
| Mean | SD | p | Mean | SD | p | |||
| Study site location | 0.95 | 0.10 | ||||||
| Birmingham, AL | 13 (17) | 68 (15) | 1.85 | 0.93 | 1.33 | 0.75 | ||
| Jackson, MS | 13 (17) | 84 (18) | 1.81 | 0.85 | 1.24 | 0.61 | ||
| San Francisco, CA | 25 (33) | 160 (35) | 1.84 | 1.00 | 1.41 | 0.81 | ||
| Atlanta, GA | 25 (33) | 148 (32) | 1.87 | 1.06 | 1.34 | 0.85 | ||
| Race and ethnicitya | 0.06 | 0.18 | ||||||
| Black non-Hispanic | 45 (59) | 347 (77) | 1.87 | 0.97 | 1.33 | 0.74 | ||
| White non-Hispanic | 20 (26) | 63 (14) | 1.59 | 0.86 | 1.33 | 0.81 | ||
| Other non-Hispanic | 6 (8) | 17 (4) | 2.10 | 1.63 | 1.63 | 1.00 | ||
| Hispanic | 5 (7) | 25 (5) | 1.75 | 0.85 | 1.21 | 0.53 | ||
| Highest level of educationa | 0.63 | 0.53 | ||||||
| <High school/GED | 11 (14) | 129 (29) | 1.83 | 0.93 | 1.31 | 0.73 | ||
| High school/GED | 19 (25) | 141 (31) | 1.84 | 0.97 | 1.31 | 0.73 | ||
| Some college/Associate | 34 (45) | 143 (32) | 1.88 | 0.98 | 1.38 | 0.77 | ||
| College and above | 12 (16) | 39 (9) | 1.69 | 0.97 | 1.32 | 0.87 | ||
| Average yearly household incomea | 0.01 | 0.17 | ||||||
| $12,000 or less | 43 (57) | 250 (57) | 1.86 | 1.00 | 1.33 | 0.76 | ||
| $12,001–24,000 | 22 (29) | 100 (23) | 1.95 | 0.93 | 1.40 | 0.87 | ||
| $24,001–36,000 | 5 (7) | 42 (10) | 1.87 | 0.94 | 1.37 | 0.66 | ||
| $36,001 or more | 6 (8) | 47 (11) | 1.50 | 0.85 | 1.14 | 0.46 | ||
| Recent illicit drug usea | 0.23 | 0.59 | ||||||
| Yes | —b | 145 (32) | 1.82 | 0.88 | 1.38 | 0.79 | ||
| No | —b | 304 (68) | 1.84 | 1.00 | 1.31 | 0.74 | ||
| ART statusa | 0.30 | 0.51 | ||||||
| On ART | 70 (92) | 420 (93) | 1.85 | 0.97 | 1.33 | 0.73 | ||
| ART naïve/Not using ART | 6 (8) | 32 (7) | 1.72 | 1.03 | 1.41 | 1.04 | ||
| ART adherence over past 6 monthsa | <0.01 | <0.01 | ||||||
| ≥95% Adherent | —b | 350 (83) | 1.80 | 0.95 | 1.29 | 0.69 | ||
| <95% Adherent | —b | 70 (17) | 2.14 | 1.03 | 1.52 | 0.87 | ||
| Mean (SD) | Mean (SD) | Correlation | p | Correlation | p | |||
| Agea | 48 (8) | 49 (9) | −0.02 | 0.51 | 0.00 | 0.99 | ||
| Time on ART, monthsa | —b | 104 (72) | −0.03 | 0.48 | 0.06 | 0.14 | ||
Data missing for some participants.
This information was not collected.
ART, antiretroviral therapy; GED, general educational development test; HCS, health care setting; SD, standard deviation.
Average age was 48 years for the qualitative sample and 49 years for the quantitative sample. Participants represented diverse racial, ethnic, and socioeconomic backgrounds. The majority of participants self-identified as non-Hispanic black (59% of interviewees and 77% of questionnaire participants). A little over 90% of both samples reported current use of ART. Questionnaire participants reported using ART for 9 years on average, and most women (83%) reported over 95% adherence to their ART regimen within the past 6 months.
Stigma in health care settings
Many of the women reported satisfaction with their health care providers and positive patient–provider interactions in qualitative interviews. Overall, women of color, women from the San Francisco and Jackson sites, and higher educated interviewees most commonly reported experiences and anticipation of stigma in health care settings. However, interviewees across settings reported both experienced and anticipated HIV-related stigma in various health care setting interactions and with different health care personnel in both quantitative and quantitative data (Table 2). Questionnaire data revealed relatively moderate levels of anticipated stigma for the future (mean = 1.84; range = 1–5) and recent experienced stigma (mean = 1.33; range = 1–5) in health care settings among study participants.
Anticipated stigma from health workers was significantly higher than recent experienced stigma from health workers (t = 13.67, SE = 0.04, p < 0.001). Levels of anticipated and experienced stigma from family members (mean = 2.29 for anticipated and 1.71 for experienced; range = 1–5), sexual/romantic partner (mean = 2.34 and 1.57; range = 1–5), and neighbors/others in the community (mean = 2.80 and 1.57; range = 1–5) were also moderate, although slightly higher than anticipated and experienced stigma from health care workers.
Generally, the mean anticipated and experienced stigma in health care setting scores did not vary by most sociodemographic and health characteristics (Table 1). Mean anticipated stigma in health care settings was significantly higher for lower income participants (mean >1.85 for income ranges below 36,000 per year vs. 1.50 for $36,001 or more; p = 0.01), and both mean anticipated and experienced stigma in health care settings were higher for study participants who reported being less adherent to ART (anticipated mean = 2.14 vs. 1.80, p < 0.01; experienced mean = 1.52 vs. 1.29, p < 0.01).
Several manifestations of HIV-related stigma in both HIV care and other health care settings commonly described by participants in the qualitative interviews emerged as themes (Table 3), including expression of (1) assumptions and (2) judgment by health care providers about the participant's current or prior HIV risk behavior, health-related decisions, or engagement in health care; (3) lack of compassion in participant–provider interactions, including as experienced in communication or other interpersonal exchange with medical doctors, nurses, administrative staff, or other clinic personnel; (4) provision of insufficient care, characterized by failure to meet the participant's medical needs or inattention to the participant's medical concerns; (5) unnecessary precautions, which may include excessive control measures such as lack of touch, use of double gloves, avoidance of physical proximity, isolation measures, and so on; (6) violation of privacy via voluntary or involuntary disclosure of participants' status or other lack of health information protection; and (7) lack of autonomy, including exertion of control or influence over the participant's medical decisions or disrespect for the participant's health care desires.
Table 3.
Key Themes and Sample Quotes Around Manifestations of Stigma and Discrimination in Health Care Settings Experienced and Anticipated by Women Living with HIV Participants in Qualitative Interviews
| Theme | Illustrative quote |
|---|---|
| Assumptions | “…almost always with any medical provider first time, they say, ‘So you've used, you know, you've injected drugs.’ ‘No, I never have. So don't assume that.’ And, ‘You've been a prostitute.’ ‘No, I never have.’ And they look at me like I'm lying…. It's like no, I had vanilla sex with a guy who's no doubt screwing around.” (multiracial participant, CA site) |
| Judgement | “…there is the whole list that [providers] have when they do their physical. Then they say, ‘Have you told your partner about your status?’ Yes. ‘Do you use a condom?’ No. ‘Well, why not?’ Then I almost kind of feel a whole lecture coming on. It's not like I haven't sat there and talked to my partner about it. It's not like I haven't informed them about it …. I have felt like [providers] kind of looked at me like you're playing with fire, you know.” (multiracial participant, CA site) |
| Lack of compassion | “I didn't necessarily like being seen here a lot of times because sometimes even by the staff members downstairs, I felt like I was just a number like I didn't freaking matter, … I cannot deal with feeling like I am some derelict or …as if you are like every other person out there with HIV.” (black participant, GA site) |
| Insufficient care | “Quite a while ago I played soccer and my knees are really screwed up. And I went to have a knee replacement and the guy found out I was HIV and he told me it was a waste of my time. [He said] I'm not going to bother …. I should have probably sued him but I was so shocked.” (white participant, CA site) |
| Unnecessary precautions | During a primary care visit: “[A healthcare provider] comes in. How's everything going? I said well, I'm doing okay. I got a little wheezing and stuff. I don't know if you know that I am HIV positive. I have a separate provider for that. As I'm saying that I'm HIV positive, I hadn't even gotten it all out of my mouth, she backed up. She's backing up away from me. I said, “Oh this isn't going to work.” (white participant, GA site) |
| Violation of privacy | “I was waiting. I had heard the nurse outside, the head nurse, saying, ‘I'm not going in that room. I have children at home. I'm not going in there and getting HIV.’ When she sent the other nurse in there, I said, “…she invaded my privacy. She's telling other people what my problem is. You don't have the curtain drawn, so everybody can hear it.” (black participant, AL site) |
| Lack of autonomy | “… [the gynecologist] came in with the paperwork talking about here, you might want to sign these, and we're going to give you a tubal ligation, I was like oh… and she was like you do want your tube ties, right because it would be best. I felt a little more coerced into getting my tubes tied because of my diagnosis and because I wasn't being cooperative with the infectious disease doctor… (black participant, GA site) |
In addition, participants shared fears of encountering the aforementioned manifestations of stigma in health care settings. Many of the women expressed previous or recent concerns about being recognized by other members of their community during HIV care visits. These concerns were especially pervasive among women who were new to HIV care: “I started seeing a doctor.… I had these shades on when I was first diagnosed, I didn't even want people to see my eyes. I was just that ashamed.… I thought people would recognize me. I didn't want anybody to even recognize me.… I mean it is known for being a clinic for STD's… and infectious disease clinic, so you know I was like okay shades on, nobody is going to ever know me” (black participant, GA site).
Related to the violation of privacy theme, interviewees commonly reflected upon worries about being “outed” as HIV positive by either health care workers or other patients that they encounter in health care settings: “I was feeling a little embarrassed to go to the pharmacy to go get my meds.… Because I would be upset that I would even have to discuss that with a line behind me” (multiracial participant, CA site).
A subgroup of participants employed in health care settings avoided disclosing their HIV status to coworkers for fear of being ostracized: “… they don't know because I don't want them to treat me different because they know that I'm HIV positive. I'm still the same person … nothing changed about me. But I don't want it to get to that point to where [they whisper] ‘Oh here she comes’ or you know they're watching what they doing, you know … [their] washing technique” (black participant, MS site).
Perceived effects of stigma in health care settings
Interview participants conveyed that stigma in health care settings is particularly disappointing, compared to other settings, given their expectations for health care providers to act respectfully and to care about the health and well-being of all patients. In a reflection upon health care encounters that are contrary to her expectations, one interviewee stated, “when my doctors treat me different …. It pisses me off to be blunt. Because doctors are professional individuals that were trained to help people like me. But the very person they're supposed to be helping, that's the ones they're hurting. And it just really ticks me off” (white participant, MS site).
Many women relayed feelings of sadness or other negative feelings about these events, as shared by a participant: “The person who drew my blood, he didn't want to touch me or something like that. I don't know what his problem was …. When you're working, you have to be one way with everybody. If you don’ want to, you can just step out of that and do something else …. I think it was because I was HIV positive. You know you don't do that to people …. It hurt me.” (black participant, CA site).
An interviewee shared how a negative experience with a medical provider affected her behavior: “… because of the way she treated me, I didn't want to go to the clinic. I didn't want to take my medicine. I didn't want to have anything to do with medical care because of her… I didn't like her because she was not nice. She was very rude…. I remember one time, I did get very sick. I didn't want to go to the doctor. I didn't want to see her…. I took the wrong decision to not go at all.” (Hispanic/Latina participant, CA site).
The women also expressed that fears of these stigmas can take a toll in a variety of ways, including where and the degree to which they engaged in HIV treatment thereafter. One participant described her reasons for driving to another town for HIV care: “At this point in my life I would not have care in my hometown, because I work at that hospital and everybody knows everybody's business…. My daughter is involved in a lot of community activities, and that's where my part of the stigma comes in. I know children can be really cruel and I don't want her to bear the sins of the mother.… That is my primary concern” (white participant, MS site).
Another health care worker described that she avoids certain therapies and times her medication dosing accordingly for similar reasons: “I don't go to any kind of [support] groups for fear that I would see somebody I knew… I just want to take the secret to my grave with me—because I work with a bunch of nurses. They'd be looking at you trying to diagnose you… No, go away, you know too much. I don't carry the pills in my purse, I just take them once a day, so I take them at night… And, most of the time, I'm alone” (black participant, MS site).
Some women shared past difficulty with initiating HIV care after diagnosis for fear of being seen by others within the community: “When I was first diagnosed, … I came here to meet the doctor, I skipped the first three appointments…. Because of the stigma of having HIV and walking in a building that says Infectious Diseases… I mean literally, I would make it, … and I would turn around and go back home. I'm like I'm not going to let those people see me walking [in] that building” (black participant, AL site).
Participants speculated that this may be a barrier for other WLWH: “I think that a lot of people are afraid to come [to the HIV clinic] because a lot of people know what [clinic name] is, even if they are not positive, they could be afraid to come to the clinic because they are afraid somebody might see them and find out they are positive, and therefore their healthcare—their health could deteriorate because they won't come pick up their meds or won't go to the doctor or something like that” (white participant, AL site).
Quantitative analyses yielded findings consistent with the qualitative results related to the potential effects of stigma in health care settings on adherence. Reported experienced and anticipated stigma in health care settings had differential quantitative effects (Table 4). Reported experienced stigma in health care settings was significantly associated with suboptimal ART adherence, even when controlling for experienced stigma from all other sources [adjusted odds ratio (AOR) = 0.58, p = 0.01].
Table 4.
Independent Associations of Anticipated and Experienced Health Care Setting Stigma with Antiretroviral Therapy Adherence
| Variable | Model 1, N = 383 | Model 2, N = 400 | Model 3, N = 382 | |||
|---|---|---|---|---|---|---|
| AOR | p | AOR | p | AOR | p | |
| Anticipated stigma | ||||||
| In health care settings | — | — | 0.65 | 0.01 | 0.67 | 0.04 |
| From family | — | — | 1.15 | 0.32 | 1.14 | 0.45 |
| From neighbors/others | — | — | 0.86 | 0.30 | 0.84 | 0.26 |
| From sexual/romantic partner | — | — | 1.07 | 0.61 | 1.27 | 0.13 |
| Experienced stigma | ||||||
| In health care settings | 0.59 | 0.01 | — | — | 0.79 | 0.34 |
| From family | 1.26 | 0.18 | — | — | 1.21 | 0.35 |
| From neighbors/others | 0.82 | 0.28 | — | — | 0.85 | 0.39 |
| From sexual/romantic partner | 0.87 | 0.36 | — | — | 0.74 | 0.10 |
| Age, years | 1.01 | 0.66 | 1.01 | 0.65 | 1.00 | 0.83 |
| Education, years | 0.81 | 0.16 | 0.85 | 0.26 | 0.80 | 0.15 |
| Income, household yearly | 1.09 | 0.33 | 1.02 | 0.82 | 1.07 | 0.44 |
| Time on ART, months | 1.00 | 0.94 | 1.00 | 0.91 | 1.00 | 0.68 |
| Illicit drug use, yes vs. no | 0.32 | 0.00 | 0.30 | 0.00 | 0.28 | 0.00 |
| Race, white vs. non-white | 1.38 | 0.51 | 1.57 | 0.35 | 1.28 | 0.63 |
AOR, adjusted odds ratio; ART, antiretroviral therapy.
Similarly, anticipated stigma in health care settings was significantly associated with suboptimal ART adherence, even when controlling for anticipated stigma from all other sources (AOR = 0.64, p = 0.004). When modeled with experienced and anticipated stigma from all other sources, anticipated stigma in health care settings was the only stigma measure significantly associated with suboptimal ART adherence (AOR = 0.67, p = 0.046). Across all three models, illicit drug use was the only covariate significantly associated with suboptimal adherence (Model 1: AOR = 0.32, p < 0.001; Model 2: AOR = 0.30, p < 0.001; Model 3: AOR = 0.28, p < 0.001).
Pathways for these effects
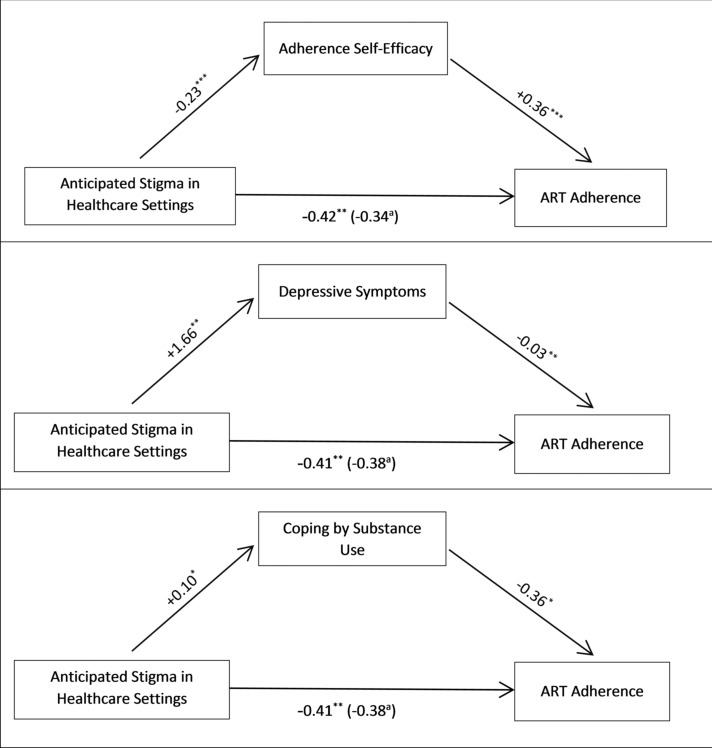
Mediation analyses revealed that the effect of anticipated stigma in health care settings on suboptimal ART adherence was mediated by treatment adherence self-efficacy, depressive symptoms, and coping by substance use (Fig. 1). More specifically, higher anticipated HIV-related stigma predicted lower social support, which in turn predicted suboptimal ART adherence (B = −0.08, SE = 0.04, 95% CI: −0.17 to −0.03). Higher anticipated HIV-related stigma also had an indirect and negative effect on adherence, as mediated by higher depressive symptoms (B = −0.05, SE = 0.03, 95% CI: −0.13 to −0.01). Finally, higher coping by substance use also individually mediated the relationship between anticipated HIV-related stigma and lower ART adherence (B = −0.04, SE = 0.02, 95% CI: −0.10 to −0.001).
FIG. 1.
Mediation models depicting the effect of anticipated stigma in health care settings on ART adherence through adherence self-efficacy, depressive symptoms, and coping by substance use among women living with HIV in the United States. Note: Associations are presented as path coefficients (unstandardized). Age, education, income, time on ART, illicit drug use, and race were also entered as control variable. aWhen adherence self-efficacy is in the model. *p < 0.05; **p < 0.01; ***p < 0.001. ART, antiretroviral therapy.
Resistance and response to stigma in health care settings
In qualitative interviews, many participants described their possible and actual reactions to anticipated stigma in health care settings. For instance, some women changed care teams to avoid future stigmatization. As one woman stated, “I don't want people judging me. One rule that I have for myself is if I ever go to a healthcare provider and I let them know that I'm HIV positive, if I detect anything that's not right, that you're backing up, and maybe I'm not getting or you're not going to give me the same kind of care you're going to give the next patient that's not HIV. You're not the one for me. I'll find someone else.” (white participant, GA site).
In the case of experienced stigma, women directly addressed stigmatizing attitudes by expressing dissent in conversation with the perpetrator of stigma or other health care staff members, or by reporting the experience to a higher authority. In one such instance, in which a participant's privacy was violated by a nurse who refused to assist her with a prescription refill, the participant reported to another provider, “‘Tell her she doesn't have to come in here. I don't need her help anyway. I've been doing this by myself for so many years. All I need is the product.’ …she said, ‘I'm sorry.’
I said it so that everybody could hear, “It's breaking the HIPAA law. I would rather not have her services and I will be reporting her tomorrow. She is a medical personnel and she knows about giving me [prescription name]. She isn't going to get HIV.’ I just rather not her come near me …. You're doing me a favor by not waiting on me.” (black participant, AL site)
Interviewees also reported instances in which medical providers responded compassionately to stigmatizing events, helped to assuage worries, and challenged patient expectations for stigma. In some of these instances, participants spoke of regular HIV care providers who act as their “cheerleader,” “normalize” patient experiences, and “take away the stigma” (white participant, CA site). Other reports were from one-time interactions, particularly with nursing staff, who left positive impressions among women who were anticipating stigma by treating them “like any other patient that came in the room” (black participant, AL site).
Discussion
To date, few studies have examined the unique effects of both experienced and anticipated stigma in health care settings.26 Both the qualitative and quantitative findings from the present study support the contention that WLWH continue to report fears and experiences of HIV-related stigma in HIV- and non-HIV-specific health care settings.40 Although the levels of stigma reported in the questionnaires may seem relatively low, any amount of feared or experienced stigma from health workers is problematic and has the potential to compromise engagement in HIV care and health outcomes.4
Interviewees described fears and experiences with manifestations of stigma in health care settings (assumptions, judgment, lack of compassion, insufficient care, unnecessary precautions, privacy violations, and lack of autonomy), and how these influenced their engagement in HIV care. Quantitative findings regarding the association between anticipated stigma in health care settings and optimal adherence to ART were robust across statistical models and persisted when controlling for stigma from all other sources. Our findings also suggest an indirect effect of anticipated stigma in health care settings on ART adherence through conceptually meaningful mechanisms,3 including coping by substance use, depressive symptoms, and adherence self-efficacy.
Consistent global and domestic evidence corroborates that anticipation and occurrence of stigma in health care settings inhibits engagement along the continuum of HIV prevention and care.41–43 The qualitative themes elucidated in this study help to identify specific health care provider behaviors that are perceived by WLWH as stigmatizing. Clinics may consider periodic measurement of provider attitudes, implicit and explicit biases that may contribute to patient perceptions, to determine the need for provider education, or other interventions.44 Ensuring that health care staff are operating in settings equipped with sufficient information and materials to provide quality care for all patients and ensuring that health care practices establish clear policies and guidelines around patient treatment and protection are keys to stigma reduction in health care settings.9
While promising that intervention development work has been conducted to address the attitudes of health care workers as potential enactors of stigma,45,46 the present study findings highlight the relative importance of addressing anticipated stigma among clients. Potential clinic side strategies that may reduce anticipated stigma include targeted health promotion initiatives to promote a culture of open, affirmative, and nonjudgmental care to all patients at health care settings.
Health care facilities may also consider assessing patient feedback about their satisfaction and experience with the care received, which may inform subsequent health care quality improvement efforts.47 Patient side approaches to reducing anticipated stigma in health care settings include interventions that promote resiliency and social capital,48 build patient capacity for stigma resistance,49 and increase patient agency in patient–provider interactions;50 which may produce additional yield in terms of increased HIV treatment and prevention adherence among WLWH.
The results of the current study's mediation analyses substantiate the position that HIV-related stigma operates on health outcomes through mental health sequelae and reduced availability of psychological resources.3 In other studies, depressive symptoms and treatment self-efficacy were found to mediate the association between internalized HIV stigma and ART adherence among PLWH.23,25,51 Another maladaptive coping response to experienced stigma (avoidant coping) was also found to be indirectly associated with health risk behavior (tobacco use) among PLWH in a separate study.52
Taken together, the results and extant literature imply a need to address the manifestations of these negative health and psychological effects of stigma, in addition to stigma-reduction efforts. In particular, programs to increase social support may produce positive change in treatment self-efficacy,36 and interventions to treat clinical as well as subclinical anxiety and depressive symptoms have the potential to reduce coping by substance use53 and improve ART adherence.54
Limitations of this study include the cross-sectional study design, which precludes conclusions about causality. In addition, self-reported adherence was assessed over the previous 6 months, and at the same time, the present-day assessment of other variables was included in the quantitative analysis. Thus, the timing of assessment may not follow our conceptualization and interpretation of the results. Similarly, quantitative HIV-related stigma items assessed recent experiences and future anticipations, whereas the qualitative data may have reflected experiences over the entire duration of the women's experiences with being HIV positive. However, our analysis was theoretically informed, and our findings are consistent with previous stigma and health research.3
In addition, while all the survey measures used to collect data for this analysis were validated previously among PLWH, not all were validated among women and in the geographic locations represented in the present study, which has implications for validity of the constructs in the current setting and population groups.55 However, the Cronbach's alphas for the scales used within the present sample were more than adequate, indicating strong internal consistency.
Along those lines, the study sample was predominantly comprised women older than the age of 40. Given that young adults (aged 18–39) are less likely to adhere to ART than older adults,56 future studies should focus on younger adult women. Finally, our sample had a limited proportion of non-Hispanic white women (14%), who comprised the reference group for the race variable included in our multivariate analyses. This may be why we did not observe mean differences in anticipated and experienced stigma by race in the bivariate analyses, and why the race variable was not significant in the multivariate analyses.
This study contributes to the literature insights about the unique manifestations of anticipated and experienced stigma in health care settings among WLWH, the association of those stigmas on self-reported adherence, and potential pathways for that association from a mixed methods analysis. Results suggest that future approaches should address stigma among health care workers as well as engage WLWH in resilience-based strategies that combat stigma and promote life-sustaining behaviors. These stigma reduction and health promotion efforts should supplement approaches to improving care continuum outcomes for minority WLWH by addressing other structural and systemic barriers.14,43
Acknowledgments
Data in this article were collected by the Women's Interagency HIV Study (WIHS). We wish to acknowledge the assistance of the WIHS program staff and the contributions of the participants who enrolled in this study. This study was funded by WIHS substudy grants from the National Institute of Mental Health, R01MH095683, and R01MH104114. The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). WIHS (Principal Investigators): UAB-MS WIHS (Mirjam-Colette Kempf and Deborah Konkle-Parker), U01-AI-103401; Atlanta WIHS (Ighovwerha Ofotokun and Gina Wingood), U01-AI-103408; Bronx WIHS (Kathryn Anastos and Anjali Sharma), U01-AI-035004; Brooklyn WIHS (Howard Minkoff and Deborah Gustafson), U01-AI-031834; Chicago WIHS (Mardge Cohen and Audrey French), U01-AI-034993; Metropolitan Washington WIHS (Seble Kassaye), U01-AI-034994; Miami WIHS (Margaret Fischl and Lisa Metsch), U01-AI-103397; UNC WIHS (Adaora Adimora), U01-AI-103390; Connie Wofsy Women's HIV Study, Northern California (Ruth Greenblatt, Bradley Aouizerat, and Phyllis Tien), U01-AI-034989; WIHS Data Management and Analysis Center (Stephen Gange and Elizabeth Golub), U01-AI-042590; Southern California WIHS (Joel Milam), U01-HD-032632 (WIHS I–WIHS IV). The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional cofunding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), and the National Institute on Mental Health (NIMH). Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Craniofacial Research (NIDCR), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the National Institute on Deafness and other Communication Disorders (NIDCD), and the NIH Office of Research on Women's Health. WIHS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR000454 (Atlanta CTSA), P30-AI-050410 (UNC CFAR), and P30-AI-027767 (UAB CFAR).
This research was also supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research CFAR, an NIH-funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Katz IT, Ryu AE, Onuegbu AG, et al. . Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J Int AIDS Soc 2013;16(Suppl 2):18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS Behav 2013;17:1785–1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health 2017;107:863–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nyblade L, Reddy A, Mbote D, et al. . The relationship between health worker stigma and uptake of HIV counseling and testing and utilization of non-HIV health services: The experience of male and female sex workers in Kenya. AIDS Care 2017;29:1364–1372 [DOI] [PubMed] [Google Scholar]
- 5. Rintamaki LS, Scott AM, Kosenko KA, Jensen RE. Male patient perceptions of HIV stigma in health care contexts. AIDS Patient Care STDS 2007;21:956–969 [DOI] [PubMed] [Google Scholar]
- 6. Sayles JN, Ryan GW, Silver JS, Sarkisian CA, Cunningham WE. Experiences of social stigma and implications For healthcare among a diverse population of HIV positive adults. J Urban Health 2007;84:814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zukoski AP, Thorburn S. Experiences of stigma and discrimination among adults living with HIV in a low HIV-prevalence context: A qualitative analysis. AIDS Patient Care STDS 2009;23:267–276 [DOI] [PubMed] [Google Scholar]
- 8. Boehme AK, Moneyham L, McLeod J, et al. . HIV-infected women's relationships with their health care providers in the rural deep south: An exploratory study. Health Care Women Int 2012;33:403–419 [DOI] [PubMed] [Google Scholar]
- 9. Nyblade L, Stangl A, Weiss E, Ashburn K. Combating HIV stigma in health care settings: What works? J Int AIDS Soc 2009;12:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lazo M, Gange SJ, Wilson TE, et al. . Patterns and predictors of changes in adherence to highly active antiretroviral therapy: Longitudinal study of men and women. Clin Infect Dis 2007;45:1377–1385 [DOI] [PubMed] [Google Scholar]
- 11. Bowleg L. The problem with the phrase women and minorities: Intersectionality—An important theoretical framework for public health. Am J Public Health 2012;102:1267–1273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Sex Orient Gend Divers 2013;1:3–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wingood GM, Diclemente RJ, Mikhail I, et al. . HIV discrimination and the health of women living with HIV. Women Health 2007;46:99–112 [DOI] [PubMed] [Google Scholar]
- 14. Almirol EA, McNulty MC, Schmitt J, et al. . Gender differences in HIV testing, diagnosis, and linkage to care in healthcare settings: Identifying African American women with HIV in Chicago. AIDS Patient Care STDS 2018;32:399–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beer L, Mattson CL, Bradley H, Skarbinski J. Understanding cross-sectional racial, ethnic, and gender disparities in antiretroviral use and viral suppression among HIV patients in the United States. Medicine 2016;95:e3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stein R. HIV testing and service delivery among black females—61 health department jurisdictions, United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2016;65:83–85 [DOI] [PubMed] [Google Scholar]
- 17. Geter A, Sutton MY, Armon C, et al. . Trends of racial and ethnic disparities in virologic suppression among women in the HIV Outpatient Study, USA, 2010–2015. PLoS One 2018;13:e0189973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. HIV in the United States by Geography. Atlanta, GA: U.S. Department of Health and Human Services; 2017 [Google Scholar]
- 19. Reif S, Pence BW, Hall I, Hu X, Whetten K, Wilson E. HIV diagnoses, prevalence and outcomes in nine southern states. J Community Health 2015;40:642–651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adimora AA, Ramirez C, Schoenbach VJ, Cohen MS. Policies and politics that promote HIV infection in the Southern United States. AIDS 2014;28:1393–1397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rice WS, Logie CH, Napoles TM, et al. . Perceptions of intersectional stigma among diverse women living with HIV in the United States. Soc Sci Med 2018;208:9–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Logie CH, Lacombe-Duncan A, Wang Y, et al. . Pathways from HIV-related stigma to antiretroviral therapy measures in the HIV care cascade for women living with HIV in Canada. J Acquir Immune Defic Syndr 2018;77:144–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Turan B, Smith W, Cohen MH, et al. . Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: The mediating roles of social isolation and depression. J Acquir Immune Defic Syndr 2016;72:198–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rice WS, Crockett KB, Mugavero MJ, Raper JL, Atkins GC, Turan B. Association between internalized HIV-related stigma and HIV care visit adherence. J Acquir Immune Defic Syndr 2017;76:482–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Turan B, Rogers AJ, Rice WS, et al. . Association between perceived discrimination in healthcare settings and HIV medication adherence: Mediating psychosocial mechanisms. AIDS Behav 2017;21:3431–3439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kay ES, Rice WS, Crockett KB, Atkins GC, Batey DS, Turan B. Experienced HIV-related stigma in healthcare and community settings: Mediated associations with psychosocial and health outcomes. J Acquir Immune Defic Syndr 2018;77:257–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Batey DS, Whitfield S, Mulla M, et al. . Adaptation and implementation of an intervention to reduce HIV-related stigma among healthcare workers in the United States: Piloting of the FRESH workshop. AIDS Patient Care STDS 2016;30:519–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Adimora AA, Ramirez C, Benning L, et al. . Cohort profile: The Women's Interagency HIV Study (WIHS). Int J Epidemiol 2018;47:393–394i [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: SAGE Publications; 2017 [Google Scholar]
- 30. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101 [Google Scholar]
- 31. Dedoose Version 7.0.23 [Computer Program]. Los Angeles, CA; 2016 [Google Scholar]
- 32. Kelso GA, Cohen MH, Weber KM, Dale SK, Cruise RC, Brody LR. Critical consciousness, racial and gender discrimination, and HIV disease markers in African American women with HIV. AIDS Behav 2014;18:1237–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dale S, Cohen M, Weber K, Cruise R, Kelso G, Brody L. Abuse and resilience in relation to HAART medication adherence and HIV viral load among women with HIV in the United States. AIDS Patient Care STDS 2014;28:136–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401 [Google Scholar]
- 35. Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: Validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES). J Behav Med 2007;30:359–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Turan B, Fazeli PL, Raper JL, Mugavero MJ, Johnson MO. Social support and moment-to-moment changes in treatment self-efficacy in men living with HIV: Psychosocial moderators and clinical outcomes. Health Psychol 2016;35:1126–1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Carver CS. You want to measure coping but your protocol's too long: Consider the brief COPE. Int J Behav Med 1997;4:92–100 [DOI] [PubMed] [Google Scholar]
- 38. Pence BW, Thielman NM, Whetten K, Ostermann J, Kumar V, Mugavero MJ. Coping strategies and patterns of alcohol and drug use among HIV-infected patients in the United States Southeast. AIDS Patient Care STDS 2008;22:869–877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press; 2013 [Google Scholar]
- 40. Boehme AK, Davies SL, Moneyham L, Shrestha S, Schumacher J, Kempf MC. A qualitative study on factors impacting HIV care adherence among postpartum HIV-infected women in the rural southeastern USA. AIDS Care 2014;26:574–581 [DOI] [PubMed] [Google Scholar]
- 41. Geter A, Sutton MY, Hubbard McCree D. Social and structural determinants of HIV treatment and care among black women living with HIV infection: A systematic review: 2005–2016. AIDS Care 2018;30:409–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: A review of the evidence. AIDS Behav 2013;17:2528–2539 [DOI] [PubMed] [Google Scholar]
- 43. Taylor BS, Fornos L, Tarbutton J, et al. . Improving HIV care engagement in the south from the patient and provider perspective: The role of stigma, social support, and shared decision-making. AIDS Patient Care STDS 2018;32:368–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Alexandra Marshall S, Brewington KM, Kathryn Allison M, Haynes TF, Zaller ND. Measuring HIV-related stigma among healthcare providers: A systematic review. AIDS Care 2017;29:1337–1345 [DOI] [PubMed] [Google Scholar]
- 45. Varas-Díaz N, Neilands TB, Cintrón-Bou F, et al. . Testing the efficacy of an HIV stigma reduction intervention with medical students in Puerto Rico: The SPACES project. J Int AIDS Soc 2013;16:18973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? J Int AIDS Soc 2013;16(Suppl 2):18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Geter A, Herron AR, Sutton MY. HIV-related stigma by healthcare providers in the United States: A systematic review. AIDS Patient Care STDS 2018;32:418–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Perez-Brumer AG, Reisner SL, McLean SA, et al. . Leveraging social capital: Multilevel stigma, associated HIV vulnerabilities, and social resilience strategies among transgender women in Lima, Peru. J Int AIDS Soc 2017;20:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Spangler SA, Abuogi LL, Akama E, et al. . From ‘half-dead’ to being ‘free’: Resistance to HIV stigma, self-disclosure and support for PMTCT/HIV care among couples living with HIV in Kenya. Cult Health Sex 2018;20:489–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chang J, Dubbin L, Shim J. Negotiating substance use stigma: The role of cultural health capital in provider-patient interactions. Sociol Health Illn 2016;38:90–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Seghatol-Eslami VC, Dark HE, Raper JL, Mugavero MJ, Turan JM, Turan B. Brief report: Interpersonal and intrapersonal factors as parallel independent mediators in the association between internalized HIV stigma and ART adherence. J Acquir Immune Defic Syndr 2017;74:e18–e22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Crockett KB, Rice WS, Turan B. Associations between multiple forms of discrimination and tobacco use among people living with HIV: The mediating role of avoidance coping. J Acquir Immune Defic Syndr 2018;78:9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Silverberg MJ, Leyden WA, Leibowitz A, et al. . Factors associated with hazardous alcohol use and motivation to reduce drinking among HIV primary care patients: Baseline findings from the Health & Motivation study. Addict Behav 2018;84:110–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. J Acquir Immune Defic Syndr 2011;58:181–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gjersing L, Caplehorn JR, Clausen T. Cross-cultural adaptation of research instruments: Language, setting, time and statistical considerations. BMC Med Res Methodol 2010;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Beer L, Skarbinski J. Adherence to antiretroviral therapy among HIV-infected adults in the United States. AIDS Educ Prev 2014;26:521–537 [DOI] [PMC free article] [PubMed] [Google Scholar]