Abstract
Background
Use of cardiovascular medication has increased over time, especially for primary and secondary prevention, with polypharmacy common.
Methods
Review of published systematic reviews of the factors and outcomes associated with adherence to cardiovascular medication using MEDLINE, Embase, CINAHL and PsycINFO databases. Quality was assessed using the AMSTAR tool.
Results
Of 789 systematic reviews identified, 45 met the inclusion criteria and passed the quality assessment; 34 focused on factors associated with adherence, and 11 on outcomes. High heterogeneity, both between and within reviews, precluded meta-analysis and so a pooled estimate of adherence levels could not be derived. Adherence was associated with disease factors, therapy factors, healthcare factors, patient factors and social factors, though with some inconsistencies. In total, 91% of reviews addressing outcomes reported that low adherence was associated with poorer clinical and economic endpoints.
Conclusions
Factors from across five key domains relate to non-adherence to cardiovascular medications, and may contribute to poorer clinical outcomes. Interventions to improve adherence should be developed to address modifiable factors and targeted at those at highest risk of non-adherence. Adherence research is highly heterogeneous to-date and efforts to standardize this should be implemented to improve comparability.
Keywords: behaviour, circulatory disease, systematic review
Introduction
Cardiovascular disease (CVD) is the leading cause of death globally.1 Due to an ageing population and proliferation of clinical trials, use of cardiovascular medication and polypharmacy have increased over time, which may contribute to non-adherence to drugs. The US National Health and Nutrition Survey (NHANES) found that 77% of adults diagnosed with hypertension had been prescribed an antihypertensive drug in 2010, compared to 63% in 2001.2 Additionally, the incidence of polypharmacy has risen, with the percentage of patients taking multiple antihypertensives in the US NHANES cohort growing by 11%.2 Within the UK, the percentage of adults aged 65–84 years who are prescribed three or more medications for chronic conditions has increased by 50.5%,3 while for those aged over 85 it has increased by 21.6%.3 This, in turn, has led to increased costs to health services: NHS England dispensed over 1000 million prescriptions in 2015, at an increase of 16.8% in costs from 2005, totalling £9267 million for net ingredient expenditure.4
Trial evidence of efficacy will only translate into real-world effectiveness if levels of adherence achieved in research studies can be replicated in the general population. In addition to disease management, cardiovascular medications are used in both primary and secondary prevention. Adherence may be particularly problematic when medication is used as a long-term, preventive strategy rather than for symptom relief.4 Patients’ perception of the risk associated with their disease may also play a role; for example, adherence to HIV medication has been shown to be 5% higher than adherence to CVD medication.5,6 The aim of this study was to review the existing published evidence of the factors and outcomes associated with adherence to CVD medications.
Methods
Searches were conducted using MEDLINE (1996–present), Embase (1996–present), CINAHL and PsycINFO (full search strategy, Appendix 1). Inclusion was restricted to systematic reviews written in English, and duplicate publications removed using EndNote X7. Titles, then abstracts, then full text were reviewed manually and included if they studied factors associated with adherence to CVD medication for management of symptoms, primary, or secondary prevention, or the association between adherence and health outcomes. Reviews that included other conditions, as well as CVD, were included but those focused exclusively on non-CVD medication were excluded. Publications were excluded if they focused on interventions to improve adherence, adherence to non-medical interventions such as behavioural change, or guidelines on management of adherence. Data extraction included information on study aims, setting, methods, search strategies and findings (overall adherence levels and differences between sub-groups where reported). Review of papers and data extraction was performed by K.L., with a 10% sample independently reviewed by C.M., Findings were compared and disagreements discussed to reach consensus.
The quality of eligible studies was assessed using the AMSTAR tool,7 with papers scored out of 11 and categorized into high quality (score of 9–11), reasonable quality (score 6–8) or poor quality (score 3–5). Papers that scored ≤2 were rejected.
Results
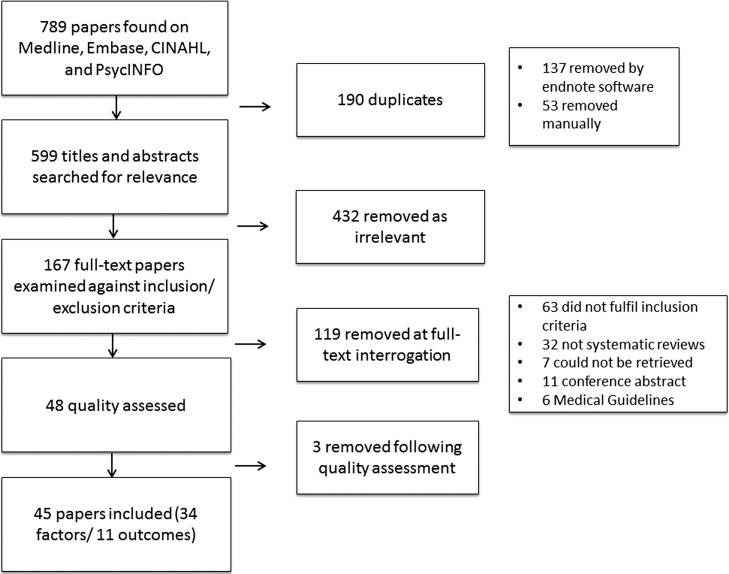
The literature search initially identified 789 papers. After review (741 papers removed) and quality assessment (3 removed) there were 45 eligible systematic reviews, 34 of which dealt with factors associated with non-adherence and 11 on outcomes (Fig. 1).
Fig. 1.
Summary flowchart of paper selection.
Most reviews scored as high quality (n = 16, 36%), or reasonable quality (n = 20, 44%) using the AMSTAR tool, but many noted that the primary studies included were of a variable standard. Results from data extraction of eligible reviews are summarized in Supplementary Tables. Most primary studies were conducted in the USA, Europe, and other developed countries, with only two systematic reviews centred on low or middle income countries (LMICS).8,9 Half of the systematic reviews reported an overall estimate of adherence, though this often had a wide range within each review, the most extreme example ranging from 20 to 88%.10 Most systematic reviews included studies employing a range of methods to study adherence, with self-reporting most common, followed by pharmacy claims, prescription refills and pill counts. Electronic monitoring methods were reported in fewer reviews (n = 11), possibly due to increased costs associated with. Measures of adherence also varied, with many studies comparing ‘good’ versus ‘bad’ adherence across a specified threshold (≥0%). The two most common adherence measures are the Medical Possession Ratio (MPR), the ‘number of days covered with medication in the refill gap, divided by the number of days in the refill gap’,11 and Proportion of Days Covered (PDC), or the ‘number of days with medication supplied divided by the length of follow-up’.11 Others considered the relative change in adherence rates between groups, or the hazard ratio for non-adherence against a reference category, though most reviews failed to specify which of these metrics was used in the primary studies.
Overall, 34 systematic reviews studied factors associated with adherence,5,6,8–39 broadly categorized into: disease factors, therapy factors, healthcare factors, patient factors and social factors6,40 (Table 1). Due to heterogeneity in study design, quality, and operational definitions of adherence, it was not possible to perform meta-analysis to derive a pooled risk estimate associated with any individual factor. Instead, detailed summaries of key factors are provided in Table 2.
Table 1.
Factors found to impact adherence
| Disease factors | Therapy factors | Healthcare factors | Patient factors | Social factors |
|---|---|---|---|---|
| Disease treated5 | Side-effects8,12,13 | Relationship/communication with physician6,14,15 | Gender9,16,17 | Socioeconomic status6,10,17,19–21 |
| Primary versus secondary disease prevention11,17,20,22 | Dosing regimen/frequency5,8,22–24 | Self-monitoring25 | Age5,17 | Level of education/health literacy9,26 |
| Comorbidity10 | Drug class10,12,13,27,28 | Cost/co-payments6,8,20,22,29–31 | Making time for appointments6,29 | Ethnicity16 |
| Depression10,14,32 | Combination pill33–37 | Routine place of care6,30 | Stress/anxiety14 | Minority status10 |
| Diabetes10,17 | Routine physician6,15,30 | Forgetfulness6,14 | Social support18 | |
| Duration of treatment20 | Practitioner disagreement with guidelines14 | Lack of understanding8,14,15,29 | ||
| Coronary artery calcium (CAC) screening39 | Alcohol consumption39 | |||
| Patient beliefs/perception of drugs6,8,14,15,21 |
Table 2.
Consistency of findings across reviews for key adherence factors
| Factors | Reviews | Findings* | Consistency |
|---|---|---|---|
| Disease | |||
| Primary versus secondary | Mann et al. 2010; Lemstra et al. 2012; Xu et al. 2016; Chen et al. 2015 |
|
Similar findings across 100% of reviews.
|
| Comorbidity- diabetes | Mann et al. 2010; Lemstra and Alsabbagh 2014 | Diabetes + | Similar findings across both reviews, though variation at study level.
|
| Comorbidity- depression | Khatib et al. 2014; Lemstra and Alsabbagh 2014; Eze-Nliam et al. 2010 | Depression − |
|
| Therapy | |||
| Drug Class | Matchar et al. 2008; Powers et al. 2012; Lemstra and Alsabbagh 2014; Kronish et al. 2011; Bramlage et al. 2009 |
|
|
| Dosing frequency/Treatment Regimen | Assawasuwannakit et al. 2015; Bowry et al. 2011; Iskedjian et al. 2002; Ingersoll et al. 2008 |
|
Largely consistent, as number of dosages per day increases adherence decreases.
|
| Healthcare | |||
| Cost | Bowry et al. 2011; AlGhurair et al. 2012; Lemstra et al. 2012; Xu et al. 2016; Marshall et al. 2012; Maimaris et al. 2013, Mann et al. 2014 | Higher costs − |
|
| Patient | |||
| Gender | Lewey et al. 2013; Mann et al. 2010; Nielsen et al. 2017 | Female gender +/- | Inconsistent. Varied with setting.
|
| Age | Assawasuwannakit et al. 2015; Mann et al. 2010 | Increasing age +/− |
|
| Perceptions | Bowry et al. 2011; Khatib et al. 2014; Rashtid et al. 2014; AlGhurair et al. 2012; McKenzie et al. 2015. |
|
|
| Social | |||
| SES | AlGhurair et al. 2012; Mann et al. 2010; Alsabbagh et al. 2014; Lemstra et al. 2012; McKenzie et al. 2015; Lemstra and Alsabbagh 2014. |
|
|
*Improved adherence (+), decreased adherence (−) or inconsistent (+/−) relationship with adherence.
Disease factors
Whilst adherence to medication for secondary prevention following acute coronary syndrome was suboptimal,11 it was nonetheless greater than adherence for primary prevention.17,20,22 The effect of comorbidity on adherence varied according to the condition. Patients with diabetes had higher adherence to CVD medications,10,17 while depression almost universally had a negative impact on adherence.10,14,32 The duration of treatment was also important, with adherence tending to decline over time.20
Therapy factors
In spite of heterogeneity in specific study characteristics,27 drug class was consistently associated with differences in adherence.10,12,13,27,28 Adherence was best with angiotensin-II receptor blockers (ARB’s),10,12,13,27,28 and in pooled results, those prescribed ARB’s were 30–33% more likely to be adherent overall compared to those prescribed other drug classes.10,27 Diuretics were associated with the lowest adherence rates10,27 and lower persistence rates of any drug class, ranging from 16 to 38% across studies,28 compared to beta-blockers, BB’s (26–50%), calcium-channel blockers, CCB’s (26–52%), angiotensin converting enzyme inhibitors, ACEi’s (28–64%), and ARB’s (26–68%).28 Differences in side-effects may partly explain these variations. Patients on ACEi’s are 68% more likely to develop a cough than those on ARB’s.12 At standard dose, side-effects are more prevalent among patients taking thiazides (occurred in 9.9%), BB’s (7.5%) and CCB’s (8.3%), compared with ACEi’s (3.8%),28 while ARB’s (0%) are not associated with any side-effects.28
Dosage and treatment regimen were also associated with adherence. Combination drugs were associated with greater adherence compared to equivalent drugs given separately, ranging from 12% in one meta-analysis,33 to 29% in another.34 Overall, adherence declined as the number of doses per day increased,5,22–24 however, this effect was reduced with increased age.5 In LMIC’s, approximately half of studies looking at dosing complexity found a significant relationship between >1 daily dosing and non-adherence.8 Of five reviews that examined treatment regimens, two did not take account of concomitant drug use as a factor,8,22 and a further two acknowledged this but stated they were unable to analyse it given the data available.5,23 Only Ingersoll et al.24 discussed polypharmacy; 66% of studies of CVD medication found a positive influence of polypharmacy on adherence, despite increasing complexity being found to have a reductive effect on adherence elsewhere. The third study produced inconsistent findings.
Healthcare factors
Medication or appointments costs to the patient was commonly identified as influencing non-adherence,6,8,20,22,29–31 largely in US settings. One review reported cost or co-payment as the most commonly studied factor related to adherence (29% of studies).22 Patients who had to make co-payments for treatment were at a 28% greater risk of non-adherence, as they were less likely to collect their statins at the appropriate time,20 and similar associations were found across cohort studies of adherence to antihypertensives.30 The impact of co-payment on adherence varied depending on the actual cost to the patient.31
Continuity of care was found to positively influence adherence.6,15,30 In one review,30 nine of eleven studies reported that it had a positive influence on patient awareness of their condition, treatment, or control of hypertension.30
Patient factors
Gender was studied in three reviews.9,16,17 The majority of studies identified an association between gender and nonadherence, with a 7–10% increased risk of non-adherence among women. However, no association with gender was reported in any of the eleven studies conducted in Canada16 and, in studies conducted in low- and middle-income countries, adherence was better among women.9 Age was also associated with adherence: pooled results by Assawasuwannakit et al.5 demonstrated a 9% improvement in adherence over a 13-year increase in age, from 40 to 53 years, among patients with hypertension, however, no data was included for patients over the age of 67 (age range: 6.9–66.7 years).5 Mann et al.17 found a ‘u-shaped’ relationship between nonadherence and age, with middle aged patients having better adherence than adults aged between 18 and 50 years, or above 70 years old.
Other patient factors associated with poorer adherence include stress, anxiety and difficulty making time for appointments.6,14,29 Alcohol consumption has a negative affect on adherence14,39 across various chronic diseases, though findings are inconsistent39 with insufficient research specific to hypertension.39
In studies using patient self-reporting to measure adherence, forgetfulness and lack of knowledge were frequently cited risk factors6,14 and patient’s perception of medication and understanding of their disease were also important. In one review investigating qualitative patient self-reported studies (n = 15), three studies (20%) cited that patients discontinue treatment due to an initial lack of symptoms or following a reduction of symptoms,14 as they do not understand the chronicity of their disease. Perceptions about the medication itself can also have an impact; in the same review, two self-reported studies (13%) cited patient fears of reliance on cardiovascular drugs14 as a barrier to adherence.
Social factors
The literature on socioeconomic status (SES) is inconsistent. In six systematic reviews reporting SES, two found no significant link6,21 although they did comment that other factors may have impacted this.21 In four reviews, high income status was associated with better adherence ranging from 11 to 26% across reviews10,17,19,20 though there was considerable variation at individual study level. In the review by Alsabbagh et al.,19 77.5% of studies found a positive association between high SES and adherence, though all but one of the remaining studies found high SES had a negative impact on adherence.
Loke et al.26 investigated the relationship between health literacy and adherence to CVD or diabetes medications, but only one of seven cardiovascular studies found a significant association.
Outcomes of non-adherence
Eleven papers41–51 reviewed studies of outcomes associated with non-adherence (Table 3), although the quality of these was lower than the reviews of risk factors; 64 and 85%, respectively, scoring reasonable or high quality. All but one study found a significant association between good adherence and improved clinical or economic outcomes; the exception of the Jongstra et al.51 review found no significant association between persistence of antihypertensive medication and cognitive function. Heterogeneity precluded meta-analysis.
Table 3.
Outcomes associated with adherence
Bramlage and Hasford28 compared cost-effectiveness across drug classes, and found newer drugs, ARB’s and ACEi’s, outperformed the others in spite of being more expensive per tablet. This may be due to greater adherence to these drug classes10,12,13,27,28 which reduces later costs of CVD treatment and adverse events. Bitton et al.43 found that, in secondary prevention of CAD, patients who took ≤80% of their prescribed medication cost up to US$868 more per patient due to increased hospitalizations compared with the adherent group. Furthermore, Shroufi and Powles49 found improving adherence may reduce healthcare costs more than earlier prescribing of statins would do, highlighting this as an important aspect of disease management.
Discussion
Main finding of this study
Previous reviews have identified five main categories of factors associated with adherence; disease, therapy, healthcare, patient and social factors.6,40 As drugs taken for prevention of CVD are often intended for life-long use, adherence is especially important; recognizing and addressing factors that can improve adherence is vital in achieving maximum clinical and cost effectiveness. Side-effects and differences in adherence across drug classes could have important implications in prescribing of CVD drugs, while identifying different population sub-groups, such as those with co-morbid conditions, different genders, SESs or age groups, could be important in informing dosage regimes or targeting interventions to improve adherence.
There is lack of consensus around the association between adherence and outcomes, though nonetheless there is some evidence suggesting that better adherence leads to improved clinical and economic consequences, and there are gaps in the literature yet to be addressed.47,48 There was much heterogeneity across all studies with regards to how adherence rates were assessed.
From these findings, it is apparent that poor adherence to CVD medications has important consequences, and is a vital area of study in order to reduce CVD morbidity and mortality and maximize the cost-effectiveness of treatment.
What is already known on this topic
It is well understood that adherence to drugs in chronic conditions is sub-optimal and there is a dearth of research into what the causative factors for this could be. However many studies are restricted in that they investigate single factors in isolation, or are of a relatively small scale and so have limited power. In terms of systematic reviews, there has been much research but little opportunity for meta-analysis owing to the huge heterogeneity existing within the literature.
What this study adds
Many previous systematic reviews tend to focus on a particular factor, rather than looking across studies to include factors from each of the five groups; disease, therapy, healthcare, patient and social factors.40 This review collates all of this information into one place, to give an overview of factors identified throughout the literature. Few systematic reviews dealt with outcomes of nonadherence, which gives scope to develop research in this area.
Some factors were found to have similar associations with adherence across the literature, a good example being the class of drug prescribed. Newer CVD drugs, ARB’s and ACEi’s, were consistently found to have higher adherence rates than BB’s CCB’s, and diuretics.10,12,13,27,28
On the other hand, some factors had inconsistent relationships with adherence across primary studies and systematic reviews: for instance, female gender was associated with an overall higher risk of nonadherence in two reviews,16,17 though not elsewhere.9 It would be worthwhile identifying cultural, societal or policy differences that may influence this. Gender is a complex factor as it can be predictive of many other confounding factors, for example, woman more commonly assume a care-giving role than men,16 and this has been associated with poorer adherence.16 Hence, better support for caregivers and social care infrastructures could potentially help contribute to better adherence in this subgroup.
Many factors are likely to impact each other. Age will be influenced by different perceptions about health, increased comorbidities, and lifestyle changes. Generally, age was associated with an increase in adherence, though in the very old there is decline.17 This could be related to disease factors, for example, comorbidities common to old age, such as a declining cognitive function and therefore an increased likelihood to forget.5
Many perception barriers, such as belief that a reduction of symptoms indicates that drugs are no longer required,14 or concerns of dependence to CVD medications,14 illustrate a lack of understanding in some patients, and improved communication is required.
Limitations of this study
Few systematic reviews were undertaken before the 1990s52 so it is unlikely that many papers would be missed by limiting searches to the 1996 version of the databases.
This review is limited in that it was restricted to papers written in the English language, contributing to potential publication bias. The huge levels of heterogeneity within systematic reviews included, and between them, made meta-analysis impossible and is a symptom of an area of research that has been largely unstandardized in its implementation. As this is an overview of systematic reviews, it would be impossible to perform meta-analysis without unpicking the individual studies to ensure none are over-represented. Another issue is that the study design and method for calculating adherence have both been found to alter the rates of adherence identified, though there is no gold standard within the literature for analysing this. Many systematic reviews failed to summarize operational definitions of adherence used by primary studies, i.e. whether studies looked at adherence as a continuous variable, or used a cut-off value above which individuals were considered adherent.
Performing a systematic review of reviews is a good way to collate and quality assess numerous studies published in this field; however, it is possible that important primary papers have been missed by focusing only on reviews.
Conclusions
There is a range of modifiable and non-modifiable risk factors that have been associated with non-adherence to cardiovascular drugs, and these must be considered when developing interventions to improve disease management. Studies to-date are of variable quality and considerable heterogeneity. While some systematic reviews consider multiple factors, many primary studies look at risk factors in isolation, not accounting for the interplay between them, and because of heterogeneity there was no opportunity to study this quantitatively. This gives scope to conduct a primary study looking at multiple adherence factors from across these groups. Vitally important to this field of research is an agreed terminology and methodology, to allow comparisons across different study populations to be made. Vrijens et al.53 have defined a taxonomy recommended for use, and if used consistently by researchers it will greatly enhance the value of adherence research.
Supplementary Material
Conflict of interest
None.
Authors’ contributions
KL conducted literature searches, extracted information, constructed summary tables and created first draft. JP helped design the study, commented on search strategies and drafts, and contributed to editing. CM helped design study,commented on drafts, and reviewed sample of papers. All authors approved the final version of the article.
Funding
Work supported by Medical Research Council (MRC) [MR/N013166/1 to K.H.L.].
References
- 1. WHO Cardiovascular Diseases (CVDs) Factsheet. Media Centre: WHO, 2016. [Google Scholar]
- 2. Gu Q, Burt VL, Dillon CF et al. Trends in antihypertensive medication use and blood pressure control among united states adults with hypertension. Circulation 2012;126(17):2105. [DOI] [PubMed] [Google Scholar]
- 3. Melzer D, Tavakoly B, Winder RE et al. Much more medicine for the oldest old: trends in UK electronic clinical records. Age Ageing 2015;44(1):46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. HSCIC , Prescriptions Dispensed in the Community: England 2005–2015 National Statistics publication. Prescribing and Medicines Team Health and Social Care Information Centre, 2016.
- 5. Assawasuwannakit P, Braund R, Duffull SB. A model-based meta-analysis of the influence of factors that impact adherence to medications. J Clin Pharm Ther 2015;40(1):24–31. [DOI] [PubMed] [Google Scholar]
- 6. AlGhurair SA, Hughes CA, Simpson SH et al. A systematic review of patient self-reported barriers of adherence to antihypertensive medications using the World Health Organization Multidimensional Adherence Model. J Clin Hypertens 2012;14(12):877–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shea BJ, Grimshaw JM, Wells GA et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007;7(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bowry ADK, Shrank WH, Lee JL et al. A systematic review of adherence to cardiovascular medications in resource-limited settings. J Gen Intern Med 2011;26(12):1479–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nielsen J, Shrestha AD, Neupane D et al. Non-adherence to anti-hypertensive medication in low- and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens 2017;31(1):14–21. [DOI] [PubMed] [Google Scholar]
- 10. Lemstra M, Alsabbagh MW. Proportion and risk indicators of nonadherence to antihypertensive therapy: a meta-analysis. Patient Prefer Adherence 2014;8:211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen H-Y, Saczynski JS, Lapane KL et al. Adherence to evidence-based secondary prevention pharmacotherapy in patients after an acute coronary syndrome: a systematic review. Heart Lung 2015;44(4):299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Matchar DB, McCrory DC, Orlando LA et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin ii receptor blockers for treating essential hypertension. Ann Intern Med 2008;148(1):16–29. [DOI] [PubMed] [Google Scholar]
- 13. Powers BJ, Coeytaux RR, Dolor RJ et al. Updated report on comparative effectiveness of ACE inhibitors, ARBs, and direct renin inhibitors for patients with essential hypertension: much more data, little new information. J Gen Intern Med 2012;27(6):716–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khatib R, Schwalm JD, Yusuf S et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One 2014;9(1):e84238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rashid MA, Edwards D, Walter FM et al. Medication taking in coronary artery disease: a systematic review and qualitative synthesis. Ann Fam Med 2014;12(3):224–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lewey J, Shrank WH, Bowry ADK et al. Gender and racial disparities in adherence to statin therapy: a meta-analysis. Am Heart J 2013;165(5):665–78.e1. [DOI] [PubMed] [Google Scholar]
- 17. Mann DM, Woodard M, Muntner P et al. Predictors of non-adherence to statins: a systematic review and meta-analysis. Ann Pharmacother 2010;44(9):1410–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Magrin ME, D’Addario M, Greco A et al. Social support and adherence to treatment in hypertensive patients: a meta-analysis. Ann Behav Med 2015;49(3):307–18. [DOI] [PubMed] [Google Scholar]
- 19. Alsabbagh MHDW, Lemstra M, Eurich D et al. Socioeconomic status and nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Value Health 2014;17(2):288–96. [DOI] [PubMed] [Google Scholar]
- 20. Lemstra M, Blackburn D, Crawley A et al. Proportion and risk indicators of nonadherence to statin therapy: a meta-analysis. Can J Cardiol 2012;28(5):574–80. [DOI] [PubMed] [Google Scholar]
- 21. McKenzie SJ, McLaughlin D, Clark J et al. The burden of non-adherence to cardiovascular medications among the aging population in Australia: a meta-analysis. Drugs Aging 2015;32(3):217–25. [DOI] [PubMed] [Google Scholar]
- 22. Xu Y, Worden CJ Adherence, compliance, and persistence with lipid-lowering therapies: a systematic review. ISPOR 21st Annual International Meeting, 2016.
- 23. Iskedjian M, Einarson TR, MacKeigan LD et al. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin Ther 2002;24(2):302–16. [DOI] [PubMed] [Google Scholar]
- 24. Ingersoll KS, Cohen J. The impact of medication regimen factors on adherence to chronic treatment: a review of literature. J Behav Med 2008;31(3):213–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fletcher BR, Hartmann-Boyce J, Hinton L et al. The effect of self-monitoring of blood pressure on medication adherence and lifestyle factors: a systematic review and meta-analysis. Am J Hypertens 2015;28(10):1209–21. [DOI] [PubMed] [Google Scholar]
- 26. Loke YK, Hinz I, Wang X et al. Systematic review of consistency between adherence to cardiovascular or diabetes medication and health literacy in older adults. Ann Pharmacother 2012;46(6):863–72. [DOI] [PubMed] [Google Scholar]
- 27. Kronish IM, Woodward M, Sergie Z et al. Meta-analysis: impact of drug class on adherence to antihypertensives. Circulation 2011;123(15):1611–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bramlage P, Hasford J. Blood pressure reduction, persistence and costs in the evaluation of antihypertensive drug treatment—a review. Cardiovasc Diabetol 2009;8(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marshall IJ, Wolfe CDA, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. Br Med J 2012;345:e3953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maimaris W, Paty J, Perel P et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med 2013;10(7):e1001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mann BS, Barnieh L, Tang K et al. Association between drug insurance cost sharing strategies and outcomes in patients with chronic diseases: a systematic review. PLoS One 2014;9(3):e89168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Eze-Nliam CM, Thombs BD, Lima BB et al. The association of depression with adherence to antihypertensive medications: a systematic review. J Hypertens 2010;28(9):1785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sherrill B, Halpern M, Khan S et al. Single-pill vs free-equivalent combination therapies for hypertension: a meta-analysis of health care costs and adherence. J Clin Hypertens 2011;13(12):898–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010;55(2):399–407. [DOI] [PubMed] [Google Scholar]
- 35. Mallat SG, Tanios BY, Itani HS et al. Free versus fixed combination antihypertensive therapy for essential arterial hypertension: a systematic review and meta-analysis. PLoS One 2016;11(8):e0161285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bangalore S, Kamalakkannan G, Parkar S et al. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med 2007;120(8):713–9. [DOI] [PubMed] [Google Scholar]
- 37. Banerjee A, Werba JP, Neto JRF et al. Health system barriers to and facilitators of adherence to medications for the secondary prevention of cardiovascular disease: a systematic review. Glob Heart 2016;1:e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mamudu HM, Paul TK, Veeranki SP et al. The effects of coronary artery calcium screening on behavioral modification, risk perception, and medication adherence among asymptomatic adults: a systematic review. Atherosclerosis 2014;236(2):338–50. [DOI] [PubMed] [Google Scholar]
- 39. Grodensky CA, Golin CE, Ochtera RD et al. Systematic review: effect of alcohol intake on adherence to outpatient medication regimens for chronic diseases. J Stud Alcohol Drugs 2012;73(6):899–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sabeté E. Adherence to Long-Term Therapies: Evidence for Action. 2003. [PubMed]
- 41. Cramer JA, Benedict Á, Muszbek N et al. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract 2008;62(1):76–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chowdhury R, Khan H, Heydon E et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J 2013;34(38):2940–8. [DOI] [PubMed] [Google Scholar]
- 43. Bitton A, Choudhry NK, Matlin OS et al. The impact of medication adherence on coronary artery disease costs and outcomes: a systematic review. Am J Med 2013;126(4):357.e7–357.e27. [DOI] [PubMed] [Google Scholar]
- 44. Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med 2012;125(9):882–887.e1. [DOI] [PubMed] [Google Scholar]
- 45. Simpson RJ Jr, Mendys P. The effects of adherence and persistence on clinical outcomes in patients treated with statins: a systematic review. J Clin Lipidol 2010;4(6):462–71. [DOI] [PubMed] [Google Scholar]
- 46. DiMatteo MR, Giordani PJ, Lepper HS et al. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care 2002;40(9):794–811. [DOI] [PubMed] [Google Scholar]
- 47. Wetzels GE, Nelemans P, Schouten JS et al. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: a systematic review. J Hypertens 2004;22(10):1849–55. [DOI] [PubMed] [Google Scholar]
- 48. Boswell KA, Cook CL, Burch SP et al. Associating medication adherence with improved outcomes: a systematic literature review. Am J Pharm Benefits 2012;4(4):97–108. [Google Scholar]
- 49. Shroufi A, Powles JW. Adherence and chemoprevention in major cardiovascular disease: a simulation study of the benefits of additional use of statins. J Epidemiol Community Health 2010;64(2):109. [DOI] [PubMed] [Google Scholar]
- 50. Abegaz TM, Shehab A, Gebreyohannes EA et al. Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine 2017;96(4):e5641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Jongstra S, Harrison JK, Quinn TJ et al. Antihypertensive withdrawal for the prevention of cognitive decline. Cochrane Database Syst Rev 2016;2016(11):CD011971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Smith V, Devane D, Begley CM et al. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 2011;11(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Vrijens B, De Geest S, Hughes DA et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 2012;73(5):691–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.