Abstract
Background
Posterior subcapsular cataract is a tissue reaction commonly found among professionals exposed to ionizing radiation.
Objective
To assess the prevalence of cataract in professionals working in hemodynamics in Brazil.
Methods
Professionals exposed to ionizing radiation (group 1, G1) underwent slit lamp examination with a biomicroscope for lens examination and compared with non-exposed subjects (group 2, G2). Ophthalmologic findings were described and classified by opacity degree and localization using the Lens Opacities Classification System III. Both groups answered a questionnaire on work and health conditions to investigate the presence of risk factors for cataract. The level of significance was set at 5% (p < 0.05).
Results
A total of 112 volunteers of G1, mean age of 44.95 (±10.23) years, and 88 volunteers of G2, mean age of 48.07 (±12.18) years were evaluated; 75.2% of G1 and 85.2% of G2 were physicians. Statistical analysis between G1 and G2 showed a prevalence of posterior subcapsular cataract of 13% and 2% in G1 and G2, respectively (0.0081). Considering physicians only, 38% of G1 and 15% of G2 had cataract, with the prevalence of posterior subcapsular cataract of 13% and 3%, respectively (p = 0.0176). Among non-physicians, no difference was found in the prevalence of cataract (by types).
Conclusions
Cataract was more prevalent in professionals exposed to ionizing radiation, with posterior subcapsular cataract the most frequent finding.
Keywords: Cataract/surgery; Radiation,Ionizing; Cardiologists; Hemodynamics; Occupational Risks; Radiation,Protection
Introduction
In the last years, due to considerable increase in the complexity of diagnostic and therapeutic procedures in cardiology, radiology and interventional neurology, health professionals have been increasingly exposed to ionizing radiation. This has been particularly seen in some areas, including interventional cardiology.1 With the development of new therapeutic devices and adjuvant therapy, cardiologists have been involved in even more complex and longer procedures, requiring longer exposure to ionizing radiation.2
Routine, continuous exposure to radiation may cause deleterious effects on human body by direct or indirect effect on the cells, causing physiological and/or functional damage to the organs. For any radiation dosage, there is the risk of neoplasm and cell death, with a direct relationship between the dose and the risk.3,4
The lens is one of the most sensitive tissues to ionizing radiation. Studies have suggested a significant risk of changes in the lens in populations exposed to low radiation doses. These populations include patients undergoing computed tomography,5 astronauts,6,7 radiologic technologists,8 patients undergoing radiotherapy,9 atomic bombing survivors,10,11 and Chernobyl survivors.12,13 The most common change in the lens reported in these studies was lens opacity classified as posterior subcapsular cataract (PSC).14 Considering health professionals, studies have shown higher prevalence of this type of cataract among individuals working in interventional radiology.15-18
In 2011, the International Commission for Radiological Protection (ICRP) revised radiation threshold levels that may cause lens damage, and reduced the occupational dose limits, aiming to reduce the incidence of cataract induced by radiation among health professionals.19
During last years, interventional cardiology has exponentially increased in Brazil; however, so far, there is no data available on the prevalence of lens opacity among exposed professionals. Therefore, the aim of the present study was to evaluate the prevalence of cataract in interventional cardiologists (ICs) and professionals working in hemodynamics and possible factors that could minimize the risk.
Methods
Subjects
Eligible participants were recruited at health conferences health. Inclusion criteria were conference attendance and signing of the consent form. Exclusion criteria were - previous ocular surgeries, including cataract, glaucoma, refractive and retina surgeries; chronic use of ocular topical medication; diabetes mellitus; chronic use of corticosteroids and systemic arterial hypertension.
Logistics
All individuals included in the study were volunteers who self-referred to the investigators expressing their willingness to participate in the study. The investigators built an exhibition stand at two medical conferences, so that the attendees had easy, fast access to it.
The individuals included in the study were allocated into one of two groups - exposed to ionizing radiation (G1) and not exposed to ionizing radiation (G2). G1 was composed of ICs and health professionals in the field of cardiac hemodynamics from several regions of Brazil, who attended the annual congress of the Latin American Society of Interventional Cardiology (SOLACI) and the Brazilian Society of Hemodynamics and Interventional Cardiology (SBHCI) that was held in Rio de Janeiro on June 08th-10th, 2016. G2 was composed of cardiologists not exposed to ionizing radiation, attending the annual congress of the Brazilian Society of Cardiology held in Fortaleza on September 23rd-25th, 2016.
Clinical assessment and ophthalmologic examination
All participants were interviewed by one of the investigators who used a detailed questionnaire on demographic data, occupational practices that may be subjected to radiation exposure (use of radiation protection devices, number of years of work, types of procedures performed, among others) and coexisting diseases.
Ophthalmologic examination was performed using slit lamp examination by two experienced ophthalmologists, after the instillation of topical ocular medication (mydriacyl), which allows examination of the whole lens. The findings were described and classified by opacity pattern and degree according to the Lens Opacities Classification System III (LOCS III).20 It consists of the classification of lens opacity by its pattern as cortical, nuclear, and posterior subcapsular, and by its severity as grade 1-6.
Statistical analysis
A convenience sample was used in the study. Continuous variables were described as mean and standard deviation or median. The Kolmogorov-Smirnov test and the Shapiro-Wilk test were used to test the normality of data distribution. Categorical variables were compared by the chi-square test. When more than 20% of the cells had expected frequency lower than 5, we used the Fisher's exact test (2 x 2 table) or the likelihood ratio test. The level of significance was set at 5% (p < 0.05). The SPSS (Statistical Package for the Social Sciences) version 19.0 was used of the analysis.
Results
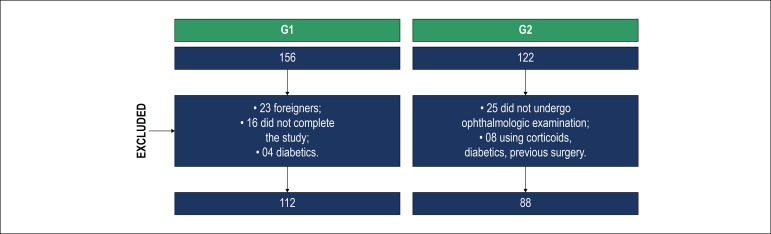
A total of 278 volunteers agreed to participate in the study, 156 in the radiation-exposed group (G1) and 122 in the non-exposed group (G2). Forty-four volunteers of G1 and 34 of G2 were excluded, and thus 112 participants in G1 and 88 in G2 were included (Figure 1). Mean age was 44.95 ± 10.23 years in the G1 and 48.07 ±12.18 years in the G2 (p = 0.0264). Sociodemographic data are described in Table 1.
Figure 1.
Flowchart of the study.
Table 1.
Sociodemographic data of the volunteers
| G1 | G2 | ||
|---|---|---|---|
| Age (mean) | 44.95 (±10.23) | 48.07 (±12.18) | |
| Age range | <36 | 28 (21.9%) | 18 (20.5%) |
| 36-45 | 45 (35.4%) | 14 (15.9%) | |
| 46-55 | 37 (32.7%) | 29 (33%) | |
| 56-65 | 10 (8.8%) | 22 (25%) | |
| >66 | 4 (3.5%) | 5 (5.7%) | |
| Sex | Female | 24 (21.4%) | 14 (15.9%) |
| Male | 88 (78.6%) | 74 (84.1%) | |
| Region | Middle-west | 7 (6.4%) | 10 (11.4%) |
| North | 6 (5.5%) | 5 (5.7%) | |
| Northeast | 20 (18.2%) | 22 (25%) | |
| South | 11 (10%) | 11 (12.5%) | |
| Southeast | 66 (60%) | 40 (45.6%) | |
| Occupation | Nurse | 21 (18.6%) | 1 (1.1%) |
| Physician | 85 (75.2%) | 75 (85.2%) | |
| Nurse technician or nursing assistant | 3 (3.1%) | 11 (12.5%) | |
| Technician or technologist | 3 (2.7%) | 1 (1.1%) | |
| Total | 112 | 88 | |
Regarding the ophthalmologic findings, 37 volunteers (33%) in G1 and only 14 (16%) in G2 had some degree of lens opacity (p = 0.0058). When analyzed by the type of cataract, no difference was found in the frequency of cortical cataract, with 15 individuals in G1 (13%) and 8 in G2 (9%) (p = 0.3438). However, PSC cataract was significantly more frequent in G1 (n = 14, 13%) than in G2 (n = 2, 2%) (p = 0.0081). Lens opacity in cortical + subcapsular was found in 28 volunteers in G1 (25%) and 10 in G2 (11%) (p = 0.0147).
Analysis by occupational category showed a mean age of 46.76 ± 9.99 years among ICs and 48.75 ± 12.32 in the control group, with no difference between the groups (p = 0.1358). Lens opacity was found in 32 ICs (38%) and 11 clinical cardiologists (CCs) (15%) (p = 0.0011). PSC cataract was found in 11 ICs (13%) and 2 CCs (3%) (p = 0.0176). The presence of cortical cataract + subcapsular cataract was found in 28% of ICs (n = 24) and 9% of CCs (n = 7) (p = 0.0025). No statistically significant difference was found in the frequency of cortical cataract (15% versus 7%, p = 0.0848).
In the group of non-physicians exposed to radiation, 5 participants showed some degree of lens opacity (18%), which was also detected in 3 control non-physicians (23%) (p = 0.7357). Subcapsular cataract was found in 3 radiation-exposed non-physicians, and in none control non-physicians (p = 0.2114).
Regarding the eye affected, cataract in the left eye was more common, with SCP cataract observed in 50% of the exposed individuals, whereas cataract in the right eye was identified in 14% of exposed participants. Cataract in both eyes was affected in 36% of these individuals. Cortical cataract was also more frequent in the left eye (46% of exposed subjects), whereas the right eye was affected in 27% of the cases.
In the control group, no eye was more prevalent than the other in the cases of cataract, with similar frequency in both eyes as well as cataract type - cortical and subcapsular - both bilateral in 60% of cases.
Most ICs reported to perform 50 procedures per month (38.1%) and from 50 to 100 procedures (43.7%) per month. Eighty-two percent of the ICs reported to perform diagnostic procedures within 30 minutes, using from four to six X-ray energy projections (46.5%) and 15 frames per second (70.9%). For therapeutic procedures, 66.1% of ICs reported that the procedures lasted 30-60 minutes, with delivery of x-ray energy in pulses (rather than in a continuous dose).
The number of years of work in hemodynamics was not a statistically significant determinant for the occurrence of lens opacity; 62% of the professionals reported less than 20 years of work years, and half of them reported between 5 and 10 years of work in the field. Although we did not find a correlation between damage and work experience time, lens opacity could occur early in those with lower time of work experience. This reinforces the importance of the use of personal and collective protective devices.
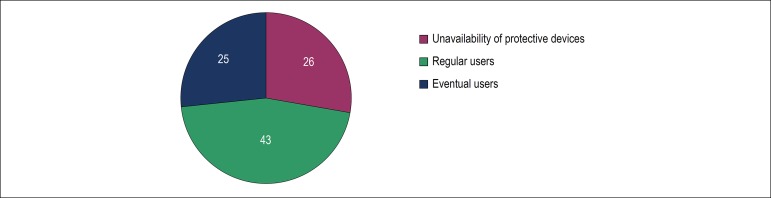
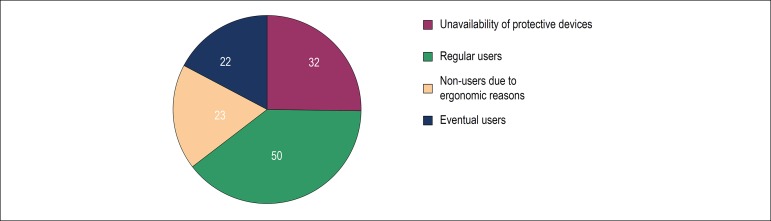
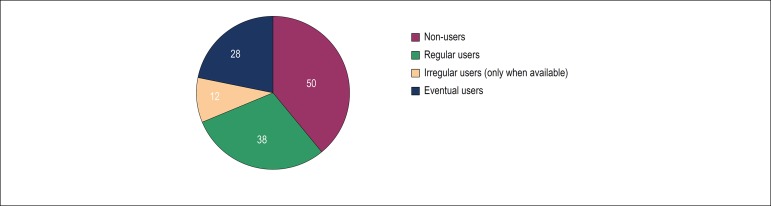
Results of the use of personal and collective protective devices reported by the physicians are described in Figures 3,4 and 5.
Figure 3.
Frequency (%) of use of lead shields placed laterally to the fluoroscopy table by interventionists (n = xx).
Figure 4.
Frequency (%) of use of lead glasses by interventionists (n = xx).
Figure 5.
Frequency (%) of use of suspended radiation protection by interventionists (n = xx).
Regarding the use of lead glasses (with or without lateral protection) 40% of the radiation-exposed volunteers reported to be regular users, although this result did not show a statistically significant correlation with the frequency of lens opacity. The same was observed with the routine use of lead shielding, reported by approximately 30% of the professionals. The reasons for the low frequency of routine use of protective devices, reported by participants, are graphically illustrated in Figures 1-3, such as - ergonomic discomfort, unavailability of protective device, among others.
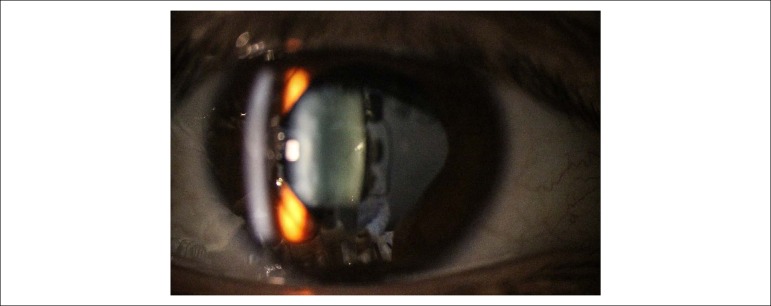
Figure 2.
Subcapsular cataract in a young interventional cardiologist.
Discussion
ICs and other professionals that work in hemodynamics are routinely exposed to ionizing radiation and hence at higher risk for the deleterious effects of this exposure. Eye lens are one of the most sensitive organs to continuous radiation exposure. Many studies in several countries have shown a higher prevalence of cataract in professionals exposed to radiation, with the PSC type more frequently correlated with ionizing radiation.21-23
The increase in the prevalence of cataract was identified with the increase in radiation doses and previously reported in literature review studies. Uncertainties about a radiation threshold that could induce lens opacity still exist. The latency period between irradiation and development of lens opacity is uncertain.24
The LOCS III grading system is considered relevant in these types of studies and have been used to compare recent data obtained from occupationally exposed individuals and atomic bomb survivors.24
In Brazil, interventional cardiology has played a prominent, internationally recognized role. Nevertheless, so far, there is no study on the prevalence of cataract among professionals or even in several areas of interventional radiology. The present study aims at filling this gap, providing nationwide information on the theme.
Our findings showed that interventional cardiology professionals have significantly more lens changes than non-exposed individuals (p = 0.0058), although the non-exposed groups were significantly older. Sucapsular cataract was more frequent in the exposed group (p = 0.0081) than in controls, confirming previously published results.18,21,23
The other types of cataract (cortical and nuclear), when separately analyzed, were not prevalent in the exposed group, corroborating results from previous studies.23 On the other hand, the prevalence of subcapsular + cortical cataract was higher in the exposed than in control group.
Our findings showed a higher prevalence of cataract in the left eye than in the right eye among participants. This was also reported in previous studies showing that, during interventional procedures, the left side of the brain receives higher doses of radiation, due to positioning of the professional during the tests.25,26
Analysis by occupational category highlighted a higher prevalence of lens opacity, of any type, in the exposed group (38% of ICs) and in clinicians that were not exposed to radiation (15%). PSC cataract, a lens opacity related to radiation exposure, was found in 13% of ICs and in only 3% of clinicians.
Elmaraezy et al.,27 in a metanalysis recently published, found a cataract prevalence, of any type, of 36% among ICs, similar to our results. In this same meta-analysis, all studies included reported a significant prevalence of subcapsular cataract in ICs, with no difference between the prevalence of cortical and nuclear opacity.
In the French O'CLOC study (Occupational Cataracts and Lens Opacities in interventional Cardiology), Jacob et al.21 found a prevalence of 17% of PSC in ICs and of 5% in the control group, similar to our findings.21 It is worth pointing out that, in the O’CLOC study, the control group was composed of non-physicians, differently from our study, in which radiation-exposed physicians were compared with medical cardiologists (non-interventionists), similar in number and age, but not exposed to ionizing radiation.
Vañó et al.18 found a significant prevalence of PSC cataract among interventional catheterization professionals - physicians, nurses and technicians. We did not find a significantly greater prevalence of cataract in radiation-exposed non-physicians when compared with the control group. This can be mainly explained by the small number of non-physicians included in the study (25% nurses and 3% nursing assistants), professional categories and years of work in catheterization laboratory.
Professional activity measured in years of work and number of procedures performed annually can be predictors of increased risk of damage, as we tend to associate them with increased cumulative dose. However, we should consider that the use of protective devices and the ability of professionals in performing the procedures may significantly change these cumulative doses. Some authors have shown that there is no clear relationship between the incidence of lens opacity and number of procedures, as in the study by Jacob et al.21 in which the number of procedures varied from 50 to 1,267, with a mean of 542 ± 312 procedures per year. In their study,21 the risk for cataract was lower in regular users of lead glasses as compared with irregular users, without statistical significance though.21
In our study, only 40% of the radiation-exposed volunteers reported to wear lead glasses on a regular basis, which make our sample size (considering both exposed and non-exposed groups) even smaller. Besides, variables such as age, work experience, number of procedures performed, lead shielding, among others make it difficult to establish any association between the regular use of protective device and the findings. Also, there are no data regarding occupational dose. Studies have highlighted the importance of the accuracy of dosimetry measurements in clinical practice to determine correlations of radiation doses and effects.28,29 In the present study, we could not estimate the radiation dose received by the participants exposed. Also, by interview of participants, we found that only 63.8% of them used personal radiation dosimeters over the lead (chest) aprons for their own control, although this device is the most reliable way to measure cumulative radiation over a month, and its usage is regulated by current radiation protection legislation.30,31
Variations in individual doses recorded in dosimeters can help in the understanding of conditions associated with increased doses and establishment of safer conditions during the procedures. Safety promotion, by means of reduction of radiation doses delivered to the patient and the staff, is a responsibility of the operator. Fluoroscopy and cinefluorography time should be controlled, as well as the total cumulative dose for the patient (air kerma) should be monitored and registered at the end of the test, For dose reduction, adequate collimation and use of virtual collimation are essential, in addition to other factors, including virtual expansion and geometric adjustments may affect the distribution of scattered radiation. The use of mobile radiation shields, including suspended radiation protection and lead shields placed laterally to the fluoroscopy table, are relevant strategies to reduce individual radiation doses, and should be used regardless of gantry angulations. The adoption of angiography device in cardiovascular procedures in terms of radiologic protection was summarized in a recent study that describes all adjustments necessary to minimize the radiation doses delivered to patients and professionals.32
Although the use of protective lead glasses was recognized as important protective devices by radiation-exposed volunteers, the reason for their low frequency of use, according to them was mainly their “weight” and “difficult adjustment to the face”. Thus, ergonomic improvements should be made to encourage the use of protective lead glasses on a routine basis.
Evidence of early occurrence of lens opacity has been discussed in the scientific community; however, the fact that participants have received a radiation dose lower than the occupational threshold (mean of 5 years, 20 mSy/year) can be attributed to the fact that they did not use personal protective apparatus regularly.18
Despite the consistent findings of our study, some limitations should be noted. There are some uncertainties regarding the use of personal and collective protective devices that cannot be measured, since these data were obtained by interview. Nevertheless, despite the uncertainties of dose estimates using a radiation dosimeter, an effective control of the doses enables the correlation of dose and tissue damage. In our study, this correlation could not be evaluated since information on individual occupation dose were not available.
Conclusions
In the present study, we detected early occurrence of lens opacity in Brazilian interventional cardiologists, who attended the annual congress of the SOLACI/SBHCI.
The questionnaire administered by interview allowed us to obtain information about the current use of radiation protective devices and to detect the need for strategies that reinforce the importance of fostering a culture of radiologic protection among professionals exposed to radiation.
Acknowledgment
To all those present at the SOLACI and SBC 2016 congresses who agreed to participate voluntarily.
Footnotes
Sources of Funding
This study was funded by Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.
Study Association
This study is not associated with any thesis or dissertation work.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Unifesp/EPM under the protocol number 1.550.372. All the procedures in this study were in accordance with the 1975 Helsinki Declaration, updated in 2013. Informed consent was obtained from all participants included in the study.
Author contributions
Conception and design of the research: Barbosa AHP, Medeiros RB; acquisition of data: Barbosa AHP, Medeiros RB, Corpa AMR, Higa FS, Souza MT, Barbosa PL, Moreira AC; analysis and interpretation of the data: Barbosa AHP, Medeiros RB, Corpa AMR, Higa FS; statistical analysis: Barbosa AHP; obtaining funding: Barbosa AHP, Lemke VMG, Cantarelli MJC; writing of the manuscript: Barbosa AHP, Medeiros RB, Corpa AMR, Cantarelli MJC; critical revision of the manuscript for intellectual content: Barbosa AHP, Medeiros RB, Quadros AS, Cantarelli MJC.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Picano E, Vañó E. The radiation issue in cardiology: The time for action is now. Cardiovasc Ultrasound. 2011 Nov 21;9:35–35. doi: 10.1186/1476-7120-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klein LW, Miller DL, Balter S, Laskey W, Haines D, Norbash A, et al. Occupational health hazards in the interventional laboratory: time for a safer environment. Radiology. 2009;250(2):538–544. doi: 10.1148/radiol.2502082558. [DOI] [PubMed] [Google Scholar]
- 3.Hamada N, Fujimichi Y. Classification of radiation effects for dose limitation purposes: history, current situation and future prospects. J Radiat Res. 2014;55(4):629–640. doi: 10.1093/jrr/rru019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hendry JH. Radiation biology and radiation protection. Ann ICRP. 2012;41(3-4):64–71. doi: 10.1016/j.icrp.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Klein BE, Klein R, Linton KL, Franke T. Diagnostic x-ray exposure and lens opacities: the Beaver Dam Eye Study. Am J Public Health. 1993;83(4):588–590. doi: 10.2105/ajph.83.4.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cucinotta FA, Manuel FK, Jones J, Iszard G, Murrey J, Djojonegro B, et al. Space radiation and cataracts in astronauts. Radiat Res. 2001;156(6):811–811. doi: 10.1667/0033-7587(2001)156[0460:sracia]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 7.Rastegar N, Eckart P, Mertz M. Radiation-induced cataract in astronauts and cosmonauts. Graefes Arch Clin Exp Ophthalmol. 2002;240(7):543–547. doi: 10.1007/s00417-002-0489-4. [DOI] [PubMed] [Google Scholar]
- 8.Chodick C, Bekiroglu N, Hauptmann M, Alexander BH, Freedman DM, Doody MM, et al. Risk of cataract after exposure to low doses of ionizing radiation: a 20-year prospective cohort study among US radiologic technologists. Am. J. Epidemiol. 2008;168(6):620–631. doi: 10.1093/aje/kwn171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hall P, Granath F, Lundell M, Olsson K, Holm LE. Lenticular opacities in individuals exposed to ionizing radiation in infancy. Radiat Res. 1999;152(2):190–195. [PubMed] [Google Scholar]
- 10.Nakashima E, Nerisihi K, Minamoto A. A reanalysis of atomic-bomb cataract data, 2000-2002: a threshold analysis. Health Phys. 2006;90(2):154–160. doi: 10.1097/01.hp.0000175442.03596.63. [DOI] [PubMed] [Google Scholar]
- 11.Nerisihi K, Nakashima E, Minamoto A, Fujiwara S, Akahoshi M, Mishima HK, et al. Postoperative cataract cases among atomic bomb survivors: radiation dose response and threshold. Radiat Res. 2007;168(4):404–408. doi: 10.1667/RR0928.1. [DOI] [PubMed] [Google Scholar]
- 12.Day R, Gorin MB, Eller AW. Prevalence of lens changes in Ukrainian children residing around Chernobyl. Health Phys. 1995;68(5):632–642. doi: 10.1097/00004032-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Worgul BV, Kundiyev YI, Sergiyenko NM, Chumak VV, Vitte PM, Medvedovsky C, et al. Cataracts among Chernobyl clean-up workers: implications regarding permissible eye exposures. Radiat Res. 2007;167(2):233–243. doi: 10.1667/rr0298.1. [DOI] [PubMed] [Google Scholar]
- 14.Vanõ E, Kleiman NJ, Duran A, Rehani MM, Echeverri D, Cabrera M. Radiation cataract risk in interventional cardiology personnel. Radiat Res. 2010;174(4):490–495. doi: 10.1667/RR2207.1. [DOI] [PubMed] [Google Scholar]
- 15.Ciraj-Bjelac O, Rehani M, Minamoto A, Sim KH, Liew HB, Vano E. Radiation-induced eye lens changes and risk for cataract in interventional cardiology. Cardiology. 2012;123(3):168–171. doi: 10.1159/000342458. [DOI] [PubMed] [Google Scholar]
- 16.Ciraj-Bjelac O, Rehani MM, Sim KH, Liew HB, Vano E, Kleiman NJ. Risk for radiation-induced cataract for staff in interventional cardiology: is there reason for concern? Catheter Cardiovasc Interv. 2010;76(6):826–834. doi: 10.1002/ccd.22670. [DOI] [PubMed] [Google Scholar]
- 17.ICRP. Stewart FA, Akleyev AV, Hauer-Jensen M, Hendry JH, Kleiman NJ, et al. ICRP publication 118: ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs-threshold doses for tissue reactions in a radiation protection context. Ann ICRP. 2012;41(1-2):1–322. doi: 10.1016/j.icrp.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Vanõ E, Kleiman NJ, Duran A, Romano-Muller M, Rehani MM. Radiation-associated lens opacities in catheterization personnel: results of a survey and direct assessments. J Vasc Interv Radiol. 2013;24(2):197–204. doi: 10.1016/j.jvir.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 19.ICRP . International Commission on Radiological Protection. ICRP [Internet] Ottawa: ICRP; 2011. [dez. 2018]. Annual Report 2011. Disponível em: http://www.icrp.org/docs/ICRP%20Annual%20Report%202011.pdf. [Google Scholar]
- 20.Chylack Jr LT, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111(6):831–836. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- 21.Jacob S, Boveda S, Bar O, Brézin A, Maccia C, Laurier D, et al. Interventional cardiologists and risk of radiation-induced cataract: results of a French multicenter observational study. Int J Cardiol. 2013;167(5):1843–1847. doi: 10.1016/j.ijcard.2012.04.124. [DOI] [PubMed] [Google Scholar]
- 22.Yuan M, Chien CW, Lee SK, Hsu NW, Chang SC, Chang SJ, et al. Health effects of medical radiation on cardiologists who perform cardiac catheterization. J Chin Med Assoc. 2010;73(4):199–204. doi: 10.1016/S1726-4901(10)70041-1. [DOI] [PubMed] [Google Scholar]
- 23.Bitarafan Rajabi A, Noohi F, Hashemi H, Haghjoo M, Miraftab M, Yaghoobi N, et al. Ionizing radiation-induced cataract in interventional cardiology staff. Rev Cardiovasc Med. 2015;4(1):e25148. doi: 10.5812/cardiovascmed.25148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hammer GP, Scheidemann-Wesp U, Samkange-Zeeb F, Wicke H, Neriishi K, Blettner M. Occupational exposure to low doses of ionizing radiation and cataract development: a systematic literature review and perspectives on future studies. Radiat Environ Biophys. 2013;52(3):303–319. doi: 10.1007/s00411-013-0477-6. [DOI] [PubMed] [Google Scholar]
- 25.Reeves RR, Ang L, Bahadorani J, Naghi J, Dominguez A, Palakodeti V, et al. Invasive cardiologists are exposed to greater left sided cranial radiation: The BRAIN Study (Brain Radiation Exposure and Attenuation During Invasive Cardiology Procedures) JACC Cardiovasc Interv. 2015;8(9):1197–1206. doi: 10.1016/j.jcin.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 26.O'Connor U, Walsh C, Gallagher A, Dowling A, Guiney M, Ryan JM, et al. Occupational radiation dose to eyes from interventional radiology procedures in light of the new eye lens dose limit from the International Commission on Radiological Protection. Br J Radiol. 2015;88(1049):20140627. doi: 10.1259/bjr.20140627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elmaraezy A, Morra ME, Mohammed AT, Al-Habaa A, Elgebaly A, Ghazy AA, et al. Risk of cataract among interventional cardiologists and catheterization lab staff: a systematic review and meta-analysis. Catheter Cardiovasc Interv. 2017;90(1):1–9. doi: 10.1002/ccd.27114. [DOI] [PubMed] [Google Scholar]
- 28.Ciraj-Bjelac O, Carinou E, Ferrari P, Gingaume M, Merce MS, O'Connor U. Occupational exposure of the eye lens in interventional procedures: how to assess and manage radiation dose. J Am Coll Radiol. 2016;13(11):1347–1353. doi: 10.1016/j.jacr.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 29.Barnard SG, Ainsbury EA, Quinlan RA, Bouffler SD. Radiation protection of the eye lens in medical workers-basis and impacto of the ICRP recommendations. Br J Radiol. 2016;89(1060):20151034. doi: 10.1259/bjr.20151034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Norma CNEN NN 3.01 [Internet] Brasilia: CNEN; Disponível em: http://appasp.cnen.gov.br/seguranca/normas/pdf/Nrm301.pdf. [Google Scholar]
- 31.Ministério da Saúde Portaria 453, de 01 de junho de 1998. Diretrizes Básicas de Proteção Radiológica em Radiodiagnóstico Médico e Odontológico. Diário Oficial da União. 1998 Jun 02; Secão 1.
- 32.Christopoulos G, Makke L, Christakopoulos G, Kotsia A, Rangan BV, Roesle M, et al. Optimizing radiation safety in the cardiac catheterization laboratory: a practical approach. Catheter Cardiovasc Interv. 2016;87(2):291–301. doi: 10.1002/ccd.25959. [DOI] [PubMed] [Google Scholar]