Introduction
We report three cases of spontaneous coronary artery dissection (SCAD), with literature review and discussion of the procedures employed. All of them occurred in women, with the diagnosis being made by coronary angiography and, in one case, confirmed by intravascular ultrasound (IVUS).
1st Case
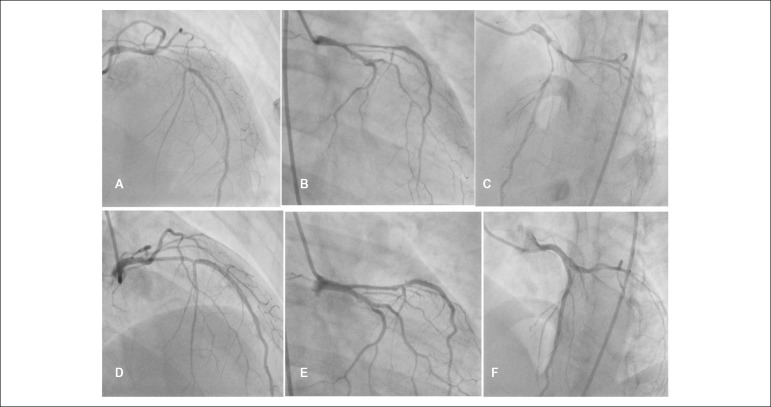
The patient was 25 years old, with no risk factors for cardiovascular disease (CVD), hospitalized with typical chest pain, elevated cardiac enzymes and electrocardiogram (ECG) with diffuse ST-depression and ST-segment elevation in aVR, underwent cardiac catheterization (CC), which disclosed moderate lesion in the left main coronary artery (LMCA), severe lesion in the proximal third of the anterior descending artery (ADA) and parietal irregularities in the circumflex artery (Cx) (Figure 1). Transthoracic echocardiogram (TTE) showed mid-apical hypokinesia of the anterior, inferolateral walls and small apical areas, with preserved biventricular systolic function. The patient was submitted to an IVUS that showed aspect compatible with intramural hematoma from the DA ostium to the first diagonal artery, and spontaneous dissection/hematoma from the proximal third of the Cx to the distal third of the first left marginal artery (image not available). Clinical treatment was chosen with excellent response. During outpatient follow-up, she remained asymptomatic. An angiographic restudy was performed six months after the event, showing significant obstruction improvement (Figure 1).
Figure 1.
Cardiac catheterization showing stenosis in the middle/distal third of the left main coronary artery and severe segmental stenosis in the ostium/ proximal third of the anterior descending artery in the right cranial (A), right caudal (B) and left cranial (C) views. Restudy, after six months, showed a significant improvement of obstructions in the right cranial (D), right caudal (E) and left cranial (F) views.
2nd Case
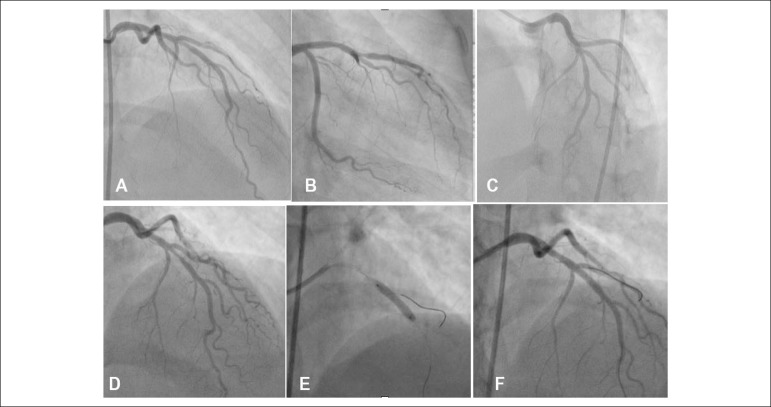
The patient was 41 years old with hypertension, hypothyroidism and was an ex-smoker, having delivered a child six months before. She sought the emergency service with typical chest pain triggered by emotional stress and ECG showing +/- in the high lateral wall. She was referred to CC, which showed moderate lesion in the middle third of the ADA and moderate/severe lesion in the distal third, suggestive of SCAD. The TTE showed no alterations. Clinical treatment was chosen. Angiographic restudy three months after the event showed persistence of moderate obstruction in the middle third of the ADA, with obstruction resolution in the distal third. At the time, stent implantation was performed in the middle third of the ADA. The procedure showed no complications and was successful (Figure 2).
Figure 2.
Cardiac catheterization showing moderate stenosis in the middle third and moderate/severe segmental stenosis in the distal third of the anterior descending artery (ADA) in the cranial (A), right caudal (B) and left cranial (C) views. Restudy, after 3 months, showed a significant improvement of the obstruction in the distal third of the ADA, with moderate obstruction in the middle third, which was treated with the direct stenting technique (cranial view, images: D, E and F).
3rd Case
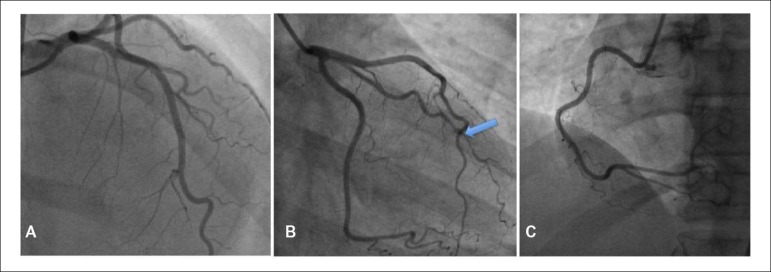
The patient was 51 years old, with no risk factors for CVD, hospitalized with typical chest pain and elevated cardiac enzymes. The ECG showed no alterations. She was referred to the hemodynamics service, and a severe lesion was disclosed in the distal third of the first left marginal artery, with a pattern suggestive of SCAD. The TTE showed moderate hypokinesia of the left ventricular inferior-lateral, with preserved biventricular systolic function. She received clinical treatment with good response to therapy (Figure 3).
Figure 3.
Cardiac catheterization showing angiographic aspect compatible with spontaneous dissection of the distal third of the first left marginal branch. The left coronary is observed in the angiographic views: cranial (A) and right caudal (B). The blue arrow (B) identifies the spontaneous dissection segment of the first left marginal branch. The right coronary artery with a normal aspect in the left oblique view (C) is observed.
Discussion
In 1931, Pretty first described SCAD during the autopsy of a 42-year-old woman who had sudden death after reporting chest pain.1 With the onset of the invasive approach to acute coronary syndrome (ACS), the number of diagnosed cases increased. Nevertheless, it is still believed that this diagnosis may be underestimated.2
SCAD is a rare cause of ACS, with an incidence of 0.1 to 4.0%.3 The clinical presentation ranges from unstable angina to sudden death, often being undiagnosed. It mainly affects young women with no classic CVD risk factors.4 In the reported cases, all of them are young women, two of which did not have CVD risk factors.
The following are described as events that may be related to SCAD: peripartum status, connective tissue diseases, vasculitis, cocaine abuse, heavy isometric exercise and use of oral contraceptives.5 The most frequently affected artery is the ADA, in 75% of cases, followed by the right coronary artery, in 20% of the patients; the Cx, in 4%, and finally the LCMA, in less than 1% of the cases.6 Among the three reported cases, two had the ADA as the main affected artery, which corroborates with data found in the literature.
The pathogenesis of SCAD has yet to be fully elucidated. It is known that the main factors responsible for spontaneous dissection are the arterial wall weakening and increased shear forces.3 It is postulated that the primary rupture of the vasa vasorum occurs, leading to hemorrhage and consequent separation of the coronary artery wall layers, creating a false lumen between the intima and media layers of the vascular wall.7
From the angiographic point of view, the diagnosis of CAD should be considered when there is a dissection line, with or without a false lumen, sudden and significant caliber reduction, or obstruction with smooth borders without the aspect of atherosclerotic disease.6 Because it is a two-dimensional aluminography, the coronary angiography reveals little in relation to the coronary artery wall, where the main SCAD alteration is found.3
The IVUS and optical coherence tomography (OCT) have been shown to be important tools in the diagnosis of SCAD, in cases where there is doubt regarding the angiography, since they allow a more detailed analysis of the lesion. The IVUS may also contribute to guide the percutaneous treatment whenever necessary.4 In fact, the use of intracoronary images, through IVUS or OCT, allows better visualization of the structure and composition of the coronary wall, allowing the evaluation of the intramural hematoma, as well as the differentiation between the true and the false lumens.3 The IVUS was performed in one of the reported cases, demonstrating an image compatible with SCAD.
The therapeutic management depends on the clinical severity, hemodynamic status, dissection topography, number of affected arteries, and distal coronary flow.6 It may range from clinical treatment, stent implantation, or myocardial revascularization surgery.7
In the cases described above, due to the clinical and hemodynamic stability with well-defined dissections, clinical treatment with dual antiplatelet therapy (clopidogrel and acetylsalicylic acid), statin and beta-blocker was initially chosen. Since percutaneous coronary intervention for SCAD is associated with a high rate of technical failures, the conservative strategy with clinical treatment and prolonged follow-up is preferable in these cases, with a high incidence of spontaneous resolution and a low incidence of adverse events.8
Recent studies have demonstrated the recurrence of cardiovascular events in hypertensive patients in the long-term, and beta-blocker therapy seems to have a protective effect.9 Therefore, these patients should remain under medical supervision. In one of the cases, during follow-up, persistence of moderate obstruction was demonstrated in the middle third of the ADA, and late stent implantation was performed, aiming at preventing event recurrence.
Finally, we emphasize that the diagnosis of SCAD should be considered in cases of ACS in young patients, especially women of childbearing age and without the classic risk factors for coronary artery disease. The test of choice for the diagnosis consists of coronary angiography, although in some cases it is necessary to perform IVUS or OCT as adjunct methods to corroborate the diagnosis or to determine lesion extent.
Footnotes
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Author contributions
Conception and design of the research, Acquisition of data and Analysis and interpretation of the data: Daniel ECA, Falcão JLAA; Writing of the manuscript: Daniel ECA; Critical revision of the manuscript for intellectual content: Falcão JLAA.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Pretty HC. Dissecting aneurysm of coronary artery in a woman aged 42: rupture. Br Med J. 1931;1:667–667. [Google Scholar]
- 2.Saw J. Spontaneous coronary artery dissection. Can J Cardiol. 2013;29(9):1027–1033. doi: 10.1016/j.cjca.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 3.Cade JR. Dissecção espontânea de artéria coronária no ciclo gravídico-puerperal: análise de uma série de 13 casos e revisão da literatura. São Paulo: faculdade de Medicina USP; 2016. [Google Scholar]
- 4.Barbosa RR, Rinaldi FS, Costa Jr JR, Feres F, Abizaid A, Sousa AGMR, et al. Infarto agudo do miocárdio por dissecção espontânea de artérias coronárias - Série de cinco casos. Rev Bras Cardiol Invasiva. 2013;21(2):193–198. [Google Scholar]
- 5.Kamissis G, Manolis A, Townend JN. Spontaneous coronary artery dissection/intramural haematoma in Young women with ST-elevation myocardial infarction: "It is not Always a plaque rupture event". Case Reports in Cardiology. 2015;2015:5–5. doi: 10.1155/2015/597234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oliveira MDP, Falcão BA, Mariani J, Campos CM, Ribeiro EE, Lemos PA. Extensa dissecção coronária espontânea com boa evolução clínica mantida sob tratamento conservador. Rev Bras Cardiol Invasiva. 2015;23(4):279–281. [Google Scholar]
- 7.Manhães EB, Gomes WF, Bezerra CG, Horta PE, Gama MN, Cesar LA, et al. Dissecção espontânea de artéria coronária: abordagem terapêutica e desfecho de uma série consecutiva de casos. Rev Bras Cadiol Invasiva. 2014;22(1):32–35. [Google Scholar]
- 8.Tweet MS, Eleid MF, Best PJ, Lennon RJ, Lerman A, Rihal CS, et al. Spontaneous coronary artery dissection revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7(6):777–786. doi: 10.1161/CIRCINTERVENTIONS.114.001659. [DOI] [PubMed] [Google Scholar]
- 9.Saw J, Humphries K, Aymong E, Sedlak T, Prakash R, Starovoytov A, et al. Spontaneous coronary artery dissection: clinical outcomes and risk of recurrence. J Am Coll Cardiol. 2017;70(9):1148–1158. doi: 10.1016/j.jacc.2017.06.053. [DOI] [PubMed] [Google Scholar]