Abstract
Infectious diseases are disorders caused by many different microorganisms that produce clinical conditions with a wide variation in patient-rated symptoms and severity. Therefore, different diagnostic and prognostic tools are needed to help make the most accurate decisions at each moment of patient´s care with suspected infection. This mini review will analyse how some biomarkers reduce the level of uncertainty in the making decision process at some phases of sepsis, including prompt identification of septic patients, early initiation of empiric broad-spectrum antimicrobials, regimen and duration.
Key words: sepsis, biomarkers, procalcitonin, lactate, MR-ProADM
Abstract
La patología infecciosa puede ser debida a microorganismos muy diferentes que producen cuadros clínicos con una expresividad muy variada tanto en los síntomas como en la gravedad. Por ello, se necesitan diferentes herramientas diagnósticas y pronósticas que ayuden a tomar las decisiones más adecuadas en cada momento de la atención a un paciente con sospecha de infección. En esta mini revisión se analizará cómo algunos biomarcadores disminuyen el nivel de incertidumbre en la toma de decisiones clínicas en algunas fases de la atención a la sepsis, como puede ser la propia identificación del paciente séptico, la necesidad de iniciar tratamiento antimicrobiano, el tipo y su duración.
Palabras clave: sepsis, biomarcador, procalcitonina, lactato, MR-ProADM
INTRODUCTION
The response to infection is such a complex process that both in patients with compromised immune system, such as neutropenic or lymphopenic patients, or in those with exaggerated reaction, this dysregulated host response results in increased mortality rates. In fact, the update of sepsis definition considers the organ system dysfunction as a result of the host response [1].
In this interaction between the host and the pathogen, a large amount of molecules are released whose usefulness as biomarkers for screening, diagnosis, risk stratification or monitoring, has been studied with some contradictious results that have questioned its clinical application [2, 3].
Unfortunately, no biomarker in sepsis has proven to have 100% sensitivity and specificity at the same time to establish the diagnosis of an infectious cause in those who suffer some organic failure or indicate when antibiotic treatment should be started or stopped, but their use help to make these decisions with a smaller margin of error. Thus, the main utility of a biomarker is given by its likelihood ratios (LR). The LR (+) = Sensitivity / (1 - specificity) and the LR (-) = (1 - sensitivity) / Specificity. For example, when a sepsis is suspected, a useful biomarker will have a high LR (+), which increases the post-test probability supporting the clinical diagnosis.
In general it is considered that LR> 10 or <0.1 generate large and often conclusive changes from pretest to posttest probability LR of 5 - 10 and 0.1 - 0.2 produce moderate shifts in pre-test to post-test probability, LR of 2 - 5 and 0.5 - 0.2 generate small (but sometimes important) changes in probability and LR of 1 - 2 and 0.5 - 1 will alter the probability to a small and rarely important degree [4].
The use of some normograms allows to better visualize how diagnostic probability post-test improves with the use of biomarkers (figure 1) [5].
Figure 1.
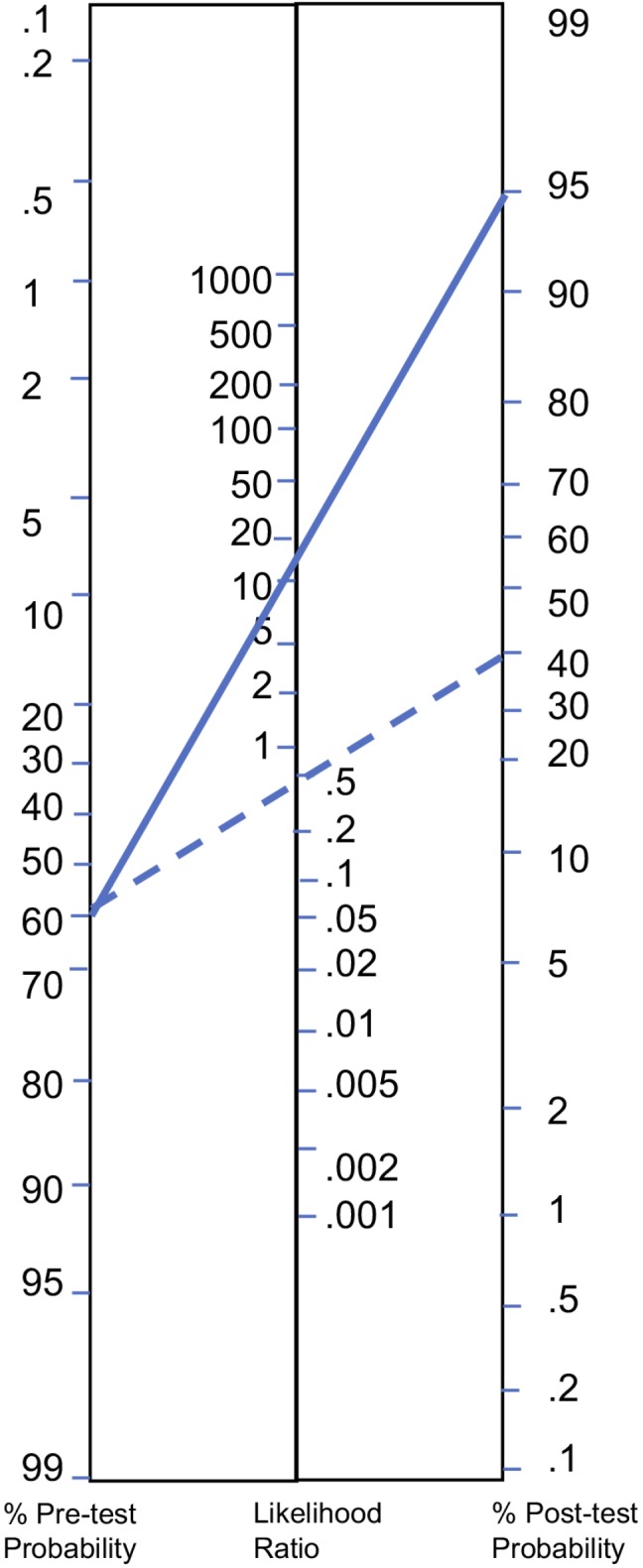
How interpret diagnostic test results. Adapted from Fagan[5].
Let us suppose a biomarker as PCT has proved to have a LR(+) to diagnosing ventilator associated pneumonia (VAP) of 13.5 and a LR(-) of 0.55 for a cut-off level of 3 ng/mL[6]. When suspecting a patient is suffering from VAP because of clinical and radiographic findings with a probability of 60% if the PCT is > 3 ng/mL the probability of VAP will raise up to 95% (continuous line) while if PCT is < 3 ng/mL the probability will decrease to around 40% (dash line) which can help us to decide starting antibiotics or not.
The determination of some biomarkers such as lactate or procalcitonin (PCT) has been automated and become cheaper in recent years, which has extended its use and several studies establish their LR at levels that produce moderate and sometimes important changes in decision making [6-8].
This “mini” review will focus on analyzing how their knowledge helps reduce the level of uncertainty in clinical decision making and can help both identify more serious patients and make better use of antibiotics. A brief consideration will be given to what can be contributed by the mid regional pro-adrenomedullin (MR-ProADM), described more recently.
THE USEFULNESS OF BIOMARKERS IN THE STRATIFICATION OF SEVERITY
The early identification of septic patients is particularly important in those who are critically ill because the rapid establishment of resuscitation measures and administration of the appropriate antimicrobial reduce mortality [9].
Recent definitions of sepsis have attempted to improve the sensitivity and specificity of the systemic inflammatory response syndrome (SIRS) to identify patients at increased risk of death in the course of an infection, by proposing q-SOFA ≥ 2 in emergency department or SOFA score ≥ 2 in patients admitted in ICU as the definition of sepsis, in other words, the infection that causes organic dysfunction [10].
According to this, in order to identify septic patients among those suffering from infection, no biomarker would be needed in the emergency department, but they are essential in the ICU to calculate SOFA score. However, it is necessary to point out that in the publication that stablishes the basis for the latest definitions of sepsis [10], the mortality of patients with lactate ≥ 2 mmol/L and q-SOFA = 0 is similar to those who had q-SOFA ≥ 2 and lactate ≤ 2 mmol/L which shows the usefulness of this biomarker to identify patients whose clinical symptoms do not express the true severity so we consider that it is essential to determine lactate in cases of high suspicion of sepsis, which may be valid in a venous blood sample for this purpose. On the other hand, these same definitions state that in order to diagnose septic shock, the presence of hyperlactacidemia ≥ 2 mmol/L is necessary as well as the need to associate vasopressors to maintain the mean arterial pressure ≥ 65 mmHg after fluid resuscitation [11].
Therefore, obtaining lactate in the initial stages of suspected sepsis is crucial and should be re-measured because it has proven to be a useful tool to know if the clinical course of sepsis is being favorable [12].
PCT values, particularly in low ranges (0.5-2 ng/mL), are not very useful in identifying the most severe patients because of its little power of discrimination. However, very high values (> 10 ng/mL) suggest a significantly increased risk of sepsis and/or septic shock [13] and low values (< 0.2 ng/mL) practically rule out bacteraemia with a negative predictive value (NPV) > 98% [14] and consequently its determination will also help to make decisions in some cases. So a patient suffering from shock, very low levels of PCT (<0.2 ng/mL) confirmed 12 hours later, make a bacterial infection unlikely and require alternative diagnoses (viral infections, autoimmune conditions or other types of shock).
Recently, the role of MR-ProADM in emergency departments and critically ill patients has been studied as a marker of severity since it is more stable and its determinations more reproducible than adrenomedullin (ADM), a peptide hormone of the calcitonin family, produced by different tissues in response to physiological and pathological stress (including sepsis).
Specifically, MR-ProADM in patients older than 75 years treated in the emergency room for infection has shown to have a predictive capacity of 30-day mortality much better than lactate, PCT or other biomarkers such as suPAR or PCR. A cut-off point of MR-ProADM > 2.07 mmol/L establishes a LR (+) of post-test death 19 times greater, which may alert of the need to admit these patients even if other biomarkers are normal. This same study shows that the predictive capacity of mortality at 30 days of the combined model qSOFA ≥ 2 and MR-proADM> 2.07 mmol/L reaches an area under the curve (AUC) of 0.87, higher than the predictive capacity of both variables separately [15].
In critical patients, it is also shown how in each range of severity measured by the SOFA scale (<6, from 7-12 and ≥ 13), increasing cut-off points of MR-ProADM (1.79, 3.25 and 5.58 mmol/L, respectively) have an AUC to predict mortality of 0.75 at 28 days [16].
In a study conducted by our hospital in 33 patients with sepsis or septic shock, in which 9 patients died with a median SOFA = 9 (RIQ: 7-10.5) for a cut-off point of MR-ProADM of 8.58 mmol/L, the AUC to predict mortality in ICU was 0.99, higher than lactate (0.80), PCT (0.72) and APACHE II score (0.82). Very interesting was also the finding that amongst patients with lactate ≤ 2 mmol/L, those who died had significantly higher levels of MR-ProADM (21.14 mmol/L) than the survivors (3.6 mmol/L), warning about the possible poor evolution of patients who apparently had a good prognosis based on lactate levels [17].
UTILITY OF BIOMARKERS TO GUIDE ANTIBIOTIC TREATMENT
Several studies have shown the importance of early administration of an adequate antibiotic treatment on the reduction of mortality, particularly in critically ill patients [18]. In this regard, if the patient is in septic shock, current biomarkers do not allow us waiting to start antibiotics until they rise up to a certain threshold level because, for instance PCT can take up to 6 hours to reach abnormal plasma levels, which would unjustifiably delay the start of treatment. However, in COPD patients with respiratory exacerbation or in cases of respiratory infection in primary care, the measurement of PCT avoids the overuse of antibiotics in a significant and safe way, compared to making decisions without knowing their value [19].
On the other hand, administering unnecessary or very prolonged antibiotics courses over time might be harmful to the patient [20], so limiting them for such period as is strictly necessary is mandatory. Some studies have shown that shorten duration treatments can be as effective and safe as longer ones [21, 22], but the fear that keeping them only for a few days decreases curation rates or increases recurrences, leads to unjustifiably prolonged treatments.
In this context, the PCT has proved useful because it becomes a tool that reduces the level of physician´s uncertainty when deciding to stop antibiotics.
Monitoring PCT levels allows shorten antibiotics in a significantly and safely way, particularly in cases of respiratory infection, an average of 2.5 days, even in critical patients [19, 23]. However, it is also important to take into account the limitations of PCT to make an adequate use of it. PCT is released to blood when monocytic cells adhere and interact with parenchymal cells as expression of systemic response to infection that might not occur in localized infections such as abscesses so PCT is not useful in those cases. The onset or duration of antibiotics in other serious infections such as endocarditis cannot be guided by PCT or other biomarker because it aims to “sterilize” the affected endocardial structure and that may require a long period of antibiotic treatment even though the PCT is normalized. Apart from that, the studies that have analyzed the role of PCT in guiding antibiotic duration have not included cases of endocarditis.
CONCLUSIONS
Biomarker measurementsarenecessaryto determine SOFA score (bilirubin, creatinine, platelets) that rapidly identify patients withsepsis, especially in those admitted in ICU. Lactate and MR-proADM help identify septic patients at high risk of death, low PCT levels (<0.2 ng/mL) in cases of respiratory infection without organ dysfunction can prevent the onset of unnecessary antibiotics and its monitoring allows to shorten antimicrobial therapy without worsening the prognosis.
REFERENCES
- 1.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-10. doi: 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marshall JC, Reinhart K, Forum IS. Biomarkers of sepsis. Crit Care Med. 2009;37(7):2290-8. doi: 10.1097/CCM.0b013e3181a02afc. [DOI] [PubMed] [Google Scholar]
- 3.Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Crit Care. 2010;14(1):R15. doi: 10.1186/cc8872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA. 1994;271(9):703-7. doi: 10.1001/jama.1994.03510330081039 [DOI] [PubMed] [Google Scholar]
- 5.Fagan TJ. Letter: Nomogram for Bayes theorem. N Engl J Med. 1975;293(5):257. doi: 10.1056/NEJM197507312930513 [DOI] [PubMed] [Google Scholar]
- 6.Sotillo-Díaz JC, Bermejo-López E, García-Olivares P, Peral-Gutiérrez JA, Sancho-González M, Guerrero-Sanz JE. [Role of plasma procalcitonin in the diagnosis of ventilator-associated pneumonia: systematic review and metaanalysis]. Med Intensiva. 2014;38(6):337-46. doi: 10.1016/j.medin.2013.07.001 [DOI] [PubMed] [Google Scholar]
- 7.Jansen TC, van Bommel J, Bakker J. Blood lactate monitoring in critically ill patients: a systematic health technology assessment. Crit Care Med. 2009;37(10):2827-39. doi: 10.1097/CCM.0b013e3181a98899. [DOI] [PubMed] [Google Scholar]
- 8.Julián-Jiménez A, González Del Castillo J, Candel FJ. Usefulness and prognostic value of biomarkers in patients with community-acquired pneumonia in the emergency department. Med Clin (Barc). 2017;148(11):501-10. doi: 10.1016/j.medcli.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 9.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 2017;45(3):486-552. doi: 10.1097/CCM.0000000000002255. [DOI] [PubMed] [Google Scholar]
- 10.Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):762-74. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):775-87. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker CA, Griffith DM, Gray AJ, Datta D, Hay AW. Early lactate clearance in septic patients with elevated lactate levels admitted from the emergency department to intensive care: time to aim higher? J Crit Care. 2013;28(5):832-7. doi: 10.1016/j.jcrc.2013.02.004 [DOI] [PubMed] [Google Scholar]
- 13.Schuetz P, Christ-Crain M, Müller B. Biomarkers to improve diagnostic and prognostic accuracy in systemic infections. Curr Opin Crit Care. 2007;13(5):578-85. doi: 10.1097/MCC.0b013e3282c9ac2a [DOI] [PubMed] [Google Scholar]
- 14.Martínez-Sagasti F, Busto-González B, Requesens-Solera M, Sánchez-Cesteros C, Blesa-Malpica A, Pérez-Cecilia Carrera E, et al. [Usefulness of procalcitonin to rule out bacteraemia in critically ill patients with fever: guide in the clinical decision making process] Med Intensiva 2015;39(Supp):1-209.24951246 [Google Scholar]
- 15.Julián-Jiménez A, Yañez MC, González-Del Castillo J, Salido-Mota M, Mora-Ordoñez B, Arranz-Nieto MJ, et al. Prognostic power of biomarkers for short-term mortality in the elderly patients seen in Emergency Departments due to infections. Enferm Infecc Microbiol Clin. 2017. doi: 10.1016/j.eimc.2017.11.017 [DOI] [PubMed] [Google Scholar]
- 16.Andaluz-Ojeda D, Nguyen HB, Meunier-Beillard N, Cicuéndez R, Quenot JP, Calvo D, et al. Superior accuracy of mid-regional proadrenomedullin for mortality prediction in sepsis with varying levels of illness severity. Ann Intensive Care. 2017;7(1):15. doi: 10.1186/s13613-017-0238-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Badía-Tejero AM, Martínez-Sagasti F, Domingo-Marín S, del, Dedo-Torre MA, Requesens-Solera M, et al. Superior accuracy of mid-regional proadrenomedullin over C reactive protein,procalcitonin and lactate for ICU mortality prediction in septic patients. Intensive Care Med Exp. 2017;5(Suppl 1):37. doi: 10.1186/s40635-017-0149-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589-96. doi: 10.1097/01.CCM.0000217961.75225.E9 [DOI] [PubMed] [Google Scholar]
- 19.Schuetz P, Wirz Y, Sager R, Christ-Crain M, Stolz D, Tamm M, et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: a patient level meta-analysis. Lancet Infect Dis. 2018;18(1):95-107. doi: 10.1016/S1473-3099(17)30592-3. [DOI] [PubMed] [Google Scholar]
- 20.Garnacho-Montero J, Gutiérrez-Pizarraya A, Escoresca-Ortega A, Corcia-Palomo Y, Fernández-Delgado E, Herrera-Melero I, et al. De-escalation of empirical therapy is associated with lower mortality in patients with severe sepsis and septic shock. Intensive Care Med. 2014;40(1):32-40. doi: 10.1007/s00134-013-3077-7 [DOI] [PubMed] [Google Scholar]
- 21.Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588-98. doi: 10.1001/jama.290.19.2588 [DOI] [PubMed] [Google Scholar]
- 22.Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372(21):1996-2005. doi: 10.1056/NEJMoa1411162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matthaiou DK, Ntani G, Kontogiorgi M, Poulakou G, Armaganidis A, Dimopoulos G. An ESICM systematic review and meta-analysis of procalcitonin-guided antibiotic therapy algorithms in adult critically ill patients. Intensive Care Med. 2012;38(6):940-9. doi: 10.1007/s00134-012-2563-7. [DOI] [PubMed] [Google Scholar]


