Abstract
Objectives. To test whether indicators of despair are rising among US adults as they age toward midlife and whether this rise is concentrated among low-educated Whites and in rural areas.
Methods. We used data from the National Longitudinal Study of Adolescent to Adult Health, a nationally representative study of US adolescents in 1994. Our sample was restricted to individuals who participated in 1 or more of 5 waves (1994–2017) and self-identified as non-Hispanic White, non-Hispanic Black, or Hispanic (n = 18 446). We examined change in indicators of despair from adolescence to adulthood using multilevel regression analysis, testing for differences by race/ethnicity, education, and rurality.
Results. We found evidence of rising despair among this cohort over the past decade. This increase was not restricted to low-educated Whites or to rural areas.
Conclusions. Results suggest that generally rising despair among the young adult cohort now reaching midlife that cuts across racial/ethnic, educational, and geographic groups may presage rising midlife mortality for these subgroups in the next decade.
At the close of 2016, the National Center for Health Statistics released a report on US mortality in the previous year. For the first time since 1993, life expectancy at birth declined, and death rates across 8 of the 10 leading causes increased.1 This trend persisted, with reports for 2016 and 2017 demonstrating continuing declines.2,3 These troubling reports suggested that progress against the leading causes of death had stalled, or even reversed. Underlying these population statistics, research demonstrated that the increase in mortality was concentrated among low-educated, middle-aged non-Hispanic Whites, who, despite longstanding declines in mortality, have experienced rising mortality since the late 1990s.4,5
Although the pronounced increase in death rates among this demographic group has been established, the drivers of this increase are under debate.6,7 Initial research identified suicides, drug overdoses, and alcohol-related liver disease as the causes of death responsible for rising midlife mortality8 and labeled these causes “deaths of despair.”7 Because of the concentration of these deaths among low-educated Whites and in rural areas where economic stagnation has been widely documented, scholars attributed the rise in midlife mortality to a general context of hopelessness and self-destructive behaviors reflecting despair.9,10
The factors underlying these patterns remain unknown. However, current explanations point to labor market changes driven by globalization and technological change, leading to deteriorating job opportunities, wage stagnation, and declining rates of upward mobility for low-educated individuals.7 These economic factors undermined social support by eroding traditional family structures and religious participation, resulting in despair.11,12 Although these trends affected all racial/ethnic groups, scholars suggest that historical advantages lead to greater feelings of relative subordination among low-educated Whites compared with low-educated racial/ethnic minorities11,13 and that Blacks may be “inured to insults of the market” and insulated by strong support networks of kin and religion.7
Using data from the nationally representative National Longitudinal Study of Adolescent to Adult Health (Add Health),14 we tested whether increases in indicators of despair have been particularly acute among White, low-educated, rural members of the cohort. We examined changes in measures of despair across the early adult life course from adolescence to adulthood from 1994 to 2017. We documented racial/ethnic, educational, and geographic-specific trends in 4 indicators of despair among US adults.
METHODS
In the analyses, we used data from Add Health, a nationally representative study of adolescents in grades 7 through 12 in 1994–1995 followed into adulthood over 5 waves of data collection.15,16 Individuals were born from 1974 to 1983. We analyzed data from wave I, conducted in 1994–1995, when individuals had an average age of 15 years; wave II, conducted in 1996, when individuals had an average age of 16 years; wave III, conducted in 2001–2002, when individuals had an average age of 22 years; wave IV, conducted in 2008–2009, when individuals had an average age of 28 years; and sample 1 wave V, conducted in 2016–2017, when individuals had an average age of 37 years. These data are ideally suited to examine longitudinal change in indicators of despair, as Add Health has detailed individual-level data on respondents in the precise age range and historical period relevant for understanding current and future midlife mortality risks.
The original wave I sample of Add Health included 20 745 respondents. We first restricted our sample to 18 446 individuals interviewed at wave I who self-identified as non-Hispanic White, non-Hispanic Black, or Hispanic (hereafter White, Black, and Hispanic; Table A, available as a supplement to the online version of this article at http://www.ajph.org). We excluded Asians and other racial/ethnic groups because of small group sizes. We estimated multilevel models for change, which accommodate unbalanced data where the number of waves of data varies across individuals. Individuals contributed between 1 and 5 observations across the 5 waves; we considered individuals who did not participate in a specific wave missing at that wave. All 18 446 individuals in the analytic sample participated in wave I, 13 161 in wave II, 13 480 in wave III, 14 138 in wave IV, and 3492 in sample 1 of wave V (Table A). The wave V design involved continuous interviewing across 3 nationally representative subsamples sequentially from 2016 to 2018 and is ongoing. Our analytic sample included sample 1 of wave V, a representative subsample for whom data were released in 2017.
Response rates ranged from approximately 77% to 88% across waves; previous studies analyzed attrition for potential bias across all waves, with results showing minimal to no bias to study estimates.17,18 Results were substantively similar when we restricted the analysis to those participating in all 5 waves. Analytic sample size varied between models (13 805–18 008), depending on missing data for outcome and predictor variables included in each model.
Measures of Despair
Indicators of despair included mental health and substance use behaviors that are upstream of the causes of death associated with the observed pattern of elevated mortality among midlife adults. We measured 4 longitudinal indicators identically at all waves. We measured depressive symptoms using a count of 4 self-reported answers to frequency in the last week of feeling unable to shake off the blues, depressed, sad, and happy (reverse coded). For each feeling, respondents were able to select 1 of 4 responses: 0 “never/rarely,” 1 “sometimes,” 2 “a lot of the time,” and 3 “most/all of the time.” We summed across the 4 items, creating a score ranging from 0 to 12.19 We measured suicidal ideation as whether the individual reported contemplation of suicide in the last 12 months. We measured heavy drinking as a report of consuming more than 4 drinks in a row for women and more than 5 drinks in a row for men on at least 1 occasion in the last 12 months.20 We measured marijuana use as self-report of use in the last 30 days.
We measured other forms of drug use and mental health diagnoses differently across the waves, preventing longitudinal analyses for those measures. However, because of the current opioid epidemic and the debate on the role of despair, we examined cross-sectional measures of current drug use and lifetime mental health diagnoses at wave V. We measured prescription opioid abuse as self-report of pain killer or opioid misuse in the last 30 days and other prescription drug abuse as self-report of sedative, tranquilizer, or stimulant misuse in the last 30 days. We measured illegal drug use as self-report of cocaine, crystal meth, heroin, or other illegal drug use in the last 30 days. We assessed diagnosed depression using self-report of whether any health provider has ever told the respondent that he or she had depression. We defined diagnosed anxiety from self-report of the same question for anxiety.
Sociodemographic Variables
We measured race/ethnicity as self-reported identification as White (reference), Black, or Hispanic. We categorized educational attainment as completing a high school diploma or less (reference) or greater than high school degree on the basis of highest grade completed reported at wave V; this definition is consistent with the educational categories used when examining rising midlife mortality.7 We measured geographic areas on the basis of location of residence at wave IV and rural-urban commuting area codes, which characterize census tracts on the basis of population density, urbanization, and daily commuting from the 2000 decennial census.21,22 We created 3 categories of geographic locale by combining all metropolitan categories into 1 urban metro area category and all micropolitan commuting classifications together. The reference category was small towns and rural locales.
Analysis
We analyzed suicidal ideation, heavy drinking, and marijuana use using multilevel logistic regression, and we analyzed depressive symptoms using multilevel Poisson regression. All models included a random effect for the intercept to account for unobserved differences between individuals. For each outcome, we first determined the most appropriate age pattern by comparing unweighted nested models with linear, quadratic, and cubic age trends using a likelihood ratio test and the Akaike information criterion to assess model fit (Table B, available as a supplement to the online version of this article at http://www.ajph.org). A cubic age pattern best described the change in all indicators of despair.
For each sociodemographic group, we fit the model with and without an interaction term between a group indicator and age (linear, quadratic, and cubic). We compared marginal effects on predicted probabilities and rates to determine whether there was statistical evidence of significant differences in change in each indicator with age across groups. We present results for the best fitting models. All models controlled for sex (the age pattern of despair was not significantly different by sex) and included longitudinal sampling weights to account for Add Health’s sampling design and attrition across waves. We constructed longitudinal weights using an array of demographic variables on which the original wave I prospective cohort was distributed to reflect the national population of 7th through 12th graders (e.g., age, race/ethnicity, census region), variables used for differential probability selection (e.g., twin status, disability, race/ethnicity), and variables that reflect differential attrition over time (e.g., risk behavior, immigrant status).23
For wave V drug use and mental health diagnoses, we compared proportions across groups using the χ2 test of independence.
RESULTS
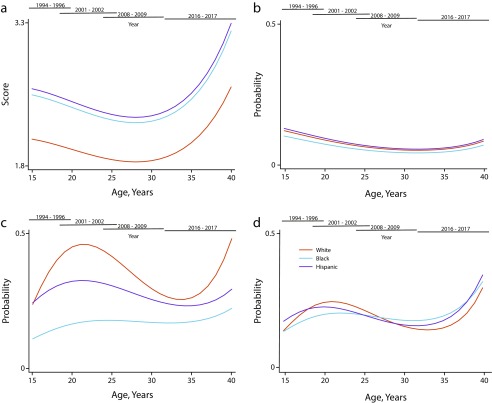
Figure 1 presents predicted levels of despair indicators by age separately for racial/ethnic groups (full results are shown in Table C, available as a supplement to the online version of this article at http://www.ajph.org). Depressive symptoms decreased with age from adolescence to the late 20s. However, depressive symptoms increased as the cohort aged into their 30s. Although this pattern was consistent across racial/ethnic groups, Blacks and Hispanics had consistently higher levels of depressive symptomology than did Whites.
FIGURE 1—
Longitudinal Measures of Despair, by Race/Ethnicity Across Age, for (a) Depressive Symptoms, (b) Suicidal Ideation, (c) Heavy Drinking, and (d) Marijuana Use: United States, 1994–2017
Note. We predicted results from multilevel logistic (suicidal ideation, marijuana use, heavy drinking) and Poisson (depressive symptoms) regression models, controlling for sex. All models include cubic age trajectories, a random intercept for individuals, and survey weights accounting for the Add Health sampling design. Year refers to the calendar year of data collection spanning particular age ranges of respondents; for example, wave IV was conducted in 2008–2009 and covers respondents aged 24–32 years. Full regression results are provided in Table C (available as a supplement to the online version of this article at http://www.ajph.org).
Starting highest in adolescence, suicidal ideation declined significantly with age similarly for Whites, Blacks, and Hispanics. Results provided marginal evidence of a recent increase in suicidal ideation as the cohort aged into their mid-30s. There was no statistically significant difference in suicidal ideation by race/ethnicity.
The age pattern of heavy drinking differed significantly across groups. The increase in heavy drinking was steepest among Whites during late adolescence and into their early 20s, declined across the late 20s and 30s, and increased again in the late 30s. The age pattern of heavy drinking was flatter for Blacks but with steady increase across this life course stage. For Hispanics heavy drinking peaked in the early 20s and then declined, with some evidence of an increase in the late 30s. The predicted probability of heavy drinking was consistently highest among Whites.
Marijuana use increased from adolescence to the early 20s, declined across the 20s and into the early 30s, and then rose rapidly into the late 30s. The age pattern varied significantly across groups, with slower increases in adolescent marijuana use among Blacks and Hispanics than among Whites and flatter trajectories of use across the 20s. However, increases in use in early adulthood were substantively similar across groups in the 30s. Although Whites had the highest predicted probability of marijuana use in their 20s, the probability of use was predicted to be higher for Blacks and Hispanics in their late 30s.
Education
Figure A (available as a supplement to the online version of this article at http://www.ajph.org) presents predicted levels of despair indicators across age separately for racial/ethnic groups categorized by educational level (full results in Table D, available as a supplement to the online version of this article at http://www.ajph.org). Low education refers to individuals with a high school degree or less, and high education refers to those with more than a high school degree.
Allowing the age pattern of depressive symptoms to vary across groups jointly improved the model fit. However, no single group’s age trajectory was significantly different from low-educated Whites. Low-educated Blacks had consistently higher levels of depressive symptoms across the age range than did all other groups. There is evidence of recent increases in depressive symptoms in the late 30s for all groups except low-educated Hispanics.
Low-educated Whites had consistently higher levels of suicidal ideation across the age range than did all other groups. However, the age pattern of consistent decline from adolescence to the early 30s, with slight increase in the late 30s, was not significantly different across groups.
The age pattern of heavy drinking and marijuana use varied across groups. However, there was no evidence that recent increases in use of either substance were isolated to low-educated Whites. Although low-educated Whites had significantly higher levels of heavy drinking in adolescence than did high-educated Whites, and high- and low-educated Blacks, high-educated Whites experienced a significantly faster increase in heavy drinking through late adolescence and early adulthood (the college years) than did low-educated Whites. Heavy drinking increased for all groups in the late 30s, although this increase was most rapid for low- and high-educated Whites and low-educated Blacks.
Low-educated Whites had significantly higher levels of marijuana use than did high-educated Whites and Blacks in adolescence. The age pattern of marijuana use differed significantly between low- and high-educated Whites, with an earlier and steeper period of decline in the 20s among high-educated Whites. There was evidence of an increase in marijuana use for all groups in the late 30s, although this increase was fastest among high-educated Whites, and slowest among low-educated Whites.
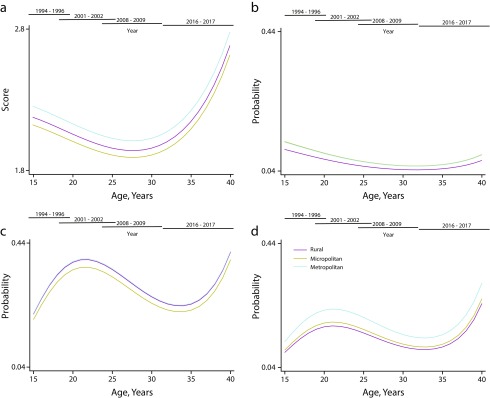
Geography
Figure 2 presents predicted levels of despair between waves separately for geographic locale (full results are shown in Table E, available as a supplement to the online version of this article at http://www.ajph.org). The level of each indicator of despair was consistently highest in metropolitan or micropolitan locales. The age pattern of despair across all indicators was not significantly different across geographic locales. These results indicate no evidence of a rural intensification of despair across the examined indicators—all geographic locales experienced similar patterns.
FIGURE 2—
Longitudinal Measures of Despair, by Geographic Locale, Across Age, for (a) Depressive Symptoms, (b) Suicidal Ideation, (c) Heavy Drinking, and (d) Marijuana Use: United States, 1994–2017
Note. We predicted results from multilevel logistic (suicidal ideation, marijuana use, heavy drinking) and Poisson (depressive symptoms) regression models, controlling for sex. All models include cubic age trajectories, a random intercept for individuals, and survey weights accounting for the Add Health sampling design. Year refers to the calendar year of data collection spanning particular age ranges of respondents; for example, wave IV was conducted in 2008–2009 and covers respondents aged 24–32. Full regression results are provided in Table E (available as a supplement to the online version of this article at http://www.ajph.org).
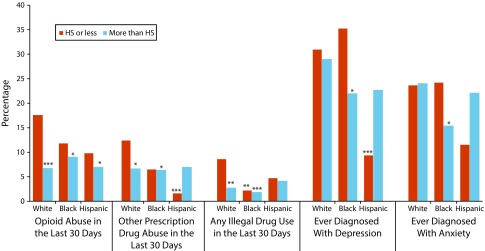
Current Drug Use and Despair
Figure 3 presents the weighted cross-sectional prevalence of drug use and mental health at wave V (2016–2017) by race/ethnicity and educational group. Of low-educated Whites, 17.5% reported opioid abuse in the last 30 days. Although low-educated Whites had significantly higher opioid abuse than did high-educated White, Black, and Hispanic respondents, their prevalence of opioid abuse was statistically similar to that of low-educated Blacks and Hispanics. Low-educated Whites also had significantly higher levels of other prescription drug abuse than did more educated Whites and Blacks and low-educated Hispanics, and significantly higher levels of illegal drug use than did high-educated Whites and all Blacks.
FIGURE 3—
Cross-Sectional Weighted Prevalence of Despair by Race/Ethnicity and Education: United States, 2016–2017
Note. HS = high school. The figure shows results for wave V of the study. The average age was 37 years. Non-Hispanic White with high school or less education was the reference category. We conducted a χ2 test of independence to compare proportions in each group to the reference category. *P < .05; **P < .01; ***P < .001.
Low-educated Blacks reported the highest levels of depression and anxiety diagnoses at wave V: 35% and 24%, respectively. Low-educated Whites experienced higher levels of diagnosed depression than did high-educated Blacks and low-educated Hispanics, as well as higher levels of diagnosed anxiety compared with high-educated Blacks. We also tested the weighted cross-sectional prevalence of drug use and mental health at wave V by geographic locale (Figure B, available as a supplement to the online version of this article at http://www.ajph.org). Levels of current opioid abuse and illegal drug use were similar across geographic locales. Levels of other prescription drug abuse were significantly higher in urban areas than in rural areas. There were no statistically significant differences in lifetime depression or anxiety diagnoses by geographic locale.
DISCUSSION
Using nationally representative longitudinal data, we examined age patterns of despair indicators from adolescence through the late 30s, covering the period 1994–2017 for a cohort of individuals born between 1974 and 1983. We found that suicidal ideation, depressive symptoms, marijuana use, and heavy drinking increased as the cohort aged into their late 30s. We found no evidence that increases in despair were limited to low-educated Whites. Furthermore, levels of despair increased across the 30s in all geographic locales. We examined current drug use and lifetime mental health diagnoses, and we found no evidence that either were consistently highest among low-educated Whites or in rural locales.
The cohort, age range, and period we examined were particularly relevant for better understanding recent trends in despair and their potential role in explaining rising midlife mortality. The Add Health cohort is nearing the age range of elevated midlife mortality (45–54 years) and is beyond the age range of highest opioid mortality risk from opioids (25–34 years).24 Importantly, increases in midlife mortality observed in other studies have been driven by increases among low-educated Whites,4 primarily outside urban areas.9 However, the specific causes of death underlying this trend are under debate. Case and Deaton pointed to rising mortality from the deaths of despair resulting from poisonings, suicide, and alcohol-related conditions.4,7 However, Masters et al. found that the factors underlying trends in suicide, chronic liver disease, other causes of death, and drug overdose are distinct and suggest that the rise in midlife mortality may be owing entirely to the opioid epidemic.6,25
Despite a lack of scientific consensus regarding the cause of elevated midlife mortality among Whites, the image of the forgotten low-educated, White, rural American has captured the public’s attention.11,26 This trope has been used to explain the opioid crisis, the results of the 2016 presidential election, and the rise of the political far right.27–29 These explanations assume that this specific demographic group has experienced a recent and intense increase in despair, distinct from the general population. There is some evidence that opioid disorders and declines in mental health are concentrated among low socioeconomic status Whites.30,31
By contrast to this narrative, our findings demonstrated a generalized increase in multiple indicators of despair among all White, Black, and Hispanic adults in their 30s. Our findings are consistent with recent evidence that opioid-related mortality increased among Whites and Blacks since 2010,32 and midlife mortality in general increased across racial/ethnic groups.33 This pattern of rising despair is not isolated to rural America but is heterogeneous across geographic locales, consistent with recent research on geographic heterogeneity in drug and suicide mortality.34,35 Our results indicate that patterns of despair potentially underlying increased midlife mortality are not restricted to low-educated Whites and caution against an overemphasis on this single demographic group.36,37 If rising despair was indeed responsible for the increases in mortality among earlier cohorts of low-educated Whites, then the generalized increases in despair we documented among a younger and more recent cohort could presage increases in midlife mortality in the coming decade for all population subgroups. Continued monitoring of the mental health, substance use and abuse, and health and mortality trends among younger cohorts as they move into midlife is clearly warranted.
Alternatively, the generalized increases in despair we documented among the younger and more recent Add Health cohort may reflect age or cohort effects. It is possible that patterns of despair will diverge across subgroups as the cohort ages, particularly as advantages accumulate differentially by race, education, and geographic location. The Add Health cohort is distinct from earlier cohorts reflected in the rising midlife mortality of low-educated Whites,4 with more highly educated parents, different perceptions of racial and ethnic diversity, and labor market entry following globalization. Nonetheless, the generalized increases in despair indicators we documented for the Add Health cohort are worrisome for forthcoming midlife mortality trends and justify continued close monitoring.
A number of important historical events occurred during Add Health data collection. For example, the attack on the World Trade Center on September 11, 2001, occurred during wave III collection, the Great Recession and the election of Barack Obama characterized the period of wave IV collection, and wave V data collection spanned the 2016 presidential election and the legalization of recreational marijuana for one fifth of the US population. We were unable to disentangle the potential role of period effects on the observed age patterns. We focused on 1 cohort of young adults as they entered midlife. It is possible that the pattern of rising despair is common across cohorts during this life stage. However, we cannot compare the Add Health age trends for these despair outcomes with the similar age trends from earlier periods because there are no other cohort data of this kind.
Limitations
Our study had potential limitations. We measured despair using several indicators of mental and emotional health and substance use. These indicators do not completely capture all domains of despair; for example, we were unable to account for economic anxiety, reports of physical pain, or hopelessness. We did not examine mortality because of its rarity in the Add Health sample of adults in their 30s. Nevertheless, the outcomes examined are emotional and behavioral manifestations of despair.
Public Health Implications
Recently rising midlife mortality in the 21st century was initially reported as isolated among Whites with a high school diploma or less and attributable to drug poisonings, alcohol abuse, and suicide.4,7 One explanation for this trend contends that as labor market prospects and social cohesion deteriorated for low-educated Whites, this cumulative disadvantage resulted in rising despair, depression, suicidality, and substance use.7,9 It follows that if rising despair was responsible for rising death rates among this group, and death rates are not rising among other subgroups, rising despair should be particularly acute among low-educated Whites. Almost all subsequent research on diseases and deaths of despair is on the basis of White samples without testing whether they are high or rising in other groups.5,6,9,25,30 Thus, rising despair is assumed to be primarily a White, low educated, rural phenomena—with direct implications that public policy need only address this segment of the population. But recent research found increases in mortality attributable to despair-related causes across all racial/ethnic groups.33
Our results show that despair indicators have indeed been rising among US young adults now entering midlife across the past decade and that such increases are not concentrated among White, low-educated, rural adults. By contrast, American young adults of all demographic groups exhibited increased despair over the past decade. Public health efforts to reduce despair targeted only to low-educated Whites, or in rural areas, would be misdirected. Instead, efforts to reduce depression, suicidality, and substance use should target the general population of US young adults who are experiencing rising despair as they enter midlife.
ACKNOWLEDGMENTS
Partial support for this research was provided by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grants F32 HD084117, P2C HD050924, P01 HD31921). We used data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill and funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant P01-HD31921), with cooperative funding from 23 other federal agencies and foundations.
The authors would like to acknowledge the helpful comments of 3 anonymous reviewers, Ryan Masters, and Shannon Monnat.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
This research was approved by the University of North Carolina, Chapel Hill institutional review board.
Footnotes
See also Carliner, p. 658.
REFERENCES
- 1.Xu J, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief. 2016;(267):1–8. [PubMed] [Google Scholar]
- 2.Kochanek KD, Murphy SL, Xu J, Arias E. Mortality in the United States, 2016. NCHS Data Brief. 2017;(293):1–8. [PubMed] [Google Scholar]
- 3.Murphy S, Xu J, Kochanek KD, Arias E. Mortality in the United States. 2017;2018(328):1–8. [PubMed] [Google Scholar]
- 4.Case A, Deaton A. Rising morbidity and mortality in midlife among White non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho JY. The contribution of drug overdose to educational gradients in life expectancy in the United States, 1992–2011. Demography. 2017;54(3):1175–1202. doi: 10.1007/s13524-017-0565-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masters RK, Tilstra AM, Simon DH. Explaining recent mortality trends among younger and middle-aged White Americans. Int J Epidemiol. 2018;47(1):81–88. doi: 10.1093/ije/dyx127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Pap Econ Act. 2017;2017:397–476. doi: 10.1353/eca.2017.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shiels MS, Chernyavskiy P, Anderson WF et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet. 2017;389(10073):1043–1054. doi: 10.1016/S0140-6736(17)30187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein EM, Gennuso KP, Ugboaja DC, Remington PL. The epidemic of despair among White Americans: trends in the leading causes of premature death, 1999–2015. Am J Public Health. 2017;107(10):1541–1547. doi: 10.2105/AJPH.2017.303941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erwin PC. Despair in the American heartland? A focus on rural health. Am J Public Health. 2017;107(10):1533–1534. doi: 10.2105/AJPH.2017.304029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cherlin AJ. Psychological health and socioeconomic status among non-Hispanic Whites. Proc Natl Acad Sci U S A. 2018;115(28):7176–7178. doi: 10.1073/pnas.1808753115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wuthnow R. The Left Behind: Decline and Rage in Rural America. Princeton, NJ: Princeton University Press; 2018. [Google Scholar]
- 13.Glei DA, Goldman N, Weinstein M. Perception has its own reality: subjective versus objective measures of economic distress. Popul Dev Rev. 2018;44(4):695–722. doi: 10.1111/padr.12183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris KM. An integrative approach to health. Demography. 2010;47(1):1–22. doi: 10.1353/dem.0.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris KM, Halpern CT, Hussey JM et al. Social, behavioral, and genetic linkages from adolescence into adulthood. Am J Public Health. 2013;103(suppl 1):S25–S32. doi: 10.2105/AJPH.2012.301181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris KM. The add health study: design and accomplishments. 2013. Available at: https://www.cpc.unc.edu/projects/addhealth/documentation/guides/DesignPaperWIIV.pdf. Accessed January 4, 2019.
- 17.Chantala K, Kalsbeek W, Andraca E. Nonresponse in Wave III of the Add Health Study. Chapel Hill; NC: Carolina Population Center; 2005. [Google Scholar]
- 18.Brownstein N, Kalsbeek W, Tabor JW, Entzel PP, Daza E, Harris KM. Non-Response in Wave IV of the National Longitudinal Study of Adolescent Health. Chapel Hill; NC: Carolina Population Center; 2011. [Google Scholar]
- 19.Perreira K, Deeb-Sossa N, Harris K, Bollen K. What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Soc Forces. 2005;83(4):1567–1601. [Google Scholar]
- 20.US Department of Health and Human Services. US Department of Agriculture; US Dietary Guidelines Advisory Committee. Dietary Guidelines for Americans 2015–2020. New York: Skyhorse; 2015. [Google Scholar]
- 21.Morrill R, Cromartie J, Hart G. Metropolitan, urban, and rural commuting areas: toward a better depiction of the United States settlement system. Urban Geogr. 1999;20(8):727–748. [Google Scholar]
- 22.US Department of Agriculture Economic Research Service. Rural–urban commuting area codes. 2016. Available at: http://www.ers.usda.gov/data-products. Accessed January 4, 2019.
- 23.Chen P, Chantala K. Guidelines for Analyzing Add Health Data. Chapel Hill; NC: Carolina Population Center; 2014. [Google Scholar]
- 24.Gomes T, Tadrous M, Mamdani M, Paterson JM, Juurlink DN. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1(2):e180217. doi: 10.1001/jamanetworkopen.2018.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Masters RK, Tilstra AM, Simon DH. Mortality from suicide, chronic liver disease, and drug poisonings among middle-aged U.S. White men and women, 1980–2013. Biodemogr Soc Biol. 2017;63(1):31–37. doi: 10.1080/19485565.2016.1248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vance J. Hillbilly Elegy—A Memoir of a Family and Culture in Crisis. New York: Harper; 2016. [Google Scholar]
- 27.Hochschild AR. The ecstatic edge of politics: sociology and Donald Trump. Contemp Sociol A J Rev. 2016;45(6):683–689. [Google Scholar]
- 28.Monnat SM, Brown DL. More than a rural revolt: landscapes of despair and the 2016 presidential election. J Rural Stud. 2017;55:227–236. doi: 10.1016/j.jrurstud.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morgan SL, Lee J. Trump voters and the White working class. Sociol Sci. 2018;5:234–245. [Google Scholar]
- 30.Goldman N, Glei DA, Weinstein M. Declining mental health among disadvantaged Americans. Proc Natl Acad Sci U S A. 2018;115(28):7290–7295. doi: 10.1073/pnas.1722023115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314(14):1468–1478. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- 32.Alexander MK, Kiang MV, Barbieri M. Trends in Black and White opioid mortality in the United States, 1979–2015. Epidemiology. 2018;29(5):707–715. doi: 10.1097/EDE.0000000000000858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woolf SH, Chapman DA, Buchanich JM, Bobby KK, Zimmerman EB, Blackburn SM. Changes in midlife death rates across racial and ethnic groups in the United States: systematic analysis of vital statistics. BMJ. 2018;362:k3096. doi: 10.1136/bmj.k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rigg KK, Monnat SM, Chavez MN. Opioid-related mortality in rural America: geographic heterogeneity and intervention strategies. Int J Drug Policy. 2018;57:119–129. doi: 10.1016/j.drugpo.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 35.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW et al. Trends and patterns of geographic variation in mortality from substance use disorders and intentional injuries among US counties, 1980–2014. JAMA. 2018;319(10):1013–1023. doi: 10.1001/jama.2018.0900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diez Roux AV. Despair as a cause of death: more complex than it first appears. Am J Public Health. 2017;107(10):1566–1567. doi: 10.2105/AJPH.2017.304041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muennig PA, Reynolds M, Fink DS, Zafari Z, Geronimus AT. America’s declining well-being, health, and life expectancy: not just a White problem. Am J Public Health. 2018;108(12):1626–1631. doi: 10.2105/AJPH.2018.304585. [DOI] [PMC free article] [PubMed] [Google Scholar]