Abstract
Despite a growing awareness about the importance of gender equity and the rising number of women in medicine, women remain persistently underrepresented in pain medicine and anesthesiology. Pain medicine ranks among the bottom quartile of medical specialties in terms of female applicants, female trainees, and proportion of female practitioners. Female pain medicine physicians are also notably disadvantaged compared with their male colleagues in most objective metrics of gender equity, which include financial compensation, career advancement, public recognition, and leadership positions. Increased gender diversity among pain medicine physicians is vital to fostering excellence in pain research, education, and clinical care, as well as creating a high quality work environment. Pain medicine stands at a crossroads as a specialty, which must examine reasons for the current gender gap in our profession and consider a call to action to address this important issue.
The Gender Gap in Pain Medicine
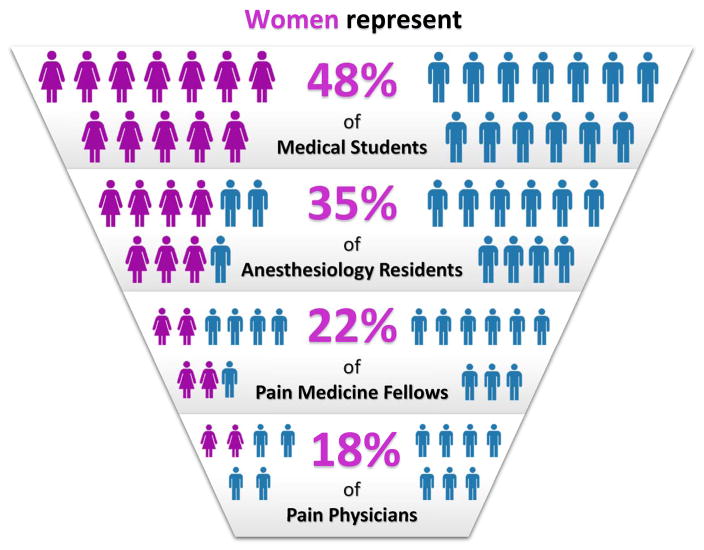
The medical profession, which identified a gender gap in professional development decades ago, has had piecemeal success in achieving parity between women and men. Female representation among medical students has grown from fewer than than 10% in 1965 to nearly 50% in recent years, and women now constitute approximately one-third of the total American physician workforce.1,2 Despite these gains, women make up a much smaller fraction of certain specialties, including in anesthesiology in general and pain medicine in particular (Fig. 1). Although 1 in 10 US physicians is an anesthesiologist,2 only a quarter (25%) of anesthesiologists and just 18% of pain management physicians are women.3 These numbers are unlikely to rise soon, with women representing just 35% of current anesthesiology residents and 22% of pain medicine fellows (Fig. 2).2,4 In fact, pain medicine ranks in the bottom quartile of medical specialties for women, only slightly above the stereotypically male-dominated training programs of orthopedic surgery (14%) and neurosurgery (17%). Meanwhile, other surgical specialties attract and retain greater numbers of women, including colorectal surgery (42%), general surgery (37%), and urology (26%) (Fig. 3).
Figure 1. Proportion of women at various stages of pain medicine training.
Data from the Accreditation Council for Graduate Medical Education (ACGME) Data Resource Book and the Association of American Medical Colleges (AAMC) Physician Specialty Data Book.3,4
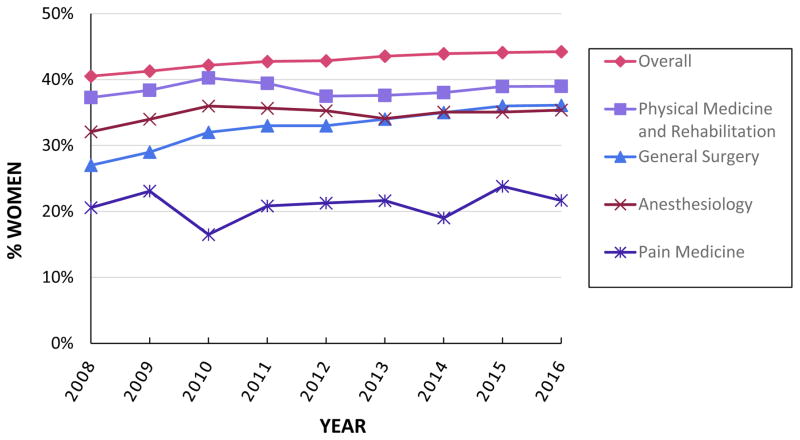
Figure 2. Percentage of Female Trainees in Selected Medical Subspecialties and Across All Specialties, 2008–2016.
Data from the ACGME Data Resource Book.4
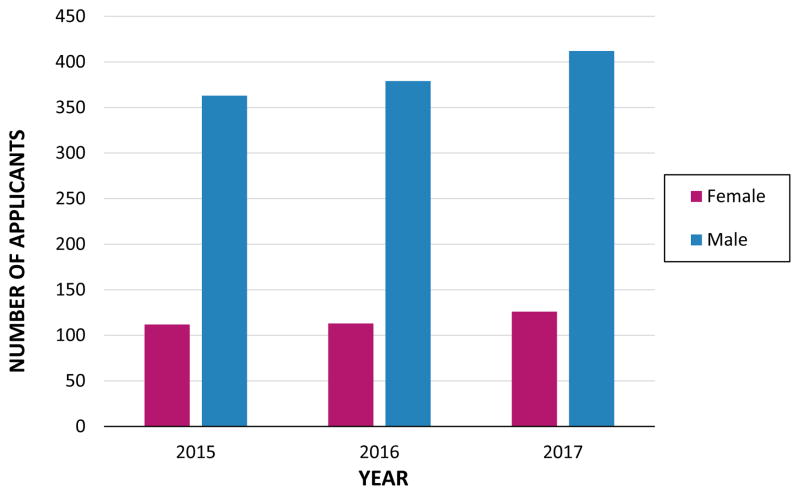
Figure 3. Pain Medicine Applicants Gender.
Data from AAMC Electronic Residency Application Services (ERAS) Statistics.33
These numbers reveal a persistent and sobering gender gap in our profession, one that begins at the early training stages and only widens as women progress in their professional careers. Women represent 33% of full-time physician faculty in anesthesiology departments at US medical schools, but only 18% of physician full professors, and just 11 out of the 106 anesthesiology department chairs nationwide are women.1 The governing boards of the premier organizations in our profession similarly lack female representation, including the American Board of Anesthesiology (4 women out of 13),5 the American Society of Anesthesiologists (3 out of 12),6 the International Anesthesia Research Society (3 out of 12),7 the American Society of Regional Anesthesia and Pain Medicine (ASRA) (2 out of 12),8 and the American Academy of Pain Medicine (1 out of 18).9
The gender disparities go beyond simple underrepresentation. A recent analysis of Medicare claims data found that female anesthesiologists receive 32.3% less in total Medicare payments than male anesthesiologists, while female pain management and interventional pain physicians received 43.5% and 32.9% less than their male counterparts, respectively.11 While various reasons have been proposed to explain these differences (eg, female physicians tend to work fewer hours, care for fewer patients, and treat patients at a lower intensity of care),10,11 the very fact that such disparities exist is both relevant and concerning.
The Benefits of Gender Diversity
As a profession that addresses complex problems in a wide range of patients, medicine can reap numerous potential benefits from improved gender diversity. Most studies have identified few or no gender differences in cognitive ability, although men on average score higher on some tests of mechanical reasoning, spatial, and mathematical abilities, while women on average score higher on tests of reading comprehension, writing, and social skills.12–14 Other studies have observed that women tend to prefer working with people and show stronger artistic, social, and conventional (organizational) interests, while men tend to prefer working with things and demonstrate stronger realistic (practical/mechanical) and investigative interests.15 Such findings suggest that members of both genders can provide important contributions to group work. Studies of group dynamics have found that more diverse groups perform better on problem-solving tasks and that gender-diverse scientific working groups produce more highly-cited publications.16,17
Women may therefore possess different skill sets and professional attributes as physicians that can complement those of men to improve overall patient care. Indeed, various studies have observed that female physicians are more likely to follow evidence-based guidelines,19 provide preventive health services,20 spend more time with patients per consultation,21 and provide more patient-centered care.22 In addition, patients of female primary care physicians have been found to have fewer hospitalizations and emergency room visits and receive more specialist referrals, even after adjusting for other provider and patient factors.23 Among Medicare patients who do get hospitalized, those under the care of female hospitalists have been found to have significantly lower mortality and readmission rates.24
There is scant research evaluating the role of physician gender on pain-related outcomes, but the relationship is likely subtle and complex. Different studies have found no significant effect of physician gender on adherence to guidelines for the management of musculoskeletal pain,25 and that female physicians prescribe lower doses of hydrocodone for chronic back pain in primary care settings,26 but are more likely to provide opioids in the emergency department.27 Other studies have suggested a more nuanced view, in which physician gender modulates how the physician’s perception of patient pain, the presence of objective pathology, and patient pain behaviors can influence treatment decisions.28,29 Patient gender may also play a significant role in how physician gender affects physician-patient interactions and medical care.22,30,31
This last point is crucial to understanding the case for more women in pain medicine. Historically, differences between men and women were not often studied in pain research until the 1990s, when several key publications noted the importance of considering pain could be influenced by sex (the biological and physiological characteristics that define men and women) and gender (the socially-constructed roles, behaviors, activities and attributes ascribed to men and women).32 Despite this awareness, women still experience minimization of pain symptoms, more frequent misdiagnosis of pain, and disparities in pain treatment options compared to men.33–35 Recognizing the importance of sex-specific research, the National Institutes of Health (NIH) has mandated the inclusion of women and minorities in clinical research.36 Moreover, it has acknowledged the bipartite problem of gender in biomedical research—women are underrepresented both as researchers and as research participants—and has developed programs supporting female researchers and women’s health, respectively.36
Finally, improving the diversity of the pain profession to reflect the diversity of the patients we serve can benefit both physicians and patients. Some women may find it easier to communicate with female physicians, particularly for gender-specific pain complaints. Others may have personal or cultural reasons to prefer female physicians. Given the clear importance of the physician-patient relationship in pain medicine and the broad range of human experience, patients should have the opportunity to receive care from a diverse pool of highly-qualified professionals.
Why Aren’t There More Women in Pain Medicine?
There are a number of possible reasons that could explain why women do not tend to pursue careers in pain medicine. The need to take additional time for fellowship training after residency may place undue personal, professional, or financial burdens on women. However, data from the Accreditation Council for Graduate Medical Education (ACGME) show that women train in all other ACGME-accredited anesthesiology fellowships in higher proportions than in pain medicine (22%): cardiothoracic anesthesiology (30%), critical care (27%), regional anesthesiology (40%), obstetric anesthesiology (59%), and pediatric anesthesiology (53%).4 The small number of fellows likely follows directly from the small number of applicants (Fig. 3). In 2016, female applicants to pain medicine were the minority (23%), in contrast to other fellowships in which women comprised the majority, such as pediatric anesthesiology (57%) and hospice and palliative medicine (63%).37
Another commonly cited reason for the underrepresentation of women in medicine is “work-life balance,” insinuating that personal and professional fulfillment are somehow mutually exclusive and that only women find them to be important. Admittedly, among early-career physician-scientists with children, women spend an average of 8.5 more hours per week on domestic activities and are more likely to take time off during disruptions of usual child care arrangements.38 Many careers in pain medicine do entail long hours, mentally and physically taxing work, and challenging interactions with the healthcare system, but the same can be said for many other medical specialties that do not have such a profound gender gap. If anything, regular pain clinic hours, limited/no-call options, and relatively few emergencies should make pain management more appealing to anyone who might prefer predictability in scheduling and flexibility in managing personal responsibilities.
One significant distinction between pain medicine and other anesthesiology subspecialties is increased exposure to radiation. Medical specialties with similar exposures, such as interventional radiology and interventional cardiology, also notably lack female representation. Perceived risks to fertility and future family may deter women from entering these professions, although this explanation is largely speculative. Decades of occupational research support the ability to minimize radiation exposure through the use of appropriate protective equipment and safety practices, such that risks to fertility and fetal development are negligible.39,40 Nevertheless, misconceptions about occupational radiation exposure persist, and they may make women less likely to consider careers in interventional specialties.
The greatest potential deterrents to female participation may actually be the culture and historical trends of pain medicine. Potential applicants may perceive the field as unfriendly to women, making the underrepresentation of women in pain medicine a self-perpetuating problem. Without female role models, female medical students and residents who might otherwise have been interested in pain medicine may pursue other subspecialties with a greater proportion of established female physicians, such as obstetric or pediatric anesthesiology. Obstetric and pediatric anesthesiology may also be more appealing to female anesthesiologists simply by association with the more female-oriented specialties of obstetrics/gynecology or pediatrics, respectively. Pain medicine physicians, by contrast, tend to share patients with male-dominated specialties (eg, orthopedic surgery and neurosurgery), making it difficult to identify female role models even in related specialties.
Unfortunately, none of the reasons presented above can provide adequate rationale for the persistent, longstanding gender gap in pain medicine—if there can even be an “adequate rationale” for such an egregious problem. The sad truth is that pain medicine as a specialty has failed to prioritize and nurture the role of women in the profession, which is less likely a reflection of overt discrimination, and more likely the vexing product of inattention and complacency. We ask the readers to reflect back on their own careers and consider their individual training institutions, employers, practices, and professional societies. At each level, what specific actions and programs have been implemented to promote and encourage women? Have their female colleagues been offered the same leadership positions, speaking invitations, and research opportunities as men? Do women receive the same high-quality referrals, marketing and publicity campaigns, and award nominations? Although these aspects have rarely been formally studied in our profession, perhaps we need to start keeping better track of what types of professional programs promote women in pain medicine, and how many women become Pain Division chairs, conference keynote speakers, professional society leaders, and major award recipients.
Promoting Women in Pain Medicine
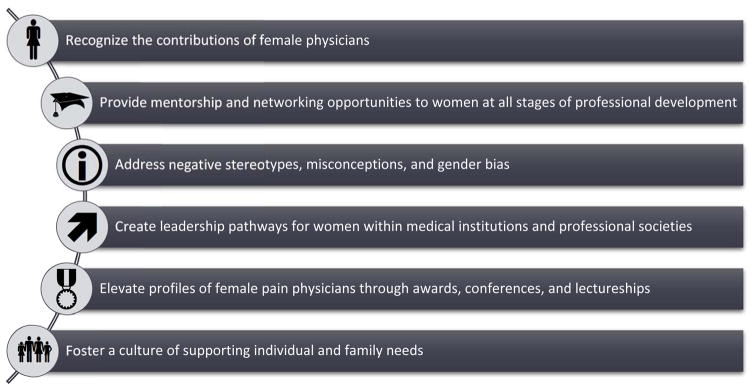
The pervasive, systematic problem of the gender gap in pain medicine must be addressed from a systems-level approach (Fig. 4). First, all pain medicine physicians—male and female—must recognize that women are critically underrepresented in pain medicine and that promoting the participation of women is vital to the continued growth and success of our profession. Individuals, institutions, and organizations must acknowledge the need for diversity and inclusion in pain medicine to create better cultures within our clinical, research, and educational environments. To do so, we need more formal, specific research into the factors that have perpetuated the gender gap in pain medicine, as well as particular interventions that can help close the gap.
Figure 4.
Strategies to promote women in pain medicine.
Second, the leaders of our profession must actively work to identify, recruit, and support women in the field, from medical trainees to clinical faculty. Residency and fellowship program directors, division chiefs, and department chairs need to examine the transitions from medical school to fellowship training and specifically identify barriers that impede the pathway for women. We must consider whether concrete actions can be taken to encourage more female applicants into the specialty at each point in the application process, including submission to the Electronic Residency Application Service (ERAS), program selection of interview candidates, interview evaluations, post-interview communication, match list selection, and post-match evaluations. During and after fellowship, we must provide early-career female physicians with appropriate guidance and mentorship to build successful careers in pain medicine.
Changes can begin at the individual level and rise throughout the specialty, and we must recognize that both men and women have important, but unique responsibilities in promoting gender diversity in our profession. Current female pain medicine physicians can make a concerted effort to reach out to trainees and junior faculty, promote pain medicine as a profession, and serve as role models. As an underrepresented minority in pain medicine, women must support each other through advice, advocacy, and action in order to advance women in the field. Established male pain medicine physicians at every level of training and leadership can serve as advocates for their female colleagues, provide mentorship to female trainees, and facilitate networking and career opportunities for female physicians. At an organizational level, institutions must develop defined pathways of career advancement that attend to the specific strengths and interests of female physicians. Professional societies need to consider the talents and contributions of women when recruiting and selecting board members, journal editors, conference speakers, and award recipients. Such increased visibility and encouragement for women in our profession sends a clear message to potential applicants that we welcome and support female physicians.
Finally, our profession must create and demonstrate ways in which pain medicine can be an appealing career choice, both for female physicians and male physicians who support women. We must counter negative stereotypes and misconceptions about the practice of pain medicine, showing potential applicants that pain medicine is more than just opioid management and radiation exposure, and that providing care to pain patients can be both intellectually and emotionally rewarding. Pain medicine offers a wide array of exciting opportunities, from academic pain research, to community-based private practice, to analgesic drug and device development, to patient advocacy and political engagement. These diverse options can offer exceptional flexibility for early-career physicians whose family responsibilities may make a career in medicine challenging. Fellowship training programs, anesthesiology departments, and medical institutions can demonstrate support for physician families—benefiting both men and women—by promoting generous parental leave policies, offering options for primary and back-up child care, and allowing flexible scheduling where possible. Consequently, by creating a paradigm of pain medicine as a profession that embraces gender diversity and the needs of families, we can demonstrate to our patients that we understand and care about individuals holistically, and that this understanding can translate into more compassionate, comprehensive care.
Conclusions
We recognize that the topic of promoting gender diversity may be particularly sensitive, fraught with potential pitfalls of political correctness, insinuations of gender superiority, and the temptation to produce buzz-worthy media. However, such topics detract from the simpler, less controversial underlying truths: 1) pain medicine lacks female physicians, 2) women provide important contributions to the field of pain medicine, and 3) concrete steps exist to promote and encourage female pain medicine physicians. In order for the field of pain medicine to remain relevant, we need to cultivate a dynamic, innovative workforce that generates the best possible ideas and provides the best possible care to our patients—and to do that, our profession needs women.
Acknowledgments
Funding:
The authors have no sources of funding to declare for this manuscript.
We wish to thank the American Society for Regional Anesthesiology and Pain Medicine (ASRA) and Elizabeth Smith at ASRA Membership Services for providing membership and historical board member data.
Footnotes
Conflicts of Interest:
The authors declare no conflicts of interest.
References
- 1.Association of American Medical Colleges. [Accessed November 2, 2017];The State of Women in Academic Medicine: The Pipeline and Pathways to Leadership, 2015–2016. https://www.aamc.org/members/gwims/statistics/. Published 2016.
- 2.The Henry J. Kaiser Family Foundation. Providers & Service Use. Kaiser Family Foundation; [Accessed November 8, 2017]. https://www.kff.org/state-category/providers-service-use/. Published 2017. [Google Scholar]
- 3.Association of American Medical Colleges. 2016 Physician Specialty Data Report. Association of American Medical Colleges; [Accessed November 8, 2017]. https://www.aamc.org/data/workforce/reports/457712/2016-specialty-databook.html. Published 2016. [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. ACGME Data Resource Book, Academic Year 2016–2017. Chicago, IL: 2017. [Accessed November 2, 2017]. http://www.acgme.org/About-Us/Publications-and-Resources/Graduate-Medical-Education-Data-Resource-Book. [Google Scholar]
- 5.Board of Directors. [Accessed November 2, 2017];The American Board of Anesthesiology. http://www.theaba.org/about/Board-of-Directors. Published 2017.
- 6.ASA Officers American Society of Anesthesiologists. [Accessed November 2, 2017]; http://www.asahq.org/about-asa/governance-and-committees/asa-officers. Published 2017.
- 7.Board of Trustees. International Anesthesia Research Society. [Accessed November 2, 2017]; http://www.iars.org/about/bot/. Published 2017.
- 8.About - American Society of Regional Anesthesia and Pain Medicine. [Accessed November 2, 2017];American Society of Regional Anesthesia and Pain Medicine. https://www.asra.com/about. Published 2017.
- 9.Board of Directors. [Accessed November 2, 2017];The American Academy of Pain Medicine. http://www.painmed.org/membercenter/board-of-directors/. Published 2017.
- 10.Baird M, Daugherty L, Kumar KB, Arifkhanova A. Regional and gender differences and trends in the anesthesiologist workforce. Anesthesiology. 2015;123:997–1012. doi: 10.1097/ALN.0000000000000834. [DOI] [PubMed] [Google Scholar]
- 11.Mahr MA, Hayes SN, Shanafelt TD, Sloan JA, Erie JC. Gender Differences in Physician Service Provision Using Medicare Claims Data. Mayo Clin Proc. 2017;92:870–880. doi: 10.1016/j.mayocp.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 12.Lindberg SM, Hyde JS, Petersen JL, Linn MC. New trends in gender and mathematics performance: A meta-analysis. Psychol Bull. 2010;136:1123–1135. doi: 10.1037/a0021276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hyde JS. The Gender Similarities Hypothesis. Am Psychol. 2005;60:581–592. doi: 10.1037/0003-066X.60.6.581. [DOI] [PubMed] [Google Scholar]
- 14.Zell E, Krizan Z, Teeter SR. Evaluating gender similarities and differences using metasynthesis. Am Psychol. 2015;70:10–20. doi: 10.1037/a0038208. [DOI] [PubMed] [Google Scholar]
- 15.Su R, Rounds J, Armstrong PI. Men and things, women and people: A meta-analysis of sex differences in interests. Psychol Bull. 2009;135:859–884. doi: 10.1037/a0017364. [DOI] [PubMed] [Google Scholar]
- 16.Hong L, Page SE. Groups of diverse problem solvers can outperform groups of high-ability problem solvers. Proc Natl Acad Sci U S A. 2004;101:16385–16389. doi: 10.1073/pnas.0403723101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campbell LG, Mehtani S, Dozier ME, Rinehart J. Gender-heterogeneous working groups produce higher quality science. PLoS One. 2013;8:e79147. doi: 10.1371/journal.pone.0079147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woolley AW, Chabris CF, Pentland A, Hashmi N, Malone TW. Evidence for a collective intelligence factor in the performance of human groups. Science. 2010;330:686–688. doi: 10.1126/science.1193147. [DOI] [PubMed] [Google Scholar]
- 19.Baumhäkel M, Müller U, Böhm M. Influence of gender of physicians and patients on guideline-recommended treatment of chronic heart failure in a cross-sectional study. Eur J Heart Fail. 2009;11:299–303.1. doi: 10.1093/eurjhf/hfn041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramirez AG, Wildes KA, Nápoles-Springer A, Pérez-Stable E, Talavera G, Rios E. Physician gender differences in general and cancer-specific prevention attitudes and practices. J Cancer Educ. 2009;24:85–93. doi: 10.1080/08858190802664396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jefferson L, Bloor K, Birks Y, Hewitt C, Bland M. Effect of physicians’ gender on communication and consultation length: a systematic review and meta-analysis. J Health Serv Res Policy. 2013;18:242–248. doi: 10.1177/1355819613486465. [DOI] [PubMed] [Google Scholar]
- 22.Bertakis KD, Azari R. Patient-centered care: the influence of patient and resident physician gender and gender concordance in primary care. J Womens Health (Larchmt) 2012;21:326–333. doi: 10.1089/jwh.2011.2903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dahrouge S, Seale E, Hogg W, et al. A comprehensive assessment of family physician gender and quality of care. Med Care. 2016;54:277–286. doi: 10.1097/MLR.0000000000000480. [DOI] [PubMed] [Google Scholar]
- 24.Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177:206–213. doi: 10.1001/jamainternmed.2016.7875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maserejian NN, Fischer MA, Trachtenberg FL, et al. Variations among primary care physicians in exercise advice, imaging, and analgesics for musculoskeletal pain: results from a factorial experiment. Arthritis Care Res (Hoboken) 2014;66:147–156. doi: 10.1002/acr.22143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weisse CS, Sorum PC, Dominguez RE. The influence of gender and race on physicians’ pain management decisions. J Pain. 2003;4:505–510. doi: 10.1016/j.jpain.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Safdar B, Heins A, Homel P, et al. Impact of physician and patient gender on pain management in the emergency department—A multicenter study. Pain Med. 2009;10:364–372. doi: 10.1111/j.1526-4637.2008.00524.x. [DOI] [PubMed] [Google Scholar]
- 28.Bernardes SF, Costa M, Carvalho H. Engendering pain management practices: The role of physician sex on chronic low-back pain assessment and treatment prescriptions. J Pain. 2013;14:931–940. doi: 10.1016/j.jpain.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Marquié L, Raufaste E, Lauque D, Mariné C, Ecoiffier M, Sorum P. Pain rating by patients and physicians: Evidence of systematic pain miscalibration. Pain. 2003;102:289–296. doi: 10.1016/S0304-3959(02)00402-5. [DOI] [PubMed] [Google Scholar]
- 30.Veldhuijzen DS, Karhof S, Leenders MEC, Karsch AM, van Wijck AJM. Impact of physicians’ sex on treatment choices for low back pain. Pain Pract. 2013;13:451–458. doi: 10.1111/papr.12015. [DOI] [PubMed] [Google Scholar]
- 31.Hirsh AT, Hollingshead NA, Matthias MS, Bair MJ, Kroenke K. The influence of patient sex, provider sex, and sexist attitudes on pain treatment decisions. J Pain. 2014;15:551–559. doi: 10.1016/j.jpain.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL., 3rd Sex, gender, and pain: A review of recent clinical and experimental findings. J Pain. 2009;10:447–485. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schäfer G, Prkachin KM, Kaseweter KA, Williams AC, de C. Health care providers’ judgments in chronic pain. Pain. 2016;157:1618–1625. doi: 10.1097/j.pain.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 34.Women in Pain Report Significant Gender Bias. [Accessed November 8, 2017];National Pain Report. 2014 http://nationalpainreport.com/women-in-pain-report-significant-gender-bias-8824696.html.
- 35.Edwards L. Women and the treatment of pain. [Accessed November 8, 2017];The New York Times. 2013 http://www.nytimes.com/2013/03/17/opinion/sunday/women-and-the-treatment-of-pain.html.
- 36.National Institutes of Health. Sex/Gender. National Institutes of Health Office of Research on Women’s Health; 2017. https://orwh.od.nih.gov/research/sex-gender/ [Google Scholar]
- 37.American Association of Medical Colleges. ERAS Statistics. American Association of Medical Colleges; 2017. [Accessed November 4, 2017]. https://www.aamc.org/services/eras/stats/359278/stats.html. [Google Scholar]
- 38.Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160:344–353. doi: 10.7326/M13-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vu CT, Elder DH. Pregnancy and the working interventional radiologist. Semin Intervent Radiol. 2013;30:403–407. doi: 10.1055/s-0033-1359735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dauer LT, Miller DL, Schueler B, et al. Occupational radiation protection of pregnant or potentially pregnant workers in IR: a joint guideline of the Society of Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J Vasc Interv Radiol. 2015;26:171–181. doi: 10.1016/j.jvir.2014.11.026. [DOI] [PubMed] [Google Scholar]