Abstract
Introduction
The purpose of this study was to assess effects of three different educational intervention arms on knowledge of and intention to receive Pap testing and HPV co-testing.
Methods
Three active educational intervention arms were developed: a fotonovela, a radionovela, and a digital story. A pilot randomized controlled trial (RCT) of 160 Latinas was conducted to assess the effectiveness of the intervention arms in increasing knowledge of cervical cancer and HPV and intention to be screened for cervical cancer compared to an attention control group (flu vaccination).
Results
Women in all three treatment arms significantly increased knowledge about cervical cancer compared to control arm (p=0.02). Knowledge about cervical cancer screening also increased in the active arms compared to control (p=0.0003). Knowledge of HPV risk also increased relative to the control (p=0.0001). There were no significant differences between the intervention arms in increased knowledge of cervical cancer or cervical cancer screening (p=0.57 and 0.16 respectively).
Discussion
This study supported the use of small media interventions in narrative education form as effective in increasing knowledge and intention to be screened for cervical cancer. The three culturally relevant interventions, built on qualitative data, were all successful in increasing knowledge.
Keywords: cervical cancer, HPV, Latinas, fotonovela, radionovela, digital story, education
INTRODUCTION
Although cervical cancer rates have steadily declined over the past several decades, over 12,000 estimated new cases and over 4,000 estimated cervical cancer deaths occurred during 2016 [1]. In 2013, the Surveillance, Epidemiology, and End Results (SEER) data indicated the rate of cervical cancer among all women in the U.S. was 7.5 cases per 100,000 and the median age at diagnosis was 49 years [1]. However, cervical cancer rates are not distributed equally; incidence rates among Latinas (9.4 per 100,000) were higher than rates among non-Hispanic White (NHW) women (7.5 per 100,000). Rates of cervical cancer mortality are similarly unequally distributed, with Latinas having higher rates than NHW women [1].
Cervical cancer is one of few cancers with established population-level screening guidelines that reduce risk of death [2]. The Papanicolaou (Pap) test is used as a screening method to identify morphological abnormalities of cervical cells that are indicative of carcinogenesis [3]. These dysplastic cells can be removed via out-patient clinical procedures. The United States Preventive Services Task Force (USPSTF) at the time of this study recommended screening women aged 21 to 65 years for cervical cancer with a Pap test every three years.[4] More recently, tests to detect infection by cervical cancer-causing strains of human papillomavirus (HPV), which results in dysplastic cervical cells, are also possible with the HPV test; more intensive screening recommended for women who test positive for high-risk strains of HPV [5]. Co-testing with the Pap and HPV tests has made early detection of cervical cancer more likely by identifying at-risk women even earlier than by Pap test alone. For women aged 30 to 65, the USPSTF recommends that Pap test and HPV test (co-testing) every five years; this extends the interval between screening visits [4]. With the advent of the HPV vaccine, the risk of cervical cancer can now be virtually eliminated if the vaccine is administered before HPV infection occurs [6].
Cervical cancer screening among age-eligible women in the U.S. remains below the Healthy People 2020 goal of 93% [7]. Overall, in 2014, 82.5% of women aged 21–65 years in the U.S. reported recent receipt of a Pap test; in the same year in Washington State, that rate was 81% [8]. As with cervical cancer incidence rates, cervical cancer screening is not equally distributed across populations. Among Latinas in the U.S., only 71.6% reported recent receipt of a Pap test and there is further variation in screening rates among Latinas by country of origin, socioeconomic status (SES), and level of acculturation [2]. Those born outside of the U.S., those with low health literacy, and those living in Latino-enclave communities are less likely to be screened than other Latinas [9–11]. Added to the barriers around screening is confusion by Latinas about the role of HPV in cervical cancer initiation [12]. Further, Latinas are less likely to be aware of HPV co-testing and the role it plays in recommendations for subsequent follow-up [12].
Interventions to educate and encourage Latinas who are under-screened for cervical cancer focus on a variety of strategies. Effective culturally appropriate communication strategies to reach under-screened Latinas have been documented [13–17], but the most effective approaches to encourage screening appear to be those that use face-to-face strategies including promotora (lay health worker) outreach via one-on-one small group sessions and small media (e.g. brochures, videos, and pamphlets) that are targeted to underserved Latinas [18–29]. Small media are recommended by The Guide to Community Preventive Services (the Community Guide), a collection of evidence-based findings of the Community Preventive Services Task Force, as an effective method to increase cervical cancer screening by Pap test [18, 30, 31]. Such media also can be targeted to reach specific audiences that experience literacy and/or cultural barriers to screening such as under-screened Latinas [32].
In this study, we built on the Community Guide’s recommendation to use small media to reach underserved Latinas to increase cervical cancer and HPV knowledge and encourage cervical cancer screening [18]. Although many small media formats exist, such as pamphlets, brochures, and electronic media, it is unclear which are most effective in increasing knowledge of and intention to obtain a Pap test and/or HPV co-test. Understanding the relative value of different media approaches will enable others to craft messages and materials to encourage non-adherent women to be screened. Because similar assessment of such interventions was not found in the literature, our goal was to develop three different small media strategies and use a pilot randomized controlled design to assess the effects of those three small media educational intervention strategies on knowledge of cervical cancer and HPV, and intention to receive cervical cancer screening.
METHODS
Setting
This project took place in the Lower Yakima Valley of Washington State. The area is heavily agricultural with farms primarily producing orchard fruits which are distributed internationally. The agricultural enterprise relies heavily on farmworkers to manage crops. The Lower Yakima Valley has a predominantly minority population of Latinos (69%). Residents are underserved in terms of social and economic factors. The poverty rate in the Valley is 19.0%, compared to 14.6% for the United States (US) as a whole.[33] Language spoken in the home is often “other than English” (40.1%).[34] Compared to Washington State, residents in the Valley are less likely to have a personal physician or medical care due to cost, and more likely to have an educational level less than high school.[35] The Community Need Index (CNI), which measures various socioeconomic indicators known to contribute to health disparities (income, culture and language, education, housing status, and insurance coverage) for every zip code in the US assigns a score on a scale of 1.0 (least need) to 5.0 (most need).The Valley’s zip code scores range from 3.8 to 4.8 on the CNI scale, indicating that people living in these communities experience substantial deficiencies in health promotion and health attainment.[36]
The Cervical Cancer and HPV Education Project
In the Lower Yakima Valley, there is little public health education about cervical cancer screening including the Pap test and the HPV co-test. Although these tests are routinely performed at the local safety-net clinic system, there has been no effort to publicly educate Latinas about the tests; further, any educational materials that do exist tend to be written in English while this Latina population speaks predominantly Spanish. As part of a larger initiative to reduce health disparities in the Lower Yakima Valley, we launched the Cervical Cancer and HPV Education Project. This two-year project was designed to educate Latinas about their increased risk of cervical cancer compared to NHW women, the role of HPV in cervical cancer, and to provide information about Pap and HPV co-testing. This project was approved by the Institutional Review Board at Fred Hutchinson Cancer Research Center in Seattle, Washington.
Focus groups to inform material development
To identify barriers and facilitators of cervical cancer screening, we held focus groups with providers from the local safety net clinics, as well as local Latinas. The provider focus groups (N=2), led by the Principal Investigator (BT), lasted 90 minutes and consisted of 24 providers who were asked questions such as, “How often do you recommend an HPV test with a Pap test?” and “How do women learn what the Pap and HPV tests are for?” The providers noted that few women knew about HPV or the HPV co-test, and that they knew little about the cervical cancer guidelines for screening. They also noted they lacked time to explain the features of the HPV co-test to women during a regular clinic visit. Despite this, providers noted that the women understood “normal” and “abnormal” results and that women indicated they would agree to have the HPV co-test.
A trained Project Coordinator in the Lower Yakima Valley led a series of two-hour focus groups (N=3) with a total of 23 Latinas. Participants were asked questions such as, “When you received your last Pap test, how do you know if you had an HPV test?” and “What will help you understand your Pap and HPV tests better?” Women indicated that they believed the Pap test could identify HPV, and that the HPV co-test was only needed if the Pap test was positive. Women also noted that they did not understand the results of the HPV co-test. Other topics that emerged were difficulties in getting to clinics during clinic hours, lack of child care, and lack of transportation. Women also reported the desire to receive information about the HPV co-test, and the fact that HPV does not cause symptoms. Overall, women expressed an eagerness to learn more.
To address the barriers and facilitators identified in the focus groups, we developed three types of small media educational intervention arms. One was a fotonovela, which has been shown to be very popular with lay Latinas [37, 38]. Another was a radionovela, that essentially used the same script as the fotonovela but in an oral radio script; this was done because Latinas in the Lower Yakima Valley receive much information from a local Spanish-language radio station [39, 40]. The last was a digital story which has been shown to be important and valuable to this population [41]. Because all three strategies had been successfully used in other intervention projects in the Valley [42–44], we developed and assessed all three media strategies to determine which one was most effective in helping women understand the messages.
Materials
Fotonovela.
The fotonovela is an illustrated booklet written in Spanish and English. The fotonovela is bilingual in that the Spanish language booklet can be turned over to access the English language version. The storyline depicts three Latinas varying in age: a young woman named Victoria, who is turning 30, her older sister, Liliana, and their mother, Doña Maribel. It also includes a female physician. Liliana is talking with her doctor about the tests she has just had and asks her doctor to explain the Pap test and HPV co-test. Using a plastic model of a woman’s reproductive system, the doctor explains the tests and discusses the human papillomavirus and the HPV co-test. She notes that a negative HPV co-test means that further Pap testing can be done less frequently. Liliana goes home and talks to her younger sister about having the HPV co-test. Their mother listens in and the sisters talk to her about having the tests. Later, Liliana gets the news that her tests were negative. She talks with the nurse who also encourages her to bring in her children aged 9 and older for the HPV vaccine. The booklet ends with some summary facts about HPV and the Pap test and encourages HPV vaccination for both girls and boys.
Radionovela.
The radionovela is a scripted conversation between the same characters. The local radio station in the Lower Yakima Valley provided actresses to play the roles of the women. The script was identical to that in the fotonovela. The Spanish version of the radio vignette lasted 5:26 minutes and the English version was 5:00 minutes.
Digital Story.
A digital story is a three to five-minute video of storytellers’ voices, music, and pictures that tell a story about an event or situation that has had an impact on someone’s life. Digital stories provide healing through sharing an important event, usually about health [41]. We created a digital story using the pictures from the fotonovela and the voices from the radionovela. The digital story was shown to the women on an iPad™. The five-minute digital story was available in both English and Spanish.
Flu Vaccine Control Arm.
We used an attention control arm so that all participants received valuable information as a result of taking part in the study. The control arm participants received a fact sheet on the need for a flu vaccine injection (flu shot). The fact sheet, available in both English and Spanish was provided by the Centers for Disease Control and Prevention (CDC). The fact sheet included information about the need for flu shots, who should be given the flu shots, and the safety of the flu vaccine [45].
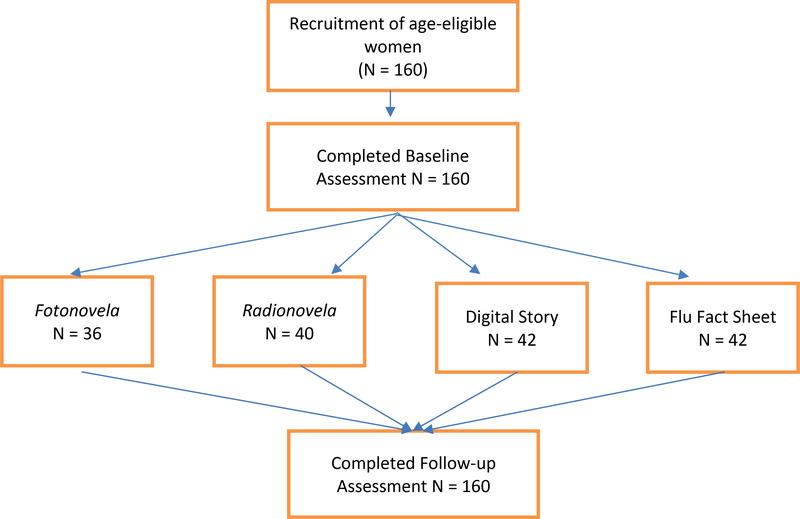
Study Design
The study design is shown in Figure 1. Project staff in the Lower Yakima Valley set up study information tables at grocery stores, retail establishments, food banks, and health fairs to recruit eligible women. Women were recruited until a total of 160 participants were enrolled. This number was chosen for two reasons. First, the study had limited funds. Second, this was a pilot study and we wished to gain information on two aims: primarily, we wished to know whether the combined intervention effect was greater than that of a control arm (the flu vaccine factsheet); and secondarily, we wished to know whether there were differences between the three intervention arms. Since we could not find information on such differences in the literature, we used this pilot to identify the various effect sizes. This pilot study would then be useful for others wishing to replicate our work. Eligibility requirements included being between the ages of 21 through 64, not pregnant, not having had a hysterectomy, and able to complete the questionnaires in English or Spanish. Women who were interested in participating also referred friends and relatives to the study. In three weeks, we recruited a total of 160 women to participate.
Figure 1:
Overview of Design
Procedures.
Study procedures were explained by study staff, who also consented each participant. Each participating woman was read the informed consent and then given an informed consent form to sign; these signed forms were returned before completing a baseline survey. All participants completed a baseline survey (available from the corresponding author upon request) in English or Spanish, as preferred by the participant. The baseline survey could also be conducted as a face-to-face interview. If this was requested by the participant, project staff read the questions to the participants and recorded the responses on the paper survey. Following completion of the baseline survey, participants were randomized to one of the four arms described above. Randomization was generated by a biostatistician at the Cancer Center via Microsoft Excel with individual assignments enclosed in separate sealed envelopes; the sealed envelopes were sequentially numbered to be opened when a woman was randomized. Study staff opened an envelope for each woman after the participant completed the baseline survey. The surveys were administered in batches of 15 to 20 depending on the number of women available at a particular time; all surveys were completed within a three-week window. Each participant received a $20 gift card.
After randomization, participants were taken to a separate room in our Lower Yakima Valley office where they read, watched, or heard the information. For the fotonovela, the participants viewed and read the booklet in English or Spanish as they preferred. The fotonovela was developed at the sixth-grade reading level and if participants had problems with reading the content, the trained promotoras who were onsite assisted them by reading the text in the fotonovela aloud. The radionovela was placed on an MP3 player and the women listened to it in their choice of English or Spanish. The digital story was played on an iPad™ and the participant watched and heard the digital story in their choice of English or Spanish. Women randomized to the control arm read the flu vaccine fact sheet in their choice of English or Spanish. Again, promotoras assisted women who had difficulty reading the fact sheet by reading the fact sheet aloud.
After the intervention, we asked participants to complete a follow-up survey (available from the corresponding author upon request) using the same procedures as followed for the baseline survey. The survey contained the same questions as the baseline survey, but added questions about the content of, and woman’s reaction to, the intervention material to which they were randomized. Retention was 100%.
Data Instruments.
Knowledge about cervical cancer and HPV, as well as intention to obtain cervical screening, was assessed pre- and post-intervention. The baseline questionnaire contained 46 questions and took about 20 minutes to complete. Cervical cancer knowledge included three specific domains: cervical cancer risk, pap testing, and HPV risk. Cervical cancer risk included two items, “Have you heard of cervical cancer?” and “Do you think HPV can cause cervical cancer?” Pap testing was assessed by two items: “How often should a woman your age have cervical cancer screening?” and “Have you heard about recent changes in the cervical cancer screening guidelines?” HPV risk was assessed by seven items asking participants whether they had heard of HPV, whether they thought HPV infection was rare, knowledge of how HPV was spread, frequency of HPV infection, possible symptoms and treatment of HPV infection. Intention to receive pap testing was assessed by asking women if they intended to obtain cervical screening, and when they expected to receive such screening.Positive responses were summed and averaged to develop a score for each domain. Knowledge of HPV co-testing was assessed by asking respondents if they had ever heard of the HPV co-test, and intention to receive HPV co-testing was established by response to “When do you expect to have your next HPV co-test?” Past pap testing was determined by responses to “When was your last pap test?” and HPV co-testing was established by response to “Have you ever had an HPV co-test?” All respondents also completed knowledge questions about the flu vaccine, including whether they had ever received the vaccine, the ages at which the vaccine should be received, the benefits of the flu vaccine, and whether they had ever talked with their doctor about the flu vaccine. Socio-demographic items included age, educational status, income, race/ethnicity, marital status, zip code, preferred language spoken and read, place of birth, years lived in the U. S., and whether the respondent worked outside of the home.
The follow-up survey included 38 questions and repeated the same knowledge and intention questions as the baseline survey with additional questions to assess responses to the three treatment strategies. Surveys were forward translated into Spanish by a native Spanish speaker experienced in the colloquial lexicon [46]. Study data were managed using REDCap electronic data capture tools hosted at Fred Hutchinson Cancer Research Center. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies.[47]
Statistical Analysis.
Differences in the distribution of demographic characteristics across the four intervention arms were tested using a non-parametric Chi-square statistic (Wald test). Linear regression models were used to assess differences in mean knowledge scores at follow-up for each of the outcome variables (see Table 3) across intervention arms adjusted for baseline knowledge score and demographic covariates, as well as intention to receive pap testing. If differences across the four intervention arms (including control) were obvious, further analyses to test for differences across the three treatment arms were also completed using a nonparametric Chi-square statistic. All analyses were conducted using Stata SE version 13.0 (StataCorp, College Station, TX).
Table 3:
Follow-up knowledge and intention across four treatment arms.
| Knowledgea | Intention for Screeningb | |||
|---|---|---|---|---|
| Cervical Cancer Risk | Cervical Screening | HPV Risk | Cervical Screening | |
| Fotonovela | 97.1 (1.9) | 36.4 (4.3) | 81.7 (2.6) | 92.5 (4.0) |
| Radionovela | 99.2 (1.2) | 32.9 (5.7) | 68.0 (2.4) | 98.5 (1.8) |
| Digital Story | 97.5 (1.7) | 23.8 (4.9) | 83.6 (2.4) | 90.2 (3.3) |
| Control | 85.5 (4.2 ) | 13.7 (3.3) | 56.5 (2.4) | 98.5 (1.7) |
| P valuesc | ||||
| For comparison of 4 treatment arms | 0.02 | 0.0003 | <0.0001 | 0.06 |
| For comparison of 3 intervention armsd | 0.57 | 0.16 | <0.0001 | -- |
Knowledge at follow-up is computed as the mean average of correct responses to survey items adjusted for baseline knowledge, age, and primary language spoken.
Intention at follow-up is computed as the mean average of endorsing responses to survey items adjusted for baseline intention, age, and primary language spoken.
Wald test for equality of means
Differences in means of three intervention arms only tested if statistically significant difference in four treatment arms.
RESULTS
One hundred sixty women were randomized to one of four intervention arms to complete the study. Intervention arms included: 1) fotonovela (n=36); 2) radionovela (n=40); 3) digital story (n=42); and 4) control group (flu fact sheet) (n=42). (See Figure 1.) All the participants (n=160) completed the follow-up survey. Using Chi-square tests no differences in the distribution of demographic characteristics across intervention arms were detected (Table 1). Most women were between 30 and 49 years of age (mean: 40.7 years; SE: 0.8), had completed 12th grade or less (79.4%), were not currently working outside of the home (65.6%), had a household income of $35,000 or less (73.1%), did not have health insurance (52.5%), did have a regular healthcare clinic (93.1%), did have a regular healthcare provider (66.9%), selected Spanish as their primary spoken language (84.4%), were married or in a relationship (70.0%), and had children within the age range (9–26 years) of eligibility for HPV vaccination (85.6%).
Table 1:
Demographic characteristics among women across four intervention arms.
| Fotonovela (N=36) N (%) | Radionovela (N=40) N (%) | Digital Story (N=42) N (%) | Control (N=42) N (%) | P value | |
|---|---|---|---|---|---|
| Age, years | 0.99 | ||||
| 21 to 29 | 5 (13.9) | 5 (12.5) | 5 (11.9) | 5 (11.9) | |
| 30 to 49 | 22 (61.1) | 27 (67.5) | 29 (69.0) | 29 (69.0) | |
| 50 or older | 9 (25.0) | 8 (20.0) | 8 (19.1) | 8 (19.1) | |
| Education | 0.52 | ||||
| 8th grade or less | 17 (47.2) | 25 (62.5) | 24 (57.1) | 19 (45.3) | |
| 9th to 12th grade | 12 (33.3) | 6 (15.0) | 10 (23.8) | 14 (33.3) | |
| HS diploma or higher | 7 (19.5) | 9 (22.5) | 8 (19.1) | 9 (21.4) | |
| Employment Status | 0.20 | ||||
| Not Working | 26 (72.2) | 23 (57.5) | 24 (57.1) | 32 (76.2) | |
| Part-time | 3 (8.3) | 9 (22.5) | 5 (11.9) | 4 (9.5) | |
| Full-time | 7 (19.5) | 8 (20.0) | 13 (31.0) | 6 (14.3) | |
| Household Income | 0.82 | ||||
| $15,000 or less | 12 (33.3) | 13 (32.5) | 11 (26.2) | 10 (23.8) | |
| $15,001 to $25,000 | 8 (22.2) | 9 (22.5) | 11 (26.2) | 10 (23.8) | |
| $25,001 to $35,000 | 9 (25.0) | 6 (15.0) | 6 (14.3) | 12 (28.6) | |
| $35,001 or higher | 5 (13.9) | 11 (27.5) | 11 (26.2) | 9 (21.4) | |
| Missing | 2 (5.6) | 1 (2.5) | 3 (7.1) | 1 (2.4) | |
| No Health Insurance | 25 (69.4) | 19 (47.5) | 21 (50.0) | 19 (45.2) | 0.14 |
| No Regular Clinic | 2 (5.6) | 1 (2.5) | 5 (11.9) | 3 (7.1) | 0.40 |
| No Regular Provider | 12 (33.3) | 10 (25.0) | 16 (38.1) | 15 (35.7) | 0.62 |
| Primary Language Spoken | 0.07 | ||||
| Spanish | 34 (94.4) | 36 (90.0) | 32 (76.2) | 33 (78.6) | |
| Spanish and/or English | 2 (5.6) | 4 (10.0) | 10 (23.8) | 9 (21.4) | |
| Marital Status | 0.12 | ||||
| Married or in relationship | 25 (69.4) | 27 (69.2) | 25 (59.5) | 35 (83.3) | |
| Not married or single | 11 (30.6) | 12 (30.8) | 17 (40.5) | 7 (16.7) | |
| Missing | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | |
| Children Eligible for HPV vaccine | 28 (96.6) | 33 (94.3) | 28 (80.0) | 31 (81.6) | 0.08 |
Differences in variable frequencies across 4 intervention arms tested by Chi-square
Past Pap and HPV Self-reported Testing Behaviors.
Similarly, the distribution of most Pap and HPV-related self-reported baseline behaviors was not significantly different across intervention arms (Table 2). Most women reported that they had received a Pap test (98.1%) and most within the past three years (82.5%). The majority reported never having received an HPV co-test (75.6%).
Table 2.
Pap and HPV behaviors among women across 4 intervention armsa.
| Fotonovela (N=36) N (%) | Radionovela (N=40) N (%) | Digital Story (N=42) N (%) | Fact Sheet (N=42) N (%) | P value | |
|---|---|---|---|---|---|
| Ever had a Pap test | 36 (100) | 39 (97.5) | 40 (95.2) | 42 (100) | 0.32 |
| Recency of Pap test | 0.14 | ||||
| ≤ 3 years | 31 (86.1) | 35 (87.5) | 31 (73.8) | 35 (83.3) | |
| > 3 years | 5 (13.9) | 5 (12.5) | 9 (19.2) | 7 (16.7) | |
| Don’t know | 0 (0.0) | 0 (0.0) | 3 (7.1) | 0 (0.0) | |
| Ever heard of HPV | 31 (86.1) | 32 (80.0) | 31 (73.8) | 34 (81.0) | 0.60 |
| Ever had an HPV test | 10 (27.8) | 9 (22.5) | 14 (33.3) | 6 (14.3) | 0.23 |
Differences in variable frequencies across four arms tested by chi-square.
Knowledge of Cervical Cancer Risk and Pap Test Screening.
When we examined level of cervical cancer-related knowledge at follow-up, adjusted for knowledge at baseline, we found that all three treatment arms (i.e. fotonovela, radionovela, and digital story) were associated with higher knowledge scores. Knowledge of cervical cancer risk was already fairly high. After accounting for baseline score, 85.5% of women in the control arm correctly answered the knowledge questions at follow-up (Table 3). Compared to women in the control group, however, knowledge among women in the fotonovela (% diff: 11.6; 95% CI: 2.4, 20.9;), radionovela (% diff: 13.7; 95% CI: 4.9, 22.5), and digital story (% diff: 11.9; 95% CI: 3.2, 20.7-) arms was even higher. Knowledge about cervical cancer screening guidelines was much lower. After accounting for baseline score, 13.7% of women in the control arm correctly answered the screening questions at follow-up. Compared to women in the control group, screening knowledge scores were also higher among women in the fotonovela (% diff: 22.7; 95% CI: 11.9, 33.6), radionovela (% diff: 19.1; 95% CI: 6.1, 32.2), and digital story (% diff: 10.0; 95% CI: −1.5, 21.7) arms. We did not find that these score increases varied across active intervention arm for either knowledge of cervical cancer risk (P=0.57) or screening (P=0.16).
Intention to Obtain Pap Testing
Level of intention to undergo pap testing was very high (Table 3). Accounting for baseline levels of intention, 98.5% of women in the control group reported that they intended to undergo pap testing. We did not find that women in the active intervention arms had significantly different levels of intention to undergo pap testing at follow-up (P=0.06).
DISCUSSION
Latinas in all groups participating in this project had high levels of baseline knowledge about cervical cancer risk. There was significantly less knowledge about cervical cancer screening and HPV co-testing. After intervention, knowledge of cervical cancer risk, cervical cancer screening, and HPV risk improved significantly in all three active intervention arms compared to the control arm. Participants in the fotonovela and digital story arms had greater knowledge increases of HPV risk compared to those in the radionovela arm.
This study substantiated the Community Guide’s recommendations regarding the efficacy of small media as an appropriate intervention tool for changing knowledge and intention to screen for cervical cancer and HPV, specifically among Latinas. Interestingly, it did not seem to make much difference which type of small media was used. All three of our treatment interventions had a positive effect on cervical cancer knowledge. Other research also notes that a key to reaching this population is the cultural relevance of the intervention; that is women relate to interventions that are built on their cultural ideas and values [48, 49]. Whether the intervention materials were digital video, audio, or written, the key was to resonate with the cultural attitudes and beliefs of the population that was being addressed.
As to the types of educational interventions that are most effective in reaching the Latina population, studies have noted that narrative education is more effective than non-narrative education [50, 51]. Narrative education includes materials such as our intervention materials which utilize individuals experiencing and reflecting on a condition while non-narrative education is the didactic and factual information presented in text books and pamphlets [52]. All of our active intervention arms had a narrative component: the fotonovela included the story of women making decisions about Pap and HPV co-testing; the radionovela and the digital story included the same story.
In a qualitative study, Kilanowski found that Latina migrant farmworker women preferred comic-book style handouts, text in both English and Spanish, and video discs [53]. In terms of written materials, they liked things in color and that were of a size that could be easily carried in one’s purse. Some of these preferred characteristics were exemplified by our active intervention materials. For example, all of our intervention materials were available in both English and Spanish. The fotonovela was in color and measured 4.25 inches by 5.5 inches in size; the digital story was also made using color photographs. This also suggests that visual and narrative materials are considered preferable to Latinas.
The participants in this study had high rates of ever having had a Pap test and this was uniform across treatment arms. Further, with one exception, participants were largely adherent with Pap testing guidelines. Thus, the high baseline rates may be responsible for not seeing a significant increase in intention to be screened at follow-up. Those randomized to the digital story arm had lower rates of testing, but the difference was not significant. The participants were largely of low socioeconomic status (SES), with less than a high school education and low family income; thus, they fulfilled the criteria of Latinas least likely to be screened. Despite this, 85% of the women had been screened within the past three years. This may be because there is a large Federally Qualified Health Center (FQHC) in the region that has an active inreach plan to encourage women to have Pap tests. This is substantiated by noting that almost all participants had a regular health clinic, despite having no health insurance.
Participants had high baseline rates of having heard about the HPV co-test, yet few noted that they ever had an HPV co-test. This is contrary to what providers told us happened at the clinics where most of the women were likely to have been seen. The FQHC recommends HPV cotesting to match the USPSTF recommendations for cervical cancer screening. It may be that women did not understand the difference between a Pap test and an HPV co-test, or may not have been aware that they had an HPV co-test.
Limitations.
This study is not without limitations. Our participants were of very low SES and thus, these results may not be generalizable to higher SES Latinas. Nevertheless, a sizeable proportion of Latinos in the U.S. are of low SES as indicated by overall high rates of poverty, low literacy, and low income [54]. Another limitation is the relatively small numbers of participants in the RCT. This may have contributed to the lack of significant differences in the various types of small media interventions. Given the limited resources of the project, we were unable to enlarge the RCT. Nevertheless, this innovative study compared the effectiveness of three small media approaches to intervention, and thus, produced effectiveness estimates that others can use in larger studies to assess the effectiveness of different intervention strategies. Future studies of a larger size are warranted. Finally, our study assessed intention to change behavior and did not document behavior change. This also should be done in subsequent studies.
Conclusions.
We can conclude from this study that small media interventions using narrative education form are efficacious in changing knowledge and intention to receive pap testing. From a clinical perspective, the intervention materials that we developed can be disseminated in clinics to inform women of the meaning of the Pap test and HPV co-test. Indeed, the clinic system that participated in this study is disseminating the fotonovela to women who come in for Pap testing and the HPV co-test, indicating that the clinic system sees value in the materials.
ACKNOWLEDGEMENTS
We are grateful to all the providers and community women who participated in this research project. We would also like to thank all the staff at the Center for Community Health Promotion. This project was supported by grant numbers 3U54CA153502, 3U54CA153502-05S1, U54 CA132381 and U54 CA132383 from the National Cancer Institute (NCI) and the Institute of Translational Health Science grant (UL1 RR025014) from the National Center for Research Resources (NCRR) at the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCI, NCRR, or the NIH.
REFERENCES
- 1.National Cancer Institute Surveillance, E., and End Results (SEER) Program Cancer Statistics Facts: Cervix Uteri Cancer. 2016.
- 2.Centers for Disease Control and Prevention (CDC), Cancer Screening Test Use. Morbidity and Mortality Weekly Report. 2015. p. 464–468. [PMC free article] [PubMed]
- 3.National Cancer Institute NCI Dictionary of Cancer Terms. 2016.
- 4.United States Preventive Services Task Force Final Update Summary: Cervical Cancer Screening. 2016.
- 5.American Cancer Society HPV and HPV Testing: Human Papilloma Virus (HPV). 2017.
- 6.Harper DM, et al. , Efficacy of a bivalent L1 virus-like particle vaccine in prevention of infection with human papillomavirus types 16 and 18 in young women: a randomised controlled trial. The lancet, 2004. 364(9447): p. 1757–1765. [DOI] [PubMed] [Google Scholar]
- 7.Brown ML, et al. , Peer Reviewed: Challenges in Meeting Healthy People 2020 Objectives for Cancer-Related Preventive Services, National Health Interview Survey, 2008 and 2010. Preventing chronic disease, 2014. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Behavioral Risk Factor Surveillance System Survey Data, C.f.D.C.a.P. (CDC), Editor. 2014: Atlanta, GA. [Google Scholar]
- 9.Goel MS, et al. , Racial and ethnic disparities in cancer screening. Journal of general internal medicine, 2003. 18(12): p. 1028–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh GK and Hiatt RA, Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreignborn populations in the United States, 1979–2003. International journal of epidemiology, 2006. 35(4): p. 903–919. [DOI] [PubMed] [Google Scholar]
- 11.Froment M-A, et al. , Impact of socioeconomic status and ethnic enclave on cervical cancer incidence among Hispanics and Asians in California. Gynecologic oncology, 2014. 133(3): p. 409–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vanslyke JG, et al. , HPV and cervical cancer testing and prevention: knowledge, beliefs, and attitudes among Hispanic women. Qualitative Health Research, 2008. 18(5): p. 584–596. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez-Esquer ME, et al. , A su salud: a quasi-experimental study among Mexican American women. Am J Health Behav, 2003. 27(5): p. 536–45. [DOI] [PubMed] [Google Scholar]
- 14.Baezconde-Garbanati L, et al. , Reducing the Excess Burden of Cervical Cancer Among Latinas: Translating Science into Health Promotion Initiatives. Calif J Health Promot, 2013. 11(1): p. 45–57. [PMC free article] [PubMed] [Google Scholar]
- 15.Fernandez ME, et al. , Cervical cancer control for Hispanic women in Texas: strategies from research and practice. Gynecol Oncol, 2014. 132 Suppl 1: p. S26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mann L, et al. , Increasing Cervical Cancer Screening Among US Hispanics/Latinas: A Qualitative Systematic Review. J Cancer Educ, 2015. 30(2): p. 374–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen NN, et al. , Understanding Cervical Cancer Screening among Latinas through the Lens of Structure, Culture, Psychology and Communication. J Health Commun, 2018: p. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guide to Community Preventive Services. Cancer Screening: Small Media Targeting Clients – Cervical Cancer. 2005. [cited 2019 January 7, 2019]; Available from: https://www.thecommunityguide.org/findings/cancer-screening-small-media-targetingclients-cervical-cancer.
- 19.Jandorf L, et al. , Breast and cervical cancer screening among Latinas attending culturally specific educational programs. Prog Community Health Partnersh, 2008. 2(3): p. 195–204. [DOI] [PubMed] [Google Scholar]
- 20.Fernández ME, et al. , Effectiveness of Cultivando La Salud: A Breast and Cervical Cancer Screening Promotion Program for Low-Income Hispanic Women. American Journal of Public Health, 2009. 99(5): p. 936–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’Brien MJ, et al. , Community health worker intervention to decrease cervical cancer disparities in Hispanic women. J Gen Intern Med, 2010. 25(11): p. 1186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luque JS, et al. , Salud es vida: development of a cervical cancer education curriculum for promotora outreach with Latina farmworkers in rural Southern Georgia. Am J Public Health, 2011. 101(12): p. 2233–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saad-Harfouche FG, et al. , Esperanza y Vida: Training Lay Health Advisors and Cancer Survivors to Promote Breast and Cervical Cancer Screening in Latinas. Journal of Community Health, 2011. 36(2): p. 219–227. [DOI] [PubMed] [Google Scholar]
- 24.Thompson B, et al. , Increasing cervical cancer screening in the United States-Mexico border region. J Rural Health, 2014. 30(2): p. 196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Molokwu J, et al. , Evaluation of the Effect of a Promotora-led Educational Intervention on Cervical Cancer and Human Papillomavirus Knowledge Among Predominantly Hispanic Primary Care Patients on the US-Mexico Border. J Cancer Educ, 2016. 31(4): p. 742–748. [DOI] [PubMed] [Google Scholar]
- 26.Thompson B, et al. , Results of a Randomized Controlled Trial to Increase Cervical Cancer Screening Among Rural Latinas. Cancer, 2017. 123(4): p. 666–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fleming K, et al. , Educating Hispanic Women about Cervical Cancer Prevention: Feasibility of a Promotora-Led Charla Intervention in a Farmworker Community. Ethn Dis, 2018. 28(3): p. 169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nuno T, et al. , A Promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.-Mexico border: a randomized controlled trial. Cancer Causes Control, 2011. 22(3): p. 367–74. [DOI] [PubMed] [Google Scholar]
- 29.Cheun ASA and Loomis J, A Culturally Sensitive Approach to Cervical Cancer Prevention in the Latina Population Using the Promotora Model. Nurs Womens Health, 2018. 22(4): p. 338–345. [DOI] [PubMed] [Google Scholar]
- 30.Sabatino SA, et al. , Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am J Prev Med, 2012. 43(1): p. 97–118. [DOI] [PubMed] [Google Scholar]
- 31.Services, T.F.o.C.P., Recommendations for client-and provider-directed interventions to increase breast, cervical, and colorectal cancer screening. American journal of preventive medicine, 2008. 35(1 Suppl): p. S21. [DOI] [PubMed] [Google Scholar]
- 32.Byrd TL, et al. , AMIGAS: a multicity, multicomponent cervical cancer prevention trial among Mexican American women. Cancer, 2013. 119(7): p. 1365–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poverty Status in the Past 12 Months; Yakima County 2013–2017 American Community Survey 5-Year Estimates, in American FactFinder Community Facts. 2017, U.S. Census Bureau: Washington, DC. [Google Scholar]
- 34.Language Spoken at Home; Yakima County 2013–2017 American Community Survey 5Year Estimates, in American FactFinder Community Facts. 2017, U.S. Census Bureau: Washington, DC. [Google Scholar]
- 35.Chronic Disease Profiles by County. 2017, Washington State Department of Health: Olympia, WA. [Google Scholar]
- 36.Community Need Index Methodology and Source Notes. 2018, Truven Health Analytics. p. 2.
- 37.Hinojosa MS, et al. , Salud de la mujer: using fotonovelas to increase health literacy among Latinas. Progress in community health partnerships: research, education, and action, 2010. 4(1): p. 25–30. [DOI] [PubMed] [Google Scholar]
- 38.Houston C, Fotonovelas and Historietas. Library Services for Multicultural Patrons: Strategies to Encourage Library Use, 2012: p. 149. [Google Scholar]
- 39.Clayman ML, et al. , Providing health messages to Hispanics/Latinos: understanding the importance of language, trust in health information sources, and media use. Journal of health communication, 2010. 15(sup3): p. 252–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ramirez AS, et al. , Seeking Information on behalf of others: an analysis of calls to a Spanish-language radio health program. Health promotion practice, 2015. 16(4): p. 501509. [DOI] [PubMed] [Google Scholar]
- 41.Briant KJ, et al. , The Power of Digital Storytelling as a Culturally Relevant Health Promotion Tool. Health Promotion Practice, 2016: p. 1524839916658023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kepka D, et al. , Evaluation of a radionovela to promote HPV vaccine awareness and knowledge among Hispanic parents. J Community Health, 2011. 36(6): p. 957–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kepka DL, et al. , Development of a Radionovela to Promote HPV Vaccine Awareness and Knowledge Among Latino Parents. Public Health Reports, 2012. 127(1): p. 130–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Briant KJ, et al. , The power of digital storytelling as a culturally relevant health promotion tool. Health promotion practice, 2016. 17(6): p. 793–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention Seasonal Influenza. 2016. [Google Scholar]
- 46.Robinson D, Becoming a translator: An introduction to the theory and practice of translation. 2012: Routledge. [Google Scholar]
- 47.Harris PA, et al. , Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 2009. 42(2): p. 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sabogal F, et al. , Printed health education materials for diverse communities: suggestions learned from the field. Health Education Quarterly, 1996. 23(1_suppl): p. 123–141. [Google Scholar]
- 49.Dixon-Gray LA, et al. , Amor y Salud (Love and Health): a preconception health campaign for second-generation Latinas in Oregon. American Journal of Health Promotion, 2013. 27(3_suppl): p. S74–S76. [DOI] [PubMed] [Google Scholar]
- 50.Murphy ST, et al. , Narrative versus nonnarrative: The role of identification, transportation, and emotion in reducing health disparities. Journal of Communication, 2013. 63(1): p. 116–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moran MB, et al. , A pilot test of the acceptability and efficacy of narrative and nonnarrative health education materials in a low health literacy population. J Commun Healthc, 2016. 9(1): p. 40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hinyard LJ and Kreuter MW, Using Narrative Communication as a Tool for Health Behavior Change: A Conceptual, Theoretical, and Empirical Overview. Health Education & Behavior, 2007. 34(5): p. 777–792. [DOI] [PubMed] [Google Scholar]
- 53.Kilanowski JF, Anticipatory guidance preferences of Latina migrant farmworker mothers. Journal of Pediatric Health Care, 2013. 27(3): p. 164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kochhar R, The occupational status and mobility of Hispanics. Education, 2000: p. 7. [Google Scholar]