Abstract
To assess facilitators and barriers to retention in care for adolescents living with HIV, we conducted in-depth, semi-structured interviews with adolescents ages 13 to 24 years who were living with HIV and being cared for in either an adolescent-friendly or standard government-supported clinic in KwaZulu-Natal, South Africa. We used inductive content analysis approach based on grounded theory derived from reviewing, coding, and interpreting data. We interviewed 28 adolescents living with HIV (16 in the adolescent clinic and 12 from the pediatric clinic) and 14 of their caregivers. Barriers to retention in care included having to attend clinic during school hours, fear of disclosure to others, social isolation, and conflict with clinical staff. Facilitators to retention in care seen in the adolescent-friendly services clinic included after school clinic hours, peer support, and connection to the clinical staff. Adolescent-friendly services are facilitators of HIV care and warrant prioritization in treatment programs.
Keywords: Adolescents, Adolescent-friendly, retention in care, HIV
Introduction:
With widespread availability of antiretroviral therapy (ART), children infected with HIV perinatally are surviving into adulthood (1). In South Africa, ART only became available in 2004, resulting in more than 300,000 perinatal HIV infections in the early and mid 2000s (1). By 2018, many of these children who survived perinatal HIV infection have entered adolescence. Studies have shown increased mortality, lower viral suppression rates, and lower retention in care in adolescents living with HIV compared to adults living with HIV (1-10). These poor outcomes may be related to delayed disclosure of HIV-positive status, stigma, treatment fatigue, mental health problems, and substance use among adolescents (1, 7, 8, 11-14).
To address many of these challenges, the World Health Organization (WHO) has issued guidance on providing adolescent-friendly services for adolescents living with HIV; however, the WHO acknowledges that this recommendation is based on very poor-quality evidence due to insufficient numbers of studies (15). A pre- and post-evaluation of adolescent-friendly services in Kenya did not find a difference in retention in care or viral suppression at 6 or 12 months after implementation (16). A study conducted by the Adolescent Medicine Trials Network for HIV/AIDS Interventions in the United States found that the most important factors in provision of adolescent-friendly services were the physical space and social environment (17). A qualitative study with healthcare providers suggested that peer support and collaboration with health providers may improve care for older adolescents living with HIV in sub-Saharan Africa (18). However, there are limited data about the effectiveness, necessary components, and mechanism of providing these services and no studies to date have evaluated the effect on mortality. We found higher retention in care and viral suppression among adolescents attending adolescent-friendly services clinic compared to standard of care in South Africa (19). This research aims to identify the factors that contribute to effective adolescent-friendly services to help optimize the development of clinics targeting this population and their impact on treatment outcomes.
To date, only a few studies have evaluated adolescent-friendly services related to retention in care. The HIV Research Network, a United States cohort, found that attending clinics with adolescent-friendly waiting areas, evening clinic hours, and adolescent-health training for providers improved retention in care (20). A recent systematic review of interventions to improve retention in care in low- and middle-income countries found that decentralization, down-referral of stable patients, task-shifting, and differentiated care improved retention among adults, but there was limited data on adolescents and young adults (21). A gap thus remains in the literature regarding how adolescent-friendly services can be best designed to improve retention in care especially in low and middle-income countries.
We previously demonstrated that adolescent-friendly services improved retention in care and viral suppression among adolescents living with HIV when compared to a standard pediatric clinic in South Africa (19). To assess why these services were effective and to evaluate their most important components, we conducted qualitative interviews with a sample of the adolescents who were evaluated in the quantitative analysis, along with their caregivers.
Methods:
Setting:
Don McKenzie Hospital is a regional tuberculosis hospital located in the Valley of 1000 Hills, which is 35 kilometers west of Durban, KwaZulu-Natal, South Africa. Ethembeni Clinic, its associated HIV clinic, opened in April 2007 and cares for >2,500 adults living with HIV, >400 children living with HIV (age birth to 12 years), and 241 adolescents living with HIV (age 13-24). Participants for this study were recruited from Ethembeni Clinic, which opened an adolescent clinic in March 2009.
Characteristics of the pediatric and adolescent clinics:
Adolescents attending the standard weekday pediatric clinic were evaluated by a doctor and counselors on weekdays every 1 to 3 months and obtained medication on the same day at an onsite pharmacy. The adolescent clinic operated on Saturday and included ART dispensing, lunch, and scheduled group activities (e.g., dancing, soccer, education, counseling). The clinic was established with the intention of improving retention in care for adolescents living with HIV before they transition to adult care. Initially, adolescents over age 13 could attend if they were fully aware of their HIV-positive status and receiving ART for 6 months. Due to limited space and funding, the adolescent clinic was closed to new enrollment after reaching 80 adolescents in November 2012 and subsequent adolescents remained in the standard pediatric clinic until additional space in the adolescent clinic became available. Adolescents transitioned to adult care after completing their matriculation exams or high school equivalency. The same physician, nurses, and counselors staffed both the adolescent clinic and pediatric clinic at the same clinical site. Funding for food, activities, and supplies was provided by local non-profit organization at a cost of $1.25 US dollars per adolescent per visit. Clinical personnel were permitted to subtract hours worked on weekends from their regular workweek hours during the month. Many caregivers do not accompany the adolescents to the weekend adolescent clinic limiting their availability for participation in the study.
Study design:
Sampling:
We used purposeful sampling to recruit adolescents in both the pediatric and adolescent clinics who were retained/not retained in care, and those virally suppressed/not virally suppressed. Viral suppression was defined as < 400 HIV-1 copies/ml at the most recent blood draw. Retention in care was defined as one clinic visit or pharmacy refill in the preceding 6 months.
Recruitment:
Study participants were recruited in person by a research assistant (author TS) during their routine clinic visits from October 2015 to April 2016. Sample category was determined by the treating physician (author CC). Adult caregiver participants gave written consent to be in the research study. Adolescent participants ≥18 years old provided written consent to be in the research study, while those <18 years old assented and written consent was obtained from the primary caregiver (22-24).
Data Collection:
We introduced the research team and explained the purpose of the study to participants prior to initiating the interview. We conducted in-depth, in-person, semi-structured interviews using open-ended questions to obtain information on barriers and facilitators to retention in care for adolescents living with HIV in South Africa. We used the same interview guide for adolescents attending the pediatric or adolescent clinics. Questions relevant to this analysis addressed the following topics: experience with clinic providers, structural barriers and facilitators to adherence and clinic attendance, experience with HIV status disclosure and stigma, and peer and other social support. Adolescents attending the adolescent clinic commented on their experiences in both types of clinics.
Interviews were conducted in person in a private space located on the grounds of the clinic. All interviews were conducted by a female research assistant trained in qualitative methods (author TS) who was not affiliated with the clinic. Interviews were audio-recorded, lasted between 60 and 90 minutes, and were conducted in isiZulu or English based on participant preference. Interviews were transcribed and translated into English as needed. Thirty-two interviews were transcribed by the research assistant and ten were transcribed by a consultant at the University of KwaZulu-Natal; both are bilingual in isiZulu and English. Each transcript was reviewed by the research assistant for quality and accuracy but were not reviewed by the study participants.
Data Analysis:
We used an inductive content analysis approach based on grounded theory that was derived from reviewing, coding, and interpreting the data. Author BCZ reviewed the first 10 transcripts and analyzed content to develop labels. He then created operational definitions and developed a codebook with selected illustrative quotes. Approximately 10% of interviews were double coded (authors BCZ and JEH) and any discrepancies were discussed until consensus was obtained. The codebook was then refined using an iterative process. Following the completion of the codebook, the remainder of transcripts were coded using Dedoose software (Version 8.0.42, (2018). Los Angeles, CA: SocioCultural Research Consultants, LLC @ www.dedoose.com). Using the coded data, categories were developed corresponding to important themes in the data. Category development included a combination of a priori categories (i.e. barriers to retention, facilitators to retention, social support) and categories that emerged from the data. The categories were further organized, definitions created, and evidence was provided using illustrative quotes from the research participants.
Ethics Statement
The Durban University of Technology Independent Review Committee, KwaZulu-Natal Department of Health and the Partners/Massachusetts General Hospital Research Ethics Board approved this protocol.
Results:
We interviewed 42 individuals including 28 adolescents and 14 caregivers. Participant characteristics are presented in Table 1. All of the adolescents were infected with HIV perinatally. Among the adolescents, 16 attended the adolescent clinic. They had a median age at HIV diagnosis of 12 (Interquartile range [IQR] 11.8 – 13.9) years and were receiving ART for a median of 66 (IQR 55 – 84) months. We interviewed 12 adolescents attending the pediatric clinic with a median age at HIV diagnosis of 11 (IQR 8.4 – 12.1) years and median of 55 (IQR 28 – 77) months of ART.
Table 1:
Participant Characteristics
| Adolescent clinic (N=16); n (%) or median (interquartile range) |
Pediatric clinic (N=12); n (%) or median (interquartile range) |
|
|---|---|---|
| Female | 9 (56%) | 5 (42%) |
| Adolescents | ||
| Less than 15 years old | 1 (6%) | 3 (25%) |
| Greater than 15 years old | 15 (94%) | 9 (75%) |
| Retained in care | 15 (94%) | 10 (83%) |
| Virally suppressed | 14 (88%) | 9 (75%) |
| Median age at HIV diagnosis (years) | 12 (11.8 – 13.9) | 11 (8.4 – 12.1) |
| Median months on ART | 66 (55 – 84) | 55 (28 – 77) |
| Caregivers | 6 | 8 |
| Caregiver as biological parent | 0 | 2 |
ART: Antiretroviral Therapy
Barriers to retention in care
Structural Barrier: Attending clinic during school hours
While attending the standard pediatric clinic, adolescents living with HIV and their caregivers reported a conflict between academic needs and health needs. Adolescents missed school frequently to attend the pediatric clinic for doctor visits, blood draws, or to collect medication. They waited in long queues and often did not return to school. Frequent clinic attendance had a negative impact on school performance, school attendance, and relationships with friends at school leading to decreased engagement in care.
“I was getting to school early the next day when I miss school - to catch up with my work, before the start of the day. I used to miss even exams or tests sometimes when I had to come out to [pediatric] clinic for my visit. Sometimes the teacher won't allow to rewrite [the exam]” -18 year-old male currently attending the adolescent clinic
“She’s been doing well [in school], but last year was her first time failing her grade. She made an excuse that the teacher was saying, [that] she missed school so much when she has to come [to the clinic] for her pills and blood.” -Caregiver of 16 year-old female attending the pediatric clinic
“…each time she needs to come to clinic that means she is going to be late for school - because she starts at the clinic first, then goes to school. It becomes a norm and known to other kids that each month she is going to be late because she starts at the clinic. Even when they don't know why, but they notice [that] there is something she is doing at the clinic. That somehow, has some effect on the child.” -Caregiver of 16 year-old female currently attending the adolescent clinic describing the time in the pediatric clinic
Conversely, other adolescents living with HIV reported infrequently visiting the clinic in order to remain in school. They only briefly attended the pediatric clinic for scheduled blood draws. These adolescents had limited time with clinicians, counselors, and support services and were less engaged in care.
“[Pediatric Clinic] was not a nice experience, coming with adults. Those moms there shouting, ‘Don't jump the queue!’ Long queues. [You] sit there for a long time. My friends were not even there. It was boring. I started to hate coming to clinic. It was not a good experience for me.“ -24 year-old female currently attending the adolescent clinic
“…when you come during the week, the queue is long and takes time and you don’t have to go to school.” -18 year-old male currently attending the adolescent clinic
“I collect the treatment. She only comes if she has to have her blood drawn or when schools are closed.” -Caregiver of 13 year-old adolescent attending the pediatric clinic
Psychosocial Barrier: Disclosure to others
Participants reported difficulty in disclosing their HIV status to friends, girlfriends, and boyfriends, especially when they felt that relationships were temporary and may end in conflict. This situation magnified internalized stigma and fear that their HIV status would be discussed with others without permission. This lead to superficial relationships with peers and increased social isolation. The decreased social support contributed to decreased engagement in care.
“None of my friends know [my HIV status]. I prefer keeping it as my secret. Friends have too much talk. Sometimes when you are not on good terms with them, they gossip.” -16 year-old female attending the pediatric clinic
“It’s scary but it’s not easy. It’s just that, we as the youth, especially for us as boys, it’s difficult to find a girlfriend. You date for 2 months then have to disclose to her. Then you date for 2 more months and break up. Then you’ll find another one, you’ll have to disclose to that one too. That is dangerous.” -21 year-old male currently attending the adolescent clinic
On conversations with school friends, a participant said: “We don't talk about personal stuff, only school things.” -17 year-old male currently attending the adolescent clinic
Psychosocial barrier: Conflict with clinical staff
Participants who were not retained in care often missed an appointment and fearing the response from the clinical staff, did not return to care.
“I forgot once to come and fetch them, and I was scared [the clinical staff] here would shout at me. That how it’s started. I ended up not coming at all.” -16 year-old female not retained in care
Facilitators to retention in care
Structural facilitator: After-school clinic hours
Participants from the adolescent clinic reported that after-school clinic hours allowed them to attend school without making excuses for absences and without experiencing stigma of missing school regularly. It also allowed them to avoid frequently missing important lessons or exams. Additionally, adolescents could attend clinic regularly. They therefore received the benefits of clinical services, routine clinical monitoring, and improved relationships with clinical staff.
“I was not missing school during [adolescent clinic] days and I was missing a lot during [pediatric] clinic.” -24 year-old female currently attending the adolescent clinic
“I used to come here first thing in the morning in my uniform and they serve me first. I go home, leave my pills, get a taxi, and go to school a bit late; and my friends used to ask me why I’m late? I used to lie and say I was not feeling well and started at the clinic. I hated doing that. Sometimes I just don’t go to school after collecting my pills.” On how this changed since attending the adolescent clinic: “I’m always present at school… I don’t have to think about lies anymore and think of things to say to my friends about my whereabouts.” -16 year-old female currently attending the adolescent clinic
Psychosocial Facilitator: Peer Support
Adolescents attending the adolescent-friendly clinic reported that regular interactions with peers were encouraging, enjoyable, and supportive. These personal connections encouraged adolescents to attend regularly and look forward to attending the clinic.
“I enjoy very much when I come [to the adolescent clinic]. We enjoy each other’s company. We talk about a lot of things when we are together. We open and pour all out our issues and problems and come up with solutions.” -15 year-old female currently attending the adolescent clinic
“I like that fact that everyone is open. You feel free to share all you want to share. You just enjoy to be around [peers.]” -17 year-old female currently attending the adolescent clinic
“Since I joined [the adolescent clinic] this year, [I have] seen that I am not the only 16 year-old who has HIV. All along since I found out about my [HIV] status, I was thinking it [was] written all over my back, that I have HIV. I was having that stigma; that everyone knows and they can see, even when they are a mile away. But joining [the adolescent clinic] was nice, [I] met lot of people [names of clinic members, then names members of staff] everyone is just nice, giving us advice about our lives…” -16 year-old female currently attending the adolescent clinic
“[The adolescent clinic] is a place where teenagers meet, chat, and solve their problems. Things can be shared in the group freely without being scared of be shouted at by the [elders].” -18 year-old male currently attending the adolescent clinic
Psychosocial Facilitator: Connection with Clinical Staff
Having adolescent-friendly hours, outside of regular school time, allowed for adolescents to be more engaged in their care while spending more time with the clinical staff. Adolescents were no longer are bound by the strict weekday clinic hours and could attend clinic regularly and for longer periods of time. This situation allowed adolescents to receive necessary health and psychosocial services and develop stronger relationships with the clinical staff.
“[At the pediatric clinic] there was no one who had time to ask you what was going on in your life. They only asked you about your health, not how your life as a whole was going. [The adolescent clinic] helped me a lot because I could talk about anything with [names doctor and counselors].” -21 year-old male currently attending the adolescent clinic.
“When you [are] coming into the [adolescent] clinic you know that you are going to meet friendly people who are supportive, so you look forward to it.” -18 year-old female currently attending the adolescent clinic
“The [adolescent] clinic is what helped me because if it wasn’t for the [adolescent] clinic I’d always just come here on a Thursday to collect treatment and go home. Maybe I’d be on drugs by now or involved in other things. The [adolescent] clinic is where you get to voice your true feelings.” -21 year-old male currently attending the adolescent clinic.
Adolescents attending the standard pediatric clinic (which was in the same facility with the same clinical staff as the adolescent clinic) did not have the same positive attitude toward the clinical staff and offered more matter-of-fact reasons for attending the clinic.
“I used to attend [the pediatric clinic]. We’d just come and join the long lines that were here, see the doctor who would check to see if there was anything wrong with you, thereafter go to the pharmacy for your treatment, then go home.” -21 year-old male currently attending the adolescent clinic
“At the [pediatric] clinic they treat me well, like any other people who attend clinic.” -16 year-old female attending pediatric clinic
“Its close home and the nurses are okay.” -16 year-old female attending the pediatric clinic
“There is nothing much I like. It's just that it's a must for me to come because there is something that brings me life - that I must fetch [my medication].” -17 year-old male attending the pediatric clinic
Discussion:
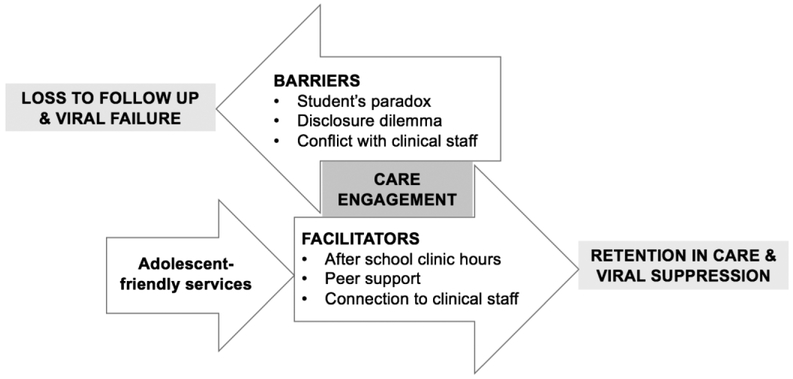
Adolescents living with HIV face significant barriers to successful long-term HIV treatment (19). In this qualitative assessment of adolescents living with HIV and attending standard pediatric care or adolescent-friendly services, we found that attending clinic during school hours is a major structural barrier to retention in care. Conflict between attending school and attending clinic creates the student’s paradox limiting retention in care. In addition, we found that disclosure and social isolation are psychosocial barriers to retention in care for adolescents living with HIV. Fear of disclosure to peers leads to superficial relationships and lack of peer support contributing to the disclosure dilemma. Adolescents often fear the response of the clinical staff after short-term lapses in adherence or missed appointments leading to long-term disengagement in care. Having an adolescent-friendly clinic with after-school hours, availability of peer discussion groups, and a closer connection to clinical staff facilitated retention in care as illustrated by Figure 1.
Figure 1:
Barriers and Facilitators to Retention in Care for Adolescents Living with HIV
For adolescents living with HIV, the balance between health and education is disrupted leading to either disengagement in care or poor academics - a process we are calling the student’s paradox. With access to ART, most school-aged children living with HIV are healthy enough to be enrolled in school (25, 26). However, a study of school-aged children living with HIV in Botswana found that 60% miss school at least one day per month and have more school problems than uninfected children (26). These children reported that missing school due to medical appointments was disruptive to their learning and affected their school performance (26). Students in our study who attend the weekday standard pediatric clinic similarly miss school frequently and suffer both academically and socially. On the other hand, students who miss clinic appointments to attend school do not receive regular clinical care, do not benefit from peer support, and do not benefit from improved connections to clinical staff. Adolescents who attend clinic outside of school hours in the adolescent clinic do not have to face this student’s paradox, thus allowing them to receive both the necessary education in school without frequent absences, as well as allowing attendance at the clinic for clinical services, monitoring, and more time with the clinical staff. Avoiding the student’s paradox could explain the improved retention in care seen in adolescents living with HIV who attend clinic after school hours and may improve school performance (19, 20).
The disclosure dilemma, where adolescents do not disclose their HIV status to their friends, results in superficial relationships with peers, increases social isolation, and makes individuals living with HIV feel different from their peers. They feel that they are keeping a secret from their friends; therefore, they find it difficult to maintain close relationships. In a closed cohort of adolescents living with HIV, everyone is aware of each other’s HIV-positive status. This knowledge allows adolescents to be free and open to discuss concerns, similar life events, and problem solve with others of similar backgrounds. With everyone’s HIV status out in the open, HIV-related issues can be discussed openly, often for the first time. This opportunity creates deeper relationships with peers and decreases social isolation (27). During adolescence the feeling of belonging contributes to self-identity and well-being; however, with the disclosure dilemma, it becomes difficult to feel part of a group of friends (28). In the adolescent clinic, all belong to a similar peer group that can relate to each other’s life experiences. This peer support makes clinic more enjoyable, encouraging regular clinic attendance and retention in care.
Peer relationships within the adolescent clinic enable adolescents to address both normative developmental needs and HIV-related stigma and disclosure. Typical adolescent relationships are transient as the adolescents begin to determine their personalities and friendship circles (4, 29, 30). HIV-related stigma is high among school-aged children in sub-Saharan Africa (31). Adolescents fear the often-negative consequences of disclosure of their HIV-positive status to peers, and this fear leads to superficial relationships and social isolation (26). Having a group of peers who are also living with HIV, where disclosure is no longer a barrier, allows for deeper personal relationships and increases peer support (32). Improved peer support has been shown to improve self-esteem and viral suppression in a long-term group intervention for adolescents living with HIV in the United States (27). When there is regular scheduled contact with peers, adolescents have the added incentive to attend clinic. In addition, if the clinical visits are enjoyable, adolescents may look forward to attending, thus improving retention in care (17, 20).
Having supportive clinical staff trained in adolescent health is an important part of adolescent-friendly services (18, 20, 33, 34). Adolescents living with HIV often require multidisciplinary healthcare teams to address some of their unique clinical needs that include: confidentiality, reproductive health, mental health, adherence support, and education or vocational training (4). Consistent relationships with the same clinical staff can be facilitated by differentiated service delivery systems such as adolescent-friendly services. After-school clinic hours increases the time that adolescents spend with the clinical staff allowing for deeper relationships. By improving connections to and communication with the clinical staff, adolescents can access available services more freely and are more likely to address clinical problems and less likely to fear responses for short term adherence lapses. Improved connection to the clinical staff facilitates the detection of clinical and psychosocial complications and can facilitate problem-solving discussions and interventions making it more likely that adolescents will remain engaged in care.
In our quantitative analysis, we found that adolescents in the adolescent-friendly clinic had higher levels retention in care and viral suppression compared to those in the standard pediatrics clinic (19). Establishing this clinic did require additional costs of $1.25 per adolescent per clinic and staff buy-in to work on weekends which could limit implementation in other settings. The strengths of this analysis include a comparison of two care delivery systems within an identical setting. However, there were some limitations with the study which include lack of randomization and that it only included a single adolescent-friendly site. These adolescent-friendly services address the disclosure dilemma by creating a peer network for support; however, it is important to note that this network does not solve the issue of disclosure to friends outside of this network or to intimate partners. Through qualitative interviews, we were able to explore modifiable structural and psychosocial barriers and facilitators to retention that are addressed by adolescent-friendly services. Other structural barriers, such as transportation and food security, were not seen in this analysis and may not be as amenable to change with the implementation of adolescent-friendly services and would likely need separate targeted interventions (35, 36).
Conclusion:
The student’s paradox, the disclosure dilemma and conflict with clinical staff are important barriers to care for adolescents living with HIV. Adolescent-friendly services that include after-school clinic hours, peer support, and trained clinical staff should be widely implemented to improve retention in care for adolescents living with HIV. Implementation of adolescent-friendly services on a larger scale will require prioritization of adolescent health within the department of health. More localized and short-term implementation of adolescent-friendly services can be achieved by engaging with non-profit organizations or philanthropists for alternate sources of funding and may require exploring differentiated staffing models to accommodate after hours clinics.
Acknowledgments
Funding: This study was funded by T32 AI 007433
Footnotes
Conflict of interest:
Brian Zanoni declares that he has no conflict of interest.
Thobekile Sibaya declares that she has no conflict of interest.
Chelline Cairns declares that she has no conflict of interest.
Jessica E. Haberer declares that she has no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the Durban University of Technology Independent Review Committee, KwaZulu-Natal Department of Health, and the Partners/Massachusetts General Hospital Research Ethics Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References:
- 1.Zanoni BA M; Buchan S; Katz I; Haberer J. Systematic Review and Meta-analysis of the Adolescent and Young Adult HIV Continuum of Care in South Africa: The Cresting Wave. BMJ Global Health. 2016(1 (3) e000004; DOI: 10.1136/bmjgh-2015-000004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Denison JA, Packer C, Stalter RM, Banda H, Mercer S, Nyambe N, et al. Factors Related to Incomplete Adherence to Antiretroviral Therapy among Adolescents Attending Three HIV Clinics in the Copperbelt, Zambia. AIDS Behav. 2017. [DOI] [PubMed] [Google Scholar]
- 3.Hogwood J, Campbell T, Butler S. I wish I could tell you but I can't: adolescents with perinatally acquired HIV and their dilemmas around self-disclosure. Clin Child Psychol Psychiatry 2013;18(1):44–60. [DOI] [PubMed] [Google Scholar]
- 4.Koenig lJ, Nesheim S, Abramowitz S. Adolescents with perinatally acquired HIV: emerging behavioral and health needs for long-term survivors. Curr Opin Obstet Gynecol 2011;23(5):321–7. [DOI] [PubMed] [Google Scholar]
- 5.Maskew M, Brennan AT, MacPhail AP, Sanne IM, Fox MP. Poorer ART outcomes with increasing age at a large public sector HIV clinic in Johannesburg, South Africa. J Int Assoc Physicians AIDS Care (Chic). 2012;11(1):57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evans D, Menezes C, Mahomed K, Macdonald P, Untiedt S, Levin L, et al. Treatment outcomes of HIV-infected adolescents attending public-sector HIV clinics across Gauteng and Mpumalanga, South Africa. AIDS Res Hum Retroviruses. 2013;29(6):892–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mutevedzi PC, Lessells RJ, Rodger AJ, Newell ML. Association of age with mortality and virological and immunological response to antiretroviral therapy in rural South African adults. PLoS One. 2011;6(7):e21795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nglazi MD, Kranzer K, Holele P, Kaplan R, Mark D, Jaspan H, et al. Treatment outcomes in HIV-infected adolescents attending a community-based antiretroviral therapy clinic in South Africa. BMC Infect Dis 2012;12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laher F, Hornschuh S, Otwombe K, Mohapi L, Violari A, Gray G. Outcomes of adolescents and young adults receiving antiretroviral therapy in Soweto, South Africa. 7th IAS Conference on HIV Pathogenesis and Treatment Abstract no MOPE056; 2013; Kuala Lumpur, Malaysia. [Google Scholar]
- 10.Davies MA, Stinson K, Technau K, Phiri S, Rabie H, Wellington M, Giddy J,R, Mofenson L, Moultrie H, editor Outcomes of Perinatally HIV-infected Adolescents on Antiretroviral Therapy in Southern Africa. Conference on Retrovirology and Opportunistic Infections (CROI) Abstract no: 930; 2014; Boston, MA. [Google Scholar]
- 11.Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDS. 2014;28(3):128–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davies MA, Tsondai P, Tiffin N, Eley B, Rabie H, Euvrard J, et al. Where do HIV-infected adolescents go after transfer? - Tracking transition/transfer of HIV-infected adolescents using linkage of cohort data to a health information system platform. Journal of the International AIDS Society. 2017;20(Suppl 3):16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ryscavage P, Anderson EJ, Sutton Sh, Reddy S, Taiwo B. Clinical outcomes of adolescents and young adults in adult HIV care. J Acquir Immune Defic Syndr. 2011;58(2):193–7. [DOI] [PubMed] [Google Scholar]
- 14.Fish R, Judd A, Jungmann E, O'Leary C, Foster C. Mortality in perinatally HIV-infected young people in England following transition to adult care: an HIV Young Persons Network (HYPNet) audit. HIV Med. 2014;15(4):239–44. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Making health services adolescent friendly: Developing national quality standards for adolescent-friendly health services In: Department of Maternal N, Child and Adolescent Health, editor. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 16.Teasdale CA, Alwar T, Chege D, Fayorsey R, Hawken MP, Abrams EJ. Impact of Youth and Adolescent Friendly Services on Retention of 10–24-Year-Olds in HIV Care and Treatment Programs in Nyanza, Kenya. J Acquir Immune Defic Syndr 2016;71(2):e56–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tanner AE, Philbin MM, Duval A, Ellen J, Kapogiannis B, Fortenberry JD, et al. "Youth friendly" clinics: considerations for linking and engaging HIV-infected adolescents into care. AIDS Care. 2014;26(2):199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pettitt ED, Greifinger RC, Phelps BR, Bowsky SJ. Improving health services for adolescents living with HIV in sub-Saharan Africa: a multi-country assessment. African journal of reproductive health. 2013;17(4 Spec No):17–31. [PubMed] [Google Scholar]
- 19.Zanoni BC, Sibaya T, Cairns C, Lammert S, Haberer JE. Higher retention and viral suppression with adolescent-focused HIV clinic in South Africa. PLoS One. 2017;12(12):e0190260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee L, Yehia BR, Gaur AH, Rutstein R, Gebo K, Keruly JC, et al. The Impact of Youth-Friendly Structures of Care on Retention Among HIV-Infected Youth. AIDS Patient Care STDS. 2016;30(4):170–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray KR, Dulli LS, Ridgeway K, Dal Santo L, Darrow de Mora D, Olsen P, et al. Improving retention in HIV care among adolescents and adults in low- and middle-income countries: A systematic review of the literature. PLoS One. 2017;12(9):e0184879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zuch M, Mason-Jones AJ, Mathews C, Henley L. Changes to the law on consent in South Africa: implications for school-based adolescent sexual and reproductive health research. BMC Int Health Hum Rights. 2012;12:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strode A, Slack C, Essack Z. Child consent in South African law: implications for researchers, service providers and policy-makers. S Afr Med J. 2010;100(4):247–9. [DOI] [PubMed] [Google Scholar]
- 24.South African Marketing Research Association (SAMRA). Guideline for Research with Children in South Africa. In: Research M, editor. Johannesburg, South Africa: SAMRA; 2015. [Google Scholar]
- 25.Cohen J, Reddington C, Jacobs D, Meade R, Picard D, Singleton K, et al. School-related issues among HIV-infected children. Pediatrics. 1997;100(1):E8. [DOI] [PubMed] [Google Scholar]
- 26.Anabwani G, Karugaba G, Gabaitiri L. Health, schooling, needs, perspectives and aspirations of HIV infected and affected children in Botswana: a cross-sectional survey. BMC Pediatr. 2016;16:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Funck-Brentano I, Dalban C, Veber F, Quartier P, Hefez S, Costagliola D, et al. Evaluation of a peer support group therapy for HIV-infected adolescents. Aids. 2005;19(14):1501–8. [DOI] [PubMed] [Google Scholar]
- 28.Menon A, Glazebrook C, Campain N, Ngoma M. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. J Acquir Immune Defic Syndr. 2007;46(3):349–54. [DOI] [PubMed] [Google Scholar]
- 29.Nozyce ML, Lee SS, Wiznia A, Nachman S, Mofenson LM, Smith ME, et al. A behavioral and cognitive profile of clinically stable HIV-infected children. Pediatrics. 2006;117(3):763–70. [DOI] [PubMed] [Google Scholar]
- 30.Cohen HJ, Papola P, Alvarez M. Neurodevelopmental abnormalities in school-age children with HIV infection. J Sch Health. 1994;64(1): 11–3. [DOI] [PubMed] [Google Scholar]
- 31.Maughan-Brown B, Spaull N. HIV-related discrimination among grade six students in nine Southern African countries. PLoS One. 2014;9(8):e102981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Midtbo V, Shirima V, Skovdal M, Daniel M. How disclosure and antiretroviral therapy help HIV-infected adolescents in sub-Saharan Africa cope with stigma. African journal of AIDS research : AJAR. 2012;11(3):261–71. [DOI] [PubMed] [Google Scholar]
- 33.Dickson KE, Ashton J, Smith JM. Does setting adolescent-friendly standards improve the quality of care in clinics? Evidence from South Africa. Int J Qual Health Care. 2007;19(2):80–9. [DOI] [PubMed] [Google Scholar]
- 34.Berg-Kelly K. Adolescent-friendly services. Acta paediatrica (Oslo, Norway : 1992). 2003;92(11):1241–2. [DOI] [PubMed] [Google Scholar]
- 35.Geng EH, Nash D, Kambugu A, Zhang Y, Braitstein P, Christopoulos KA, et al. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep 2010;7(4):234–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, Gross R, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156(11):817–33, W-284, W-5, W-6, W-7, W-8, W-9, W-90, W-91, W-92, W-93, W-94. [DOI] [PMC free article] [PubMed] [Google Scholar]