Chronic sleep disturbance is a global pandemic with two-thirds of individuals failing to obtain the recommended 7–9 hours of sleep each night [1]. Further, up to 10% of people meet criteria for clinical insomnia [2]. Unlike sleep deprivation (shortened sleep due to external restriction of the opportunity to sleep—e.g., staying up late to meet a deadline), clinical insomnia is the difficulty initiating or maintaining sleep or the experience of non-restorative sleep that is present despite the effort to sleep. These difficulties are accompanied by daytime impairment for at least 3 days per week for 3 months [3]. Given the heterogeneity of the diagnostic criteria for insomnia [4] and its varied operationalizations (e.g., insomnia as a symptom vs. a diagnosis) [5], for the purpose of this paper, the term sleep disturbance will be used to describe both the clinical and subclinical experience of insufficient and/or poor sleep despite attempts to sleep.
The average adult spends 25–30 years of one’s life asleep. As such, this time-consuming activity unlikely serves a single and unimportant function for wellbeing. Indeed, inadequate sleep is linked to increased risk of cancer [6], Alzheimer’s disease [7], diabetes [8], cardiovascular disease [9], psychological disorders (e.g., depression, anxiety) [10], and lower life span via motor vehicle accidents [11] and suicide [12]. Despite the incidence and grave consequences of sleep disturbance, the majority of people who report insufficient and/or poor sleep remain unhelped by the most commonly used treatments, namely prescription and over-the-counter sleep aids (e.g., sedative hypnotics such as sleeping pills). Meta-analyses indicate that pharmacological treatments for insomnia confer no objective benefit (measured via polysomnography) compared to placebo [13]. Sedative hypnotics are also associated with daytime residual effects, with increases in the risks for falls, fractures, and traumatic brain injury, particularly in older adults [14].
Results from pharmacological studies may be unsurprising given that the underlying factors that contribute to sleep disturbance are not targeted by this treatment approach. Psychobehavioral factors such as poor sleep hygiene (e.g., irregular bed and wake times, excessive caffeine and/or alcohol consumption) and cognitive processes (e.g., rumination) that maintain psychophysiological arousal are primary risk factors for sleep disturbance [15]. Thus, the most effective treatments for insomnia are psychological and behavioral interventions that incorporate varied treatment components including stimulus control, sleep restriction, relaxation, and cognitive therapy [16,17].
Cognitive behavioral therapy for insomnia (CBT-I) is one of the most effective treatments for insomnia and is recommended as first-line treatment [18]. However, additional treatment approaches are needed for the up to 25% of individuals who do not respond to CBT-I or who experience only partial symptomatic relief [19]. Also, CBT-I and similar clinical interventions are not readily available to patients because they require treatment from therapists with specialized training and involve time-intensive sessions that may not be covered by insurance [20]. They are also intended for patients with clinical insomnia. Collectively, these considerations support the need for additional or complementary treatments that are accessible, affordable, and effective for the treatment of insomnia and subclinical sleep disturbance, with a focus on prevention of insomnia and associated consequences.
Etiological model of sleep disturbance
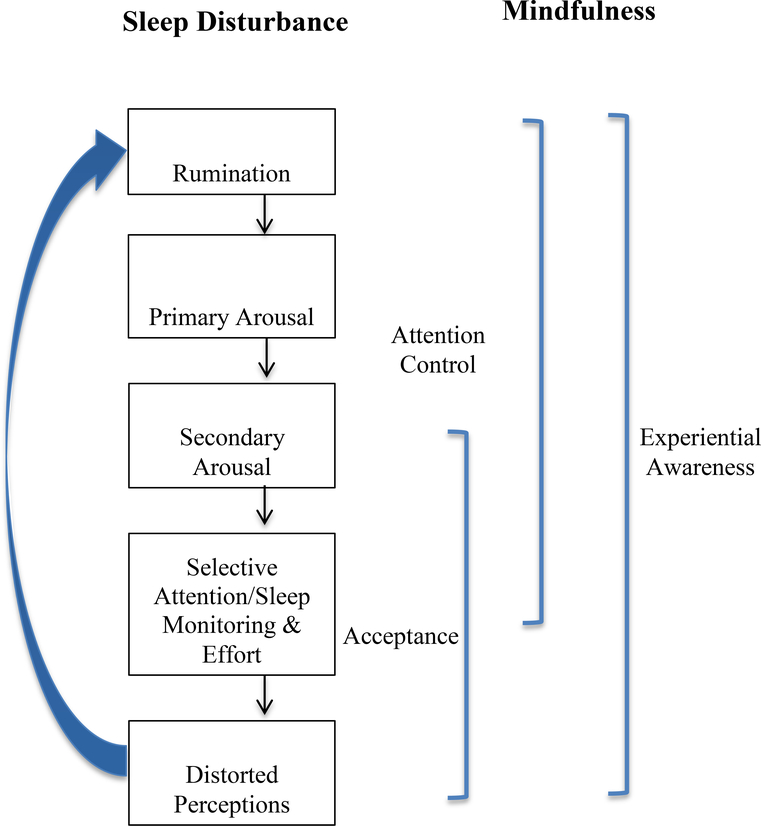
Sleep disturbance is thought to be initiated and perpetuated by the following sequential cognitive and behavioral processes: (1) Excessive daytime and nighttime rumination [21] 2) Primary arousal (i.e., initial negative appraisal about daytime consequences of poor sleep that results in distress and physiological activation)—”If I don’t sleep tonight, I’m going to fail at my job tomorrow and be fired.” [22]; (3) Secondary arousal (i.e., the negative secondary or metacognitive evaluation or judgment of initial (primary) arousal, which leads to continuing distress and physiological activation)—”I hate how I’m feeling and shouldn’t be feeling this way.” [23]; (4) Excessive monitoring of and selective attention to internal (e.g., bodily sensations) and/or external (e.g., clock) sleep cues that are either consistent or inconsistent with falling asleep [22]. Hand in hand with selective attention is a dysfunctional perceived need for control and engagement in sleep effort (e.g., actively trying to sleep or increasing sleep opportunity) [24]; and (5) Distorted perceptions about sleep impairment (i.e., regularly overestimating sleep loss) [25]. Misperceptions of sleep deficit frequently lead to excessive negative cognitions about sleep thus fortifying a vicious cycle of sleep disturbance.
Theoretical framework for mindfulness and sleep disturbance
In Figure 1, we present an integrative etiological model of sleep disturbance from several cognitive and behavioral frameworks and demonstrate how processes that are core to the practice of mindfulness may target key risk factors for sleep disturbance [26]. The practice of mindfulness involves three core processes (experiential awareness, attentional control, and acceptance) that have the potential to target each of the risk factors for sleep disturbance. For example, mindfulness-based practices (e.g., breath-focused meditation, body scanning, sensory meditations) promote experiential awareness of a range of experiences including internal (e.g., thoughts, emotions, physiological sensations) and external stimuli (e.g., sights, sounds) (4). During these exercises, participants acquire skills in attentional control by focusing attention on the breath (sustained attention) and redirecting attention to this anchor whenever one’s thoughts wander (attention inhibition) [27,28]. Finally, participants learn to change their relationship to their experiences by learning to accept, rather than avoid or control negatively perceived thoughts, emotions, and physical sensations. Skills in acceptance are learned by non-judgmentally observing one’s thoughts, feelings, and physical sensations and by viewing such experiences as passing events, rather than facts [29].
Figure 1.
A model for the effects of mindfulness practice on cognitive and metacognitive risk processes for the development and maintenance of sleep disturbance.
Collectively, mindfulness practices target each of the cognitive and behavioral vulnerabilities associated with poor sleep (see Figure 1). Increased awareness of internal and external experiences (e.g., thoughts and behaviors) should target each of the processes that contribute to the maintenance of sleep disturbance: (1) Rumination; (2) Primary arousal; (3) Secondary arousal; (4) Sleep monitoring/selective attention and effort; and (5) Distorted perceptions. Attentional control should enable individuals to disengage from negative thoughts and/or beliefs about sleeplessness by disrupting selective attention toward internal/external sleep-related threat cues. Thus, skills in attentional control should target processes (1)-(4) above.
Finally, skills in acceptance should foster a less contentious and more flexible relationship to one’s thoughts, emotions, and sensations by promoting the ability to approach, rather than avoid, and to engage with such experiences with equanimity instead of with judgment. Therefore, acceptance should target the following processes: (3) Secondary arousal; (4) Sleep monitoring/selective attention and effort; and (5) Distorted perceptions.
Mindfulness-based interventions and sleep
The literature on the effects of mindfulness for sleep is comprised primarily of investigations that have tested mindfulness-based stress reduction (MBSR) or mindfulness-based therapy for insomnia (MBTI), a tailored derivative of MBSR and CBT-I (for reviews see [30,31]. The most compelling evidence for the effects of MBIs for insomnia come from randomized controlled trials that have compared MBIs to rigorous comparison conditions. For example, in one study, MBSR demonstrated greater improvements in self-reported sleep quality and quantity compared to a pharmacotherapy (PCT) (Cohen’s d = −1.68; large within group effect) and showed comparable improvements on sleep efficiency, measured using sleep diary and actigraphy at post-intervention [32]. In another RCT, a three-arm trial comparing MBTI to MBSR and a self-monitoring condition, MBTI showed greater improvements in insomnia severity index scores (ISI) (d = 2.56 at 6-month follow-up; large within group effect); MBTI also showed higher treatment remission and response rates at 6-month follow-up [33]. Also in individuals with insomnia, Wong et al. demonstrated short-term benefits of an MBI compared to a rigorous psychoeducation control condition on post-intervention ISI scores (d = 0.36; small between group effect; p = 0.02). However, significant group differences were not found for remission rates and ISI scores did not differ between groups beyond a 5-month follow-up [34].
In addition to studies conducted in people with insomnia, several studies have examined MBIs in patients with chronic diseases and psychiatric conditions who also suffer from comorbid sleep disturbance (for Reviews see [31,35]). Two recent meta-analyses indicate that MBIs show promise for improving sleep outcomes across a range of patient populations [36,37]. Overall, evidence across randomized and non-randomized trials supports that MBIs are associated with significant improvements in self-reported total sleep time (TST) and sleep efficiency (SE) and decreased sleep onset latency (SOL) and waking after sleep onset (WASO) assessed with sleep diaries [36]. Among only RCTs that have compared MBIs to waitlist control or attention control groups, pooled results measured using standardized weight mean differences (SMD) did not support significant effect sizes for TST (SMD = .28; p = 0.30). Pooled results for effects of MBIs versus controls were significant for improved sleep quality using standardized sleep inventories (SMD = .85; medium effect size), and also reduced SOL (SMD = −.53; small effect size) and SE assessed with sleep diaries (SMD = 1.09; large effect size) [37]. Effects of MBIs on sleep parameters (e.g., SOL, SE, TST, WASO) using actigraphy or polysomnography were not significant across eight studies [36]. Collectively, conclusions from these meta-analyses are difficult to draw, however, due to high variability in: a) sleep parameters assessed; b) methodology (e.g., actigraphy, sleep diaries, standardized sleep inventories); c) treatment protocol (e.g., MBSR, MBTI, MBCT, # of sessions, etc.); d) single-arm vs. RCT design; e) type of comparison condition in RCT (e.g., waitlist, attention control, alternative active treatment); f) study sample (e.g., type and severity of chronic illness); and g) baseline levels of sleep disturbance. Further, the majority of extant research is comprised of predominantly uncontrolled studies [36].
Despite the heterogeneity among studies and the limited number of RCTs, theoretical considerations and burgeoning evidence support that MBIs (e.g., MBSR) or the combination of mindfulness with existing treatments for insomnia (e.g., MBTI) are promising treatments for sleep disturbance. One advantage to adding a mindfulness component to existing treatments such as CBT-I may be that it presents an additional treatment option for patients who relate more to acceptance-based approaches than to cognitive restructuring. Also, the benefits of mindfulness may generalize across greater domains of healthy functioning (e.g., reductions in somatic and/or mood symptoms associated with other comorbid conditions) that may directly or indirectly improve sleep. In sum, mindfulness appears to involve basic cognitive, affective, and behavioral processes that undergird sleep and a range of other psychological disorders and chronic diseases that are co-morbid with sleep dysfunction. Thus, mindfulness is a promising transdiagnostic approach for the treatment and prevention of sleep disturbance.
Future directions
A prevalent criticism of evidence-based psychological treatments for sleep disturbance (e.g., CBT-I) and also of MBIs is that they are not readily accessible, scalable, or affordable [26]. Although recent reviews suggest that alternative delivery (e.g., online vs. in person) [38] or minimal facilitator involvement [39] could be encouraging intervention directions, we are unaware of any published results from studies that have tested alternatives to in-person delivery of MBIs for sleep disturbance. Nonetheless, some researchers are working towards ensuring greater accessibility and scalability of MBIs. For example, Black and colleagues’ 6-week mindfulness awareness practices (MAPs) program, which outperformed a rigorous active control condition for sleep outcomes [40], is available to communities at low cost via either online or in-person delivery. Other studies are beginning to test alternative delivery (e.g., telephone-based) of MBIs for sleep outcomes [41].
Another area worthy of investigation is characterizing the mechanisms underlying the effects of MBIs for sleep outcomes. As an initial step, it is important to understand the specificity of the effects of MBIs for sleep disturbance (i.e., whether observed benefits are due to mindfulness rather than non-specific therapeutic elements such as alliance with instructor or group members). The Black and colleagues investigation offers some evidence that MBIs confer unique benefits above and beyond non-specific therapeutic components such as time, attention, group support, and expectancy [40]. Also, this study demonstrated that changes in sleep outcomes were correlated with changes in the non-reactivity scale of the five facet of mindfulness questionnaire in the MAPs group but not the active control group. This finding, along with converging evidence from other studies, support that cognitive (e.g., rumination, selective attention), emotional (e.g., affective symptoms, physiological arousal), and behavioral processes (e.g., clock monitoring, effortful attempts to control sleep) may underlie effects of MBIs on sleep outcomes [33,42,43]. Still, a definitive test of the mechanisms of MBIs for sleep would require several assessments of the hypothesized mediator (i.e., pre-intervention, during, and post-intervention) in order to detect the time course of intervention-related changes, and a demonstration that the mechanisms of MBIs differ from the mechanisms underlying the effects of attention control conditions [29]. Prior to this, however, additional work may be required to develop a clear conceptual model to guide the testing of treatment mechanisms. We and others have started to lay the necessary initial groundwork by integrating extant theory from cognitive and behavioral models with mindfulness-based concepts and processes (e.g., metacognition and secondary arousal) that are associated with sleep disturbance and that are targeted by MBIs [23,26].
Highlights.
Sleep disturbance is common and is associated with serious health consequences
Mindfulness practice may target several risk factors for sleep disturbance
More RCTs are needed to test efficacy of mindfulness interventions (MBIs) for sleep
Mechanisms of MBIs for sleep outcomes are poorly understood
MBIs for sleep disturbance need to be more affordable, accessible, and scalable
Acknowledgements
This work was supported by the National Institutes of Health [grant number K23AT009208]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest statement
Nothing declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Amanda J. Shallcross, New York University School of Medicine, amanda.shallcross@nyumc.org
Pallavi D. Visvanathan, Manhattan Mindfulness-Based Cognitive Behavioral Therapy
Sarah H. Sperber, New York University School of Medicine
Zoe T. Duberstein, New York University School of Medicine
References
References and recommended reading
• of special interest
•• of outstanding interest
Papers of particular interest, published within the period of review, have been highlighted as:
- [1].Walker MP: Why We Sleep. Scribner; 2017. [Google Scholar]
- [2].Singareddy R, Vgontzas AN, Fernandez-Mendoza J, Liao D, Calhoun S, Shaffer ML, Bixler EO: Risk factors for incident chronic insomnia: A general population prospective study. Sleep Med 2012, 13:346–53 doi: 10.1016/j.sleep.2011.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].American Psychiatric Association: DSM-V. American Psychiatric Publishing; 2013. [Google Scholar]
- [4].Roth T: Insomnia: Definition, prevalence, etiology, and consequences. J Clin Sleep Med 2007, 146:1387–1394 doi: 10.1378/chest.14-0970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ohayon MM, Reynolds CF: Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD). Sleep Med 2009, 10:952–60 doi: 10.1016/j.sleep.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Irwin M, Fortner M, Clark C, McClintick J, Costlow C, White J, Ancoli-Israel S, Gillin JC: Reduction of natural killer cell activity in primary insomnia and in major depression. Sleep Res 1995, 24:256. [Google Scholar]
- [7].Lim ASP, Kowgier M, Yu L, Buchman AS, Bennett DA: Sleep fragmentation and the risk of incident Alzheimer’s disease and cognitive decline in older persons. Sleep 2013, 36:1027–1032 doi: 10.5665/sleep.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Knutson KL, Van Cauter E: Associations between sleep loss and increased risk of obesity and diabetes. Ann Ny Acad Sci 2008, 1129:287–304 doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gupta S, Arnedt JT: Sleep and Cardiovascular Disease In Psychiatry and Heart Disease: The Mind, Brain, and Heart. Edited by Riba M, Wulsin L, Rubenfire M, Ravindranath D. Wiley-Blackwell; 2012:135–152. [Google Scholar]
- [10].Ohayon MM, Roth T: Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res 2003, 37:9–15 doi: 10.1016/S0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- [11].Léger D, Bayon V, Ohayon MM, Philip P, Ement P, Metlaine A, Chennaoui M, Faraut B: Insomnia and accidents: Cross-sectional study (EQUINOX) on sleep-related home, work and car accidents in 5293 subjects with insomnia from 10 countries. J Sleep Res 2014, 23:143–52 doi: 10.1111/jsr.12104. [DOI] [PubMed] [Google Scholar]
- [12].Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, Wallace R: Risk factors for late-life suicide: A prospective, community-based study. Am J Geriatr Psychiatry 2002, 10:398–406 doi: 10.1097/00019442-200207000-00006. [DOI] [PubMed] [Google Scholar]
- [13].Huedo-Medina TB, Kirsch I, Middlemass J, Klonizakis M, Siriwardena AN: Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: Meta-analysis of data submitted to the Food and Drug Administration. BMJ 2012,345 doi: 10.1136/bmj.e8343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Tom SE, Wickwire EM, Park Y, Albrecht JS: Nonbenzodiazepine sedative hypnotics and risk of fall-related injury. Sleep 2016, 39:1009–1014 doi: 10.5665/sleep.5742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Espie CA: Insomnia: Conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol 2002, 53:215–243 doi: 10.1146/annurev.psych.53.100901.135243. [DOI] [PubMed] [Google Scholar]
- [16].Morgenthaler T, Kramer M, Alessi C, et al. : Practice parameters for the psychological and behavioral treatment of insomnia: an update. An american academy of sleep medicine report. Sleep 2006, 29:1415–1419 doi: 10.1093/sleep/29.11.1415. [DOI] [PubMed] [Google Scholar]
- [17].Morin CM: Cognitive-behavioral therapy of insomnia. Sleep Med Clin 2006, 1:375–386 doi: 10.1016/j.jsmc.2006.06.008. [DOI] [Google Scholar]
- [18].NIH CS: NIH State-of-the-Science Conference Statement on manifestations and management of chronic insomnia in adults. NIH Consens State Sci Statements 2005. doi:2005-00025-STMT. [PubMed] [Google Scholar]
- [19].Morin CM, Culbert JP, Schwartz SM: Nonpharmacological interventions for insomnia: A meta-analysis of treatment efficacy. Am J Psychiatry 1994, 151:1172–1180 doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- [20].Perlis ML, Smith MT: How can we make CBT-I and other BSM services widely available? J Clin Sleep Med 2008, 4:11–13. [PMC free article] [PubMed] [Google Scholar]
- [21].Carney CE, Harris AL, Moss TG, Edinger JD: Distinguishing rumination from worry in clinical insomnia. Behav Res Ther 2010, 48:540–6 doi: 10.1016/j.brat.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Harvey AG: A cognitive model of insomnia. Behav Res Ther 2002, 40:869–894 doi: 10.1016/S0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- [23].Ong JC, Ulmer CS, Manber R: Improving sleep with mindfulness and acceptance: A metacognitive model of insomnia. Behav Res Ther 2012, 50:651–60 doi: 10.1016/j.brat.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Espie CA, Broomfield NM, MacMahon KMA, Macphee LM, Taylor LM: The attention-intention-effort pathway in the development of psychophysiologic insomnia: A theoretical review. Sleep Med Rev 2006, 10:215–245 doi: 10.1016/j.smrv.2006.03.002. [DOI] [PubMed] [Google Scholar]
- [25].Harvey AG, Tang NKY: (Mis)perception of sleep in insomnia: A puzzle and a resolution. Psychol Bull 2012, 138:77–101 doi: 10.1037/a0025730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shallcross AJ, Visvanathan PD: Mindfulness-based cognitive therapy for insomnia In Mindfulness-Based Cognitive Therapy: Innovative Applications. Edited by Eisendrath SJ. Springer International Publishing; 2016:19–29. Presents a theoretical model and summarizes evidence for the use of mindfulness-based cognitive therapy (MBCT) as a treatment for insomnia. Evidence indicates that MBCT is a promising intervention for improving sleep outcomes, especially in those with a history of recurrent major depression and/or individuals with elevated depressive symptoms. [Google Scholar]
- [27].Jha AP, Krompinger J, Baime MJ: Mindfulness training modifies subsystems of attention. Cogn Affect Behav Neurosci 2007, 7:109–119 doi: 10.3758/CABN.7.2.109. [DOI] [PubMed] [Google Scholar]
- [28].Tang Y-Y, Ma Y, Wang J, Fan Y, Feng S, Lu Q, Yu Q, Sui D, Rothbart MK, Fan M, Posner MI: Short-term meditation training improves attention and self-regulation. Proc Natl Acad Sci 2007, 104:17152–17156 doi: 10.1073/pnas.0707678104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Shallcross AJ, Troy A, Mauss IB: Regulation of Emotions Under Stress In Emerging Trends in the Social and Behavioral Sciences. Edited by Scott R, Kosslyn S. John Wiley & Sons, Inc; 2015:1–16. [Google Scholar]
- [30].Garland SN, Zhou ES, Gonzalez BD, Rodriguez N: The quest for mindful sleep: a critical synthesis of the impact of mindfulness-based interventions for insomnia. Curr Sleep Med Reports 2016, 2:142–151 doi: 10.1007/s40675-016-0050-3. Summarizes theory behind mindfulness meditation as an intervention for sleep disturbance and reviews the body of literature exploring this relationship. The authors find a significant impact of mindfulness interventions on sleep quality, particularly in studies that target sleep as a primary outcome. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Winbush NY, Gross CR, Kreitzer MJ: The effects of mindfulness-based stress reduction on sleep disturbance: A systematic review. Explor J Sci Heal 2007, 3:585–591 doi: 10.1016/j.explore.2007.08.003. [DOI] [PubMed] [Google Scholar]
- [32].Gross CR, Kreitzer MJ, Reilly-Spong M, Wall M, Winbush NY, Patterson R, Mahowald M, Cramer-Bornemann M: Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: A randomized controlled clinical trial. Explor J Sci Heal 2011, 7:76–87 doi: 10.1016/j.explore.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Ong JC, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt JK: A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep 2014,37:1553–1563. doi: 10.5665/sleep.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Wong SY, Zhang D, Li CC, et al. : Comparing the effects of mindfulness-based cognitive therapy and sleep psycho-education with exercise on chronic insomnia: A randomised controlled trial. Psychother Psychosom 2017, 86:241–253 doi: 10.1159/000470847. A randomized controlled trial evaluating the effects of mindfulness-based cognitive therapy compared to a sleep psycho-education with exercise control group for insomnia. MBCT was more beneficial in the short-term with no significant benefit compared to control at an 8-month followup. [DOI] [PubMed] [Google Scholar]
- [35].Zeichner SB, Zeichner RL, Gogineni K, Shatil S, Ioachimescu O: Cognitive behavioral therapy for insomnia, mindfulness, and yoga in patients with breast cancer with sleep disturbance: A literature review. Breast Cancer Basic Clin Res 2017, 11. doi: 10.1177/1178223417745564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kanen JW, Nazir R, Sedky K, Pradhan BK: The effects of mindfulness-based interventions on sleep disturbance: A meta-analysis. Adolesc Psychiatry 2015, 5:105–115 doi: 10.2174/2210676605666150311222928s. A meta-analysis of the effects of mindfulness-based interventions (MBIs) for sleep disturbance. MBIs are efficacious for sleep outcomes measured using questionnaires and sleep diaries. Minimal evidence exists for effects on outcomes measured using polysomnography or actigraphy. Conclusions are based on a minimal number of randomized controlled trials and are limited by heterogeneity of samples, design, and methods across studies. [DOI] [Google Scholar]
- [37].Gong H, Ni C-X, Liu Y-Z, Zhang Y, Su W-J, Lian Y-J, Peng W, Jiang C-L: Mindfulness meditation for insomnia: A meta-analysis of randomized controlled trials. J Psychosom Res 2016, 89:1–6 doi: 10.1016/j.jpsychores.2016.07.016. A meta-analysis of randomized controlled trials that investigate the effects of mindfulness meditation (MM) for insomnia. MM may mildly improve total wake time, sleep onset latency, sleep quality, and sleep efficiency. MM can serve as an auxiliary treatment to medication for sleep complaints. [DOI] [PubMed] [Google Scholar]
- [38].Toivonen KI, Zernicke K, Carlson LE: Web-based mindfulness interventions for people with physical health conditions: Systematic review. J Med Internet Res 2017, 19:e303 doi: 10.2196/jmir.7487. Reviews evidence for web-based mindfulness-based interventions (MBIs) in individuals with physical health conditions. Evidence supports that web-based MBIs may be helpful in alleviating symptom burden, particularly when interventions are tailored for specific symptoms. There was no evidence of differences between synchronous versus asynchronous or facilitated versus self-directed web-based MBIs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Fish J, Brimson J, Lynch S: Mindfulness interventions delivered by technology without facilitator involvement: What research exists and what are the clinical outcomes? Mindfulness 2016, 7:1011–1023 doi: 10.1007/s12671-016-0548-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR: Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances. JAMA Intern Med 2015, 175:494–501 doi: 10.1001/jamainternmed.2014.8081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Spruill TM, Reynolds HR, Dickson VV, et al. : Telephone-based mindfulness training to reduce stress in women with myocardial infarction: Rationale and design of a multicenter randomized controlled trial. Am Heart J 2018, 202:61–67 doi: 10.1016/j.ahj.2018.03.028. A randomized controlled trial investigating the efficacy of a community-accessible mindfulness-based intervention (MBI) on sleep disturbance in older adults, as compared to a sleep hygiene education control. The MBI demonstrated superior benefits for sleep quality immediately following the intervention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Ong JC, Shapiro SL, Manber R: Mindfulness meditation and cognitive behavioral therapy for insomnia: A naturalistic 12-Month follow-up. Explor J Sci Heal 2009. 5:30–6 doi: 10.1016/j.explore.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Ong JC, Shapiro SL, Manber R: Combining mindfulness meditation with cognitive-behavior therapy for insomnia: A treatment-development study. Behav Ther 2008. 39:171–82 doi: 10.1016/j.beth.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]