ABSTRACT
Integrated care has been postulated to result in improvements to diabetes outcomes, including reduced hospitalisation. The Diabetes Integrated Care Initiative (DICI) aimed to integrate primary, secondary and community diabetes care in East Cambridgeshire and Fenland (ECF). The aims of this study were to describe changes in care and hospitalisation rates over the first 3 years of the initiative, 2009–2012. The evaluation involved a mixed-methods approach, including a before-after design with controls from adjacent geographical areas and from patients without diabetes, alongside a 30-month ethnographic study including interviews with patients and health professionals. Over the three years, admission rates among patients with diabetes in the intervention area continued to grow. In fact, the increases in admissions in ECF were 7.4% (95% CI 5.2–9.2) and 45.5% (95% CI 42.5–48.5) greater than in the neighbouring areas of Huntingdonshire and Greater Cambridge, respectively. The rates of increase in diabetic foot, non-elective or other hospital admissions were not reduced. In summary, the DICI was not associated with improved diabetes care or reduced diabetes hospitalisation over the 3 years studied, despite substantial investment. While the principle of integration remains an ideal, linking different providers in ECF, especially those that are positioned between primary and secondary care, created barriers rather than bridges to better diabetes outcomes.
KEYWORDS : Diabetes, integrated care, hospital admission, HbA1c hypophysitis, encephalopathy
Background
Many new models of diabetes service delivery have been described.1–4 These include community-based ‘intermediate services’, which are established to reduce referrals to hospital diabetes clinics and their associated costs. These services are led by specialist nurses or by a general practitioner with a special interest.5-8 Evaluation of the outcomes of these models (including effects on hospitalisation, complications and death) has been remarkably limited. When part of a medical service, nurse-run clinics have been shown to improve blood pressure and dyslipidaemia in patients with diabetes.9 Furthermore, nurses using pre-defined protocols, whose work is integrated with medical services, appear to provide care for certain types of patients that is at least equivalent to that provided by typical diabetes clinics.10 Intermediate services, however, operate outside of medical clinics.
Some intermediate services have been associated with reductions in glycated haemoglobin (HbA1c)7 but it is, as yet, unknown whether such services are associated with any changes in hospitalisation rates. There are concerns that ‘intermediate’ care providers may fragment care, resulting in a loss of continuity for patients and a reluctance by primary care services to refer patients to more specialist services when needed.11
Integrated care, in which all health workers work closely together, independent of their organisational affiliation, to address the different needs of patients should theoretically be associated with improved outcomes.12–15 However, integrating pathways across potentially competing health organisations (horizontally integrated care) in the current English NHS has not been associated with improvements.16 We describe the degree of implementation of a rural integrated diabetes care approach comprised of three domains (hospital, general practice and community care), and its impact on hospitalisation rates and metabolic disease control, as well as feedback from patients and healthcare professionals.
The East Cambridgeshire and Fenland Diabetes Integrated Care Initiative
East Cambridgeshire and Fenland (ECF) is a largely rural region that includes several socio-economically deprived communities. There is no major hospital in ECF and the region is divided into the catchment areas for five different hospitals. Each hospital has its own specialist diabetes service with general diabetes clinics, complications clinics (including diabetes foot clinics), diabetes in pregnancy clinics and diabetes inpatient services. Structured type 1 diabetes education is provided by all hospital clinics, with two hospitals providing dose adjustment for normal eating (DAFNE) programmes. A separate intermediate service led by community-based diabetes specialist nurses was established in ECF in 2003 to support primary care and reduce hospital clinic referrals.6
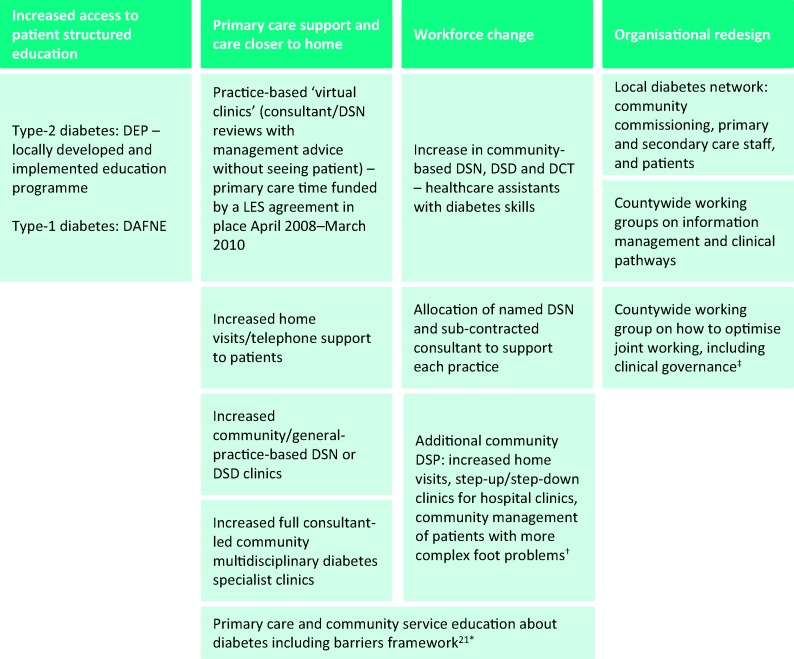
From April 2009, the intermediate service was replaced with a new Diabetes Integrated Care Initiative (DICI), which was funded by additional finance (£250,000 per annum), in an attempt to address continuing health disparities between different areas of the country.17 Although there were no changes in the organisational structures, the DICI included a number of new and enhanced activities designed to help the different diabetes services work together and to increase patient access to diabetes specialist care (Fig 1).17,18
Fig 1.
Components of the DICI. †Neuropathy, vascular impairment and/or deformity with heavy callus, advanced in-growing toenails and/or previous foot ulceration. *Most of the 17 general practices already had a lead -GP and/or practice nurse trained in diabetes management. ‡ Under the Sustainable Health Partnership (2010–2011 www.sustainablehealthcambs.nhs.uk/Workstreams/Diabetes.htm accessed 10/4/2013). DAFNE = dose adjustment for normal eating; DCT = diabetes care technician; DEP = diabetes education programme; DICI = Diabetes Integrated Care Initiative; DSD = diabetes specialist dietician; DSN = diabetes specialist nurse; DSP = diabetes specialist podiatrist; LES = Local Enhanced Service.
In broad terms, the DICI provided:
greater diabetes specialist care away from the hospital-based specialist services
greater within-practice diabetes specialist support for primary care
increased linkage with hospital diabetes specialists
increased access to patient diabetes education
a tool to assist practice nurses to assess and address barriers to care.18
The DICI team were able to access general-practice-based electronic records on site, but not from outside the practice.
The DICI ran alongside countywide initiatives that also involved the two other parts of the county: Greater Cambridge (Cambridge City and South Cambridgeshire) and Huntingdonshire. These initatives aimed to align information technology and diabetes referral pathways, and to encourage joint working (for example, there was a local enhanced service (LES) payment to GPs for joint patient reviews with specialists). Electronic data sharing between general practice and other health services (hospitals and community services) was not allowed despite this countywide work over the 3 years studied. Similarly, no long-term agreement was reached over joint working. No other major service changes occurred elsewhere during the study period, although Huntingdonshire gained an additional community DSN from 2008.
Methods
The process was evaluated using the Medical Research Council guidelines for evaluating complex interventions.19 Ethics approval was received from the National Research Ethics Service Committee – East of England (June 2011: 11/EE/0148).
Quantitative analysis
De-identified electronic Secondary Uses Service data from across Cambridgeshire were obtained for all hospitalisation and outpatient attendances between April 2007 (2 years before the DICI contract commenced) and March 2012. Practice, patient age, elective/non-elective status, and International Classification of Diseases (ICD10) and Health Related Group (HRG) codes were included in the dataset. Diabetes was considered to be present if the E10–E14 designations were coded in any ICD10 field, and as the primary cause of admission if coded in the first field. Diabetes foot was identified as the cause of admission upon the presence of the relevant HRG codes and diabetic ketoacidosis (DKA) upon the presence of relevant ICD10 codes.
Annual referral data for type-1 diabetes education programmes were obtained from Cambridge University Hospitals Foundation Trust (A Housden, personal communication). Collateral data were obtained from the Quality and Outcome Framework (QoF) database (www.gpcontract.co.uk/download), which provided both diabetes and overall population by area and QoF metrics on an annual basis.
Statistical analysis
The Mantel Haenszel test was used to compare the proportion of hospital episodes required by patients with diabetes in ECF with those in the other two areas in Cambridgeshire (Huntingdonshire and Greater Cambridge) in 2009 and 2012. Hospital episodes and outpatient attendances were compared before and after the commencement of the DICI, first between those with and without diabetes, and second, between the three Cambridgeshire areas. Changes over time were investigated by comparing the mean monthly number of hospital episodes or outpatient attendances before and after each month (constructed using a Poisson regression model)17 between April 2007 and March 2012. The regression models incorporated terms that described an annual sinusoidal pattern in the numbers of episodes to allow for residual seasonality. The modelling of potential confounders was completed by the inclusion of indicator variables for each week. Each monthly point shows the 95% confidence intervals (CIs) for the estimate of mean change.
Sensitivity analyses were conducted (i) excluding terms to describe an annual sinusoidal pattern in the number of hospital admissions; (ii) incorporating terms to describe an annual linear pattern in the number hospital admissions; and (iii) including dummy variables for days during Christmas and New Year bank holidays. These analyses identified insufficient change in the results to alter the conclusions.
All analyses were conducted in STATA [STATA/SE 11.0. StataCorp, Texas]. All tests were two tailed; p < 0.05 is taken as significant.
Qualitative analysis
Ethnographic field notes were collated from observations by social scientists. Semi-structured interviews, supplemented by more casual interactions, were carried out with 21 patients (in primary care (n = 7), DICI service (n =7), hospital multidisciplinary clinic (n =7)) and 20 healthcare professionals (10 DICI staff, 6 hospital staff (3 podiatrists, 1 consultant, 1 DSN and 1 DSD) across two hospitals, and with 4 primary care staff (2 practice nurses and 2 GPs) across 4 practices). The patients were purposively selected by age, gender, rural/semi-rural home address and some specific criteria (whether an individual has had diabetes for more than five years and has had a recent HbA1c test of >9% (>75 mmol/mol) or had any hospitalisation in the previous 12 months). Patients were asked to participate by a known health professional (2 declined and 2 were not contactable). Three healthcare professionals were not contactable. Most of the patients (17/21) were interviewed on two occasions at least 6 months apart to obtain insight into how care and perspectives changed. All interviews were conducted by an experienced social scientist. Each interview lasted 25–90 minutes and was recorded digitally. Patients were interviewed at home whenever possible in order to ensure that they felt at ease and were able to comment freely about their experiences.
A telephone survey was undertaken with ECF practice nurses (PN) from 14 out of the 16 general practices involved in DICI (one PN was excluded because she became a member of the DICI team). The survey covered use of a barriers framework,20 confidence with insulin management, referral to diabetes specialist services, access to specialist podiatry, and how closely the PN felt they were now working with the community diabetes team and local hospital diabetes services.
Interview data and ethnographic notes were transcribed and entered into NVivo 9 for analytical coding using a grounded theory approach.20 The datasets were cross-referenced for further refinement and corroboration.
Results
Between 2009 and 2011, the increase in number of patients diagnosed with diabetes was comparable across ECF (11.0% (9,052 to 10,051)), Greater Cambridge (9.6% (7,276 to 7,977)) and Huntingdonshire (13.5% (6,041 to 6,855)). The crude diabetes prevalence increased from 4.8% to 5.2%, 2.9% to 3.1% and 3.8% to 4.3%, respectively, during this time. Referrals to DAFNE changed from 10–14 per annum during the 2003–2009 period, to 25 in 2010 and 16 in 2011. Consultant virtual clinics occurred in 16 general practices: 23 clinics were performed in 2009 (when the LES was in place), 14 in 2010 and 9 in 2011.
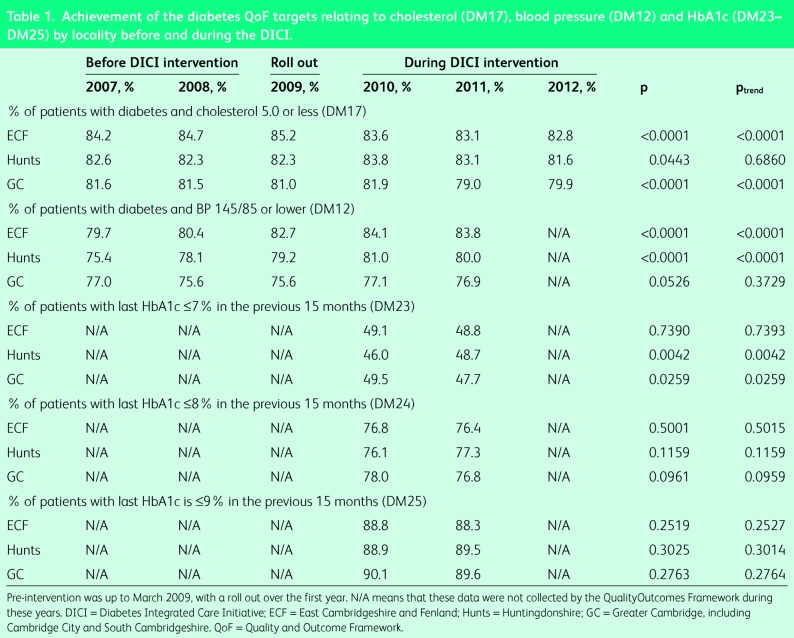
General practices in the three areas within the county had patients with similar glycaemia, blood pressure and cholesterol QoF scores at baseline (Table 1). There was no improvement in the achievement of diabetes QoF targets in ECF over the 5 years either overall or by individual QoF score.
Table 1.
Achievement of the diabetes QoF targets relating to cholesterol (DM17), blood pressure (DM12) and HbA1c (DM23–DM25) by locality before and during the DICI.
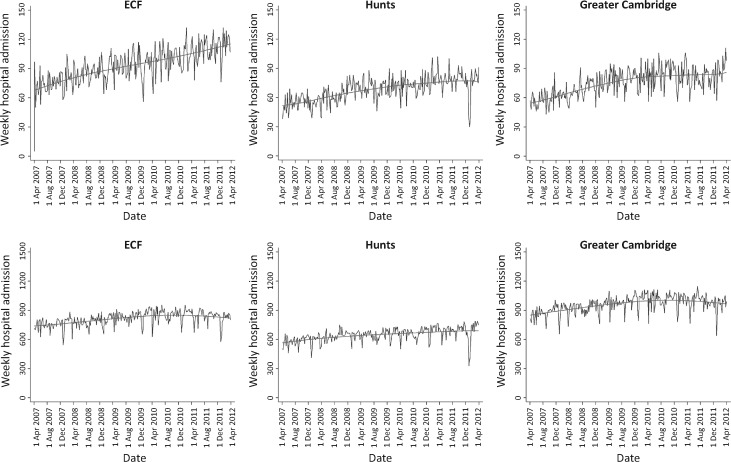
Fig 2 shows the weekly hospital episode rate. The proportion of admissions of those with diabetes increased in all three areas over the 3-year CISI period. The increase in admissions in ECF were substantially greater than those in Huntingdonshire (by 7.4% (95% CI 5.2–9.2)) and in Greater Cambridge (by 45.5% (95% CI 42.5–48.5)).
Fig 2.
Hospitalisations (number/week) among those with and without diabetes over the five years by area. Each plot is fitted with a LOWESS fit line.
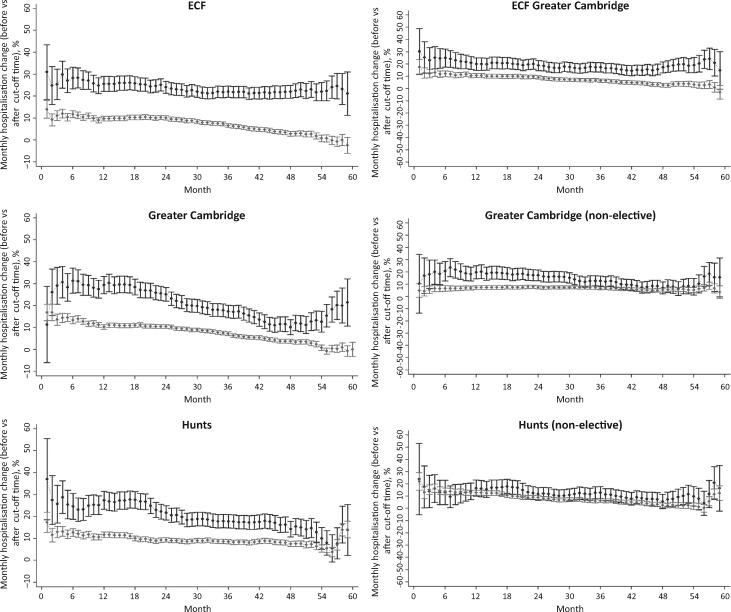
Fig 3 shows the monthly hospitalisation change overall and for non-elective admissions by area for those with and without diabetes. In Huntingdonshire and Greater Cambridge, but not in ECF, the monthly non-elective hospitalisation change became similar for patients with and without diabetes. In ECF, the difference in monthly change in hospitalisation between those with and without diabetes appears to widen after the introduction of the DICI. The difference between the areas was most marked in those aged 75+ years (Fig S1).
Fig 3.
Monthly percentage change in hospital admission rate (monthly hospital admission rate before and after each month) across areas for all patients and for non-elective patients. The plots on the left show all-caused hospitalisation; those on the right show non-elective hospitalisations. The black (upper) plots represent percentage change in hospital admissions for those with diabetes. The grey (lower) plots represent percentage change in hospital admissions for those without diabetes. Figures above 0% indicate that the mean monthly hospitalisation rate after the index month is greater than the mean hospitalisation rate before the index month. 95% confidence intervals are shown for each month.
Rates for DKA admissions, diabetic foot admissions and any admission with diabetes as the primary cause were comparable at baseline between the three areas. There were no significant reductions, and no differences compared with the other two areas, throughout the DICI in hospitalisation rates for diabetic foot, DKA or for diabetes as the primary cause of admission.
A reduction in integration between primary care and hospitals was reported by 6/14 PNs across the different hospital catchments, with a reciprocal increase in integration with community services reported by 8/14 PNs. All PNs reported referrals to the community DSN. Most PNs reported an increase in their confidence in the use of insulin (9/14, although one indicated a reduction in confidence) and 7/14 reported that they referred foot ulcers to the community DSP earlier than before.
The patients interviewed were aged 28–66 years and included 13 men and 8 women. One interviewee was of South Asian descent, all others were of British descent. Relevant quotes can be found in S2. Three relevant overarching themes emerged from the patient and healthcare professional interviews: the need for integration, continuity of care (including relationships) and tailored care.
Integration
Patients often spoke about their desire for integrated care. Among the majority of secondary care professionals and some patients however, there was a feeling that the intervention often increased barriers to direct access to hospital services rather than facilitating it. For example, in podiatry, it was said that an ‘extra layer into the referral pathway’ had been added (see HCP1 in S2). Patients expressed frustration with the delays caused by what they perceived of as new additional layers to their care, one describing the system as a ‘layer cake’ with ‘layers of care’ that ‘don't correspond properly’ (see patient 1 in S2).
Continuity of care
Across the interviews, it was common for patients to comment positively on the new multidisciplinary community clinic (for example, see patient 2 in S2). Such positive experiences provided the setting for, and were in part predicated on, the continuity of the DICI staff. The DICI was seen by many to provide a better level of personalised care than they had had access to previously (for example, see patient 3 in S2). This new continuity of patient experience was, however, negatively affected by a lack of functioning information-sharing systems, with the consequence that patients felt they became the ‘carrier’ of information between sites (for example, see patient 4 in S2).
Tailored care
Patients found the tailored nature of the DICI appealing because they felt that it put them, as individuals, at the centre of the various services (for example, see patient 5 in S2). In some instances, however, patients felt that the long-term systems of care were not responsive enough to changes in their condition (for example, see patient 6 in S2).
Discussion
The DICI was successfully implemented across ECF, with positive patient experiences, improved PN clinical confidence, and early reports of clinical benefit.17,18,21 However, over the 3 years studied, the DICI was associated with worsening rates of hospitalisation among those with diabetes. Reductions in hospitalisation (including for DKA) through greater integration are achievable within single providers (as seen in examples in the USA14,15) and with integrated insurance schemes (such as those studied in South Africa22). Similarly, significant improvements in diabetes care have occurred with multifaceted interventions,23 including disease management in the US24 and ‘integrated care’ in Germany,25 which can be associated with reductions in hospital costs.26 The English NHS does allow for such integrated approaches: it will permit a joint venture model (in which specialist diabetes and primary care services create a joint company to deliver diabetes care)3 or a prime contractor approach (in which one diabetes specialist service holds the contract and is accountable for other diabetes services). However, the impacts of these English NHS models on hospitalisation across the population served have not yet been published.
Conversely, the DICI was a three-component model (involving GP, hospital and community services) and it involved the expansion of a community service that had originally been established, in part, to reduce referrals to (and therefore expenditure in) hospital clinics.6 Similar emphasis on reducing hospital outpatient referrals (ergo payments) was included in the DICI contract and have been seen elsewhere it the English NHS.27 The service was essentially a competitor to hospital-based outpatient services, who were initially supportive, under the false assumption that there would be close cooperation and that patients would benefit.
Although DICI was established to help integrate care, in reality, organisational cultures, management, clinical governance and information systems remained separate. Patients clearly perceived a fragmented service, and many PNs reported that their contact with hospital services was reduced, suggesting that the placement of the DSNs between the practice and the hospital service created a barrier, not a bridge, to optimal care. An insight into how this could increase hospitalisation is perhaps provided by the failure to reduce diabetic foot admissions, including amputation, over the 3 years. Better service coordination has previously been reported to be negatively correlated with amputation rates.28 In ECF, the diabetes specialist podiatrist (DSP) made major, and successful, efforts to link in with the hospital diabetes foot clinics. Nevertheless, the interviews suggest that these efforts were associated with delayed referral for multidisciplinary team (MDT) foot care, that is, the DICI service promoted avoidance of the hospital clinic rather than avoidance of hospital admission. This failure to see a reduction in admissions was not simply a function of time because reductions have been seen within 1 year elsewhere.29,30
The failure to implement integrated information management systems almost certainly contributed to communication and integration difficulties. Most integrated care initiatives attempt to include data sharing,31 but this was not possible within the local information governance arrangements. This was noticed by the patients and was a source of frustration.
Whether our findings result from a unique set of circumstances or might be expected as part of a three-component model is unclear. There are calls for more integration and less fragmentation in healthcare,31 yet the evidence on what works in England is limited.15,16 If the experience here is reproduced elsewhere, the latest changes in commissioning in the English NHS, with emphasis on the need to consider ‘any qualified provider’ in service delivery and associated market procurement approaches, could well impair the quality of diabetes care while increasing overall cost.
One weakness of the study is that as an observational study, it was potentially influenced by historical, secular and other changes. We excluded possible confounders such as changes in hospital admission and diabetes coding policies because the changes occurred independent of hospital. The proportion of patients who had diabetes admitted with and without diabetes as the primary diagnosis were the same or lower than those in other areas, indicating that our findings did not result from differences in pre-existing morbidity. Too short a lead in time (3 years) could explain the lack of reduction in hospitalisation to some extent, but the absence of any positive impact on foot admissions or acute glycaemic admissions, in spite of a major increase in resource, suggests that something inherent in the model obstructed improvement. Some comparisons were not possible because of limitations in data availability, including emergency department attendance data for hypoglycaemia, which were not considered adequate as the result of coding issues (personal communication, M Thoresby, NHS Cambridgeshire). Pharmaceutical data were inaccessible, and some HbA1c data from QoF were not used because the HbA1c thresholds changed during the study period.
Conclusions
There was no improvement in outcomes following investment in a separate community diabetes specialist service. The increased capacity of the intermediate service increased fragmentation between primary and secondary care. There was insufficient support for integration of overall clinical and financial governance, clinical pathways and information management. There is an urgent need for studies of alternative population-based models of diabetes care that demonstrate improvements in diabetes outcomes, including amputations, DKA and overall hospitalisation, rather than descriptions of arrangements or changes in metabolic control in selected subgroups.
References
- 1.Kar P. The ‘super six’ for the acute trust; all else under primary care? Pract Diabetes 2011;28:308–9. [Google Scholar]
- 2.Nagi D, Wilson J. Integrated diabetes care: the Wakefield diabetes service redesign. Pract Diabetes 2011;28:310–1. [Google Scholar]
- 3.Rea RD, Gregory S, Browne M, et al. Integrated diabetes care in Derby: new NHS organisations for new NHS challenges. Pract Diabetes 2011;28:312–3. [Google Scholar]
- 4.Wroe C, Laitner S. Delivering integrated care: a prime contractor model. Pract Diabetes 2011;28:314–5. [Google Scholar]
- 5.Department of Health/Royal College of General Practitioners Guidelines for the appointment of general practitioners with -special -interests in the delivery of clinical services: Diabetes. London: DH, 2003. [Google Scholar]
- 6.Hollern H, Lunn J. Development of a primary care specialist -diabetes nursing service. J Diabetes Nursing 2004;8:344–8. [Google Scholar]
- 7.Hicks D, James J, Hill J, Vanterpool G. Audit of the effectiveness of nurse consultant led intermediate diabetes care services in England. Pract Diabetes 2012;29:54–7. [Google Scholar]
- 8.Armstrong N, Baines D, Baker R. et al.; ICCD Study Group. A cluster randomized controlled trial of the effectiveness and cost-effectiveness of intermediate care clinics for diabetes (ICCD): study protocol for a randomized controlled trial. Trials 2012;13:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mason JM, Freemantle N, Gibson JM, New JP; SPLINT trial Specialist nurse-led clinics to improve control of hypertension and hyperlipidemia in diabetes: economic analysis of the SPLINT trial. Diabetes Care 2005;28:40–6. [DOI] [PubMed] [Google Scholar]
- 10.Arts EEA, Landewe-Cleuren SANT, Schaper NC, Vrijhoef HJM. The cost-effectiveness of substituting physicians with diabetes nurse specialists: a randomized controlled trial with 2-year follow-up. J Advanced Nursing 2012. 68:1224–34. [DOI] [PubMed] [Google Scholar]
- 11.Rayman G, Kilvert A. The crisis in diabetes care in England. BMJ 2012;345:e5446. [DOI] [PubMed] [Google Scholar]
- 12.Enthoven AC. Integrated delivery systems: the cure for fragmentation. Am J Manag Care 2009;15:S284–90. [PubMed] [Google Scholar]
- 13.Ham C. Integrating NHS care: lessons from the front line. London: Nuffield Trust, 2008. [Google Scholar]
- 14.Jha A, Perlin J, Kizer K, Dudley R. Effect of the transformation of the veterans health care system on the quality of care. New Engl J Med 2003;348:2218–27. [DOI] [PubMed] [Google Scholar]
- 15.Ham C, Curry N. Integrated care: what is it? Does it work? What does it mean for the NHS? London: The King's Fund, 2011. [Google Scholar]
- 16.RAND Europe, Ernst & Young LLP National Evaluation of the Department of Health's integrated care pilots: final report. London: RAND Europe, Ernst & Young LLP, 2012. [Google Scholar]
- 17.Simmons D, Yu D, Wenzel H. Changes in hospital admissions and inpatient tariff associated with a Diabetes Integrated Care Initiative: preliminary findings. J Diabetes 2014;6:81–9. [DOI] [PubMed] [Google Scholar]
- 18.Harwood E, Bunn C, Caton C, Simmons D. Addressing barriers to diabetes care and self-care in general practice: a new framework for practice nurses. J Diab Nursing 2013;17:186–91. [Google Scholar]
- 19.Anderson R. New MRC guidance on evaluating complex interventions. BMJ 2008;337:a1937. [DOI] [PubMed] [Google Scholar]
- 20.Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hollern H, Simmons D. Cost saving and improved glycaemic -control in an integrated diabetes service. Prim Care Diabetes 2011;13:176–81. [Google Scholar]
- 22.Distiller LA, Brown MA, Joffe BI, Kramer BD. Striving for the impossible dream: a community based multi-practice -collaborative model of diabetes management. Diabetes Med 2010;27:197–202. [DOI] [PubMed] [Google Scholar]
- 23.Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care 2001;24:1821–33. [DOI] [PubMed] [Google Scholar]
- 24.Norris SL, Nichols PJ, Caspersen CJ, et al. The effectiveness of -disease and case management for people with diabetes: a systematic review. Am J Prev Med 2002;22:15–38. [DOI] [PubMed] [Google Scholar]
- 25.Rothe U, Muller G, Schwartz PEH, et al. Evaluation of a diabetes management system based on practice guidelines, integrated care, and continuous quality management in a federal state of Germany: a population-based approach to health care research. Diabetes Care 2002;25:684–9. [DOI] [PubMed] [Google Scholar]
- 26.Sidorov J, Shull R, Tomcavage J, et al. Does diabetes disease -management save money and improve outcomes? Diabetes Care 2002;25:684–9. [DOI] [PubMed] [Google Scholar]
- 27.Hill J. Seamless diabetes care: the role of the nurse consultant. J Diab Nursing 2008;12:149–54. [Google Scholar]
- 28.Wrobel JS, Charns MP, Diehr P, et al. The relationship between -provider coordination and diabetes-related foot outcomes. Diabetes Care 2003;26:3042–7. [DOI] [PubMed] [Google Scholar]
- 29.Patout Jr. CA, Birle JA, Horswell R, Williams D, Cerise FP. Effectiveness of a comprehensive diabetes lower-extremity -amputation prevention program in a predominantly low-income African-American population. Diabetes Care 2000;23:1339–42. [DOI] [PubMed] [Google Scholar]
- 30.Driver VR, Madsen J, Goodman RA. Reducing amputation rates in patients with diabetes at a military medical center: the Limb Preservation Service model. Diabetes Care 2005;28:248–53. [DOI] [PubMed] [Google Scholar]
- 31.Ham C, Walsh N. Making integrated care happen at scale and pace. London: The Kings Fund, 2013. [Google Scholar]