Abstract
Pulmonary alveolar microlithiasis is rare disease characterized by accumulation of calcium phosphate microlithis in the alveoli. The pathogenesis relates to mutation in the gene SLC34A2 (solute carrier family 34 member 2) located on chromosome 4p15.2, which produces a defective sodium-phosphate cotransporter in alveolar epithelial type-2 cells, making these cells unable to clear phosphorus released during recycling of surfactant [1].
Keywords: SLC34A2 gene, Alveolar microlithiasis, Interstitial lung disease, Bone scan scintography of the lung, Hypoxemia, Lung calcification
In this article we report a case of pulmonary alveolar microlithiasis who presented with progressive dyspnea on exersion, and was diagnosed based on typical imaging findings, obviating the need for lung biopsy.
Case presentation
A 67-year-old female presented with complaints of slowly progressive shortness of breath on exertion and intermittent dry cough for 7 years. She was a nonsmoking teacher with no previously known pulmonary disease until 2012. She was suspected to have an interstitial lung disease because of persistent bilateral infiltrates on chest xray (CXR) (Fig. 1); however, no further workup was done at that time. She denied fever or hemoptysis. She was treated empirically multiple times in the past with steroids with no improvement in her symptoms.
Fig. 1.
Chest X-ray showing diffuse bilateral infiltartes.
On physical examination, she was found to be tachypnic RR 24, and hypoxemic with SpO2 of 87% on room air improved to 92% on 2 L nasal O2. Bilateral fine crackles were noted on auscultation with finger clubbing but no peripheral edema. Routine biochemistry including serum calcium and phosphorus were normal.
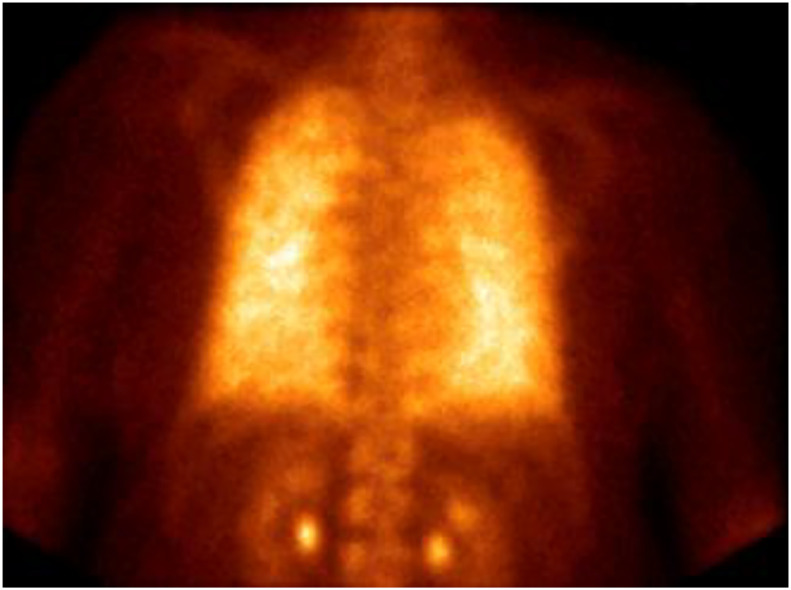
A chest radiograph showed bilateral diffuse opacities with sandstorm-like appearance suggestive of alveolar microlithiasis. A chest CT showed diffuse calcifications in the form of intra-alveolar microliths, calcified interlobular septa, and diffuse ground-glass attenuation with septal thickening (Figs. 2,3). To further confirm the diagnosis Technetium 99m-methylene diphosphonate bone scan was done, and showed diffuse radiotracer uptake (Fig. 4). These finding were deemed adequate to establish a diagnosis of pulmonary alveolar microlithiasis (PAM). Patient refused lung transplant referral on discharge and she was provided with 3 L nasal O2 after assessed for home oxygen requirement.
Fig. 3.
CT Scan of the chest without contrast showing diffuse ground glass attenuation with septal thickening.
Fig. 2.
CT Scan of the chest without contrast showing diffuse calcification with septal thickening.
Fig. 4.
Technetium 99m-methylene diphosphonate (Tc99m-MDP) showing diffuse radiotracer uptake.
Discussion
PAM is a rare autosomal recessive disease with high penetrance, in which concretions composed of calcium phosphate fill alveolar spaces, despite normal serum calcium and phosphorus, and absence of any systemic disease of calcium metabolism [2]. Over 1000 cases were reported worldwide especially in Mediterranean countries [3]. Several mutations in the gene SLC34A2 on chromosome 4p15.2 are well known to cause the disease [1], [4].
This disease is typically diagnosed accidently between 30 and 50 years of age with no significant gender differences found. The golden key in the diagnosis of this disease is clinical-radiological dissociation as patients have less severity of symptoms compared to radiologic finding. Symptomatic patients tend to have dyspnea, as well as a nonproductive cough, mainly on exertion. Blood chemistry tests usually produce results within the normal range. Chest radiographic findings in PAM show diffuse, sandstorm-like infiltration, particularly in lower bases. Chest radiographs may include black pleura sign seen as a strip of tangential peripheral lucency underlying the ribs as compared to the adjacent diffusely dense calcified lung. CT scan of the chest shows numerous sandstorm-like calcifications throughout the lungs with subpleural and peribronchial distribution. Bone scintigraphy using technetium-99m labeled diphosphonate compounds have affinity for calcification foci at soft tissue and can detect early pulmonary calcification [5]. Histopathology is not always required and it is done by open lung or transbronchial biopsy, showing intra-alveolar laminated calcium phosphate concretions. There is no treatment available for this disease. Thus, long-term oxygen therapy is required for hypoxemia and chronic respiratory failure. In our patient lung biopsy was not performed as she had typical findings on the bone scan.
Footnotes
Competing Interests: The authors declare that there is no conflict of interest regarding the publication of this paper.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2019.03.032.
Appendix. Supplementary materials
References
- 1.Kashyap S., Mohapatra P.R. Pulmonary alveolar microlithiasis. Lung India. 2013;30(2):143–147. doi: 10.4103/0970-2113.110424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira Francisco F.A., Pereira e Silva J.L., Hochhegger B., Zanetti G., Marchiori E. Pulmonary alveolar microlithiasis. State-of-the-art review. Respir Med. 2013;107(1):1–9. doi: 10.1016/j.rmed.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Castellana G., Castellana G., Gentile M., Castellana R., Resta O. Pulmonary alveolar microlithiasis: review of the 1022 cases reported worldwide. Eur Respir Rev. 2015;24(138):607–620. doi: 10.1183/16000617.0036-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamin, H. Pulmonary alveolar microlithiasis caused by two homozygous mutations, in B42. Interstitial lung disease: a potpourri of cases. p. A3438-A3438.
- 5.Sahoo M.K., Karunanithi S., Bal C.S. Pulmonary alveolar microlithiasis: imaging characteristics of planar and SPECT/CT bone scan versus 18F-FDG and 18F-sodium fluoride PET/CT scanning. Jpn J Radiol. 2013;31(11):766–769. doi: 10.1007/s11604-013-0250-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.