Highlights
-
•
CAD is one of the most important predisposing factors of cerebral ischaemia in young adults.
-
•
Focal motor seizures with the involvement of the neck may represent a risk condition of developing CAD
-
•
A heightened awareness for CAD should be recommended in patients affected by epilepsy, carotid dopplers may confirm the clinical suspicion in case of significant neck trauma associated with seizures
1. Introduction
Carotid artery dissection (CAD) is one of the most important predisposing factors of cerebral ischemia in young adults. Incidence rate for CAD has been reported to be 1.72 per 100,000 [1]. Various clinical symptoms associated with CAD may be benign (e.g., headache, neck pain, Horner's syndrome, cranial-nerve palsy) or more severe such as stroke and transient ischemic attack (TIA). Seizures rarely represent a predisposing cause of CAD, although carotid artery dissection has been reported in association with minor trauma.
2. Case report
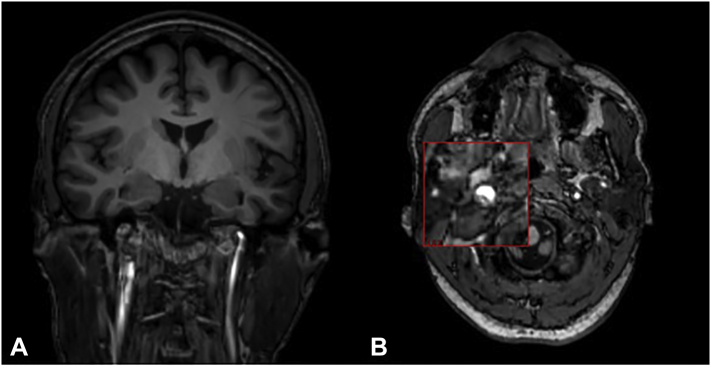
A 45-year-old right-handed man, with personal history of epilepsy beginning at the age of 10, was admitted to our emergency department because of sudden onset of jerking movements of the head to the right associated with blinking of the right eye with narrowing of the homolateral palpebral fissure and right hemi-facial myoclonus starting approximately 30 min prior to arrival. During the neurological examination, the patient was restless and incapable to follow commands and answer questions. A 21 channel EEG recording demonstrated continuous left fronto-temporal spike–wave complexes. The patient was then treated with a bolus of lorazepam 8 mg and underwent continuous EEG monitoring. Over the next 10 min there was a complete normalization of the EEG with a resolution of all neurological symptoms. General examination was unremarkable. Brain Magnetic Resonance Imaging (MRI) and magnetic resonance angiogram (Angio-MRI) performed 24 h after recovery, revealed a right skull base carotid artery dissection without infarction (Fig. 1, A and B). Pre-morbid brain MRI had demonstrated normal carotid flow voids.
Fig. 1.
Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA)of the brain performed after SE recovery.
In A) Coronal T1 sequence and in B) Axial T1 sequence showing right skull base carotid artery dissection without infarction.
3. Discussion
CAD may represent a severe complication associated with epilepsy and seizures. In the previous literature, a case report of acute symptomatic CAD after a generalized tonic–clonic seizure was described [2].
However, we report how focal motor seizures with the involvement of the neck may also represent a risk condition of developing CAD, in particular if the patient presents with status epilepticus or a series of focal motor seizures. Several anamnestic data could be useful in predicting the risk of CAD: trauma to the neck, infections, migraine, hyperhomocysteinemia and 5,10-methylenetetrahydrofolate reductase gene (MTHFR) 677TT mutation represent the most well-known risk factors associated with CAD [3]. Nevertheless, our patient's medical history was unremarkable with focal seizures representing the only predisposing risk factor for CAD.
4. Conclusion
We describe the first case of asymptomatic CAD to our knowledge associated with focal status epilepticus. We therefore speculate that CAD is an underestimated phenomenon in patients with epilepsy. Periodic eco-color Doppler of the carotids should be considered in patient with epilepsy following motor seizures, especially when the neck is traumatized in order to identify the potential life-threatening condition of CAD.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sector.
Declaration of interest
None.
Conflicts of interest
The authors affirm that they do not have conflicts of interest.
Contributor Information
Fedele Dono, Email: fedele.dono@alumni.unich.it.
Marco Onofrj, Email: onofrj@unich.it.
References
- 1.Lee V.H., Brown R.D., Mandrekar J.N., Mokri B. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006;67:1809–1812. doi: 10.1212/01.wnl.0000244486.30455.71. [DOI] [PubMed] [Google Scholar]
- 2.Child Nicholas D., Cascino Gregory D. Carotid dissection following a generalized tonic–clonic seizure. Neurology. May 2013;80(20):1911. doi: 10.1212/WNL.0b013e318292a356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Debette S., Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009;8:668–678. doi: 10.1016/S1474-4422(09)70084-5. [DOI] [PubMed] [Google Scholar]