Abstract
Purpose
Radiation dose to the heart correlates with cardiac-related deaths and may partially diminish the benefit of radiation for breast cancer. This study assessed the current nationwide trends in heart-sparing techniques for breast cancer radiation.
Methods and Materials
In November 2017, an institutional review board–approved survey was sent to radiation oncologists in the United States. Questions assessed demographics and the type and frequency of heart-sparing techniques. Data were analyzed using descriptive statistics and χ2 tests.
Results
In total, 530 responses (13%) were obtained. Most physicians had practiced >15 years (46%), with most in a private setting (59%). Eighty-three percent of physicians offered prone positioning and/or deep inspiration breath hold (DIBH). This was more common in academic practice (P < .01). Seventy-three percent of physicians used heart-sparing techniques for more than three-fourths of left-sided patients. The most commonly used technique was DIBH, and 43% of physicians used the technique more than three-fourths of the time. Commonly used DIBH systems were Varian RPM (54%) and Vision RT/Align RT (31%). No increase in DIBH use was observed with regional nodal irradiation, and coverage of internal mammary chain nodes varied. Patient tolerance (78%) and cardiac-to-chest wall distance (72%) were the most common determinants of DIBH in left-sided patients. Twenty-three percent of physicians used DIBH for right-sided patients, with lung (64%) and heart sparing (46%) as the most common reasons for use. Lack of facilities was the most common reason not to use DIBH (61%).
Conclusions
Most respondents offer heart-sparing techniques for breast cancer radiation; this is more common in academic centers. DIBH is the most common technique across all practice settings. DIBH is much less commonly used in right-sided patients but is still used by >20% of practitioners, with lung and heart sparing cited as reasons for use. More data are needed to determine if and when this technique should be used in right-sided cases.
Introduction
Radiation for breast cancer, as part of either breast-conserving or postmastectomy therapy, has been shown to have both a local control and overall survival benefit.1, 2 However, studies have demonstrated a correlation, not only between radiation for left-sided breast cancer and cardiac mortality,3, 4 but more specifically between radiation dose to the heart and cardiac-related deaths.5 Unfortunately, this cardiac toxicity may partly diminish the survival benefit of radiation therapy for breast cancer.6, 7 In fact, data suggest that the risk of major coronary events increases 7.4% per gray of mean dose to which the heart is exposed,8 which highlights the importance of monitoring heart dose and minimizing heart radiation exposure whenever possible.
Over the years, numerous techniques have been created and used with the aim of reducing radiation dose to the heart, and radiation therapy has been shown in recent years to have less cardiac toxicity compared with prior older studies.4, 7, 9, 10 More recent techniques including prone irradiation,11, 12, 13 deep inspiration breath hold (DIBH), intensity modulated radiation therapy (IMRT),14 and proton therapy,15, 16 have all been shown to be beneficial in helping to reduce radiation dose to the heart. However, one study found that IMRT was associated with increased mean heart dose, though this was partly related to whether the patient underwent forward or inverse planning, highlighting the importance of setting appropriate constraints and cost functions.17
DIBH relies on the increased distance between the chest wall and the heart during inspiration, which decreases the volume of the heart being irradiated,18 and DIBH has been shown to decrease radiation heart dose when compared with prone and standard supine positioning.19 In fact, DIBH can decrease mean heart dose by 25% to 67% compared with standard free breathing.20 Recent data also suggest that DIBH can decrease ipsilateral lung dose in patients undergoing internal mammary chain (IMC) radiation21 and in right-sided patients,22 which raises the question of whether DIBH may be beneficial in these cases.
However, the use of these cardiac-sparing techniques varies from physician to physician and institution to institution. Even with the use of DIBH, there is variation in the DIBH technique (eg, voluntary vs moderate or active breathing control [ABC]) and the systems used. Voluntary DIBH (vDIBH) uses patient coaching throughout the respiratory cycle,23 whereas ABC DIBH is delivered using a spirometer-like device.24, 25 Both techniques have been shown to be effective, although data suggest that patients may better tolerate vDIBH.23 In addition, heart-sparing techniques can also be used in combination, such as prone positioning and DIBH.26, 27
Although a number of cardiac sparing techniques are available, techniques such as prone breast radiation and DIBH can be more labor-intensive and require longer treatment times than traditional supine free-breathing radiation treatments. It is unclear what particular anatomic or patient-specific factors can predict which patients would benefit most from techniques such as DIBH. Little is known about the current trends in the frequency and type of heart-sparing techniques used by radiation oncologists across the United States, and these results may help direct future research and practice patterns.
Methods and Materials
Institutional review board approval was granted per institutional protocol (PRO00030288). An electronic survey was created using SurveyMonkey software. The questions were directed at assessing demographic information, the percentage of time spent treating patients with breast cancer, and the type and frequency of various heart-sparing techniques and the scenarios in which they were used.
In November 2017, the survey was emailed to 4015 radiation oncologists practicing in various settings across the United States using the American Society of Therapeutic Radiation Oncology database. Emails included a cover letter informing potential participants of the aims, benefits, and risks of the survey, as well as a link to SurveyMonkey (cover letter and survey available online at https://dx.doi.org/10.1016/j.adro.2019.01.001). Both complete and incomplete surveys were included in the final analysis.
Data were obtained from SurveyMonkey and analyzed using MedCalc Statistical Software, version 18.5 (MedCalc Software bvba, Ostend, Belgium). One reminder email was sent with the survey link again to improve the response rate. Only one survey per e-mail address was allowed. The data were analyzed using descriptive statistics and χ2 testing. A significance value of P < .05 was used.
Results
Demographics
Results were obtained from 530 radiation oncologists, resulting in a response rate of 13%. The overwhelming majority (99%) had completed radiation oncology training in the United States. Participants consisted of physicians practicing in academic (38%), private practice (59%), and government (2%) settings. Forty-six percent of all responding physicians had been practicing >15 years. Of the responding physicians, 37% noted that 11% to 25% of their clinical time is devoted to treating patients with breast cancer, and 35% answered that 26% to 50% of their time is devoted to these patients. Detailed demographics are shown in Table 1.
Table 1.
Respondent demographics
| Demographic | Total N = 529 |
DIBH and/or prone N = 440 |
No DIBH and/or prone N = 89 |
P-value |
|---|---|---|---|---|
| Years practicing | ||||
| 1-5 | 125 (24%) | 116 (93%) | 9 (7%) | < .001 |
| 6-10 | 104 (20%) | 87 (84%) | 17 (16%) | |
| 11-15 | 54 (10%) | 50 (93%) | 4 (7%) | |
| >15 | 241 (46%) | 184 (76%) | 57 (24%) | |
| Training in United States | ||||
| Yes | 525 (99%) | 438 (83%) | 87 (17%) | - |
| Practice setting | ||||
| Academic—main site | 121 (23%) | 117 (97%) | 4 (3%) | < .001 |
| Academic—satellite site | 84 (16%) | 72 (86%) | 12 (14%) | |
| Private practice | 314 (59%) | 245 (78%) | 69 (22%) | |
| Government—Veterans Affairs | 10 (2%) | 6 (60%) | 4 (40%) | |
| % Clinical time devoted to breast cancer | ||||
| <10% | 51 (10%) | 42 (82%) | 9 (18%) | < .001 |
| 11%-25% | 195 (37%) | 150 (77%) | 45 (23%) | |
| 26%-50% | 183 (35%) | 152 (83%) | 31 (17%) | |
| Majority | 98 (19%) | 94 (96%) | 4 (4%) | |
Abbreviation: DIBH = deep inspiration breath hold.
Demographics are presented in aggregate, as well as divided into those who provide DIBH and/or prone positioning, and those who do not. Associated P-values are presented.
Frequency of heart-sparing techniques
The cardiac constraints most commonly used by responding physicians were mean heart dose (83%) and volumetric constraints (67%). In this survey, 83% of responding physicians provided breast cancer treatment with prone positioning and/or DIBH. This was more common in physicians practicing in academic (92%) versus private practice (78%) settings (P < .01). Results also revealed that 73% of respondents used heart-sparing techniques for more than three-fourths of patients with left-sided breast cancer. For these physicians, the most commonly used heart-sparing technique was DIBH, and 43% of responding physicians use this technique more than three-fourths of the time (Fig. 1). Proton therapy was used the least, with 87% of physicians responding they never use protons.
Fig. 1.
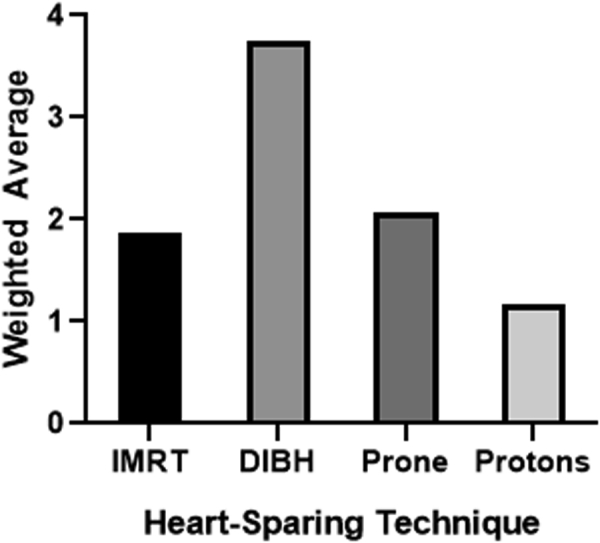
Frequency of heart-sparing modalities. The relative frequency of different heart-sparing techniques is represented by the weighted average on the y-axis.
Use of DIBH
For physicians who use DIBH, the most commonly used techniques were Varian RPM (54%) and Vision RT/Align RT (31%). Elekta ABC was used 10% of the time. Three-dimensional conformal therapy (90%) was the most commonly used planning modality for patients undergoing DIBH. DIBH was used at approximately the same frequency in patients with left-sided breast cancer, whether they received whole-breast/chest-wall radiation alone or with regional nodal irradiation. Patient tolerance (78%) and cardiac-to-chest wall distance (72%) were the most common factors determining whether DIBH was used in patients with left-sided breast cancer. Interestingly, 23% of responding physicians used DIBH in patients with right-sided breast cancer, with lung sparing (64%) and heart sparing (46%) cited as the most common reasons for its use. Right-sided DIBH was also used more commonly in patients undergoing regional nodal irradiation. Right-sided DIBH was more common in academic (30%) versus private practice (18%) settings (P < .01). Lack of facilities (61%) was cited as the most common reason not to use DIBH. Detailed results related to the use of DIBH are included in Table 2.
Table 2.
Specifics regarding the use of DIBH among study participants
| DIBH Modality | |
| Elekta ABC | 39 (10%) |
| Varian RPM | 208 (54%) |
| Vision RT/Align RT | 120 (31%) |
| Anzai Respiratory Belt | 8 (2%) |
| Other | 68 (18%) |
| DIBH Treatment Planning | |
| 2D | 5 (1%) |
| 3D | 371 (90%) |
| IMRT | 90 (22%) |
| Prone Positioning | 10 (2%) |
| Patient Factors | |
| Body Habitus | 134 (35%) |
| Breast Size | 77 (20%) |
| Cardiac-to-Chest Wall Distance | 280 (72%) |
| Age | 86 (22%) |
| Comorbidities | 109 (28%) |
| Tolerance | 304 (78%) |
| Other | 80 (21%) |
| Reasons for DIBH in Right-Sided Patients | |
| Heart Sparing | 44 (46%) |
| Liver Sparing | 20 (21%) |
| Lung Sparing | 61 (64%) |
| Motion Management | 17 (18%) |
| Other | 19 (20%) |
| Reasons for Not Using DIBH | |
| Lack of Familiarity | 8 (9%) |
| Lack of Facilities | 53 (61%) |
| Increased Planning and Treatment Time | 13 (15%) |
| Lack of Reimbursement | 8 (9%) |
| Cost to Patient | 0 (0%) |
| Other | 33 (38%) |
The number of respondents (%) for various questions assessing use of DIBH is shown. Note that respondents could choose more than one item for each question.
IMC radiation
The majority of respondents (43%) included IMC nodes 1% to 25% of the time for left-sided patients undergoing regional nodal irradiation (Fig. 2). Twenty-one percent of respondents included IMC nodes more than three-fourths of the time. This proportion differed between academics (31%) and private practice (13%; P < .01). Four percent of respondents did not include IMC nodes.
Fig. 2.
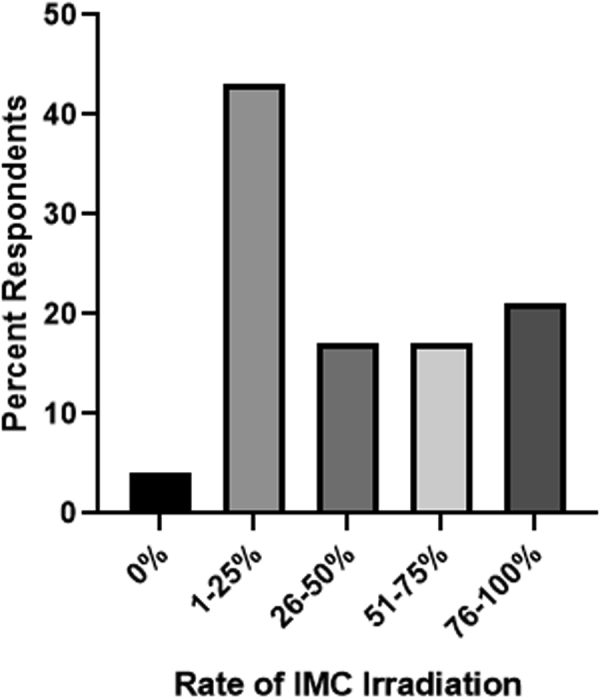
Rate of internal mammary chain irradiation. The x-axis represents how often internal mammary chain nodes are included for left-sided patients undergoing regional nodal irradiation.
Discussion
Over the years, many techniques have been introduced with the aim of the reducing radiation dose to the heart and thus reducing radiation-induced cardiac toxicity. However, with the various techniques available, as well as differences in application and delivery, practice patterns across the country vary greatly. This study aimed to assess practice patterns for heart-sparing techniques used in radiation therapy for breast cancer. To our knowledge, this is the first survey of its kind in the United States.
As indicated in the survey results, most responding physicians in the United States offer heart-sparing techniques for patients with breast cancer, with 83% offering prone positioning and/or DIBH. However, the proportion of physicians who use these techniques was higher in academic compared with private practice settings. The reason for this remains unclear, but a lack of facilities was the most common reason cited for not offering DIBH, and the proportion of physicians who answered so did not differ significantly between private practice and academic settings (P = .65). Although only 15% of respondents answered that the increased planning and treatment time was a factor in not using DIBH, the fact that the technique can be more labor intensive may deter some physicians.
The dosimetric advantage of DIBH has been demonstrated in numerous studies, with decreases in both mean heart and left anterior descending artery doses compared with free-breathing.20 Despite these data, approximately 12% of respondents from a private practice setting who did not use DIBH cited lack of major clinical benefit as the reason. Although small, the number was higher compared with that in the academic group, and it is not clear from the current data if this is a more widespread belief that may prevent physicians from using the technique. It could be that there is a lack of education about the dosimetric benefit of DIBH, or perhaps uncertainty among physicians about the dosimetric benefit translating into a clinical benefit. Nonetheless, despite a statistically significant difference between private practice and academic settings, the vast majority of physicians across both practice settings appear to use these techniques. This is even more encouraging given that the majority of responding physicians had been practicing >15 years, suggesting that even those physicians who trained in an area where these techniques did not exist are now using them often.
DIBH was the most commonly used heart-sparing technique used across all practice settings. This appears to correlate with a German study of a similar nature that assessed patterns of care in Germany, Austria, and Switzerland. In this study, breathing-adapted radiation therapy, such as DIBH, was the most commonly used heart-sparing technique (65% of departments).28 In our survey, DIBH was more commonly used in patients with left-sided breast cancers, but 23% of responding physicians reported using DIBH for right-sided patients as well. Lung and heart sparing were cited as the most commonly reported reasons for use of right-sided DIBH; however, DIBH was also used more frequently in patients with right-sided breast cancer undergoing regional nodal radiation.
Data on the use of DIBH in right-sided patients are limited, although there are some data to suggest that DIBH may allow for a reduction in ipsilateral lung dose in patients who require radiation of the IMC nodes.21 Another study specifically analyzed patients with right-sided breast cancer and noted that DIBH decreased both the ipsilateral lung dose and volume of the liver receiving 50% of the dose.22 This raises the question of whether select patients with right-sided breast cancers, especially those undergoing IMC radiation, may benefit from the use of DIBH.
This also highlights the need for more data on the use of DIBH in right-sided patients to determine if and when DIBH should be used. The inclusion of IMCs in the radiation field is often physician- and/or practice-specific. IMCs are included in many studies that demonstrate a benefit from regional nodal radiation,29, 30 and although there are also data that suggest IMC treatment may not be beneficial,31 the study had some notable flaws and may not be as applicable in the modern era.
With these recent studies demonstrating the potential benefits of nodal irradiation on overall survival and breast cancer recurrence, the number of patients undergoing regional nodal radiation, and subsequently IMC radiation, may increase.29, 30 However, interestingly, despite these data, almost half of the responding physicians in our study noted that they only included IMC nodes for left-sided patients undergoing regional nodal radiation 1% to 25% of the time. Additionally, some variation existed in the inclusion of IMCs between physicians in academic and private practice settings. Combined, these findings suggest that more data on practice patterns related to IMC coverage are needed to better elucidate its use.
Varian RPM and Vision RT/Align RT were the most commonly used DIBH modalities. The UK HeartSpare study demonstrated that vDIBH was preferred and deemed more comfortable by patients23; this may be related to patient tolerance being cited as the most common reason determining when DIBH was used. Cardiac-to-chest wall distance was also commonly cited as a factor determining when DIBH was used. Data have shown that the distance of the heart in the radiation field32 and the number of slices on computed tomography scans in which the heart contacts the chest wall33, 34 correlate with mean heart dose. Based on the responses, physicians appear to use such anatomic parameters to assess which patients may be the best candidates and gain the most benefit from DIBH.
Also notable was that a considerable proportion of respondents (2%) used institutional in-house DIBH techniques. This highlights that even among those who use DIBH, treatment modalities and techniques differ greatly. Some of these in-house techniques rely on therapist monitoring and control, which highlights the need for proper therapist and patient training of the technique to ensure appropriate treatment.
Proton therapy was the least used cardiac-sparing modality. Proton therapy has been demonstrated to have decreased heart doses compared with photon therapy,15, 16 even when compared with patients treated using IMRT with DIBH.35 There was also an advantage to proton therapy when examining patients with breast cancer who underwent regional nodal radiation.36 However, limited access to proton centers and their associated cost likely explain the low number of respondents using the therapy.
Another interesting question not assessed in the survey was whether physicians use a combination of heart-sparing techniques simultaneously. Some studies have shown that there may be a benefit to doing DIBH in the prone position. Mulliez et al found that prone DIBH reduced the mean heart dose from 2.2 Gy for standard prone treatment to 1.3 Gy for prone DIBH.27 The same study also found that the lung dose was slightly worse with prone DIBH compared with standard prone treatment, although the doses were low regardless and much less when compared with supine free breathing and DIBH.27 With these data, further research is needed to address the feasibility and benefit of combining these techniques, especially when considering the question with regard to lung dose and intensity of set up.
This study had certain limitations. One limitation is that, as a survey, the data reflect the views and practice patterns only of those physicians who responded. With a response rate of 13%, the data do not include a large proportion of practicing radiation oncologists and therefore may not fully represent nationwide trends. With the majority of respondents being private practice physicians, our data may appear to be skewed toward the views of this population. However, this could simply mirror the relatively higher number of radiation oncologists in private practice. In this sense, academic physicians may be relatively overrepresented in this sample.
Additionally, because of the nature and topic of the survey, the survey could overestimate the proportion of radiation oncologists who use heart-sparing techniques; physicians interested in breast radiation and heart sparing may have been more likely to respond to the survey. Similarly, the study population was less likely to include those who do not commonly treat breast cancer.
Conclusions
Despite the limitations inherent to voluntary surveys, this study brings to light a number of interesting observations with regard to current practice patterns for the use of cardiac-sparing radiation techniques for patients with breast cancer. Based on the results of this project, a number of potential clinical study questions are raised (eg, when should DIBH be considered for patients with right-sided breast cancer), and practice patterns on IMC radiation and the role of heart-sparing techniques in patients undergoing regional nodal irradiation are further elucidated. Hopefully, this study will fuel further research on heart-sparing techniques for breast cancer radiation, including when and how certain techniques should be used.
Footnotes
Sources of support: No funding was received for this study. Dr Bergom received support from Institutional Research Grant 86-004-26 from the American Cancer Society, Mary Kay Foundation Award Grant No. 017-29, Susan G. Komen Grant #CCR17483233, Cardiovascular Center and Cancer Center at the Medical College of Wisconsin, and the National Institutes of Health Grant 8KL2TR000056.
Conflicts of interest: The authors have no conflicts of interest to disclose.
Supplementary material for this article can be found at https://doi.org/10.1016/j.adro.2019.01.001.
Supplementary Data
References
- 1.Early Breast Cancer Trialists' Collaborative Group Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: Meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–1716. doi: 10.1016/S0140-6736(11)61629-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Early Breast Cancer Trialists' Collaborative Group Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: Meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383:2127–2135. doi: 10.1016/S0140-6736(14)60488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rutqvist L.E., Johansson H. Mortality by laterality of the primary tumour among 55,000 breast cancer patients from the Swedish Cancer Registry. Br J Cancer. 1990;61:866–868. doi: 10.1038/bjc.1990.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henson K.E., McGale P., Taylor C., Darby S.C. Radiation-related mortality from heart disease and lung cancer more than 20 years after radiotherapy for breast cancer. Br J Cancer. 2013;108:179–182. doi: 10.1038/bjc.2012.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gyenes G., Rutqvist L.E., Liedberg A., Fornander T. Long-term cardiac morbidity and mortality in a randomized trial of pre- and postoperative radiation therapy versus surgery alone in primary breast cancer. Radiother Oncol. 1998;48:185–190. doi: 10.1016/s0167-8140(98)00062-0. [DOI] [PubMed] [Google Scholar]
- 6.Early Breast Cancer Trialists' Collaborative Group Favourable and unfavourable effects on long-term survival of radiotherapy for early breast cancer: An overview of the randomised trials. Lancet. 2000;355:1757–1770. [PubMed] [Google Scholar]
- 7.Hooning M.J., Aleman B.M., van Rosmalen A.J., Kuenen M.A., Klijn J.G., van Leeuwen F.E. Cause-specific mortality in long-term survivors of breast cancer: A 25-year follow-up study. Int J Radiat Oncol Biol Phys. 2006;64:1081–1091. doi: 10.1016/j.ijrobp.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 8.Darby S.C., Ewertz M., McGale P. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–998. doi: 10.1056/NEJMoa1209825. [DOI] [PubMed] [Google Scholar]
- 9.Cuzick J., Stewart H., Rutqvist L. Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol. 1994;12:447–453. doi: 10.1200/JCO.1994.12.3.447. [DOI] [PubMed] [Google Scholar]
- 10.Darby S.C., McGale P., Taylor C.W., Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: Prospective cohort study of about 300,000 women in U.S. SEER cancer registries. Lancet Oncol. 2005;6:557–565. doi: 10.1016/S1470-2045(05)70251-5. [DOI] [PubMed] [Google Scholar]
- 11.Formenti S.C., DeWyngaert J.K., Jozsef G., Goldberg J.D. Prone vs supine positioning for breast cancer radiotherapy. JAMA. 2012;308:861–863. doi: 10.1001/2012.jama.10759. [DOI] [PubMed] [Google Scholar]
- 12.Krengli M., Masini L., Caltavuturo T. Prone versus supine position for adjuvant breast radiotherapy: A prospective study in patients with pendulous breasts. Radiat Oncol. 2013;8:232. doi: 10.1186/1748-717X-8-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lymberis S.C., deWyngaert J.K., Parhar P. Prospective assessment of optimal individual position (prone versus supine) for breast radiotherapy: Volumetric and dosimetric correlations in 100 patients. Int J Radiat Oncol Biol Phys. 2012;84:902–909. doi: 10.1016/j.ijrobp.2012.01.040. [DOI] [PubMed] [Google Scholar]
- 14.Lohr F., El-Haddad M., Dobler B. Potential effect of robust and simple IMRT approach for left-sided breast cancer on cardiac mortality. Int J Radiat Oncol Biol Phys. 2009;74:73–80. doi: 10.1016/j.ijrobp.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Ares C., Khan S., Macartain A.M. Postoperative proton radiotherapy for localized and locoregional breast cancer: Potential for clinically relevant improvements? Int J Radiat Oncol Biol Phys. 2010;76:685–697. doi: 10.1016/j.ijrobp.2009.02.062. [DOI] [PubMed] [Google Scholar]
- 16.MacDonald S.M., Jimenez R., Paetzold P. Proton radiotherapy for chest wall and regional lymphatic radiation; dose comparisons and treatment delivery. Radiat Oncol. 2013;8:71. doi: 10.1186/1748-717X-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pierce L.J., Feng M., Griffith K.A. Recent time trends and predictors of heart dose from breast radiation therapy in a large quality consortium of radiation oncology practices. Int J Radiat Oncol Biol Phys. 2017;99:1154–1161. doi: 10.1016/j.ijrobp.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 18.Latty D., Stuart K.E., Wang W., Ahern V. Review of deep inspiration breath-hold techniques for the treatment of breast cancer. J Med Radiat Sci. 2015;62:74–81. doi: 10.1002/jmrs.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verhoeven K., Sweldens C., Petillion S. Breathing adapted radiation therapy in comparison with prone position to reduce the doses to the heart, left anterior descending coronary artery, and contralateral breast in whole breast radiation therapy. Pract Radiat Oncol. 2014;4:123–129. doi: 10.1016/j.prro.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Bergom C., Currey A., Desai N., Tai A., Strauss J.B. Deep inspiration breath hold: Techniques and advantages for cardiac sparing during breast cancer irradiation. Front Oncol. 2018;8:87. doi: 10.3389/fonc.2018.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohamad O., Shiao J., Zhao B. Deep inspiration breathhold for left-sided breast cancer patients with unfavorable cardiac anatomy requiring internal mammary nodal irradiation. Pract Radiat Oncol. 2017;7:e361–e367. doi: 10.1016/j.prro.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 22.Conway J.L., Conroy L., Harper L. Deep inspiration breath-hold produces a clinically meaningful reduction in ipsilateral lung dose during locoregional radiation therapy for some women with right-sided breast cancer. Pract Radiat Oncol. 2017;7:147–153. doi: 10.1016/j.prro.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 23.Bartlett F.R., Colgan R.M., Carr K. The UK HeartSpare Study: Randomised evaluation of voluntary deep-inspiratory breath-hold in women undergoing breast radiotherapy. Radiother Oncol. 2013;108:242–247. doi: 10.1016/j.radonc.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 24.Wong J.W., Sharpe M.B., Jaffray D.A. The use of active breathing control (ABC) to reduce margin for breathing motion. Int J Radiat Oncol Biol Phys. 1999;44:911–919. doi: 10.1016/s0360-3016(99)00056-5. [DOI] [PubMed] [Google Scholar]
- 25.Remouchamps V.M., Letts N., Vicini F.A. Initial clinical experience with moderate deep-inspiration breath hold using an active breathing control device in the treatment of patients with left-sided breast cancer using external beam radiation therapy. Int J Radiat Oncol Biol Phys. 2003;56:704–715. doi: 10.1016/s0360-3016(03)00010-5. [DOI] [PubMed] [Google Scholar]
- 26.Mulliez T., Van de Velde J., Veldeman L. Deep inspiration breath hold in the prone position retracts the heart from the breast and internal mammary lymph node region. Radiother Oncol. 2015;117:473–476. doi: 10.1016/j.radonc.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 27.Mulliez T., Veldeman L., Speleers B. Heart dose reduction by prone deep inspiration breath hold in left-sided breast irradiation. Radiother Oncol. 2016;114:79–84. doi: 10.1016/j.radonc.2014.11.038. [DOI] [PubMed] [Google Scholar]
- 28.Duma M.N., Münch S., Oechsner M., Combs S.E. Heart-sparing radiotherapy in patients with breast cancer: What are the techniques used in the clinical routine? A pattern of practice survey in the German-speaking countries. Med Dosim. 2017;42:197–202. doi: 10.1016/j.meddos.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Poortmans P.M., Collette S., Kirkove C. Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med. 2015;373:317–327. doi: 10.1056/NEJMoa1415369. [DOI] [PubMed] [Google Scholar]
- 30.Whelan T.J., Olivotto I.A., Parulekar W.R. Regional nodal irradiation in early-stage breast cancer. N Engl J Med. 2015;373:307–316. doi: 10.1056/NEJMoa1415340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hennequin C., Bossard N., Servagi-Vernat S. Ten-year survival results of a randomized trial of irradiation of internal mammary nodes after mastectomy. Int J Radiat Oncol Biol Phys. 2013;86:860–866. doi: 10.1016/j.ijrobp.2013.03.021. [DOI] [PubMed] [Google Scholar]
- 32.Kong F.M., Klein E.E., Bradley J.D. The impact of central lung distance, maximal heart distance, and radiation technique on the volumetric dose of the lung and heart for intact breast radiation. Int J Radiat Oncol Biol Phys. 2002;54:963–971. doi: 10.1016/s0360-3016(02)03741-0. [DOI] [PubMed] [Google Scholar]
- 33.Rochet N., Drake J.I., Harrington K. Deep inspiration breath-hold technique in left-sided breast cancer radiation therapy: Evaluating cardiac contact distance as a predictor of cardiac exposure for patient selection. Pract Radiat Oncol. 2015;5:e127–e134. doi: 10.1016/j.prro.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 34.Lee G., Rosewall T., Fyles A., Harnett N., Dinniwell R.E. Anatomic features of interest in women at risk of cardiac exposure from whole breast radiotherapy. Radiother Oncol. 2015;115:355–360. doi: 10.1016/j.radonc.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Lin L.L., Vennarini S., Dimofte A. Proton beam versus photon beam dose to the heart and left anterior descending artery for left-sided breast cancer. Acta Oncol. 2015;54:1032–1039. doi: 10.3109/0284186X.2015.1011756. [DOI] [PubMed] [Google Scholar]
- 36.Bradley J.A., Dagan R., Ho M.W. Initial report of a prospective dosimetric and clinical feasibility trial demonstrates the potential of protons to increase the therapeutic ratio in breast cancer compared with photons. Int J Radiat Oncol Biol Phys. 2016;95:411–421. doi: 10.1016/j.ijrobp.2015.09.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


