Abstract
Cannabinoid receptor CB2 (CB2R) is upregulated on activated microglia and astrocytes in the brain under inflammatory conditions and plays important roles in many neurological diseases, such as Alzheimer’s disease, amyotrophic lateral sclerosis, and ischemic stroke. The advent of positron emission tomography (PET) using CB2R radiotracers has enabled the visualization of CB2R distribution in vivo in animal models of central nervous system inflammation, however translation to humans has been less successful. Several novel CB2R radiotracers have been developed and evaluated to quantify microglial activation. In this review, we summarize the recent preclinical and clinical imaging results of CB2R PET tracers and discuss the prospects of CB2R imaging using PET.
Keywords: cannabinoid receptor CB2, microglia, inflammation, neurological diseases, positron emission tomography
Cannabinoid receptor CB2R
Cannabinoid receptors, including CB1R and CB2R subtypes, are G-protein-coupled receptors that are involved in endocannabinoid signaling and various physiological processes, such as pain, mood, and memory [1]. CB1R is expressed abundantly in the central nervous system (CNS), whereas CB2R exists mainly in the peripheral organs (e.g., spleen) and is undetectable in the brain under physiological conditions. In the periphery, CB2R is expressed on leukocytes and macrophages and regulates inflammation and immune functions, such as phagocytosis inhibition, B and T cell differentiation, and the balance of pro-inflammatory/anti-inflammatory cytokines. Under CNS inflammation, CB2R expression is upregulated on microglia, astrocytes, and oligodendrocytes and on post-synaptic neurons [2] in the hippocampus, brainstem, and cerebellum of both mouse/rat models [1, 3–5] and humans [6]. CB2R has mainly been associated with anti-inflammatory/immuno-suppressive roles and reductions in nuclear factor NF-κB and inflammatory mediators. Its low baseline expression and disease-induced increase make CB2R a promising diagnostic and therapeutic target for CNS inflammation.
Microglia and astrocytes are major players in the brain innate immune system. They are morphologically dynamic and undergo priming based on the local context [7]. Ramified microglia are activated in response to brain injury and immune stimuli and develop a “classical activation, pro-inflammation” status or an “alternative activation, anti-inflammation” status [8]. The extent to which inflammation is beneficial or detrimental in disease processes has not been fully elucidated. Acute inflammation consists of an immediate and early response to a stimulus, such as stroke or trauma, and a subsequent defensive response that facilitates repair. Chronic CNS inflammation resulting from persistent stimuli is an important component in the pathophysiology of many neurological diseases, such as Alzheimer’s disease (AD), Parkinson’s disease [9], amyotrophic lateral sclerosis (ALS) [10], multiple sclerosis (MS) [11], and Huntington disease [12].
CNS inflammation tracers
Positron emission tomography (PET) enables the in vivo detection of molecular changes in animal models and in humans, thus facilitating the understanding of disease mechanisms. The development of CNS inflammation tracers has been challenging, partly due to the diverse and changing states of astrocytes and microglia. Tracers for translocator protein (TSPO) have been the most applied probes in studying the microglial activation status in patients with neurological disorders [13, 14]. Several TSPO tracers have been evaluated in animal models and patients, including the first-generation [11C]PK11195, second-generation molecules such as [11C]DAA1106, [11C]PBR28, and [18F]DPA-714 [15], and third-generation rs6971-insensitive radiotracers such as [11C]ER176 [16] and [18F]GE180 [17, 18]. Although it has had varying degrees of utility in different neurological diseases, TSPO imaging has the limitations of specificity of binding, data quantification (reference region), and mixed binders of the second-generation tracers due to the polymorphism in the TSPO gene [14, 19]. New classes of tracers detecting, e.g., CB2R, monoamine oxidase B [20] cyclooxygenases (COX 1, 2), and arachidonic acid [17, 21], are under development as potential tracers for CNS inflammation.
PET tracers for imaging CB2R
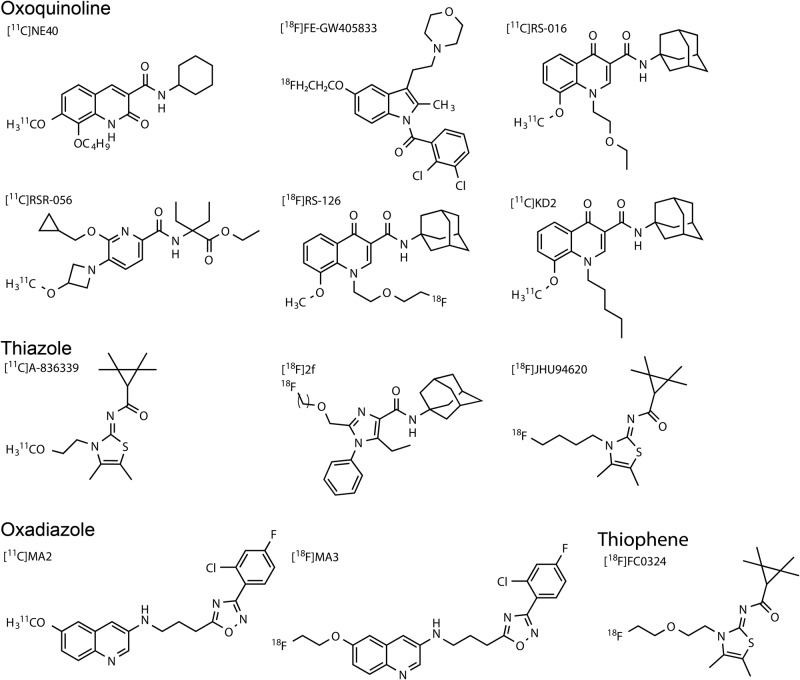
Several CB2R tracers have been developed, including the oxoquinoline derivatives [11C]KD2 [22], [11C]KP23 [23], [11C]RS-016 [24, 25], [11C]RSR-056 [26], [11C]RS-028, and [18F]RS-126 [22, 25–31], and [11C]NE40 [32]; and the thiazole derivatives [11C]A-836339 [33, 34], [18F]JHU94620 [35, 36], and [18F]2f [37]. They have shown high-affinity binding to CB2R and sufficient selectivity over CB1R. The oxadiazole derivatives [11C]MA2 and [18F]MA3 [38] and thiophene-based tracers [11C]AAT-778, [11C]AAT-015 [29], and [18F]FC0324 [39] show high affinity to CB2R but suboptimal selectivity over CB1R. Table 1 summarizes the relevant properties of the CB2R radiotracers. Figure 1 shows the chemical structures of different classes of CB2R tracers. For the structure-activity relationships of CB2R tracers, see the recent review published by Spinelli et al. [40]. Some of the most important prerequisites for a useful CNS PET tracer for imaging CB2R include: (1) high-nanomolar-affinity binding to CB2R to obtain a high target signal in vivo (BPnd or %ID/g) given the low concentration of CB2R in the brain; (2) suitable LogP (range 1–3) for blood-brain barrier passage; (3) specific binding to CB2R with 1000-fold higher selectivity over CB1R; (4) no radiometabolites in the brain; and (5) low interaction with plasma proteins. This review focuses on the evaluations of CB2R tracers in animal models and patients with neurological diseases involving CNS inflammation.
Table 1.
Summary of CB2R tracer properties
| Class | Tracer | Affinity hCB2R | Selectivity CB1R | LogP | Human | Animal model | Ref |
|---|---|---|---|---|---|---|---|
| Thiazole | [11C]A-836339 | 0.64 nM | >400 | 2.97 | AD mouse model; stroke, LPS, AMPA injected rat model | [33, 34] | |
| [18F]2f | 0.1 nM | >300 | 3.4 | Healthy Wistar rat LPS-injected CD1 mouse | [41] | ||
| [18F]JHU94620 | 0.38 nM | 1000 | [35, 36] | ||||
| [18F]15 | 0.29 nM | >1000 | [37] | ||||
| Oxoquinoline | [11C]NE40 | 9.6 nM | 100 | 3.5 | In vivo AD; healthy control | SD/Wistar rat stroke model; rhesus monkey | [32, 42–48] |
| [11C]RSR-056 | 2.5 nM | >1000 | 1.94 | Post-mortem AD brain, ALS spinal cord | LPS-injected mouse | [26] | |
| [11C]RS-016 | 0.7 nM | >1000 | 2.78 | [25, 30] | |||
| [11C]KD2 | [22] | ||||||
| [11C]KP23 | |||||||
| [18F]RS-126 | 1.99 | ALS spinal cord | [23, 28] | ||||
| [11C]RS-028 | [31] | ||||||
| [11C]6f | 5.4 nM | 1851 | [49] | ||||
| [11C]6b | 9.4 nM | 1067 | |||||
| Indole | [18F]FE-GW405833 | 27 nM | 6000 | 2.5 | [50] | ||
| [11C]Methoxy-Sch225336 | 4.5 nM | 78 | 2.15 | [51] | |||
| Oxadiazole | [11C]MA2 | 87 nM | 19 | NMRI mouse | [38] | ||
| [18F]MA3 | 0.8 nM | 127 | |||||
| Thiophene | [11C]AAT-015 | 3.3 nM | 303 | 4.11 | Rat | [29] | |
| [11C]AAT-778 | 4.3 nM | 256 | 6 | ||||
| [18F]FC0324 | 0.1 nM | 296 | Rat | [39] | |||
| Amid | [18F]1,2 | 2.3 nM | >500 | CD1 mouse | [52] | ||
| [11C]10 | 11.5 nM | 130 | [53] |
Fig. 1.
Chemical structures of CB2R tracers of oxoquinoline, thiazole, oxadiazole, and thiophene-based derivatives
CB2 imaging in animal models
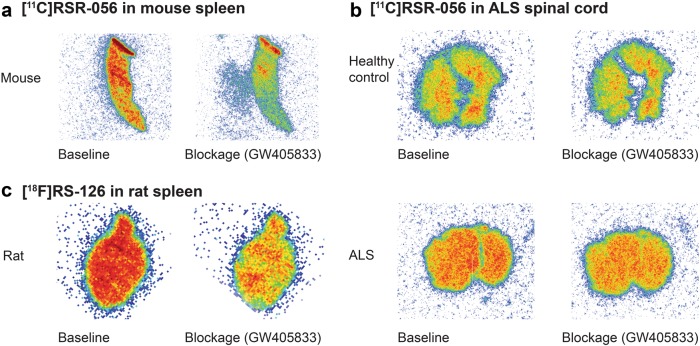
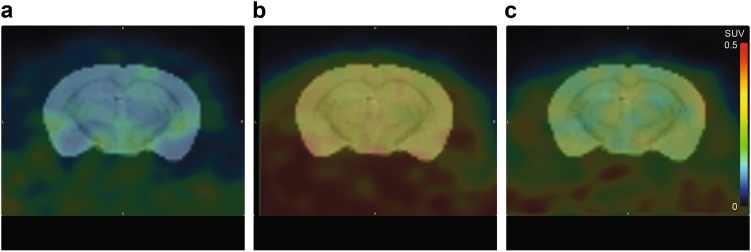
Spleen tissue, which is rich in CB2R, obtained from animals has been used to evaluate the specificity of CB2R tracers. Several CB2R tracers bind with high specificity in spleen tissue slices. Figure 2a, c show autoradiograms showing the specific binding using the PET tracers [11C]RSR-056 and [18F]RS-126. The accumulation of [11C]RSR-056 and [18F]RS-126 was blocked with the CB2R antagonist GW405833 in spleen slices obtained from a CD1 mouse and a Wistar rat. Different animal models have been used for the in vivo evaluation of CB2R tracers using PET imaging: (1) mouse and rat models with local human CB2R overexpression, as well as rhesus monkey [42] and (2) lipopolysaccharide (LPS)-injected mice and rats. The uptake of CB2R tracer in the brain is rather low, with a %ID/g of 0.1–0.4 at 1 h [33, 42] and a binding potential of 1.4–3 in animal models. Figure 3 shows the coronal view of [11C]RSR-056-PET overlaid on structural magnetic resonance imaging, demonstrating higher radioactivity retention in the cortex and hippocampus of an LPS-injected mouse (b) compared to a vehicle-injected mouse (a) and an LPS-injected + GW405833-treated mouse (c). The PET images were generated from averaged dynamic data at 20–60 min after the intravenous injection of [11C]RSR-056. The upregulation of CB2R detected by using [11C]RSR-056 appeared to be global instead of local, which might have been related to the specificity of the radiotracer. The results from a PET study using [11C]A-836339 showed no specific uptake in the rat brain intrastriatally injected with LPS and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid [34], although immunostaining for CB2R showed positive signals. Another PET study using [18F]RS-126 [28] or [18F]JHU94620 [35, 36] showed specific uptake in the CB2R-rich spleen, but not sufficient signals in the brain, of LPS-treated mice. LPS-injected models have been used to represent a pro-inflammatory rather than anti-inflammatory state. Thus, they might not be the most suitable for evaluating of CB2R.
Fig. 2.
Representative in vitro autoradiograms of CB2R tracers. a [11C]RSR-056 on spleen slices from a wild-type CD1 mouse. b [11C]RSR-056 on cervical spinal cord from a healthy control and a patient with amyotrophic lateral sclerosis (ALS). c [18F]RS-126 on spleen slices from a Wistar rat. Left: baseline binding; right: blockade with CB2R antagonist GW405833
Fig. 3.
Representative in vivo microPET images of coronal CD1 mouse brain sections (Bregma −1.5 mm ± 0.3 mm) by averaging dynamic data at 20–60 min after the intravenous injection of [11C]RSR-056. a Vehicle-treated mouse. b LPS-treated mouse. c LPS-treated mouse with antagonist GW405833. Scale 0–0.5. SUV standard uptake value
CB2R imaging in an animal model of stroke
Ischemic stroke involves a cascade of hemodynamic, vascular, structural, and inflammatory responses in a time-dependent manner [54–56]. Inflammation is implicated in the initial neuronal loss and consists mainly of pro-inflammatory responses and the extension of the lesion in the penumbra; the subsequent functional recovery involves anti-inflammatory responses. Upregulated CB2R mRNA was reported in a mouse focal ischemia model, peaking at 5 days and returning to normal at 10 days after occlusion [54]. Treatment with CB2R agonists has neuroprotective effects and attenuates macrophage/microglial activation in ischemic mouse models [54, 56–59].
The models of CB2R imaging in ischemic stroke animal have been inconclusive. An increased [11C]NE40 binding with no change in the binding of TSPO tracer [11C]PK11195 [43] was reported in an SD rat model of photothrombotic stroke at 24 h after surgery. Another study using [11C]NE40 imaging did not show an upregulated signal in a Wistar rat model of photothrombotic stroke [48], despite the minor increase in the level of CB2R seen by immunostaining. Low [11C]A-836339 uptake was detected in a rat model over 1–28 days after occlusion, despite positive immunostaining for CB2R and CD11 (markers for microglial activation) [34]. The utility of animal models of cerebral ischemia has been demonstrated in previous studies using TSPO tracers. Possible reasons for the different observations include the time point of assessment and differences between the stroke models. Different methods for inducing acute stroke (transient or permanent ischemia) result in variations in size, the severity of the ischemic regions, and the expression of inflammatory markers [56]. Since the pathophysiology and inflammatory levels and types evolve during the course of ischemic stroke, it is critical to reduce variations and make assessments at the optimal times. As CB2R are mostly associated with anti-inflammation, performing imaging, flow cytometry, and mRNA measurements at a subacute window 4–5 days after ischemia might be suitable [54].
CB2R imaging in animal models of Alzheimer's disease
AD is the most common neurodegenerative disease. The abnormal accumulation of amyloid-beta (Aβ) and tau aggregates leads to a cascade of pathophysiological changes, including inflammation, microvascular alternations, synaptic dysfunction, and neuronal loss. Microglia play a phagocytic role in the clearance of pathological protein deposits [60] and act as pro-inflammatory agents [61, 62]. Treatment with CB2R agonists in AD mouse models reverses Aβ-induced memory impairment [63]. MicroPET using [11C]A-836339 showed specific uptake in the brain areas with Aβ depositions in an APPswe/PS1dE9 mouse model of AD [33]. PET studies in some other AD mouse models using [11C]deprenyl in APPswe mice [20] and TSPO tracer [18F]GE180 in APP23 mice suggested increased astrocytosis and microgliosis at early disease stages. However, as age-related inflammation is also a confounding factor for the relatively mild inflammation in AD mouse models, these models might not be ideal for evaluating CB2R tracers.
CB2R imaging in animal models of multiple sclerosis
MS is an autoimmune inflammatory demyelinating disease [11]. In an experimental autoimmune encephalomyelitis (EAE) model of MS [64, 65], activated microglial cells had upregulated CB2R at the protein (10-fold) and at mRNA levels (100-fold) compared to ramified microglia. Recent clinical trials on the CB2R inhibitor delta(9)-tetrahydrocannabinol in patients with MS showed an ameliorating effect on the symptoms, including perceived spasticity and pain [66, 67]. Thus, PET tracers for CB2R receptors have the potential to detect the pathophysiology of MS and monitor the effects of treatment targeting CB2R in MS. However, in the EAE animal model, a clear disease status is considered difficult to define. Therefore, the EAE animal model might not be an ideal model for the evaluation of CB2R tracers.
Potential clinical use of CB2R PET imaging of CNS inflammation
Few clinical evaluations of CB2R PET imaging have been reported [45, 47]. The hurdles in CB2R tracer development and translation may include: (1) species differences between humans and rodents in their immune systems, microglia subtypes, and levels of CB2R expression [68], as well as distinct age-related changes, with a more pro-inflammatory type in humans [69] according to transcriptomic analysis; (2) low expression level of CB2R in the brain, even under inflammatory conditions [70]; (3) lack of specific CB2R antibody for post-mortem validation of in vivo imaging results [43, 55, 71]; (4) lack of full CB2R knock-out mice [72]; and 5) developing a reference region for modeling [73].
CB2R imaging in patients with amyotrophic lateral sclerosis
ALS is a progressive and fatal motor neuron disease [74]. A variety of genetic factors drive the degeneration of motor neurons and increase the susceptibility to ALS or influence the disease progression rate. A greater density of CB2R-positive microglia and macrophages was observed in the post-mortem spinal cord tissues from patients with ALS compared to healthy controls. Autoradiography using [11C]RSR-056 showed higher and specific binding on the post-mortem spinal cord tissues from patients with ALS compared to that from healthy controls (Fig. 2b). Similar increases were reported in other studies on ASL spinal cord tissues using [11C]RS-028 [31] and [11C]KD2 [22].
CB2R imaging in patients with Alzheimer's disease
Emerging evidence indicates the involvement of CB2R and increased levels of complements, cytokines, and chemokines in the brain of patients with AD. Reactive astrocytes, activated microglia, and upregulated CB2R were observed in the vicinity of Aβ plaques in post-mortem AD mouse model brains and patients with AD [62, 75–88]. PET using [11C]NE40 showed reduced signal along with Aβ deposition visualized by [11C]PIB in AD patients [47]. Further studies are needed to validate the utility of this tracer. A possible reason for these findings is that CB2R upregulation is below the detection threshold, which is evident in the spinal cord from patients with ALS (Fig. 2b). In addition, as CNS inflammation is considered an early event, evaluating patients with mild cognitive impairment at the early stage of the disease process will be informative.
Outlook
We propose several points for consideration during the development of CB2R tracers: (1) Subnanomolar-affinity CB2R tracers should be developed, considering the low expression level of the receptor. (2) We should elucidate whether CB2R upregulation is disease-stage dependent and relates to a certain type of microglia or astrocyte. (3) Structural optimization to improve the physicochemical and pharmacological properties of this new class of CB2R tracer will be necessary. (4) Flow cytometry should be used for surface phenotype characterization, e.g., CD45 and CD11 positivity and differentiating pro- and anti-inflammatory microglial subtypes and astrocytes. (5) Imaging results using CB2R and TSPO tracers should be compared head to head. Given that CB2R more closely represents anti-inflammatory features, additional knowledge of the inflammatory status in the CNS will be provided by PET imaging using both CB2R and TSPO tracers [43]. (6) The mRNA expression of CB2R should be measured. (7) Rational translation evaluation processes will be vital. Mouse and rat models of cerebral ischemia at 4–5 days after reperfusion might be a suitable model to test and validate CB2R tracers.
CB2R is also expressed on activated immune cells outside the CNS which represent potential targets for CB2R PET imaging. Recent CB2R imaging using [11C]RS-016 shows the detection of vascular inflammation in the post-mortem carotid plaque from humans and mouse models of atherosclerosis [30].
Conclusion
CB2R PET ligands will serve as useful tools for tracking the in vivo alterations in CNS inflammation during the progression of these disorders and for understanding the disease mechanisms. CB2R PET ligands will also help illuminate new treatment strategies for neurological disorders in which CNS inflammation is implicated.
Acknowledgements
This work was partly funded by the University of Zurich and the ETH Zurich Foundation through a Seed Grant of “University Medicine Zurich/Hochschulmedizin Zürich” and University of Zurich grant “Forschungskredit (Nr. FK-17-052)”.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stempel AV, Stumpf A, Zhang HY, Ozdogan T, Pannasch U, Theis AK, et al. Cannabinoid type 2 receptors mediate a cell type-specific plasticity in the hippocampus. Neuron. 2016;90:795–809. doi: 10.1016/j.neuron.2016.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Marzo V, Stella N, Zimmer A. Endocannabinoid signalling and the deteriorating brain. Nat Rev Neurosci. 2015;16:30–42. doi: 10.1038/nrn3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Sickle MD, Duncan M, Kingsley PJ, Mouihate A, Urbani P, Mackie K, et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310:329–332. doi: 10.1126/science.1115740. [DOI] [PubMed] [Google Scholar]
- 4.Xi ZX, Peng XQ, Li X, Song R, Zhang HY, Liu QR, et al. Brain cannabinoid CB(2) receptors modulate cocaine’s actions in mice. Nat Neurosci. 2011;14:1160–6. doi: 10.1038/nn.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang HY, Gao M, Liu QR, Bi GH, Li X, Yang HJ, et al. Cannabinoid CB2 receptors modulate midbrain dopamine neuronal activity and dopamine-related behavior in mice. Proc Natl Acad Sci USA. 2014;111:E5007–E5015. doi: 10.1073/pnas.1413210111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benito C, Tolón RM, Pazos MR. Cannabinoid CB2 receptors in human brain inflammation. Br J Pharmacol. 2008;153:277–85. doi: 10.1038/sj.bjp.0707505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heneka MT, Golenbock DT, Latz E. Innate immunity in Alzheimer’s disease [Review] Nat Immunol. 2015;16:229–36. doi: 10.1038/ni.3102. [DOI] [PubMed] [Google Scholar]
- 8.Graeber MB, Li W, Rodriguez ML. Role of microglia in CNS inflammation. FEBS Lett. 2011;585:3798–805. doi: 10.1016/j.febslet.2011.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Hirsch EC, Hunot S. Neuroinflammation in Parkinson’s disease: a target for neuroprotection? Lancet Neurol. 2009;8:382–97. doi: 10.1016/S1474-4422(09)70062-6. [DOI] [PubMed] [Google Scholar]
- 10.Philips T, Robberecht W. Neuroinflammation in amyotrophic lateral sclerosis: role of glial activation in motor neuron disease. Lancet Neurol. 2011;10:253–63. doi: 10.1016/S1474-4422(11)70015-1. [DOI] [PubMed] [Google Scholar]
- 11.Frischer JM, Bramow S, Dal-Bianco A, Lucchinetti CF, Rauschka H, Schmidbauer M, et al. The relation between inflammation and neurodegeneration in multiple sclerosis brains. Brain. 2009;132:1175–89. doi: 10.1093/brain/awp070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crotti A, Glass CK. The choreography of neuroinflammation in Huntington’s disease. Trends Immunol. 2015;36:364–73. doi: 10.1016/j.it.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rupprecht R, Papadopoulos V, Rammes G, Baghai TC, Fan J, Akula N. Translocator protein (18 kDa) (TSPO) as a therapeutic target for neurological and psychiatric disorders. Nat Rev Drug Discov. 2010;9:971–88. doi: 10.1038/nrd3295. [DOI] [PubMed] [Google Scholar]
- 14.Owen DR, Yeo AJ, Gunn RN, Song K, Wadsworth G, Lewis A, et al. An 18-kDa Translocator Protein (TSPO) polymorphism explains differences in binding affinity of the PET radioligand PBR28. J Cereb Blood Flow Metab. 2011;32:1–5. doi: 10.1038/jcbfm.2011.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamelin L, Lagarde J, Dorothee G, Leroy C, Labit M, Comley RA, et al. Early and protective microglial activation in Alzheimer’s disease: a prospective study using 18F-DPA-714 PET imaging. Brain. 2016;139:1252–64. doi: 10.1093/brain/aww017. [DOI] [PubMed] [Google Scholar]
- 16.Ikawa M, Lohith TG, Shrestha S, Telu S, Zoghbi SS, Castellano S, et al. 11C-ER176, a radioligand for 18-kDa translocator protein, has adequate sensitivity to robustly image all three affinity genotypes in human brain. J Nucl Med. 2017;58:320–5. doi: 10.2967/jnumed.116.178996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacobs AH, Tavitian B. Noninvasive molecular imaging of neuroinflammation. J Cereb Blood Flow Metab. 2012;32:1393–415. doi: 10.1038/jcbfm.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dupont AC, Largeau B, Santiago Ribeiro MJ, Guilloteau D, Tronel C, Arlicot N. Translocator protein-18 kDa (TSPO) Positron Emission Tomography (PET) imaging and its clinical impact in neurodegenerative diseases. Int J Mol Sci. 2017;18:785. doi: 10.3390/ijms18040785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kreisl WC, Lyoo CH, McGwier M, Snow J, Jenko KJ, Kimura N, et al. In vivo radioligand binding to translocator protein correlates with severity of Alzheimer’s disease. Brain. 2013;136:2228–38. doi: 10.1093/brain/awt145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodriguez-Vieitez E, Ni R, Gulyas B, Toth M, Haggkvist J, Halldin C, et al. Astrocytosis precedes amyloid plaque deposition in Alzheimer APPswe transgenic mouse brain: a correlative positron emission tomography and in vitro imaging study. Eur J Nucl Med Mol Imaging. 2015;42:1119–32. doi: 10.1007/s00259-015-3047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Varley J, Brooks DJ, Edison P. Imaging neuroinflammation in Alzheimer’s and other dementias: Recent advances and future directions. Alzheimers Dement. 2015;11:1110–20. doi: 10.1016/j.jalz.2014.08.105. [DOI] [PubMed] [Google Scholar]
- 22.Mu L, Bieri D, Slavik R, Drandarov K, Muller A, Cermak S, et al. Radiolabeling and in vitro /in vivo evaluation of N-(1-adamantyl)-8-methoxy-4-oxo-1-phenyl-1,4-dihydroquinoline-3-carboxamide as a PET probe for imaging cannabinoid type 2 receptor. J Neurochem. 2013;126:616–24. doi: 10.1111/jnc.12354. [DOI] [PubMed] [Google Scholar]
- 23.Mu L, Slavik R, Muller A, Popaj K, Cermak S, Weber M, et al. Synthesis and preliminary evaluation of a 2-oxoquinoline carboxylic acid derivative for PET imaging the cannabinoid type 2 receptor. Pharm (Basel) 2014;7:339–52. doi: 10.3390/ph7030339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yrjola S, Sarparanta M, Airaksinen AJ, Hytti M, Kauppinen A, Pasonen-Seppanen S, et al. Synthesis, in vitro and in vivo evaluation of 1,3,5-triazines as cannabinoid CB2 receptor agonists. Eur J Pharm Sci. 2015;67:85–96. doi: 10.1016/j.ejps.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Slavik R, Herde AM, Bieri D, Weber M, Schibli R, Kramer SD, et al. Synthesis, radiolabeling and evaluation of novel 4-oxo-quinoline derivatives as PET tracers for imaging cannabinoid type 2 receptor. Eur J Med Chem. 2015;92:554–64. doi: 10.1016/j.ejmech.2015.01.028. [DOI] [PubMed] [Google Scholar]
- 26.Slavik R, Grether U, Muller Herde A, Gobbi L, Fingerle J, Ullmer C, et al. Discovery of a high affinity and selective pyridine analog as a potential positron emission tomography imaging agent for cannabinoid type 2 receptor. J Med Chem. 2015;58:4266–77. doi: 10.1021/acs.jmedchem.5b00283. [DOI] [PubMed] [Google Scholar]
- 27.Slavik R, Bieri D, Cermak S, Muller A, Kramer SD, Weber M, et al. Development and evaluation of novel PET tracers for imaging cannabinoid receptor type 2 in brain. Chim (Aarau) 2014;68:208–10. doi: 10.2533/chimia.2014.208. [DOI] [PubMed] [Google Scholar]
- 28.Slavik R, Muller Herde A, Haider A, Kramer SD, Weber M, Schibli R, et al. Discovery of a fluorinated 4-oxo-quinoline derivative as a potential positron emission tomography radiotracer for imaging cannabinoid receptor type 2. J Neurochem. 2016;138:874–86. doi: 10.1111/jnc.13716. [DOI] [PubMed] [Google Scholar]
- 29.Haider A, Muller Herde A, Slavik R, Weber M, Mugnaini C, Ligresti A, et al. Synthesis and biological evaluation of thiophene-based cannabinoid receptor type 2 radiotracers for PET imaging. Front Neurosci. 2016;10:350. doi: 10.3389/fnins.2016.00350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meletta R, Slavik R, Mu L, Rancic Z, Borel N, Schibli R, et al. Cannabinoid receptor type 2 (CB2) as one of the candidate genes in human carotid plaque imaging: Evaluation of the novel radiotracer [11C]RS-016 targeting CB2 in atherosclerosis. Nucl Med Biol. 2017;47:31–43. doi: 10.1016/j.nucmedbio.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 31.Haider A, Spinelli F, Herde AM, Mu B, Keller C, Margelisch M, et al. Evaluation of 4-oxo-quinoline-based CB2 PET radioligands in R6/2 chorea huntington mouse model and human ALS spinal cord tissue. Eur J Med Chem. 2018;145:746–59. doi: 10.1016/j.ejmech.2017.12.097. [DOI] [PubMed] [Google Scholar]
- 32.Postnov A, Ahmad R, Evens N. Quantification of 11C-NE40, a novel PET radioligand for CB2 receptor imaging. J Nucl Med. 2013;54:2101–3. [Google Scholar]
- 33.Horti AG, Gao Y, Ravert HT, Finley P, Valentine H, Wong DF, et al. Synthesis and biodistribution of [11C]A-836339, a new potential radioligand for PET imaging of cannabinoid type 2 receptors (CB2) Bioorg Med Chem. 2010;18:5202–7. doi: 10.1016/j.bmc.2010.05.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pottier G, Gomez-Vallejo V, Padro D, Boisgard R, Dolle F, Llop J, et al. PET imaging of cannabinoid type 2 receptors with [11C]A-836339 did not evidence changes following neuroinflammation in rats. J Cereb Blood Flow Metab. 2017;37:1163–78. doi: 10.1177/0271678X16685105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moldovan RP, Deuther-Conrad W, Teodoro R, Wang Y, Fischer S, Pomper M, et al. 18F-JHU94620, a high affinity PET radioligand for imaging of cannabinoid subtype 2 receptors (CB2R) J Nucl Med. 2015;56:1048–1048. [Google Scholar]
- 36.Moldovan RP, Teodoro R, Gao Y, Deuther-Conrad W, Kranz M, Wang Y, et al. Development of a high-Affinity PET radioligand for imaging cannabinoid subtype 2 receptor. J Med Chem. 2016;59:7840–55. doi: 10.1021/acs.jmedchem.6b00554. [DOI] [PubMed] [Google Scholar]
- 37.Moldovan RP, Hausmann K, Deuther-Conrad W, Brust P. Development of highly affine and selective fluorinated cannabinoid type 2 receptor ligands. ACS Med Chem Lett. 2017;8:566–71. doi: 10.1021/acsmedchemlett.7b00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahamed M, van Veghel D, Ullmer C, Van Laere K, Verbruggen A, Bormans GM. Synthesis, biodistribution and in vitro evaluation of brain permeable high affinity type 2 cannabinoid receptor agonists [11C]MA2 and [18F]MA3. Front Neurosci. 2016;10:431. doi: 10.3389/fnins.2016.00431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caillà F, Cacheux F, Peyronneau MA, Jaumain E, Pottier G, Ullmer C, et al. Biodistribution of [18F] FC0324, a new PET tracer targeting CB2 receptors. J Nucl Med. 2017;58:855–855. [Google Scholar]
- 40.Spinelli F, Mu L, Ametamey SM. Radioligands for positron emission tomography imaging of cannabinoid type 2 receptor. J Label Comp Radiopharm. 2018;61:299–308. doi: 10.1002/jlcr.3579. [DOI] [PubMed] [Google Scholar]
- 41.Caille F, Cacheux F, Peyronneau MA, Jego B, Jaumain E, Pottier G, et al. From structure-activity relationships on thiazole derivatives to the in vivo evaluation of a new radiotracer for cannabinoid subtype 2 PET imaging. Mol Pharm. 2017;14:4064–78. doi: 10.1021/acs.molpharmaceut.7b00746. [DOI] [PubMed] [Google Scholar]
- 42.Evens N, Vandeputte C, Coolen C, Janssen P, Sciot R, Baekelandt V, et al. Preclinical evaluation of [11C]NE40, a type 2 cannabinoid receptor PET tracer. Nucl Med Biol. 2012;39:389–99. doi: 10.1016/j.nucmedbio.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 43.Hosoya T, Fukumoto D, Kakiuchi T, Nishiyama S, Yamamoto S, Ohba H, et al. In vivo TSPO and cannabinoid receptor type 2 availability early in post-stroke neuroinflammation in rats: a positron emission tomography study. J Neuroinflamm. 2017;14:69. doi: 10.1186/s12974-017-0851-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rühl T, Deuther-Conrad W, Fischer S, Günther R, Hennig L, Krautscheid H, et al. Cannabinoid receptor type 2 (CB2)-selective N-aryl-oxadiazolyl-propionamides: synthesis, radiolabelling, molecular modelling and biological evaluation. Org Med Chem Lett. 2012;2:32. doi: 10.1186/2191-2858-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahmad R, Koole M, Evens N, Serdons K, Verbruggen A, Bormans G, et al. Whole-body biodistribution and radiation dosimetry of the cannabinoid type 2 receptor ligand [11C]-NE40 in healthy subjects. Mol Imaging Biol. 2013;15:384–90. doi: 10.1007/s11307-013-0626-y. [DOI] [PubMed] [Google Scholar]
- 46.Vandeputte C, Casteels C, Struys T, Koole M, van Veghel D, Evens N, et al. Small-animal PET imaging of the type 1 and type 2 cannabinoid receptors in a photothrombotic stroke model. Eur J Nucl Med Mol Imaging. 2012;39:1796–806. doi: 10.1007/s00259-012-2209-6. [DOI] [PubMed] [Google Scholar]
- 47.Ahmad R, Postnov A, Bormans G, Versijpt J, Vandenbulcke M, Van Laere K. Decreased in vivo availability of the cannabinoid type 2 receptor in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2016;43:2219–27. doi: 10.1007/s00259-016-3457-7. [DOI] [PubMed] [Google Scholar]
- 48.Vandeputte C, Casteels C, Struys T, Koole M, van Veghel D, Evens N, et al. Small-animal PET imaging of the type 1 and type 2 cannabinoid receptors in a photothrombotic stroke model. Eur J Nucl Med Mol Imaging. 2012;39:1796–806. doi: 10.1007/s00259-012-2209-6. [DOI] [PubMed] [Google Scholar]
- 49.Gao M, Wang M, Miller KD, Hutchins GD, Zheng QH. Synthesis and in vitro biological evaluation of carbon-11-labeled quinoline derivatives as new candidate PET radioligands for cannabinoid CB2 receptor imaging. Bioorg Med Chem. 2010;18:2099–106. doi: 10.1016/j.bmc.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 50.Evens N, Vandeputte C, Muccioli GG, Lambert DM, Baekelandt V, Verbruggen AM, et al. Synthesis, in vitro and in vivo evaluation of fluorine-18 labelled FE-GW405833 as a PET tracer for type 2 cannabinoid receptor imaging. Bioorg Med Chem. 2011;19:4499–505. doi: 10.1016/j.bmc.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 51.Evens N, Bosier B, Lavey BJ, Kozlowski JA, Vermaelen P, Baudemprez L, et al. Labelling and biological evaluation of [(11)C]methoxy-Sch225336: a radioligand for the cannabinoid-type 2 receptor. Nucl Med Biol. 2008;35:793–800. doi: 10.1016/j.nucmedbio.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 52.Teodoro R, Moldovan RP, Lueg C, Gunther R, Donat CK, Ludwig FA, et al. Radiofluorination and biological evaluation of N-aryl-oxadiazolyl-propionamides as potential radioligands for PET imaging of cannabinoid CB2 receptors. Org Med Chem Lett. 2013;3:11. doi: 10.1186/2191-2858-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bertini S, Parkkari T, Savinainen JR, Arena C, Saccomanni G, Saguto S, et al. Synthesis, biological activity and molecular modeling of new biphenylic carboxamides as potent and selective CB2 receptor ligands. Eur J Med Chem. 2015;90:526–36. doi: 10.1016/j.ejmech.2014.11.066. [DOI] [PubMed] [Google Scholar]
- 54.Yu SJ, Reiner D, Shen H, Wu KJ, Liu QR, Wang Y. Time-dependent protection of CB2 receptor agonist in stroke. PLoS ONE. 2015;10:e0132487. doi: 10.1371/journal.pone.0132487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.England TJ, Hind WH, Rasid NA, O’Sullivan SE. Cannabinoids in experimental stroke: a systematic review and meta-analysis. J Cereb Blood Flow Metab. 2015;35:348–58. doi: 10.1038/jcbfm.2014.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bravo-Ferrer I, Cuartero MI, Zarruk JG, Pradillo JM, Hurtado O, Romera VG, et al. Cannabinoid type-2 receptor drives neurogenesis and improves functional outcome after stroke. Stroke. 2017;48:204–12. doi: 10.1161/STROKEAHA.116.014793. [DOI] [PubMed] [Google Scholar]
- 57.Ronca RD, Myers AM, Ganea D, Tuma RF, Walker EA, Ward SJ. A selective cannabinoid CB2 agonist attenuates damage and improves memory retention following stroke in mice. Life Sci. 2015;138:72–77. doi: 10.1016/j.lfs.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zarruk JG, Fernandez-Lopez D, Garcia-Yebenes I, Garcia-Gutierrez MS, Vivancos J, Nombela F, et al. Cannabinoid type 2 receptor activation downregulates stroke-induced classic and alternative brain macrophage/microglial activation concomitant to neuroprotection. Stroke. 2012;43:211–9. doi: 10.1161/STROKEAHA.111.631044. [DOI] [PubMed] [Google Scholar]
- 59.Zhang M, Martin BR, Adler MW, Razdan RK, Jallo JI, Tuma RF. Cannabinoid CB(2) receptor activation decreases cerebral infarction in a mouse focal ischemia/reperfusion model. J Cereb Blood Flow Metab. 2007;27:1387–96. doi: 10.1038/sj.jcbfm.9600447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Perry VH, Holmes C. Microglial priming in neurodegenerative disease. Nat Rev Neurol. 2014;10:217–24. doi: 10.1038/nrneurol.2014.38. [DOI] [PubMed] [Google Scholar]
- 61.Savonenko AV, Melnikova T, Wang Y, Ravert H, Gao Y, Koppel J et al. Cannabinoid CB2 receptors in a mouse model of Aβ amyloidosis: immunohistochemical analysis and suitability as a PET biomarker of neuroinflammation. PloS ONE. 2015;10:e0129618. [DOI] [PMC free article] [PubMed]
- 62.Aso E, Juves S, Maldonado R, Ferrer I. CB2 cannabinoid receptor agonist ameliorates Alzheimer-like phenotype in AβPP/PS1 mice. J Alzheimers Dis. 2013;35:847–58. doi: 10.3233/JAD-130137. [DOI] [PubMed] [Google Scholar]
- 63.Wu J, Bie B, Yang H, Xu JJ, Brown DL, Naguib M. Activation of the CB2 receptor system reverses amyloid-induced memory deficiency. Neurobiol Aging. 2013;34:791–804. doi: 10.1016/j.neurobiolaging.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 64.Maresz K, Carrier EJ, Ponomarev ED, Hillard CJ, Dittel BN. Modulation of the cannabinoid CB2 receptor in microglial cells in response to inflammatory stimuli. J Neurochem. 2005;95:437–45. doi: 10.1111/j.1471-4159.2005.03380.x. [DOI] [PubMed] [Google Scholar]
- 65.Zrzavy T, Hametner S, Wimmer I, Butovsky O, Weiner HL, Lassmann H. Loss of ‘homeostatic’ microglia and patterns of their activation in active multiple sclerosis. Brain. 2017;140:1900–13. doi: 10.1093/brain/awx113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zajicek J, Ball S, Wright D, Vickery J, Nunn A, Miller D, et al. Effect of dronabinol on progression in progressive multiple sclerosis (CUPID): a randomised, placebo-controlled trial. Lancet Neurol. 2013;12:857–65. doi: 10.1016/S1474-4422(13)70159-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Palazuelos J, Davoust N, Julien B, Hatterer E, Aguado T, Mechoulam R, et al. The CB(2) cannabinoid receptor controls myeloid progenitor trafficking: involvement in the pathogenesis of an animal model of multiple sclerosis. J Biol Chem. 2008;283:13320–9. doi: 10.1074/jbc.M707960200. [DOI] [PubMed] [Google Scholar]
- 68.Smith AM, Dragunow M. The human side of microglia. Trends Neurosci. 2014;37:125–35. doi: 10.1016/j.tins.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 69.Galatro TF, Holtman IR, Lerario AM, Vainchtein ID, Brouwer N, Sola PR, et al. Transcriptomic analysis of purified human cortical microglia reveals age-associated changes. Nat Neurosci. 2017;20:1162–71. doi: 10.1038/nn.4597. [DOI] [PubMed] [Google Scholar]
- 70.Chen DJ, Gao M, Gao FF, Su QX, Wu J. Brain cannabinoid receptor 2: expression, function and modulation. Acta Pharmacol Sin. 2017;38:312–6. doi: 10.1038/aps.2016.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nagayama T, Sinor AD, Simon RP, Chen J, Graham SH, Jin K, et al. Cannabinoids and neuroprotection in global and focal cerebral ischemia and in neuronal cultures. J Neurosci. 1999;19:2987–95. doi: 10.1523/JNEUROSCI.19-08-02987.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Constantinescu CS, Farooqi N, O’Brien K, Gran B. Experimental autoimmune encephalomyelitis (EAE) as a model for multiple sclerosis (MS) Br J Pharmacol. 2011;164:1079–106. doi: 10.1111/j.1476-5381.2011.01302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li Y, Kim J. Neuronal expression of CB2 cannabinoid receptor mRNAs in the mouse hippocampus. Neurosci. 2015;311:253–67. doi: 10.1016/j.neuroscience.2015.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Taylor JP, Brown RH, Jr, Cleveland DW. Decoding ALS: from genes to mechanism. Nature. 2016;539:197–206. doi: 10.1038/nature20413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Solas M, Francis PT, Franco R, Ramirez MJ. CB2 receptor and amyloid pathology in frontal cortex of Alzheimer’s disease patients. Neurobiol Aging. 2013;34:805–8. doi: 10.1016/j.neurobiolaging.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 76.Schmole AC, Lundt R, Ternes S, Albayram O, Ulas T, Schultze JL, et al. Cannabinoid receptor 2 deficiency results in reduced neuroinflammation in an Alzheimer’s disease mouse model. Neurobiol Aging. 2015;36:710–9. doi: 10.1016/j.neurobiolaging.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 77.Wu J, Hocevar M, Foss JF, Bie B, Naguib M. Activation of CB2 receptor system restores cognitive capacity and hippocampal Sox2 expression in a transgenic mouse model of Alzheimer’s disease. Eur J Pharmacol. 2017;811:12–20. doi: 10.1016/j.ejphar.2017.05.044. [DOI] [PubMed] [Google Scholar]
- 78.Koppel J, Vingtdeux V, Marambaud P, d’Abramo C, Jimenez H, Stauber M, et al. CB2 receptor deficiency increases amyloid pathology and alters tau processing in a transgenic mouse model of Alzheimer’s disease. Mol Med. 2014;20:29–36. doi: 10.2119/molmed.2013.00140.revised. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kofalvi A, Lemos C, Martin-Moreno AM, Pinheiro BS, Garcia-Garcia L, Pozo MA, et al. Stimulation of brain glucose uptake by cannabinoid CB2 receptors and its therapeutic potential in Alzheimer’s disease. Neuropharmacology. 2016;110:519–29. doi: 10.1016/j.neuropharm.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 80.Jayant S, Sharma BM, Bansal R, Sharma B. Pharmacological benefits of selective modulation of cannabinoid receptor type 2 (CB2) in experimental Alzheimer’s disease. Pharmacol Biochem Behav. 2016;140:39–50. doi: 10.1016/j.pbb.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 81.Aso E, Andres-Benito P, Carmona M, Maldonado R, Ferrer I. Cannabinoid receptor 2 participates in amyloid-beta processing in a mouse model of Alzheimer’s disease but plays a minor role in the therapeutic properties of a cannabis-based medicine. J Alzheimers Dis. 2016;51:489–500. doi: 10.3233/JAD-150913. [DOI] [PubMed] [Google Scholar]
- 82.Benito C, Nunez E, Tolon RM, Carrier EJ, Rabano A, Hillard CJ, et al. Cannabinoid CB2 receptors and fatty acid amide hydrolase are selectively overexpressed in neuritic plaque-associated glia in Alzheimer’s disease brains. J Neurosci. 2003;23:11136–41. doi: 10.1523/JNEUROSCI.23-35-11136.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Glass CK, Saijo K, Winner B, Marchetto MC, Gage FH. Mechanisms underlying inflammation in neurodegeneration. Cell. 2010;140:918–34. doi: 10.1016/j.cell.2010.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fuger P, Hefendehl JK, Veeraraghavalu K, Wendeln AC, Schlosser C, Obermuller U, et al. Microglia turnover with aging and in an Alzheimer’s model via long-term in vivo single-cell imaging. Nat Neurosci. 2017;20:1371–6. doi: 10.1038/nn.4631. [DOI] [PubMed] [Google Scholar]
- 85.Cagnin A, Brooks D, Kennedy A, Gunn R, Myers R, Turkheimer F, et al. In-vivo measurement of activated microglia in dementia. Lancet. 2001;358:461–7. doi: 10.1016/S0140-6736(01)05625-2. [DOI] [PubMed] [Google Scholar]
- 86.Martin-Moreno AM, Brera B, Spuch C, Carro E, Garcia-Garcia L, Delgado M, et al. Prolonged oral cannabinoid administration prevents neuroinflammation, lowers beta-amyloid levels and improves cognitive performance in Tg APP 2576 mice. J Neuroinflamm. 2012;9:8. doi: 10.1186/1742-2094-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Saccomanni G, Pascali G, Carlo SD, Panetta D, De Simone M, Bertini S, et al. Design, synthesis and preliminary evaluation of (18)F-labelled 1,8-naphthyridin- and quinolin-2-one-3-carboxamide derivatives for PET imaging of CB2 cannabinoid receptor. Bioorg Med Chem Lett. 2015;25:2532–5. doi: 10.1016/j.bmcl.2015.04.055. [DOI] [PubMed] [Google Scholar]
- 88.Ramirez BG, Blazquez C, Gomez del Pulgar T, Guzman M, de Ceballos ML. Prevention of Alzheimer’s disease pathology by cannabinoids: neuroprotection mediated by blockade of microglial activation. J Neurosci. 2005;25:1904–13. doi: 10.1523/JNEUROSCI.4540-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]