Abstract
Increasingly, patients are seeking minimally invasive methods to tighten skin and remodel adipose tissue. A large treatment gap exists among 3 types of patients: (1) the younger demographic, who increasingly desire soft tissue tightening without traditional operations, scars, and downtime; (2) patients with soft tissue laxity who are not “severe enough” to justify an excisional procedure, but not “mild enough” to rely on liposuction with soft tissue contraction alone; and (3) those with recurrent laxity who already underwent traditional excisional procedures. In these populations, plastic surgeons risk under- or overtreating with traditional methods. The purpose of this supplement is to describe the utility of radiofrequency (RF) microneedling (Fractora modified to Morpheus8 InMode Aesthetic Solutions, Lake Forest, CA) in combination with bipolar RF (FaceTite/BodyTite, InMode Aesthetic Solutions). By combining these procedures, the aforementioned treatment gap can be addressed. The RF microneedling allows for subdermal adipose remodeling and skin tightening. Addition of bipolar RF also tightens the skin by contraction of the underlaying fibroseptal network in addition to induction of neocollagenesis, elastogenesis, and angiogenesis at skin surface temperatures of 40° to 50°C. In our experience, these technologies have been effective and safe in these patient populations.
Level of Evidence: 4
Minimally invasive skin tightening and adipose reduction has long been an elusive goal of aesthetic surgery.1-5 Multiple energy-based technologies including laser, high-intensity focused ultrasound, and radiofrequency (RF) have evolved to meet this rising demand.1,6-12 RF technology has steadily gained popularity since the early 2000s with consecutive increases in use of 10% or more annually.11-13 These gains encompass aesthetic surgery as well as numerous nonaesthetic applications (tissue electrodissection, cardiac catheter ablation, ophthalmic surgery, etc.).11
Public demand for minimally invasive skin tightening continues to grow.11 This has been in response to a widening treatment gap prevalent among 3 cohorts of patients: (1) the younger demographic, who increasingly desire soft tissue tightening without traditional operations, scars, and downtime; (2) patients with soft tissue laxity who are not “severe enough” to justify an excisional procedure, but not “mild enough” to rely on liposuction with soft tissue contraction alone; and (3) those with recurrent laxity who already underwent traditional excisional procedures. In these populations, plastic surgeons risk under- or overtreating with traditional methods.
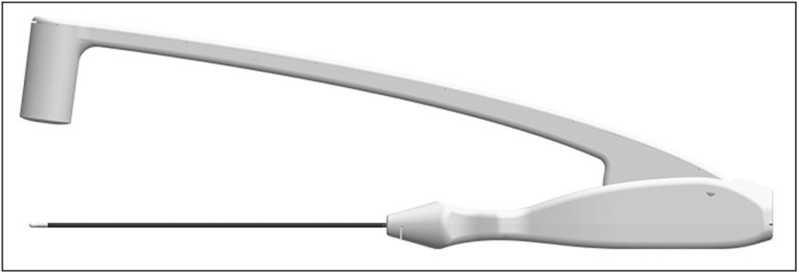
RF achieves skin tightening by thermal heating of the reticular dermis, which triggers a healing cascade leading to collagen formation.14,15 Tissue resistance of electrical current allows for variable impedance and rates of heat generation. For example, fat is an insulator and has high resistance to current flow (producing more heat), and water is closest to a pure conductor (producing less heat).4,16 New collagen, elastin, and blood vessel formation occurs as skin surface temperatures reach 40° to 45°C.1,2,17-19 In contrast to laser, RF is chromophore independent and has a better safety profile for all skin types in terms of pigmentation changes.16 There are different types of RF for medical utilization including monopolar, bipolar, fractional, and multipolar energy modes. Monopolar RF utilizes one emitting pole with the body serving as a ground. In the bipolar RF devices, there are 2 electrodes at a set distance with a current flowing between them (Figure 1). Multipolar RF utilizes multiple electrodes to emit energy at various changing directions to allow for deeper as well as more superficial penetration of energy.
Figure 1.
Bipolar radiofrequency device (Facetite, InMode Aesthetic Solutions, Lake Forest, CA).
Non-energy-based devices such as microneedling serve as a minimally invasive method to induce dermal collagen formation and skin resurfacing through induction of an inflammatory cascade while preserving the epidermal barrier. This technology was first introduced by Orentreich in 1995 for the treatment of atrophic scars and rhytids. It has since been successfully employed for acne, melasma, photodamage, transcutaneous drug delivery, alopecia, and skin rejuvenation.6,9,20-23 The local injury induced by dermal penetration of the microneedles releases growth factors (ie, TFG-alpha, beta, VEGF, PDGF) that stimulate collagen and elastin fiber production, as well as angiogenesis.
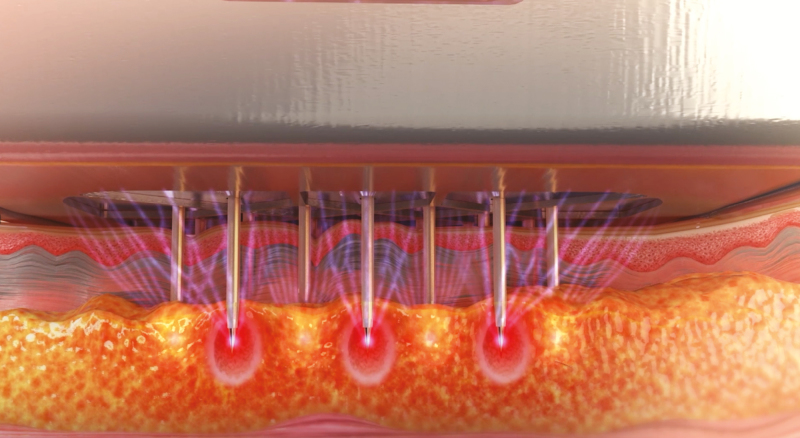
RF microneedling systems advance existing technology by adding heat at controlled depths (Figure 2). Similar to fractional laser, fractional RF microneedling treats segments of the skin and soft tissue, leaving islands of untreated areas to reduce recovery time. Studies have shown active dermal remodeling by 10 weeks post-procedure with increased reticular dermal volume, hyaluronic acid, and elastin content.8,24 This purpose of this manuscript is to describe the utilization of RF microneedling (Fractora modified to Morpheus8, InMode Aesthetic Solutions) with or without bipolar RF (FaceTite/BodyTite, InMode Aesthetic Solutions).
Figure 2.
Radiofrequency microneedling device (Morpheus8, InMode Aesthetic Solutions, Lake Forest, CA).
RADIOFREQUENCY MICRONEEDLING
The Morpheus8 (InMode Aesthetic Solutions) is a fractional RF device with programmable penetration depth and energy delivery (Figure 2). The 24 coated needles penetrate into the subdermal tissue, leading to coagulation of fat as well as contraction of the reticular dermis and surrounding connective tissue. At the same time, directional RF energy stimulates neocollagenesis, elastogenesis, and angiogenesis (Figure 3). The adjustable penetration depth and energy settings allow the clinician to customize treatment. In the face, treatment may be 1 to 2 mm, whereas for body areas a 3-mm to 4-mm depth penetration would be appropriate. There is an additional 1-mm zone of heat effect that should be accounted for when planning treatment.
Figure 3.
Illustration of radiofrequency microneedling depth and effect.
Treatment Procedure
Pretreatment
A detailed history and physical are obtained to determine if there are any contraindications to treatment (ie, collagen disorders, active infection, immunocompromised state, pregnancy, poor wound healing, unrealistic expectations). Valcyclovir is recommended for patients with a history of herpes simplex.
Anesthesia
Numerous anesthesia options are available depending on energy employed, depth of treatment, and patient tolerance. Topical anesthesia applied for 45 to 60 minutes can be utilized if energy is limited and tolerated by the patient. Some patients require nerve blocks or local anesthesia for higher energy settings.
Treatment
RF microneedling treatment parameters are (Table 1):
Table 1.
Radiofrequency Treatment Parameters
| Depth | Treatment areas | Depth of penetration | RF energy level | Treatment mode (cycle/fixed) | No. of sessions | Weeks between sessions | Downtime (days) |
|---|---|---|---|---|---|---|---|
| Periorbital | Bony areas, periorbital, forehead, chin | 2 mm | 15-30 | Cycle | 1-3 | 3-6 | 2-5 |
| Facial | Soft tissue, neck | 3 mm | 20-40 | Cycle/fixed | 1-3 | 3-6 | 2-5 |
| Body | Body areas | 4 mm | 25-40 | Cycle/fixed | 1-3 | 3-6 | 2-5 |
RF, radiofrequency.
Depth: automatically set for the anatomic area
RF energy: varies from 5 to 62 kw
Cycle mode: needles penetrate the skin and retract from the skin with every pulse
Fixed mode: needles are inserted into the skin and energy is delivered when the footswitch is activated. The needles retract from the skin and energy stops once the footswitch is released. This can be employed for stacking of pulses when desired.
Repetition mode: single pulse mode or autorepeat mode when pulses are delivered automatically with predetermined pulse repetition rate.
The handpiece is applied firmly and perpendicular to the treatment area. The footswitch is pressed to deliver RF energy: one press for each pulse for sensitive and small areas like the periorbital region, or continuous press for fixed mode. The handpiece is moved to the adjacent area with an overlap of approximately 50%. The handpiece should be completely released from the skin rather than sliding the needles to avoid abrasions. Then 1 to 2 additional pulses may be applied at the same site (stacking) in fixed mode. However, pulses should not be stacked over bony areas such as the forehead, periorbita, jawline, etc. (Video 1). Minor pinpoint bleeding may be encountered. Treatment may be applied to all skin types. It is important to restrict energy when treating dark Fitzpatrick skin types by starting at 15 kw or lower, adding 5 kw of energy gradually with each treatment course (to a maximum energy level of 40 kw over soft tissue, 25 kw over bone). Higher RF energy can be applied to deeper treatment areas. When working on thin skin (ie, neck) or in bony areas (ie, forehead, jawline), energy should be reduced by 20% and stacking of pulses should be avoided.
Post-Treatment
Cooling of the skin immediately post-procedure can reduce discomfort and erythema/edema. Antibiotic ointment is typically applied 1 to 3 days post-procedure. During this time, patients should refrain from other topical agents (ie, sunscreen or makeup). Once the microneedle holes close (within 1-3 days), makeup, moisturizer, and sunscreen may be applied.
EXAMPLES OF CLINICAL APPLICATIONS OF RF MICRONEEDLING
Early Facial Aging and Recurrent Laxity After Facelift
Increasingly, young patients present with early facial aging (ie, jowls, neck skin laxity) and are not yet optimal candidates for a traditional facelift. Additionally, there is a large population of patients who already underwent a facelift and suffer from recurrent laxity. These groups are ideal candidates for RF microneedling, which reliably and safely achieves skin tightening and subdermal adipose remodeling. Similarly, in this group of patients, conventional liposuction of the neck and mandibular border often leads to unpredictable soft tissue contraction.
We have noticed in our clinical practice that patients respond best to RF microneedling combined with bipolar RF (Embrace Protocol, InMode Aesthetic Solutions). The RF microneedling component allows for tightening of the skin and remodeling of the subdermal adipose tissue, and the bipolar RF (FaceTite, InMode Aesthetic Solution) produces deep tissue heating (pre- superficial-musculo-aponeurotic-system/platysma) to tighten the overlying fibroseptal network. This combination of deep and superficial energy delivery optimizes treatment and soft tissue response (Figures 4 and 5; Video 2).
Figure 4.
(A) Preoperative view of this 55-year-old woman with submental and jowl skin laxity. (B) Postoperative view of the patient 6 months after radiofrequency microneedling to jowls and submental area demonstrating improved skin laxity.
Figure 5.
(A) This is a 47-year-old woman with abdominal skin laxity. (B) Six months after bipolar radiofrequency and radiofrequency microneedling treatment of anterior abdomen. Note preoperative supraumbilical skin laxity that is improved with radiofrequency treatment and not suction assisted liposuction alone.
We prospectively evaluated 247 patients (224 female, 23 male; mean age, 55 years; range, 26-67 years) undergoing this combination RF therapy for neck laxity and jowling. Their pretreatment average Baker Face Neck Classification was 3.1 (standard deviation ± 1.4). The post-treatment objective improvement was 1.4 points (standard deviation ± 1.1), and 93% of patients indicated they were pleased with their results and would undergo the procedure again. Complications included prolonged swelling >6 weeks (4.8%, 12/247), hardened area >12 weeks (3.2%, 8/247), and neuropraxia (1.2%, 3/247), which all resolved without further intervention.
Brachioplasty
According to the 2017 American Society of Aesthetic Plastic Surgery Data Bank, approximately 18,000 arm lifts were performed, up 20.1% from the prior year.12 Despite this increasing number, brachioplasty is limited by poor scarring, dehiscence, seroma, and infection. There are often focal areas of adiposity proximal to the elbow as well as of the lateral chest that are challenging to treat with traditional arm-lift and lead to contour deformities. Ultrasonic and laser-assisted liposuction have attempted to solve this problem with superficial application of heat to induce skin tightening. However, these have been complicated by inadequate tightening (ie, inadequate generation of heat) and high risk for contour deformities.
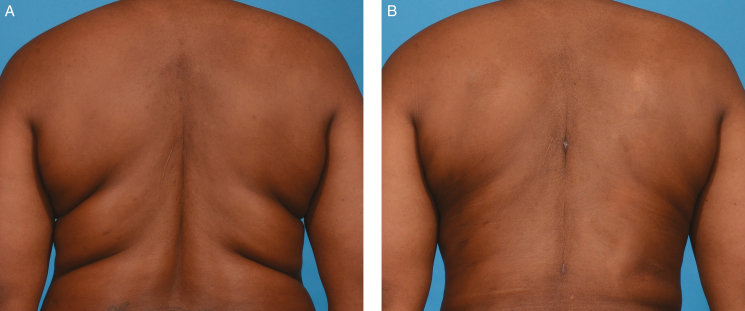
Theodorou et al described near circumferential (270 degrees) RF-assisted liposuction of the upper arms in 40 patients.3,4 An objective plastic surgeon evaluated the results as good to excellent tightening of the soft tissue envelope in the majority of patients. There were minimal complications in this cohort (1 seroma resolved with aspiration and 1 burn treated with wound care).3 In our clinical experience, the addition of RF microneedling to this protocol serves to augment the tightening effect of bipolar RF as well as broadens the ability to treat challenging areas such as fat pads proximal to the elbow or at the arm/axillary junction (Figure 6).
Figure 6.
(A) This is a 44-year-old woman who was bothered by backrolls. (B) Six months after treatment of backrolls with bipolar radiofrequency and radiofrequency microneedling.
Focal Areas of Excess Skin Adiposity
Common areas of localized adiposity include the axillary rolls, soft tissue proximal to the knee, as well as supra and infraumbilical region. These areas are especially challenging in patients with poor skin elasticity who do not desire skin excision but also would not retract with traditional liposuction techniques. The large number of these “in between” patients represents a treatment gap that has been shown to benefit from RF microneedling. These areas benefit from deeper treatment (4000 μm) to ablate the adipose tissue as well as maximally tighten the skin, with or without bipolar RF tightening of fibroseptal networks.
DISCUSSION
The addition of RF microneedling to bipolar RF in the face and body has allowed for a safe, reliable, and effective treatment of patients who fall into the aforementioned treatment gap. In properly selected patients, we have combined these technologies to the application of RF heat from the superficial and deep directions and achieved satisfactory results without increased complications.
Bipolar RF provides deep heat generation to the overlaying soft tissue and ultimately reticular dermis. Utilizing a parachute analogy, the heat contracts the strings (fibroseptal network) holding the parachute (ie, skin) in place, leading to a uniform and concerted contraction effect from below. The addition of RF microneedling augments our results by heating tissue from the superficial surface directly to the dermis and subdermal elements. One significant advantage of the RF microneedling treatment is the ability to directly generate heat in the subdermal adipose tissue and impact the contour of fat in this region while tightening the overlaying dermis.
Numerous clinical studies support the efficacy of RF therapy for aesthetic skin tightening of the face and body. The goal of RF therapy is not to replace excisional procedures when indicated, but rather to achieve skin tightening in the “treatment gap” population, broadening the plastic surgeon’s armamentarium. Seo et al compared facial soft tissue laxity improvement with RF vs surgical facelift employing blinded grading of photographs. They demonstrated a 49% improvement in skin laxity relative to baseline for surgical facelift compared with 16% for fractional RF. Further, the mean laxity improvement from a single fractional RF treatment was 37% of the surgical facelift.25 Peterson et al also studied objective measurements of mechanical skin properties and demonstrated a statistically significant improvement (5%-12% decrease in Young’s modulus and 10%-16% decrease in retraction time) as well as 1.42 grade improvement on the Fitzpatrick scale for wrinkles and 0.66 on the Alexiades scale for skin laxity, increasing to 1.57 and 0.70, respectively, improvement at 6 months. Patient satisfaction was noted to be “very high” for >90% of patients.17
As demonstrated in this manuscript, our clinical experience has shown that the combination of bipolar RF and RF microneedling can achieve substantial skin tightening and subdermal adipose coagulation and necrosis in patients who are not candidates or prefer to not undergo surgery. Complications are rare when employed judiciously in the appropriately selected patients; however, they may include thermal burns, contour deformities, and superficial nerve injury. There are a number of limitations to our study including the subjectivity of the Baker face scale as well as patient satisfaction survey. There are more objective scales that are currently being applied to prospectively collected data including the Fitzpatrick wrinkle scale and Alexiades skin laxity scale as well as surface area measurements.
CONCLUSIONS
The demand for minimally invasive solutions to avoid traditional operative treatment continues to increase. RF technology has emerged as an effective method to safely tighten skin and reduce underlying adipose tissue. As our armamentarium expands, we have the opportunity to treat large portions of the population who were previously considered premature or borderline candidates for excisional operations. In our experience, combination RF technology (RF microneedling and bipolar RF) advances and broadens our ability to achieve tissue retraction that does not reliably occur with other energy-based devices and liposuction alone.
Disclosures
Dr Dayan is a Consultant to InMode Aesthetic Solutions and Owner of wikiPlasticSurgery.com. Drs Chia and Theodorou are Consultants to InMode Aesthetic Solutions. Dr Burns is a Consultant to Allergan, HINTMD, InMode Aesthetic Solutions, and Sciton.
Funding
This article was supported by the InMode Corporation (Toronto, Canada), who co-funded the development of this supplement.
Supplementary Material
REFERENCES
- 1. Chia CT, Theodorou SJ, Hoyos AE, Pitman GH. Radiofrequency-assisted liposuction compared with aggressive superficial, subdermal liposuction of the arms: a bilateral quantitative comparison. Plast Reconstr Surg Glob Open. 2015;3(7):e459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Theodorou SJ, Paresi RJ, Chia CT. Radiofrequency-assisted liposuction device for body contouring: 97 patients under local anesthesia. Aesthetic Plast Surg. 2012;36(4):767-779. [DOI] [PubMed] [Google Scholar]
- 3. Theodorou S, Chia C. Radiofrequency-assisted liposuction for arm contouring: technique under local anesthesia. Plast Reconstr Surg Glob Open. 2013;1(5):e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Theodorou SJ, Del Vecchio D, Chia CT. Soft tissue contraction in body contouring with radiofrequency-assisted liposuction: a treatment gap solution. Aesthet Surg J. 2018;38(suppl_2):S74-S83. [DOI] [PubMed] [Google Scholar]
- 5. Irvine Duncan D. Nonexcisional tissue tightening: creating skin surface area reduction during abdominal liposuction by adding radiofrequency heating. Aesthet Surg J. 2013;33(8):1154-1166. [DOI] [PubMed] [Google Scholar]
- 6. Alster TS, Graham PM. Microneedling: a review and practical guide. Dermatol Surg. 2018;44(3):397-404. [DOI] [PubMed] [Google Scholar]
- 7. Brightman L, Weiss E, Chapas AM, et al. Improvement in arm and post-partum abdominal and flank subcutaneous fat deposits and skin laxity using a bipolar radiofrequency, infrared, vacuum and mechanical massage device. Lasers Surg Med. 2009;41(10):791-798. [DOI] [PubMed] [Google Scholar]
- 8. Fritz K, Salavastru C. Ways of noninvasive facial skin tightening and fat reduction. Facial Plast Surg. 2016;32(3):276-282. [DOI] [PubMed] [Google Scholar]
- 9. Iriarte C, Awosika O, Rengifo-Pardo M, Ehrlich A. Review of applications of microneedling in dermatology. Clin Cosmet Investig Dermatol. 2017;10:289-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sadick NS, Makino Y. Selective electro-thermolysis in aesthetic medicine: a review. Lasers Surg Med. 2004;34(2): 91-97. [DOI] [PubMed] [Google Scholar]
- 11. American Society of Plastic Surgeons. New Statistics Reveal the Shape of Plastic Surgery 2018 https://www.plasticsurgery.org/news/press-releases/new-statistics-reveal-the-shape-of-plastic-surgery. Accessed November 10, 2018.
- 12. Cosmetic Surgery National Data Bank Statistics. Aesthet Surg J. 2018;38(suppl_3):1-24. [DOI] [PubMed] [Google Scholar]
- 13. Sadick N, Rothaus KO. Minimally invasive radiofrequency devices. Clin Plast Surg. 2016;43(3):567-575. [DOI] [PubMed] [Google Scholar]
- 14. Hantash BM, Ubeid AA, Chang H, Kafi R, Renton B. Bipolar fractional radiofrequency treatment induces neoelastogenesis and neocollagenesis. Lasers Surg Med. 2009;41(1):1-9. [DOI] [PubMed] [Google Scholar]
- 15. Kaplan H, Kaplan L. Combination of microneedle radiofrequency (RF), fractional RF skin resurfacing and multi-source non-ablative skin tightening for minimal-downtime, full-face skin rejuvenation. J Cosmet Laser Ther. 2016;18(8):438-441. [DOI] [PubMed] [Google Scholar]
- 16. Alster TS, Lupton JR. Nonablative cutaneous remodeling using radiofrequency devices. Clin Dermatol. 2007;25(5):487-491. [DOI] [PubMed] [Google Scholar]
- 17. Peterson JD, Palm MD, Kiripolsky MG, Guiha IC, Goldman MP. Evaluation of the effect of fractional laser with radiofrequency and fractionated radiofrequency on the improvement of acne scars. Dermatol Surg. 2011;37(9):1260-1267. [DOI] [PubMed] [Google Scholar]
- 18. Fajkošová K, Machovcová A, Onder M, Fritz K. Selective radiofrequency therapy as a non-invasive approach for contactless body contouring and circumferential reduction. J Drugs Dermatol. 2014;13(3):291-296. [PubMed] [Google Scholar]
- 19. Seo KY, Kim DH, Lee SE, Yoon MS, Lee HJ. Skin rejuvenation by microneedle fractional radiofrequency and a human stem cell conditioned medium in Asian skin: a randomized controlled investigator blinded split-face study. J Cosmet Laser Ther. 2013;15(1):25-33. [DOI] [PubMed] [Google Scholar]
- 20. Shah KB, Shah AN, Solanki RB, Raval RC. A comparative study of microneedling with platelet-rich plasma plus topical minoxidil (5%) and topical minoxidil (5%) alone in androgenetic alopecia. Int J Trichology. 2017;9(1):14-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cercal Fucci-da-Costa AP, Reich Camasmie H. Drug delivery after microneedling: report of an adverse reaction. Dermatol Surg. 2018;44(4):593-594. [DOI] [PubMed] [Google Scholar]
- 22. Konicke K, Knabel M, Olasz E. Microneedling in dermatology: a review. Plast Surg Nurs. 2017;37(3):112-115. [DOI] [PubMed] [Google Scholar]
- 23. Ramaut L, Hoeksema H, Pirayesh A, Stillaert F, Monstrey S. Microneedling: Where do we stand now? A systematic review of the literature. J Plast Reconstr Aesthet Surg. 2018;71(1):1-14. [DOI] [PubMed] [Google Scholar]
- 24. Issa MC, de Britto Pereira Kassuga LE, Chevrand NS, et al. Transepidermal retinoic acid delivery using ablative fractional radiofrequency associated with acoustic pressure ultrasound for stretch marks treatment. Lasers Surg Med. 2013;45(2):81-88. [DOI] [PubMed] [Google Scholar]
- 25. Seo KY, Yoon MS, Kim DH, Lee HJ. Skin rejuvenation by microneedle fractional radiofrequency treatment in Asian skin; clinical and histological analysis. Lasers Surg Med. 2012;44(8):631-636. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.