Abstract
Background
Ethiopia is one of the four low income countries in achieving MDG4, however, minimizing child undernutrition became critical undertaking thus far. This review aimed at identifying the predictors of under-5 children nutrition in Ethiopia.
Methods
Databases searched were Med Line, HINARY, MedNar and Embase. Furthermore, gray literatures were also sought. All papers selected for inclusion in the review were subjected to a rigorous critical appraisal using standardized critical appraisal instruments from the Joanna Briggs Institute. Quantitative papers were pooled for statistical analysis and narrative synthesis. Odds ratios and their 95% confidence intervals were calculated for analysis. Papers of optimal quality but without optimal data set for meta-analysis were subjected for narrative synthesis
Results
Nonadherence towards Optimal feeding recommendations was the most reported predictor of stunting and wasting, while, maternal education and ‘Water, Sanitation and Hygiene’ factors were the second. The findings of the Meta-analysis showed no evidence of association between household income/wealth and stunting of children in Ethiopia (OR=1.14, 95% CI= 0.97, 1.34), heterogeneity test: i2 = 92%, df = 20, (P < 0.00001). On the other hand, children in low income/wealth group were 1.73 times more likely to have wasting compared to children of the higher income/wealth households (OR=1.73, 95% C I= 1.51, 1.97) heterogeneity test: i2 = 71%, df = 20, (P < 0.00001).
Conclusion
An over-reliance on macroeconomic growth as a solitary factor towards undernutrition should not be the way forward. Supplementary and more focused nutrition specific and sensitive interventions are needed in Ethiopia.
Keywords: child undernutrition, systematic review, metaanalysis, Ethiopia
Introduction
In 2010, the Ethiopian government endorsed a comprehensive implementation plan to reduce the prevalence of stunting of under five children from 44.4 to 30% and wasting from 9.7 to 3% through the remained era of Millennium Development Goal (1). However the results were far below, only 6.4% and 0.7% percent reductions of stunting and wasting were achieved (2). There existed very high proportion of stunting (38%) and wasting (9%) among under-five children in Ethiopia (2). On the other hand, the country recorded substantial reductions in child mortality through the extraordinary commitment given to the millennium development goals for the same age group (3). Being one of the four low income countries in the world in achieving MDG4, yet, having high level of malnutrition for the same age group seems paradoxical. Ethiopia has enjoyed strong and broad based economic growth over the past decade, averaging 10.8% per year in 2003/04 – 2014/15 compared to the regional (east African) average of 5.4% (4). However, minimizing the amenable size of child undernutrition in the country has been critical undertaking thus far.
Child under nutrition and economic growth are not always at par across the globe. According to a study, the elasticity of stunting with respect to growth in per capita is on average −0.2 in a country having 30% stunting prevalence, which is at the most one-tenth of the growth elasticity of income/consumption (5). This insignificant effect may explain why considerable variation existed in the prevalence of chronic malnutrition in less developed world (5% to 65%) (6). The extreme disparity further signals the need for in-depth look towards drivers of better child nutrition beyond macro-economic variables. Contrary to what the economy would suggest, a number of Sub-Saharan African countries has lower levels of stunting compared to East and South Asia (7). Some nations are experiencing disproportionately high levels of stunting for their economy such as India (8). Similar disparity also exist within the same continent context too, Senegal have much lower level of stunting level(19%) than its neighboring countries with similar economy such as Mali (39%) and Guinea (31%) during the period of 2010–2015 (9).
It is certainly plausible that an increase in household's income possibly influence child's nutritional outcome either by improving dietary intake or access for health care and better environment. On the other hand, poverty erodes household's potential for optimal child care and feeding leading to under nutrition. Contrary to the above more likely conditions, a significant portion of under-5 children among richest households were affected by under nutrition across the globe (10–13). In the regions with the highest rates of stunting (Sub-Saharan Africa and South Asia) quarter of the stunted under 5 children were members of richest households (12). Socioeconomic inequality in malnutrition between children of poor and rich families vary from country to country, large gaps observed in Peru and very small in Egypt (13). In summary, the existing research indicates income/expenditures matters for nutrition but the link tends to be not sufficient enough (5, 10–14). One of the reason can be due to strong suboptimal proximal factors such as inadequate feeding and ill health which could dilute any positive gains possibly achieved by distal determinants (income/expenditures).
Some measure of household economic well-being is assessed in health and nutrition studies mostly as income or wealth. However, direct expenditure on nutritional factors such as food and health care would have been appropriate to measure direct effects of economic environment on nutritional outcomes (15). In majority of nutrition studies done in developing world consumption expenditure data were not collected due to complex methodological issues (16). Studies including demographic health surveys (DHS) instead compute asset based wealth index as proxy measure of economic wellbeing (1, 15–17). The underlying assumption of using wealth index as a proxy of expenditure could possibly confounded by a number of important issues such as intra-household resource allocation and control over resource (15–16). Despite the limitations, using wealth indices as alternative methods is better than measuring income (15).
Most nutritional decision in the Ethiopia are based on DHS which were thus far descriptive and limited in terms of analysis of associations between nutritional status and immediate, underlining and basic factors as depicted in global framework for malnutrition (1, 12). Combining these two data set through gregarious systematic review process is appropriate in order to generate the best available evidence on determinants of under-5 children nutritional status of the country. Some of these studies were conducted with the aim of studying determinants of malnutrition, yet didn't consider economic measures such as wealth index or income. Though, such analysis seems technically correct, it does not allow to understand the isolated effect of variables like maternal education, as it is not adjusted for poverty; making the results less valuable as policy making.
The primary objective of the review was to systematically identify, appraise and synthesize the best available evidence on association of economic wellbeing of households and under-5 children nutritional outcomes in Ethiopia. Thus, we specifically questioned whether there is an association between low HH income/wealth and undernutrition among under 5 children in Ethiopia existed or not. Since the review dealt with extreme conditions, aggregating income and wealth index as the same proxy may not be a concern. Meanwhile, we also set out to critically appraise, identify and present the commonest predictors of under-5 children stunting and wasting in Ethiopia
Methods
To conduct the present review the recommendations and tools of the Systematic the Joanna Briggs Institute (JBI) Model for Systematic Reviews of Evidence was adopted (18). Studies which included children of under five years of age, with objectively measured nutritional outcome in terms of height for age and weight for height reported, regardless of other demographic characteristics were included. All types of quantitative observational and analytical studies (cohort studies, case-control studies and crosssectional studies) made from January 1st, 2000 to December 31st 2016 were included. No exclusion were made based on publication format and study characteristics. Conference proceedings, qualitative studies, case series and reports were excluded. The lowest income/wealth group of households as reported in the studies were extracted to compare against the remaining groups of households in the studies. All studies including those without optimal data for the metaanalysis were also subjected for the narrative synthesis done for the second objective.
Three staged search strategy was used to identify all relevant published literature in English language. An initial search of MEDLINE and Google Scholar followed by analysis of the text words in the text and abstract was done to generate comprehensive list of words and index terms. A second search was made using all identified key words and index terms across all data bases. The third search was done by analyzing reference list of included study. Databases searched were Med Line, HINARY, MedNar and Embase. Furthermore, gray literatures were sought from SCOPUS, Ethiopian higher institutions depositaries and the Ethiopian government websites. The search strategy used or modified for the various databases and search engines was with initial keywords/search terms: [“stunting” or “wasting” or “malnutrition” or “mal-nutrition” “under nutrition” or “under-nutrition” or “acute malnutrition” or “chronic malnutrition” or “protein energy malnutrition”] and [“under 5 children” or “children” or “infant” or “young child”] and [“Ethiopia”]. Further entry terms were collected following what was obtained from initial search.
Study selection appraisal and extraction were made in duplicate to reduce reviewer error. All papers selected for inclusion in the review were subjected to a rigorous, independent appraisal by the investigators prior to inclusion in the review using standardized critical appraisal instruments from the Joanna Briggs Institute (JBI-MAStARI critical appraisal tool) (18). This check list has different modules based on the study design. Appraisal were made by both reviewers independently and disagreements were solved through discussion. For inclusion, only studies which scored above 50% of the risk of bias assessment were included as per the instrument recommendations.
Quantitative papers were pooled in statistical meta-analysis using the Review Manager Software (Rev Man 5.3) (19). We used random effect model in the Meta-analysis and Mantel-Haenszel model to calculate odds ratios and their 95% confidence intervals. Papers of optimal quality but without optimal data for meta-analysis were subjected for narrative synthesis. Data on the outcome and their distribution in income/wealth were extracted as proportions while predictors were listed out for descriptive analysis. To enhance objectivity and considering their variability in measurement we have pre-formulated composite predictors thematically as optimal feeding, ‘Water and Environmental sanitation and hygiene’ (WASH) factors, sociodemographic, biologic and health care seeking and related factors.
Results
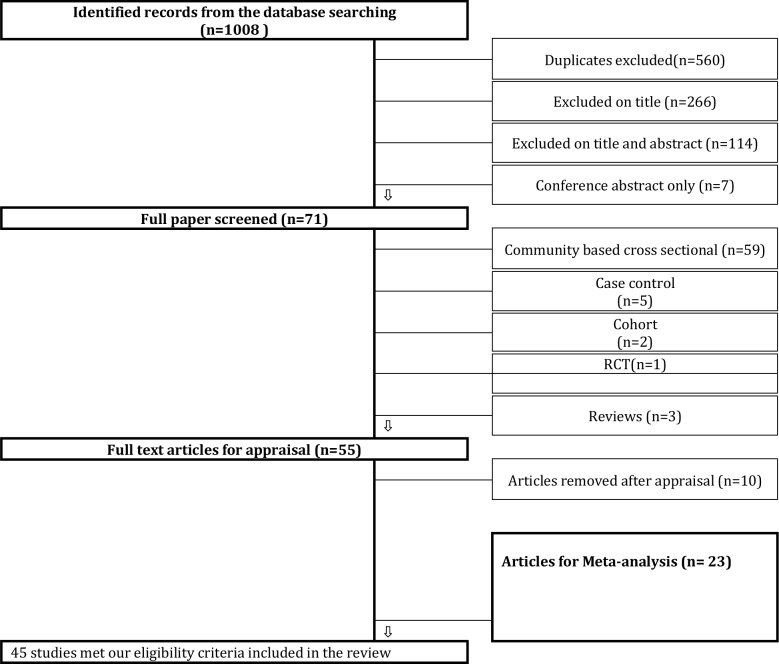
A total of 1008 relevant papers were identified in the literature search, 560 were duplicates, remaining 448 were retrieved for examination. Following review of titles and abstracts against the review objectives and inclusion criteria, 377 titles were excluded. The full texts of the remaining 71 studies were retrieved for detailed evaluation, after which, 16 of these were excluded. The remaining 55 studies were assessed for methodological quality using the JBI-MAStARI critical appraisal tool, and, subsequently 10 were excluded because of sub optimal quality. The remaining 45 were included in the current systematic review. Over 90% of the included studies were surveys, distributed north to south. Data set to conduct meta-analysis for the primary objective were available only in 23 studies. All studies were included in the narrative synthesis (Figure 1).
Figure 1.
Flowchart of literature review process
Association of stunting and households income/wealth in Ethiopia
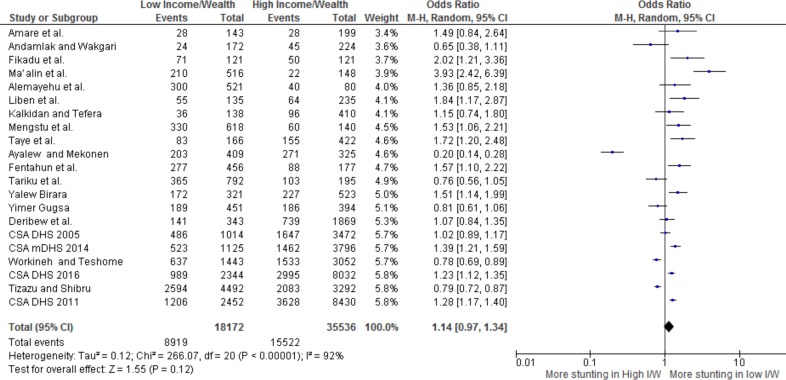
On Meta-analysis, anthropometric data of 53,708 children were stratified based on their income/wealth strata, as low and high income/wealth households. Accordingly, from the total children, 18172 were members of households with low income/wealth, while the remaining 35,536 children were residents of households with higher income/wealth. Among children of households with low income/wealth almost half (49%) had stunting. On the other hand, 15,522 (43.7%) of children living in higher income/wealth group were found to have stunting.
The finding of the Meta-analysis showed no evidence of association between income/wealth and stunting of children in Ethiopia (Odds ratio=1.14, 95% Confidence Interval= 0.97, 1.34), heterogeneity test: i2 = 92%, df = 20, (P < 0.00001). The test for overall effect also showed statistical insignificance at conventional levels (P=0.12) (Figure 2).
Figure 2.
Forest plot Income/wealth versus under 5 children stunting in Ethiopia
Association of wasting and households income/wealth in Ethiopia
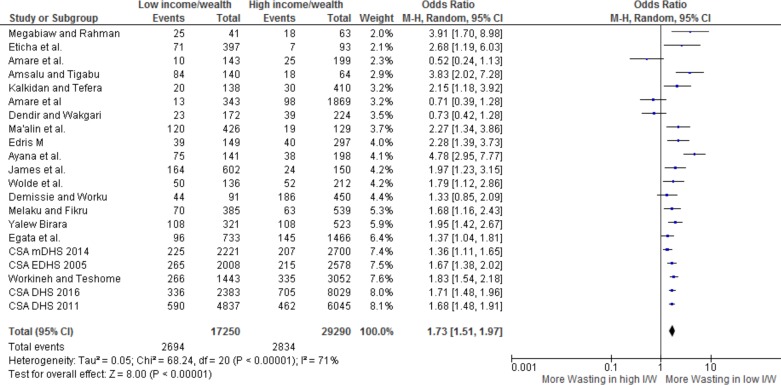
On Meta-analysis, anthropometric data of 46540 children were stratified based on their household income/wealth strata, of which 17250 were children living in households having low income/wealth Among households in low income/wealth, 2694 (15.6%) children were found to have wasting. On the other hand a lower proportion of children were found in households having higher income/wealth group 2834 (9.7%). The finding of the Meta-analysis showed children in low income/wealth group were 1.73 times more likely to have wasting compared to children of the higher income/wealth households (Odds ratio=1.73, 95% Confidence Interval= 1.51, 1.97) heterogeneity test: i2 = 71%, df = 20, (P < 0.00001). The test for overall effect also showed a high statistical significance at conventional levels (P<0.00001) (Figure 3).
Figure 3.
Forest plot Income/wealth versus under 5 children stunting in Ethiopia
Predictors of wasting and stunting in Ethiopia
In the current review, non-adherence towards Optimal feeding recommendations of WHO was found the most reported predictor of stunting (n=21studies) while maternal education is the second most reported independent predictor (n=19studies) of stunting. Among biologic factors Child's age (n=18 studies) and child's Sex (n=10 studies) reported as predictors of stunting. Morbidity (n=6 studies), optimal health care practice by the mother or the child (immunization, deworming, antenatal care, family planning) were also reported by 4 studies. Residence (urban versus rural) is the most reported socio-demographic variable (n=9 studies) while ‘Water, Sanitation and Hygiene’ (WASH) factors were reported by five authors predicting stunting. Morbidity (fever, diarrhea, ARI) was reported by six authors. Few authors reported food insecurity as predictor of stunting (n=2 studies). In similar analysis of wasting, non-adherence towards Optimal feeding recommendations of WHO was found the most reported predictor of wasting (n=12 studies). Unlike stunting factors “Water, Sanitation and Hygiene” factors were found the second most important predictors (n=10 studies). Maternal education is also reported by six authors. Among biologic factors Child's age (n=4studies) and child Sex of the child (n=6 studies) were the most reported predictor of wasting. Morbidity (n=6 studies), optimal health care practice by the mother or the child (immunization, antenatal care and family planning) were reported as predictor by four authors. Residence and family size were reported each by three authors. Similar to stunting predictors, food insecurity is reported only by two authors as predictor of wasting.
Discussion
In the current review, results of both analysis were complimentary, affirming the need to have more reliance on optimal child feeding and maternal education to achieve better under-5 children nutrition than macroeconomic growth in Ethiopia. It is not surprising to have optimal child feeding appeared the commonest predictor of undernutrition in the studies, considering the prevalent maternal illiteracy in the country (47.6 %) (2). According to the recent DHS reports, only 2% of mother adhere to the WHO IYCF recommendations and only 7 percent of children age 6–23 months have met the criteria for a minimum acceptable diet (2, 39). The fact that optimal feeding and maternal education commonly appearing in the reviewed literatures has a clear policy implication regarding the focus of nutrition interventions. Making the mother at “the center” of policy and nutrition programs is indispensable in Ethiopia. Similar to the current review, maternal education regularly emerges as a key element of an overall strategy to address malnutrition in developing world (63–64). A global study of Smith et al (2009), also confirmed women education responsible for 43% of the total 15.5% reduction in the child malnutrition rate of 63 developing countries during the period 1970–95(64).
The present review findings fairly decline the association of low income/wealth of households and chronic malnutrition of under-five children in Ethiopia. The review finding corroborates, a study in The Lancet Global Health, which looks at DHS data from 1990 to 2011 of 36 low- and middle-income countries, and suggested that increases in per-head gross domestic product in the last two decades have generally not been associated with improvements in childhood nutritional status (65). Phenomenally, in Ethiopia, progress against child under nutrition since the millennium has been solid, with stunting prevalence reduced by 1.4 percent points per year between 2001 and 2011, then slowed down to 1.0 point per year since 2011 despite unchanged economic potential (66). The current review finding also decline earlier findings by Headey (2014) and Biadglign et al (2016) regarding wealth and stunting (66–67). The possible explanation for difference could be due to the superiority the current review in terms of number of studies included and difference in methods of analysis. Despite our approach is different, there is exact similarity of our findings with Woodruff et al, who identified variables that could have contributed to the decline of stunting in Ethiopian children less than 5 years of age as markers of child health, mother's nutritional status, mother's educational level, and environmental hygiene (57).
Unlike stunting, wasting in the current meta-analysis showed association with income/wealth. Children living in low income/wealth households were found 1.7 times more likely to have wasting. The positive effect of higher income/wealth on wasting prevalence is comprehendible as wasting drag better attention for all segment of care giving continuum. In most cases, wasting is a reflection of a recent and severe process of weight loss associated with acute starvation and/or disease state. Thus, there is high probability of wealthier families to take their sick child to health facilities before evident wasting process on their child begins. Such associations are reported throughout the DHS reports of the country (2, 39–41). On the other hand stunting often goes unrecognized in communities where short stature is so common. “Water, Sanitation and Hygiene” factors were critical in wasting prevalence in Ethiopia indicating the inter play of disease process (most likely diarrhea) in the existing prevalence (68). In conclusion, factors related to optimal care were dominantly appeared as predictor of under-5 children nutrition in Ethiopia over the studied economic indicators (income or wealth). In general the present evidence emphasize the need to have more focus on factors beyond economic measures to achieve local and global goals, such as, the Seqota declaration and the sustainable development goals of countries by the end of 2030 (69). The Seqota Declaration reflects the strong commitment to end child malnutrition in Ethiopia by reaching vulnerable households. In guiding such interventions, economic vulnerability alone shouldn't be taken to identify and locate vulnerable households for development of chronic malnutrition. Assessment of multiple aspects of proximal to distal determinants of optimal nutritional outcome are critically needed. Thus, an overreliance on macroeconomic growth as a compelling solitary factor to revert chronic malnutrition should be avoided. Instead, supplementary and more focused nutrition sensitive and specific interventions that aimed at improving optimal feeding practice and child rearing environment would be more important in Ethiopia.
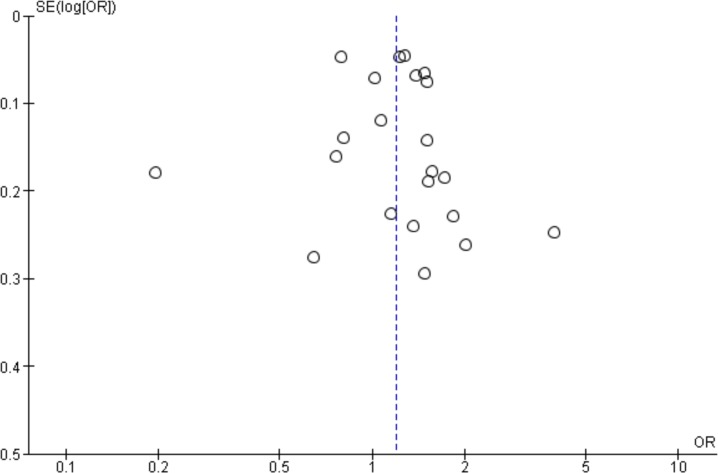
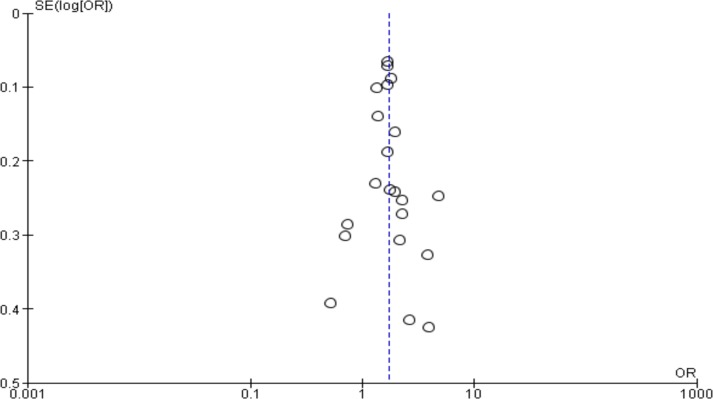
While using the present evidence, one should note the strength and limitations in the present analysis. The study documented less publication bias as it sourced out all quality gray literatures (figure 4 and 5), subjected for critical appraisal. The funnel plot also showed studies plotted near the average, and studies which spread evenly on both sides of the average, creating a roughly funnel-shaped distribution indicating less publication bias. However, data were generally not available on important aspects of income such as intrahousehold resource allocation to have subgroup analysis of important aspect of income/wealth identify. Second, The analysis showed a significant heterogeneity as measured by Cochrane's I2, which could be resulted from the variation among the included studies in measuring wealth/income.
Figure 4.
Funnel lot for assessment of publication bias, Income/wealth versus stunting
Figure 5.
Funnel lot for assessment of publication bias, Income/wealth versus stunting
Acknowledgements
We would like to acknowledge Dr. Yimam Workineh for editorial support.
References
- 1.Government of the Federal Democratic Republic of Ethiopia, author. National Nutrition Programme, June 2013 — June 2015. Addis Ababa Ethiopia: [02 December 16]. Available at: https://www.unicef.org/ethiopia/National_Nutrition_Programme.pdf. [Google Scholar]
- 2.Central Statistical Agency and ICF International, Ethiopian Demographic, Health Survey. Addis Ababa, Ethiopia and Calverton, Maryland, USA: 2016. [02 January 17]. Available at: https://dhsprogram.com/pubs/pdf/PR81/PR81.pdf. [Google Scholar]
- 3.The World Bank, author. Ethiopia, Economic Overview. [02 January 17]. Available at: http://www.worldbank.org/en/country/ethiopia/overview. [Google Scholar]
- 4.Heltberg R. Malnutrition, poverty, and economic growth. Health Economics. 2009 Apr 1;18(S1) doi: 10.1002/hec.1462. [DOI] [PubMed] [Google Scholar]
- 5.Wang H, Bhutta ZA, Coates MM, et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016 Oct 8;388(10053):1725–1774. doi: 10.1016/S0140-6736(16)31575-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO, author. Global Database on Child Growth and Malnutrition. [02 January 17]. Available at: http://www.who.int/nutgrowthdb/about/introduction/en/index2.html.
- 7.Misselhorn M, Harttgen K. A Multilevel Approach to Explain Child Mortality and Undernutrition in South Asia and Sub-Saharan Africa. Discussion papers//Ibero America Institute for Economic Research. 2006. [02 December 16]. Available at: http://www2.vwl.wiso.unigoettingen.de/ibero/working_paper_neu/DB152.pdf.
- 8.Subramanian SV, Mejía-Guevara I, Krishna A. Rethinking policy perspectives on childhood stunting: time to formulate a structural and multifactorial strategy. Maternal & child nutrition. 2016 May 1;12(S1):219–236. doi: 10.1111/mcn.12254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UNICEF, author. UNICEF Data; Monitoring the Situation of Children and Women. [02 January 17]. Available at: https://data.unicef.org/resources/jointchild-malnutrition-estimates-2016-edition/
- 10.Subramanyam MA, Kawachi I, Berkman LF, Subramanian SV. Is economic growth associated with reduction in child undernutrition in India? PLoS Med. 2011 Mar 8;8(3):e1000424. doi: 10.1371/journal.pmed.1000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Breisinger C, El-Batrawy R. Nutrition and economic development: Exploring Egypt's exceptionalism and the role of food subsidies. Intl Food Policy Res Inst. 2016 Nov 15; [Google Scholar]
- 12.Unicef, author. Improving child nutrition: the achievable imperative for global progress. New York: 2013. Apr, [02 December 16]. Available at: https://www.unicef.org/gambia/Improving_Child_Nutritionthe_achievable_imperative_for_global_progress.pdf. [Google Scholar]
- 13.Adam W, Naoke W. World Bank Policy Research Working Paper No. 2434. “Socioeconomic Inequalities in Child Malnutrition in the Developing World”. [Google Scholar]
- 14.Vollmer S, Harttgen K, Subramanyam MA, Finlay J, Klasen S, Subramanian SV. Association between economic growth and early childhood undernutrition: evidence from 121 Demographic and Health Surveys from 36 low-income and middle-income countries. The lancet global health. 2014 Apr 30;2(4):e225–e234. doi: 10.1016/S2214-109X(14)70025-7. [DOI] [PubMed] [Google Scholar]
- 15.Howe LD, Hargreaves JR, Huttly SR. Issues in the construction of wealth indices for the measurement of socio-economic position in low-income countries. Emerging themes in epidemiology. 2008 Jan 30;5(1):3. doi: 10.1186/1742-7622-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rutstein Shea O. The DHS Wealth. 11785 Beltsville Drive, Suite 300, Calverton: Demographic and Health Research Division, ICF International; Available at: https://dhsprogram.com/pubs/pdf/CR6/CR6.pdf. [Google Scholar]
- 17.Howe LD, Hargreaves JR, Gabrysch S, Huttly SR. Is the wealth index a proxy for consumption expenditure? A systematic review. Journal of epidemiology and community health. 2009 Nov 1;63(11):871–877. doi: 10.1136/jech.2009.088021. [DOI] [PubMed] [Google Scholar]
- 18.Joanna Briggs Institute, author. The JBI Approach. [02 September 16]. Available at; http://joannabriggs.org/jbiapproach.html.
- 19.Review Manager (RevMan) [Computer program]. Version [5.3] Copenhagen: The Nordic Cochrane Centre, the Cochrane Collaboration; 2014. [Google Scholar]
- 20.Edris M. Assessment of nutritional status of preschool children of Gumbrit, North West Ethiopia. Ethiopian Journal of Health Development. 2007;21(2):125–129. [Google Scholar]
- 21.Deribew A, Alemseged F, Tessema F, et al. Malaria and under-nutrition: a community based study among under-five children at risk of malaria, south-west Ethiopia. PLoS One. 2010 May 21;5(5):e10775. doi: 10.1371/journal.pone.0010775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.James P, Sadler K, Wondafrash M, Argaw A, Luo H, Geleta B, Kedir K, Getnet Y, Belachew T, Bahwere P. Children with Moderate Acute Malnutrition with No Access to Supplementary Feeding Programmes Experience High Rates of Deterioration and No Improvement: Results from a Prospective Cohort Study in Rural Ethiopia. PloS one. 2016 Apr 21;11(4):e0153530. doi: 10.1371/journal.pone.0153530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fentahun W, Wubshet M, Tariku A. Undernutrition and associated factors among children aged 6–59 months in East Belesa District, northwest Ethiopia: a community based cross-sectional study. BMC public health. 2016 Jun 13;16(1):506. doi: 10.1186/s12889-016-3180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eticha K, Solomon S, Fikru T. Prevalence and Determinants of Child Malnutrition in Gimbi district. 2006. Jun, [02 November 16]. pp. 27–39. Available at: http://hdl.handle.net/123456789/3097. [Google Scholar]
- 25.Mengistu K, Alemu K, Destaw B. Prevalence of malnutrition and associated factors among children aged 6–59 months at Hidabu Abote District, North Shewa, Oromia Regional State. J Nutr Disorders Ther. doi: 10.4172/2161-0509.T1-001. T1 001. [DOI] [Google Scholar]
- 26.Amare D, Negassie A, Tsegaye B, et al. Prevalence of Undernutrition and Its Associated Factors among Children below Five Years of Age in Bure Town, West Gojjam Zone, Amhara National Regional State, Northwest Ethiopia. Advances in Public Health. 2016 Aug 1; 2016. [Google Scholar]
- 27.Wolde T, Adeba E, Sufa A. Prevalence of Chronic Malnutrition (Stunting) and Determinant Factors among Children Aged 0–23 Months in Western Ethiopia: A Cross-Sectional Study. Journal of Nutritional Disorders & Therapy. 2014 Oct 31; 2014. [Google Scholar]
- 28.Dendir A, Wakgari D. Disclosing the Relationship between Maternal Empowerment and Food Security Status on Stunting, Underweight and Wasting among 6–36 Month Old Children in Gurage Zone, Southern Ethiopia. [02 November 16]. Available at: etd.aau.edu.et/bitstream/123456789/8232/1/Andamlak%20Dendir.pdf.
- 29.Demissie S, Worku A. Magnitude and factors associated with malnutrition in children 6–59 months of age in pastoral community of Dollo Ado district, Somali region, Ethiopia. Science Journal of Public Health. 2013;1(4):175–183. [Google Scholar]
- 30.Melese Birara. Prevalence of Malnutrition and Associated Factors among Children Age 6–59 Months at Lalibela Town Administration, North Wollo Zone, Northern Ethiopia. J Nutr Disorders Ther. 4:132. doi: 10.4172/2161-0509.1000132. [DOI] [Google Scholar]
- 31.Gugsa Y. Malnutrition among children in Southern Ethiopia: Levels and risk factors. Ethiopian Journal of Health Development. 2000;14(3):283–292. [Google Scholar]
- 32.Liben ML, Abuhay T, Haile Y. Determinants of Child Malnutrition among Agro Pastorals in Northeastern Ethiopia: A Cross-Sectional Study. Health Science Journal. 2016;10(4):15. [Google Scholar]
- 33.Tariku B, Mulugeta A, Tsadik M, Azene G. Prevalence and Risk Factors of Child Malnutrition in Community Based Nutrition Program Implementing and Non implementing Districts from South East Amhara, Ethiopia. OALib Journal. 2014;1:e425. doi: 10.4236/oalib.1100425. [DOI] [Google Scholar]
- 34.Ma'alin A, Birhanu D, Melaku S, et al. Magnitude and factors associated with malnutrition in children 6–59 months of age in Shinille Woreda, Ethiopian Somali regional state: a cross-sectional study. BMC Nutrition. 2016 Jul 15;2(1):44. [Google Scholar]
- 35.Ayana AB, Hailemariam TW, Melke AS. Determinants of acute malnutrition among children aged 6–59 months in Public Hospitals, Oromia region, West Ethiopia: a case-control study. BMC Nutrition. 2015 Nov 19;1(1):1. [Google Scholar]
- 36.Egata G, Berhane Y, Worku A. Predictors of acute undernutrition among children aged 6 to 36 months in east rural Ethiopia: a community based nested case-control study. BMC pediatrics. 2014 Apr 4;14(1):1. doi: 10.1186/1471-2431-14-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amsalu S, Tigabu Z. Risk factors for ever acute malnutrition in children under the age of five: a case-control study. Ethiopian Journal of Health Development. 2008;22(1):21–25. [Google Scholar]
- 38.Central Statistical Agency, author. Mini demographic and health survey. Addis Ababa, Ethiopia: 2014. [15 December 15]. Available at: http://www.unicef.org/ethiopia/Mini_DHS_2014__Final_Report.pdf. [Google Scholar]
- 39.Central Statistical Agency and ICF International, Ethiopian Demographic, Health Survey. Addis Ababa, Ethiopia and Calverton, Maryland, USA: 2011. [02 January 16]. Available at: http://www.unicef.org/ethiopia/ET_2011_EDHS.pdf. [Google Scholar]
- 40.Central Statistical Agency and ICF International, Ethiopian Demographic, Health Survey. 2005. Available at: https://www.unicef.org/ethiopia/DHS_2005_Ethiopia.pdf.
- 41.Ayalew E, Mekonin H. The prevalence of stunting and associated factors among children age 6–59 months at mizan-aman town, bench Maji zone, SNNP region, Ethiopia. Addis Ababa university institutional depository; 2015. [02 January 17]. Available at: http://etd.aau.edu.et/bitstream/123456789/7955/1/Ermias%20Ayalew.pdf. [Google Scholar]
- 42.Abate KH, Belachew T. Care and not wealth is a predictor of wasting and stunting of ‘The Coffee Kids' of Jimma Zone, southwest Ethiopia. Nutrition and health. 2017 Sep;23(3):193–202. doi: 10.1177/0260106017706253. [DOI] [PubMed] [Google Scholar]
- 43.Central Statistical Agency and ICF International, Ethiopian Demographic, Health Survey. 2000. [02 January 17]. Available at: www.dhsprogram.com/pubs/pdf/FR118/FR118.pdf.
- 44.Teshome B, Kogi-Makau W, Getahun Z, Taye G. Magnitude and determinants of stunting in children underfive years of age in food surplus region of Ethiopia: the case of west gojam zone. Ethiopian Journal of Health Development. 2009 Jan 1;23(2) [Google Scholar]
- 45.Girma W, Genebo T. Determinants of Nutritional Status of Women and Children in Ethiopia. Calverton, Maryland, USA: ORC Macro; [02 January 17]. Available at: http://www.popline.org/node/234790. [Google Scholar]
- 46.Yisak H, Gobena T, Mesfin F. Prevalence and risk factors for under nutrition among children under five at Haramaya district, Eastern Ethiopia. BMC pediatrics. 2015 Dec 16;15(1):1. doi: 10.1186/s12887-015-0535-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taye A, Tsedeke W, Anwar S. Undernutrition and Related Factors among Children Aged 6–59 Months in Gida Ayana District, Oromiya Region, West Ethiopia: A Community Based Quantitative Study. J Nutr Food Sci. 2016;6:5. doi: 10.4172/2155-9600.1000543. [DOI] [Google Scholar]
- 48.Asfaw M, Wondaferash M, Taha M, Dube L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public health. 2015 Jan 31;15(1):1. doi: 10.1186/s12889-015-1370-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alemayehu M, Tinsae F, Haileslassie K, Seid O, Gebregziabher G, Yebyo H. Undernutrition status and associated factors in under-5 children, in Tigray, Northern Ethiopia. Nutrition. 2015 Aug 31;31(7):964–970. doi: 10.1016/j.nut.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 50.Fikadu T, Assegid S, Dube L. Factors associated with stunting among children of age 24 to 59 months in Meskan district, Gurage Zone, South Ethiopia: a case-control study. BMC public health. 2014 Aug 7;14(1):1. doi: 10.1186/1471-2458-14-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roba K, O'Connor T, Belachew T, O'Brien N. Variations between post-and pre-harvest seasons in stunting, wasting, and Infant and Young Child Feeding (IYCF) practices among children 6–23 months of age in lowland and midland agro-ecological zones of rural Ethiopia. The Pan African medical journal. 2016:24. doi: 10.11604/pamj.2016.24.163.9387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ersino G, Henry CJ, Zello GA. Suboptimal Feeding Practices and High Levels of Undernutrition among Infants and Young Children in the Rural Communities of Halaba and Zeway, Ethiopia. Food and nutrition bulletin. 2016 Jul 11; doi: 10.1177/0379572116658371. 0379572116658371. [DOI] [PubMed] [Google Scholar]
- 53.Kang Y, Kim S, Sinamo S, Christian P. Effectiveness of a community-based nutrition programme to improve child growth in rural Ethiopia: a cluster randomized trial. Maternal & Child Nutrition. 2017 Jan 1;13(1) doi: 10.1111/mcn.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abdurahman AA, Mirzaei K, Dorosty AR, et al. Household Food Insecurity May Predict Underweightand Wasting among Children Aged 24–59 Months. Ecology of Food and Nutrition. 2016 Sep 2;55(5):456–472. doi: 10.1080/03670244.2016.1207069. [DOI] [PubMed] [Google Scholar]
- 55.Abebe Z, Haki GD, Baye K. Health Extension Workers' Knowledge and Knowledge-Sharing Effectiveness of Optimal Infant and Young Child Feeding Are Associated With Mothers' Knowledge and Child Stunting in Rural Ethiopia. Food and nutrition bulletin. 2016 Jun 6; doi: 10.1177/0379572116651209. 0379572116651209. [DOI] [PubMed] [Google Scholar]
- 56.Fentahun N, Belachew T, Lachat C. Determinants and morbidities of multiple anthropometric deficits in southwest rural Ethiopia. Nutrition. 2016 Nov-Dec;32(11–12):1243–1249. doi: 10.1016/j.nut.2016.03.023. ISSN 0899-9007, [DOI] [PubMed] [Google Scholar]
- 57.Woodruff BA, Wirth JP, Bailes A, Matji J, Timmer A, Rohner F. Determinants of stunting reduction in Ethiopia 2000–2011. Maternal & child nutrition. 2017 Apr 1;13(2) doi: 10.1111/mcn.12307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Haile D, Azage M, Mola T, Rainey R. Exploring spatial variations and factors associated with childhood stunting in Ethiopia: spatial and multilevel analysis. BMC pediatrics. 2016 Apr 15;16(1):1. doi: 10.1186/s12887-016-0587-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Motbainor A, Worku A, Kumie A. Stunting Is Associated with Food Diversity while Wasting with Food Insecurity among Underfive Children in East and West Gojjam Zones of Amhara Region, Ethiopia. PLoS ONE. 2015;10(8):e0133542. doi: 10.1371/journal.pone.0133542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mulugeta A, Hagos F, Kruseman G, Linderhof V, Stoecker B, Abraha Z, Yohannes M, Samuel GG. Child malnutrition in Tigray, northern Ethiopia. East African medical journal. 2010 Jun;87(6):248–254. doi: 10.4314/eamj.v87i6.63083. [DOI] [PubMed] [Google Scholar]
- 61.Medhin G, Hanlon C, Dewey M, et al. Prevalence and predictors of undernutrition among infants aged six and twelve months in Butajira, Ethiopia: the P-MaMiE Birth Cohort. BMC Public Health. 2010 Jan 20;10(1):1. doi: 10.1186/1471-2458-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tizazu B, Shibru T. Stunting Status of Under-Five Children in Rural Ethiopia: Multilevel Logistic Regression Analysis. [02 December 16]. Available at: etd.aau.edu.et/handle/123456789/10882. [Google Scholar]
- 63.Christiaensen L, Alderman H. Child malnutrition in Ethiopia: can maternal knowledge augment the role of income? Economic Development and cultural change. 2004 Jan;52(2):287–312. [Google Scholar]
- 64.Smith LC, Haddad LJ. Explaining child malnutrition in developing countries: A cross-country analysis. Intl Food Policy Res Inst. 2000 Intl Food Policy Res Inst; 2000. [Google Scholar]
- 65.Vollmer S, Harttgen K, Subramanyam MA, Finlay J, Klasen S, Subramanian SV. Association between economic growth and early childhood undernutrition: evidence from 121 Demographic and Health Surveys from 36 low-income and middle-income countries. The lancet global health. 2014 Apr 30;2(4):e225–e234. doi: 10.1016/S2214-109X(14)70025-7. [DOI] [PubMed] [Google Scholar]
- 66.Headey D. An analysis of trends and determinants of child undernutrition in Ethiopia, 2000–2011. International Food Policy Research Institute (IFPRI) 2014 Dec [Google Scholar]
- 67.Biadgilign S, Shumetie A, Yesigat H. Does Economic Growth Reduce Childhood Undernutrition in Ethiopia? PloS one. 2016 Aug 10;11(8):e0160050. doi: 10.1371/journal.pone.0160050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Onis M, Branca F. Childhood stunting: a global perspective. Maternal & child nutrition. 2016 May 1;12(S1):12–26. doi: 10.1111/mcn.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.SUN, author. Ethiopia commits to ending undernutrition by 2030 with the Seqota Declaration. [07 December 18]. Available at: http://scalingupnutrition.org/news/ethiopia-commits-to-ending-under-nutrition-by-2030-with-the-seqota-declaration/