Abstract
Purpose:
Acute respiratory distress syndrome (ARDS) is heterogeneous in etiology, which may affect outcomes. Stratification into biologically-defined subtypes may reduce heterogeneity. However, it is unknown whether pediatric ARDS has clinically relevant subtypes. We aimed to determine whether clinical characteristics and predictors of mortality differed between direct and indirect ARDS, and separately between infectious and non-infectious ARDS.
Methods:
Single center, prospective cohort study of 544 children with ARDS (Berlin) between July 2011 and June 2017, stratified into direct versus indirect ARDS, and separately into infectious versus non-infectious ARDS. Multiple logistic regression was used to test for predictors of mortality in the entire cohort, and separately within subtypes. Effect modification by subtype was assessed using interaction tests.
Results:
Direct ARDS had lower severity of illness (p < 0.001) but worse oxygenation (p < 0.001), relative to indirect. Predictors of mortality were similar for direct and indirect ARDS. When comparing infectious and non-infectious ARDS, infectious ARDS had lower severity of illness (p < 0.001), worse oxygenation (p = 0.014), and lower mortality (p = 0.013). In multivariable analysis, immunocompromised status demonstrated effect modification between infectious and non-infectious ARDS (p = 0.005 for interaction), with no association with mortality in non-infectious ARDS.
Conclusions:
In children, direct and indirect ARDS have distinct clinical characteristics, but similar outcomes and similar predictors of mortality. In contrast, infectious and non-infectious ARDS demonstrate heterogeneity of clinical characteristics, mortality, and predictors of mortality, with traditional predictors of ARDS mortality only applicable to infectious ARDS.
Keywords: ARDS, PARDS, children, direct ARDS, infectious ARDS
INTRODUCTION
Acute respiratory distress syndrome (ARDS) encompasses multiple diverse etiologies, leading to significant variability in clinical presentation. Patient heterogeneity may contribute to the absence of therapies for ARDS, despite multiple trials, predominantly in adults. Sub-classification of ARDS into subtypes is one approach for reducing heterogeneity. In adults, ARDS has been divided into direct (pulmonary) and indirect (non-pulmonary) etiologies [1–3], infectious or non-infectious [4], focal versus non-focal radiographs [5], and on the basis of biomarkers [1, 6]. One shortcoming of phenotyping using biomarkers is their inaccessibility at bedside. Prior studies have shown that direct and indirect ARDS are associated with biomarker profiles consistent with predominantly alveolar epithelial versus endothelial damage, respectively [1]. Therefore, it is possible that subtyping based on readily available clinical data could prove similarly informative.
To date, no studies have queried whether relevant subgroups exist in pediatric ARDS. Additionally, while several studies have tested for predictors of mortality in pediatric ARDS [7–9], no study has assessed whether prognostic factors differ between subtypes. The goal of the present study was to determine whether clinical characteristics and predictors of mortality differed between direct and indirect ARDS, and separately between infectious and non-infectious ARDS, in a large, well-phenotyped pediatric cohort.
METHODS
Patient Selection
This was an analysis of an ongoing prospective cohort, approved by the Children’s Hospital of Philadelphia’s (CHOP) Institutional Review Board (IRB), with requirement for informed consent waived. The cohort has previously been described in detail [10]. Briefly, intubated children meeting American-European Consensus Conference criteria for acute lung injury (two consecutive Pao2/Fio2 ≤ 300 separated by ≥ 1 hour with bilateral infiltrates) admitted to the CHOP pediatric intensive care unit (PICU) between July 1, 2011 and June 30, 2017 were enrolled. As the study was initiated prior to the Berlin definition [11], minimum PEEP was not specified; however, CHOP PICU does not utilize PEEP < 5 cmh2o. Thus, all patients met Berlin criteria. Similarly, as the study was initiated prior to the Pediatric Acute Lung Injury Consensus Conference (PALICC) definition of pediatric ARDS (PARDS) [12], we did not screen using OI; however, all but one patient met PARDS criteria by OI.
Demographics, ventilator settings, Pao2/Fio2 and OI at ARDS onset and 24 hours, and treatments for the first 3 days were recorded prospectively. Absent a standardized ventilator protocol, our practice is to initiate conventional ventilation with PEEP ≥ 5 cmh2o, and to wean Fio2 to ≤ 0.60, keeping PaO2 ≥ 60 mmHg. Inability to wean Fio2 prompts PEEP escalation. Persistently elevated peak pressures (≥ 35 cmh2o), hypercarbia (Paco2 ≥ 80), or hypoxemia (inability to wean Fio2 ≤ 0.60 despite increased PEEP) prompted consideration for changing mode of ventilation or escalating to extracorporeal membrane oxygenation (ECMO). Actual transition or use of ancillary therapy was left to the discretion of the attending physician.
Determination of Cause of ARDS
Etiology of ARDS was determined prospectively, most commonly by concurrent chart abstraction, or in unclear cases, by querying the treating PICU attending on the likely etiology. Remaining uncertain cases were adjudicated by a three-person team of PICU physicians, with discussion until unanimous consent. Infectious pneumonia, aspiration, drowning, pulmonary contusion, and smoke inhalation were considered direct ARDS; non-pulmonary sepsis, non-thoracic trauma, non-cardiogenic shock, transfusion-related acute lung injury (TRALI), and pancreatitis were indirect. Infectious pneumonia and non-pulmonary sepsis were considered infectious ARDS; all other etiologies were non-infectious.
Equations and Definitions
Oxygenation was measured using Pao2/Fio2 or OI (mean airway pressure [mPaw] × Fio2 × 100)/ Pao2). Vasopressor score [13] was: dopamine (μg/kg/min) × 1 + dobutamine (μg/kg/min) × 1 + epinephrine (μg/kg/min) × 100 + norepinephrine (μg/kg/min) × 100 + phenylephrine (μg/kg/min) × 100 + vasopressin (U/kg/min) × 10,000 + milrinone (μg/kg/min) × 10. Non-pulmonary organ failures were identified using accepted definitions in children [14]. The designation “immunocompromised” required presence of an immunocompromising diagnosis (oncologic, immunologic, rheumatologic, or transplant) and active immunosuppressive chemotherapy, or a congenital immunodeficiency [10, 15]. Severity of illness score used was the Pediatric Risk of Mortality (PRISM) III at 12 hours.
Outcomes
Primary outcome was PICU mortality. Secondary outcomes were 1) a composite of either ECMO or PICU mortality (ECMO/mortality) and 2) probability of extubation. Cause of death was classified as either hypoxemia, multisystem organ failure (MSOF), or neurologic, as we have done previously [10, 16]. Duration of ventilation and ventilator-free days (VFD) at 28 days were also reported. All mention of “ventilation” implies invasive ventilation; non-invasive support was not counted. “Day 1” was initiation of invasive ventilation. Liberation from ventilation ≥ 24 hours defined duration of ventilation. Patients requiring re-initiation of invasive ventilation had the extra days counted towards total ventilator days. VFD was determined by subtracting total ventilator days from 28 in survivors. Patients with ≥ 28 ventilator days and PICU non-survivors were assigned VFD = 0.
Statistical Analysis
Analyses were performed using Stata 14.2 SE. Data are expressed as percentages or medians [interquartile range] and analyzed using Wilcoxon rank-sum or Fisher exact tests. Select univariate analyses are also presented using survival curves analyzed using log-rank tests.
To determine risk factors for mortality, we tested univariate association with mortality on the whole cohort, then repeated the analysis after stratifying by direct or indirect ARDS, and separately by infectious or non-infectious. Variables associated with mortality in univariate analysis (p < 0.1) were entered into a logistic regression model. We considered a Cox proportional hazard model rather than a logistic for determining independent predictors of mortality. However, variable inspection demonstrated that not all variables (specifically, immunocompromised status) met the proportional hazard assumption, thus precluding a Cox model. Therefore, we opted for the logistic model which required fewer assumptions of our data. Because of collinearity between oxygenation and ventilator variables at ARDS onset and 24 hours, only OI at 24 hours was modeled, as it incorporates both oxygenation and ventilator pressures, and because we and others have demonstrated 24-hour oxygenation is a superior prognostic metric of ARDS severity [10, 17–19]. We then used a manual backward stepwise process by removing the term with the highest p value, and compared models using likelihood ratio (LR) testing and Akaike Information Criterion (AIC)[20]. This continued until no further variables could be removed and AIC was minimized. To evaluate whether variables had differential effects based on ARDS subtype, we then introduced interaction terms (separately) for indirect ARDS and for non-infectious ARDS, and tested terms against each variable. After interaction testing, we constructed the final model (with interactions) and compared with simpler models using LR testing and AIC. Multicollinearity of the model was assessed using variance inflation factors. Model fit was assessed using the Hosmer-Lemeshow test. Additional models were identically constructed to test the outcome ECMO/mortality, and for subgroup analyses.
We also tested for variables associated with probability of extubation given the competing risk of death using Fine and Gray regression [21], wherein extubation is considered the primary outcome and death the competing event. This provides a subdistribution hazard ratio (SHR) for probability of extubation accounting for competing risk of death. By censoring outcomes at 28 days, this outcome becomes analogous to VFD at 28 days. The multivariate model was constructed by manual backward stepwise variable selection minimizing AIC and testing for significance of interaction terms using the Wald test. The proportional hazard assumption was assessed by testing for interaction with a time-dependent covariate.
Classification and Regression Tree Analysis
To provide a tool to visualize and implement mortality prediction, we performed classification and regression tree (CART) analysis (Salford Predictive Modeler v8.2; Salford Systems, San Diego, CA) using variables from the final model. Terminal nodes that did not improve classification by class probability were pruned. The model was developed with 10-fold cross-validation, and area under the receiver operating characteristic (AUROC) curve calculated.
RESULTS
Description of the Cohort
During the study period, 544 children with ARDS were included (Table 1). Direct lung injury accounted for 384 (71%) of cases, of which 282 (73% of 384) were infectious. Infection accounted for 404 (74%), of which 282 (70% of 404) were direct. Thirty-nine subjects required adjudication for determination of ARDS etiology, most commonly (24 cases) differentiating between infectious pneumonia and non-pulmonary sepsis. Non-survivors (n = 93, 17%) were older, had greater severity of illness, worse oxygenation, and were more commonly immunocompromised. Berlin (Figure 1) demonstrated better discrimination and calibration of outcome at 24 hours, relative to ARDS onset, whereas PALICC was similar at both timepoints (Supplementary Figure 1).
Table 1:
Characteristics of the cohort stratified by survival status
| Variables | All patients (n = 544) |
Survivors (n = 451) |
Non-survivors (n = 93) |
p value |
|---|---|---|---|---|
| Age (years) | 4.6 [1.5, 12.2] | 4.1 [1.4, 11.4] | 7.2 [3.2, 14.3] | < 0.001 |
| Female (%) | 239 (44) | 202 (45) | 37 (40) | 0.422 |
| Severity of illness | ||||
| PRISM III at 12 hours | 11 [5, 18] | 9 [4, 15] | 19 [12, 31] | < 0.001 |
| Non-pulmonary organ failures | 2 [1, 3] | 1 [1, 2] | 3 [2, 4] | < 0.001 |
| Vasopressor score | 10 (3, 20) | 8 [3, 17] | 20 [8, 55] | < 0.001 |
| Co-morbidities (%) | ||||
| None | 220 (40) | 186 (41) | 34 (37) | 0.419 |
| Prematurity | 68 (13) | 67 (15) | 2 (2) | < 0.001 |
| Genetic syndrome | 88 (16) | 79 (18) | 10 (11) | 0.124 |
| Epilepsy | 79 (15) | 75 (17) | 6 (6) | 0.010 |
| Malignancy | 75 (14) | 52 (12) | 23 (25) | 0.002 |
| Immunocompromised | 106 (19) | 65 (14) | 41 (44) | < 0.001 |
| Cause of ARDS (%) | ||||
| Direct (%) | 384 (71) | 326 (72) | 58 (62) | 0.061 |
| Infectious (%) | 404 (74) | 345 (77) | 59 (63) | 0.013 |
| Cause of ARDS (%) | ||||
| Infectious pneumonia | 282 (52) | 250 (55) | 32 (34) | |
| Aspiration pneumonia | 69 (13) | 54 (12) | 15 (17) | |
| Drowning | 15 (3) | 9 (2) | 6 (6) | |
| Thoracic trauma/contusion | 13 (2) | 10 (2) | 3 (3) | |
| Smoke inhalation | 5 (1) | 3 (1) | 2 (2) | 0.008 |
| Non-pulmonary sepsis | 122 (22) | 95 (21) | 27 (29) | |
| Non-thoracic trauma | 22 (4) | 17 (4) | 5 (5) | |
| Non-cardiogenic shock | 12 (2) | 10 (2) | 2 (2) | |
| TRALI | 3 (0.6) | 2 (0.4) | 1 (1) | |
| Pancreatitis | 1 (0.2) | 1 (0.2) | 0 | |
| ARDS onset | ||||
| PaO2/FIO2 | 158 [105, 218] | 162 [113, 220] | 135 [71, 206] | < 0.001 |
| OI | 10.2 [7, 17.7] | 10 [7, 15.8] | 15.4 [7.3, 25.8] | < 0.001 |
| PIP (cmH2O) | 30 [26, 35] | 30 [26, 35] | 31 [28, 38] | < 0.001 |
| PEEP (cmH2O) | 10 [8, 12] | 10 [8, 12] | 10 [8, 12] | < 0.001 |
| ΔP (cmH2O) | 21 [16, 25] | 20 [16, 24] | 21 [17, 26] | < 0.001 |
| VT (mL/kg) | 7.5 [6.6, 8.4] | 7.4 [6.5, 8.4] | 7.7 [6.8, 8.3] | < 0.001 |
| Berlin category at ARDS onset | ||||
| Mild | 175 (32) | 148 (33) | 27 (29) | 0.001 |
| Moderate | 245 (45) | 214 (47) | 31 (33) | |
| Severe | 124 (23) | 89 (20) | 35 (38) | |
| 24 hours after onset | ||||
| PaO2/FIO2 | 223 [158, 283] | 231 [170, 292] | 182 [106, 251] | < 0.001 |
| OI |
6.9 [4.8, 12] | 6.6 [4.7, 10.8] | 9.3 [5.7, 23.8] | < 0.001 |
| PIP (cmH2O) | 27 [24, 32] | 27 [23, 31] | 30 [25, 35] | < 0.001 |
| PEEP (cmH2O) | 10 [8, 10] | 10 [8, 10] | 10 [8, 12] | < 0.001 |
| ΔP (cmH2O) | 18 [14, 22] | 17 [14, 22] | 20 [15, 24] | < 0.001 |
| VT (mL/kg) | 7.3 [6.5, 8.1] | 7.3 [6.5, 8.1] | 7.1 [6.3, 8] | < 0.001 |
| Berlin category at 24 hours | ||||
| Resolved | 109 (20) | 97 (22) | 12 (13) | |
| Mild | 206 (38) | 183 (41) | 23 (26) | < 0.001 |
| Moderate | 174 (32) | 142 (31) | 32 (36) | |
| Severe | 51 (9) | 29 (6) | 22 (25) | |
| Ancillary therapies (%) | ||||
| Inhaled nitric oxide | 201 (37) | 148 (33) | 53 (57) | < 0.001 |
| Neuromuscular blockade | 256 (47) | 214 (47) | 42 (45) | 0.733 |
| Corticosteroids | 297 (55) | 231 (51) | 66 (71) | 0.001 |
| Alternative ventilator modes | 168 (31) | 136 (30) | 32 (34) | 0.460 |
| Extracorporeal support | 22 (4) | 18 (4) | 4 (4) | 0.779 |
OI: oxygenation index; PRISM: Pediatric Risk of Mortality; PEEP: positive end expiratory pressure; PIP: peak inspiratory pressure; ΔP: PIP minus PEEP; TRALI: transfusion associated acute lung injury; VT: tidal volume
Figure 1:
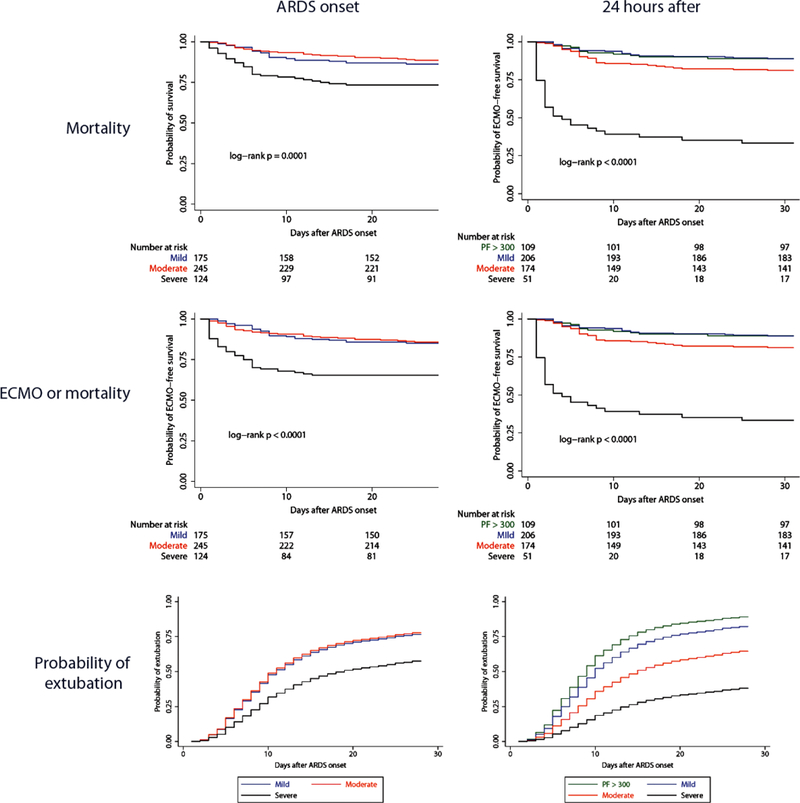
Kaplan-Meier survival curves for the outcomes of survival, ECMO-free survival, or probability of extubation given the competing risk of death, stratified by Berlin severity categories, at ARDS onset and at 24 hours. All curves are censored at 28 days. At ARDS onset, there is overlap of mild (blue) and moderate (blue) categories, whiles severe (black) demonstrates worse survival, ECMO-free survival, and lower probability of extubation. By 24 hours, there is improved separation of the categories for all outcomes, with residual overlap between resolved (green) and mild (red) ARDS.
Direct versus Indirect ARDS
Subjects with indirect ARDS were older, had greater severity of illness, and were more commonly immunocompromised than those with direct (Supplementary Table 1). Patients with indirect ARDS had better oxygenation (both Pao2/Fio2 and OI) at ARDS onset, and a lower OI at 24 hours. Inhaled nitric oxide, continuous neuromuscular blockade, and non-conventional ventilation were more common for direct ARDS. Non-survivors of indirect ARDS were more likely to die from MSOF. In univariate analysis, greater severity of illness and immunocompromised status were associated with mortality in both direct and indirect ARDS (Supplementary Table 2). Worse OI and higher ventilator pressures at both ARDS onset and at 24 hours were associated with mortality in direct ARDS, whereas only oxygenation and ventilator pressures at 24 hours were associated with mortality in indirect ARDS.
Infectious versus Non-Infectious ARDS
Subjects with non-infectious ARDS were older, had greater severity of illness, and were less likely to have any co-morbidities than those with infectious ARDS (Supplementary Table 3). Subjects with non-infectious ARDS had improved oxygenation 24 hours after ARDS onset, and a shorter duration of ventilation in survivors. However, non-infectious ARDS subjects had higher mortality (24%) relative to infectious (15%, p = 0.013), and were more likely to die from neurologic causes. Severity of illness was associated with mortality for both infectious and non-infectious ARDS (Supplementary Table 4). Oxygenation and ventilator pressures at ARDS onset were associated with mortality in infectious ARDS, while only OI and tidal volume at onset were associated with mortality in non-infectious. By 24 hours, oxygenation and ventilator pressures were only associated with mortality in infectious ARDS. Immunocompromised status and presence of a malignancy was similarly only associated with mortality in infectious ARDS.
Independent Risk Factors between ARDS Subtypes
We performed multiple logistic regression using a manual backward selection process. The model without any interaction terms (Supplementary Table 5) showed mortality was associated with PRISM III, number of non-pulmonary organ failures, immunocompromised status, direct ARDS etiology, and higher OI at 24 hours. We then introduced interaction terms (separately) for indirect ARDS (reference: direct) and non-infectious ARDS (reference: infectious), testing for interactions with each variable in the model. Immunocompromised status had a significant interaction with both indirect ARDS and with non-infectious ARDS (both p < 0.05). Inclusion of both interaction terms improved model fit (p = 0.005 for LR test relative to simpler model without interaction terms), resulting in the final model (Table 2). Immunocompromised status had a differential effect on infectious versus non-infectious ARDS, with an association between immunocompromised status and increased mortality only seen in infectious ARDS. Within infectious ARDS, there was a larger effect of immunocompromised status on direct ARDS, relative to indirect (Table 2, Figure 2). When constructing models for the composite endpoint ECMO/mortality (Supplementary Table 6) and probability of extubation (Supplementary Table 7), we again saw an interaction between infectious/non-infectious ARDS and immunocompromised status, but direct/indirect was no longer retained.
Table 2:
Final model for PICU mortality with both interaction terms included
| Variable | aOR (95% CI) | p value |
|---|---|---|
| PRISM III | 1.05 (1.02 to 1.09) | 0.001 |
| Organ failures | 2.27 (1.68 to 3.06) | < 0.001 |
| Indirect ARDS | 0.75 (0.31 to 1.81) | 0.525 |
| Non-infectious ARDS | 2.34 (1.09 to 5.04) | 0.030 |
| Immunocompromised | ||
| Direct/Infectious | 12.81 (4.87 to 33.71) | < 0.001 |
| Indirect/Infectious | 3.27 (1.22 to 8.77) | 0.019 |
| Direct/Non-infectious | 1.71 (0.43 to 6.73) | 0.446 |
| Indirect/Non-infectious | 0.43 (0.11 to 1.78) | 0.247 |
| Interaction terms | ||
| Direct/Indirect*Immunocompromised | 0.25 (0.07 to 0.91) | 0.036 |
| Infectious/Non-infectious*Immunocompromised | 0.13 (0.03 to 0.55) | 0.005 |
| OI 24 hours after ARDS onset | 1.02 (1.00 to 1.04) | 0.037 |
OI: oxygenation index; PRISM: Pediatric Risk of Mortality
Figure 2:
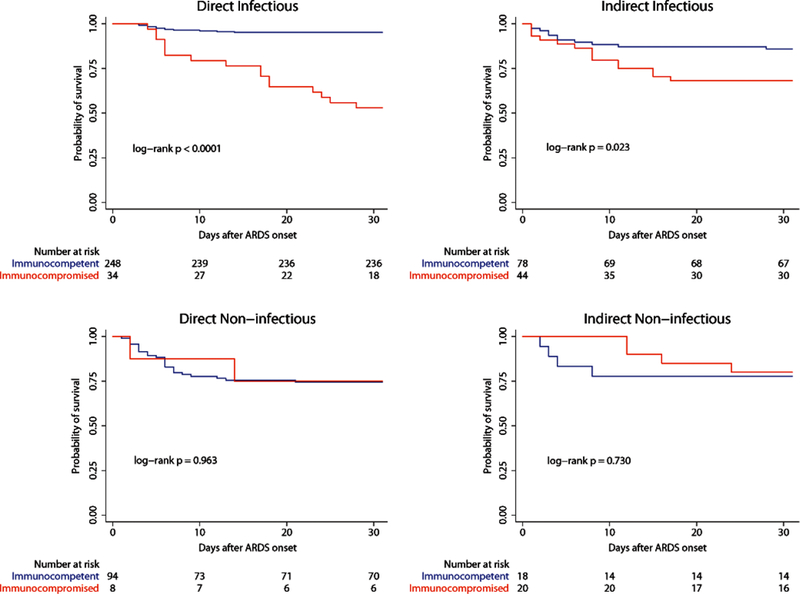
Kaplan-Meier survival curves for immunocompetent (blue) and immunocompromised (red) subjects stratified by ARDS subtype. All curves are censored at 28 days.
Subgroup Analyses
Because OI may perform differently in non-conventional ventilation, we repeated our analysis restricted to subjects only on conventional ventilation (Supplementary Table 8). We again demonstrated that immunocompromised status had a differential effect on infectious versus non-infectious ARDS. When we excluded subjects dying of neurologic causes (Supplementary Table 9), the final model retained organ failures, immunocompromised status, and OI at 24 hours as associated with PICU mortality. Finally, we constructed models predicting outcomes in immunocompetent subjects (Supplementary Table 10). PRISM score, organ failures, and non-infectious ARDS were associated with mortality and ECMO/mortality, while OI at 24 hours was also associated with ECMO/mortality. Increasing organ failures and OI at 24 hours were associated with lower probability of extubation, while indirect ARDS was associated with higher probability of extubation.
CART Analysis
To visualize and implement mortality prediction, we performed CART analysis using the variables in Table 2. The final tree (Figure 3) retained non-pulmonary organ failure, OI at 24 hours, infectious/non-infectious ARDS, and immunocompromised status. There were five terminal nodes: one low-risk (green, 2% mortality), one intermediate (blue, 8% mortality), and 3 high-risk (red, ≥ 33% mortality). This model had AUROC of 0.81 (95% CI 0.76 to 0.86) for discriminating PICU mortality. Consistent with the regression model, infectious ARDS had a subsequent branch point for immunocompromised status, whereas non-infectious ARDS did not.
Figure 3:
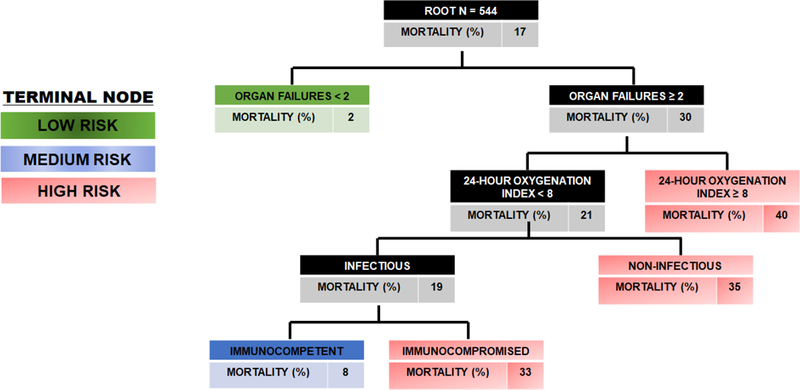
Decision tree for mortality constructed from variables retained in final model using classification and regression tree (CART) methodology. The tree contains mortality at each decision point and the decision rules. The final model resulted in a tree with five terminal nodes: one low-risk (green), one intermediate risk (blue), and 3 high-risk (red).
DISCUSSION
Clinical characteristics differ between direct and indirect ARDS, as well as between infectious and non-infectious ARDS. While severity of illness predicted mortality consistently across all subtypes, immunocompromised status was differentially associated with mortality in infectious versus non-infectious ARDS. This may be due to the higher prevalence of neurologic deaths in non-infectious ARDS. Traditional predictors of mortality, such as immunocompromised status and oxygenation, were only associated with mortality in infectious ARDS. This is the first description of associations between clinical characteristics and mortality in different subtypes of pediatric ARDS.
Direct and indirect ARDS present differently, with higher severity of illness and more immunocompromised subjects in indirect ARDS, and worse oxygenation in direct. After adjustment, the direct/indirect designation was not associated with mortality. Infectious and non-infectious ARDS also differed clinically: non-infectious had higher severity of illness, better oxygenation, and higher mortality. After adjustment for confounders, non-infectious ARDS retained association with mortality (odds ratio 2.34, 95% CI 1.09 to 5.04, p = 0.030).
Severity of illness as measured by PRISM III and organ failures was consistently associated with mortality in all subtypes. OI at 24 hours was also associated with mortality in the full model, as previously shown [22], but not when restricted to non-infectious ARDS. It is unclear whether worse OI reflects a pulmonary-specific risk factor, or whether it is the pulmonary manifestation of MSOF. The higher mortality in non-infectious ARDS, despite improved oxygenation and shorter ventilator duration in survivors, confirms that subjects were likely dying from causes other than severe ARDS, including neurologic etiologies, for which OI at 24 hours is not a risk factor.
Immunocompromised status was independently associated with mortality with evidence of effect modification. Immunocompromised status was not a predictor of mortality in non-infectious ARDS in either univariate or multivariate analysis. This is the first study to suggest that non-infectious pediatric ARDS has different outcome predictors. Previous cohorts have suggested immunocompromised status as a predictor of mortality [8, 23]. Given that the most common etiologies in those cohorts, as in ours, was pneumonia and non-pulmonary sepsis, it is possible that over-representation of infectious ARDS, and particularly pneumonia, made apparent an association of immunocompromised status and mortality for the entire cohort. Our results are consistent with previous studies but are large enough to test for differential effects of immunocompromised status within subtypes. The largest effect of immunocompromised status on mortality was seen in direct infectious ARDS (i.e., pneumonia), which accounts for the majority of ARDS etiologies in most cohorts [7, 8, 10, 18]. The interaction between immunocompromised status and infectious/non-infectious ARDS disappeared when excluding subjects who died from neurologic causes, suggesting that the lack of association between immunocompromised status and mortality in non-infectious ARDS is due to a higher proportion of severe neurologic failure among non-infectious ARDS, making the presence of an immunocompromising condition less relevant for mortality. Importantly, the differential impact of immunocompromised status on infectious versus non-infectious ARDS was confirmed in CART analysis. This is significant as CART is a non-parametric methodology which performs automatic variable selection and is often used to “discover” interactions between variables de novo. CART analysis retained infectious versus non-infectious ARDS and immunocompromised status and discovered an interaction effect between these variables. Direct versus indirect ARDS was not retained in the CART analysis, highlighting the greater significance of the infectious categorization, rather than the direct/indirect designation, for short-term mortality prediction.
Differences in mortality predictors between infectious and non-infectious etiologies support the existence of subtypes within pediatric ARDS. In adults, emerging literature suggests that different ARDS subtypes exist, and potentially impact outcomes [1, 3, 6, 24–27]. Recently, adult ARDS subtypes have been identified using latent class analysis of clinical and biochemical variables [6, 24], broadly corresponding to hypo- and hyperinflammatory phenotypes. These subtypes have differential responses to PEEP [6] and fluid management [24]. Comparable analyses have not been performed in children, limited by lower prevalence of pediatric ARDS, smaller available cohorts, fewer clinical trials, and lower mortality [10, 28, 29]. Future pediatric ARDS trials should stratify by type of lung injury, or pre-specify post-hoc analyses, to account for differential effects of intervention between subtypes. Our data suggest that infectious or non-infectious ARDS is a more important stratification, relative to direct or indirect.
Our study has limitations. The single-center nature limits generalizability, although ARDS etiologies, severity, and mortality were comparable to others [7, 8, 18, 30, 31]. We did not screen using Berlin or PALICC definitions as these were not available at the start of our study, although all subjects met Berlin criteria. Our results are not generalizable to subjects with unilateral infiltrates, which are allowed under PALICC. Similarly, as we did not screen using Spo2, we may have missed subjects lacking arterial access, as well as explicit Spo2-based classification allowed by PALICC. It is possible that a cohort screened using more modern definitions of ARDS would result in a model with different predictors. Only recorded variables were tested in the regression model, and it is possible that relevant predictors went unmeasured. However, our data collection focused on variables with prior associations with mortality. We were not able to perform the commonly accepted Cox regression because of limitations in our data, which precludes some information regarding the shape of the survival curves and time to death. Despite the size of the cohort, division into subtypes results in smaller sample sizes, with as few as 34 deaths in non-infectious ARDS, limiting identification of factors associated with mortality in subgroups. However, the main conclusion of a differential effect of immunocompromised status in infectious versus non-infectious ARDS is consistent throughout all analyses. Finally, as there is no gold standard for assigning ARDS etiology, it is possible that some subjects were misclassified.
Our study has several strengths. This is a large, prospective cohort from a tertiary PICU with detailed data collection, and the first study powered to address the existence of ARDS subtypes. Etiologies were assigned nearly in real-time, with a protocolized procedure for uncertain cases. The dense, registry-style phenotyping allowed us to assess the association between mortality and several relevant variables. We tested multiple outcomes, including a composite of ECMO/mortality and probability of extubation, and provided an operational tree to stratify mortality risk. While our results require external validation, they provide a framework for future observational and interventional studies in pediatric ARDS.
CONCLUSIONS
In pediatrics, direct and indirect ARDS have different clinical characteristics, but similar outcomes and similar predictors of mortality. By contrast, infectious and non-infectious ARDS demonstrate differences in clinical characteristics, mortality, and predictors of mortality. Immunocompromised status, a traditional predictor of mortality, is only applicable to infectious ARDS. Infectious and non-infectious ARDS have distinct features differentially affecting risk prediction and outcome, which should be accounted for in future studies.
Supplementary Material
Kaplan-Meier survival curves for the outcomes of survival, ECMO-free survival, or probability of extubation given the competing risk of death, stratified by PALICC severity categories, at ARDS onset and at 24 hours. All curves are censored at 28 days.
Footnotes
CONFLICTS OF INTEREST
Dr. Yehya’s institution receives funding from the NIH (K12-HL-136688). Dr. Thomas reports personal fees from Therabron and Carefusion, all outside of the submitted work.
REFERENCES
- 1.Calfee CS, Janz DR, Bernard GR, May AK, Kangelaris KN, Matthay MA, Ware LB, (2015) Distinct molecular phenotypes of direct vs indirect ARDS in single-center and multicenter studies. Chest 147: 1539–1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Willson DF, Truwit JD, Conaway MR, Traul CS, Egan EE, (2015) The Adult Calfactant in Acute Respiratory Distress Syndrome Trial. Chest 148: 356–364 [DOI] [PubMed] [Google Scholar]
- 3.Luo L, Shaver CM, Zhao Z, Koyama T, Calfee CS, Bastarache JA, Ware LB, (2017) Clinical Predictors of Hospital Mortality Differ Between Direct and Indirect ARDS. Chest 151: 755–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Heart L, Blood Institute ACTN, Truwit JD, Bernard GR, Steingrub J, Matthay MA, Liu KD, Albertson TE, Brower RG, Shanholtz C, Rock P, Douglas IS, deBoisblanc BP, Hough CL, Hite RD, Thompson BT, (2014) Rosuvastatin for sepsis-associated acute respiratory distress syndrome. N Engl J Med 370: 2191–2200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mrozek S, Jabaudon M, Jaber S, Paugam-Burtz C, Lefrant JY, Rouby JJ, Asehnoune K, Allaouchiche B, Baldesi O, Leone M, Lu Q, Bazin JE, Roszyk L, Sapin V, Futier E, Pereira B, Constantin JM, Azurea n, (2016) Elevated Plasma Levels of sRAGE Are Associated With Nonfocal CT-Based Lung Imaging in Patients With ARDS: A Prospective Multicenter Study. Chest 150: 998–1007 [DOI] [PubMed] [Google Scholar]
- 6.Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA, Network NA, (2014) Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. The Lancet Respiratory medicine 2: 611–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flori HR, Glidden DV, Rutherford GW, Matthay MA, (2005) Pediatric acute lung injury: prospective evaluation of risk factors associated with mortality. Am J Respir Crit Care Med 171: 995–1001 [DOI] [PubMed] [Google Scholar]
- 8.Erickson S, Schibler A, Numa A, Nuthall G, Yung M, Pascoe E, Wilkins B, Paediatric Study G, Australian, New Zealand Intensive Care S, (2007) Acute lung injury in pediatric intensive care in Australia and New Zealand: a prospective, multicenter, observational study. Pediatr Crit Care Med 8: 317–323 [DOI] [PubMed] [Google Scholar]
- 9.Yehya N, Bhalla AK, Thomas NJ, Khemani RG, (2016) Alveolar Dead Space Fraction Discriminates Mortality in Pediatric Acute Respiratory Distress Syndrome. Pediatr Crit Care Med 17: 101–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yehya N, Servaes S, Thomas NJ, (2015) Characterizing degree of lung injury in pediatric acute respiratory distress syndrome. Crit Care Med 43: 937–946 [DOI] [PubMed] [Google Scholar]
- 11.Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS, (2012) Acute respiratory distress syndrome: the Berlin Definition. JAMA 307: 2526–2533 [DOI] [PubMed] [Google Scholar]
- 12.Pediatric Acute Lung Injury Consensus Conference G, (2015) Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med 16: 428–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR, Hirsch JC, (2010) Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11: 234–238 [DOI] [PubMed] [Google Scholar]
- 14.Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric S, (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6: 2–8 [DOI] [PubMed] [Google Scholar]
- 15.Yehya N, Topjian AA, Thomas NJ, Friess SH, (2014) Improved oxygenation 24 hours after transition to airway pressure release ventilation or high-frequency oscillatory ventilation accurately discriminates survival in immunocompromised pediatric patients with acute respiratory distress syndrome*. Pediatr Crit Care Med 15: e147–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yehya N, Wong HR, (2017) Adaptation of a Biomarker-Based Sepsis Mortality Risk Stratification Tool for Pediatric Acute Respiratory Distress Syndrome. Crit Care Med [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villar J, Perez-Mendez L, Lopez J, Belda J, Blanco J, Saralegui I, Suarez-Sipmann F, Lopez J, Lubillo S, Kacmarek RM, Network H, (2007) An early PEEP/FIO2 trial identifies different degrees of lung injury in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 176: 795–804 [DOI] [PubMed] [Google Scholar]
- 18.Lopez-Fernandez Y, Azagra AM, de la Oliva P, Modesto V, Sanchez JI, Parrilla J, Arroyo MJ, Reyes SB, Pons-Odena M, Lopez-Herce J, Fernandez RL, Kacmarek RM, Villar J, Pediatric Acute Lung Injury E, Natural History N, (2012) Pediatric Acute Lung Injury Epidemiology and Natural History study: Incidence and outcome of the acute respiratory distress syndrome in children. Crit Care Med 40: 3238–3245 [DOI] [PubMed] [Google Scholar]
- 19.Villar J, Perez-Mendez L, Blanco J, Anon JM, Blanch L, Belda J, Santos-Bouza A, Fernandez RL, Kacmarek RM, Spanish Initiative for Epidemiology S, Therapies for AN, (2013) A universal definition of ARDS: the PaO2/FiO2 ratio under a standard ventilatory setting--a prospective, multicenter validation study. Intensive Care Med 39: 583–592 [DOI] [PubMed] [Google Scholar]
- 20.Lindsey JK, Jones B, (1998) Choosing among generalized linear models applied to medical data. Statistics in medicine 17: 59–68 [DOI] [PubMed] [Google Scholar]
- 21.Fine JP, Gray RJ, (1999) A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association 94: 496–509 [Google Scholar]
- 22.Yehya N, Thomas NJ, (2017) Disassociating Lung Mechanics and Oxygenation in Pediatric Acute Respiratory Distress Syndrome. Crit Care Med 45: 1232–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spicer AC, Calfee CS, Zinter MS, Khemani RG, Lo VP, Alkhouli MF, Orwoll BE, Graciano AL, Boriosi JP, Howard JP, Flori HR, Matthay MA, Sapru A, (2016) A Simple and Robust Bedside Model for Mortality Risk in Pediatric Patients With Acute Respiratory Distress Syndrome. Pediatr Crit Care Med 17: 907–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Famous KR, Delucchi K, Ware LB, Kangelaris KN, Liu KD, Thompson BT, Calfee CS, Network A, (2017) Acute Respiratory Distress Syndrome Subphenotypes Respond Differently to Randomized Fluid Management Strategy. Am J Respir Crit Care Med 195: 331–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reilly JP, Bellamy S, Shashaty MG, Gallop R, Meyer NJ, Lanken PN, Kaplan S, Holena DN, May AK, Ware LB, Christie JD, (2014) Heterogeneous phenotypes of acute respiratory distress syndrome after major trauma. Ann Am Thorac Soc 11: 728–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheu CC, Gong MN, Zhai R, Chen F, Bajwa EK, Clardy PF, Gallagher DC, Thompson BT, Christiani DC, (2010) Clinical characteristics and outcomes of sepsis-related vs non-sepsis-related ARDS. Chest 138: 559–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim SJ, Oh BJ, Lee JS, Lim CM, Shim TS, Lee SD, Kim WS, Kim DS, Kim WD, Koh Y, (2004) Recovery from lung injury in survivors of acute respiratory distress syndrome: difference between pulmonary and extrapulmonary subtypes. Intensive Care Med 30: 1960–1963 [DOI] [PubMed] [Google Scholar]
- 28.Zimmerman JJ, Akhtar SR, Caldwell E, Rubenfeld GD, (2009) Incidence and outcomes of pediatric acute lung injury. Pediatrics 124: 87–95 [DOI] [PubMed] [Google Scholar]
- 29.Khemani RG, Smith LS, Zimmerman JJ, Erickson S, Pediatric Acute Lung Injury Consensus Conference G, (2015) Pediatric acute respiratory distress syndrome: definition, incidence, and epidemiology: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med 16: S23–40 [DOI] [PubMed] [Google Scholar]
- 30.Trachsel D, McCrindle BW, Nakagawa S, Bohn D, (2005) Oxygenation index predicts outcome in children with acute hypoxemic respiratory failure. Am J Respir Crit Care Med 172: 206–211 [DOI] [PubMed] [Google Scholar]
- 31.Khemani RG, Rubin S, Belani S, Leung D, Erickson S, Smith LS, Zimmerman JJ, Newth CJ, (2015) Pulse oximetry vs. PaO2 metrics in mechanically ventilated children: Berlin definition of ARDS and mortality risk. Intensive Care Med 41: 94–102 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Kaplan-Meier survival curves for the outcomes of survival, ECMO-free survival, or probability of extubation given the competing risk of death, stratified by PALICC severity categories, at ARDS onset and at 24 hours. All curves are censored at 28 days.


