Abstract
Duchenne muscular dystrophy (DMD) is associated with an increased risk of endocrine complications due to the effects of prolonged glucocorticoid therapy as well as progressive muscle weakness. Categories of complications include obesity and its comorbidities, short stature, pubertal delay, and adrenal insufficiency. Obesity prevention is important for long-term management of patients with DMD. Preventing glucocorticoid-induced weight gain fosters patient mobility, ease of transfer, and reduces sleep-disordered breathing. Metabolic complications from obesity (glucose intolerance, dyslipidemia) also can be avoided. Short stature and pubertal delay may negatively affect self-esteem and peer relationships, and careful monitoring of growth and pubertal development can allow anticipatory counseling, Adrenal insufficiency, a potentially life-threatening complication associated with prolonged glucocorticoid use, must be recognized so as to allow prompt treatment. In this article, we provide a summary of current guidance to ensure comprehensive endocrine management is followed in patients with DMD.
The effect of glucocorticoid therapy on the clinical phenotype in patients with Duchenne muscular dystrophy (DMD) has led to the need for clear recommendations about weight management and the monitoring and treatment of endocrine complications. The appetite-promoting and fat deposition effects of GC therapy are prominent in this condition and perpetuate serious obesity-related comorbidities such as diabetes, dyslipidemia, and sleep apnea. Glucocorticoid therapy also suppresses the hypothalamic and pituitary axes, causing an often profound linear growth failure and marked delay in pubertal development. The linear growth failure of DMD is further affected by a direct adverse effect of glucocorticoid therapy on growth plate function. Glucocorticoid dependence due to adrenal insufficiency is another serious consequence of the high-dose glucocorticoid therapy that is typically prescribed in DMD.
All of these issues (obesity, growth failure, delayed puberty, and adrenal insufficiency) can adversely affect quality of life, and adequate treatment of adrenal insufficiency in patients with glucocorticoid dependence is a potential life-saving measure.1 In this review, we target pediatricians, neurologists, endocrinologists, and weight management clinicians involved in the care of patients with DMD by providing specific guidance on clinical practice in these areas. With appropriate prevention and treatment of glucocorticoid-related comorbidities, it is anticipated that the need to withdraw glucocorticoid therapy to treat the underlying disease will be largely or wholly obviated.
OVERWEIGHT, OBESITY, AND RELATED COMORBIDITIES
Vulnerability to obesity is largely driven by genetic, prenatal, developmental, and psychosocial risk factors. In individuals with DMD, this risk is increased further because of glucocorticoid use, decreased mobility, and reduced energy expenditure due to limited options for physical activity. Increased time and financial pressures for families with children who have special health care needs such as DMD also can contribute to risk of obesity and create barriers to successful weight management.2 Once weight is gained, biologic adaptations make it extremely difficult to lose weight and therefore prevention strategies are critical.3 In individuals with DMD, obesity can negatively affect mobility and physical functioning, resulting in falls and fractures; obesity can also exacerbate the metabolic complications associated with glucocorticoid use. Therefore, it is imperative that both obesity prevention strategies and management are incorporated into the care of individuals with DMD.
Little research has been conducted in the area of obesity prevention or management strategies in DMD and in children with physical and developmental disabilities in general.4 Family-based behavioral interventions have shown modest reduction in BMI in the short-term for children and youth with obesity in the absence of developmental and physical disabilities.5,6 One small study (n = 3) on the treatment of obesity in children with DMD that targeted parents revealed inconsistent changes in body weight, increases in children’s perceived quality of life, and increases in healthy foods available at home. However, a larger randomized controlled trial (RCT) is needed to more effectively examine the efficacy of such an approach.7 Two small pharmacotherapeutic trials have been conducted, one with metformin8 and the other with topimarate,9 but there remains insufficient evidence regarding the benefit and safety of these medications in this clinical context. Given the paucity of evidence and research in this area, the unique determinants of obesity in individuals with DMD should be used to guide effective obesity prevention and management strategies that can feasibly be implemented in their care.
Obesity Prevention
Obesity prevention strategies should be introduced at 3 key time points: (1) diagnosis, (2) time of glucocorticoid initiation, and (3) time of loss of mobility. Particular attention should be given to patients who have a family history of obesity, given the highly hereditary nature of obesity.10 An increase in weight or BMI z score of ≥0.5 also should trigger intervention.11
Obesity prevention strategies should aim to facilitate a healthy home food environment of mostly whole foods, regular and predictable times for meals and snacks that are mostly home prepared, family meals, limits on sugar-sweetened beverage consumption and restaurant meals, and encouragement of screen-free meals and snacks at the table. This should be done in consultation with a dietitian. Obesity prevention strategies also should include counseling around appropriate sleep hygiene and duration, limitations on screen time, and psychosocial assessments and support for both the patients and their caregivers.12,13
Although physical activity is a mainstay of obesity prevention strategies, the approach to physical activity recommendations in patients with DMD is more measured, and the role of physical activity in DMD remains controversial.14 To avoid disuse atrophy and other secondary complications of inactivity, it is necessary that those who are ambulatory or in the early nonambulatory stage participate in gentle functional strengthening activity, including a combination of swimming pool exercises and recreation-based exercises in the community. Swimming is highly recommended from the early ambulatory to early nonambulatory phase and could be continued in the nonambulatory phase as long as it is medically safe. Additional benefits might be provided by low-resistance strength training and optimization of upper body function. Significant muscle pain or myoglobulinuria in the 24-hour period after a specific activity is a sign of overexertion and that the activity should be modified.15
Monitoring of Weight Status
Monitoring weight status should include measuring body weight and linear height in ambulatory patients or arm span and segmental length in nonambulatory patients at least every 6 months. Both BMI and weight should be plotted on the appropriate curve to determine the percentile for age. Optimal weight status is defined as BMI between the 10th and 85th percentiles. If height is unavailable or there are significant concerns about its accuracy, weight for age can be used, and an appropriate weight gain trajectory as per the growth curve can be another indicator of optimal weight gain. An increase in weight for age or BMI z scores by >0.5 between visits should raise concern and prompt intervention.11
Although body composition is altered in individuals with DMD (lower lean body mass and higher fat mass), the role of direct measurement of body composition remains unclear and is not routinely recommended. Direct measures of adiposity have limited accessibility in most clinical settings and are not sufficiently accurate.16 Although reference data for a number of pediatric dual-energy x-ray absorptiometry body composition measures have been published,17–19 it remains unclear what their clinical applicability will be both within and outside of the population with DMD. Longitudinal data on the relation of adiposity in children to future disease risk in adults also is lacking; therefore, no agreement exists about cut-points for excess adiposity that would constitute obesity.20
Weight Management
More intensive weight management strategies should be introduced if weight for age or BMI z score is increased by >0.5 between visits and/or if BMI is >85th percentile. A referral to an intensive interdisciplinary weight management program or to a clinician with expertise in pediatric weight management should be made if BMI is >85th percentile with associated weight-related health complications and/or if BMI is >95th percentile.
Evidence-based guidelines for managing obesity in individuals with DMD or children with physical and developmental disabilities do not currently exist4; therefore, an adaptation of current clinical practice guidelines for managing pediatric obesity, with the exception of physical activity recommendations, should be applied. The principles of weight management are in essence a more intensive application of obesity prevention strategies (as above). Family participation in lifestyle change is essential, and interventions must include nutritional and psychosocial reassessment and support, with frequent follow-up.6 High-intensity programs (>25 hours of contact with the child and/or family over a 6-month period) were able to demonstrate improvement in weight status 12 months after beginning the intervention.6 These interventions were focused on counseling and behavioral management techniques to assist with implementation of lifestyle change. Interventions may incorporate a structured daily eating plan with the addition of some self-monitoring (through the use of logs) under the supervision of a dietitian who has training in weight management, with careful attention paid to avoid overly restrictive dieting practices. Personnel should include a registered dietitian, physical activity expert, and mental health professional (social worker, counselor, and/or psychologist) who have training in motivational interviewing, goal setting, monitoring, and positive reinforcement techniques. Interventions must be mindful of, and adapted to, the unique needs of the patient and family. More specific recommendations can be found within the “Recommendations for Treatment of Child and Adolescent Overweight and Obesity.”21 Practical clinical resources include The 5As of Pediatric Obesity Management22 and the Healthy Active Living for Families Program.22
Monitoring Weight-Related Health Complications
Metabolic complications of obesity include glucose dysregulation, type 2 diabetes, dyslipidemia, and hypertension. The metabolic complications of obesity are often silent and need to be screened to identify and manage them. Table 1 lists comorbidities for which regular monitoring and possible intervention are recommended. Metabolic complications also are highly heritable, and a family history should result in increased vigilance around screening.23 Glucocorticoid use increases the risk of both obesity and its metabolic complications.
TABLE 1.
Recommended Monitoring for Obesity-Related Comorbidities
| Recommended Monitoring | Intervention | |
|---|---|---|
| Hyperglycemia | History: polyuria, polydipsia Annual random blood glucose and A1C If asymptomatic with random blood glucose ≥11.1 mmol/L, repeat random blood glucose within 1 wk | Dietary assessment Endocrine consultation if: symptomatic with random blood glucose ≥200 mg/dL (11.1 mmol/L) or 2 random blood glucose readings ≥200 mg/dL (11.1 mmol/L) in the absence of symptoms and/or A1C ≥6.5 (American Diabetes Association Clinical Practice Guidelines 2015) |
| Hypertension | Blood pressure should be monitored at each clinic visit (minimum annually, ideally every 6 mo) | Dietary assessment Referral to hypertension clinic if blood pressure >95th% for height and sex on ≥3 occasions taken over wk to mo (Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents, NIH) |
| Dyslipidemia | Random lipid profile annually. If abnormal, arrange for fasting lipid profile | Dietary assessment Refer to lipid clinic if LDL-C ≥160 mg/dL (4.2 mmol/L) and/or non- HDL-C ≥190 mg/dL (4.9 mmol/L) on ≥2 fasting lipid profiles done months apart23 |
| Gastroesophageal reflux disease | Inquire about GERD symptoms (heartburn); minimum annually, ideally every 6 mo | H2 blocker or proton pump inhibitors if symptomatic (2010 guidelines) |
| Obstructive sleep apnea and/or sleep disordered breathing | Inquire about symptoms: morning headaches, daytime somnolence, change in mood, decreased ability to concentrate and/or focus (minimum annually, ideally every 6 mo) | Sleep study and referral to sleep clinic if abnormal |
| Mental health assessment | Inquire about mood and anxiety symptoms, disordered eating patterns, body image, and school functioning | Referral to mental health professional (social worker, psychologist, counselor) for further assessment and support |
GERD, gastroesophageal reflux disease; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; NIH, National Institutes of Health.
Signs and symptoms of obesity-induced biomechanical complications can typically be elicited on routine history and physical examination. Effective management of biomechanical complications, especially sleep apnea and sleep-disordered breathing, may help improve success with weight management.24
Children and youth with obesity are at increased risk of social isolation and stigmatization.25 Childhood psychiatric disorders (depression, anxiety), school difficulties, body dissatisfaction, dysregulated eating behaviors, teasing, and bullying have all been linked with pediatric obesity.26,27 Mental health disorders, as well as some of the pharmacotherapeutic agents that are used to manage them, can complicate weight management, promote weight gain, and affect prognosis and therefore should be routinely monitored through history at clinic visits.28
ENDOCRINE DISORDERS: SHORT STATURE, PUBERTAL DELAY, AND ADRENAL INSUFFICIENCY
Growth Failure Causing Short Stature
Short stature is common in individuals with DMD. Observational studies of glucocorticoid-naïve, ambulatory patients with DMD have described a growth pattern marked by (1) normal length at birth, (2) below-average growth velocity in early life, and (3) age-appropriate growth velocity at a below-average height percentile for the remainder of childhood.28,29 A study of ambulatory patients with DMD revealed that participants were shorter than expected for age by an average of 4.3 cm compared with reference data.30,31 The authors of a natural history study reported that the median height of participants at age 18 years was below the fifth percentile.32 The etiology of the impaired growth in individuals with DMD remains unclear because growth hormone secretion in response to provocative testing,33 circulating growth factors,28 and skeletal maturation29 were normal in patients with DMD.
Growth impairment in DMD is exacerbated by glucocorticoid treatment.34–36 Current recommendations support the initiation of glucocorticoid therapy before functional decline; therefore, patients are exposed to the deleterious effects of glucocorticoid for the majority of their growth.37 Glucocorticoid treatment regimens vary and may affect growth differently. Growth impairment was observed irrespective of agent (prednisone, prednisolone, deflazacort) in a natural history study.38 However, an RCT revealed that a weekend-only prednisone regimen resulted in greater growth compared with daily dosing.39 The mechanisms underlying the growth inhibitory effects of glucocorticoids are complex. Glucocorticoid exposure appears to inhibit growth hormone release,40 antagonize the peripheral action of growth hormone and IGF-1,41–43 and induce chondrocyte apoptosis at the growth plate.44
Growth should be verified every 6 months in all patients with DMD until puberty has finished and final adult height has been reached.37 Standing height is acceptable for patients who are still walking, with the results compared with a standardized growth curve. A DMD-specific growth curve derived from glucocorticoid-naïve patients is available for patients ages 2 to 12 years, although its clinical usefulness is untested.30 Growth is evaluated differently in nonambulatory patients, ideally starting before loss of ambulation to permit tracking of the growth rate during transition from walking to nonambulatory. Arm span, ulnar and tibia lengths, knee height, and segmental measurements of recumbent length have been proposed.45 However, these methods have not been specifically validated in DMD. A finding of impaired growth (downward crossing of percentile for height, height velocity <4 cm/year, or height below the third percentile) should prompt consultation with an endocrinologist. A standard clinical evaluation should be performed in all patients with DMD with growth failure to identify treatable hormonal or other causes (Fig 1, Table 2).
FIGURE 1.
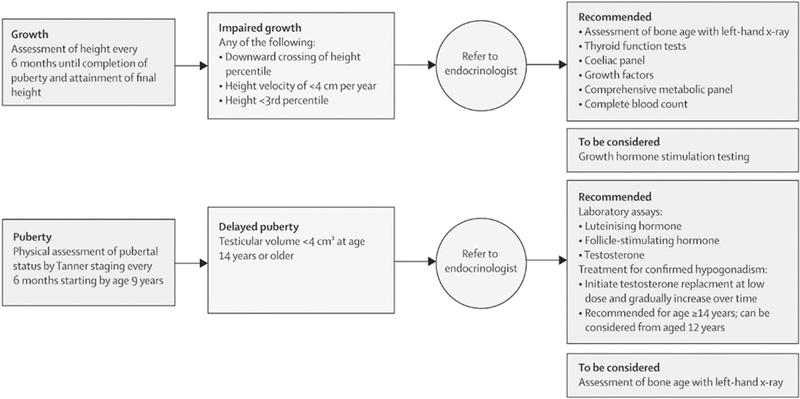
Assessments and interventions for impaired growth and delayed puberty in patients with DMD. (Reproduced with permission from Birnkrant DJ, Bushby K, Bann CM, et al; DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, an update, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018;17[3]:258.)
TABLE 2.
Recommended Biochemical and Radiographic Tests for the Evaluation of Impaired Growth and Delayed Puberty in Individuals With DMD
| Impaired growth at any age as defined by any of the following | |
| Downward crossing of height percentile | |
| Height velocity of <4 cm/y | |
| Height less than third percentile | |
| Recommended | To be considered |
| Bone age radiograph of left hand | Growth hormone stimulation testinga |
| Thyroid function testsb | |
| Celiac panel | |
| Growth factorsc | |
| Comprehensive metabolic paneld | |
| Complete blood count | |
| Delayed puberty as defined by | |
| Testicular volume <4 cm3 at age 14 y or older | |
| Recommended | To be considered |
| Luteinizing hormonee | Bone age radiograph of left hand |
| Follicular stimulating hormone |
Routine use of growth hormone in the treatment of impaired growth is not recommended. Stimulation testing should be performed on an individual basis only in patients in whom a compelling clinical case for the use of growth hormones exists.
Thyrotropin and total or free thyroxine.
Insulin-like growth factor 1 and/or insulin-like growth factor binding protein 3.
Sodium, potassium, chloride, bicarbonate, serum urea nitrogen, creatinine, calcium, albumin, alkaline phosphatase, and alanine- and aspartate-aminotransferase.
Luteinizing hormone, follicular stimulating hormone, and testosterone should be checked at 8:00 am and assessed by using appropriate pediatric or ultrasensitive assay.
The treatment of DMD-related short stature is controversial. Recombinant human growth hormone (rhGH) is commonly used to treat hypothalamic and/or pituitary growth hormone deficiency and a handful of other childhood conditions.46 To date, no RCTs have been conducted to evaluate the efficacy and safety of rhGH to improve growth in individuals with DMD. The only RCT of rhGH conducted in this population was designed to investigate cardiac outcomes. The researchers found that rhGH was well tolerated and that left ventricular mass increased with treatment. However, no height outcomes were reported.40 The largest report of clinical rhGH use in individuals with DMD included 39 boys and revealed that growth velocity increased from 1.3 to 5.2 cm/year over 12 months.47 No detrimental musculoskeletal or pulmonary effects were observed, although 3 boys developed known rhGH-related adverse events (impaired fasting glucose, worsening of scoliosis, and benign intracranial hypertension). Adding to the controversy are theoretical concerns that increased growth may worsen muscle function in this context.48,49 The relevance of this evidence to humans remains uncertain, however, and clinical trials investigating the use of mazindol, a postulated inhibitor of growth hormone release, yielded inconsistent effects on growth suppression and no benefits on muscle strength.33, 50–53 In light of limited data and the ongoing controversy, regular use of rhGH in the population with DMD is not recommended. The decision to use rhGH should be made on a case-by-case basis with biochemical evidence of growth hormone deficiency, and after a discussion of the benefits and known plus unknown risks. For example, it is unknown whether rhGH adversely affects muscle strength.
Delayed Pubertal Development
Delayed or absent pubertal development in glucocorticoid-treated patients with DMD is due to hypogonadotropic hypogonadism54 and may negatively affect physical health, psychosocial development, and self-esteem. Studies have revealed that pubertal delay in individuals with DMD is common, with a prevalence of 50% to 100% in glucocorticoid-treated boys.55,56 No published RCTs have contained assessments of the safety and efficacy of testosterone to induce puberty in individuals with DMD. However, the authors of a retrospective study of 14 boys treated with testosterone reported patient satisfaction with treatment and increased growth velocity in the first year of therapy.57 Testosterone is widely used in pediatrics to induce puberty and is specifically advised in treatment of adult men with glucocorticoid- induced hypogonadism.58
All patients with DMD should undergo monitoring of pubertal development by physical examination every 6 months starting at age 9 years (Fig 1).37 A finding of delayed puberty (absence of testicular enlargement ≥4 cm3 by age 14 years) should prompt referral to an endocrinologist. Testosterone is recommended starting by age 14 years (or by 12 years in those on glucocorticoids) at a low dose and should be increased gradually over 2 to 3 years until adult testosterone levels are achieved. Examples of commonly used testosterone regimens are provided in Table 3. Patients and families should be counseled about expected effects, including body odor, facial hair, acne, growth spurt, growth plate closure, and increased libido. Testosterone levels should be monitored to adjust dose. Annual monitoring of hemoglobin and/or hematocrit, lipids, and serum glucose should be considered.58 An unexpected adverse effect on muscle or cardiac health may warrant discontinuation or dose reduction.
TABLE 3.
Example Testosterone Replacement Regimens in DMD Patients With Confirmed Hypogonadism
| Formulationa | Dose Titrationb |
|---|---|
| Intramuscular | |
| Testosterone enanthate or cypionate | Initiate at 50 mg once monthly Increase dose by 50 mg every 3–6 mo over a period of 2–3 y Typical adult regimens include 150–200 mg every 2 wk or 75–150 mg every wk Serum testosterone levels should be monitored every 3–6 mo Target testosterone levels (drawn 1 wk after injection) in the midnormal range (350–750 ng/dL [12–26 nmol/L]) |
| Transdermal | |
| Gels (pumps or packets) | Initiate at lowest possible daily dose given formulation |
| 1% gel (12.5–50 mg per application) | Increase dose gradually every 3–6 mo over a period of 2–3 y |
| 1.62% gel (20.25–40.5 mg per application) | Typical adult regimens range from 20.25 to 100 mg daily based on formulation |
| 2% gel (10 mg per application) | Serum testosterone levels should be monitored every 3–6 mo Target testosterone levels (drawn any time) in the midnormal range (350–750 ng/dL [12–26 nmol/L]) |
| Patch | Not commonly used to initiate puberty |
| 2–4 mg per patch applied daily | May be a convenient option for some patients once typical adult replacement levels have been achieved Typical adult regimens range from 2 to 4 mg daily Serum testosterone levels should be monitored every 3 to 6 mo Target testosterone levels (drawn 3–12 h after patch placed) in the midnormal range (350–750 ng/dL [12–26 nmol/L]) |
Other testosterone formulations may be available depending on country. Consult prescribing information provided by manufacturer for recommended dosing.
Adult dosing and monitoring recommendations adapted from the Endocrine Society Clinical Practice Guideline for testosterone therapy in adult men with androgen deficiency syndromes.58
Currently, the expected benefit of restoring testosterone to normal physiologic levels is felt to outweigh potential risks of treatment. However, future studies are needed to identify the optimal timing and regimen for testosterone replacement in individuals with DMD.
Glucocorticoid Dependence and Adrenal Insufficiency
Chronic glucocorticoid therapy at the doses used on individuals with DMD leads to a suppressed hypothalamic-pituitary-adrenal (HPA) axis. Patients are therefore at risk for life-threatening adrenal crisis should glucocorticoid therapy be stopped suddenly and also during times of severe injury or illness.59 All patients on glucocorticoids should be taught the symptoms, signs, and appropriate management of adrenal crisis at the time of initial glucocorticoid prescription, including intramuscular hydrocortisone administrative for home use in the event the patient cannot take his usual glucocorticoid therapy because of vomiting. Patient education should also include emergency administration of intramuscular hydrocortisone and instructions for stress dosing during times of illness, trauma, or surgical intervention (Table 4). The need for education around intramuscular hydrocortisone is testament to the potentially life-threatening nature of adrenal suppression in the face of illness and surgery. Glucocorticoid therapy is never discontinued abruptly, but rather tapered slowly to allow HPA recovery. A steroid taper should adhere to the following guidance: (1) gradual dose reduction; (2) monitoring for signs and/or symptoms of adrenal insufficiency (fatigue, headache, nausea and/or vomiting, hypoglycemia, hypotension); (3) dose increase and slowing of taper in response to signs or symptoms; and (4) continuation of stress steroid coverage until the taper is complete and the HPA axis has been proven normal by an adequate cortisol response to corticorelin or corticotropin stimulation (peak cortisol >20 μg/dL [550 nmol/L]).60 HPA axis recovery can take months to years.61,62 Periodic monitoring of 8:00 AM cortisol levels for a return to a normal value (eg, >6 μg/dL [165 nmol/L])63 can guide the decision around when to discontinue daily steroid therapy and to perform stimulation testing, recognizing that the precise threshold that is used to define a normal 8:00 AM cortisol may vary depending on institution-specific practice standards. Irrespective of the specific threshold that is used to signal discontinuation of daily physiologic steroid therapy, an expert in adrenal suppression management should interpret the 8:00 AM cortisol results in light of the child’s clinical status and in accordance with local practice standards. These decisions are typically made in collaboration with an endocrinologist. A protocol for the management of adrenal suppression has been developed previously64 and endorsed by the DMD Care Considerations Working Group.
TABLE 4.
Management of Adrenal Suppression in Patients on Chronic Glucocorticoid Therapy
| Stress Situation | Stress Dosing Recommendations |
|---|---|
| Mild | 25 mg/m2 per da hydrocortisone or equivalentb divided every 6–8 h PO |
| Mild febrile illness | Continue for 24 h after return to baseline health |
| Minor surgical procedure requiring anesthesia | |
| Moderate | 50 mg/m2 per d hydrocortisone or Eq divided every 6–8 h PO, IM, or IV |
| Moderate illness requiring hospital admission | Consider taper as clinical condition improves |
| Major elective surgery requiring anesthesia | |
| Severe | 100 mg/m2 hydrocortisone IM or IV followed by |
| Severe vomiting, loss of consciousness | 100 mg/m2 per d hydrocortisone divided every 4–6 h IV |
| Septic shock | Consider taper as clinical condition improves |
| Severe trauma or illness requiring emergent surgery | |
| Example steroid taperc | |
| Decrease prednisone and/or deflazacort dose by 20%–25% every 2 wk | |
| Once physiologic dose is achieved (3 mg/m2 per d of prednisone and/or deflazacort) switch to hydrocortisone 12 mg/m2 per d divided in 3 equal doses | |
| Continue to wean dose by 20%–25% every 2 wk until a dose of 2.5 mg hydrocortisone every other d is achieved | |
| After 2 wk of every other d dosing, discontinue hydrocortisone | |
| Periodically check am cortisol or CRH and/or corticotropin stimulated cortisol level until HPA axis is determined to be normald | |
| Continue stress dose coverage until HPA axis has recovered. This may take up to 12 mo or longer | |
AM, morning; CRH, corticorelin; IM, intramuscular; IV, intravenous; PO, per os (oral).
Doses expressed in terms of milligram per body surface area (in meters2).
Or equivalent. Multiply prednisone dose (milligram) by 4 to convert to hydrocortisone equivalents (milligram). Many patients on standard prednisone regimens will not require supplemental hydrocortisone for mild or moderate stress if able to continue usual home doses.
Adapted from Parent Project Muscular Dystrophy.1
Adequate cortisol response to CRH or ACTH stimulation (peak cortisol >20 μg/dL [550 nmol/L]).
CONCLUSIONS
Because of the positive effects of glucocorticoid therapy on ambulation, mitigation of scoliosis, and cardiorespiratory function in individuals with DMD, glucocorticoid therapy has been widely adopted as the standard of care for pediatric and adult patients with DMD. At the same time, the adverse effects of glucocorticoid therapy on weight management and the hormonal milieu are often troubling for patients and in some cases are potentially life-threatening (in the case of glucocorticoid-dependence and adrenal insufficiency). To maintain a positive benefit-to-toxicity ratio, glucocorticoid therapy to treat the underlying disease should be integrated with clinical programs that effectively address the resulting side effects. In most cases, this will require a multidisciplinary effort, with input from neuromuscular specialists, endocrinologists, primary health care providers, and clinicians with expertise in obesity management. A comprehensive approach to monitoring and managing these important side effects should not be viewed as optional but rather a mandatory component of the approach to glucocorticoid therapy in this setting.
ACKNOWLEDGMENTS
We thank Victor Konji for his assistance in the preparation of references for the manuscript. Dr Leanne M. Ward was supported by the Canadian Institutions for Health Research Operating Grants Program, the Canadian Child Health Clinician Scientist Program, the Children’s Hospital of Eastern Ontario Research Institute, the University of Ottawa Research Chair Program, and the Children’s Hospital of Eastern Ontario Departments of Pediatrics and Surgery.
FUNDING: Supported in part by the Cooperative Agreement, NU38OT000167, funded by the Centers for Disease Control and Prevention. Dr Ward was supported by a Research Chair from the University of Ottawa.
ABBREVIATIONS
- DMD:
Duchenne muscular dystrophy
- HPA:
hypothalamic-pituitary-adrenal
- RCT:
randomized controlled trial
- rhGH:
recombinant human growth hormone
Footnotes
POTENTIAL CONFLICT OF INTEREST: Dr Weber has previously served as a paid consultant for Marathon Pharmaceuticals; Drs Ward, Hadjiyannakis, McMillan, and Noritz have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: Other than those listed under Potential Conflict of Interest; the other authors have indicated they have no financial relationships relevant to this article to disclose.
The guidelines or recommendations in this article are not American Academy of Pediatrics policy and publication herein does not imply endorsement.
Dr Ward served as chairperson for the Duchenne Muscular Dystrophy Care Considerations Endocrine and Bone Health Working Group, as convened by the Centers for Disease Control and Prevention, and drafted the initial outline for the manuscript; Drs Weber and Hadjiyannakis served on the Duchenne Muscular Dystrophy Care Considerations Endocrine and Bone Health Working Group, as convened by the Centers for Disease Control and Prevention, contributed to the development of corresponding recommendations, and drafted the initial manuscript; Drs McMillan and Noritz served on the Duchenne Muscular Dystrophy Care Considerations Endocrine and Bone Health Working Group, as convened by the Centers for Disease Control and Prevention, and contributed to the development of corresponding recommendations; and all authors reviewed and revised the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
REFERENCES
- 1.Kinnett K, Noritz G. The PJ Nicholoff steroid protocol for Duchenne and Becker muscular dystrophy and adrenal suppression. PLoS Curr. 2017;9:ecurrents.md.d18deef 7dac96ed135e0dc8739917b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Must A, Curtin C, Hubbard K, Sikich L, Bedford J, Bandini L. Obesity prevention for children with developmental disabilities. Curr Obes Rep. 2014;3(2):156–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz AV. Diabetes mellitus: does it affect bone? Calcif Tissue Int. 2003;73(6):515–519 [DOI] [PubMed] [Google Scholar]
- 4.Bandini L, Danielson M, Esposito LE, et al. Obesity in children with developmental and/or physical disabilities. Disabil Health J. 2015;8(3):309–316 [DOI] [PubMed] [Google Scholar]
- 5.Vincent C, Gagnon D, Routhier F, et al. ; ADMI Group. Service dogs in the province of Quebec: sociodemographic profile of users and the dogs’ impact on functional ability. Disabil Rehabil Assist Technol. 2015;10(2):132–140 [DOI] [PubMed] [Google Scholar]
- 6.Barton M; US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125(2):361–367 [DOI] [PubMed] [Google Scholar]
- 7.Arikian A, Boutelle K, Peterson CB, Dalton J, Day JW, Crow SJ. Targeting parents for the treatment of pediatric obesity in boys with Duchenne muscular dystrophy: a case series. Eat Weight Disord. 2010;15(3):e161–e165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casteels K, Fieuws S, van Helvoirt M, et al. Metformin therapy to reduce weight gain and visceral adiposity in children and adolescents with neurogenic or myogenic motor deficit. Pediatr Diabetes. 2010;11(1):61–69 [DOI] [PubMed] [Google Scholar]
- 9.Carter GT, Yudkowsky MP, Han JJ, McCrory MA. Topiramate for weight reduction in Duchenne muscular dystrophy. Muscle Nerve. 2005;31 (6):788–789 [DOI] [PubMed] [Google Scholar]
- 10.Farooqi S, O’ Rahilly S Genetics of obesity in humans. Endocr Rev. 2006; 27(7):710–718 [DOI] [PubMed] [Google Scholar]
- 11.Ford AL, Hunt LP, Cooper A, Shield JP What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child. 2010;95(4):256–261 [DOI] [PubMed] [Google Scholar]
- 12.Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4): S164–S192 [DOI] [PubMed] [Google Scholar]
- 13.Tremblay MS, Carson V, Chaput JP et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016; 41(6 suppl 3):S311–S327 [DOI] [PubMed] [Google Scholar]
- 14.Markert CD, Ambrosio F, Call JA, Grange RW. Exercise and Duchenne muscular dystrophy: toward evidence-based exercise prescription. Muscle Nerve. 2011;43(4):464–478 [DOI] [PubMed] [Google Scholar]
- 15.Bushby K, Finkel R, Birnkrant DJ, et al. ; DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, part 2: implementation of multidisciplinary care. Lancet Neurol. 2010;9(2):177–189 [DOI] [PubMed] [Google Scholar]
- 16.Wells JC, Fewtrell MS. Measuring body composition. Arch Dis Child. 2006;91(7):612–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogden CL, Li Y, Freedman DS, Borrud LG, Flegal KM. Smoothed percentage body fat percentiles for U.S. children and adolescents, 1999–2004. Natl Health Stat Rep. 2011;(43):1–7 [PubMed] [Google Scholar]
- 18.Wells JC, Williams JE, Chomtho S, et al. Body-composition reference data for simple and reference techniques and a 4-component model: a new UK reference child. Am J Clin Nutr. 2012;96(6):1316–1326 [DOI] [PubMed] [Google Scholar]
- 19.Weber DR, Moore RH, Leonard MB, Zemel BS. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am J Clin Nutr 2013;98(1):49–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics. 2009;124(suppl 1):S23–S34 [DOI] [PubMed] [Google Scholar]
- 21.Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007; 120(suppl 4):S254–S288 [DOI] [PubMed] [Google Scholar]
- 22.American Academy of Pediatrics. Healthy Active Living for Families (HALF) program. 2016. Available at: https://www.aap.org/en-us/advocacy-and-policy/a ap-health-in itiatives/HALF-Implementation-Guide/Pages/About-HALF.aspx. Accessed July 20, 2016
- 23.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213–S256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harsch IA, Konturek PC, Koebnick C, et al. Leptin and ghrelin levels in patients with obstructive sleep apnoea: effect of CPAP treatment. Eur Respir J. 2003;22(2):251–257 [DOI] [PubMed] [Google Scholar]
- 25.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull. 2007;133(4):557–580 [DOI] [PubMed] [Google Scholar]
- 26.Gonzalez A, Boyle MH, Georgiades K, Duncan L, Atkinson LR, MacMillan HL. Childhood and family influences on body mass index in early adulthood: findings from the Ontario Child Health Study. BMC Public Health. 2012;12:755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Russell-Mayhew S, McVey G, Bardick A, Ireland A. Mental health, wellness, and childhood overweight/obesity. J Obes. 2012;2012:281801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagel BH, Mortier W, Elmlinger M, Wollmann HA, Schmitt K, Ranke MB. Short stature in Duchenne muscular dystrophy: a study of 34 patients. Acta Paediatr. 1999;88(1):62–65 [PubMed] [Google Scholar]
- 29.Eiholzer U, Boltshauser E, Frey D, Molinari L, Zachmann M. Short stature: a common feature in Duchenne muscular dystrophy. Eur J Pediatr. 1988;147(6):602–605 [DOI] [PubMed] [Google Scholar]
- 30.West NA, Yang ML, Weitzenkamp DA, et al. Patterns of growth in ambulatory males with Duchenne muscular dystrophy. J Pediatr. 2013;163(6): 1759–1763.e1 [DOI] [PubMed] [Google Scholar]
- 31.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11 2002;(246):1–190 [PubMed] [Google Scholar]
- 32.McDonald CM, Abresch RT, Carter GT et al. Profiles of neuromuscular diseases. Duchenne muscular dystrophy. Am J Phys Med Rehabil. 1995;74(suppl 5):S70–S92 [DOI] [PubMed] [Google Scholar]
- 33.Zatz M, Rapaport D, Vainzof M, et al. Effect of mazindol on growth hormone levels in patients with Duchenne muscular dystrophy. Am J Med Genet 1988;31 (4):821–833 [DOI] [PubMed] [Google Scholar]
- 34.Biggar WD, Harris VA, Eliasoph L, Alman B. Long-term benefits of deflazacort treatment for boys with Duchenne muscular dystrophy in their second decade. Neuromuscul Disord. 2006;16(4):249–255 [DOI] [PubMed] [Google Scholar]
- 35.Houde S, Filiatrault M, Fournier A, et al. Deflazacort use in Duchenne muscular dystrophy: an 8-year follow-up. Pediatr Neurol. 2008;38(3):200–206 [DOI] [PubMed] [Google Scholar]
- 36.Moxley RT III, Pandya S, Ciafaloni E, Fox DJ, Campbell K. Change in natural history of Duchenne muscular dystrophy with long-term corticosteroid treatment: implications for management. J Child Neurol. 2010;25(9):1116–1129 [DOI] [PubMed] [Google Scholar]
- 37.Birnkrant DJ, Bushby K, Bann CM, et al. ; DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol. 2018;17(4):347–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bello L, Gordish-Dressman H, Morgenroth LP, et al. ; CINRG Investigators. Prednisone/ prednisolone and deflazacort regimens in the CINRG Duchenne Natural History Study. Neurology. 2015;85(1 2):1048–1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Escolar DM, Hache LP, Clemens PR, et al. Randomized, blinded trial of weekend vs daily prednisone in Duchenne muscular dystrophy. Neurology. 2011;77(5):444–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cittadini A, Ines Comi L, Longobardi S, et al. A preliminary randomized study of growth hormone administration in Becker and Duchenne muscular dystrophies. Eur Heart J. 2003;24(7):664–672 [DOI] [PubMed] [Google Scholar]
- 41.Wehrenberg WB, Janowski BA, Piering AW, Culler F, Jones KL. Glucocorticoids: potent inhibitors and stimulators of growth hormone secretion. Endocrinology. 1990;126(6):3200–3203 [DOI] [PubMed] [Google Scholar]
- 42.Allen DB, Julius JR, Breen TJ, Attie KM. Treatment of glucocorticoid- induced growth suppression with growth hormone. National Cooperative Growth Study. J Clin Endocrinol Metab. 1998;83(8):2824–2829 [DOI] [PubMed] [Google Scholar]
- 43.Jux C, Leiber K, Hügel U, et al. Dexamethasone impairs growth hormone (GH)-stimulated growth by suppression of local insulin-like growth factor (IGF)-I production and expression of GH- and IGF-I-receptor in cultured rat chondrocytes. Endocrinology. 1998;139(7):3296–3305 [DOI] [PubMed] [Google Scholar]
- 44.Chrysis D, Ritzen EM, Sävendahl L. Growth retardation induced by dexamethasone is associated with increased apoptosis of the growth plate chondrocytes. J Endocrinol. 2003;176(3):331–337 [DOI] [PubMed] [Google Scholar]
- 45.Lohman TG, Roche AF, Martorell R, eds. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics Books; 1988 [Google Scholar]
- 46.Hardin DS, Kemp SF, Allen DB. Twenty years of recombinant human growth hormone in children: relevance to pediatric care providers. Clin Pediatr (Phila). 2007;46(4):279–286 [DOI] [PubMed] [Google Scholar]
- 47.Rutter MM, Collins J, Rose SR, et al. Growth hormone treatment in boys with Duchenne muscular dystrophy and glucocorticoid-induced growth failure. Neuromuscul Disord. 2012;22(12):1046–1056 [DOI] [PubMed] [Google Scholar]
- 48.Zatz M, Rapaport D, Vainzof M, et al. Relation between height and clinical course in Duchenne muscular dystrophy. Am J Med Genet 1988;29(2):405–410 [DOI] [PubMed] [Google Scholar]
- 49.Bodor M, McDonald CM. Why short stature is beneficial in Duchenne muscular dystrophy. Muscle Nerve. 2013;48(3):336–342 [DOI] [PubMed] [Google Scholar]
- 50.Coakley JH, Moorcraft J, Hipkin LJ, Smith CS, Griffiths RD, Edwards RH. The effect of mazindol on growth hormone secretion in boys with Duchenne muscular dystrophy. J Neurol Neurosurg Psychiatry. 1988;51 (12):1551–1557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zatz M, Rapaport D, Pavanello RC, Rocha JM, Vainzof M, Nicolau W. Nocturnal rhythm of growth hormone in Duchenne patients: effect of different doses of mazindol and/ or cyproheptadine. Am J Med Genet 1989;33(4):457–467 [DOI] [PubMed] [Google Scholar]
- 52.Collipp PJ, Kelemen J, Chen SY, Castro-Magana M, Angulo M, Derenoncourt A. Growth hormone inhibition causes increased selenium levels in Duchenne muscular dystrophy: a possible new approach to therapy. J Med Genet 1984;21 (4):254–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Griggs RC, Moxley RT III, Mendell JR, et al. Randomized, double-blind trial of mazindol in Duchenne dystrophy. Muscle Nerve. 1990;13(12):1169–1173 [DOI] [PubMed] [Google Scholar]
- 54.Rosen H, Jameel ML, Barkan AL. Dexamethasone suppresses gonadotropin-releasing hormone (GnRH) secretion and has direct pituitary effects in male rats: differential regulation of GnRH receptor and gonadotropin responses to GnRH. Endocrinology. 1988;122(6):2873–2880 [DOI] [PubMed] [Google Scholar]
- 55.Merlini L, Gennari M, Malaspina E, et al. Early corticosteroid treatment in 4 Duchenne muscular dystrophy patients: 14-year follow-up. Muscle Nerve. 2012;45(6):796–802 [DOI] [PubMed] [Google Scholar]
- 56.Dooley JM, Bobbitt SA, Cummings EA. The impact of deflazacort on puberty in Duchenne muscular dystrophy. Pediatr Neurol. 2013;49(4):292–293 [DOI] [PubMed] [Google Scholar]
- 57.Wood CL, Cheetham TD, Guglieri M, et al. Testosterone treatment of pubertal delay in Duchenne muscular dystrophy. Neuropediatrics. 2015;46(6):371–376 [DOI] [PubMed] [Google Scholar]
- 58.Bhasin S, Cunningham GR, Hayes FJ, et al. ; Task Force, Endocrine Society. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536–2559 [DOI] [PubMed] [Google Scholar]
- 59.Shulman DI, Palmert MR, Kemp SF; Lawson Wilkins Drug and Therapeutics Committee. Adrenal insufficiency: still a cause of morbidity and death in childhood. Pediatrics. 2007;119(2). Available at: www.pediatrics.org/cgi/content/full/119/2/e484 [DOI] [PubMed] [Google Scholar]
- 60.Puar TH, Stikkelbroeck NM, Smans LC, Zelissen PM, Hermus AR. Adrenal crisis: still a deadly event in the 21st century. Am J Med. 2016;129(3):339 e1–339.e9 [DOI] [PubMed] [Google Scholar]
- 61.Huber BM, Bolt IB, Sauvain MJ, Flück CE. Adrenal insufficiency after glucocorticoid withdrawal in children with rheumatic diseases. Acta Paediatr. 2010; 99(12):1889–1893 [DOI] [PubMed] [Google Scholar]
- 62.Jamilloux Y, Liozon E, Pugnet G, et al. Recovery of adrenal function after long-term glucocorticoid therapy for giant cell arteritis: a cohort study. PLoS One. 2013;8(7):e68713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Charmandari E, Nicolaides NC, Chrousos GP. Adrenal insufficiency. Lancet. 2014;383(9935):2152–2167 [DOI] [PubMed] [Google Scholar]
- 64.Birnkrant DJ, Bushby K, Bann CM, et al. ; DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018; 17(3):251–267 [DOI] [PMC free article] [PubMed] [Google Scholar]


