Short abstract
Objective
To compare medium-term clinical and radiological outcomes of primary unilateral uncemented (UN) or cemented (CE) femoral component total hip arthroplasty (THA) in elderly patients with osteoporosis.
Methods
Consecutive patients with osteoporosis who underwent primary unilateral UN or CE THAs at our institution from 2006 to 2013 were retrospectively reviewed. All consecutive procedures were managed by high-volume surgeons, using UN or CE THA approaches. Follow-up assessments occurred at 1, 3, 6, 9, and 12 months postoperatively, and yearly thereafter. Patient-related functional outcomes were assessed using the Harris Hip Score (HHS). Primary and secondary endpoints were early revision (<5 years) and functional outcome.
Results
In total, 496 primary unilateral THAs (CE, n = 184; UN, n = 182) were assessed with a median follow-up period of 75 months (range, 65–86 months). From 3 months after surgery to the final follow-up, HHS was consistently superior in the CE group. Respective prosthetic loosening rates in the UN and CE groups were 26.4% and 16.8% at a minimum of 5 years. There was a significant difference in rate of early revision (7.6% CE vs. 14.8% UN).
Conclusion
Compared with UN THA, CE THA exhibits a superior outcome in elderly patients with primary osteoporosis.
Keywords: Total hip arthroplasty, revision, osteoporosis, failure, uncemented, cemented
Introduction
Total hip arthroplasty (THA) is a mature and economically effective surgical treatment for femoral neck fractures or hip joint diseases in elderly patients.1,2 The primary purpose of this treatment is to reduce pain, as well as to improve joint function and quality of life.3 In recent years, the hip joint function and the prosthesis survival rate following THAs have made remarkable progress, based on the development of clinical THAs, deepening of scientific research, and continuous improvement and innovation in the field of prosthesis.4 The success of THA and increasing utilization of this treatment approach are supported by the development of bone cement and improvement of low prosthesis-related wear rate; these contribute to extended survival of prostheses.5 However, prosthesis design and technical characteristics of bone cement lead to “bone cement disease,” which is regarded as the primary cause of prosthesis loosening.1 Although biological fixation of uncemented (UN) femoral component THA has resolved some problems caused by fixation of cemented (CE) femoral component THA, some phenomena remain, such as prosthesis loosening and bone dissolution.2,6 Thus far, there is no consensus regarding the efficacies of UN and CE femoral component THAs.
The purpose of this study was to compare medium-term clinical and radiological outcomes of primary unilateral UN or CE femoral component THA in elderly patients with osteoporosis. The primary endpoint was early revision (<5 years); the secondary endpoint was functional outcome.
Material and methods
Study population
This study was approved by the Medical Ethics Committee (The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology; The First Affiliated Hospital, Sun Yat-sen University; Jinshan Hospital, Fudan University); a waiver for the requirement of informed consent was obtained from the appropriate Investigational Ethics Review Board.
This was a retrospective analysis of prospectively gathered data from the total joint registry of the South China Hip Arthroplasty Registry, which was established in 1997 and contains the records (e.g., demographics, surgery and implant details, evaluation time, complications, pain, radiographs, and functional evaluations) of consecutive patients with osteoporosis who underwent primary CE or UN femoral component THA from June 2006 to February 2013. The International Classification of Diseases (9th revision, code 81.51) and Current Procedural Terminology (4th edition, code 27130) were utilized to identify patients for this analysis. Primary THA was performed using available bone stock, to correct femoral deformity, by proficient, fellowship-trained surgeons; all surgeons had 10–12 years of experience in performing the direct anterior approach (DAA). Follow-up was calculated with reference to the first day after primary THA surgery. Patient-related clinical and radiological outcomes were analyzed. Patients who were unable to attend the clinic due to remote location or frailty were followed up at community clinics or by phone interview; remote X-rays were performed to assess THA-related status since primary THA. For patients who had died from irrelevant diseases, information regarding THA-related status prior to death was collected from the patients’ families. Inclusion criteria were as follows: patients aged 60–80 years; patients with osteoporosis who underwent primary unilateral UN or CE femoral component THA (Stryker Corporation, Kalamazoo, MI, USA) using the Vitalock acetabular component (a 28-mm modular chromium-cobalt femoral head, Stryker Howmedica, Warsaw, IN, USA); patients who were able to walk independently without aid, prior to THA, and who could comprehend instructions and follow a rehabilitation program. Exclusion criteria were as follows: patients with inadequate clinical data; patients who refused to participate; patients with pathological fractures, ipsilateral lower-limb surgery, planned surgery, Injury Severity Score ≥9, severe medical-related disease, advanced tumor, co-occurring mental illness, cognitive dysfunction, and/or an American Society of Anesthesiologists score of IV or V.
Surgical technique
Preoperative preparation included applicable prosthesis selection to optimize the reproduction of the anatomic geometry of the hip, to restructure the center of rotation, offset, and limb length. All surgeries were performed by the senior authors (JJL, CY, YZ, and MZ), using a single surgical technique. The patient was placed in the lateral decubitus position. Under general anesthesia, DAA, a modification of the classic Smith-Peterson approach, began 2–3 cm posterior and distal to the anterior superior iliac spine; the approach then was extended slightly obliquely, in a posterior direction, for 8–10 cm. After division of the skin and subcutis, the fascia layer was exposed and separated in the direction of the muscle fiber. Along the adipose bands, blunt dissection was performed from the fingers to the top of the femur neck. The tensor fascia lata was carefully separated from the sartorius, to expose the joint capsule. The lower extremity was fully turned inward; simultaneously, the greater trochanter was rotated from the lateral rear to the lateral. This was followed by femoral neck osteotomy, removal of the femoral head, and widening of the acetabulum. The proximal end of the femur was lifted by external rotation, and the posterolateral joint capsule was excised. Acceptable positioning of the femoral stem was confirmed with fluoroscopy, then followed by placement of a head on the femoral component. The femoral component and acetabular cup were installed in the conventional manner, using surgical techniques described in detail in previous literature.7
Perioperative management
Cefazolin, intravenous prophylactic antibiotic therapy, was administered 30 minutes prior to surgery, and continued for 3 days. Intravenous tranexamic acid (10 mg/kg) was administered 30 minutes prior to surgery if patients had no history of thromboembolism. Oral rivaroxaban was administered 6 hours after surgery, and continued for 2 months. Drainage was removed 2 days postoperatively. Under the guide of rehabilitation therapists, patients were required to complete a short mobilization on the day of surgery and begin full weight-bearing with walking aids during the 2nd week after surgery.
Method of assessment
Patients were reviewed clinically and radiographically at 1, 3, 6, 9, and 12 months postoperatively, and yearly thereafter. Preoperative, postoperative, and follow-up time point standard anteroposterior radiographs of the pelvis and lateral radiographs of the femur were acquired for all patients. Complications were recorded, including loosening, fracture, infection, heterotopic ossification, lateral femoral cutaneous nerve injury, and revision. Hip function was evaluated using the Harris Hip Score (HHS).
Definitions of descriptive variables
Revision was defined as exchange of a portion or the entire prosthesis, or removal of the prosthesis. Osteoporosis was defined as a bone mineral density T-score of ≤−2.5 at the femoral neck. The diagnosis of primary osteoporosis was made in accordance with a previously published description.8 Moreover, femoral component loosening was assessed in accordance with previously published criteria.8,9 Heterotopic ossification was graded using the Brooker classification system.10 Implant failure was defined as any condition that required revision surgery with an exchange of the implant. Lateral femoral cutaneous nerve injury was defined as numbness and/or burning sensation on the anterolateral thigh.11
Statistical analysis
Statistical analysis was performed using SPSS Version 24.0 (SPSS Inc., Chicago, IL, USA). Independent-samples t-tests were used to compare continuous variables between groups; these were expressed as mean ± standard deviation. Categorical variables were analyzed by using the chi-squared test or Fisher’s exact test, where appropriate. Two-tailed, unpaired t-tests were used to evaluate differences between the two groups; two-tailed, paired t-tests were used to detect changes between preoperative and postoperative outcome scores. The level of significance was set at p < 0.05.
Results
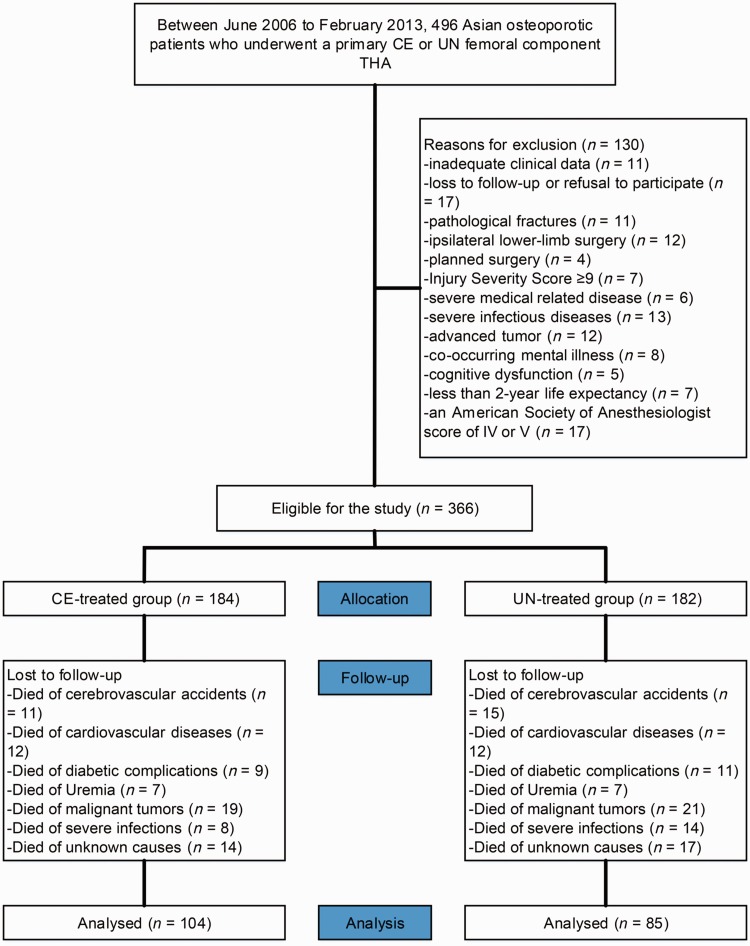
In total, 496 Asian patients with osteoporosis who underwent primary CE or UN THA were assessed for inclusion in the study. Of these, 366 patients (CE-treated group: n = 184; mean age, 71.3 ± 8.2 years and UN-treated group: n = 182; mean age, 71.7 ± 7.8 years), for whom all relevant information was available, met the inclusion criteria. The mean follow-up period was 75 months (range, 65–86 months). No statistically significant differences were detected in postoperative mortality between groups. The study flow chart is shown in Figure 1, and the included patients’ demographics are presented in Table 1.
Figure 1.
Flow diagram demonstrating methods for identification of studies to compare long-term clinical and radiological outcomes of primary unilateral uncemented (UN) or cemented (CE) femoral component total hip arthroplasty (THA) in the elderly with osteoporosis, and reasons for exclusion.
Table 1.
Patient demographics and outcomes.
| Variable | CEa (n = 184) | UNa (n = 182) | p-value |
|---|---|---|---|
| Sex, No. male/female | 70/114 | 64/118 | 0.568*,b |
| Age (years) | 71.3 ± 8.2 | 71.7 ± 7.8 | 0.105*,c |
| Body mass index (kg/m2) | 27.4 ± 8.0 | 26.8 ± 9.5 | 0.139*,c |
| Bone mineral density | −3.8 ± 0.3 | −3.8 ± 0.5 | 0.154*,c |
| Side, No. left/right | 87/97 | 83/99 | 0.748*,b |
| Comorbidities | 0.935*,d | ||
| Hypertension | 43 | 47 | |
| Diabetes mellitus | 32 | 37 | |
| Hyperlipidemia | 54 | 58 | |
| Underlying diagnoses for primary total hip arthroplasty | 0.872*,d | ||
| Osteoarthritis | 44 | 46 | |
| Posttraumatic arthritis | 32 | 27 | |
| Femoral neck fractures | 40 | 41 | |
| Avascular necrosis | 40 | 36 | |
| Rheumatoid arthritis | 28 | 32 | |
| Sequela of developmental hip dysplasia | 8 | 10 | |
| ASA Index | 0.892*,d | ||
| 1 | 45 | 40 | |
| 2 | 86 | 92 | |
| 3 | 53 | 50 | |
| Preoperative Harris Hip Score | 55.2 ± 12.7 | 54.8 ± 11.6 | 0.103*,c |
| Follow-up period (months) | 75.3 ± 9.7 | 75.7 ± 10.4 | 0.087*,c |
*Not statistically significant.
aStryker Corporation, Kalamazoo, MI, USA; bAnalyzed using the chi-squared test; cAnalyzed using an independent-samples t-test; dAnalyzed using the Mann-Whitney test. UN: uncemented; CE: cemented; ASA: American Society of Anesthesiologists.
Functional outcomes
More than 69% of patients who underwent primary UN or CE THA had acceptable functional scores at the final follow-up. At 1 month after surgery, no significant difference between groups was detected. From 3 months after surgery to the final follow-up, HHS was consistent superior in the CE group, as shown in Table 2. A total of 32% of UN-treated patients reported a degree of hip pain in the resting state; this proportion increased to 47% in the active state. Notably, severe pain was frequently reported in the UN group. A total of 21% of CE-treated patients described no or mild hip pain in the resting state; this proportion increased to 36% in the active state. However, there was no significant difference in mean pain score between groups at the final follow-up.
Table 2.
Medium-term follow-up functional outcome: Harris Hip Score.
| Follow-up duration (months postoperatively) | CEa (n = 184) | UNa (n = 182) | p-value |
|---|---|---|---|
| 1 | 80.3 ± 7.5 | 80.2 ± 7.7 | 0.247 |
| 3 | 83.2 ± 5.4 | 80.7 ± 6.4 | 0.024* |
| 6 | 84.2 ± 7.3 | 81.3 ± 5.4 | 0.017* |
| 9 | 85.2 ± 6.7 | 82.2 ± 7.1 | 0.015* |
| 12 | 85.4 ± 8.1 | 82.0 ± 6.6 | 0.031* |
| 18 | 85.3 ± 7.2 | 79.5 ± 9.3 | 0.002* |
| 24 | 86.2 ± 4.7 | 80.4 ± 9.6 | 0.001* |
| 30 | 85.7 ± 6.1 | 79.6 ± 5.3 | 0.001* |
| 36 | 83.7 ± 5.3 | 78.4 ± 9.7 | 0.025* |
| 42 | 80.6 ± 7.4 | 76.4 ± 8.2 | 0.032* |
| 48 | 79.5 ± 3.9 | 75.0 ± 8.8 | 0.027* |
| 54 | 78.4 ± 7.9 | 74.7 ± 8.8 | 0.021* |
| 60 | 77.3 ± 9.5 | 74.6 ± 9.8 | 0.026* |
| Final follow-up | 76.9 ± 8.2 | 70.6 ± 10.0 | 0.000* |
*Statistically significant.
aStryker Corporation, Kalamazoo, MI, USA. UN: uncemented; CE: cemented.
Radiographic outcomes
The major imaging results were prosthetic loosening that could not be adjusted or repaired in a non-surgical setting; periprosthetic fracture; lower limb shortening (>1.5 cm); and implant failure (Table 3). The respective prosthetic loosening rates in the UN and CE groups were 26.4% and 16.8% at a minimum of 5 years (p = 0.027). There was a significant difference in the rate of early revision at the final follow-up (7.6% CE vs. 14.8% UN, p = 0.028). Approximately 39.2% of UN THAs were revised for femoral loosening, compared with 21% of CE THAs (p = 0.033). Early failure following loosening occurred more frequently in UN THAs than in CE THAs (p = 0.031).
Table 3.
Medium-term follow-up radiographic outcomes: 5-year assessment.
| Variable | CEa (n = 184) | UNa (n = 182) | p-value |
|---|---|---|---|
| Prosthetic loosening | 31 (16.8%) | 48 (26.4%) | 0.027*,b |
| Prosthetic Revision | 14 (7.6%) | 27 (14.8%) | 0.028*,b |
| Periprosthetic fracture | 3 (1.6%) | 3 (1.6%) | 0.989 |
| Femur shaft fracture | 6 (3.3%) | 5 (2.7%) | 0.774 |
| Lower limb shortening (>1.5 cm) | 1 (0.5%) | 7 (3.8%) | 0.097 |
| Heterotopic ossification | 6 (3.3%) | 6 (3.3%) | 0.985 |
*Statistically significant.
aStryker Corporation, Kalamazoo, MI, USA; bAnalyzed using the chi-square test. N: uncemented; CE: cemented.
Discussion
In this study involving elderly patients with osteoporosis, UN THA resulted in an increased rate of early revision, compared with the rate following CE THA. UN THA was associated with lower HHS, compared with that observed in patients who underwent CE THA. Our study suggests that CE THA was superior to UN THA, with regard to early revision and HHS for elderly patients with primary osteoporosis.
Our findings were consistent with those of previous studies.1–3,12 A large meta-analysis suggested that CE THA exhibited equivalent or greater effectiveness, compared with UN THA, in elderly patients with osteoporosis.13 Significant improvement in HHS was observed in patients who underwent CE THA, because the rate of early revision was significantly lower than that observed in patients who underwent UN THA. Although significantly greater incidences of adverse events and reduced health-related quality of life were observed among patients who underwent UN THA, rapid recovery was also observed in these same patients; moreover, there was no difference in HHS between groups at 1 month postoperatively. Based on the increasing incidence of adverse events, the optimal surgical regimen has been controversial.5,6,14 A retrospective, single-center study15 showed that CE THA was superior to UN THA with respect to early revision and HHS; this was consistent with the findings of our study. Despite the potential benefits of CE THA regarding early revision and HHS, an increasing (but limited) body of literature5 has suggested that significantly higher rates of early revision occur following CE THA among patients with osteoporosis in other hospital settings.
Since the development of artificial joints, controversy regarding CE vs. UN femoral components in THA has been an important issue in the field of prosthesis replacement.16 The principles of CE fixation and low friction associated with metal-polyethylene have been important in the development of modern THA.3 Mechanical stability of the interface is achieved through bulk filling of bone cement between the prosthesis and bone, as well as by microscopic interlocking.11 Failure of CE THA is generally considered to be the primary cause of medium-term artificial joint loosening, and the concept of “bone cement disease” has been proposed.14,17 CE THA technology has been continuously improved and developed, particularly through vacuum centrifugal stirring, pulse irrigation, cement gun pressure, and the application of the 4th-generation cement technology; these changes have enhanced the medium-term clinical efficacy of THA.15,18 CE THA remains the gold standard for assessing other new prosthetic replacement approaches; moreover, early weight-bearing can be achieved following CE THA.8
Although CE THA has been particularly successful, the subsequent incidence of prosthetic loosening has remained high among young and active patients.5,19 Thus, UN THA emerged to address this limitation; this approach relies on fixation through compression between prosthesis and bone.8,19 Therefore, initial stability primarily relies on the degree of matching between prosthesis and bone; in contrast, subsequent stability primarily relies on the “healing” effect.5,20 The biological fixation effect is attained through bone integration, which is achieved by tight compression and bone ingrowth between the prosthesis and bone tissue.1,8 UN THA failure occurs as a result of multiple factors, including material selection, prosthesis design, and interface fixing method.2,21 The underlying cause of early failure is generally attributed to insufficient initial stability of the interface.16 Because the initial stability of UN THA depends primarily on fixation between the prosthesis and bone, selection of suitable patients is needed, in combination with the use of an appropriate prosthesis and effective surgical techniques.6,11 Following changes in prosthesis design and surface coating technology, short-term and medium-term success of UN THA have led to wide acceptance among clinicians.5,22 However, clinical follow-up beyond 5 years demonstrated that, although biological fixation resolves some of the problems caused by bone cement, medium-term prosthesis-related loosening and osteolysis remain problematic for patients. Furthermore, the incidence rate of prosthesis-related loosening and osteolysis after UN THA is comparable with that after CE THA.8,23
The rate of prosthesis revision following THA is the most important index for evaluating postoperative efficacy.8,24 Berend et al.25 performed a statistical analysis of 2551 patients who underwent THA; they showed that, following proximal femoral fracture, rates of femoral component survival were 95.8% for uncemented stems and 91.7% for cemented stems. The main reason for this difference in rate of revision may be the superior performance of the UN acetabular cup; notably, the rate of revision of the UN femoral component may be high due to loosening and periprosthetic fractures within 2 years after surgery.
Regarding postoperative pain score, our results showed that early pain improvement in patients who underwent CE THA was better than that of patients who underwent UN THA. Furthermore, there was no significant difference over time in pain between the groups. This may be because CE THA tends to achieve immediate stability after surgery due to good bone-cement-prosthesis integration; patients were thus inclined to achieve early weight-bearing, which allowed early and more perceptible improvement in pain. However, for UN THA, early fixation stability relies mainly on good pressure distribution between prosthesis and bone;5,21 biological stability requires the ingrowth of bone tissue or inlay on the prosthesis;2 thus, firm stability is achieved over time,1,24 and pain improvement may be slow and prolonged.
This study should be interpreted in light of important limitations. First, we may have failed to address all potentially confounding variables in our analyses. Second, this was a retrospective study that involved all problems inherent with such methodology. Patient- and surgeon-related confounding factors may have existed, but both groups were well-matched; this allowed us to draw conclusions that were not associated with the patients’ demographics.
In conclusion, the rate of revision and HHS among patients who underwent CE THA were better than those of patients who underwent UN THA, in this cohort of elderly Asian patients with osteoporosis. Thus far, there remains controversy regarding the selection of THA approach; considerations should include the patient's age, life expectancy, and activity level, as well as the surgeon’s skill level, to achieve optimal efficacy. This study had several limitations; however, our results were consistent with those of previous meta-analyses of randomized controlled trials in this field.22
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received funding from the Shanghai Municipal Health and Family Planning Commission Fund Project (Grant No. 201640057), and the National Natural Science Foundation of China (Grant No. 81770876; 81270011; 81472125).
References
- 1.Rahman WA, Kazi HA, Gollish JD. Results of single stage exchange arthroplasty with retention of well fixed cement-less femoral component in management of infected total hip arthroplasty. World J Orthop 2017; 8: 264–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costi K, Solomon LB, McGee MA, et al. Advantages in using cemented polished tapered stems when performing total hip arthroplasty in very young patients. J Arthroplasty 2017; 32: 1227–1233. [DOI] [PubMed] [Google Scholar]
- 3.Clarke-Jenssen J, Westberg M, Roise O, et al. Reduced survival for uncemented compared to cemented total hip arthroplasty after operatively treated acetabular fractures. Injury 2017; 48: 2534–2539. [DOI] [PubMed] [Google Scholar]
- 4.Hoskins W, van Bavel D, Lorimer M, et al. Polished cemented femoral stems have a lower rate of revision than matt finished cemented stems in total hip arthroplasty: an analysis of 96,315 cemented femoral stems. J Arthroplasty 2018; 33: 1472–1476. [DOI] [PubMed] [Google Scholar]
- 5.Makela K, Eskelinen A, Pulkkinen P, et al. Cemented total hip replacement for primary osteoarthritis in patients aged 55 years or older results of the 12 most common cemented implants followed for 25 years in the Finnish arthroplasty register. J Bone Joint Surg Br 2008; 90: 1562–1569. [DOI] [PubMed] [Google Scholar]
- 6.Sukeik M, Patel S, Haddad FS. Aggressive early debridement for treatment of acutely infected cemented total hip arthroplasty. Clin Orthop Relat Res 2012; 470: 3164–3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lovell TP. Single-incision direct anterior approach for total hip arthroplasty using a standard operating table. J Arthroplasty 2008; 23: 64–68. [DOI] [PubMed] [Google Scholar]
- 8.Soen S, Fukunaga M, Sugimoto T, et al. Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab 2013; 31: 247–257. [DOI] [PubMed] [Google Scholar]
- 9.Temmerman OPP, Raijmakers P, Berkhof J, et al. Accuracy of diagnostic imaging techniques in the diagnosis of aseptic loosening of the femoral component of a hip prosthesis - A meta-analysis. J Bone Joint Surg Br 2005; 87: 781–785. [DOI] [PubMed] [Google Scholar]
- 10.Brooker AF, Bowerman JW, Robinson RA, et al. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 1973; 55: 1629–1632. [PubMed] [Google Scholar]
- 11.Chen M, Luo Z, Ji X, et al. Direct anterior approach for total hip arthroplasty in the lateral decubitus position: our experiences and early results. J Arthroplasty 2017; 32: 131–138. [DOI] [PubMed] [Google Scholar]
- 12.Smabrekke A, Espehaug B, Havelin LI, et al. Operating time and survival of primary total hip replacements - An analysis of 31745 primary cemented and uncemented total hip replacements from local hospitals reported to the Norwegian Arthroplasty Register 1987-2001. Acta Orthop Scand 2004; 75: 524–532. [DOI] [PubMed] [Google Scholar]
- 13.Wang JX, Zhu C, Cheng T, et al. A systematic review and meta-analysis of antibiotic-impregnated bone cement use in primary total hip or knee arthroplasty. PLoS One 2013; 8: e82745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sierra RJ, Timperley JA, Gie GA. Contemporary cementing technique and mortality during and after Exeter total hip arthroplasty. J Arthroplasty 2009; 24: 325–332. [DOI] [PubMed] [Google Scholar]
- 15.Hui Z, Pei FX, Shen B, et al. Total hip arthroplasty with a cementless acetabular component and a cemented femoral component in the treatment of Chinese patients with femoral head necrosis. J Arthroplasty 2008; 23: 1022–1030. [DOI] [PubMed] [Google Scholar]
- 16.Wang L, Lei PF, Xie J, et al. Medium-term outcomes of cemented prostheses and cementless modular prostheses in revision total hip arthroplasty. Sci Rep 2013; 3: 2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mata-Fink A, Philipson DJ, Keeney BJ, et al. Patient-reported outcomes after revision of metal-on-metal total bearings in total hip arthroplasty. J Arthroplasty 2017; 32: 1241–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angerame MR, Fehring TK, Masonis JL, et al. Early failure of primary total hip arthroplasty: is surgical approach a risk factor? J Arthroplasty 2018; 33: 1780–1785. [DOI] [PubMed] [Google Scholar]
- 19.Temmerman OPP, Raijmakers P, Berkhof J, et al. Diagnostic accuracy and interobserver variability of plain radiography, subtraction arthrography, nuclear arthrography, and bone scintigraphy in the assessment of aseptic femoral component loosening. Arch Orthop Trauma Surg 2006; 126: 316–323. [DOI] [PubMed] [Google Scholar]
- 20.Lichtinger TK, Schürmann N, Müller RT. [Early loosening of a cemented hip endoprosthesis stem of titanium]. Unfallchirurg 2000; 103: 956–960. [DOI] [PubMed] [Google Scholar]
- 21.Watts CD, Abdel MP, Hanssen AD, et al. Anatomic hip center decreases aseptic loosening rates after total hip arthroplasty with cement in patients with Crowe type-II dysplasia: a concise follow-up report at a mean of thirty-six years. J Bone Joint Surg Am 2016; 98: 910–915. [DOI] [PubMed] [Google Scholar]
- 22.Corten K, Bourne RB, Charron KD, et al. What works best, a cemented or cementless primary total hip arthroplasty? Minimum 17-year follow-up of a randomized controlled trial. Clin Orthop Relat Res 2011; 469: 209–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Conroy JL, Chawda M, Kaushal R, et al. Does use of a “Rim Cutter” improve quality of cementation of the acetabular component of cemented Exeter total hip arthroplasty? J Arthroplasty 2009; 24: 71–76. [DOI] [PubMed] [Google Scholar]
- 24.Konopka JF, Buly RL, Kelly BT, et al. The effect of prior hip arthroscopy on patient-reported outcomes after total hip arthroplasty: an institutional registry-based, matched cohort study. J Arthroplasty 2018; 33: 1806–1812. [DOI] [PubMed] [Google Scholar]
- 25.Berend ME, Smith A, Meding JB, et al. Long-term outcome and risk factors of proximal femoral fracture in uncemented and cemented total hip arthroplasty in 2551 hips. J Arthroplasty 2006; 21: 53–59. [DOI] [PubMed] [Google Scholar]