Short abstract
Objective
We aimed to assess knowledge, attitudes, and practices regarding breast and cervical cancer and screening methods among women living western Turkey.
Methods
A questionnaire survey was administered to women aged ≥21 years. Data were collected using a 12-item questionnaire measuring women's knowledge, attitudes, and practice levels, including among participants who were health workers.
Results
A total 668 women were included in the study. The average age was 37.48 ± 11.85 years. Most women had a primary-level education (43.4%) and most (50.3%) were homemakers; 27.1% of participants were health care workers. The differences in age, education, and occupation among participants were evaluated according to whether participants perform breast self-examination and have undergone Pap testing. The distribution of women according to age group showed that with increased age, the frequency of performing these two behaviors decreased, with women over 55 years old accounting for a significantly higher proportion than other age groups.
Conclusions
In our study, the level of knowledge and attitudes regarding breast and cervical cancers among women was similar to that in previous studies and was higher than expected, especially among women who were health workers. However, all women had inadequate frequency of performing screening tests.
Keywords: Knowledge, attitudes, breast cancer, cervical cancer, screening, women
Introduction
According to the World Health Organization's (WHO) World Cancer Report published in 2008, breast cancer is one of the most common cancers among women globally. The disease accounts for 23%–25% of all cancers in women and 1.1 million new cases of breast cancer occur each year.1,2 Breast cancer incidence increases by 1%–2% annually worldwide, and about 410.000 women globally die from this disease.3 With early identification and appropriate treatment, the survival rate for breast cancer is high.4 Breast self-examination (BSE) is recommended for early recognition of breast cancer by many experts around the world. BSE is recommended as an effective method for the early diagnosis of breast cancer if performed regularly each month. BSE has the advantage of being easy to apply at home, thereby representing a cost-free method for the early recognition of disease.5–7
It has been reported that 90% of breast cancers are first recognized by the patient herself. Nevertheless, whether BSE is useful for early detection of breast cancer is still debated. In some countries, including Turkey, breast cancer is the leading cancer among women and the age of occurrence is gradually decreasing. Breast cancer is an important public health problem because it can lead to death, yet such outcomes can be avoided by early detection. After the age of 20 years, BSE is an important component of early detection for breast cancer. For women living in regions with limited accessibility to screening facilities, performing BSE in a consistent and correct manner is beneficial.8,9
Cervical cancer is another major health problem among women. Routine screening of cervical cancer is recommended for women older than 20 years of age.10 Every year, around 500.000 new cases are diagnosed worldwide and 274.000 women die owing to cervical cancer.11,12 Screening programs for cervical cancer have been implemented in developing countries for decades and have been shown to be effective in reducing mortality from this disease.13
In this study, we aimed to investigate women's knowledge and attitudes regarding cancer risk and secondary and primary prevention, as well as their related health behaviors. In addition, we conducted comparisons with the knowledge, attitudes, and practice among participants who were health workers. Health care workers have an important role in helping to increase public awareness of disease prevention, together with other occupational groups. We believe that health care workers have incomplete knowledge regarding breast and cervical cancers, which can affect all of society. Thus, we aimed to determine whether there is a lack of information and practice among health workers, as well as a general population of women in Turkey.
Materials and methods
All participants gave their verbal informed consent to participate in this study. Thereafter, questionnaires prepared by the investigators were administered in a personal interview. In the first part of the questionnaire, we collected sociodemographic data of participants. The second part of the questionnaire included questions about breast and cervical cancer knowledge; the last part of the survey queried attitudes and behaviors regarding BSE, gynecological examination, mammography and ultrasonography, Pap testing, as well as sexual activity.
For this study, we recruited women who were or had been sexually active, aged 21 years or older, and who attended the Family Medicine Polyclinic between October and December in 2015. Women who had previously been diagnosed with cervical cancer or breast cancer were excluded from the study. We collected information about participants’ age, education, occupation, and level of knowledge and attitudes about breast and cervical cancer, as well the frequency of undergoing Pap testing or breast examination at a clinic. We obtained approval for this study from the Dumlupınar University Local Ethics Board (decision number 2015/12) and all required ethics committees.
Statistical analysis
Continuous data are given as mean ± standard deviation (SD). Categorical data are given as percentage (%). The Shapiro–Wilk test was used to investigate the normal distribution of the data. Statistical significance between women and health workers was analyzed using Mann–Whitney U tests. The Kruskal–Wallis H test was used to analyze the cases for three or more groups. Pearson chi-square, Pearson exact chi-square, and Fisher's chi-square tests were used to analyze the cross tabulations. IBM SPSS version 21.0 was used for analyses (IBM Corp., Armonk, NY, USA). Differences were considered significant at P < 0.05.
Results
The total study population included 668 women, with average age 37.48 ± 11.85 (range, 20–69) years. A total 22.9% of participants were university graduates and 7% were illiterate. Most (50.5%) participants in our study were homemakers and 27.1% were health care workers. The sociodemographic characteristics of participants are summarized in Table 1.
Table 1.
Sociodemographic characteristics.
| N | % | |
|---|---|---|
| Age (y) | ||
| <25 | 112 | 16.8 |
| 25–34 | 223 | 33.4 |
| 35–44 | 162 | 24.3 |
| 45–54 | 105 | 15.7 |
| ≥55 | 66 | 9.9 |
| Education | ||
| Uneducated | 47 | 7.0 |
| Primary education | 290 | 43.4 |
| High school | 178 | 26.6 |
| University | 153 | 22.9 |
| Profession | ||
| Homemaker | 336 | 50.3 |
| Office worker | 151 | 22.6 |
| Health care worker | 181 | 27.1 |
| Total | 668 | 100 |
Differences in age, education, and occupation of participants were evaluated according to their performance of BSE and receiving a Pap test. We examined the distribution of women according to age group. We found that the above two behaviors decreased with increased age. This was particularly true for women over age 55 years, with a significantly higher proportion than for other age groups (P < 0.05), as shown in Table 2.
Table 2.
Comparison of sociodemographic characteristics among participants, according to BSE and Pap testing.
| Performs BSE |
Undergoes Pap testing |
|||
|---|---|---|---|---|
| Non (%) | Yesn (%) | Non (%) | Yesn (%) | |
| Age (y) | ||||
| <25 | 41 (36.6) | 71 (63.4) | 83 (74.1) | 29 (25.9) |
| 25–34 | 86 (42.2) | 118 (57.8) | 151 (74.0) | 53 (26.0) |
| 35–44 | 85 (47.0) | 96 (53.0) | 144 (79.6) | 37 (20.4) |
| 45–54 | 55 (52.4) | 50 (47.6) | 88 (83.8) | 17 (16.2) |
| ≥55 | 44 (66.7) | 22 (33.3) | 58 (87.9) | 8 (12.1) |
| P | 0.001 | 0.051 | ||
| Education | ||||
| Uneducated | 28 (59.6) | 19 (40.4) | 38 (80.9) | 9 (19.1) |
| Primary education | 132 (45.5) | 158 (54.5) | 233 (80.3) | 57 (19.7) |
| High school | 90 (50.6) | 88 (49.4) | 142 (79.8) | 36 (20.2) |
| University | 61 (39.9) | 92 (60.1) | 111 (72.5) | 42 (27.5) |
| P | 0.065 | 0.250 | ||
| Profession | ||||
| Homemaker | 149 (44.3) | 187 (55.7) | 262 (79.0) | 74 (22.0) |
| Office worker | 76 (50.3) | 75 (49.7) | 119 (78.8) | 32 (21.2) |
| Health care worker | 86 (47.5) | 95 (52.5) | 144 (79.6) | 37 (20.4) |
| P | 0.451 | 0.914 | ||
As participants’ education level increased, the frequency of performing BSE and undergoing Pap testing increased, but with no statistically significant difference (P > 0.05). When we examined the distribution of these health behaviors among women according to occupation, homemakers and health workers performed these practices more often, but with no significant difference (P > 0.05). The results of these analyses are presented in Table 2.
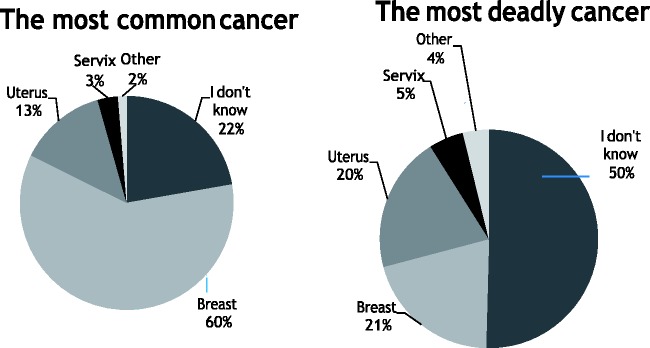
Figure 1 shows the percentage of participants who perform BSE and have undergone Pap testing according to their knowledge of these practices. Women with higher knowledge levels regarding BSE and Pap testing had significantly higher rates of performing both of these health behaviors (P < 0.001).
Figure 1.
Level of knowledge regarding BSE and Pap testing.
Percentage of participants who perform BSE and undergo Pap testing, according to their knowledge (*P < 0.001).
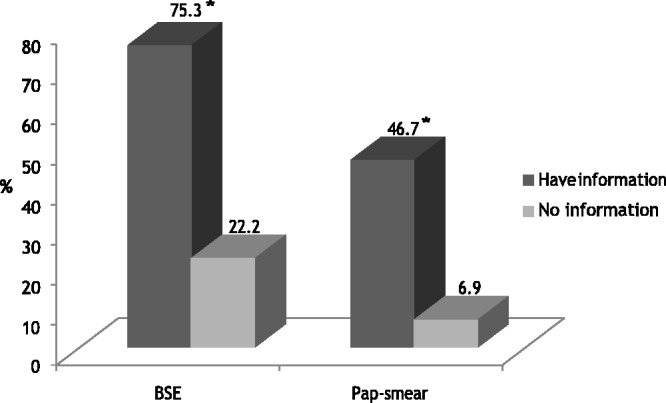
When participants were asked about the most common cancer and the most lethal cancer, breast cancer was the response given by 61.9% (n = 320) and 19.5% (n = 101) of participants, respectively (Figure 2).
Figure 2.
Knowledge about the most common cancer and the most lethal cancer.
When we queried sexual activity status, 77% of health workers and 78.3% of the remaining participants reported that they were sexually active. The difference between these groups was not significant (P > 0.05).
Interestingly, we observed that 52% of participants were primary and secondary school graduates, but only 15% of university graduates reported undergoing Pap testing. Among participants aged ≥40 years, the proportion who had received mammography and/or breast ultrasonography at least once was 12.6%.
We queried whether participants regularly attended a gynecology clinic; 82.6% (n = 551) of participants reported that they did not and only 17.4% (n = 117) reported having regular gynecological examinations. Most women who were regularly followed in gynecology outpatient clinics had lower educational levels, but this was not statistically significant.
Discussion
Breast cancer is the second leading and cervical cancer the fourth leading cancer-related cause of death worldwide.14 According to the WHO, in 2018 breast cancer was newly diagnosed in 2.1 million women and cervical cancer was newly diagnosed in 570,000 women.15 According to the literature, the incidences of breast and cervical cancer increase in women over aged ≥40 years.16,17 In women 50–75 years old, mortality from breast and cervical cancer is reduced by 25%–30% with routine mammography and Pap testing. In women aged ≥40 years, especially those with a high risk for breast cancer, BSE and screening mammography provide early detection with high accuracy. For this reason, monthly BSE, annual clinical examination, and mammographic screening every 2 years is recommended for women aged ≥40 years.16,17 Pap screening is recommended for all women aged 35–40 years at least once; the test is then repeated at intervals of 5 years. Screening can be terminated in women aged 70 years who have negative results in their previous three tests.18 In our study, BSE and Pap testing decreased significantly with increased age. The age-related decline in screening behaviors in health care workers among our study participants was similar to that in other participants. As health workers are a source of information about preventive health behaviors in the community, these results are concerning.
Previous studies show that women generally have insufficient knowledge about screening methods for breast and cervical cancer, and if they are knowledgeable about these, they do not regularly perform BSE or receive regular mammography.19,20 In our study, although the level of knowledge among participants was adequate, health screening behaviors were lacking. In this respect, our results are compatible with the literature.
Another study showed that 36% of women did not perform BSE, according to results of a questionnaire;21 the prevalence of BSE performed correctly was 6% among medical staff and 0.4% in the general population. In that study, there was a statistically significant difference among level of education, socioeconomic status, being a medical professional, and the prevalence of BSE.21 In our study, we determined that about half of health professionals (43.8%) did not undergo regular mammography and/or breast ultrasonography; the fact that most health workers in our study were under 40 years of age is thought to be a factor in these findings.
Özçam et al. noted that about one-third of women who were specialist physicians and half of those who were nurses had never undergone any breast cancer screening tests.21 It is known that female health workers, who serve as models for the population at each step of their occupational life, do not undergo early diagnostic testing for several reasons, such as “forgetting”, “finding it unnecessary”, or “lacking the time”.22
In our study, the rates of cancer screening were generally low. When we evaluated health care workers separately, the rate of breast cancer screening remained low. In similar studies in Turkey, it has been reported that female health care workers, who are expected to have greater awareness about this issue, very rarely undergo gynecological examination.23
Conclusion
Our findings showed that the level of knowledge about breast and cervical cancer among our population of women in Turkey was similar to that of previous studies and was higher than expected, especially for health workers. However, all women had inadequate rates of performing screening tests. Our results suggest that the rate of Pap testing has decreased, regardless of education level. Therefore, it is important to regularly provide preventive cancer education regardless of professional group or education level, to increase community awareness about breast and cervical cancers.
Acknowledgments
The author wish to thank the study participants for their contribution to the research and Ceylan Ayada for her professional support in preparation of the manuscript.
Declaration of conflicting interest
The author declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Boyl P, Levin B. World cancer report. International Agency for Research on Cancer 2008; 4: 1–512. [Google Scholar]
- 2.Yaban Z, Ergin A. Breast cancer and integrative medicine approaches. Turkiye Klinikleri J Obstet Womens Health Dis Nurs-Special Topics 2017; 3: 134–140. http://www.turkiyeklinikleri.com/article/en-meme-kanseri-ve-integratif-tedavi-yaklasimlari-79264.html [Google Scholar]
- 3.Altunkan H, Akın B, Ege E. Self breast examination practice behaviors and awareness levels of women aged 20-60 years. J Breast Health 2008; 4: 84–91. [Google Scholar]
- 4.Kenyon M, Mayer DK, Owens AK. Late and long-term effects of breast cancer treatment and surveillance management for the general practitioner. J Obstet Gynecol Neonatal Nurs 2014; 43: 382–398. [DOI] [PubMed] [Google Scholar]
- 5.Kutlu R, Biçer Ü. Evaluation of breast cancer risk levels and its relation with breast self-examination practices in women. J Breast Health 2017; 13: 34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doshi D, Reddy S, Kulkarni S, et al. Breast self-examination: knowledge, attitude, and practice among female dental students in Hyderabad City, India. Indian J Palliat Care 2012; 18: 68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma P, Dillu R. Study to assess the knowledge and attitude about breast cancer and breast self examination among women of 20-50 years of age in a selected hospital of Haryana. IJSR 2017; 6: 270–277. [Google Scholar]
- 8.Bodapati SL, Babu GR. Oncologist perspectives on breast cancer screening in India- results from a qualitative study in Andhra Pradesh. Asian Pac J Cancer Prev 2013; 14: 5817–5823. [DOI] [PubMed] [Google Scholar]
- 9.Franek GA, Nowak-Kaputsa ZE, Cabaj M. Breast cancer prophylaxis among nurses. Wiad Lek 2004; 57: 82–84. [PubMed] [Google Scholar]
- 10.ICO Information Centre on HPV and cancer. Human Papillomavirus and Related Diseases in India Summary Report. 2014.
- 11.Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. Cancer J Clin 2005; 55: 74–108. [DOI] [PubMed] [Google Scholar]
- 12.Güner H, Taşkıran Ç. Cervical cancer epidemiology and human papilloma virüs. Turk J Obstet Gynecol 2007; 4: 11–19. http://www.tjoddergisi.org/archives/archive-detail/article-preview/epdemology-of-cervcal-cancer-and-the-role-of-human/9500 [Google Scholar]
- 13.Jusman Y, Ng SC, Abu Osman NA. Intelligent screening systems for cervical cancer. Sci World J 2014; 2014: 810368 10.1155/2014/810368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bray F, Ferlay J, Soerjomwataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J 2018; 68: 394–424. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. World Cancer Rep 2018.
- 16.Kimmick GG, Balducci L. Breast cancer and aging. Hematol Oncol Clin North Am 2000; 14: 213–233. [DOI] [PubMed] [Google Scholar]
- 17.Kimmick GG, Muss HB. Breast cancer in older patients. Semin Oncol 2004; 31: 234–248. [DOI] [PubMed] [Google Scholar]
- 18.Dickinson J, Tsakonas E, Conner Gorber S, et al. Recommendations on screening for cervical cancer. CMAJ 2013; 185: 35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lostao L, Joiner T, Pettit JW, et al. Health be liefs and illness attitudes as predictors of breast cancer screening attendance. Eur J Public Health 2001; 11: 274–279. [DOI] [PubMed] [Google Scholar]
- 20.Dewal L. Testicular and breast self-examination knowledge and practices of certified athletic trainers and these condary prevention of such cancers in intercollegiate student-athletes. Am J Health Stud 2006; 21: 28–35. [Google Scholar]
- 21.Özçam H, Cimen G, Uzuncakmak C, et al. Evaluation of the knowledge, attitude, and behavior of female health workers about breast cancer, cervical cancer, and routine screening tests. İstanbul Med J 2014; 15: 154–160. [Google Scholar]
- 22.Coskun S, Can H, Turan S. Knowledge about cervical cancer and Pap smear testing behavior among Turkish primary health care workers. APJCP 2013; 14: 6389–6392. 10.7314/APJCP.2013.14.11.6389 [DOI] [PubMed] [Google Scholar]
- 23.Can H, Erdem O, Oztekin C, et al. Are primary health care workers aware of cervical cancer risk? Asian Pac J Cancer Prev 2014; 15: 6669–6671. [DOI] [PubMed] [Google Scholar]